Abstract
Cushing’s disease is a condition of hypercortisolism caused by an adrenocorticotropic hormone (ACTH)-secreting pituitary adenoma. While rare, it is associated with significant morbidity and mortality, which suggests that early and aggressive intervention is required. The primary, definitive therapy for patients with Cushing’s disease in the majority of patients is pituitary surgery, generally performed via a transsphenoidal approach. However, many patients will not achieve remission or they will have recurrences. The consequences of persistent hypercortisolism are severe and, as such, early identification of those patients at risk of treatment failure is exigent. Medical management of Cushing’s disease patients plays an important role in achieving long-term remission after failed transsphenoidal surgery, while awaiting effects of radiation or before surgery to decrease the hypercortisolemia and potentially reducing perioperative complications and improving outcome. Medical therapies include centrally acting agents, adrenal steroidogenesis inhibitors and glucocorticoid receptor blockers. Furthermore, several new agents are in clinical trials. To normalize the devastating disease effects of hypercortisolemia, it is paramount that successful patient disease management includes individualized, multidisciplinary care, with close collaboration between endocrinologists, neurosurgeons, radiation oncologists, and general surgeons. This commentary will focus on recent advances in the medical treatment of Cushing’s, with a focus on newly approved ACTH modulators and glucocorticoid receptor blockers.
Introduction
Cushing’s syndrome results from prolonged exposure to excessive levels of circulating glucocorticoids. Cushing’s disease is a condition of hypercortisolism caused by an ACTH-secreting pituitary adenoma. While rare, it is associated with significant morbidity and mortality [1,2], which suggests that early and aggressive intervention to prevent excessive mortality is required.
To normalize the devastating disease effects of hypercortisolemia, it is paramount that successful patient disease management and treatment includes individualized, multidisciplinary care, with close collaboration between endocrinologists, neurosurgeons, radiation oncologists, and general surgeons.
The primary, definitive therapy for patients with Cushing’s disease is pituitary surgery, generally performed via a transsphenoidal approach [3,4]. In the hands of the most experienced neurosurgeon, cure rates can range from 65 to 90% for microadenomas, with much lower rates for macroadenomas [5-8]. Patients with recurrent Cushing’s disease (the risk of recurrence over time is up to 20%) are sometimes considered for a second pituitary surgery, and more so if the initial surgery was performed at a center considered to be less experienced. However, remission rates are lower with a second surgical intervention [3]. Patients with recurrent Cushing’s disease may also be considered for radiation therapy. However, this requires several years of waiting for hypercortisolemia control and there is an increased risk of hypopituitarism. Medical therapy is required in the interim. Bilateral adrenalectomy is generally considered as a third-line option for patients with Cushing’s disease [3,5,9].
In most Cushing’s syndrome cases with residual hypercortisolemia, ketoconazole has been used as a first-line medical therapy. However, ketoconazole has not been approved by the US Food and Drug Administration (FDA) for Cushing’s treatment and recent FDA warnings that ketoconazole can cause severe liver injury and that there are harmful interactions with other medications, which could potentially further limit use. In those patients who cannot tolerate ketoconazole, metyrapone has historically been used, although availability is limited worldwide. However, in some countries, metyrapone can be available by directly contacting the manufacturer.
Pasireotide (Signifor), which has been approved for adult Cushing’s disease treatment by the FDA and the European Commission, is a somatostatin receptor ligand (SRL) with high binding affinity for somatostatin receptor 5 (sstr5). In a large phase III clinical trial, pasireotide was shown to reduce urine free cortisol (UFC) in most Cushing’s disease patients [10]. A subset of patients showed UFC normalization and tumor shrinkage, but the degree and severity of hyperglycemia was high. Other adverse events were similar to those seen with other SRLs. Studies in healthy volunteers showed that hyperglycemia associated with pasireotide is related to decreases in insulin secretion, glucagon-like peptide-1 and gastric inhibitory peptide, with no changes in insulin sensitivity [11]. Further studies are needed to address the management of pasireotide-induced hyperglycemia in Cushing’s disease.
Mifepristone, a glucocorticoid receptor blocker, was recently approved by the FDA for hyperglycemia in patients with Cushing’s syndrome. Improvements in signs and symptoms of Cushing’s and glycemic control were notable in the majority of patients in a phase III open-label study of the efficacy and safety of mifepristone [5]. Considering there is no biochemical parameter to assess efficacy, mifepristone dose should be adjusted based strictly on clinical improvements and tolerance. Patients need to be closely monitored for any adverse events, particularly adrenal insufficiency, hypokalemia and vaginal bleeding in women.
Few studies of cabergoline and retinoic acid in Cushing’s disease patients have shown promising results. Furthermore, in vitro data on epidermal growth factor receptor have opened the way for a better understanding and development of novel treatment targets and pathways.
While the use of combination therapy is on the increase and has the potential advantage of improving drug treatment efficacy while reducing side effects, it is important to keep in mind that combination drug therapy knowledge is largely driven by case reports and small open-label study data.
A recent systematic review reported an overall paucity of high-quality Cushing’s disease medical therapy data, with only one medication (pasireotide) achieving a “moderate” level of evidence rating [9]. The author recommends caution when comparing medical therapy efficacy rates because of variability in study design and quality. Furthermore, as mentioned above, there are other medical treatments that have been widely used off-label (i.e. for indications not approved by the FDA) for many years by physicians who are familiar with both the advantages and disadvantages of each treatment for Cushing’s disease.
