Abstract
Background
The number of female veterans is increasing. Veterans Administration (VA) enrollment increased over 40% from past eras. However, little research has focused on their mental health. We reviewed literature to examine associations of substance use with suicide in female veterans, identify research gaps, and inform future studies.
Methods
Google Scholar, Pub Med, and PsychINFO were searched using: substance use, female veteran, and suicide. Exclusion criteria (e.g., not discussing U.S. veterans) left 17 articles.
Results
Nine studies examined completed suicide among veterans. In most recent years, rates of deaths were greater for veterans than nonveterans, including females. Completed suicide was associated with past trauma, young age, and a mental disorder. Studies have often not addressed substance use. Three studies examined completed suicide among VA treated veterans without examining substance use as an associated factor. Rates of completed suicides were also higher among veterans than nonveterans, including females. A large proportion of females also had a mental diagnosis. Five studies examined substance use and attempted or completed suicide among VA treated veterans. Veterans in poor mental health had increased odds of suicide mortality; women with a substance use disorder (SUD) had a higher hazard ratio for completed suicide than men with a SUD. Engagement in substance abuse treatment decreased odds of suicide attempt among veterans.
Conclusion
Available data suggest that suicide rates are higher among female veterans than women in the general population. Substance use may increase the likelihood of suicidal behaviors among female veterans, particularly those with a mental diagnosis.
Keywords: Female Veteran, Suicide, Substance Abuse, Substance Use
1. INTRODUCTION
Women with military service are a growing population. They currently make up 11.3% of military personnel and 8% of veterans in the United States (U.S.; Batuman et al., 2011). Modern warfare increases women's exposure to trauma (Murdoch et al., 2006), and the mental health needs of female veterans are increasing (Goldberg et al., 2008). However, veteran's mental health research has traditionally focused on men, creating disparity in knowledge about women (Goldzweig et al., 2006). The psychiatric status of women who served in Operation Iraqi Freedom (OIF), Operation New Dawn (OND), and Operation Enduring Freedom (OEF) (N=299,548 as of February 28, 2013) requires research to inform female veteran's mental health needs (Nunnink et al., 2010). Given the reported increase of suicide and substance use among veterans (Nunnink et al., 2010; Kang and Bullman, 2009) and identified associations between substance use and completed suicide (Allen et al., 2005), there is a compelling need to investigate suicide and substance use in the understudied female veteran population. To aid efforts, we conducted a literature review to:
Examine the extent of suicide measures (ideation, suicidal behavior, completed suicide) among veterans, with a particular focus on female veterans,
Examine the potential for an association between substance use and suicide measures in female veterans,
Discuss reasons female veterans may be particularly likely to misuse substances and endorse suicide measures, and
Identify research gaps for future research.
To provide context for this review, we begin with a background on substance use among female military personnel, the role substance use might play in increasing suicide, and the challenges in studying substance abuse and suicide among female veterans. We then review available findings on male and female veteran suicide, including suicide among those who use Veterans Administration (VA) services, with an emphasis on females and gender differences. We also review studies on associations between suicide and substance use, including substance use disorder (SUD), among veterans. Finally, we discuss factors that increase female veteran's vulnerability to suicide and substance use.
1.1 Female Military Service and Substance Use
Problematic substance use is prevalent in the military. In 2008, prevalence of binge drinking (≥ 5 drinks in men; ≥ 4 drinks in women on ≥ 1 day in the past 30 days) ranged from 39% in the Air Force to 57.6% in the Marine Corp (Bray et al., 2009). Although problematic drinkers were more often male (Bray et al., 2009), Jacobson et al. (2008) assessed alcohol use among 48,481 active duty personnel (30% female) and found that women were 1.21 times more likely than men to begin heavy weekly drinking between baseline (July, 2001-June, 2003) and follow-up (June, 2004-February, 2006). In addition, 32% of women reported binge drinking, 8% heavy weekly drinking, and 7% alcohol related problems (Jacobson et al., 2008). Further, a 2005 survey of 1,200 Army soldiers found that women engaged in unsafe drinking at a rate nearly twice that of men (9.1% vs. 5.1%; Lande et al., 2007).
Bray and Hourani (2007) analyzed 1980-2005 survey data collected from >150,000 active duty service members and found that, while illicit drug use declined in the general military population from 1980-1998 before leveling off, past-month prevalence of illicit drug use among female soldiers increased from 1998-2002 (from 1.9%-2.9%). Bray et al. (2009) further found that nonmedical prescription drug use increased through 2008 and that past-month prevalence of any illicit or nonmedical drug use was higher among females than males (13.3% vs. 11.7%, respectively).
Data from the 2004-2006 National Survey on Drug Use and Health (NSDUH) found that 5.8% of female veterans had a SUD (SAMHSA, 2007). While lower than the 9.2% in the general population (individuals aged 12+ years) with a SUD in 2006 (SAMHSA, 2007a), the proportion of female veterans who engage in problem substance use is likely higher than estimated. Although more recent data were not available, a 1998 survey found that, among 1,259 female Veterans Health Affairs (VHA) patients, 24% of respondents engaged in binge drinking. Of respondents who drank, 11% binge drank ≥1 time a month (Bradley et al., 2001). Similarly, 31.1% of female veterans treated by the VHA and surveyed in 1998 reported hazardous or problem drinking, and 4.9% reported past-year drug use (Davis et al., 2003).
1.2 Suicide and Substance Use
Depending on the study measures, suicide variables may include ideation (suicidal thoughts and contemplation), behavior (attempted suicide), or completed suicide (Kaplan et al., 2007). Studies show an association between substance use (e.g., alcohol, opiates, inhalants) and increased odds of suicidal behaviors in the samples of general populations (Borges et al., 2000; Cherpitel et al., 2004; Wilcox et al., 2004). In 2009, almost one third of US Army suicide deaths involved prescription drug abuse; from 2003-2009, 45% of unsuccessful suicidal attempts were reported to involve alcohol or drug use (US Army, 2010).
Joiner (2005) proposed that, to commit suicide, people must perceive themselves a burden to others, feel they don't belong, and be physically capable of self-harm. Substance use may improve the likelihood of these factors. Substances may alter neurological pathways to increase impulsivity, triggering suicidal behavior (Braquehais et al., 2010). Veterans suffering from posttraumatic stress disorder (PTSD) may also use substances to relieve PTSD symptoms (Leeies et al., 2010; Jakupcak et al., 2009), and the situations that contribute to PTSD may decrease veteran's fear of harm, habituate them to pain and violence, and allow them to acquire the ability to self-harm (Joiner, 2005). Inability to reintegrate into civilian life may lead to social alienation and a failed sense of belonging (Brenner et al., 2008). Finally, substances, such as opiates, work as a mechanism of death through overdose (Best et al., 2000). If substance use triggered or increased odds of suicide ideation, attempted suicide, or completed suicide, interventions on substance use might improve mental health, reduce suicide ideation, and help prevent or reduce suicide attempt and completion.
