Summary
Background
The possibility of recanalization and the need for retreatment are the most important drawbacks of intracranial aneurysm embolization. The purpose of the study was to prospectively analyze the results of early follow-up angiography of embolized ruptured aneurysms in an attempt to determine factors predicting the presence of residual flow.
Material/Methods
Evaluation included 72 patients with 72 aneurysms, which were followed-up 3 months after the treatment. Analysis of residual flow predictors included: age and gender, clinical state in Hunt-Hess scale, aneurysm localization, aneurysm three dimensions and volume, neck width, sac-to-neck ratio, initial result of embolization, number of coils used and the use of hydrogel coils and stents.
Results
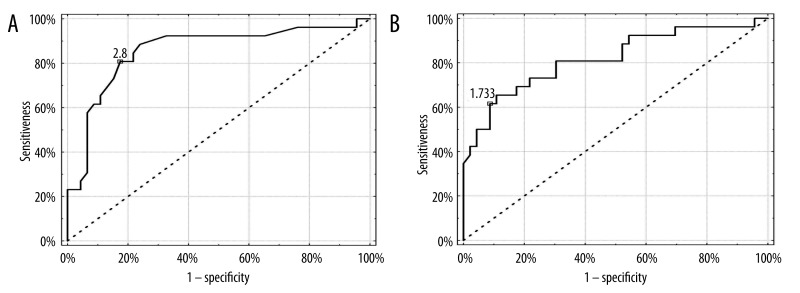
Mean sac diameter was 6.5±3.9 mm, and mean neck width was 2.9±1.4 mm. Follow-up angiography presented residual flow in 26 aneurysms (36.1%): class 2 in 8 aneurysms (11.1%), and class 3 in 18 cases (25.0%). Stable aneurysm filling was observed in 45 cases (62.5%), progression of residual flow in 25 cases (34.7%), and regression in 2 cases (2.8%). According to ROC analysis independent predictors of residual flow were aneurysm neck diameter (AUC 0.857, 95% CI: 0.755–0.928, p<0.0001) and sac-to-neck ratio (AUC 0.817, 95% CI: 0.708–0.898, p<0.0001). Cut-off point of the ROC curve was established at 2.8 mm for neck diameter, and 1.73 for sac-to-neck ratio.
Conclusions
Aneurysm neck diameter and sac-to-neck ratio are independently related to the residual flow in embolized ruptured aneurysms at early follow-up.
MeSH Keywords: Follow-up Imaging, Embolization, Therapeutic, Intracranial Aneurysm
Background
Intracranial aneurysms are local, abnormal arterial dilations visible upon illumination with light and containing all the components of the vessel wall. Incidence of aneurysms in the general population, based on autopsy and angiographic studies, is estimated to be 1.7–3.1% [1]. The most serious symptom and complication of an aneurysm is its rupture with subsequent subarachnoid hemorrhage (SAH), which is fatal in 32–67% of patients or results in permanent disability in 10–20% of cases [2–4].
Treatment of intracranial aneurysms aims to prevent complications by eliminating it from blood circulation. Nowadays, the treatment of choice of intracranial aneurysms at many medical centers is an endovascular embolization [5,6]. Major advantage of embolization, in comparison to surgical procedures, is its less invasive nature. Endovascular treatment does not require opening of the cranial cavity, causes less vasospasm, procedure is usually shorter and does not require a blood product [7].
The main drawbacks of embolization, include: significant incidence of recanalization and the need for re-treatment [8–11]. Aneurysm recurrence is caused by recanalization of a thrombus formed in response to reduced blood flow within the coil basket compression due to pulsating blood flow in the parent vessel wall or at the site of aneurysm not inflated with coils. The risk of recurrence or, more broadly, residual flow is estimated at 21–34% in a control study [8,9]. As a result, the possibility of a rupture of a treated aneurysm and subarachnoid hemorrhage is estimated to be at 0.11% person-years [10].
The purpose of this study was to prospectively evaluate the results of early control after embolization of ruptured intracranial aneurysms in terms of finding the predictors of residual flow.
