Abstract
Infection with human papillomaviruses (HPVs) characterizes a distinct subset of head and neck squamous cell cancers (HNSCCs). HPV-positive HNSCC preferentially affect the oropharynx and tonsils. Localized HPV-positive HNSCCs have a favorable prognosis and treatment outcome. However, the impact of HPV in advanced or metastatic HNSCC remains to be defined. In particular, it is unclear whether HPV modulates the response to cetuximab, an antibody targeting the epidermal growth factor receptor (EGFR), which is a mainstay of treatment of advanced HNSCC. To this end, we have examined the sensitivity of HPV-positive and -negative HNSCC models to cetuximab and cytotoxic drugs in vitro and in vivo. In addition, we have stably expressed the HPV oncogenes E6 and E7 in cetuximab-sensitive cancer cell lines to specifically investigate their role in the antibody response. The endogenous HPV status or the expression of HPV oncogenes had no significant impact on cetuximab-mediated suppression of EGFR signaling and proliferation in vitro. Cetuximab effectively inhibited the growth of E6- and E7-expressing tumors grafted in NOD/SCID mice. In support, formalin-fixed, paraffin-embedded tumor samples from cetuximab-treated patients with recurrent or metastatic HNSCC were probed for p16INK4a expression, an established biomarker of HPV infection. Response rates (45.5% versus 45.5%) and median progression-free survival (97 versus 92 days) following cetuximab-based therapy were similar in patients with p16INK4A-positive and p16INK4A-negative tumors. In conclusion, HPV oncogenes do not modulate the anti-EGFR antibody response in HSNCC. Cetuximab treatment should be administered independently of HPV status.
Keywords: HNSCC, cetuximab, HPV, resistance, EGFR, ADCC
Squamous cell carcinomas of the head and neck (HNSCC) are the sixth most common cancer entity. Globally 600 000 patients per year are newly diagnosed. The most important risk factors for HNSCC development are tobacco smoking and alcohol consumption. Recently, human papilloma virus (HPV)-associated HNSCC has been described as a distinct clinical entity with preferential tumor localization in the oropharynx, and strong association with ethnical background and risk behavior.1 Depending on the patient population that was studied up to 40% of HNSCC are associated with HPV infection.2, 3, 4, 5, 6, 7 The viral oncoproteins E5, E6 and E7 are main players in HPV-associated carcinogenesis. Although E6 induces proteasomal degradation of the tumor-suppressor p53, thereby compromising cell-cycle arrest and apoptosis, E7 overrides cell cycle checkpoints at the level of cyclin-dependent kinase inhibitors and the retinoblastoma tumor-suppressor protein (pRb).8, 9, 10 As pRb represses the transcription of the INK4A gene, HPV infection leads to increased expression of the p16INK4A gene product, a cyclin-dependent kinase inhibitor. Accordingly, high p16INK4A expression has been established as surrogate marker for HPV infection in tumors.11, 12, 13 The oncoprotein E5 was reported to promote proliferation by increasing membrane expression of the epidermal growth factor receptor (EGFR) through inhibition of its internalization and degradation.14
EGFR expression is detected in more than 90% of HNSCC, and high EGFR levels were associated with dismal prognosis.15, 16 Current data on the interaction of HPV status, EGFR expression and EGFR-mediated signaling are inconsistent.15, 16, 17, 18 Patients with localized HNSCC are treated with surgery and radiation therapy.19, 20, 21 Of all patients with localized HNSCC, those patients with HPV-positive tumors have more favorable outcomes.22 Radiotherapy of HNSCC is more effective when cytotoxic agents such as 5-fluorouracil (5FU) and cisplatin, or the anti-EGFR antibody cetuximab are simultaneously administered.19, 20, 21, 23, 24 Patients with relapsing or primary metastatic HNSCC are treated with cetuximab in combination with 5FU and cisplatin.25 Thus, the anti-EGFR antibody cetuximab is a highly important modality in the care of patients with locally advanced or metastatic HNSCC. Nevertheless, the impact of the HPV status on cetuximab response and treatment outcome in HNSCC still remains to be defined.
Against this background, we have studied the functional interaction of HPV oncogenes with the cetuximab response of HNSCC models in vitro and in vivo. In addition, we have analyzed the outcome of cetuximab treatment in a population of HNSCC patients in relation to intratumoral expression of p16INK4A, an established biomarker for HPV-positive cancers.11, 12, 13, 26, 27
Results
Functional impact of endogenous HPV status on the cetuximab response of HNSCC models
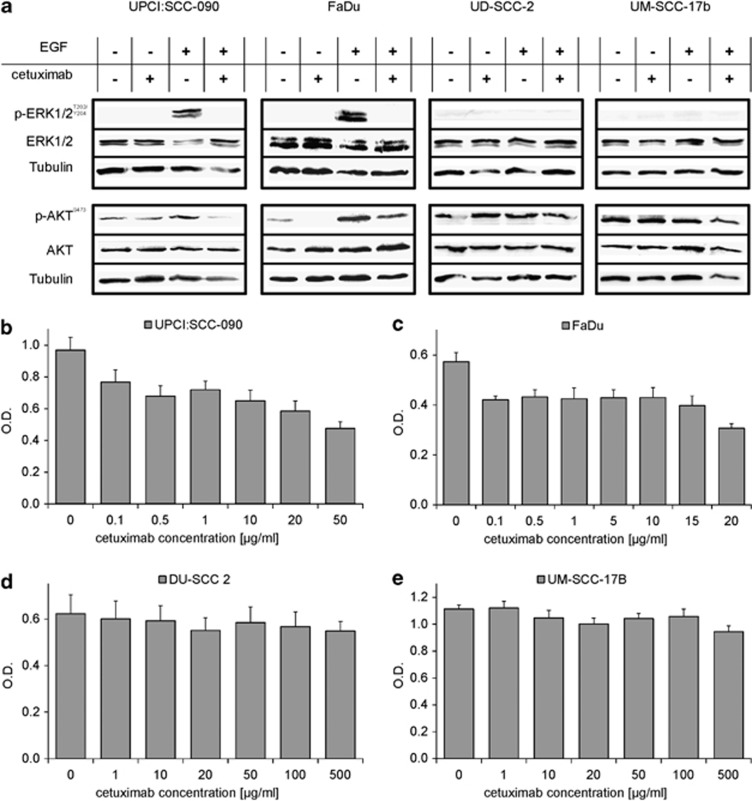
To study cetuximab responses at a functional level, we characterized the HPV-negative HNSCC cell lines FaDu and UM-SCC-17b, and the HPV-positive cell lines UPCI:SCC-090 and UD-SCC-2. The HPV status was confirmed by PCR-based detection of HPV E6 and E7 sequences in genomic DNA isolated from each cell line (Supplementary Figures 1A and B). Evaluating the expression pattern of the ERBB family receptors EGFR/HER1, HER2, HER3 and HER4 by flow cytometry failed to reveal a correlation with the HPV status (Table 1). Next, we studied the impact of cetuximab on the activation of the mitogen-activated protein kinase and phosphatidyl inositide-3 kinase pathways. In UPCI:SCC-090 (HPV-positive) and FaDu (HPV-negative) cells, cetuximab suppressed constitutive and EGF-induced phosphorylation of ERK and AKT (Figure 1a). In contrast, no such effect was observed in UD-SCC-2 (HPV-positive) and UM-SCC-17b (HPV-negative) cells, which both exhibited constitutive phosphorylation of AKT (Figure 1a). In conclusion, cetuximab treatment inhibited the proliferation of UPCI:SCC-090 and FaDu cells, but not of UD-SCC-2 and UM-SCC-17b cells (Figures 1b–e).