1.3 Methodological Challenges
Several methodological challenges are present when studying female veterans, the first being small numbers of service women that make it difficult to accrue sufficient samples for generating meaningful results. Because of the demographic makeup of the military, unweighted rates calculated using military populations (e.g., active duty, veterans) for the denominator tend to disproportionately represent males and mask their associations with women's health indicators (Kaplan et al., 2007). Additionally, veteran suicide research has traditionally used samples identified through the Department of Veterans Affairs system (VA); however, only one quarter of veterans have historically received care through these facilities (Kaplan et al., 2007). Studies that consider illicit drug use also often include only small subsamples of women, limiting the analysis of associations between drug use and suicide variables (Wilcox et al., 2004). Because events of suicide attempt or death are often rare in a given study, analyses of suicidal events are constrained by a relatively small number of cases (Allen et al., 2005). Men are more likely than women to complete suicide and women tend to attempt it (Cibis et al., 2012). Thus, studies that use completed suicide as an outcome measure miss some women at risk for suicide related injury. Because female veterans and people who commit or attempt suicide are difficult to study, the influence of one behavior over another (e.g., substance abuse increasing potential suicide) may go undetected if not targeted for research. The aim of this review is to identify whether a relationship exists between suicide and substance abuse in this population to inform future research and prevention efforts.
2. METHODS
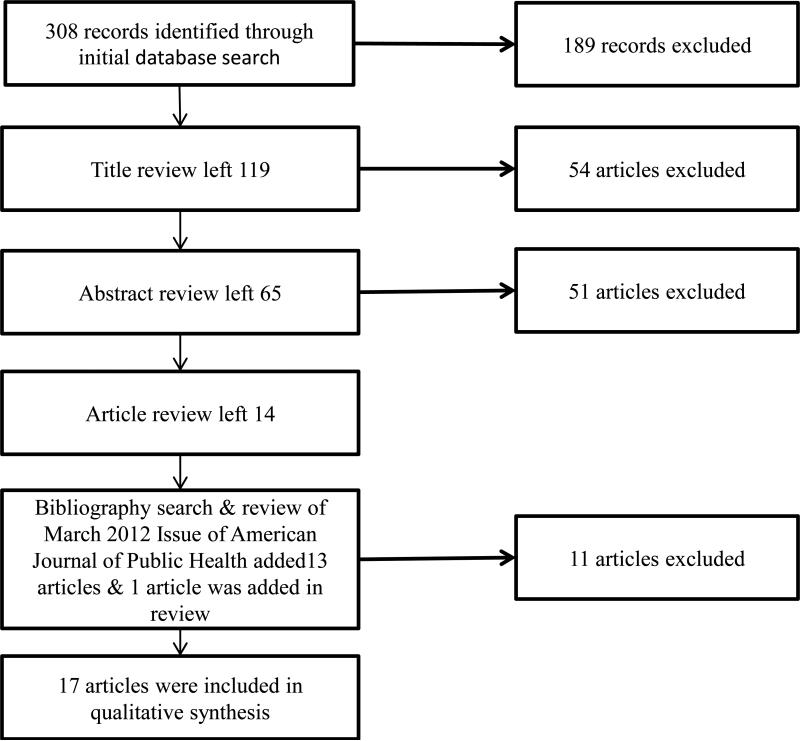
We searched Google Scholar, Pub Med, and PsychINFO using keywords and terms substance use, female veteran, and suicide, instructing search engines to include “and” between each term (Figure 1). Searches resulted in 308 hits. Exclusion criteria included: failure to discuss U.S. veterans, U.S. veteran suicide, or U.S. veteran substance use, not written in English, published before 1985, or duplicating another hit. Title review eliminated 189 hits. Abstract review eliminated 54. Full reading of the remaining 65 articles eliminated 51. Bibliographic review and review of the March 2012 issue of the American Journal of Public Health, which was devoted to veteran suicide, produced 13 additional articles for a total of 27 articles. Final review of the 27 articles left 16 that are included in this review, and one article was added in review (Figure 1).
Figure 1.
Literature Review Flowchart
3. RESULTS
3.1 Summary of Identified Studies
The focus of this paper is on associations of substance use with suicide among female veterans. Here, we present information on suicide first to demonstrate how problematic suicide is in this population and to show that only few available studies of suicide among veterans have explored substance use as a related variable. We identified nine studies that analyzed completed suicide among veterans (Table 1): all included large data sets (n≥5,948). Three studies examined completed suicide among VA treated veterans are summarized in Table 2 (n≥10,163). Additionally, five studies examined substance use and either completed or attempted suicide (Table 3); four focused on VA patients (n≥8,807); one focused on veterans in substance abuse treatment (n=625).
Table 1.
