Abstract
Background
In patients admitted to the emergency department with complaints of chest pain and unstable angina pectoris, ST-elevation MI scoring is done according to risk factors used to calculate risks of urgent revascularization, MI, and death within 14 days. For this calculation, the most widely used scoring system is TIMI risk score.
Materila/Methods
In this prospective, cross-sectional descriptive study, we evaluated and compared the effectiveness of TIMI and Gensini scores of patients with chest pain who were admitted to Hacettepe University Hospitals Emergency Department between March 2011 and September 2011 and who underwent coronary angiography.
Results
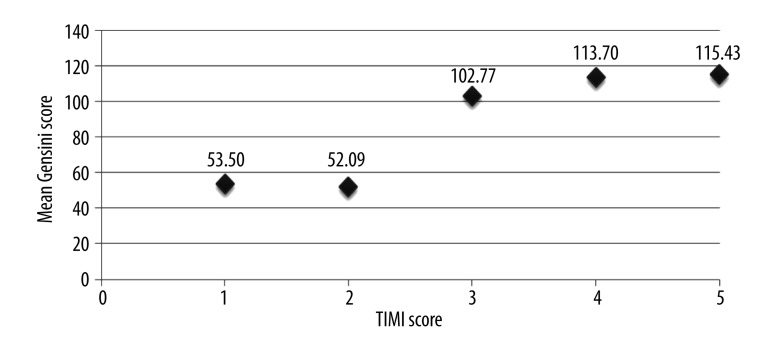
The mean (range) age of 165 patients was 62 (31–88) years. Moderate correlation between TIMI and Gensini scores was detected (mean values of Gensini score for TIMI 1 is 53.50, for TIMI 2 it is 52.09, for TIMI 3 it is 102.77, for TIMI 4 it is 113.70, and for TIMI 5 it is 115.43). There was also a positive correlation between TIMI score and the results.
Conclusions
TIMI risk stratification score is safe and easy to use for rapid assessment of mortality and MI risk, despite its low possibility of predicting the outcome.
MeSH Keywords: Acute Coronary Syndrome, Coronary Angiography, Gensini Score, TIMI Score, Myocardial Infarction
Background
Acute coronary syndrome (ACS) occurs due to myocardial ischemia and presents with symptoms and clinical findings. The most commonly used scoring system to identify the risk of heart attack in patients presenting to the emergency room is the TIMI (Thrombolysis In Myocardial Infarction) risk score. By using this score, one can calculate the risk of MI, as well as risk of death and emergency revascularization at 14 days, in unstable angina pectoris, non-ST elevated MI (myocardial infarction) patients. Another parameter used to evaluate the severity of coronary artery disease is the Gensini score. There are 2 coronary angiography scores: vascular scoring and stenosis scoring. These techniques have been described by Gensini. According to the angiographic degree of stenosis, narrowing between 0–25%, 25–50%, 50–75%, 75–90%, 90–99%, and 100%, stenosis is scored as, 1, 2, 4, 8, 16, and 32 points, respectively [1,2].
In this study, we evaluated the power of the TIMI score in predicting the postangiography Gensini score, and the power of TIMI and Gensini scores in predicting the treatment plans after coronary angiography.
Material and Methods
This prospective, cross-sectional, descriptive study was conducted with permission from the Hacettepe University Scientific Research Ethics Council, number HEK 11/42-16. Throughout the course of the research, patients who presented to the E.R. and who were consulted with the department of cardiology provided informed consent after a brief presentation. The results of the angiography were recorded by the principal investigator. For standardization purposes, all attending physicians and residents underwent a brief presentation on TIMI and Gensini scores, and the nature and structure of the study. The TIMI and Gensini scoring research forms were filled out by senior residents who had at least 3 years of post-graduate medical training, under the supervision of attending physicians.
Inclusion criteria
Patients who presented to the E.R. with chest pain and had a differential diagnosis of acute coronary syndrome, and who underwent coronary angiography and followed-up, were included in the study.
