Abstract
Background and Aims: Recent reports indicate that a variety of light-based devices have been used for acne treatment and skin rejuvenation. A new technology combining intense pulsed light with negative pressure, photopneumatic technology, has recently attracted interest. The present study assessed acne treatment and skin rejuvenation with this novel approach
Subjects and Methods: Acne, 450 nm tip. Five Japanese volunteers (1 male, 4 female; mean age 28.6 yr; skin type III) with mild to moderate/moderate active acne participated. The face was treated with 2 sessions, 2 weeks apart. Biopsies were obtained immediately after the first session and 1 week after the second session, and routinely processed for transmission electron microscopy (TEM). Rejuvenation, profusion tip with topical preparation. In 5 Japanese volunteers (3 male, 2 female; mean age 37.6 yr, skin type III), the volar aspect of both forearms was treated with the 530 nm head at P6 (around 12 J/cm2). The left arm was then treated with a pre-infused profusion tip and vacuum only. Four sessions were given, 14-day intervals. Biopsies were taken from both arms 2 weeks after the 2nd session and 3 weeks after the 4th session. One-half of each biopsy was assessed with histo-and immunohistochemistry, and the other with TEM.
Results
Acne trial: A combination of physical extraction of comedones, mild photothermal damage of the follicle and damage to identified bacilli was noted post-treatment, with macroscopic improvement of the skin. Rejuvenation with profusion: Significant morphological and immunohistochemical differences were seen between the control and profusion-treated arms at the first assessment. These differences became less significant at the 2nd assessment.
Conclusions
Macroscopically and histologically, photopneumatic technology improved acne lesions, suggesting a synergistic effect between the components of the technology. In skin rejuvenation, the profusion therapy accelerated the regenerative process, and could have excellent additional potential as a noninvasive transepidermal drug delivery system.
Keywords: IPL, Vacuum effect, endogenous PDT, proliferating cell nuclear antibody, skin rejuvenation
Introduction
The application of lasers and light-based systems in the field of dermatology has dramatically progressed based on Anderson and Parish's theory of selective pho-tothermolysis 1), in which very short pulses of laser energy with high peak powers at a given wavelength are selectively absorbed by target chromophores such as melanin and hemoglobin, but delivering minimum damage to the normal tissue surrounding the target. Based on this theory, markedly good therapeutic effects have been reported for the ruby, alexandrite and Nd:YAG lasers on melanogenic lesions, such as Ohta's nevus, tattoos and solar UV-related pigmentation, in addition to the efficacy of pulsed dye lasers in the treatment of vascular lesions, such as vascular malformations and telangiectasia. The application of these lasers in the extended theory of photothermolysis has currently expanded to include the treatment of acne and for hair removal.
For these lasers, higher fluences and longer wavelengths of light are delivered to overcome the limited penetration depths of shorter wavelength visible light, and epidermal cooling systems are employed to reduce the extent of epidermal damage. Furthermore, there are also problems with transient skin changes such as crusting in varying degrees occurring immediately after treatment of melanogenic pigmented lesions that can persist for 1 to 2 weeks, and of purpura that occurs after treatment of vascular lesions with a pulsed dye laser, that can persist for approximately 2 weeks. These have now been classed as examples of patient downtime, 2) meaning the period for which patients are restricted by these sequalae from their normal social and work activities.
It has been suggested that intense pulsed light (IPL) devices 3) are superior to conventional lasers in reducing such downtime, particularly the later generations of these systems. In addition, unlike single-wavelength lasers, IPL devices use a broadband light source that covers wavelengths absorbed by melanin and hemoglobin, specific semi-selectivity being achieved with the use of cutoff filters at the desired wavelengths. Therefore, with the right parameters, IPL devices can be effective in treating both solar pigmentation and teleangiectasia, which are often the targets as part of a skin rejuvenation program. With the ability to deliver good efficacy with lower fluences these devices are now frequently used in the treatment of Asian patients 4,5), including Japanese patients, without induction of postinflammatory hyperpigmentation (PIH), and for some practitioners have become the first choice for the purpose of skin rejuvenation.
As already stated, the use of a filter between the IPL system flashlamp and the target tissue enables IPL devices to produce a band of light which is ‘cut off at the desired wavelength, preventing shorter wavelengths from being emitted. It must be remembered, however, that all the longer wavelengths, both visible and near-infrared, are still emitted as a pulse of polychromatic energy unless a cut-on filter is also employed to remove these wavebands.
Some device types necessitate the use of a topical gel to couple the light energy to the skin surface, while others do not. The topical gel can also be useful for cooling and protecting the skin surface. However, the time and effort needed to apply the topical gel and differences in the irradiation and fluence due to uneven gel application are problematic in device types that require gel. On the other hand, protection of the skin surface is problematic in device types that do not involve the use of a topical gel or other form of cooling or optical coupling.
A recently developed novel approach, photop-neumatic technology 6), has been developed in which the skin in the area to be irradiated is stretched by inducing negative pressure, i.e., suction, making the upper dermis ischemic, and thereby reducing adverse effects and potentially increasing efficacy. The current article describes this new technology combining negative pressure and IPL energy, and presents histological assessments of its application in the treatment of acne and skin rejuvenation.