Suicide among Veterans from the Vietnam to Modern Eras
| Authors | Samples & Years Data Collected | Study Designs | Outcome Measures | Key Findings on Suicide Variables |
|---|---|---|---|---|
| Gibbons et al., 2012 | • 27,391 (24.6% active or former military) suicide deaths among men aged >17; • 2005-2008. |
Cross-sectional | Completed Suicide | • Estimated 24% of all suicides were by former military, Risk Ratio 1.29; • Veterans Aged 17-24 Relative Risk 3.84; Veterans Aged 25-75 1.5; Veterans Aged >75 1.36. |
| McFarland et al., 2010 | • 5,948 Female Suicidal Descendants; • 2004-2007. |
Cross-sectional | Completed Suicide | • Standardized Mortality Ratio (SMR) Military Service Population: aged 18-34 1.76, CI 1.32-2.27; aged 35-44 1.76, CI 1.32-2.27; aged 35-44 1.30, CI 1.00-1.66; • SMR Veterans aged 18-34 3.05, CI 2.31-3.96; aged 35-44 1.78, CI 1.37-2.29; aged 45-64 1.58, CI 1.27-1.95. |
| Kaplan et al., 2009 | • 28,534 (30% women) Suicide Decedents; • 2003-2006 |
Cross-sectional | Completed Suicide | • Female veterans aged 18-34 had the highest rate; |
| Kang & Bullman, 2008 | • 490,346 OIF/OEF veterans; • October 2001-December 2005 |
Retrospective Cohort Study | Completed Suicide | • SMR 1.15, CI 0.97-1.35; • Active Duty Veterans SMR 1.33, CI 1.03-1.69; • Veterans with Mental Disorder SMR 1.77, CI 1.01-2.87 |
| Cypel & Kang, 2008 | • 9,911 Females (46% Vietnam Veterans); • Through 2004 |
Retrospective Cohort Study | Completed Suicide | • Vietnam veterans had lower mortality than women in the US population for all causes (SMR = 0.87, 95% CI 0.80-0.94); • Adjusted Suicide Relative Risk 0.90, CI 0.44-1.85. |
| Boehmer et al., 2004 | • 18,313 Army Vietnam Veterans; • Discharge (1965-1977)-2000 |
Retrospective Cohort Study | Completed Suicide | • 0-5 years from discharge, 34.5% Veterans and 20.1% non-Veterans committed suicide for a Crude Rate Ratio (CRR)=1.72, CI 0.76-3.88; • >5 years from discharge, 23.7% Veterans and 25.7% non-Veterans (CRR 0.93, CI 0.64-1.34). |
| Kang & Bullman, 2001 | • 621,902 Gulf War (7% women) & 746,291 non War Veterans (13.3% women); • 1991-1997 |
Retrospective Cohort Study | Completed Suicide | • Suicide Rate for Male War Veterans 1.8,* non War Veterans 1.9; • Male Adjusted Rate Ration (ARR) 0.92, CI 0.83-1.02. • Suicide Rate for Female War Veterans 0.8, Non War Veterans 0.6; • Female ARR 1.29, CI 0.78-2.31. |
| Bullman & Kang, 1996 | • 34,534 Wounded Army Vietnam Veterans; • Injury to death or 1991 |
Retrospective Cohort Study | Completed Suicide | • Standardized Mortality Ratio (SMR)=1.12, CI 0.96-1.30; • Wounded ≥ 2 times SMR 1.58, CI 1.06-2.26; • Hospitalized ≥ 2 SMR 1.73, CI 1.10-2.60. |
| Kang & Bullman, 1996 | • 695,516 (7.2% women) Gulf War & 746,291 (13.3% women) Non War Veterans; • 1990-September 1993 |
Retrospective Cohort Study | Completed Suicide | • Adjusted Suicide Rate Ratio 1.47, CI 0.63-3.43 • War Veterans Suicide Mortality Rate 1.53* vs. non-War Veterans 1.54 (ARR) =0.94, CI 0.79-1.12) |
per 10,000 person-years
**per 100,000 person-years.
Table 2.
Suicides among Veterans Administration (VA) Treated Veterans
| Authors | Samples & Years Data Collected | Study Designs | Outcome Measures | Key Findings on Suicide Variables (Females Only) |
|---|---|---|---|---|
| Weiner et al., 2011 | • 10,163 (8.8% female) former VA patients; • 1993-2002. |
Retrospective Cohort Study | Completed Suicide | • Suicide was the leading cause of death for females (25%); • 22.7% had some form of psychoses; • 20.3% had depression. • The most common comorbidities were alcohol abuse or disorder and drug abuse or disorder; - 31.8% abused alcohol or had an alcohol use disorder (32.9% males and 20.7% females); - 21.8% abused drugs or had a drug use disorder (22.6% male and 13.5% female). |
| McCarthy et al., 2009 | • 4,670,968 (10.1% female) former VA patients; • 2000-2001. |
Cross-sectional | Completed Suicide | • SMR Female VHA patients 1.87, CI 1.35-2.47; • SMR Female VHA patients Aged 40-49 2.15, CI 1.25-3.29; • SMR Female VHA patients Aged 50-59 2.36, CI 1.22-3.88. |
| Maynard & Boyko, 2006 | 62,080 (4% female) Washington veterans; Using and not using VA care from1998-2002. | Longitudinal | Completed Suicide | • Suicide was the 8th cause of death for VA treated veterans, higher among those using the VA compared to those who did not (1.6% vs. 0.9%); • Drug and alcohol related deaths were more common in the VA system and 6th leading cause of death (5.2% vs. 1.7%); • Drug and alcohol related deaths were 2x more likely among female veterans using the VA when compared to female veterans not using it; • Female veterans with drug or alcohol induced deaths were more likely to be young, single or divorced, and smoke cigarettes when compared to those who died from other causes (e.g., cardiovascular disease). |
Table 3.
Suicide and Substance Use among Veterans in the Modern Era
| Authors | Samples & Years Data Collected | Study Designs | Outcome Measure | Key Findings on Suicide and Substance Use |
|---|---|---|---|---|
| Ilgen et al., 2010 | • 3,291,891 (10% female) former VA patients; • Treated 1999-1998 & followed 2000-2007. |
Prospective Cohort Study | Completed Suicide | • 46.8% of completed suicides had a psychiatric condition; • The most common was depression (31.2%) followed by a substance use disorder (21.3%); • Women with any substance abuse or dependence were at increased risk of suicide when compared to men; • Women with the greatest risk were those with a substance use disorder; • In men, risk was greatest for those with bipolar disorder, followed by depression, and substance use disorder. |
| Jakupcak et al., 2009 | • 435 Operation Enduring Freedom/Operation Iraqi Freedom Veterans referred to VA mental health services from 2004-2007 | Cross-Sectional | Suicidal Ideation | • Veterans with PTSD + 2 comborbidities that included either major depressive disorder, alcohol abuse or drug abuse were 5.7 times more likely to endorse suicidal ideation than veterans with PTSD only. • Veterans with PTSD and one comorbidity were not more likely to endorse suicidal ideation. |
| Ilgen et al., 2007 | • 8,807 (4% women) veterans seeking VA treatment for substance use disorders; • 49% in treatment for alcohol, 26% for combined alcohol and drug use, 10% cocaine, 6% poly-drug use, 3% heroin, and 2% marijuana; • Years data collected not provided. |
Retrospective Cohort | Suicide Attempt | • 4% reported a suicide attempt within 30 days of follow-up; • Three baseline indices were unique risks for a suicide attempt: severity of suicidal/psychiatric symptoms, number of days of alcohol problems, and age adjusted years of cocaine use; • Only involvement in the criminal justice system was protective; • Substance use treatment did not mediate the effect of risk factors on suicide attempt, but the final model was additive, indicating increased risk with each factor; • Greater engagement in treatment cut suicide risk from 10%-5%. |
| Ziven et al., 2007 | • 1,683 veterans (2.7% women) treated by the VA for depression; • 1999-2004 |
Longitudinal | Completed Suicide | • Veterans with a substance abuse diagnosis had a higher rate of suicide than those without. • Ratio among male to female veterans was 3:1 vs. 4:1 in the general population. |
| Benda, 2005 | • 315 homeless male & 310 homeless female veterans; • In treatment for substance abuse. |
Prospective Cohort Study | Suicide ideation and attempt | • 44.4% of males contemplated suicide and 26.7% attempted it; • 48.7% of females contemplated suicide and 36.5% attempted it; • Sexual or physical abuse in childhood, current sexual abuse, family problems, partner problems, depression, and fearfulness predicted suicidal measures among women; • Self-esteem and social support were protective. |
3.2 Suicide among Veterans (Table 1)
Nine studies analyzed completed suicide among veterans. Three examined male and female data, one did not differentiate males and females within the study sample, three examined males only, and two focused on females only. Newest data were collected in 2008. Studies compared rates to the general population or compared combat veteran rates with non-combat veteran rates. None has examined substance use.