Material and Methods
Embolization procedure
Treatment was preceded by digital subtraction angiography (DSA), performed under local or general anesthesia, depending on the patient’s condition. Embolizations were performed with platinum coils or platinum and hydrogel coils or platinum coils with stent remodeling. Embolization procedures used the following: platinum GDC Detachable Coils (Boston Scientific, Natick, USA), Axium and Nexus (ev3 Corporate, Plymouth, USA) and MicroPlex (MicroVention, Inc., Tustin, USA), hydrogel coils HydroCoil and HydroSoft (MicroVention, Inc., Tustin, USA), and intracranial stents Neuroform3 (Boston Scientific, Natick, USA). During the procedure, heparin was administered at an intra-arterial dose of 30–60 mg, and in case of significant vasospasm, papaverine at a dose of 20–40 mg intra-arterially. Control 3D DSA was performed about 3 months after the embolization to evaluate the early results of treatment. The results of embolization were evaluated according to Roy et al. classification [11].
Statistical analysis
Statistical analysis was performed using MedCalc software 11.6.0 (MedCalc Software, Mariakerke, Belgium), Statistica 9 (StatSoft Inc., Tulsa, USA) and Microsoft Excel 2007 (Microsoft Corp., Redmond, USA). Distribution compatibility of measurable variables with normal distribution was tested using W Shapiro-Wilk test. The results were considered statistically significant at a confidence level of p<0.05.
Besides descriptive statistics, an attempt to identify potential factors associated with the presence of residual flow within the aneurysm in a control study, was made. The following parameters were taken into account: age and gender, clinical condition according to the Hunt-Hess scale on admission, aneurysm location, dimensions in 3 axes, aneurysm volume, neck width, sac-to-neck width ratio, initial result of embolization (Class 1–3), number of coils used and the use of hydrogel coil stents. The analysis was performed by comparing aneurysm groups with flow against a group with no flow during control test, through the U Mann-Whitney test and Fisher’s exact test. Additionally, for each variable the area under the ROC curve was calculated with a 95% confidence interval (95% CI). Statistical significance of AUC was analyzed using the Z-test.
Results
Technical results of therapy
The analysis included 72 patients with 72 embolized aneurysms, who reported for a follow-up DSA 3 months after embolization. The summary of patient demographic data is shown in Table 1 The largest mean diameter of the sac was 6.5 (±3.9) mm and mean neck width 2.9 (±1.4) mm. Average aneurysm volume was 1.92 (±5.54) ml.
Table 1.
Demographic data of study participants (n=72).
| Parameter | Value | |
|---|---|---|
| Age (mean ± SD) | 51.5 ±12.4 lat | |
| Gender | Male | 24 (33.3%) |
| Female | 48 (66.6%) | |
| Status at admission according to Hunt-Hess scale | I | 9 (12.5%) |
| II | 24 (33.3%) | |
| III | 26 (36.1%) | |
| IV | 7 (9.7%) | |
| V | 6 (8.3%) | |
| Aneurysm location | ICA | 40 (55.6%) |
| ACoA, ACA | 17 (23.6%) | |
| MCA | 10 (13.9%) | |
| BA/VA | 5 (6.9%) | |
| Aneurysm size | Small (≤5 mm) | 26 (36.1%) |
| Medium (5.1–15 mm) | 42 (58.3%) | |
| Large (15.1–25 mm) | 5 (6.9%) | |
| Giant (>25 mm) | 0 (0.0%) | |
| Sac-to-neck width ratio | ≤1.5 | 15 (20.8%) |
| 1.6–2.5 | 36 (48.6%) | |
| >2.5 | 21 (29.2%) | |
The course and immediate treatment outcomes are summarized in Table 2. On average, 6.0 (±3.5) coils were used during embolization, per aneurysm. Platinum coils (66.6%) were mainly used and almost all cases (97.2%) used at least one 3D coil (spherical). Hydrogel coils were introduced at our medical center at the beginning of the study. However, their use in urgent cases grew gradually with operator experience. Eight aneurysms (11.1%) were supplied with coils following stent implantation, and in every case an attempt was made to place the first coil without the stent. The procedure was terminated in the absence of contrast medium flow into the aneurysm on a 3D DSA or when the introduction of a coil resulted in reduced flow in adjacent vessels or caused the loop to penetrate the proper vessel. In 2 cases of aneurysm, a coexisting arteriovenous malformation (AVM) was observed, one of which was treated with additional embolization using histoacryl.
Table 2.