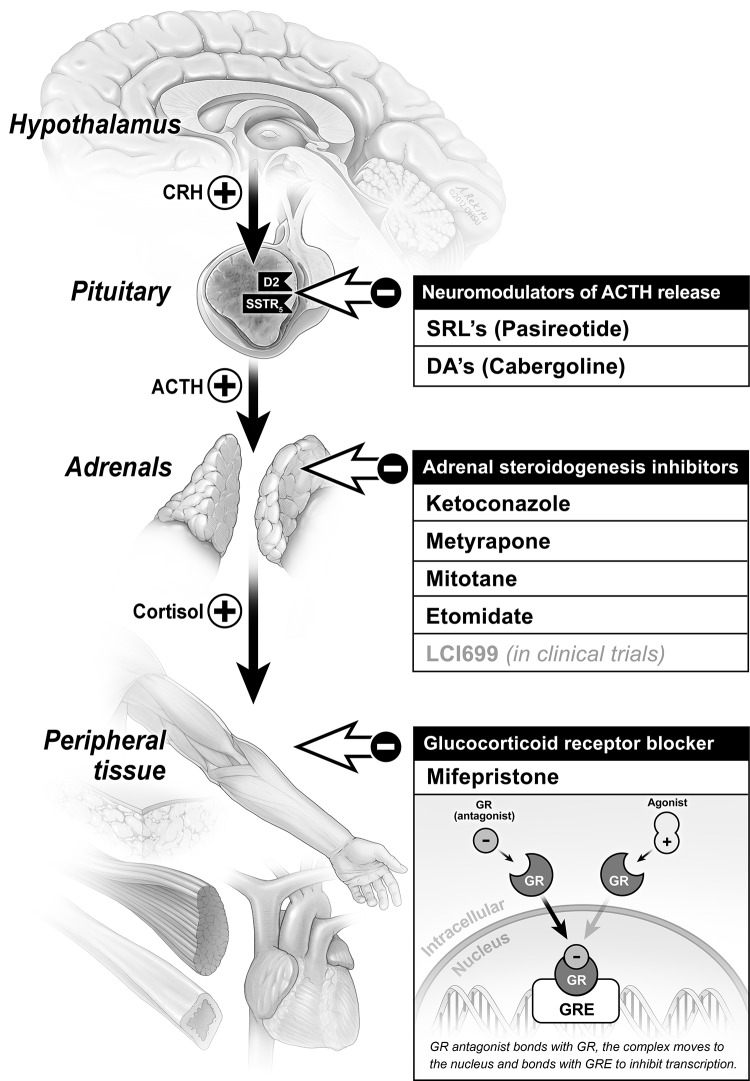
This commentary will address recent advances in the medical treatment of Cushing’s, with a focus on newly approved ACTH modulators and glucocorticoid receptor blockers (Figure 1).
Figure 1. Mechanism of action and targets for therapy in Cushing’s disease.
ACTH, adrenocorticotropic hormone; CRH, corticotropin-releasing factor; DA, dopamine agonist; GR, glucocorticoid receptor; GRE, glucocorticoid response element; SRL, somatostatin receptor ligand.
Reprinted from Neurosurg Clin N Am volume 23(4);653-668, Fleseriu, M., Medical management of persistent and recurrent Cushing’s disease, page 657, Copyright (2012), with permission from Elsevier.
Adrenocorticotropic hormone modulators
SRLs and dopamine agonists (DAs) can lower ACTH secretion caused by a pituitary adenoma and, as such, represent attractive drug options for Cushing’s disease treatment. Data on the effects of these medications on tumor size are limited [12]. However, there is a potential advantage in using them, particularly with large tumors [3,6,7,9,13].
Somatostatin receptor ligands:Pasireotide (Signifor)
Formerly referred to as SOM230, pasireotide diaspartate (SigniforTM, Novartis Pharmaceuticals) is a cyclic hexapeptide with a high affinity for somatostatin receptors sstr1, 2, 3 and 5 [14,15]. Affinity for subtypes 1 and 5 is high, while affinity for subtype 2 is lower when compared with octreotide.
As determined in a phase III clinical trial, patients were found to exhibit declines in urine free cortisol (UFC) levels at 6 months, median percentage changes in UFC levels from baseline to 6 months were -47.9% (600 μg group) and -47.9% (900 μg group); 15% (600 μg group) and 26% (900 μg group) of patients met the primary endpoint of a UFC level that was within the normal range without a pasireotide dose increase. If patients had a dose increase at month 3, this increased to 16% and 29%, respectively. Response rate in mild Cushing’s disease (UFC >1.5–2 x upper limit of normal) was even higher, up to 50% in the 900 μg group [10]. Moreover, the majority of patients who will respond to treatment can be identified within the first 2 months of treatment. Twenty patients (out of the 36 patients who achieved normalization of UFC levels at 6 months) maintained normal levels at 1 year, including some patients who had dose reductions. In the overall population, the mean percentage change in the midnight salivary cortisol level was -3.7% and -12.4% at months 6 and 12, respectively. The mean percentage change in plasma ACTH level was -12.8% and -16.9% at months 6 and 12, respectively. Patients showed significant improvements in signs and symptoms of hypercortisolism during the trial, including reductions in systolic (-6.1 mmHg) and diastolic (-3.7 mmHg) blood pressure, triglycerides, low-density lipoprotein cholesterol, and body weight (-6.7 kg). The time-course of many of these improvements closely followed that of UFC reduction. At month 6 and 12, improvements in facial rubor, supraclavicular and dorsal fat pads were seen in patients with available photographs. Patients also reported significant increases in health-related quality of life. Of the 75 patients who had measurable baseline magnetic resonance image pituitary tumors, tumor volume changed, on average at month 12, by -9.1 and -43.8% in the 600 and 900 μg groups, respectively [10].