Rate of completed suicide was no higher among early era combat veterans when compared to noncombat veterans and the general population. Kang and Bullman (1996 and 2001) compared Defense Manpower Data Center reported suicide deaths of Gulf War veterans to reported suicide deaths of noncombat military personnel (n=695,516, women representing 7.2% of the sample; n=746,291, women representing 13.3% of the sample, respectively) and found no differences in suicide mortality rate between Gulf War veterans and noncombat military personnel. By analyzing female veteran data reported by the Veterans Affairs beneficiary file and Social Security Administration Death Master File through 2004, Cypel and Kang (2008) also found no differences in suicide mortality rates between deployed female Vietnam veterans (n=4,586) and not deployed female veterans (n=5,325). Cypel and Kang (2008) did not examine variations in suicide mortality based on factors outside of women's deployment status. However, Bullman and Kang (1996) explored whether trauma affected suicide mortality among 34,534 combat-wounded, male Vietnam veterans tracked from their time of injury to 1991 (or death) and found that the Standardized Mortality Ratio (SMR) increased with combat trauma and the number of times a soldier was wounded. Similarly, Boehmer et al. (2004) examined completed suicides among 18,313 male U.S. Army Vietnam veterans followed from discharge (1965-1977) through 2000; they found that rates of completed suicides were slightly higher for combat veterans than non-combat veterans for the first five years from discharge but not after. More recent data show a more complex picture. Although not differentiating the proportion of the sample that was female, Kang and Bullman (2008) compared the number of suicide deaths among 490,346 OIF/OEF veterans who left active duty from October 2001-December 2005 and who were followed through December 2005 to suicide deaths in the general population. They found that proportions of suicide deaths were higher among veterans with a mental disorder when compared to those without one. Taken together, it appears that the prevalences of combat veteran completed suicides are not higher than those in the general population or in noncombat veterans in the past. However, in all male samples or recent studies that did not differentiate by sex, the number of completed suicides was increased by traumatic experience and presence of a mental disorder. These studies, however, have not examined substance use status.
Of note, more recent data comparing veterans to nonveterans found a higher prevalence of completed suicide among veterans, particularly women. Kaplan et al. (2009) examined a total of 28,534 suicide decedents (women, 30% of the sample) from the 2003-2006 data files in the National Violent Death Reporting System (NVDRS) and found that the suicide rate among male veterans was 47% higher than the rate among nonveterans. Among female veterans, the suicide rate was nearly three times higher than that among nonveterans. Male and female veterans aged 18-34 years had the highest suicide rate. In a similar analysis of 27,391 completed suicides (2005-2008) among male veterans aged ≥17 years (24.6% active or former military) and reported by the NVDRS, Gibbons et al. (2012) found those in the youngest age group (17-24 years) were almost 4 times more likely to commit suicide than same aged men with no service. In a similar analysis of data from 2004-2007 female only NVDRS and American Community Survey (ACS), McFarland et al. (2010) found that, among 5,948 women (aged 18-64) who committed suicide, Standardized Mortality Ratios (SMR; using female veterans as one denominator and a broader military service population as another) were greater than 1, indicating an elevated rate. The highest ratio was among veterans aged 18-34 (SMR=3.05, 95% CI=2.31-3.96). Age related results were similar for women with military service. Younger veterans had greater likelihood to complete suicide than older ones. Young female veterans in particular may have higher suicide mortality when compared to other women in the military and female nonveterans. It is unclear why younger age is a factor in completed suicides. Gibbons et al. (2012) suggests that it may represent a cohort effect related to particular conflicts or experiences returning from conflict. It may also be that suicide always occurs most often immediately after service (Gibbons et al., 2012). These studies, however, have not included substance use in their analyses.
In summary, data from past eras have not shown differences in completed suicide between veterans and members of the general population. However, more recent data indicated more suicide deaths among veterans than nonveterans, including among females. Studies that examined all male samples or did not differentiate by gender also found that completed suicides increased with traumatic exposure and presence of a mental health disorder. Male and female veterans aged 18-34 years had a higher suicide rate than older adults. Young female veterans in particular had higher suicide mortality when compared to women in the military and female nonveterans. These studies of female veterans did not explore factors associated with suicide beyond age and deployment status, and no studies have addressed substance use status. However, given that substance abuse among veterans is similarly associated with younger ages, combat exposure, and poor mental health (Seal et al., 2011), there is a need to explore the link between suicide and substance abuse measures.
3.3 Suicide among VA Treated Veterans (Table 2)
Of note, female VA enrollment has increased over 40% from past eras (Batuman et al., 2011). The need for research with a focus on VA treated female veterans is at an all time high. We found three studies that addressed suicide among VA treated veterans (Table 2). One did not include substance use status (McCarthy et al., 2009); one examined the prevalence of substance use in the sample (Weiner et al., 2011); and one explored drug and alcohol induced deaths (Maynard and Boyko, 2006). All data were collected during or before 2002.