Course and results of embolizations (n=72).
| Parameter | Number of procedures (%) | |
|---|---|---|
| Features of vasospasm in DSA view, before procedure | 14 (19.4%) | |
| Number of coils used | <3 | 15 (20.8%) |
| 4–6 | 25 (34.7%) | |
| >6 | 32 (44.4%) | |
| Type of spiral used | Platinum | 48 (66.6%) |
| Mixed* | 24 (33.3%) | |
| Embolization with remodeling | 8 (11.1%) | |
| Embolization result** | Class 1 | 64 (89.9%) |
| Class 2 | 8 (11.1%) | |
| Class 3 | 0 (0.0%) | |
| Technical complications | 5 (6.9%) | |
| Features of vasospasm in DSA view, after procedure | 9 (12.5%) | |
Platinum and hydrogel coils;
embolization result classification according to Roy et al. [11].
In most cases, immediately after the procedure absence of flow within the aneurysm was observed (Class 1) – Table 1. Cases of suboptimal filling resulted from a weakened flow in the vessel or its branch (n=2, 2.8%) or coil loop displacement into the proper vessel (n=6, 8.3%). Signs of vasospasm were observed during the procedure in 34 patients (47.2%). In most cases, shrinkage was moderate and resolved after the administration of 40–120 mg of papaverine through a guide catheter. Technical complications that occurred during the procedure, include aneurysm perforation (n=3, 4.2%) and permanent displacement of the coil to the lumen of the parent vessel (n=2, 2.8%) Figure 1. None of these events have caused any clinical complications, including neurological deficits.
Figure 1.
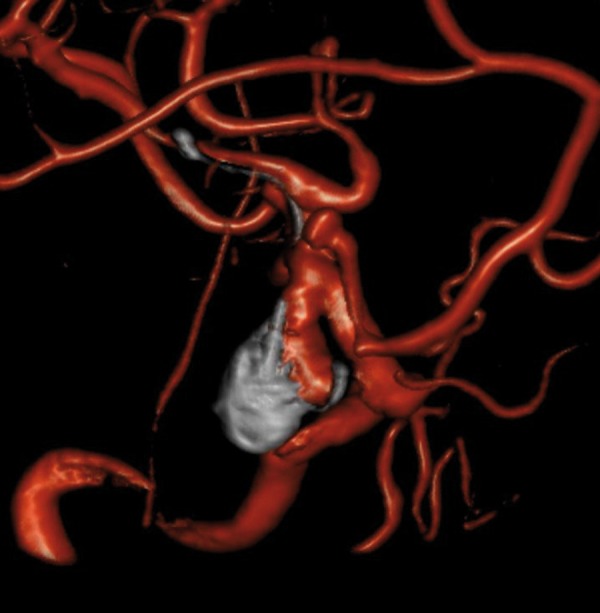
Follow-up 3D DSA after embolization of the LICA aneurysm. There is a residual flow type 3 and a coil loop released from the aneurysm, which lays in LMCA and ends in one of its branches. There are also two small aneurysms: at the orifice of LACA and in the trifurcation of LMCA.
Early results of treatment
The average time between the procedure and the follow-up was 92.8 (±24.7) days. Follow-up angiography revealed residual flow in 26 (36.1%) aneurysms. In 8 cases (11.1%) the flow was class 2 and in 18 cases (25.0%) class 3. Among the patients, stable aneurysm was observed in 45 cases (62.5%), progression of residual flow was seen in 25 cases (34.7%) and regression in 2 cases (2.8%). There was no evidence of arterial obstruction, nor thrombosis on stent surfaces. There were no adverse effects associated with arterial angiography.
Predicting factors of residual flow in an aneurysm
Among the analyzed demographic and morphological parameters, only neck width varied significantly between the group of aneurysms with residual flow in the follow-up examination and the group of completely embolized aneurysms (mean value 4.0±1.6 mm and 2.3±0.8 mm, p<0.0001). However, according to the ROC analysis, significant predictors of residual flow occurrence were: the width of aneurysm neck (AUC 0.857, 95% CI: 0.755–0.928, p<0.0001) and sac-to-neck width ratio (AUC 0.817, 95% CI: 0.708–0.898 p<0.0001) (Figure 2). The cut-off point for neck width was estimated at 2.8 mm, which means that above this value, there may be residual flow in the aneurysm with a sensitivity of 80.8% and a specificity of 82.6%. However, the cut-off point for sac-to-neck width ratio was estimated to be 1.73, which means that below this value the existence of residual flow may be predicted with a sensitivity of 91.3% and a specificity of 61.5%.