Photopneumatic technology 6)
Features of the Isolaz (Solta Medical, Inc., CA, USA), the first representative device that used photopneumatic technology, are now described. This device is characterized by a vacuum created by the handpiece, as shown in Figure 1. When the handpiece is applied to the skin surface, a negative pressure is generated; the skin is then pulled toward the handpiece crystal, irradiated by the flashlamp and released. A vacuum pressure of 3 pounds per square inch (PSI), approximately one-fifth of the normal atmospheric pressure (14.696 PSI), is generated. The system offers 3 choices for the length of vacuum application (V1, V2 and V3) with the IPL-associated vacuum times of 0.2, 0.6 or 1 s, and the profusion-associated vacuum times of 1, 1.5 and 2 s. Using this approach has enabled the fluence to be reduced by 60 to 80% compared with normal IPL systems in an initial laboratory test (data not shown). Decreasing the atmospheric pressure lowers the boiling point of water, and in the device described herein the approach termed Evaporative Cooling™ by the manufacturers provides cooling by lowering the boiling point of the tissue water from 100°C to 65°C. Thus, a cooling gel is not needed with this photopneumatic approach, unlike other IPL devices.
Fig. 1:
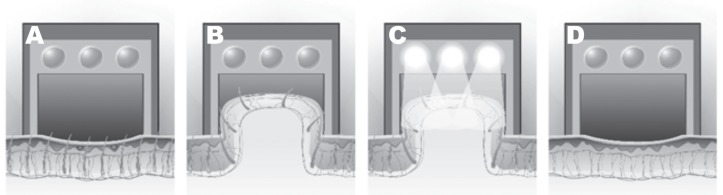
Photopneumatic technology illustrated
The handpiece is applied to the skin surface on the area to be treated, making sure there is a good seal between the tip and the skin surface. (Fig. 1A). Negative pressure is applied automatically, and the skin is then lifted up toward the irradiation port reducing the distance between the skin surface and the target dermal tissue (Fig. 1B), followed by irradiation from the flash lamp (Fig. 1C). The vacuum is released and the skin surface then automatically returns to normal after the irradiation (Fig. 1D).
The flashlamp of the system emits broadband light with wavelengths ranging from 400 nm shortwave visible blue to 1000 nm in the near infrared. Three filter tips (shown in Figure 2) can be used according to the intended purpose. The 400 nm tip is mainly used for the treatment of acne, the 530 nm tip for skin rejuvenation and the 580 nm tip for hair removal. The manufacturer mainly recommends the use of this device for acne treatment at present.
Fig. 2:
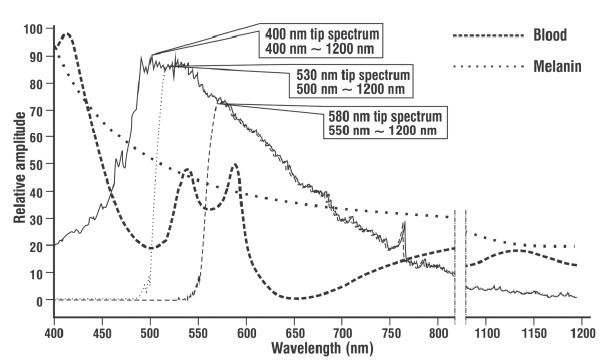
Spectral distribution of the system tips and cut-off filters
The system flashlamp emits broadband light with wavelengths from 400 to 1200 nm, and 3 different tips with cut-off filters can be used, according to the purpose. The 400-nm tip with its active range in the 400–550 nm waveband is mainly used for treating acne, the 530-nm tip with its active range in the 515–600 nm waveband is used for skin rejuvenation, and the 580-nm tip with its active range in the 570–600 nm waveband can be used for hair removal. The manufacturer currently recommends acne treatment and skin rejuvenation as the main indications.
The system offers another feature to assist in the delivery of creams or ointments through the stratum corneum, referred to by the manufacturers as profusion therapy 7). In this approach, a sponge in the dedicated disposable profusion tip is presoaked with the preparation to be applied to the skin. The cream used in the present study was the High-potency Cream manufactured by I.C.I. Cosmetics Japan Co. Ltd., Tokyo, Japan, and it is commercially available. Five grams, usually the amount that will fit from the tube on the tips of 2 gloved fingers, is applied to the sponge before each application for each patient. This preparation consists of epidermal growth factor, hyaluronate (hyaluronic acid), copper peptide GHK-Cu, other active peptides, ceramides and antioxidants (alpha lipoic acid, vitamin D, lutein and astaxanthin). Negative pressure is applied to the target tissue, so that the spaces in the stratum corneum, cell-cell junctions in the stratum spinosum and interstitial spaces in the superficial dermis are expanded thereby increasing skin permeability, and the preparation is more easily delivered deeper into the skin (Figure 3).