Weiner et al. (2011) examined records of a total of 10,163 veterans (women, 8.8% of the sample) previously treated at the VA for a suicide attempt (1993-1998) and followed through 2002. Contrary to prior observation that men were generally more likely than women to complete suicide (Cibis et al., 2012), Weiner et al. (2011) found that female veterans treated by the VA for a suicide attempt had a higher proportion of completed suicides when compared to similarly treated male veterans. It was unclear from the findings why a greater proportion of women than men completed suicide. However, more women than men in their study sample had psychoses (female 22.7% vs. male 21.0%) or depression (female 20.3% vs. male 18.3%). Completed suicide was the leading cause of death for women (25% of deaths); suicide was the second leading cause of death among men (12.7%), following heart disease. While SUD was prevalent in the sample for men (32.9% abused alcohol; 22.6% abused drugs) and women (20.7% abused alcohol; 13.5% abused drugs), relationships between substance use and suicide variables were not explored.
Additionally, suicide mortality was higher among females seen by the VA than among women in the general population. McCarthy et al. (2009) computed SMRs for those committing suicide among 4,670,968 (10.1% female) former VA patients. Patients were seen by the VA in 2000 and followed to their date of death or through 2001. Rates were computed based on suicide deaths in 2001 and adjusted for age. Overall, rate of suicide deaths among VA patients (male and female) were an estimated 66% higher than suicide deaths in the general population (SMR 1.66; 95% CI: 1.58, 1.75). Suicide deaths among VA treated males were also 66% greater than suicide deaths among males in the general population (1.66; 95% CI: 1.58, 1.74). Among females, suicide deaths were 87% higher than suicide deaths among women in the general population (1.87; 95% CI: 1.35, 2.47). Substance use was not explored.
Further, data from veterans in the VA show a high prevalence of completed suicide and alcohol/drug related deaths. Maynard and Boyko (2006) compared causes of death for Washington veterans (n=62,080; 4% of the sample female) by VA care status from 1998-2002 and found that, while suicide was the 8th cause of death for VA treated veterans, it was higher among those using the VA compared to those who did not (1.6% vs. 0.9%). Alcohol or drug induced deaths, identified with veteran death certificates, were more common among patients in VA and represented the 6th leading cause of death (5.2% vs. 1.7%). Of note, alcohol or drug induced deaths were two times more likely among female veterans using the VA when compared to female veterans not using it. Female veterans with alcohol or drug induced deaths were more likely to be young, single or divorced, and smoke cigarettes when compared to female veterans who died from other causes (e.g., cardiovascular disease).
Taken together, women who used VA services were more likely to commit suicide than women in the general population (McCarthy et al., 2009). Alcohol or drug induced deaths were twice as likely among females treated by the VA when compared to females not treated by the VA (Maynard and Boko, 2006). However, it is unclear whether substance-related deaths were completed suicides or accidents (Maynard and Boko, 2006). In a study of VA treated veterans with a previous suicide attempt, women also had a higher proportion of completed suicides than males (Weiner et al., 2011). In the same study, a greater proportion of women than men were also diagnosed with psychoses or depression (Weiner et al., 2011). Collectively, research could explore whether and how psychiatric status contributes to this finding (e.g. more psychopathology among women than men in VA).
3.4 Suicide and Substance use Among Female Veterans (Table 3)
Five studies examined relationships between suicide variables and substance use, with four focusing on the VA populations. Two examined veterans seeking or in substance abuse treatment, and two examined veterans seeking or in mental health treatment. Two used completed suicide as their outcome measure; one used suicide attempt; one determined suicide attempt and suicidal contemplation; one used suicidal ideation. Age of data was not always reported, but the newest data were from 2007.
When substance use is implicated in increased suicide measures, it appears that multiple factors may be at work. Among 407 OIF/OEF veterans (9.06% of the sample was female) seeking mental health services through the VA in Puget Sound, Jakupcak et al. (2009) found that diagnosis with PTSD and two comorbid mental disorders, either major depressive disorder, alcohol abuse disorder, or drug abuse disorder, increased odds of suicide ideation 5.7 times (95% CI 2.09–23.85). Diagnosis with PTSD and a single comorbid condition did not increase odds. That alcohol abuse, drug abuse, or both were required to increase suicide ideation suggests that these interact with PTSD to endanger veterans.
Prolonged alcohol and cocaine use also appears to increase odds of suicide attempts among veterans using VA services. Ilgen et al. (2007) examined a national sample of 8,807 (4% of the sample was female) veterans who sought treatment for a SUD through the VA at intake and an average of 13 months after and found that 4.0% reported a suicide attempt within 30 days of follow-up. Three indices increased odds of suicide attempt: severe suicidal or psychiatric symptoms, an increased number of days of alcohol problems, and longer years of cocaine use. The effects of the three indices were found to be additive. Greater engagement in substance abuse treatment decreased odds of suicide attempt from 10%-5%, suggesting the importance of treating substance use problems. Involvement with the criminal justice system also decreased odds of suicide attempt, which may reflect receipt of substance use treatment while incarcerated. Results suggest that current models used to predict suicide behavior may be strengthened by including a broader array of factors, such as past suicide attempt and substance use, and that substance use treatment might reduce suicidality (Ilgen et al., 2007).
VA treated veterans with a SUD had a higher suicide mortality rate than those without a disorder. Zivin et al. (2007) examined completed suicides among 807,694 veterans (2.7% females in the sample) treated by the VA for depression between April 1, 1999-September 30, 2004 and found a high rate of completed suicide (88.25 per 100,000 person-years vs. 13.50 per 100,000 person-years in the general population). The suicide rate among veterans treated for depression with a comorbid SUD rose to 119.73 per 100,000 person-years, although veterans treated for comorbid PTSD and depression had a reduced rate (Hazard Ratio 0.77, 95% CI 0.68, 0.87). Young veterans were more likely than older ones to commit suicide, and men more likely than women. The suicide relative risk ratio among male to female veterans was 3:1, which was smaller than the 4:1 ratio found for men to women in the general population. The lower ratio suggests a closer suicide gap between men and women in the studied sample and that completed suicide may disproportionately affect women in the VA treated veteran population, which may relate to poor mental health or substance abuse among treated female veterans (Ziven et al., 2007).
Among VA treated veterans, another study showed that psychiatric diagnosis, particularly SUD, is associated with the highest hazard ratio for completed suicide among women. Ilgen et al. (2010) examined data for 3,291,891 veterans treated by the VA and followed from FY2000-FY2007 or until death and found that 46.8% of those who had committed suicide had a psychiatric condition. The second most common condition was SUD (21.3%), following depression (31.2%). While completed suicide hazard ratios were higher for males compared to females (hazard ratios for females 0.28, CI 0.25-0.32), women with any current mental disorder had increased hazard ratios for completed suicide when compared to men. For men, the highest hazard ratio for completed suicide was observed with bipolar disorder. For women, the highest hazard ratio for completed suicide was observed with a SUD, suggesting the need for research to elucidate the effects of SUD on suicide for women.