Exclusion criteria
Patients were excluded who had ST elevation myocardial infarction, known coronary artery disease, who were referred for by-pass (surgery), had non-cardiac etiology for chest pain, and who came to the ER with chest pain but did not undergo coronary angiography.
Statistical analysis
The data obtained were evaluated using SPSS 15.0 for Windows and NCSS 2007. The patients were included in the study according to whether they underwent coronary angiography. They were further sub-classified into 7 groups with respect to their TIMI scores. When the Gensini scores showed normal distribution, the presence of statistically significant difference was tested using the one-way analysis of variance; when distribution was not normal, the Kruskal-Wallis test was used. For multiple comparisons, LSD (least significant difference) test, Kruskal-Wallis test, and Z-Value Test (Dunn’s Test) were used. The relationship between qualitative variables was analyzed using the chi-square test. The relationship between the TIMI and Gensini scores was tested using Spearman’s rho correlation coefficient. For numeric variables we present descriptive statistics, mean, standard deviation, median, and minimum and maximum values. For qualitative variables, number counts and percentages are given. The statistical significance of the difference between independent groups with normal distribution was tested using the independent samples t-test. For groups with no normal distribution, the Mann-Whitney U test was used. For the analysis of the statistical significance of the difference between multiple group means, the one-way ANOVA test was used. P value less than 0.05 were considered as significant.
Results
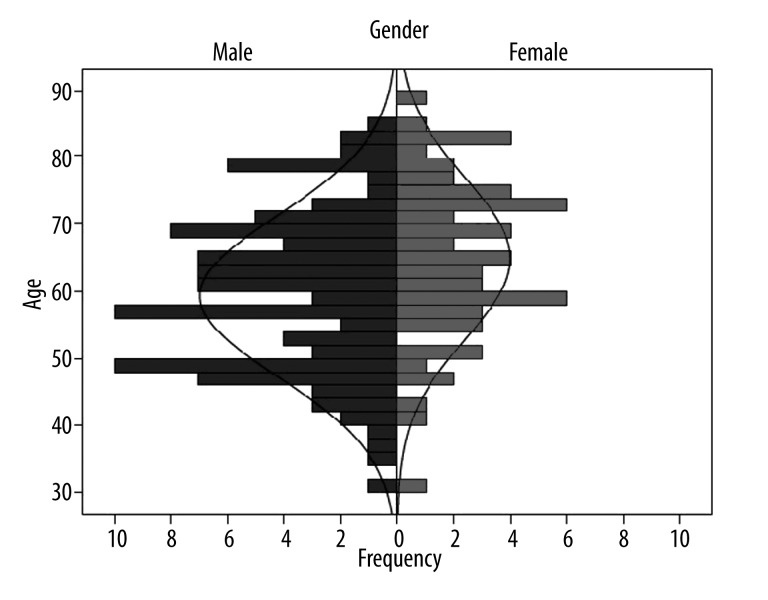
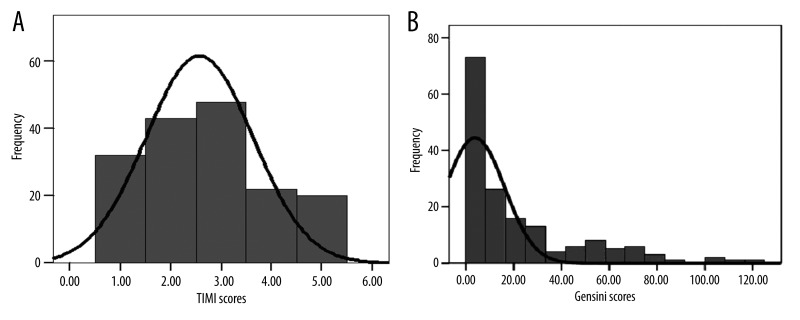
A total of 165 patients were included in the study. The median age was 62 (range 31–88) years; 105 were male (63.6%). The mean age of the female patients was significantly higher than the male patients (64.95±12.03 vs. 59.34±12.00, p=0.004, t=−2.882). The distribution of the patients with respect to age is shown in Figure 1. There was a mild relationship between the TIMI and Gensini scores (Spearman’s rho=0.552, p<0.05). The distribution of the patient’s TIMI and Gensini scores is given in Figure 2. The average Gensini scores of the patients with respect to the TIMI scores are given in Figure 3.