Table 1. Characterization of cellular models.
| Cell line | Origin | HPV status | HER1 (EGFR) expression | HER2 expression | HER3 expression | HER4 expression | Cetuximab sensitivity | Tumor-forming capacitiy in vivo |
|---|---|---|---|---|---|---|---|---|
| FaDu | HNSCC | − | ++ | + | + | − | ++ | + |
| UD-SCC-17B | HNSCC | − | ++ | + | + | − | − | − |
| UPCI:SCC-090 | HNSCC | + | + | + | + | − | ++ | + |
| DU-SCC-2 | HNSCC | + | + | (+) | − | − | − | − |
| DIFI | CRC | − | ++ | + | + | − | +++ | + |
| A431 | Epidermoid cell carcinoma | − | +++ | + | (+) | − | + | + |
−: negative; (+): weak positive; +: positive; ++: strong positive; +++: highest intensity
Figure 1.
Sensitivity of EGFR-positive cancer cell lines to the anti-EGFR antibody cetuximab in relation to HPV status. (a) Inhibition of constitutive and ligand-induced (EGF 10 ng/ml for 10 min) phosphorylation of ERK and AKT by cetuximab (1 μg/ml for 2 h) in HPV-positive UPCI:SCC-090 and HPV-negative FaDu cells. Note that ERK and AKT phosphorylation are unresponsive to EGF or cetuximab in UD-SCC-2 (HPV positive) and UM-SCC-17b (HPV-negative) cells. (b–e) The HPV-positive UPCI:SCC-090 and UD-SCC-2 and the HPV-negative FaDu and UM-SCC-17b HNSCC cell lines were grown in the presence of cetuximab at the indicated concentrations for 72 h (FaDu) or 96 h (UPCI:SCC-090, UD-SCC-2 and UM-SCC-17b). Optical density (OD; +s.d.) of formazan solution from three independent 3-[4,5–dimethylthiazol–2–yl]-2,5-diphenyl tetrazolium bromide assays is shown
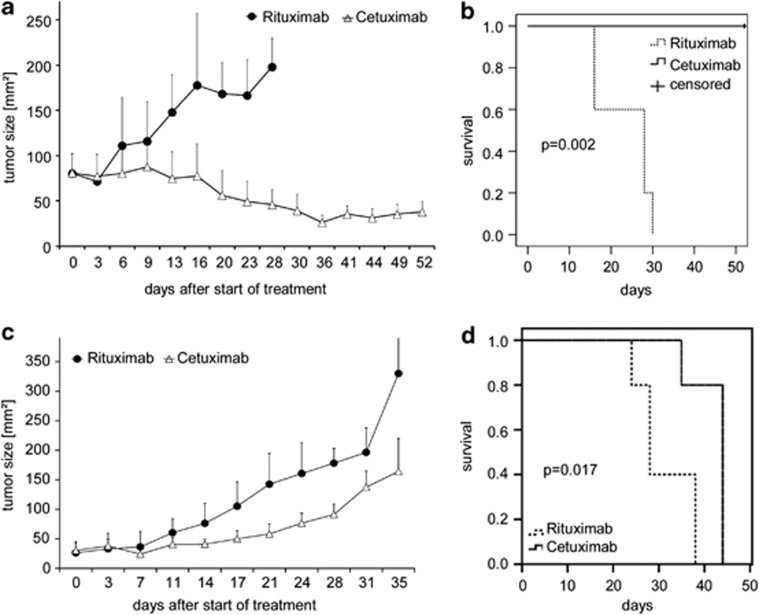
To extend this observation in an organismal context, we subcutaneously implanted HNSCC cells in immune compromised NOD/SCID mice. This model allows to study direct effects of cetuximab as well as cetuximab-mediated antibody-dependent cellular cytotoxicity in vivo.28 Tumors reproducibly developed within 14 days following the injection of HPV-negative FaDu or HPV-positive UPCI:SCC-090 cells. In contrast, UD-SCC-2 and UM-SCC-17b revealed no tumor-forming capacity in vivo (Table 1). Biweekly intraperitoneal injections of cetuximab (1 mg) induced remissions in NOD/SCID mice bearing established HPV-negative FaDu tumors, which resulted in a significantly prolonged survival as compared with treatment with the control antibody rituximab (Figures 2a and b). Also, mice bearing HPV-positive UCPI:SCC-090 tumors were responsive to cetuximab, which delayed tumor growth and prolonged survival as compared with the control antibody (Figures 2c and d). In summary, there was no apparent correlation between HPV status, expression levels of ERBB family receptors and cetuximab response of HNSCC models in vitro and in vivo.
Figure 2.