The most common side effects reported in the most recent phase III trial seen in >18% of patients were diarrhea, nausea, hyperglycemia, cholelithiasis, headache, abdominal pain, fatigue and diabetes. Hyperglycemia-related effects occurred in up to 73% of the patients. 48% of the non-diabetic patients had a glycated hemoglobin >6.5% at study end. Hypothyroidism is also a well-recognized side effect due to inhibition of thyroid stimulating hormone (TSH) secretion. There is no information regarding glycemia control in Cushing’s disease patients treated with pasireotide. However, in 90 healthy volunteers, the mechanism of pasireotide-induced hyperglycemia has been noted as related to decreases in insulin secretion and incretin hormone responses, without changes in hepatic/peripheral insulin sensitivity [11].
Due to the presence of insulin resistance in the majority of patients with Cushing’s syndrome, a recently published proposal for management of hyperglycemia in pasireotide-treated Cushing’s disease patients recommends metformin as first-line medical treatment for those patients who develop new or worsening hyperglycemia. Adjunctive dipeptidyl peptidase 4 (DPP-4) inhibitor, sulfonylurea/glinide, and/or glucagon-like peptide-1 (GLP-1) analog could be required to achieve glycemic control. Metformin plus insulin is recommended if such combination therapy is not tolerated or insufficient, and early intervention with insulin is recommended on a case-by-case basis [16].
Few patients have been treated long-term with pasireotide. In an extension to the phase II study, reductions in mean UFC persisted in all patients who were on the study drug at month 24 [14]. Despite variability in serum cortisol levels, there was an overall reduction in serum cortisol and plasma ACTH relative to the core baseline that was maintained throughout the extension phase [14]. A recently published study case report illustrated long-term UFC control without escape or serious adverse event during more than 7 years of treatment with subcutaneous pasireotide [17]. A randomized, double-blind, multicenter, phase III study to evaluate the efficacy and safety of pasireotide long acting release (LAR) in patients with Cushing’s disease is now underway [18].
Dopamine agonists: Cabergoline
Pivonello et al. studied D2 receptor expression on corticotroph pituitary tumors, the effects of in vitro DA on ACTH secretion and the effect of in vivo DA therapy in 20 patients who underwent transsphenoidal resection for Cushing’s disease [19]. A three-month course of treatment (10 patients) with cabergoline (1–3 mg/week) was found to suppress cortisol in 60% of the patients with remission rates reported in 40%. Initial dosing was 1 mg/week. Monthly increases of 1 mg/week were made until normalization of daily urinary cortisol excretion occurred (up to a maximum dose of 3 mg/week). A prospective, open-label, single-arm study [20] with short-term (5 months) and long-term (1 year) evaluations in 20 patients showed a response rate of approximately 30%, which was dependent on the endpoint.
More recently, Godbout et al. performed a retrospective analysis of 30 patients with Cushing’s disease, treated with 0.5–6 mg/week of cabergoline [21]. The initial cabergoline dose was 0.5–1 mg/week, increasing by 0.5–1.0 mg/week at 1 or 2 month intervals until reaching a maximal dose of 6 mg/week or complete remission (defined as normalization of UFC). Approximately 40% of patients achieved remission in 4.2 months. Long-term treatment resulted in complete remission in 30% of patients with average doses of 2.1 mg/week, with an average treatment duration of 37 months. While cardiac valve dysfunction is a concern with high-dose therapy used in patients with Parkinson’s disease, this has not been observed in pituitary studies, although doses were lower than those used for Cushing’s. Cabergoline is not FDA approved for the treatment of Cushing’s, but these results are promising.
Retinoic acid
The retinoic acid receptor is a type II non-steroid nuclear receptor involved with transcriptional regulation. In a study by Pecori Giraldi et al., using retinoic acid in Cushing’s disease, a marked reduction in UFC levels (22–73% of baseline) in 5 of 7 patients (“responders”), and UFC normalization in 3 patients was noted [22]. In patients who were considered retinoic acid treatment responders, mean plasma ACTH levels decreased in the first month with a subsequent return to pretreatment levels. Changes in plasma cortisol were not significant at any study time-point.
Epidermal growth factor receptor blockers
The epidermal growth factor receptor (EGFR) has recently been studied as a therapeutic target for Cushing’s disease. Gefitinib (an EGFR tyrosine kinase inhibitor) was shown to attenuate pro-opiomelanocortin expression, inhibit corticotroph tumor cell proliferation, and induce apoptosis in surgically resected human and canine corticotroph cultured tumors. Furthermore, treatment with gefitinib decreased tumor size, corticosterone levels and reversed signs of hypercortisolemia, including elevated glucose levels and excess omental fat in mice. In mice, these results indicate that inhibiting EGFR signaling may be a novel strategy for treating Cushing’s disease [23].