Figure 1.
Distribution of patients with respect to gender and age.
Figure 2.
Distribution of Patients’ TIMI (A) and Gensini (B) scores.
Figure 3.
Correlation of patients’ TIMI and Gensini scores.
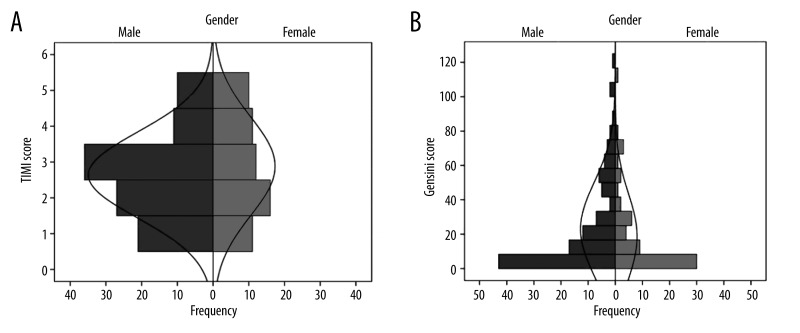
The TIMI and Gensini scores did not show normal distribution with respect to patient sex. The TIMI and Gensini scores were similar in both groups (p>0.05). The distribution of the scores with respect to sex is given in Figure 4. The relationship of TIMI scores and outcomes is summarized in Table 1. There was a positive correlation between the TIMI scores and outcomes (p<0.001, likelihood ratio=91.761). Most patients with low TIMI scores were only monitorized.
Figure 4.
Distribution of TIMI (A) and Gensini (B) Scores with respect to gender.
Table 1.
TIMI score-outcomes cross table.
| Outcome | Total | |||||
|---|---|---|---|---|---|---|
| Medical monitorization (n) | Stent (n) | By-pass (n) | None* (n) | |||
| TIMI Score | 1 | 25 | 4 | 3 | 0 | 32 |
| 2 | 37 | 4 | 1 | 1 | 43 | |
| 3 | 11 | 19 | 10 | 8 | 48 | |
| 4 | 4 | 8 | 6 | 4 | 22 | |
| 5 | 0 | 10 | 5 | 5 | 20 | |
| Total | 77 | 45 | 25 | 18 | 165 | |
Patients who would not benefit from neither medical nor surgical intervention n: number of patients.
There was no relationship between the patients’ outcomes and sex and age. The relationship of final outcome and age and sex is given in Table 2. Patients who underwent coronary angiography had an increased rate of vascular occlusion, and this showed a parallel, statistically significant increase with age (p=0.025).
Table 2.
Distribution of the patient outcomes with respect to gender and age.
| Outcome | Age (years) | Gender | ||||
|---|---|---|---|---|---|---|
| Minimum | Maximum | Mean | Std. deviation | Male (n) | Female (n) | |
| Monitorization | 31 | 88 | 58,62 | 12,521 | 48 | 29 |
| Stent application | 42 | 85 | 62,02 | 11,698 | 28 | 17 |
| By-pass | 42 | 84 | 65,56 | 13,058 | 18 | 7 |
| None* | 49 | 83 | 65,78 | 8,902 | 11 | 7 |
| Total | 31 | 88 | 61,38 | 12,288 | 105 | 60 |
Patients who would not benefit from neither medical nor surgical intervention.