One study examined suicide ideation and attempted suicide among veterans in substance abuse treatment. In a study of 315 male and 310 female homeless veterans in treatment for substance abuse, Benda (2005) found that previous suicidal ideation was higher in females (48.7%) than males (44.4%), and so was a past suicide attempt (36.5% vs. 26.7%, respectively). Sexual or physical abuse in childhood, current sexual abuse, family problems, partner problems, depression, and fearfulness predicted suicidal ideation and attempt among women, while self-esteem and social support decreased odds of suicidal ideation and attempt (Benda, 2005).
In summary, PTSD increased suicide risk among male and female VA treated veterans when it co-occurred with substance abuse and another mental disorder, either a different kind of substance abuse or major depressive disorder. Women with a current SUD had a higher hazard ratio for completed suicide compared to men with a current SUD (Ilgen et al., 2010). Of all mental disorders examined, women with a SUD had the highest hazard ratio for completed suicide (Ilgen et al., 2010). Veterans with comorbid depression and a SUD also had a higher suicide mortality rate than veterans with depression and no SUD (Ziven et al., 2007). Collectively, substance abuse or dependence may increase odds of completed suicide in women and that comorbid depression and SUD may interact to increase odds of suicide among female veterans. Previous suicidal ideation was also higher in female veterans in treatment for substance abuse than in males, and so was a past suicide attempt (Benda, 2005). On the other hand, engagement in substance abuse treatment can decrease odds of suicide attempt among VA treated veterans (Ilgen et al., 2007).
4. DISCUSSION
Substance use problems and suicide appear to disproportionately affect female veterans. Data showed high levels of problematic substance use by female veterans using the VA (Bradley et al., 2001; Davis et al., 2003). Military women also had increased odds of initiating problem drinking and more often engaged in unsafe drinking and illicit or nonmedical drug use compared to military men (Jacobson et al., 2008; Lande et al., 2007; Bray and Hourani 2007). Data also showed a disproportionately high prevalence of suicide deaths among female veterans, with two studies finding a female veteran suicide rate three times higher than that of women in the general population (Kaplan et al., 2009; McFarland et al., 2010). Additionally, gender specific comparison found women using the VA completed suicide in disproportionately high numbers when compared to men using the VA (Zivin et al., 2007). Among VA treated veterans, substance use was implicated in increased suicide ideation, attempt, or completion (Ziven et al., 2007; Ilgen et al., 2007; Jakupcak et al., 2009), and completed suicide hazard ratios for females were highest for those with a SUD (Ilgen et al., 2010). Veteran substance abuse or disorder and completed suicide share common correlates, including younger age, combat exposure/deployment, and poor mental health. How each correlate relates to female veterans is discussed below.
Poor mental health positively correlates with suicide and substance use, and diagnosis with either depression or PTSD and a comorbid SUD increased the likelihood of completed suicide and suicidal ideation among VA treated veterans (Ziven et al. 2007; Jakupcak et al., 2009). While poor mental health and a SUD increased suicide measures for males and females, female veterans appear particularly vulnerable to adverse effects. Data from the 2004-2006 NSDUH found that female veterans were twice as likely as male veterans to experience past-year severe psychological distress (14.5 vs. 6.5 percent; SAMHSA, 2007), and Weiner et al. (2011) found that the association between a psychiatric diagnosis and suicide was greater for female than male veterans. Female veterans in the VA SUD outpatient treatment setting also had high prevalences of comorbid mental disorders, with 47.6% also having PTSD, 38.7% serious mental illness, and 31.9% major depressive disorder (Gifford et al., 2011). In addition, females who served in OIF/OEF and used large quantities of alcohol and drugs screened positive for PTSD more than those not using substances, and comparison of women screening positive versus negative for PTSD found only alcohol use predicting the PTSD status (Nunnink et al., 2010). When examining relations among SUD, poor mental health, and suicide, it is worth noting that SUD may be uniquely important. Jakupcak et al. (2009) found that, while PTSD and one comorbid diagnosis (depression, alcohol abuse, or drug abuse) did not increase suicide ideation among VA treated veterans, PTSD and diagnosis with two did. Ziven et al. (2007) also found an increased suicide rate among VA treated veterans with comorbid depression and SUD but a decreased rate among VA treated veterans with comorbid PTSD and depression. Among female veterans, clustering of substance use and poor mental health may indicate a severe pattern of psychopathology, as substance abuse could intensify existing mental disorders (Leeies et al., 2010).
Combat exposure also increased the likelihood for suicide and substance use among veterans. This may relate to poor mental health, as exposure to violence can result in conditions, such as PTSD. Past violence increased the likelihood of suicide ideation and attempt among individuals seeking SUD treatment when controlling for demographic factors and depressive symptoms in a national sample (Ilgen et al., 2010a). More extreme violence increased the likelihood of multiple suicide attempts (Ilgen et al., 2010a). Data predating OIF/OEF suggests that female veterans are more likely than male veterans to meet PTSD criteria after traumatic exposure (Tolin and Foa, 2006). Direct combat exposure is increasing for women due to the changing nature of warfare (Hoge et al., 2007), and the recent lift on the ban restricting women from some combat roles, including positions in the infantry, armor, and special operations (Rand, 2013), suggests that this trend will continue. However, even women not directly in combat may experience associated trauma through support activities, such as handling human remains (Hoge et al., 2007). Repeated traumatic exposure increases the likelihood of PTSD (Cloitre et al., 2009), and Sadler found that 54% of 520 female veterans reported a history of physical or sexual violence before service. Sexual harassment and abuse also may increase odds of PTSD, depression, or SUD (Kimerling et al., 2010; Booth et al., 2011), and service women are more often subjected to sexual misconduct than service men (Street et al., 2009). Of 3,946 (59% female) veterans, Gradus et al. (2008) found women who experienced sexual harassment had increased odds of harmful drinking, men did not, and the relationship was accounted for by depressive symptoms. It appears that a history of violence and co-occurring combat and sexual traumas may have cumulative psychological effects (Street et al., 2009). Women specific deployment stressors also affect mental health. For example, among 495 (25% female) Gulf War veterans, Vogt et al. (2005) found that concerns about family/relationship disruptions and lack of social support during deployment affected women's post deployment mental health more than men's (Vogt et al., 2005). OIF/OEF data also showed that deployed women more often developed major depression and SUD than deployed men (Shen et al., 2012). Upon return, difficulties readjusting to previous familial and social roles, public and private perceptions of what it means to be a female veteran, and inability to access health care can exacerbate problems (Street et al., 2009). Female military personnel and veterans face multiple stressors that can impact mental health.