Fig. 3:
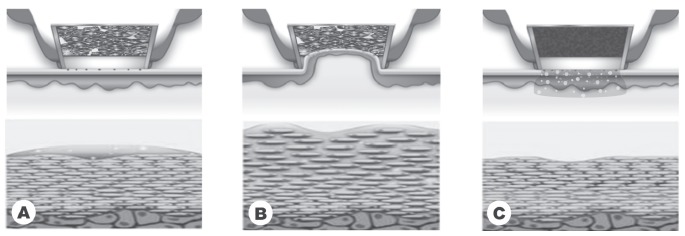
Profusion therapy
In this technology, the sponge in the profusion tip is soaked with a nutritive and regenerative preparation and the tip is placed on the target skin, ensuring a good seal between the tip and the skin surface. (A) Negative pressure is applied so that the spaces in the stratum corneum, stratum spinosum and superficial dermis are expanded (B) and when the vacuum is released the preparation can then be more easily delivered into the deeper layers of the skin (C).
In the present article, the author will concentrate on morphological and immunohistochemical assessments of the photopneumatic technology for the treatment of acne and for skin rejuvenation with the profusion therapy approach.
Techniques for clinical application
A general protocol for photopneumatic technology is described below. First, the face is washed before treatment. It is necessary to adequately remove oil and cosmetics in this step. Next, an appropriate tip is selected as mentioned in the previous section. The 400 nm tip is mainly used for acne treatment, and there are large and small tips. Induction of negative pressure is essential in photopneumatic technology, and if there is a gap between the operative field and the tip that allows air leakage, an adequate vacuum cannot be generated. Therefore, an appropriate tip size needs to be selected depending on the topography of the skin area to be treated. For example, a small tip should be used for the treatment of curved areas, such as the forehead and the sides of the nose, and a larger tip for flatter areas.
A test shot is recommended when patients receive the treatment for the first time, after a considerable interval, or when sunburned. With respect to the fluence used in the test shot, power 3 is usually recommended for Fitzpatrick skin type I, power 3 or 2 for skin type II, power 2 or 1 for skin type III, and power 1 for skin types IV to VI. A vacuum duration of 1 sec (V3) is recommended. Topical gel is not needed on the target skin, but it is always important to moisturize the skin surface to be treated.
If patients feel that the IPL treatment is too warm or the suction is too strong, the fluence or the vacuum level needs to be lowered, respectively, as necessary. The appearance of excessive erythema after irradiation or purpura due to suction would also necessitate decreasing the fluence and vacuum level. Lowering both the fluence and the vacuum by 1 level is recommended in patients with looser skin. The clinician should wait at least 5 minutes after the test shot before performing the treatment to allow the effects to become clearly visible. The darker the skin type, the longer it takes to see the actual effects because of the masking effect of native levels of melanin on erythema.
As stated, it is also important to moisturize the surface of the skin to be treated during the actual treatment. In addition, to prevent adverse effects, it is necessary to allow the tip to cool down after every 7 to 10 irradiations. For easier generation of the vacuum, it is advisable to apply the tip after a little stretching of the skin with the fingers to prevent formation of a gap between the skin and the tip. Stronger effects can be obtained with an additional 2–3 treatment passes, depending on the conditions of the skin and the effects of the treatment. In addition, it is always necessary to ensure and confirm that the tip lumen is not contaminated by sebum, skin particles and so on. Finally the treatment is completed by gently washing the face to avoid stimulation of the skin of the face. Marked clinical effects have reportedly been obtained using this technology and treatment approach after 4–5 treatments with a 1- to 3-week interval.
In profusion therapy, the sponge in the disposable tip is packed with 5 g of the High Potency Cream as described previously to deliver the compound efficiently into the skin through altering the permeability of the protective strata corneum and spinosum through the vacuum mechanism. In general, 50–60 shots can be given per single loading, usually enough for each patient. The tip is discarded after each session and replaced with a new one. The vacuum durations for the profusion tip are 1, 1.5 and 2 s, corresponding to levels 1, 2 or 3. In addition, there are 2 settings with respect to time in which the vacuum is generated, the normal vacuum generation time (normal mode) and a longer vacuum generation time (soft mode). In the case of profusion therapy following photopneumatic treatment with IPL, the face is washed first after the IPL/vacuum treatment before profusion therapy is applied.
Photopneumatic technology for acne therapy
Acne is an extremely common disease that is found in a wide-range of age groups, from the teens to the 40s and over It is easily diagnosed and is usually treated with oral/topical antibiotics, and occasionally with oral/topical vitamin A. However, antibiotics are problematic because they readily produce resistant bacteria and vitamin A is problematic because of adverse reactions to medications containing it. New approaches for acne appeared in the 1990s and into the first decade of the New Millennium, including chemical peeling, lasers, treatment with IPL systems and LED phototherapy. These treatments have been described in numerous clinical reports. 8–11)
In addition to these, the author has recently applied the photopneumatic approach, 6,12) and considers it very suitable for acne treatment, because treatment is performed using the 400 nm acne tip (peak waveband 400 – 550 nm) together with the suction function described above. Clinical and histological studies have been performed as follows.