Discussion
In patients presenting to the emergency room with unstable angina pectoris, non-ST elevation MI, the MI risk, death, and emergency revascularization risk in 14 days must be calculated. Each of the following risk factors are evaluated and calculated 1 score: Age 65 and over, presence of 3 or more risk factors, coronary artery narrowing greater than 50%, history of use of acetyl salicylic acid in the last 7 days, chest pain in the last 24 hours, presence of ST change greater than 0.5 mm, and increase in cardiac markers. The point risk correlations are as follows: 0/1 points, as 4.7% risk, 2 points 8.3% risk, 3 points 13.2% risk, 4 points 19.9% risk, 5 points 26.2% risk, and 6/7 points 40.9% risk. Giglioli et al., retrospectively evaluated 517 patients [2] undergoing percutaneous coronary intervention (PCI), and found no statistically significant difference in mortality or cardiac ischemia with respect to presentation at the hospital and initial time of symptoms. In this study, the TIMI score was also evaluated, and a higher TIMI score was associated with increased mortality. In our study the power of the TIMI score in predicting the Gensini score was evaluated, and a correlation was identified (p<0.001, likelihood ratio=91.761). Patients with low TIMI scores were followed up medically. The increase in TIMI score was associated with an increased use of stents. Additionally, the number of patients who had vascular structures that could not be treated with interventional and medical methods increased. A mild relationship between TIMI and Gensini scores has also been identified (Spearman’s rho=0.552, p<0.05). Eren et al. reported the mortality rates of TIMI scores as follows: TIMI score of 3 is 25.9%, 4 is 29.6%, and 5 is 44.4% [3]. In a study conducted in France from 2002 to 2006, the utility of TIMI scores in ACS patients with CAD (n=239), the severity of the disease, and angiographic findings were analyzed. That study classified the patients as Group 1 (TIMI 0–2: n=121), Group 2 (TIMI 3–4: n=100), and Group 3 (TIMI 5–7: n=18). The rates of patients in these groups that have normal coronary artery findings were 36.3%, 13%, and 0%, respectively. While similar outcomes were achieved in Groups 1 and 2, there was a 28.9% difference between Groups 1 and 3 with respect to single-vessel lesions. In the presence of 2 vessel lesions, there were no difference between groups, but the rates in 3-vessel or left main vessel lesions were 13.2%, 26%, and 66.7%, respectively [4]. Lakhani et al., in their study conducted in 2008, evaluated 200 patients presenting to the ER [5], showing that early PCI is beneficial in patients with TIMI score>4 and more than 70% of vessel occlusion. In parallel to these studies, our study has also shown that the vascular lesions and Gensini scores increased in relation to the TIMI score.
The ACS registry system “Global Registry of Acute Coronary Events (GRACE)” has data from a wide range of patients. The GRACE risk scoring system, which was created from the data available, includes risk factors that help predict in-hospital and 6-month death rates. It is the main scoring system recommended in the 2007 European Society of Cardiology (ESC) diagnosis and treatment guidelines for non-ST elevated MI. The scoring system takes into consideration age, heart rate, systolic blood pressure, Killip class, presence of ST depression, cardiac markers, and occurrence of cardiac arrest. Although the GRACE model has good predictive power, the necessity to use specialized computer software, graphs, and scores renders its bedside use difficult. However, when direct comparisons are considered, GRACE emerges as the routine model that should be preferred in routine use [6]. The TIMI risk score was obtained from the TIMI II-B study population (100) and was confirmed in the TIMI II-B and ESSENCE (The Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-wave Coronary Events) patients. The TIMI risk score has been put into use to identify treatment efficacy in different risk groups. Although its power in predicting unexpected events is less, the ease of use has made TIMI widely accepted [7]. De Araújo Gonçalves et al. has shown that TIMI risk score has a moderate power in predicting the 1-year MI or death risk [6]. Van Der Zee et al. has shown that GRACE and TIMI scores can help distinguish long-term cardiovascular mortality [8]. Lee et al., in their study involving 4743 patients, compared the 30-day outcomes of the TIMI, GRACE, and PURSUIT scores and showed that TIMI scores are more powerful compared to the other scoring systems [9]. In all of the aforementioned studies, the TIMI and GRACE scoring systems have been compared and TIMI has emerged as being easier to interpret.