Younger age also associated with suicide and substance use. This may represent a cohort effect, relating to particular conflicts or time-specific experiences that occur when returning from conflicts (Gibbons et al., 2012). It might also be that veteran suicide is time sensitive, most often occurring immediately after leaving the service (Gibbons et al., 2012). Alternatively, it could be that younger individuals are more likely than older ones to engage in self-injury (Serras et al., 2010). Bakst et al. (2010) analyzed data for 529 individuals with psychotic illness to develop a suicide risk index and also found that younger age increased likelihood of suicide attempt, and so did lifetime substance abuse. Historical findings also suggest that, compared to older individuals who completed suicide, younger individuals who completed suicide were more likely to have used drugs (Rich et al., 1986). While young age positively associates with suicide and substance use among female veterans, the nature of the relationship is unclear.
The identified associations among substance use, poor mental health, and suicide relate have important clinical applications. A challenge in suicide prevention is identifying subgroups of individuals to benefit from suicide-related intervention (Ilgen et al., 2010). Findings suggest that female veterans with SUD and comorbid depression or PTSD are such a subgroup. Female veterans in poor mental health are likely to endorse multiple health problems, suggesting a need for primary care strategies tailored toward them (Dobie et al., 2004). Knowledge of suicide risk may also be low among SUD treatment providers (Ilgent et al., 2010), who should be made aware of the potential for suicide behaviors among female veterans seeking assistance (Ilgen et al., 2007). The high prevalence of comorbid SUD and other mental disorders indicates a need for evidence-based treatment programs to address multiple disorders, something largely lacking from current VA services (Seal et al., 2011). Additionally, SUD often goes undiagnosed among Iraq and Afghanistan veterans (Seal et al., 2011), which may be especially true of women who were historically often missed by traditional screening measures (Davis et al., 2003). Better screening is needed to identify those needing services (Seal et al., 2011), as engagement in substance abuse treatment may decrease odds of suicide attempt (Ilgen et al., 2007).
Current findings suggest avenues for future research. It is likely that multiple factors are at work, and studies must explore how substance use, poor mental health, and suicidal behaviors interact in this vulnerable population. Some female veterans may self-medicate with substances to relieve psychological symptoms (Leeies et al., 2010). However, female veterans seeking VA assistance for psychological problems are more vulnerable to drug abuse due to gender differences in VA prescribing practices. For example, females presenting to the VA for PTSD received benzodiazepines 38.3% of the time, while similar males received them only 29.8% (Bernardy et al., 2012). Benzodiazepines are contraindicated in PTSD cases, have high potential for dependence (Bernardy et al., 2012), and are implicated in increased competed suicides among veterans (Pfeiffer et al., 2009). Similarly, female veterans with PTSD may be more susceptible to self-harm because of past exposure to pain and violence (Joiner, 2005). With each of these, substance use might increase impulsivity and trigger suicidal action (Braquehais et al., 2010), and thus offer a unique opportunity to intervene. Longitudinal data are needed to elucidate the temporal associations (i.e., SUD leading to mental disorder or mental disorder leading to SUD) among female veterans to inform intervention efforts. Additionally, substance use studies should include suicide variables and vice versa. Because women are more likely to attempt suicide and men complete it (Cibis et al., 2012), studies with a special focus on suicide attempt may be warranted to help identify more female veterans in need of targeted intervention efforts. As most studies that examined suicide and substance use had female samples at ≤ 10%, this may be especially warranted. The proportion of women with military service is increasing, as are their mental health needs. New research must address the needs of this population.
While the overall proportion of female veterans in studies that examined suicide and substance use were small, results were suggestive. There is a clear association between suicide and substance use among female veterans, particularly when comorbid mental illness is included in analyses. How this relationship works is unclear and research is needed to explore pathways and potential interventions. Because women traditionally made up only a small proportion of veterans, female veteran mental health needs have often gone overlooked (Goldzweig et al., 2006). Women are the fastest growing cohort in the veteran community, and the VA is committed to identifying and serving female veteran's unique health care needs (Friedman et al., 2011). Overall, findings highlight the importance of assessing suicidal measures in female veterans with complex psychiatric profiles, particularly those who misuse substances.
Acknowledgments
Role of Funding Source
This work is made possible by research support from the U.S. National Institutes of Health (R33DA027503, R01DA019623, R01DA019901, and R01MD007658; PI: Li-Tzy Wu). The sponsoring agency had no further role in the writing of this paper or the decision to submit the paper for publication. The opinions expressed in this paper are solely those of the authors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Author Chapman conducted the literature search. Authors Chapman and Wu wrote the manuscript.
Conflict of Interest
Authors declare they have no conflicts of interest.