Clinical study 8,12)
Five Japanese volunteers (1 male, 4 female; mean age 28.6 yr; skin type III) with mild to moderate/moderate active acne participated in this study. All subjects were treated with two photopneumatic sessions at the P2 and V2 settings for IPL power and vacuum, respectively, 2 sessions, 2 weeks apart. The system used in the present study offers two distinct advantages in the treatment of acne compared with conventional IPL systems; first, the pores are mechanically cleansed by the suction, and the follicular ostia are opened to evacuate sebum. These effects have also been demonstrated his-tologically, as described below. This means that effects can be expected to continue to some extent even after a single treatment session, due to the comedonal extraction effect of the suction, and patients are satisfied. In addition, it also improves post-acne inflammatory erythema, common with other IPL devices. An improvement can usually be noted after 4–5 treatments at 2-weekly intervals (Figure 4).
Fig. 4:
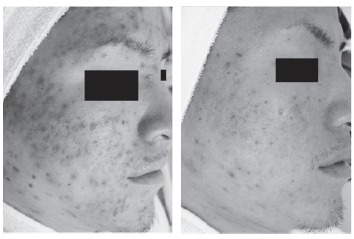
: Acne therapy with the photopneumatic tech¬nique 32
year old male. Facial acne lesions were treat¬ed with 2 sessions of photopneumatic therapy at power setting P2 and vacuum setting V2 with a 2 week interval. The left panel shows the pre-treatment baseline and the right panel shows the results 4 weeks after baseline and 2 weeks after the second exposure, with good clearance. Further treatments will improve the results.
Five subjects for each trial might at first appear to be too few. In fact, the author recognizes that a patient population of 5 is not sufficient for a clinical trial per se, however the main thrust of the present article was a histological assessment to examine in vivo the morphological changes and the cellular and subcellular mechanisms triggered by the photopneumatic technique for both acne treatment and rejuvenation, the latter also comparing the IPL/vacuum approach with and without the profusion tip. For this purpose, a patient population of 5 each for both trials was sufficient to see any pattern on which future large-scale clinical trials could be based, and such patterns were clearly demonstrated in the histology and immunohistochemistry as shall be seen below.
Histological study and Discussion
The author and colleagues have carried out the following investigations to histologically examine changes in the skin after irradiation using the photopneumatic approach. The subjects were those in the clinical study. The facial acne was treated as above. Three millimeter skin punch biopsies were then obtained from each subject immediately following the first treatment session and one week after the second treatment session. The specimens were then examined using transmission electron microscopy 14) (75 kV, Hitachi H-7500; Hitachi, Tokyo, Japan).
Dilatation of the epidermal openings and enlarged pilosebaceous ducts were observed in comedones in the biopsy tissues sampled immediately following the first treatment session. Inspissated material was found within the comedones that had extruded through the epidermal openings onto the skin surface (Figure 5), showing that expulsion of the comedone contents from follicular openings occurred immediately following the irradiation, implying that the effect of suction on acne lesions may contribute to the expulsion of the comedone contents.
Fig. 5:
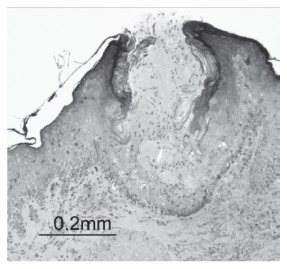
Comedonal opening with the photopneumatic technique.
Dilatation of the epidermal openings and enlarged pilosebaceous ducts are observed in comedones in the biopsy tissues sampled immediately following the first treatment session. Inspissated material can be found within the comedones that were extruded through the epidermal openings on to the skin surface.
Although not observed immediately following the first session of irradiation, the lumina of the piloseba-ceous ducts were necrotic due to thermal damage in the biopsy tissues sampled one week after the second session of irradiation. The squamous epithelium in the lumina of the pilosebaceous ducts was necrotic, and the squamous epithelial layer of the lower layer was found to have separated. No necrosis or inflammatory cell infiltration was observed in the surrounding tissue, therefore, these changes were not a result of the first session of irradiation, but occurred as an effect of the second session of irradiation. In addition, no characteristic changes in the squamous epithelial layer of the lower layer of the detached squamous epithelium were noted, so these changes were histologically mild. These changes were therefore thought to have begun to occur from 3–7 days after the initial irradiation. The underlying mechanism is assumed to be photothermal rather than photochemical.
Bacteria were observed inside the acne components in the specimens. These bacteria were considered to be bacilli because of their shape, potentially examples ofPropionibacterium acnes (P. acnes). Their morphological structure was almost normal immediately following the first session of treatment. However, 1 week after the second treatment session, injured bacteria could be observed. Necrotic stratified cells could also be observed (Figure 6).
Fig. 6:
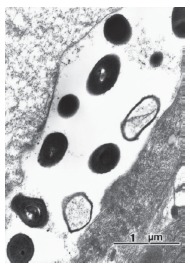
Injured bacteria after the photopneumatic technique.