Effective treatment of established HPV-negative and HPV-positive tumors by treatment with cetuximab in vivo. Palpable flank tumors were established by subcutaneous injection of (a and b) FaDu (HPV-negative) or (c and d) UPCI:SCC-090 (HPV-positive) cells in NOD/SCID mice. After 14 days, tumor-bearing mice were treated twice weekly by intraperitoneal injections of cetuximab (1 mg, white triangles) or the control antibody rituximab (1 mg, black circles). (a and c) Tumor growth was monitored by palpation and quantified using a caliper. Mean bidimensional tumor sizes (+s.d.) of a representative experiment (five mice per treatment group) are given. (b and d) Kaplan–Meier plots of survival of tumor-bearing NOD/SCID mice. (b) HPV-negative FaDu; (d) HPV-positive UPCI:SCC-090. Mice were treated as in a and c with cetuximab (solid line), or the control antibody rituximab (dashed line). Cetuximab-treated mice exhibited a significantly prolonged survival as compared with rituximab-treated mice. In the FaDu model, median survival time for cetuximab-treated mice was not reached. It was 28 days for mice receiving rituximab (P=0.002, log rank test). In the UPCI:SCC-090 model, median survival time for cetuximab-treated mice was 44 days, and 28 days for rituximab-treated mice (P=0.017, log rank test)
Functional consequences of enforced HPV oncogene expression on cetuximab response
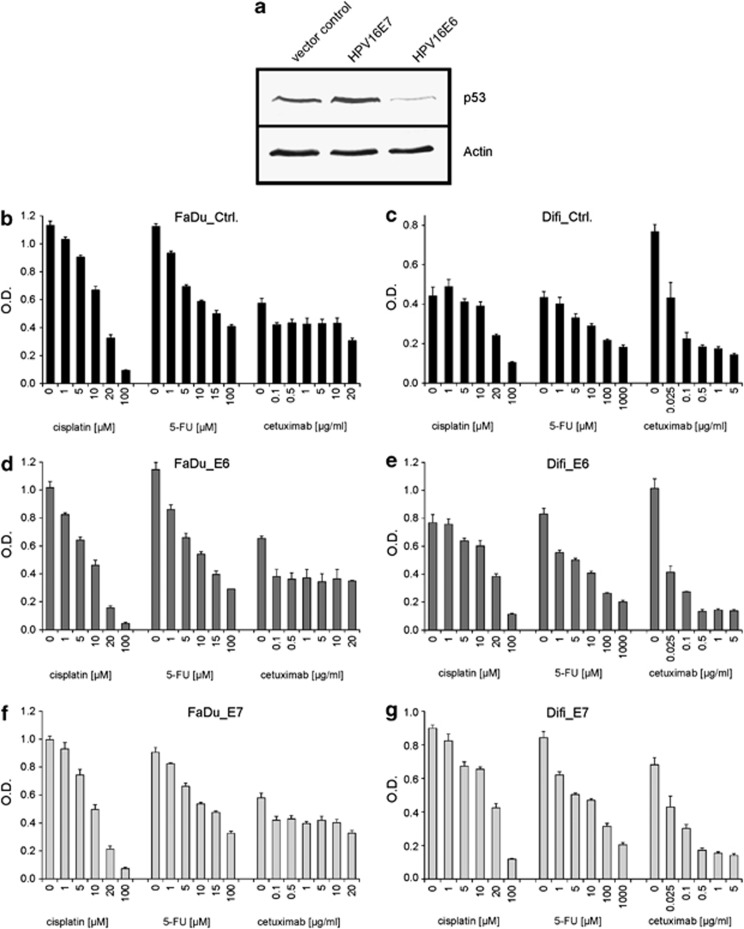
The outcome of experiments in cell lines with endogenous HPV positivity could be very well determined by cell-intrinsic factors in addition to HPV status. To unambiguously study the impact of HPV oncogenes on the cetuximab response, we stably expressed the human papilloma virus 16 (HPV16) oncogenes E6 and E7 in HPV-negative FaDu HNSCC cells. In addition, we studied the cancer cell lines Difi and A431, which we had previously characterized with respect to their cetuximab response.28 HPV E6 and E7 transgene expression and function were confirmed by PCR (Supplementary Figure 1B) and immunoblot analyses (Figure 3a). As expected, E6 expression significantly reduced the stability of the p53 tumor-suppressor protein, whereas E7 induced p53 accumulation, thus confirming the functional activity of both viral oncogenes.8, 10 FaDu, Difi and A431 cells expressing E6, E7 or a control vector showed similar antiproliferative responses upon treatment with cetuximab (Figures 3b and c and data not shown). Also, there was no impact of HPV oncogene expression on the sensitivity to cisplatin and 5FU, two main HNSCC drugs (Figures 3d–g).29
Figure 3.
The HPV oncogenes E6 and E7 do not modulate the cetuximab response of EGFR-positive cancer cells in vitro. The EGFR-positive cetuximab-sensitive cancer cell lines FaDu, Difi and A431 were retrovirally transduced to stably express the HPV16 oncogenes E6 and E7 or a control vector. (a) Increased and decreased p53 levels in response to expression of HPV16 E7 or E6. A representative immunoblot of FaDu cells is shown; similar results were obtained in Difi and A431 (not shown). (b–g) FaDu and Difi cells expressing HPV16 E6, E7 or a control vector (ctrl) were grown for 72 h in the presence of cetuximab, cisplatin or 5-fluorouracil (5-FU) at the indicated concentrations. Optical density (OD; +s.d.) of formazan solution from three independent 3-[4,5–dimethylthiazol–2–yl]-2,5-diphenyl tetrazolium bromide assays is shown
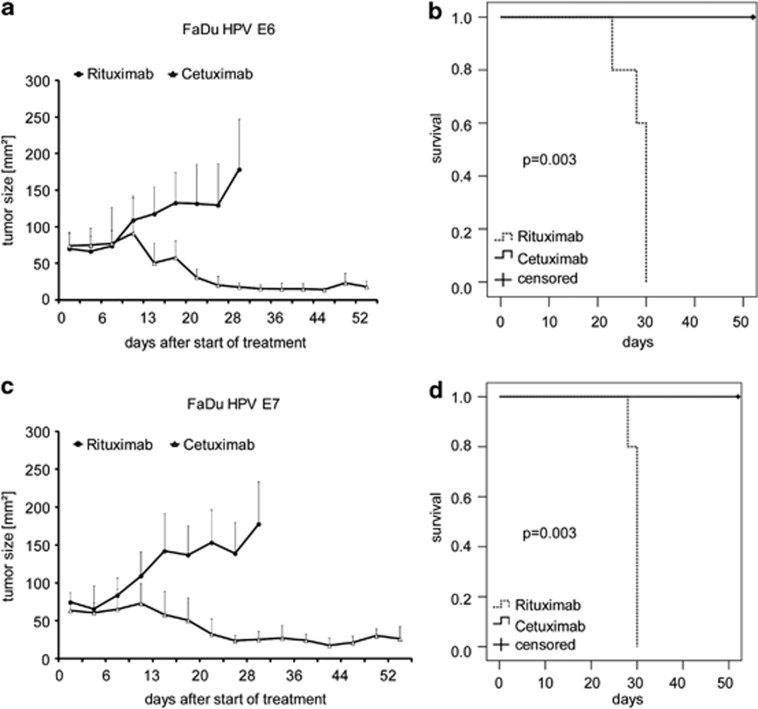
Next, we established FaDu tumors expressing E6, E7 oncogenes or a control vector in NOD/SCID mice. Following the outgrowth of palpable tumors, mice were treated with intraperitoneal injections of cetuximab or the control antibody rituximab. Again, cetuximab induced tumor regressions and significantly prolonged survival of mice. However, cetuximab responses in vivo were not altered by the expression of the HPV16 oncogenes E6 or E7 (Figures 2a and4a–d).
Figure 4.