Patient’s demographic characteristics, chronic diseases like diabetes, clinical findings, EKG findings, and elevation in markers form the foundation of determining the risk level. The mortality due to coronary artery disease in the 45–74 age group in European countries is 2–9/1000 for males and 0.6–3/1000 for females [10,11]. The TEKHARF study (Heart Health and Risk Factors in Turkish Adults’) has shown the rate of mortality due to coronary artery disease is 8.5/1000 in males and 4.5/1000 in females. For men, after Lithuania and Estonia, Turkey ranks third in coronary disease mortality, and first in women [12]; 105 (63.6%) of the patients in the study were men. The mean age of the women included in our study was 64.95±12.03 years and was statistically significantly higher than men 59.34±12.00 (p=0.004, t=−2.882). This may be because women have a longer life expectancy in our country. On the other hand, the incidence and prevalence of coronary artery disease increases with age, so age might be considered as the most significant risk factor [13]. Although atherosclerotic lesions begin to appear early in childhood, the ratio of death due to coronary artery disease and its clinical significance appear only later in life, increasing with every decade. In our study there was a parallel increase in age and the ratio of stenotic vessels (p=0.025). In a study conducted Karounos et al., TIMI scores and sex were evaluated and although no statistically significant difference was identified, the lower TIMI scores were related with poorer outcomes in males [14].
Age over 45 in men and 55 in women is a strong risk factor for coronary artery disease [15]. When all other risk factors are set equal, men are more prone to atherosclerotic disease than are women. Until menopause, women are protected from advanced atherosclerosis, and other than in cases with diabetes and some rare (and most frequently familial) hyperlipidemia cases or uncontrolled hypertension, pre-menopausal myocardial infarction is rare in women. The coronary artery disease incidence rate in men is equal to that in women who are on average 10 years older [16]. The rate of coronary artery disease related death in the 35–55 years age group in women is one-fifth of that of men. This difference is equalized after menopause, and the rate of myocardial infarction begins to decrease after the seventh and eighth decades. Approximately 52% of women and 46% of men die because of atherosclerotic disease [17]. In our study, the TIMI and Gensini scores were similar in both groups (p>0.05). However, it must be noted that men were the majority of our patient group.
Hess et al. evaluated TIMI as a prognostic tool and showed that patients with TIMI score of 0 had a 1.8% rate of cardiac events within 30 days [18], and noted that this score is by itself insufficient for making the discharge decision. Similarly, Maureen et al. has studied ACS patients with delayed diagnoses and atypical symptoms [19]. Like these studies, our study has also shown that an increase in the TIMI score is associated with an increased risk factor, but TIMI scoring is insufficient for determining patient discharge. Although TIMI scores represent vascular lesions, in our study there were patients who had low TIMI scores but severe vascular lesions. Therefore, we support that TIMI score is not enough for discharging a patient.
Body et al., in their study using a modified TIMI score, have given ischemic EKG change and elevated troponin-T levels 5 points, and 1 point for other risk factors [20]. The modified scoring was shown to be more accurate in determining the 30-day outcomes. Vorlat et al., in their study evaluating 500 patients, showed that cardiac markers are the most important prognostic indicators. [9]. Correia et al., after adding C-reactive protein results (CRP) to the TIMI score, evaluated 86 patients and compared it to the original form [21]. The CRP-added scoring was shown to have a higher specificity (86% vs. 63%). In our study, every risk factor was equally scored. Different scores for each risk factor may prove useful, but this must be validated in larger trials.
Maureen et al. conducted a study utilizing TIMI scores and cocaine users [22], reporting that TIMI score failed to provide correct information regarding 30-day death, MI, and emergency revascularization in this sub-group of patients. Although cocaine has been shown to advance atherosclerotic lesions, because other risk factors are rarely seen in the cocaine-using patient population (which consists of young males with few comorbidities) TIMI scoring is not accurate. For this reason, TIMI scores must not be used to predict cardiac events in such patient populations.