These bacteria were considered to be bacilli (most probably Propionibacterium acnes) because of their shape. Their morphological structure was almost normal immediately following the first session of treatment. However, 1 week after the second treatment session, injured bacteria can be observed in this specimen, together with necrotic stratified cells.
An important factor in the potential treatment of acne using light is the endogenous production of por-phyrins by P. acnes, namely protoporphyrin IX and coproporphyrin III. Porphyrins are raised to a triplet state by shortwave blue light, which in turn generates singlet oxygen (1O2) from intracellular ground state oxygen, a potent reactive oxygen species which induces apoptotic cell death in P. acnes, thus this form of acne treatment is considered to be extremely effective. 10,11,15) The acne tip of the system in the present study delivered a major portion of the peak power in the visible blue waveband (Rf Figure 2), and damage to the P. acnes may well be brought about by the blue light delivered by this tip.
The clinical and histological findings demonstrated above suggested that the squamous epithelium in the lumina of the pilosebaceous ducts was damaged by the IPL energy through photothermal and photochemical mechanisms, and that the bacteria were damaged by the blue spectrum of the delivered light via endogenous PDT. Treatment of acne using photopneumatic technology is thus suggested as offering an effective approach, and merits further controlled or comparative studies with larger populations and possibly a split face component.
Profusion therapy with vacuum technology
Skin rejuvenation includes the improvement of wrinkles, fine lines, skin texture, skin hydration and overall appearance. Rejuvenation devices have also been used to treat benign and malignant neoplasms. Chemical peels as well as IPL, lasers (ablative, pulsed dye, diode), light-emitting diodes (LED), radiofrequency (RF), and fractional devices have been reported to have varying degrees of efficacy. 16,19) Although effective against pigmented lesions, IPL has not been demonstrated to deliver dramatic improvement to the dermal structure required to achieve skin rejuvenation. In attempts to overcome this limitation, investigators have combined IPL with chemical peeling, botulinum toxin injections, RF devices, laser devices and photodynamic therapy (PDT), and in the present study, with a vacuum to deliver photopneumatic therapy as described above.
A profusion tip is also supplied with the system being used in the present study, whereby the penetration of a topical skin rejuvenating compound in a sponge applicator is potentially enhanced with the use of the suction technology, but without IPL energy. The profusion tip has been shown to actually increase the penetration of drugs through pig skin in vivo as compared to a simple surface application. 20) In a study on a high-potency cream (I.C.I. Cosmetics Japan Co. Ltd., Tokyo, Japan) containing kinetin and matrixyl packed into the profusion tip the skin was analyzed using using the replica method and showed that the use of the profusion tip significantly improved to penetration of the cream into the skin compared with simple topical application (p <0.05).
Clinical study
The photopneumatic technique was applied to the face for acne scar treatment and skin rejuvenation under the following conditions: the device was set at P6 (approximately 12 J/cm2), 25-ms pulse width, and doublepulse mode with a 200-ms delay, and vacuum level V2 (0.6 s). The 530-nm hand piece was used for all treatments. After the photopneumatic technique, following washing of the face the patients also received profusion therapy (no IPL, only the sponge applicator charged with the compound described already) The vacuum treatment configuration was set to a duration of 1500 ms with a 1500 ms delay (profusion level V2) and two passes were delivered. Treatment was repeated over 4 sessions, 2 weeks between sessions. Improvement of the acne scars and skin rejuvenation effects were obtained 2 weeks after the 4th session as shown in Figure 7.
Fig. 7:
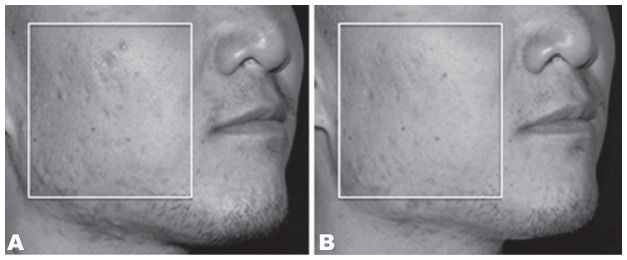
Acne scar treatment and skin rejuvenation with the photopneumatic technique followed by profusion technology.
34 year old male. The device was set at Power level 6 (approximately 12 J/cm2), 25-ms pulse width, and double-pulse mode with a 200-ms delay. The 530-nm hand piece was used for all treatments. After the photopneumatic treatment, the patients also received profusion therapy with a 1500-ms pulse duration and a 1500-ms pulse delay (profusion V2) treatment configuration (two passes). The left panel shows the findings at baseline, and the right panel shows the results 2 weeks after the 4th Profusion therapy.
Histological Study and Discussion
We performed a histological study to examine the histological changes that may occur in association with profusion therapy. 21) Healthy adult informed and consenting Japanese volunteers (n = 5, age 32 to 46 years [mean, 37.6], 3 male, 2 female, Fitzpatrick skin type III) were recruited. The volar aspect of both arms in each subject was treated with the photopneumatic technique set at the same setting as for the clinical trial (P6, V2). After the photopneumatic treatment, the tip was changed to the profusion tip with preloaded sponge applicator and profusion therapy (vacuum, no IPL) was applied only to the left arm (profusion V2, 1.5 s). Each subject received 4 treatment sessions at 2-week intervals.