Glucocorticoid receptor antagonism: mifepristone
Mifepristone binds to the glucocorticoid receptor with a 4-fold higher affinity than dexamethasone and an 18-fold higher affinity than cortisol [7]. Since the 1980s, several case reports and case series have reported mifepristone treatment for refractory Cushing’s syndrome [5,13,24]. In 2012, mifepristone (Korlym, Corcept Therapeutics) was FDA approved for treatment of hyperglycemia associated with Cushing’s syndrome. A large open-label, 24-week multicenter study (study of the efficacy and safety of CORLUX in the treatment of endogenous Cushing’s syndrome or SEISMIC) demonstrated a reduction in glucose, and improvement in a number of other parameters in 50 Cushing’s syndrome mifepristone-treated patients, 43 of whom had Cushing’s disease [25]. There were two patient groups, determined by diabetes or hypertension presence, treated with mifepristone 300–1200 mg (mean 900 mg). Overall, 60% of the patients with glucose intolerance or diabetes (n = 29; P <0.0001) were responders (defined as a ≥25% reduction in glucose on a standard oral glucose tolerance test from baseline to 24 weeks). There was a continued improvement in glucose tolerance measured at each of the evaluations at week 6, 10, and 16, and at week 24. Seven of 12 patients taking insulin at baseline cut their daily dose by at least 50% and glycated hemoglobin (HbA1c) also improved over the study course. In all hypertensive patients (in both groups n = 40), 42.5% had ≥5 mm decrease in diastolic blood pressure and 52% had either a decrease in diastolic blood pressure or a reduction in antihypertensive medications at week 24. Over half of the patients experienced weight loss (≥5% compared to baseline; P < 0.001) and the mean reduction in waist circumference (compared to baseline) was 6.8 cm in females and 8.4 cm for males (P <0.0001 for both groups) [25]. An independent data review board assessed overall clinical response based on data from eight clinical categories, including glucose homeostasis, blood pressure, lipids, body composition, strength, psychiatric and cognitive function, physical appearance, and quality of life. Global clinical response was determined to have improved in 87% of patients [26].
In the SEISMIC study, as expected, hypokalemia was common (mild to moderate) and associated with alkalosis and edema. There were three reported cases of severe hypokalemia (potassium ≤2.5 mmol/l), which in all cases was responsive to high dose spironolactone [25]. Antiprogestin effects of mifepristone were evident; an increase in endometrial thickness was observed in half of the female subjects. Five women experienced vaginal bleeding (two with prolonged bleeding after stopping mifepristone) and, while three reported no bleeding, they had endometrial thickening >20 mm at 6 months and underwent dilation and curettage. Overall, risk-benefit analysis for mifepristone in Cushing’s disease patients was acceptable [5,25]. Long-term mifepristone safety and outcome data are still to come and studies with larger Cushing’s disease patient populations are needed.
Additional post hoc analysis of the clinical response data was recently reported, and demonstrated a progressive clinical benefit of mifepristone, with the greatest proportion of responses by the end of the study at 24 weeks. While twice as many women as men were evaluated, the authors suggest that there may be a gender-dependent effect with mifepristone as there was a more rapid clinical benefit in men, although there was no significant gender difference by the end of the study [26].
72% of the patients with Cushing’s disease treated with mifepristone had at least a two-fold increase in ACTH, cortisol or both. Practitioners must rely on the clinical response and doses should be titrated based on the symptoms (mood and cognition), clinical features (body weight and composition and blood pressure) and biochemical parameters, such as glucose and HbA1c.
Adverse reactions that occurred in ≥20% of the patients included nausea, fatigue, headache, hypokalemia, arthralgia, vomiting, peripheral edema, hypertension, dizziness, decreased appetite and endometrial hyperplasia. Other abnormalities included a reduction in high-density lipoprotein levels and asymptomatic elevations in TSH. Recommended monitoring should include measurement of serum potassium, clinical assessment of adrenal insufficiency and yearly vaginal ultrasound in women to evaluate for endometrial hyperplasia [5].
The anti-glucocorticoid effect of mifepristone is dose dependent and was observed for single doses of 4 mg/kg. Effects are reversible by glucocorticoid administration at high doses (1 mg of dexamethasone usually antagonizes the effects of 400 mg of mifepristone). Special precautions should be taken in the treatment of adrenal insufficiency, due to the long half-life of mifepristone and its strong glucocorticoid receptor affinity. Dexamethasone is the preferred glucocorticoid, usually in high doses until any acute situation has stabilized.
Steroidogenesis inhibitors
Adrenal blocking drugs suppress adrenal cortisol production via inhibition of steroidogenic enzymes. Ketoconazole and metyrapone are most frequently used for this purpose; however, chronic treatment with these drugs can be limited by side effects like hepatotoxicity (ketoconazole) and increased androgen and mineralocorticoid production (metyrapone). Etomidate can be used to rapidly reverse cortisol excess in patients with acute complications of (severe) hypercortisolism, such as psychosis. All the steroidogenisis inhibitors are currently used as “off label” in the treatment of Cushing’s syndrome [5-7,13,27].