In this study, our objective was to establish the relationship between risk factors and vascular lesions in patients presenting to the ER with chest pain. It was shown that with an increase in the number of risk factors in patients who present to the ER with chest pain, the number of vascular lesions increases. Pollack et al. studied the use of TIMI risk scoring system in non-ST-elevated MI patients and showed that in high risk patients, this score may help in planning antithrombotic, antiplatelet, and vascular interventional treatments [23]. In our study, as TIMI and Gensini scores were proportional, we believe that medical treatment must be initiated promptly.
Conclusions
Although the TIMI risk scoring system does not give as accurate results as the GRACE scoring system, its ease of use renders it a good scoring system for mortality and MI risk prediction. In emergency conditions, neither GRACE score nor Gensini score can be established accurately. Therefore, TIMI score can be used for risk prediction and follow-up.
Although TIMI 6–7 patients rarely present to the ER, in patients with TIMI 6 and 7 scores, mostly ST elevation is present, thus these scores have not been evaluated. One of the limitations of the study is the low number of patients. Long-term, prospective studies using larger patient populations are necessary to validate the use of these scoring systems in the context presented in this study.
Footnotes
Source of support: Departmental sources
References
- 1.Içli A, Gök H, Altunkeser BB, et al. Evaluation of “admission index of insulin resistance (AIRI)” as an early stage risk predictor in nondiabetic acute coronary syndromes. Anadolu Kardiyol Derg. 2002;2(3):194–201. [in Turkish] [PubMed] [Google Scholar]
- 2.Giglioli C, Cecchi E, Landi D, et al. Early invasive strategy and outcomes of non-ST-elevation acute coronary syndrome patients: is time really the major determinant? Intern Emerg Med. 2013;8(2):129–39. doi: 10.1007/s11739-011-0596-5. [DOI] [PubMed] [Google Scholar]
- 3.Eren NK, Ertas F, Yuksek U, et al. Additive prognostic value of NT-proBNP over TIMI risk score in intermediate-risk patients with acute coronary syndrome. Turk Kardiyol Dern Ars. 2009;37(1):1–8. [PubMed] [Google Scholar]
- 4.Ben Salem H, Ouali S, Hammas S, et al. Correlation of TIMI risk score with angiographic extent and severity of coronary artery disease in non-ST-elevation acute coronary syndromes. Ann Cardiol Angeiol (Paris) 2011;60(2):87–91. doi: 10.1016/j.ancard.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 5.Lakhani MS, Qadir F, Hanif B, et al. Correlation of thrombolysis in myocardial infarction (TIMI) risk score with extent of coronary artery disease in patients with acute coronary syndrome. J Pak Med Assoc. 2010;60(3):197–200. [PubMed] [Google Scholar]
- 6.de Araujo Goncalves P, Ferreira J, Aguiar C, Seabra-Gomes R. TIMI, PURSUIT, and GRACE risk scores: sustained prognostic value and interaction with revascularization in NSTE-ACS. Eur Heart J. 2005;26(9):865–72. doi: 10.1093/eurheartj/ehi187. [DOI] [PubMed] [Google Scholar]
- 7.Ramsay G, Podogrodzka M, McClure C, Fox KA. Risk prediction in patients presenting with suspected cardiac pain: the GRACE and TIMI risk scores versus clinical evaluation. QJM. 2007;100(1):11–18. doi: 10.1093/qjmed/hcl133. [DOI] [PubMed] [Google Scholar]
- 8.van der Zee PM, Verberne HJ, Cornel JH, et al. GRACE and TIMI risk scores but not stress imaging predict long-term cardiovascular follow-up in patients with chest pain after a rule-out protocol. Neth Heart J. 2011;19(7–8):324–30. doi: 10.1007/s12471-011-0154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee B, Chang AM, Matsuura AC, et al. Comparison of cardiac risk scores in ED patients with potential acute coronary syndrome. Crit Pathw Cardiol. 2011;10(2):64–68. doi: 10.1097/HPC.0b013e31821c79bd. [DOI] [PubMed] [Google Scholar]