A biopsy specimen was obtained from both arms of each patient 2 weeks after the second treatment session and 3 weeks after the fourth treatment session. The subsequent biopsy specimens were collected at least 10 cm from the site of the first biopsy. One half of each specimen was fixed in buffered formalin and stained with hematoxylin and eosin (H&E) and elastica van Gieson (EVG) stains. The avidin-biotin complex (ABC) immunoperoxidase method was used to assess the expression of proliferating cell nuclear antibody (PCNA) 22) (Dako Co., Ltd., Denmark) and p53 21,22) (Visiobiosystems, UK). Reaction products were visualized with diaminobenzidine tetrahydrochloride and hydrogen peroxide. The other half of each specimen was examined with electron microscopy. 14)
Two weeks after two treatment sessions, examination of the HE- and EVG-stained specimens from the left arm (treated with the photopneumatic approach together with profusion therapy) revealed an increase in elastin fibers in the papillary layer directly under the epidermis. On the other hand, no such significant increase was observed in the specimens from the right arm, which had been treated with the IPL/vacuum approach alone. The number of PCNA-positive cells on the left arm ranged from 136.7 to 192.6 (mean, 1739), as compared to 75.4 to 152.3 (mean, 101.0) on the right arm. The difference in the number of such cells between the right and left arms was significant (P < 0.05) (Figure 8). Staining for p53 was negative in all specimens.
Fig. 8:
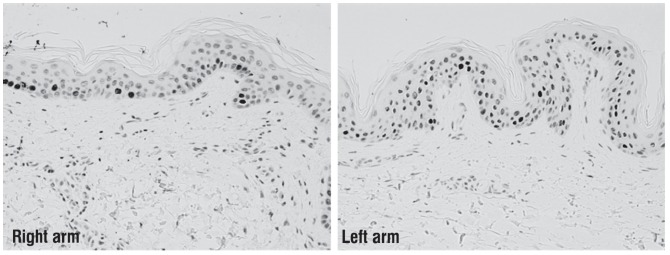
PCNA reaction after therapy.
The left panel shows the right arm and the right panel shows the left arm. PCNA-positive cells can be observed mainly in the basal layer, with smaller numbers in the middle layer of the epidermis on the right side (photopneumatic therapy-only side). On the other hand, a larger number of these cells is observed from the basal layer to just beneath the epidermis on the photopneumatic plus profusion therapy side. In addition, PCNA-positive cells are only rarely observed in the basal layer of normal skin.
In the right arm, electron-microscopic examination revealed abnormal elaunin fibers directly below the epidermis (Figure 9, left), irregularly arranged collagen fibers, and abnormal elaunin fibers around the capillaries. In the left arm, fibroblasts and a proliferation of normal elastic fibers were observed directly under the epidermis, and around the capillaries (Figure 9, right). No elaunin fibers were observed in the left arm sections.
Fig. 9:
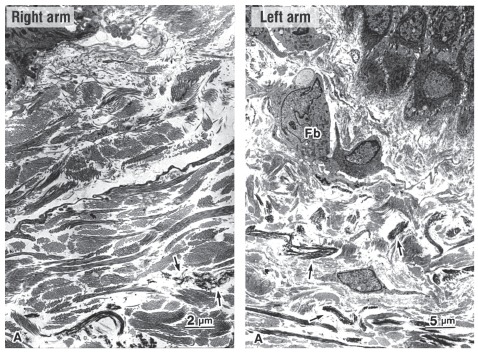
Ultrastructural differences between photopneumatic therapy only and the photopneumatic technique with profusion therapy.
(Left panel) Representative electron photomicrographs of the right arm treated with the photopneumatic device alone after the second treatment session. Abnormal elaunin fibers are visualized under the epidermis (A), and irregularly arranged collagen fibers and abnormal elaunin fibers ( ↑ ) are present around the capillaries.
(Right panel) Representative electron photomicrographs of the left arm treated with the Isolaz device and Profusion Tip in combination after the second treatment session. Fibroblasts (Fb) and numerous normal elastic fibers are visualized under the epidermis (A), and normal elastic fibers ( ↑ ) are found around the capillaries.
At 3 weeks after the fourth treatment session, the HE- and EVG-stained biopsy specimens showed evidence of angiogenesis in the papillary layer of the dermis, starting directly under the dermis, in both arms. An increase in the number of fibroblasts in the papillary layer of the dermis and a mild increase in lymphocytic infiltration were seen around the blood vessels in the superficial layer of the dermis, also in both arms.
After the fourth treatment session, the number of PCNA-positive cells ranged from 124.9 to 275.8 (mean, 188.7) in the left arm, and from 135.8 to 280.3 (mean, 190.4) in the right arm without significant difference. Staining for p53 was negative in all specimens. Electron microscopy showed an increase in the number of collagen fibers below the epidermis in both arms. An increase in the number of elastic fibers below the epidermis in the right arm was observed in only one subject and in the left arm in every subject.