Ketoconazole
Ketoconazole is an antifungal agent that inhibits a number of steroidogenic enzymes, including 11β-hydroxylase, 17α-hydroxylase and 18-hydroxylase, resulting in a reduction of adrenal steroid production. In the largest retrospective study eligible for inclusion in this review [28], 38 patients with Cushing’s disease received ketoconazole, as a primary treatment or after unsuccessful surgery, at a starting dose of 200–400 mg/day, up-titrated to a maximum of 1200 mg/day until biochemical remission. Urine free cortisol was normalized in 17 of 38 patients (45%). Biochemical control was achieved with ketoconazole during the first month in eight patients and 3 months after dose titration in nine patients. Blood pressure and weight were also reduced in these responders. Of the remaining patients with uncontrolled disease, five patients initially had normalized UFC after treatment, but later experienced escape from response (secondary failure of medication). Therefore, the overall rate of escape from response among patients who had normalized UFC levels at some point during the study was 5 of 22 (23%). However, no factor predictive of disease control other than gender (all patients with controlled disease were female) was noted. Gastrointestinal symptoms are commonly reported with ketoconazole treatment, for example, in the study included in this analysis, five patients discontinued due to nausea and diarrhea in the first week of treatment. Although rare, hepatotoxicity is a serious concern, and the FDA issued a black-box warning for potential liver problems.
Etomidate
Etomidate, an intravenous medication used for anesthesia induction, inhibits cholesterol side chain cleavage and 11-B hydroxylase. Etomidate has been successfully used as a short-term treatment in critically ill Cushing’s syndrome patients unable to take oral medications. Etomidate is available as an intravenous preparation only, which makes it an ideal option in emergent settings for rapid control of hypercortisolemia [29].
Mitotane
Mitotane reduces cortisol synthesis through the inhibition of 11B-hydroxylase, 18-hydroxylase, 3-α hydroxylase, hydroxysteroid dehydrogenase and several cholesterol side chain cleavage enzymes. It is also an adrenolytic agent at doses greater than 4 g per day, and is used most often for the treatment of adrenocortical carcinoma.
Mitotane has also been studied for the management of Cushing’s syndrome from both ACTH-dependent and ACTH-independent causes [6,13,30,31]. Adjustments in mitotane dose are usually based on monitoring plasma levels (target: 10 mg/l), which allows adequate control of hypercortisolism in the majority of patients with slow onset of action (weeks or months). Mitotane is unique in that this long-lasting action could potentially limit escape phenomenon.
LCI699
LCI699 is a potent inhibitor of aldosterone synthase and 11β-hydroxylase currently under investigation in a proof-of-concept study in patients with Cushing’s disease [19,32]. Since 11β-hydroxylase catalyzes the final step of cortisol synthesis, LCI699 is a potential new treatment for all forms of Cushing’s syndrome and has demonstrated efficacy with a satisfactory safety profile in a small proof-of-concept study in patients with Cushing’s disease.
The primary endpoint (defined as normal or a 50% decrease in UFC) was achieved by all 12 patients who completed the active treatment phase. UFC normalization was associated with median LCI699 doses of between 5 and 10 mg twice daily. At the end of the study, mean systolic blood pressure decreased by 13.1 mmHg from baseline. LCI699 was generally well tolerated; the most frequently reported adverse events were fatigue, nausea and headache. Five patients experienced ACTH level increases >two-fold compared with baseline. Four patients experienced study drug-related hypokalemia (potassium <3.5 mmol/l; minimum 3.1 mmol/l). Hyperandrogenism in women could be expected due to mechanism of action. However, for now, there are no available data. There were no serious adverse events of suspected drug relationship.
Combination therapies
The rationale behind combination therapy is that the treatment of Cushing’s disease patients with a somatostatin receptor ligand and a DA may have additive or synergistic effects in decreasing ACTH secretion from corticotroph adenomas. There are a limited number of studies that have examined this scenario.
In a study by Feelders and Hofland of 17 Cushing’s disease patients, pasireotide at doses of 100–250 μg three times per day was shown to normalize UFC levels in five patients, and the addition of cabergoline (0.5–1.5 mg every other day) normalized UFC levels in four further patients. Among the remaining eight patients, subsequent addition of ketoconazole (200 mg three times daily) normalized UFC levels in six, leaving only two patients who still had elevated UFC levels [1]. Thus, sequential therapy using these three agents shows promise, but requires further efficacy and safety study.
Cabergoline and ketoconazole have also been used in combination [33,34]. Vilar et al. studied cabergoline monotherapy in 12 patients after failed surgery and, after 6 months of treatment in doses of up to 3 mg/week, nine patients did not adequately respond. The addition of ketoconazole (up to 400 mg/day) led to normalized UFC in another six of nine patients, while the remaining patients achieved a significant reduction in UFC of 44–52% [33].
Recently, a triple combination of adrenal steroidogenesis inhibitors as an alternative to urgent adrenalectomy has also been discussed [35].