- 10.Ceylan Y, Kaya Y, Tuncer M. Akut Koroner Sendrom Kliniği ile Başvuran Hastalarda Koroner Arter Hastalığı Risk Faktörleri. Van Tıp Dergisi. 2011;18(3):147–54. [in Turkish] [Google Scholar]
- 11.Bissinger A, Grycewicz T, Grabowicz W, Lubiński A. Endothelial function and left ventricular remodeling in diabetic and non-diabetic patients after acute coronary syndrome. Med Sci Monit. 2011;17(2):CR73–77. doi: 10.12659/MSM.881390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.TEKHARF; Oniki Yıllık İzleme Deneyimine Göre Türk Erişkinlerinde Kalp Sağlığı. Prof. Dr. Altan Onat, Prof. Dr. Vedat Sansoy, Prof. Dr. İnan Soydan, Prof. Dr. Lale Tokgözoğlu, Prof. Dr. Kamil Adalet. Argos İletişim Hizmetleri Reklamcılık ve Ticaret Anonim Şirketi. Temmuz 2003, İstanbul [in Turkish]
- 13.Fuster V, Alexander RW, O’Rourke R. Baskısının Türkçe çevirisi. 1th ed. Danışmanlık Eğitim Yayıncılık ve Organizasyon Ltd. Şti; 2002. Hurst’s The Heart. 10. [Turkish Translation of Hurst’s The Heart] [Google Scholar]
- 14.Karounos M, Chang AM, Robey JL, et al. TIMI risk score: does it work equally well in both males and females? Emerg Med J. 2007;24(7):471–74. doi: 10.1136/emj.2007.048207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Süleymanlar İ, İliçin G, Biberoğlu K, Ünal S. İç Hastalıkları. 2. ed. Güneş Kitabevi/Publications; 2003. [in Turkish] [Google Scholar]
- 16.Castelli WP. Epidemiology of coronary heart disease: the Framingham study. Am J Med. 1984;76(2A):4–12. doi: 10.1016/0002-9343(84)90952-5. [DOI] [PubMed] [Google Scholar]
- 17.Thom TJ. Cardiovascular disease mortality among United States woman. In: Eaker ED, editor. Coronary Heart Disease in Women. Hay market Doyma; New York: 1987. [Google Scholar]
- 18.Hess EP, Agarwal D, Chandra S, et al. Diagnostic accuracy of the TIMI risk score in patients with chest pain in the emergency department: a meta-analysis. CMAJ. 2010;182(10):1039–44. doi: 10.1503/cmaj.092119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chase M, Robey JL, Zogby KE, et al. Prospective validation of the Thrombolysis in Myocardial Infarction Risk Score in the emergency department chest pain population. Ann Emerg Med. 2006;48(3):252–59. doi: 10.1016/j.annemergmed.2006.01.032. [DOI] [PubMed] [Google Scholar]
- 20.Body R, Carley S, McDowell G, et al. Can a modified thrombolysis in myocardial infarction risk score outperform the original for risk stratifying emergency department patients with chest pain? Emerg Med J. 2009;26(2):95–99. doi: 10.1136/emj.2008.058495. [DOI] [PubMed] [Google Scholar]
- 21.Correia LC, Lima JC, Rocha MS, et al. Does high-sensitivity C-reactive protein add prognostic value to the TIMI-Risk Score in individuals with non-ST elevation acute coronary syndromes? Clin Chim Acta. 2007;375(1–2):124–28. doi: 10.1016/j.cca.2006.06.026. [DOI] [PubMed] [Google Scholar]
- 22.Chase M, Brown AM, Robey JL, et al. Application of the TIMI risk score in ED patients with cocaine-associated chest pain. Am J Emerg Med. 2007;25(9):1015–18. doi: 10.1016/j.ajem.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 23.Pollack CV, Jr, Sites FD, Shofer FS, et al. Application of the TIMI risk score for unstable angina and non-ST elevation acute coronary syndrome to an unselected emergency department chest pain population. Acad Emerg Med. 2006;13(1):13–18. doi: 10.1197/j.aem.2005.06.031. [DOI] [PubMed] [Google Scholar]