Expression of high levels of PCNA 19 has been reported in cycling cells during the last 5% of the G1 phase and during the first 35% of the S phase. PCNA is essential for progression of the cell cycle, and high levels of PCNA are found in the epidermis and capillaries during wound healing. p53 21,22) has been reported to be capable of inducing programmed cell death (apoptosis). Since p53 staining was negative in every subject, the level of vacuum used in profusion therapy did not appear to have induced apoptosis in the normal skin cells of our subjects. In other words, the vacuum did not damage any cells, at least to the extent of apoptosis induction.
After the second treatment, the number of PCNA-positive cells was significantly greater in the profusion-treated left arm compared with the IPL/vacuum only treated right arm, but at 3 weeks after the fourth treatment there was no significant difference the in the number of PCNA-positive cells between left and right arms. The lack of any statistical significance in the difference of these specific cells between the arms after the fourth treatment may be attributed to the cellular activity in the left arm having reached a plateau after the second or third treatment session, which is consistent with the observed histological changes in the dermis, whereas it took the right arm the full four sessions without the profusion tip to reach similar levels of cellular activity.
The morphological changes observed in the dermal layers of all treated arms suggest that dermal reorganization and neofibrogenesis had started at an earlier stage in the combination-treated left arm than in the photopneumatic alone-treated right arm. This is based on the hypothesis that the observed morphological changes in the elastin fibers represented the regenerative process. Support for this interpretation comes from the following: (1) the formation of new elastin fibers (elastogenesis) appears to involve a transformation of oxytalan fibers to elastin fibers in the presence of elaunin fibers, (2) elaunin fibers have been observed at an early stage of skin rejuvenation, 14) and (3) elaunin fibers were observed only in the right arms of our subjects after two treatment sessions.
After the fourth treatment session, an increase in the number of collagen fibers was seen in both the left arm and the right arm, and the histological differences between the right and left arms were smaller than those after the second treatment session. This suggests that after the fourth treatment session, neofibrogenesis of the dermis was nearly complete in the right arm and had reached a plateau in the left arm. These results suggest that 4 treatment sessions with photopneumatic treatment alone resulted in remodeling of the dermis in normal skin. The addition of the profusion tip contents appeared to have hastened the appearance of these effects, so that the dermal remodeling began at an earlier stage than with treatment using photopneumatic treatment alone.
Precautions and adverse effects
Adverse effects can be reduced by the generation of the vacuum in the system under study, as described above, and there are fewer adverse effects and taboos with respect to the use of photopneumatic treatment than is the case in normal IPL devices. However, some precautions associated with other IPL devices are also valid in the case of photopneumatic treatment. It is essential to lower the fluence for Fitzpatrick skin types III–IV because of the risks of burn and hyperpigmentation due to higher endogenous epidermal melanin content.
Contraindications include treatment within 2 weeks after obtaining a suntan naturally or using a suntan parlor, treatment for tattoos, patients with a history of hypertrophic scars or keloids, photosensitivity, history of taking oral medications that can cause photosensitivity, and treatment for melasma. In addition, although not specifically contraindicated, the treatment should be performed carefully for patients who are pregnant or wish to become pregnant, and for patients who have pigmentation in the area to be irradiated.
The system used in the present study is an IPL device that can cause similar adverse effects to other IPL devices. Specifically, erythema and burns may occur immediately after to intense a dose of irradiation. Purpura due to reverse osmosis of blood from microvessels after a strong vacuum effect can also occasionally be found. Cooling is necessary after treatment when such adverse effects are observed. Any purpura usually disappears within 1 week, however, informed consent must be obtained after providing sufficient explanation before the treatment. As with any IPL treatment, delayed hyperpigmentation and hypopigmentation may occur after some time. Hyperpigmentation usually disappears within a few months and can be treated with the use of topical hydroquinone, etc., however, the hypopigmentation may not disappear for a few years.
Conclusions
The system presented and assessed in the present study was an IPL device used in combination with a vacuum. Therefore, it offered advantages in that the extent of epidermal damage could be reduced and the intended effects could be easily obtained. In addition, the suction effect is highly effective to expel comedone contents and is considered to be effective, particularly for acne treatment. The addition of the profusion tip appeared to offer greater efficacy in increasing skin absorption of the preparation on the sponge applicator, as compared to usual topical treatments, and its application as a new drug delivery system is considered possible in the future. However, sufficient attention will need to be paid to the safety of topical medicaments after incorporation into the body through the skin barrier. Further controlled trials with larger populations are warranted for both the photopneumatic approach and profusion therapy with this system.