Aggressive corticotroph adenomas
Aggressive pituitary adenomas and carcinomas, though rare, pose a significant clinical challenge. Temozolomide (Temodar® or Temodal®, Schering Corporation, Kenilworth, NJ) is an oral alkylating agent approved by the FDA for the treatment of glioblastoma multiforme. It has 100% oral bioavailability and readily crosses the blood-brain barrier. Furthermore, the efficacy of temozolomide for treating aggressive pituitary adenomas and carcinomas, including corticotroph adenomas, has been reported in a limited number of patients [27,36]. Contrary to glioblastoma multiforme data, the expression of O6-methylguanine-DNA methyl-transferase has no association with aggressiveness and relapse of pituitary adenomas, and temozolomide-based combination therapy may also expand treatment options for patients with aggressive pituitary adenomas or carcinomas. Temozolomide’s potential to augment the effectiveness of radiotherapy, as is observed with other intracranial tumors, should also be investigated for pituitary tumors. Salvage medical therapy with temozolomide should be considered in the treatment armamentarium of all aggressive life-threatening pituitary tumors after failure of conventional treatments.
Conclusion
Since first described by Harvey Cushing in 1912, Cushing’s disease has remained a major clinical challenge to physicians and patients. After failed pituitary surgery, repeat pituitary surgery, or bilateral adrenalectomy and radiotherapy can result in control of hypercortisolism, but they are associated with variable response rates and significant risks. There have been several recent reports detailing the use of medical therapy to control hypercortisolemia prior to surgery to optimize the patient’s preoperative state, to control the metabolic effects and help reduce the anesthesiological risk. Moreover, medical treatment plays a pivotal role in the treatment of patients waiting for the full effect of pituitary radiotherapy and is often essential for patients where surgery has failed to control Cushing’s disease, since it helps in reducing or normalizing hypercortisolemia.
This review provides a synopsis of new advances in the development of pituitary-active drugs as well as receptor blockers of glucocorticoid action: effective pharmacological agents capable of chronically reversing biochemical and clinical manifestations of hypercortisolemia in Cushing’s syndrome.
In the future, Cushing’s syndrome management may involve combination drug therapy via different pathways. For example, combining low-dose pasireotide and cabergoline or low-dose pasireotide and ketoconazole could potentially increase the number of patients whose Cushing’s syndrome can be controlled while minimizing adverse effects. Furthermore, a better understanding of corticotroph adenoma receptor expression patterns may pave the way for the development of therapies specifically tailored to individual patients following surgical pathology analysis. Finally, however, monitoring therapy success will remain a challenge, both clinically and biochmically.
Acknowledgments
The author thanks Shirley McCartney, PhD, for editorial assistance.
Abbreviations
- ACTH
adrenocorticotropic hormone
- DA
dopamine agonist
- EGFR
epidermal growth factor receptor
- FDA
US Food and Drug Administration
- HbA1c
glycated hemoglobin
- LAR
long acting release
- SRL
somatostatin receptor ligand
- sstr
somatostatin receptor
- TSH
thyroid stimulating hormone
- UFC
urine free cortisol
Disclosures
Dr. Fleseriu has received research grants to Oregon Health & Science University (OHSU) from Novartis and Corcept Therapeutics and has been an ad hoc consultant for Genentech, Ipsen and Novartis. Dr. Fleseriu has received payments for consulting for Novartis; this potential conflict of interest has been reviewed and managed by OHSU.
The electronic version of this article is the complete one and can be found at: http://f1000.com/prime/reports/m/6/18
References
- 1.Feelders RA, Hofland LJ. Medical treatment of Cushing’s disease. J Clin Endocrinol Metab. 2013;98:425–38. doi: 10.1210/jc.2012-3126. [DOI] [PubMed] [Google Scholar]
- 2.Clayton RN, Raskauskiene D, Reulen RC, Jones PW. Mortality and morbidity in Cushing’s disease over 50 years in Stoke-on-Trent, UK: audit and meta-analysis of literature. J Clin Endocrinol Metab. 2011;96:632–42. doi: 10.1210/jc.2010-1942. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/8537957
- 3.Biller BMK, Grossman AB, Stewart PM, Melmed S, Bertagna X, Bertherat J, Buchfelder M, Colao A, Hermus AR, Hofland LJ, Klibanski A, Lacroix A, Lindsay JR, Newell-Price J, Nieman LK, Petersenn S, Sonino N, Stalla GK, Swearingen B, Vance ML, Wass JAH, Boscaro M. Treatment of adrenocorticotropin-dependent Cushing’s syndrome: a consensus statement. J Clin Endocrinol Metab. 2008;93:2454–62. doi: 10.1210/jc.2007-2734. [DOI] [PMC free article] [PubMed] [Google Scholar]; http://f1000.com/prime/718270046