Figure 2.
ROC graphs present a relationship between the presence of residual flow in the aneurysm and aneurysm neck width (A) and the sack-to-neck-ratio (B). Cut-off points of ROC curves are marked.
Discussion
Many authors believe that some of the biggest drawbacks of endovascular treatment of intracranial aneurysms include the risk of recanalization of the lesion and subsequent SAH [4,8,12–15].
The most complete study of the incidence of recanalization was presented by Ferns et al. [8]. Their meta-analysis covered 46 studies involving 8,161 patients who were followed for an average of 14.1 months. Initially, complete filling of the aneurysm was achieved in 91.2% of patients. Recanalization was observed in 20.8% of cases, while re-treatment was performed in 10.3% of patients. Particularly interesting was an observation of a lower incidence of relapse in cases with a history of aneurysm rupture (11.4%) and higher incidence in cases involving only change in the posterior circulation (22.5%). Regression analysis revealed a weak correlation between the size of aneurysms greater than 10 mm and an increased incidence of recanalization and reembolization. The list of potential risk factors for the recurrence of an aneurysm as presented by other authors, includes: insufficient filling density of the lesion [16], an incomplete initial embolization (with residual flow) [17], presence of a thrombus in the sac or clotting during the procedure [18], large dimensions of aneurysm [8,19], a wide neck [20] and location in the posterior circulation [8]. The answer to the question of which aneurysms are characterized by frequent recanalization, ruptured or unruptured, remains unanswered [8,21].
This large number of risk factors reflects the limited knowledge about the true causes and mechanisms of aneurysm recanalization and recurrence following endovascular treatment. Consequently, it is difficult to develop an optimal post-embolization follow-up protocol, one that would help prevent subarachnoid bleeding from reoccurring and avoid unnecessary diagnostic procedures. It appears that some of the discussed risk factors for recanalization may result from the lack of multivariate statistical analysis of raw data or its improper execution, and therefore, are not true predictors of aneurysm relapse. For instance, aneurysms located within the anterior circulation can be treated endovascularly or, in case of unfavorable morphology, surgically. In contrast, lesions in the posterior circulation are much more difficult to clip, therefore embolizations are performed even in cases of aneurysms with very difficult configuration leading to more frequent relapses.
Presence of a thrombus within the sac of an aneurysm or clotting during embolization involves the risk of spontaneous fibrinolysis after the procedure and loosening of the densely packed coils. It is equally difficult to obtain a stable and dense packing of embolization material in giant aneurysms, where higher rigidity of long coils tends to form unfilled compartments later predisposing to recanalization. Furthermore, due to the risk of causing a mass effect by an embolized giant aneurysm, the procedure is usually stopped once flow within the sac stops, rather than continuing until no more coils can be introduced. These factors contribute to a weaker filling of giant aneurysm sacs, as compared to the treatment of smaller lesions. Similar situation occurs in cases of aneurysms with a wide neck, where the tendency for weaker filling stems from the possibility of coil loop protrusion into the lumen of the parent vessel. Predictors of flow in the study were the following: neck width of aneurysm sac and sac-to-neck width ratio. ROC analysis allowed for the calculation of cutoff points. Presence of flow during follow-up examination was more likely in case of aneurysms with neck width >2.8 mm and sac-to-neck width ratio <1.73. These results confirm data already published by larger clinical trials, although specific cut-off points depend on the population analyzed [20–22].