References
- 1: Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983; 220: 119-126 [DOI] [PubMed] [Google Scholar]
- 2: Dawson E, Willey A, Lee K. Adverse events associated with nonablative cutaneous laser, radiofrequency, and light-based devices. Semin Cutan Med Surg. 2007; 26: 15-21 [DOI] [PubMed] [Google Scholar]
- 3: Babilas P, Schreml S, Szeimies RM, Landthaler M. Intense pulsed light (IPL): a review. Lasers Surg Med. 2010; 42: 93-104 [DOI] [PubMed] [Google Scholar]
- 4: Ho SG, Chan HH. The Asian dermatologic patient: review of common pigmentary disorders and cutaneous diseases. Am J Clin Dermatol. 2009; 10: 153-168 [DOI] [PubMed] [Google Scholar]
- 5: Negishi K, Wakamatsu S, Kushikata N, Tezuka Y, Kotani Y, Shiba K. Photorejuvenation for Asian skin by intense pulsed light. Lasers Surg Med. 2002; 30: 298-305 [DOI] [PubMed] [Google Scholar]
- 6: Narurkar VA. Novel photopneumatic therapy delivers highefficiency photons to dermal targets. Cosmet Dermatol. 2005; 18: 115-120 [Google Scholar]
- 7: Narurkar VA, Anderson R, Zand S. Profusion therapy — a novel combination of light with topical delivery for enhanced clinical outcomes on acne and skin rejuvenation. Aesthera Corporation 2008. [white paper].
- 8: Gold MH, Biron-BS J. Efficacy of a novel combination of pneumatic energy and broadband light for the treatment of acne. J Drugs Dermatol. 2008; 7: 139-145 [PubMed] [Google Scholar]
- 9: Omi T: Acne-Treatment and care. Nankodo (Tokyo). 2008; 9-27
- 10:Goldberg DG and Russell B:Combination blue (415 nm) and red (633 nm) LED phototherapy in the treatment of mild to severe acne vulgaris. J Cos Laser Therapy, 2004. 8: 71-75 [DOI] [PubMed] [Google Scholar]
- 11: Lee SY, You CE, Park MY: Blue and red light combination LED phototherapy for acne vulgaris in patients with skin phototype IV. Lasers Surg Med, 2007. 39: 180-188 [DOI] [PubMed] [Google Scholar]
- 12: Munavalli GS, Weiss RA. Evidence for laser and light based treatment of acne vulgaris. Semin Cutan Med Surg. 2008; 27: 207-211 [DOI] [PubMed] [Google Scholar]
- 13: Omi T, Munavalli GS, Kawana S, Sato S. Ultrastructural evidence for thermal injury to pilosebaceous units during the treatment of acne using photopneumatic therapy. J Cosmet Laser Ther. 2008; 19: 7-11 [DOI] [PubMed] [Google Scholar]
- 14: Sato S, Sasaki Y, Adachi A, Dai W, Liu XL, Namimatsu S. Use of oolong tea extract (OTE) for elastin staining and enhancement in ultrathin specimens, Med Electron Microsc. 2003; 36: 179-182 [DOI] [PubMed] [Google Scholar]
- 15: Omi T, Bejrring P, Sato S. et al: 420 nm intense continuous light therapy for acne. J Cosmet Laser Ther. 2004; 6: 156-162 [DOI] [PubMed] [Google Scholar]
- 16: Omi T, Sato S, Numano K, Kawana S. Ultrastructural observations of chemical peeling for skin rejuvenation. J Cosmet Laser Ther. 2010; 12: 21-24 [DOI] [PubMed] [Google Scholar]
- 17: Rokhsar CK, Lee S, Fitzpatrick RE. Review of photorejuvenation: devices, cosmeceuticals or both. Dermatol Surg. 2005; 31: 1166-1178 [DOI] [PubMed] [Google Scholar]
- 18: Trelles MA, Mordon S, Calderhead RG. Facial rejuvenation and light: our personal experience. Lasers Med Sci. 2007; 22: 93-99 [DOI] [PubMed] [Google Scholar]
- 19: Lee SY, Park KH, Choi JW, Kwon JK, et al. , A prospective, randomized, placebo-controlled, double-blinded, and split-face clinical study on LED phototherapy for skin rejuvenation: Clinical, profilometric, histologic, ultrastructural, and biochemical evaluations and comparison of three different treatment settings. J Photochem Photobiol (B), 2007; 88: 51-67 [DOI] [PubMed] [Google Scholar]
- 20: Okuyama M, Omi T, Kawana S Effects on cutaneous condition and wrinkle reduction of a cream product containing Kinetin and Matrixyl. Aesthetic Dermatology. 2003; 13: 161-165 [Google Scholar]
- 21: Omi T, Kawana S, Sato S, et al. Histological evidence for skin rejuvenation using a combination of pneumatic energy, broadband light, and growth factor therapy. J Cosmet Lase Ther. 2010; 12: 222-226 [DOI] [PubMed] [Google Scholar]
- 22: Waseem NH, Lane DP. Monoclonal antibody analysis of the proliferating cell nuclear antigen (PCNA). Structural conservation and the detection of a nucleolar form. J Cell Sci. 1990; 96: 121-129 [DOI] [PubMed] [Google Scholar]
- 23: Banks L, Matlashewski G, Crawford L. Isolation of human p53 specific monoclonal antibodies and their use in the studies of human p53 expression. Eur J Biochem. 1986; 159: 529-534 [DOI] [PubMed] [Google Scholar]