Impact of enforced HPV E6 and E7 expression on the cetuximab response of HPV-negative HNSCC cells in vivo. (a and c) Tumor growth following injection of FaDu cells stably expressing HPV16 E6 (a) or HPV16 E7 oncogenes (c) in NOD/SCID mice. After 14 days, tumor-bearing mice received biweekly intraperitoneal injections of cetuximab (1 mg, white triangles) or the control antibody rituximab (black circles). Mean bidimensional tumor sizes (+s.d.) of five mice per group are given. Rapid and sustained tumor shrinkage was observed following cetuximab treatment. In contrast, tumors from rituximab-treated mice continuously progressed. (b and d) Kaplan–Meier plots of survival of NOD/SCID mice bearing FaDu tumors expressing HPV16 E6 (b) or HPV16 E7 (d). Mice were treated with cetuximab (solid line), or the control antibody rituximab (dashed line) as in a and c. Cetuximab-treated mice showed significantly prolonged survival as compared with rituximab-treated mice. Median survival time was not reached for cetuximab-treated FaDu HPV E6 tumour-bearing mice. It was 30 days for mice treated with rituximab (P=0.003, log rank test). In the FaDu HPV E7 model, median survival time for cetuximab-treated mice was not reached, and was 30 days for rituximab-treated mice (P=0.003, log rank test)
Response of HNSCC patients to cetuximab is not determined by the HPV status
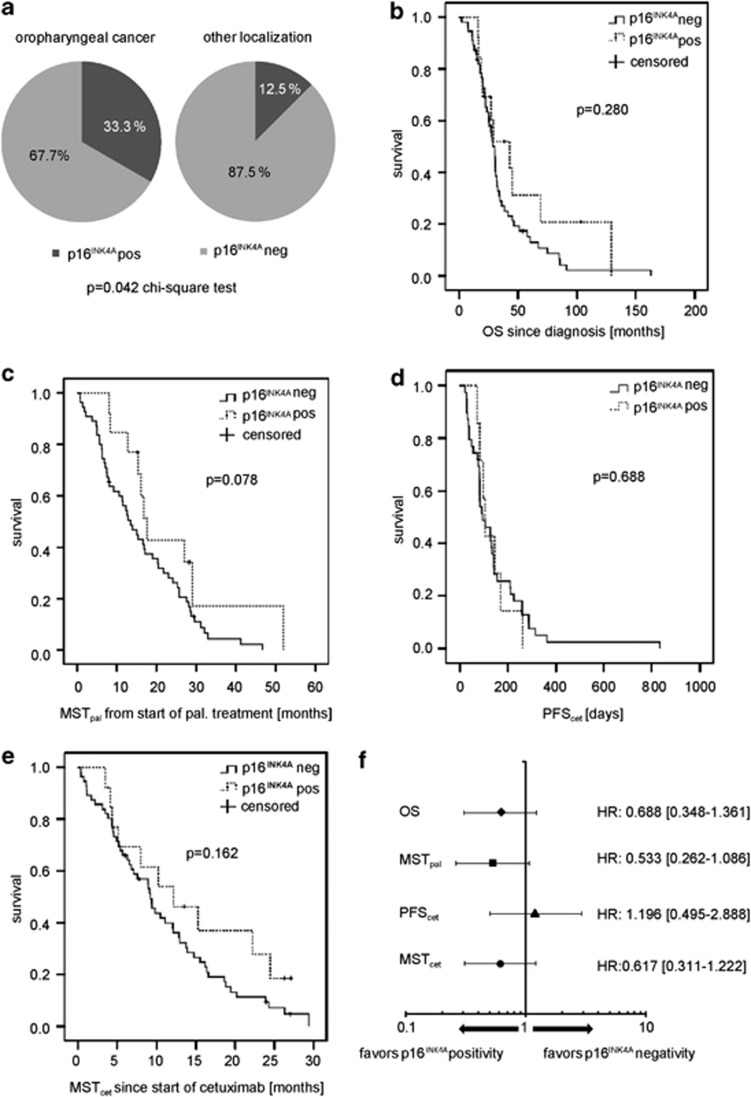
To corroborate our preclinical findings and to identify a potential clinical interaction of HPV status with the treatment response to cetuximab-based therapies, we studied a cohort of HNSCC patients treated at the West German Cancer Center, an urban comprehensive cancer center serving the densely populated Ruhr area in Germany (Supplementary Table 1). Formalin-fixed, paraffin-embedded (FFPE) surplus tumor tissue obtained at diagnostic biopsy or resection was available for analysis from 69 HNSCC patients, who had been treated between 2006 and 2011 (Table 2a). All patients suffered from recurrent, metastatic or locally advanced disease and were ineligible for curative resection or radiochemotherapy. Tissue sections were immunohistochemically studied for p16INK4A expression, an established biomarker for HPV infection.11, 12, 13, 25, 26 Tumors from 13 patients (19%) stained positively for p16INK4A (Table 2a) and were thus considered HPV positive. HPV-positive tumors were more frequently localized to the oropharynx (33% of oropharyngeal HNSCC) as compared with other localizations (12.5%, P<0.05 for comparison; Figure 5a). These findings were in line with the current epidemiology of HNSCC in Western Europe.7, 30, 31 There was no significant correlation of HPV positivity with histology, tumor grade or tumor stage (Table 2a).
Table 2a. p16INK4A staining of 69 patients with HNSCC.
| All | p16INK4A+/− | % Positive | P-value |
|---|---|---|---|
| N=69 | 13 | 18.8 | |
| Localization | |||
| Oral cavity | 1/7 | 12.5 | 0.626 |
| Tonsilla | 1/3 | 25 | 0.745 |
| Oropharynx | 7/14 | 33.3 | 0.042* |
| Hypopharynx | 0/13 | 0 | 0.054 |
| Larynx | 2/9 | 18.2 | 0.951 |
| Nasopharynx | 2/4 | 33.3 | 0.342 |
| Other | 0/6 | 0 | 0.217 |
| Histology | |||
| Keratinizing SCC | 6/38 | 13.6 | |
| Non-keratinizing SCC | 5/17 | 22.7 | 0.064 |
| Other | 2/1 | 66.7 | |
| T-status | |||
| T1 | 4/7 | 36.4 | |
| T2 | 2/12 | 14.3 | |
| T3 | 3/14 | 17.6 | 0.527 |
| T4 | 4/20 | 16.7 | |
| Tx | 0/3 | 0 | |
| N-status | |||
| N0 | 4/18 | 18.2 | |
| N1 | 1/10 | 9.1 | |
| N2 | 7/26 | 21.2 | 0.678 |
| N3 | 0/1 | 0 | |
| Nx | 1/1 | 50 | |
| M-status | |||
| M0 | 10/45 | 18.2 | |
| M1 | 2/9 | 18.2 | 0.895 |
| Mx | 0/1 | 0 | |
Abbreviation: SCC, squamous cell carcinoma
denotes statistical significance (P<0.05, chi-square)
Figure 5.