Particularly interesting is the fact that the data revealed no relationship between the presence of flow during follow-up examination and the initial outcome of embolization. This may suggest the presence of dynamic processes of coagulation and recanalization within the treated aneurysms or according to the hypothesis by Ries et al., the existence of a subclass of aneurysms with increased mechanical compliance and likelihood of recanalization [23]. On the other hand, recent studies pointed to the subjective nature of the assessment of filling of an aneurysm. In the PRESAT study, baseline results and the results at 1-year follow-up were worse in the assessment of independent observers, than the doctors who performed the procedures [24]. Additionally, multivariate regression analysis of embolization results performed during the PRESAT study revealed that the initial assessment by objective observers was the only predictor of residual flow at 1-year follow-up, with high OR – 2.8 (95% CI 1.2–7.0). Similarly, Daugherty et al. during their study on the variability of treatment qualifications of recanalized aneurysms, demonstrated significant differences between the assessment of the same patients by different neuroradiologists. The differences pertained the qualifications for re-embolization (κ compliance rate only 0.27) and a method of treatment. Depending on the researcher, qualifications for clipping ranged from 7% to 67% [25]. These results demonstrate the need for an objective evaluation of aneurysms immediately after the embolization, but also during follow-up examinations.
Conclusions
Neck width of an aneurysm and sac-to-neck width ratio are associated with residual flow in cases of ruptured intracranial aneurysms treated with embolization.
References
- 1.Rinkel GJ, Djibuti M, Algra A, et al. Prevalence and risk of rupture of intracranial aneurysms: a systematic review. Stroke. 1998;29(1):251–56. doi: 10.1161/01.str.29.1.251. [DOI] [PubMed] [Google Scholar]
- 2.Ellegala DB, Day AL. Ruptured cerebral aneurysms. N Engl J Med. 2005;352(2):121–24. doi: 10.1056/NEJMp048301. [DOI] [PubMed] [Google Scholar]
- 3.Hop JW, Rinkel GJ, Algra A, et al. Case-fatality rates and functional outcome after subarachnoid hemorrhage: a systematic review. Stroke. 1997;28(3):660–64. doi: 10.1161/01.str.28.3.660. [DOI] [PubMed] [Google Scholar]
- 4.Olafsson E, Hauser WA, Gudmundsson G. A population-based study of prognosis of ruptured cerebral aneurysm: mortality and recurrence of subarachnoid hemorrhage. Neurology. 1997;48(5):1191–95. doi: 10.1212/wnl.48.5.1191. [DOI] [PubMed] [Google Scholar]
- 5.Qureshi AI, Vazquez G, Tariq N, et al. Impact of International Subarachnoid Aneurysm Trial results on treatment of ruptured intracranial aneurysms in the United States. J Neurosurg. 2010;114(3):834–41. doi: 10.3171/2010.6.JNS091486. [DOI] [PubMed] [Google Scholar]
- 6.Gnanalingham KK, Apostolopoulos V, Barazi S, et al. The impact of the international subarachnoid aneurysm trial (ISAT) on the management of aneurysmal subarachnoid haemorrhage in a neurosurgical unit in the UK. Clin Neurol Neurosurg. 2006;108(2):117–23. doi: 10.1016/j.clineuro.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Dumont AS, Crowley RW, Monteith SJ, et al. Endovascular treatment or neurosurgical clipping of ruptured intracranial aneurysms: effect on angiographic vasospasm, delayed ischemic neurological deficit, cerebral infarction, and clinical outcome. Stroke. 2010;41(11):2519–24. doi: 10.1161/STROKEAHA.110.579383. [DOI] [PubMed] [Google Scholar]
- 8.Ferns SP, Sprengers ME, van Rooij WJ, et al. Coiling of intracranial aneurysms: a systematic review on initial occlusion and reopening and retreatment rates. Stroke. 2009;40(8):e523–29. doi: 10.1161/STROKEAHA.109.553099. [DOI] [PubMed] [Google Scholar]
- 9.Raymond J, Guilbert F, Weill A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003;34(6):1398–403. doi: 10.1161/01.STR.0000073841.88563.E9. [DOI] [PubMed] [Google Scholar]