- 4.Fleseriu M, Loriaux DL, Ludlam WH. Second-line treatment for Cushing’s disease when initial pituitary surgery is unsuccessful. Curr Opin Endocrinol Diabetes Obes. 2007;14:323–8. doi: 10.1097/MED.0b013e328248b498. [DOI] [PubMed] [Google Scholar]
- 5.Fleseriu M, Molitch ME, Gross C, Schteingart DE, Vaughan TB, Biller BMK. A new therapeutic approach in the medical treatment of Cushing’s syndrome: glucocorticoid receptor blockade with mifepristone. Endocr Pract. 2013;19:313–26. doi: 10.4158/EP12149.RA. [DOI] [PubMed] [Google Scholar]
- 6.Fleseriu M, Petersenn S. Medical management of Cushing’s disease: what is the future? Pituitary. 2012;15:330–41. doi: 10.1007/s11102-012-0397-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nieman LK. Update in the medical therapy of Cushing’s disease. Curr Opin Endocrinol Diabetes Obes. 2013;20:330–4. doi: 10.1097/MED.0b013e3283631809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hameed N, Yedinak CG, Brzana J, Gultekin SH, Coppa ND, Dogan A, Delashaw JB, Fleseriu M. Remission rate after transsphenoidal surgery in patients with pathologically confirmed Cushing’s disease, the role of cortisol, ACTH assessment and immediate reoperation: a large single center experience. Pituitary. 2013;16:452–8. doi: 10.1007/s11102-012-0455-z. [DOI] [PubMed] [Google Scholar]
- 9.Gadelha MR, Vieira Neto L. Efficacy of medical treatment in Cushing’s disease: a systematic review. Clin Endocrinol (Oxf) 2014;80:1–12. doi: 10.1111/cen.12345. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718142049
- 10.Colao A, Petersenn S, Newell-Price J, Findling JW, Gu F, Maldonado M, Schoenherr U, Mills D, Salgado LR, Biller BMK. A 12-month phase 3 study of pasireotide in Cushing’s disease. N Engl J Med. 2012;366:914–24. doi: 10.1056/NEJMoa1105743. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/717970454
- 11.Henry RR, Ciaraldi TP, Armstrong D, Burke P, Ligueros-Saylan M, Mudaliar S. Hyperglycemia associated with pasireotide: results from a mechanistic study in healthy volunteers. J Clin Endocrinol Metab. 2013;98:3446–53. doi: 10.1210/jc.2013-1771. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718020253
- 12.Shimon I, Rot L, Inbar E. Pituitary-directed medical therapy with pasireotide for a corticotroph macroadenoma: pituitary volume reduction and literature review. Pituitary. 2012;15:608–13. doi: 10.1007/s11102-012-0427-3. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718205963
- 13.Tritos NA, Biller BMK. Advances in medical therapies for Cushing’s syndrome. Discov Med. 2012;13:171–9. [PubMed] [Google Scholar]
- 14.Boscaro M, Bertherat J, Findling J, Fleseriu M, Atkinson AB, Petersenn S, Schopohl J, Snyder P, Hughes G, Trovato A, Hu K, Maldonado M, Biller BMK. Extended treatment of Cushing’s disease with pasireotide: results from a 2-year, Phase II study. Pituitary. 2013 doi: 10.1007/s11102-013-0503-3. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boscaro M, Ludlam WH, Atkinson B, Glusman JE, Petersenn S, Reincke M, Snyder P, Tabarin A, Biller BMK, Findling J, Melmed S, Darby CH, Hu K, Wang Y, Freda PU, Grossman AB, Frohman LA, Bertherat J. Treatment of pituitary-dependent Cushing’s disease with the multireceptor ligand somatostatin analog pasireotide (SOM230): a multicenter, phase II trial. J Clin Endocrinol Metab. 2009;94:115–22. doi: 10.1210/jc.2008-1008. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/1157701
- 16.Reznik Y, Bertherat J, Borson-Chazot F, Brue T, Chanson P, Cortet-Rudelli C, Delemer B, Tabarin A, Bisot-Locard S, Vergès B. Management of hyperglycaemia in Cushing’s disease: experts’ proposals on the use of pasireotide. Diabetes Metab. 2013;39:34–41. doi: 10.1016/j.diabet.2012.10.005. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/717967964
- 17.Targher G. Pasireotide in Cushing’s disease. N Engl J Med. 2012;366:2134. doi: 10.1056/NEJMc1204078. author reply 2134-5. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718270047
- 18.Clinical Trials.gov: A Randomized, Double-blind, Multicenter, Phase III Study to Evaluate the Efficacy and Safety of Pasireotide LAR in Patients With Cushing’s Disease. [ http://clinicaltrials.gov/show/NCT01374906]
- 19.Pivonello R, Fleseriu M, Guignat L, Zhang Y, Robinson P, Taylor A, Watson C, Maldonado M, Hamrahian AH, Boscaro M, Biller BM. Patients with Cushing Disease Achieve Normal Urinary Cortisol with LCI699, a Potent 11β-Hydroxylase Inhibitor: Preliminary Results from a Multicenter, Proof-of-Concept Study [abstract] Endocr Rev. 2012;33:OR49–41. [Google Scholar]
- 20.Lila AR, Gopal RA, Acharya SV, George J, Sarathi V, Bandgar T, Menon PS, Shah NS. Efficacy of cabergoline in uncured (persistent or recurrent) Cushing disease after pituitary surgical treatment with or without radiotherapy. Endocr Pract. 2010;16:968–76. doi: 10.4158/EP10031.OR. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718270048