Clinical outcome and cetuximab response of patients with recurrent or metastatic HNSCC in relation to p16INK4A expression. (a) Immunohistochemically detectable p16INK4A expression in relation to HNSCC localization. Oropharyngeal cancers exhibited a statistically significant higher prevalence of p16INK4A positivity as compared with HNSCC of other localizations. Patients with tumors expressing p16INK4A were considered HPV positive. (b) Kaplan–Meier plot of overall survival (OS) from first diagnosis of patients with p16INK4A-negative (solid line) and p16INK4A-positive (dashed line) recurrent or metastatic HNSCC. Patients with p16INK4A-positive tumors demonstrated a numerically prolonged OS (42.97 versus 30.03 months), which did not reach statistical significance (P=0.280, log rank). (c) Kaplan–Meier plot of median survival time from initiation of palliative treatment (MSTpal) in patients with p16INK4A-negative (solid line) and p16INK4A-positive (dashed line) relapsed or metastatic HNSCC. Patients with p16INK4A-positive tumors had a numerically prolonged MSTpal (17.64 versus 13.44 months). The difference did not reach statistical significance (P=0.078, log rank). (d) Kaplan–Meier plot of median progression-free survival following cetuximab treatment (PFScet) in patients with p16INK4A-negative (solid line) and p16INK4A-positive (dashed line) HNSCC. Median PFScet was identical in both groups (P=0.688, log rank). (e) Kaplan–Meier plot of median survival time from start of cetuximab treatment (MSTcet) in patients with p16INK4A-negative (solid line) and p16INK4A-positive (dashed line) recurrent or metastatic HNSCC. Patients with p16INK4A-positive HNSCC showed a trend toward longer MSTcet as compared with patients with p16INK4A-negative HNSCC (12.16 versus 9.23 months, P=0.162, log rank). (f) Forrest blot of hazard ratios (HR) and 95% confidence intervals (CI) of OS, MSTpal, PFScet and MSTcet. A HR<1 favors p16INK4A positivity, and a HR>1 favors p16INK4A negativity. There was no trend toward an interaction between the PFScet and p16INK4A status
Fifty-five patients (80%) were evaluable for response to cetuximab-based treatments, whereas fourteen patients (20%) had stopped treatment early, died before first evaluation or were lost to follow-up. All 69 patients were evaluable for survival analyses. Median overall survival from primary diagnosis and median survival time from start of palliative treatment (MSTpal) were numerically longer in patients with HPV-positive HNSCC. However, this difference failed to reach statistical significance (Figures 5b, c and f, Table 2b). Hence, HPV positivity could not be formally established as a prognostic factor in this limited, retrospective cohort of patients with advanced, recurrent or metastatic HNSCC treated with cetuximab-based therapies. To explore a potential interaction of HPV status with response to cetuximab-based therapy, we calculated the response rate (RR) and the disease-control rate (DCR, patients achieving objective tumor regressions or stable disease) following cetuximab-based therapy (Table 2b). There was no difference between patients with HPV-positive (RR: 45.5%, DCR: 72.7%) and HPV-negative cancers (RR: 45.5%, DCR: 70.5%). Median progression-free survival following cetuximab treatment (PFScet) was 97 days for patients with HPV-positive and 92 days for HPV-negative tumors (P=0.688, log rank). MSTcet of the entire patient cohort was 9.43 months showing a trend toward longer MSTcet in patients with HPV-positive tumors (12.16 versus 9.23 months for HPV-negative tumors, P=0.162, log rank, Table 2b and Figures 5d–f). In summary, no interaction of HPV status with response to cetuximab-based therapy was detected in this cohort of patients with advanced, recurrent or metastatic HNSCC.
Table 2b. Clinical outcome of HNSCC patients in relation p16INK4A expression.
| Response rates | N=55 | % | p16INK4A negative | % | p16INK4A positive | % | P-value |
|---|---|---|---|---|---|---|---|
| CR | 1 | 1.8 | 1 | 2.3 | 0 | 0 | 0.614 |
| PR | 24 | 43.6 | 19 | 43.2 | 6 | 45.5 | 0.892 |
| NC | 14 | 25.5 | 11 | 25 | 3 | 27.3 | 0.877 |
| PD | 16 | 29.1 | 13 | 29.5 | 3 | 27.3 | 0.882 |
| ORR (CR+PR) | 25 | 45.5 | 20 | 45.5 | 5 | 45.5 | 1.0 |
| DCR (CR+PR+NC) | 39 | 70.9 | 31 | 70.5 | 8 | 72.7 | 0.882 |
| Survival times | N=69 | p16INK4A negative | p16INK4A positive | P-value |
|---|---|---|---|---|
| OS since diagnosis (months; interquartile range) | 30.03 (20.21–45.43) | 30.03 (20.4–45.44) | 42.97 (20.21–68.96) | 0.280 |
| OS since diagnosis HR (95% CI) | 0.688 (0.348–1.361) | 0.283 | ||
| MST from initiation of palliative treatment (months; interquartile range) | 15.38 (7.56–27) | 13.44 (6.87–25.27) | 17.64 (15.38–29.01) | 0.078 |
| MST from initiation of palliative treatment HR (95% CI) | 0.533 (0.262–1.086) | 0.083 | ||
| PFS (days) (interquartile range) | 95 (71–144) | 92 (56–156) | 97 (82–144) | 0.688 |
| PFS HR (95% CI) | 1.196 (0.495–2.888) | 0.690 | ||
| MST upon cetuximab (month; interquartile range) | 9.43 (4.53–16.39) | 9.23 (4.47–15.51) | 12.16 (5.06–24.48) | 0.162 |
| MST upon cetuximab HR (95% CI) | 0.617 (0.311–1.222) | 0.166 |
Abbreviations: CR, complete remission; HR, hazard ratio; PD, progressive disease; PR, partial remission
Discussion
It was shown that HPV infection impacts on prognosis and treatment outcome of patients with localized HNSCC. HPV-positive HNSCC patients are frequently younger and often lack risk factors such as tobacco smoking and excessive alcohol consumption. Also, HPV-positive tumors are preferentially found in the oropharynx and tonsils. These observations argue for a distinct carcinogenic process and tumor biology of localized HPV-positive HNSCC. However, it remains controversial whether this still holds true once the tumor has relapsed after primary therapy or in patients with metastatic disease.
The EGFR is expressed by the vast majority of localized and metastatic HNSCC. It is involved in tumor pathophysiology, and higher expression levels were correlated with poor prognosis. Hence, EGFR constitutes an attractive therapeutic target, which has been clinically addressed by small-molecule receptor tyrosine kinase inhibitors and monoclonal antibodies. So far, the chimeric anti-EGFR antibody cetuximab is the only targeted agent with convincing therapeutic activity in HNSCC. Cetuximab enhances the efficacy of simultaneously administered radiotherapy in patients with localized HNSCC.23, 24 In metastatic or recurrent disease, cetuximab has single agent activity and is also combined with platin- and 5FU-based chemotherapy.25, 26, 32, 33 Cetuximab only confers a modest improvement in outcome of the overall patient population. So far, there is no biomarker to predict those patients who derive a greater benefit from antibody therapy. As HPV was shown to promote tumor growth via increased membrane expression of EGFR, it could be hypothesized that HPV-positive HNSCC are more susceptible to cetuximab treatment. On the other hand, HPV oncogenes functionally override important tumor suppressor proteins such as p53 and pRb, which impact on the tumor phenotype and on the response to radiation and cytotoxic anticancer agents. It is unknown whether those tumor suppressors participate in the therapeutic response to anti-EGFR antibodies, which primarily act by abrogating EGFR-mediated growth and survival signaling and by immune mechanisms. Against this background, we have explored whether the HPV status could determine the response of HNSCC to cetuximab. Using HPV-positive and HPV-negative HNSCC models as well as enforced expression of the HPV oncogenes E6 and E7 in cetuximab-sensitive cell systems, we have determined that the HPV status does not impact on the cetuximab response in vitro and in vivo. This was corroborated by correlating the outcome of cetuximab-based treatment and survival of a cohort of HNSCC patients with HPV status as indicated by p16INK4A expression.