- 10.Molyneux AJ, Kerr RS, Birks J, et al. Risk of recurrent subarachnoid haemorrhage, death, or dependence and standardised mortality ratios after clipping or coiling of an intracranial aneurysm in the International Subarachnoid Aneurysm Trial (ISAT): long-term follow-up. Lancet Neurol. 2009;8(5):427–33. doi: 10.1016/S1474-4422(09)70080-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roy D, Milot G, Raymond J. Endovascular treatment of unruptured aneurysms. Stroke. 2001;32(9):1998–2004. doi: 10.1161/hs0901.095600. [DOI] [PubMed] [Google Scholar]
- 12.Molyneux A, Kerr R, Stratton I, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. Lancet. 2002;360(9342):1267–74. doi: 10.1016/s0140-6736(02)11314-6. [DOI] [PubMed] [Google Scholar]
- 13.Schaafsma JD, Sprengers ME, van Rooij WJ, et al. Long-term recurrent subarachnoid hemorrhage after adequate coiling versus clipping of ruptured intracranial aneurysms. Stroke. 2009;40(5):1758–63. doi: 10.1161/STROKEAHA.108.524751. [DOI] [PubMed] [Google Scholar]
- 14.Kwee TC, Kwee RM. MR angiography in the follow-up of intracranial aneurysms treated with Guglielmi detachable coils: systematic review and meta-analysis. Neuroradiology. 2007;49(9):703–13. doi: 10.1007/s00234-007-0266-5. [DOI] [PubMed] [Google Scholar]
- 15.Serafin Z, Strześniewski P, Osmański M, et al. Technical aspects and short-term results of primary coiling of giant intracranial aneurysms: a 12-year, single-center experience. Med Sci Monit. 2010;16(Suppl 1):33–39. [Google Scholar]
- 16.Sluzewski M, van Rooij WJ, Slob MJ, et al. Relation between aneurysm volume, packing, and compaction in 145 cerebral aneurysms treated with coils. Radiology. 2004;231(3):653–58. doi: 10.1148/radiol.2313030460. [DOI] [PubMed] [Google Scholar]
- 17.Grunwald IQ, Papanagiotou P, Struffert T, et al. Recanalization after endovascular treatment of intracerebral aneurysms. Neuroradiology. 2007;49(1):41–47. doi: 10.1007/s00234-006-0153-5. [DOI] [PubMed] [Google Scholar]
- 18.Iihara K, Murao K, Yamada N, et al. Growth potential and response to multimodality treatment of partially thrombosed large or giant aneurysms in the posterior circulation. Neurosurgery. 2008;63(5):832–42. doi: 10.1227/01.NEU.0000313625.15571.1B. [DOI] [PubMed] [Google Scholar]
- 19.Ferns SP, Sprengers ME, van Rooij WJ LOTUS Study Group. Late reopening of adequately coiled intracranial aneurysms: frequency and risk factors in 400 patients with 440 aneurysms. Stroke. 2011;42(5):1331–37. doi: 10.1161/STROKEAHA.110.605790. [DOI] [PubMed] [Google Scholar]
- 20.Ries T, Siemonsen S, Thomalla G, et al. Long-term follow-up of cerebral aneurysms after endovascular therapy prediction and outcome of retreatment. Am J Neuroradiol. 2007;28(9):1755–61. doi: 10.3174/ajnr.A0649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tan IY, Agid RF, Willinsky RA. Recanalization rates after endovascular coil embolization in a cohort of matched ruptured and unruptured cerebral aneurysms. Interv Neuroradiol. 2011;17(1):27–35. doi: 10.1177/159101991101700106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fiehler J, Byrne JV. Factors affecting outcome after endovascular treatment of intracranial aneurysms. Curr Opin Neurol. 2009;22(1):103–8. doi: 10.1097/WCO.0b013e32831af1c1. [DOI] [PubMed] [Google Scholar]
- 23.Ries T, Wulff A, Wegscheider K, et al. Unexpected kink in aneurysm recurrence volume distribution is associated with retreatment decision. Neuroradiology. 2010;52(7):657–58. doi: 10.1007/s00234-010-0693-6. [DOI] [PubMed] [Google Scholar]
- 24.Taki W, Sakai N, Suzuki H. Prospective Registry of Subarachnoid Aneurysms Treatment (PRESAT) group: Importance of independent evaluation of initial anatomic results after endovascular coiling for ruptured cerebral aneurysms. J Clin Neurosci. 2013;20(4):527–31. doi: 10.1016/j.jocn.2012.01.058. [DOI] [PubMed] [Google Scholar]
- 25.Daugherty WP, Rad AE, White JB, et al. Observer agreement regarding the necessity of retreatment of previously coiled recurrent cerebral aneurysms. Am J Neuroradiol. 2011;32(3):566–69. doi: 10.3174/ajnr.A2336. [DOI] [PMC free article] [PubMed] [Google Scholar]