- 21.Godbout A, Manavela M, Danilowicz K, Beauregard H, Bruno OD, Lacroix A. Cabergoline monotherapy in the long-term treatment of Cushing’s disease. Eur J Endocrinol. 2010;163:709–16. doi: 10.1530/EJE-10-0382. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718270049
- 22.Pecori Giraldi F, Ambrogio AG, Andrioli M, Sanguin F, Karamouzis I, Karamouzis I, Corsello SM, Scaroni C, Arvat E, Pontecorvi A, Pontercorvi A, Cavagnini F. Potential role for retinoic acid in patients with Cushing’s disease. J Clin Endocrinol Metab. 2012;97:3577–83. doi: 10.1210/jc.2012-2328. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718205965
- 23.Fukuoka H, Cooper O, Ben-Shlomo A, Mamelak A, Ren S, Bruyette D, Melmed S. EGFR as a therapeutic target for human, canine, and mouse ACTH-secreting pituitary adenomas. J Clin Invest. 2011;121:4712–21. doi: 10.1172/JCI60417. [DOI] [PMC free article] [PubMed] [Google Scholar]; http://f1000.com/prime/13414979
- 24.Carmichael JD, Fleseriu M. Mifepristone: is there a place in the treatment of Cushing’s disease? Endocrine. 2013;44:20–32. doi: 10.1007/s12020-012-9846-1. [DOI] [PubMed] [Google Scholar]
- 25.Fleseriu M, Biller BMK, Findling JW, Molitch ME, Schteingart DE, Gross C. Mifepristone, a glucocorticoid receptor antagonist, produces clinical and metabolic benefits in patients with Cushing’s syndrome. J Clin Endocrinol Metab. 2012;97:2039–49. doi: 10.1210/jc.2011-3350. [DOI] [PubMed] [Google Scholar]
- 26.Katznelson L, Loriaux DL, Feldman D, Braunstein GD, Schteingart DE, Gross C. Global clinical response in Cushing’s syndrome patients treated with mifepristone. Clin Endocrinol (Oxf) 2013 doi: 10.1111/cen.12332. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bertagna X, Guignat L. Approach to the Cushing’s disease patient with persistent/recurrent hypercortisolism after pituitary surgery. J Clin Endocrinol Metab. 2013;98:1307–18. doi: 10.1210/jc.2012-3200. [DOI] [PubMed] [Google Scholar]
- 28.Castinetti F, Morange I, Jaquet P, Conte-Devolx B, Brue T. Ketoconazole revisited: a preoperative or postoperative treatment in Cushing’s disease. Eur J Endocrinol. 2008;158:91–9. doi: 10.1530/EJE-07-0514. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718270050
- 29.Heyn J, Geiger C, Hinske CL, Briegel J, Weis F. Medical suppression of hypercortisolemia in Cushing’s syndrome with particular consideration of etomidate. Pituitary. 2012;15:117–25. doi: 10.1007/s11102-011-0314-3. [DOI] [PubMed] [Google Scholar]
- 30.Baudry C, Coste J, Bou Khalil R, Silvera S, Guignat L, Guibourdenche J, Abbas H, Legmann P, Bertagna X, Bertherat J. Efficiency and tolerance of mitotane in Cushing’s disease in 76 patients from a single center. Eur J Endocrinol. 2012;167:473–81. doi: 10.1530/EJE-12-0358. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718270051
- 31.Donadille B, Groussin L, Waintrop C, Abbas H, Tenenbaum F, Dugué M, Coste J, Bertagna X, Bertherat J. Management of Cushing’s syndrome due to ectopic adrenocorticotropin secretion with 1,ortho-1, para’-dichloro-diphenyl-dichloro-ethane: findings in 23 patients from a single center. J Clin Endocrinol Metab. 2010;95:537–44. doi: 10.1210/jc.2009-1317. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718270052
- 32.Bertagna X, Pivonello R, Fleseriu M, Zhang Y, Robinson P, Taylor A, Watson CE, Maldonado M, Hamrahian AH, Boscaro M, Biller B. LCI699, a potent 11β-hydroxylase inhibitor, normalizes urinary cortisol in patients with Cushing’s disease: results from a multicenter, proof-of-concept study. J Clin Endocrinol Metab. 2013 doi: 10.1210/jc.2013-2117. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 33.Vilar L, Naves LA, Azevedo MF, Arruda MJ, Arahata CM, Moura E, Silva L, Agra R, Pontes L, Montenegro L, Albuquerque JL, Canadas V. Effectiveness of cabergoline in monotherapy and combined with ketoconazole in the management of Cushing’s disease. Pituitary. 2010;13:123–9. doi: 10.1007/s11102-009-0209-8. [DOI] [PubMed] [Google Scholar]; http://f1000.com/prime/718270053
- 34.Barbot M, Albiger N, Ceccato F, Zilio M, Frigo AC, Denaro L, Mantero F, Scaroni C. Combination therapy for Cushing’s disease: effectiveness of two schedules of treatment. Should we start with cabergoline or ketoconazole? Pituitary. 2013 doi: 10.1007/s11102-013-0475-3. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 35.Kamenický P, Droumaguet C, Salenave S, Blanchard A, Jublanc C, Gautier J, Brailly-Tabard S, Leboulleux S, Schlumberger M, Baudin E, Chanson P, Young J. Mitotane, metyrapone, and ketoconazole combination therapy as an alternative to rescue adrenalectomy for severe ACTH-dependent Cushing’s syndrome. J Clin Endocrinol Metab. 2011;96:2796–804. doi: 10.1210/jc.2011-0536. [DOI] [PubMed] [Google Scholar]
- 36.Dillard TH, Gultekin SH, Delashaw JB, Yedinak CG, Neuwelt EA, Fleseriu M. Temozolomide for corticotroph pituitary adenomas refractory to standard therapy. Pituitary. 2011;14:80–91. doi: 10.1007/s11102-010-0264-1. [DOI] [PubMed] [Google Scholar]