These findings seem surprising in the light of the established predictive and prognostic impact of HPV status in patients undergoing curative therapy for localized HNSCC. Possibly, HPV oncogenes have a more dominant role in early-stage disease. Genomic studies have revealed high frequencies of mutational inactivation of the p53 tumor suppressor and additional cell-cycle checkpoint regulators in HNSCC. Although HPV oncogenes also inactivate such mechanisms, patients with localized HPV-positive oropharyngeal cancer are less likely to be heavy smokers and alcohol abusers. Almost certainly this will result in a lower mutational burden with decreased likelihood of additional oncogenic events. Also, the on average younger age and more favorable sociodemographic profile of patients with localized HPV-positive HNSCC may positively impact on the outcome of surgery and radiation. These patients may be more capable of mounting constitutive and treatment-induced immune responses than the deprived, comorbid and elderly patient population with HPV-negative HNSCC, which could be sustained by the expression of immunogenic viral antigens In contrast, recurrent HNSCC after curatively intended radiochemotherapy have undergone selection for more resistant phenotypes. Further, they have acquired radiation-induced mutations. Distant metastases must have evaded additional defense mechanisms of the host, and have been shaped by the metastatic niche and their new, pathological environments. Against this background, the HPV oncogenes may be less determinant for the entire phenotype of relapsing and metastatic HNSCC as well as their treatment response.
In summary, our comprehensive functional studies and correlative translational evidence support the clinical application of cetuximab in HNSCC patients independently of the HPV status of the tumor. Further studies are required to define new biological hypotheses for the definition of biomarkers predictive of the cetuximab response in this disease.
Material and Methods
Cell lines and reagents
The human HNSCC cell lines FaDu and UPCI:SCC-090, and the human epidermoid cancer cell line A431 were obtained from DSMZ (Braunschweig, Germany). The human HNSCC cell lines UM-SCC-17b and UD-SCC-2 were provided by Professor Thomas Hoffmann (University of Ulm, Ulm, Germany). The colorectal cancer cell line Difi was provided by Dr. Robert Coffey (Nashville, TN, USA). FaDu, A431 and Difi cells were cultured in DMEM medium supplemented with 10% fetal bovine serum (PAA, Coelbe, Germany), L-glutamine, penicillin and streptomycin (Invitrogen, Frankfurt, Germany). UPCI:SCC-090, UM-SCC-17b and UN-SCC-2 were cultured in DMEM medium supplemented with 15% fetal bovine serum (PAA), L-glutamine, penicillin and streptomycin and non-essential amino acids (Invitrogen). Complementary DNAs encoding HPV16 oncogenes E6 and E7 were cloned into the bicistronic retroviral vector pQCXIN (Clontech Laboratories, Mountain View, CA, USA). Cell lines were transduced to stably express HPV16-E6 and HPV16-E7 as described previously.34
Clinical grade cetuximab (Erbitux, Merck Serono, Darmstadt, Germany), rituximab (Mabthera, Roche, Grenzach-Wyhlen, Germany), cisplatin and 5FU were purchased from the pharmacy of the University Hospital Essen.
RNA and protein analyses
For gene expression analysis, total RNA was isolated (High Pure RNA Isolation Kit, Roche Diagnostics, Mannheim, Germany) and reversely transcribed into cDNA (Transcription High Fidelity cDNA Synthesis Kit, Roche Diagnostics) following the manufacturer's instructions. Quantitative PCR analysis was performed on a LC480 instrument (Roche Diagnostics) using SYBR Green 1 Master chemistry (Roche Diagnostics) as described previously.35 Primer sequences were HPV16-E6 5′-TTGCTTTTCGGGATTTATGC-3′ and 5′-CAGGACACAGTGGCTTTTGA-3′, HPV16-E7 5′-CAGCTCAGAGGAGGAGGATG-3′ and 5′-GCCCATTAACAGGTCTTCCA-3′ and human ACTB 5′-TCAGCTGTGGGGTCCTGT-3′ and 5′-GAAGGGACAGGCAGTGAG-3′.
Protein expression and phosphoepitopes were detected by immunoblotting, immunohistochemistry or flow cytometry following established protocols. Primary antibodies were: p53, phospho-ERK1/2T202/Y204, ERK 1/2, phospho-EGFRY1068 (all from Cell Signaling Technology, Danvers, MA, USA), β-actin (C4, ICN, Irvine, CA, USA), EGFR/HER1-, HER2-, HER3- and HER4-Phycoerythrin (R&D Systems, Minneapolis, MN, USA).
Cellular assays
Cancer cells (3, 5 or 10 × 105 cells per well) were seeded in triplicates in 96-well plates and grown in the presence or absence of antibodies or cytotoxic agents. Proliferation and survival were quantified by measuring the produced formazan of 3-[4,5–dimethylthiazol–2–yl]-2,5-diphenyl tetrazolium bromide by a spectrophotometer following the manufacturer's instructions (Roche Diagnostics). Apoptosis was quantified by flow cytometric determination of cells with subgenomic DNA content following hypotonic lysis and staining with propidium iodide as previously described.34 All results were obtained from at least three independent experiments. For statistical analysis, the unpaired t-test was used.
Animal models
All animal studies were conducted in compliance with institutional guidelines and German Animal Protection Law, and were approved by the responsible regulatory authority (Landesamt für Natur, Umwelt und Verbraucherschutz Nordrhein-Westfalen, Az. G969/08). NOD/SCID mice (Charles River Laboratories, L'Arbresle, France) received single subcutaneous flank injections of 1 × 107 FaDu or UPCI:SCC-090 cells suspended in 200 μl saline, or 100 μl saline and 100 μl Matrigel basement membrane matrix (Beckton Dickinson, Franklin Lakes, NJ, USA), respectively. Animals were monitored twice weekly for tumor development. Tumor growth was bidimensionally quantified using a caliper. Tumor-bearing mice were treated with biweekly intraperitoneal injections of cetuximab or rituximab (used as control antibody) dissolved in 200 μl saline.
Analysis of tumor samples from HNSCC patients
Surplus FFPE tumor tissues were retrieved from 69 patients with recurrent or metastatic HNSCC treated with cetuximab at the West German Cancer Center. Patient demographics and characteristics are summarized in Supplementary Table 1. Tissue sections were analyzed for p16INK4a expression by immunohistochemistry (clone JC8, DCS Innovative Diagnostik-Systeme, Hamburg, Germany) following standard diagnostic protocols of the Institute of Pathology, University Hospital Essen. Expression of p16INK4A was classified by a modified scoring system.36 HPV status was rated positive (>50% of the tumor cells with strong nuclear as well as cytoplasmatic staining) or negative (<50% of the tumor cells staining positively). All studies on human samples were approved by the Ethics Committee of the Medical Faculty of the University Duisburg-Essen (Az 13-5486-BO).
Statistical analyses
Patient characteristics and outcomes, and animal experiments were statistically analyzed using the PASW Statistics 18 software (IBM SPSS Inc., Ehningen, Germany). Overall survival was defined as the period of time from the first diagnosis to death. MSTpal was defined as the period of time from the start of palliative chemotherapy or palliative radiation until death. Cetuximab-related progression-free survival (PFScet) was defined as the start of cetuximab treatment until radiological or clinical progression; median survival time from the start of cetuximab (MSTcet) was defined as the period of time from the start of cetuximab treatment until death.
Acknowledgments
We thank Sabrina Schilling, Malte Vogelsang, Sabine Harde, Annika Hohmann, the staff of the Central Animal Facility and the Pathology and Molecular Pathology Laboratories, University Hospital Essen, for their help. This work was supported by grants from the Deutsche Krebshilfe (110099 to M.P.), M.E.R.C.U.R. (An-2011-0031 to S.K.), the Wiedenfeld Foundation (to S.K.), the Wilhelm Sander-Stiftung (2005.136.3 to M.S.), intramural research funds of the Medical Faculty of the University Duisburg-Essen (IFORES 107-10430 to M.S.) and an Oncology Center of Excellence grant by the Deutsche Krebshilfe to the West German Cancer Center. M.P was supported by the program ‘Mentoring by Nobel Laureates' of the Centre for Medical Biotechnology of the University of Duisburg-Essen. We thank Professor/Dr Harald zur Hausen for mentoring M.P. within this program.
Glossary
- DCR
disease control rate
- EGFR
epidermal growth factor receptor
- FFPE
formalin-fixed, paraffin-embedded
- HNSCC
head and neck squamous cell cancer
- HR
hazard ratio
- HPV
human papilloma virus
- MST
median survival time
- PFS
progression-free survival
- RR
response rate
- SCC
squamous cell cancer
M Pogorzelski, T Gauler, M Schuler are affiliated to Merck Serono and S Kasper is affiliated to Merck Serono, Amgen. The remaining authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on Cell Death and Disease website (http://www.nature.com/cddis)
Edited by T Brunner
Supplementary Material
References
- Leemans CR, Braakhuis BJ, Brakenhoff RH. The molecular biology of head and neck cancer. Nat Rev Cancer. 2011;11:9–22. doi: 10.1038/nrc2982. [DOI] [PubMed] [Google Scholar]
- Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29:4294–4301. doi: 10.1200/JCO.2011.36.4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong AM, Grulich AE, Jones D, Lee CS, Garland SM, Dobbins TA, et al. Squamous cell carcinoma of the oropharynx in Australian males induced by human papillomavirus vaccine targets. Vaccine. 2010;28:3269–3272. doi: 10.1016/j.vaccine.2010.02.098. [DOI] [PubMed] [Google Scholar]
- Mork J, Lie AK, Glattre E, Hallmans G, Jellum E, Koskela P, et al. Human papillomavirus infection as a risk factor for squamous-cell carcinoma of the head and neck. N Engl J Med. 2001;344:1125–1131. doi: 10.1056/NEJM200104123441503. [DOI] [PubMed] [Google Scholar]
- Nasman A, Attner P, Hammarstedt L, Du J, Eriksson M, Giraud G, et al. Incidence of human papillomavirus (HPV) positive tonsillar carcinoma in Stockholm, Sweden: an epidemic of viral-induced carcinoma. Int J Cancer. 2009;125:362–366. doi: 10.1002/ijc.24339. [DOI] [PubMed] [Google Scholar]
- Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst. 2000;92:709–720. doi: 10.1093/jnci/92.9.709. [DOI] [PubMed] [Google Scholar]
- Ramqvist T, Dalianis T. Oropharyngeal cancer epidemic and human papillomavirus. Emerg Infect Dis. 2010;16:1671–1677. doi: 10.3201/eid1611.100452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demers GW, Halbert CL, Galloway DA. Elevated wild-type p53 protein levels in human epithelial cell lines immortalized by the human papillomavirus type 16 E7 gene. Virology. 1994;198:169–174. doi: 10.1006/viro.1994.1019. [DOI] [PubMed] [Google Scholar]
- Dyson N, Howley PM, Münger K, Harlow E. The human papilloma virus-16 E7 oncoprotein is able to bind to the retinoblastoma gene product. Science. 1989;243:934–937. doi: 10.1126/science.2537532. [DOI] [PubMed] [Google Scholar]
- Scheffner M, Werness BA, Huibregtse JM, Levine AJ, Howley PM. The E6 oncoprotein encoded by human papillomavirus types 16 and 18 promotes the degradation of p53. Cell. 1990;63:1129–1136. doi: 10.1016/0092-8674(90)90409-8. [DOI] [PubMed] [Google Scholar]
- Duncan LD, Winkler M, Carlson ER, Heidel RE, Kang E, Webb D. p16 Immunohistochemistry Can Be Used to Detect Human Papillomavirus in Oral Cavity Squamous Cell Carcinoma. J Oral Maxillofac Surg. 2013;71:1367–1375. doi: 10.1016/j.joms.2013.02.019. [DOI] [PubMed] [Google Scholar]
- Smeets SJ, Hesselink AT, Speel EJ, Haesevoets A, Snijders PJ, Pawlita M, et al. A novel algorithm for reliable detection of human papillomavirus in paraffin embedded head and neck cancer specimen. Int J Cancer. 2007;121:2465–2472. doi: 10.1002/ijc.22980. [DOI] [PubMed] [Google Scholar]
- Wittekindt C, Gultekin E, Weissenborn SJ, Dienes HP, Pfister HJ, Klussmann JP. Expression of p16 protein is associated with human papillomavirus status in tonsillar carcinomas and has implications on survival. Adv Otorhinolaryngol. 2005;62:72–80. doi: 10.1159/000082474. [DOI] [PubMed] [Google Scholar]
- Straight SW, Hinkle PM, Jewers RJ, McCance DJ. The E5 oncoprotein of human papillomavirus type 16 transforms fibroblasts and effects the downregulation of the epidermal growth factor receptor in keratinocytes. J Virol. 1993;67:4521–4532. doi: 10.1128/jvi.67.8.4521-4532.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reimers N, Kasper HU, Weissenborn SJ, Stützer H, Preuss SF, Hoffmann TK, et al. Combined analysis of HPV-DNA, p16 and EGFR expression to predict prognosis in oropharyngeal cancer. Int J Cancer. 2007;120:1731–1738. doi: 10.1002/ijc.22355. [DOI] [PubMed] [Google Scholar]
- Wheeler S, Siwak DR, Chai R, LaValle C, Seethala RR, Wang L, et al. Tumor epidermal growth factor receptor and EGFR PY1068 are independent prognostic indicators for head and neck squamous cell carcinoma. Clin Cancer Res. 2012;18:2278–2289. doi: 10.1158/1078-0432.CCR-11-1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troy JD, Weissfeld JL, Youk AO, Thomas S, Wang L, Grandis JR. Expression of EGFR, VEGF, and NOTCH1 suggest differences in tumor angiogenesis in HPV-positive and HPV-negative head and neck squamous cell carcinoma. Head Neck Pathol. 2013;7:344–355. doi: 10.1007/s12105-013-0447-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spangle JM, Munger K. The HPV1 6 E6 oncoprotein causes prolonged receptor protein tyrosine kinase signaling and enhances internalization of phosphorylated receptor species. PLoS Pathog. 2013;9:e1003237. doi: 10.1371/journal.ppat.1003237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adelstein DJ, Li Y, Adams GL, Kish JA, Ensley JF, Schuller DE, et al. An intergroup phase III comparison of standard radiation therapy and two schedules of concurrent chemoradiotherapy in patients with unresectable squamous cell head and neck cancer. J Clin Oncol. 2003;21:92–98. doi: 10.1200/JCO.2003.01.008. [DOI] [PubMed] [Google Scholar]
- Bernier J, Domenge C, Ozsahin M, Matuszewska K, Lefèbvre JL, Greiner RH, et al. Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med. 2004;350:1945–1952. doi: 10.1056/NEJMoa032641. [DOI] [PubMed] [Google Scholar]
- Cooper JS, Pajak TF, Forastiere AA, Jacobs J, Campbell BH, Saxman SB, et al. Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med. 2004;350:1937–1944. doi: 10.1056/NEJMoa032646. [DOI] [PubMed] [Google Scholar]
- Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363:24–35. doi: 10.1056/NEJMoa0912217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonner JA, Harari PM, Giralt J, Azarnia N, Shin DM, Cohen RB, et al. Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N Engl J Med. 2006;354:567–578. doi: 10.1056/NEJMoa053422. [DOI] [PubMed] [Google Scholar]
- Bonner JA, Harari PM, Giralt J, Cohen RB, Jones CU, Sur RK, et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol. 2010;11:21–28. doi: 10.1016/S1470-2045(09)70311-0. [DOI] [PubMed] [Google Scholar]
- Vermorken JB, Mesia R, Rivera F, Remenar E, Kawecki A, Rottey S, et al. Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med. 2008;359:1116–1127. doi: 10.1056/NEJMoa0802656. [DOI] [PubMed] [Google Scholar]
- Vermorken JB, Stohlmacher-Williams J, Davidenko I, Licitra L, Winquist E, Villanueva C, et al. Cisplatin and fluorouracil with or without panitumumab in patients with recurrent or metastatic squamous-cell carcinoma of the head and neck (SPECTRUM): an open-label phase 3 randomised trial. Lancet Oncol. 2013;14:697–710. doi: 10.1016/S1470-2045(13)70181-5. [DOI] [PubMed] [Google Scholar]
- Psyrri A, Licitra L, De Blas B, Celik I, Vermorken JB. Safety and efficacy of cisplatin plus 5-FU and cetuximab in HPV-positive and HPV-negative recurrent and/or metastatic squamous cell carcinoma of the head and neck (R/M SCCHN): analysis of the phase III EXTREME trial. Ann Oncol. 2012;23 (Suppl 9):10180. [Google Scholar]
- Kasper S, Breitenbuecher F, Reis H, Brandau S, Worm K, Köhler J, et al. Oncogenic RAS simultaneously protects against anti-EGFR antibody-dependent cellular cytotoxicity and EGFR signaling blockade. Oncogene. 2013;32:2873–2881. doi: 10.1038/onc.2012.302. [DOI] [PubMed] [Google Scholar]
- Jacobs C, Lyman G, Velez-Garcia E, Sridhar KS, Knight W, Hochster H, et al. A phase III randomized study comparing cisplatin and fluorouracil as single agents and in combination for advanced squamous cell carcinoma of the head and neck. J Clin Oncol. 1992;10:257–263. doi: 10.1200/JCO.1992.10.2.257. [DOI] [PubMed] [Google Scholar]
- Blomberg M, Nielsen A, Munk C, Kjaer SK. Trends in head and neck cancer incidence in Denmark, 1978-2007: focus on human papillomavirus associated sites. Int J Cancer. 2011;129:733–741. doi: 10.1002/ijc.25699. [DOI] [PubMed] [Google Scholar]
- Kreimer AR, Johansson M, Waterboer T, Kaaks R, Chang-Claude J, Drogen D, et al. Evaluation of human papillomavirus antibodies and risk of subsequent head and neck cancer. J Clin Oncol. 2013;31:2708–2715. doi: 10.1200/JCO.2012.47.2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermorken JB, Trigo J, Hitt R, Koralewski P, Diaz-Rubio E, Rolland F, et al. Open-label, uncontrolled, multicenter phase II study to evaluate the efficacy and toxicity of cetuximab as a single agent in patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck who failed to respond to platinum-based therapy. J Clin Oncol. 2007;25:2171–2177. doi: 10.1200/JCO.2006.06.7447. [DOI] [PubMed] [Google Scholar]
- Burtness B, Goldwasser MA, Flood W, Mattar B, Forastiere AA, Eastern Cooperative Oncology Group Phase III randomized trial of cisplatin plus placebo compared with cisplatin plus cetuximab in metastatic/recurrent head and neck cancer: an Eastern Cooperative Oncology Group study J Clin Oncol 2005238646–8654.Erratum in: J Clin Oncol 2006; 24: 724. [DOI] [PubMed] [Google Scholar]
- Schuler M, Maurer U, Goldstein JC, Breitenbücher F, Hoffarth S, Waterhouse NJ, et al. p53 triggers apoptosis in oncogene-expressing fibroblasts by the induction of Noxa and mitochondrial Bax translocation. Cell Death Differ. 2003;10:451–460. doi: 10.1038/sj.cdd.4401180. [DOI] [PubMed] [Google Scholar]
- Kasper S, Breitenbuecher F, Heidel F, Hoffarth S, Markova B, Schuler M, et al. Targeting MCL-1 sensitizes FLT3-ITD-positive leukemias to cytotoxic therapies. Blood Cancer J. 2012;2:e60. doi: 10.1038/bcj.2012.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaes R, Friedrich T, Spitkovsky D, Ridder R, Rudy W, Petry U, et al. Overexpression of p16(INK4A) as a specific marker for dysplastic and neoplastic epithelial cells of the cervix uteri. Int J Cancer. 2001;92:276–284. doi: 10.1002/ijc.1174. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.