REFERENCES
- Allen JP, Cross G, Swanner J. Suicide in the army: a review of current information. Mil. Med. 2005;170:580–584. doi: 10.7205/milmed.170.7.580. [DOI] [PubMed] [Google Scholar]
- Brenner LA, Gutierrez PM, Cornette MM, Betthauser LM, Bahraini N, Staves PJ. A qualitative study of potential suicide risk factors in returning combat veterans. J. Ment. Health Couns. 2008;30:211. [Google Scholar]
- Bakst S, Rabinowitz J, Bromet EJ. Antecedents and patterns of suicide behavior in first-admission psychosis. Schizophr. Bull. 2010;36:880–889. doi: 10.1093/schbul/sbp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batuman F, Bean-Mayberry B, Goldzweig CL, Huang C, Miake-Lye M, Washington DL, Yano EM, Zephyrin LC, Shekelle PG. Health Effects of Military Service on Women Veterans. VA-ESP Project # 05-226. Department of Veterans Affairs; Washington D.C.: 2011. [PubMed] [Google Scholar]
- Benda BB. Gender differences in predictors of suicidal thoughts and attempts among homeless veterans that abuse substances. Suicide Life Threat. Behav. 2005;35:106–116. doi: 10.1521/suli.35.1.106.59262. [DOI] [PubMed] [Google Scholar]
- Bernardy NC, Lund BC, Alexander B, Jenkyn AB, Schnurr PP, Friedman MJ. Gender differences in prescribing among veterans diagnosed with posttraumatic stress disorder. J. Gen. Intern. Med. 2012;28:S542–S548. doi: 10.1007/s11606-012-2260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Best D, Gossop M, Man L-H, Finch E, Greenwood J, Strang J. Accidental and deliberate overdose among opiate addicts in methadone maintenance treatment: are deliberate overdoses systematically different? Drug Alcohol Rev. 2000;19:213–216. [Google Scholar]
- Boehmer TK, Flanders WD, McGeehin MA, Boyle C, Barrett DH. Postservice mortality in Vietnam Veterans: 30-year follow-up. Arch. Intern. Med. 2004;164:1908–1916. doi: 10.1001/archinte.164.17.1908. [DOI] [PubMed] [Google Scholar]
- Booth BM, Mengeling M, Torner J, Sadler AG. Rape, sex partnership, and substance use consequences in women veterans. J. Trauma Stress. 2011;24:287–294. doi: 10.1002/jts.20643. [DOI] [PubMed] [Google Scholar]
- Borges G, Walters EE, Kessler RC. Associations of substance use, abuse, and dependence with subsequent suicidal behavior. Am. J. Epidemiol. 2000;151:781–789. doi: 10.1093/oxfordjournals.aje.a010278. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, Maynard C, Burman ML, Ktvalahan DR. Two brief alcohol-screening tests from the alcohol use disorders identification test (AUDIT). Arch. Intern. Med. 2003;163:821–829. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Braquehais MD, Oquendo MA, Baca-Garcia, Sher L. Is impulsivity a link between childhood abuse and suicide. Compr. Psychiatry. 2010;51:121–129. doi: 10.1016/j.comppsych.2009.05.003. [DOI] [PubMed] [Google Scholar]
- Bray RM, Pemberton MR, Hourani LL, Witt M, Olmsted KLR, Weimer B, Lane ME, Marsden ME, Scheffler S, Vandermaas-Peeler R, Aspinwall KR, Anderson E, Spangnola K, Close K, Gratton JL, Calvin S, Bradshaw M. 2008 Department of Defense Survey of Health Related Behaviors among Active Duty Military Personnel: A component of the Defense Lifestyle Assessment Program (DLAP). [July 5, 2012];Research Triangle Institute. 2009 On-line: http://www.tricare.mil/tma/2008HealthBehaviors.pdf.
- Bray RM, Hourani LL. Substance use trends among active duty military personnel: findings from the United States Department of Defense Health Related Behavior Surveys, 1980–2005. Addiction. 2007;102:1092–1101. doi: 10.1111/j.1360-0443.2007.01841.x. [DOI] [PubMed] [Google Scholar]
- Bray RM, Fairbank JA, Marsden ME. Stress and substance use among military women and men. Am. J. Drug Alcohol Abuse. 1999;25:239. doi: 10.1081/ada-100101858. [DOI] [PubMed] [Google Scholar]
- Bullman TA, Kang HK. The risk of suicide among wounded Vietnam veterans. Am. J. Public Health. 1996;86:662–667. doi: 10.2105/ajph.86.5.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ, Borges GLG, Wilcox HC. Acute alcohol use and suicidal behavior: a review of the literature. Alcohol. Clin. Exp. Res. 2004;28:18s–28s. doi: 10.1097/01.alc.0000127411.61634.14. [DOI] [PubMed] [Google Scholar]
- Cibis A, Mergl R, Bramesfeld A, Althaus D, Niklewski G, Schmidtke A, Hegerl U. Preference of lethal methods is not the only cause for higher suicide rates in males. J. Affect. Disord. 2012;136:9–16. doi: 10.1016/j.jad.2011.08.032. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stolbach BC, Herman JL, van der Kolk B, Pynoos R, Wang J, Petkova E. A developmental approach to complex PTSD: childhood and adult cumulative trauma as predictors of symptom complexity. J. Trauma Stress. 2009;22:399–408. doi: 10.1002/jts.20444. [DOI] [PubMed] [Google Scholar]
- Cypel Y, Kang H. Mortality patterns among women Vietnam-Era veterans: results of a retrospective cohort study. Ann. Epidemiol. 2008;18:244–252. doi: 10.1016/j.annepidem.2007.11.009. [DOI] [PubMed] [Google Scholar]
- Davis T, Bush KR, Kivlahan DR, Dobie DJ, Bradley KA. Screening for substance abuse and psychiatric disorders among women patients in the VA Health Care System. Psychiatr. Serv. 2003;54:214–218. doi: 10.1176/appi.ps.54.2.214. [DOI] [PubMed] [Google Scholar]
- Dobie DJ, Kivlahan DR, Maynard C, Bush KR, Davis TM, Bradley KA. Posttraumatic stress disorder in female veterans: associated with self-reported health problems and functional impairment. Arch. Intern. Med. 2004;164:394–400. doi: 10.1001/archinte.164.4.394. [DOI] [PubMed] [Google Scholar]
- Friedman SA, Phibbs CS, Schmitt SK, Hayes PM, Herrera L, Frayne SM. New women veterans in the VHA: a longitudinal profile. Womens Health Issues. 2011;21:S103–S111. doi: 10.1016/j.whi.2011.04.025. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Brown CH, Hur K. Is the rate of suicide among veterans elevated? Am. J. Public Health. 2012;102:S17–S19. doi: 10.2105/AJPH.2011.300491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gifford E, Tavakoli S, Wang R, Matthews K. Female Veterans in Outpatient Substance Use Disorder Specialty Care. Center for Health Care Evaluation; Palo Alto, CA: 2011. [Google Scholar]
- Goldberg KC. The epidemiology of health problems in returning Operation Iraqi Freedom and Operation Enduring Freedom veterans. A national and North Carolina-based summary. N.C. Med. J. 2008;69:31–34. [PubMed] [Google Scholar]
- Goldzweig CL, Balekian TM, Rolon C, Yano EM, Shekelle PG. The state of women veterans’ health research. Results of a systematic literature review. J. Gen. Intern. Med. 2006;21(Suppl. 3):S82–S92. doi: 10.1111/j.1525-1497.2006.00380.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gradus JL, Street AE, Kelly K, Stafford J. Sexual harassment experiences and harmful alcohol use in a military sample: differences in gender and the mediating role of depression. J. Stud. Alcohol Drugs. 2008;69:348–351. doi: 10.15288/jsad.2008.69.348. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Terhakopian A, Castro CA, Messer SC, Engel CC. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. Am. J. Psychiatry. 2007;164:150–153. doi: 10.1176/ajp.2007.164.1.150. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Harris AHS, Moos RH, Tiet QQ. Predictors of a suicide attempt one year after entry into substance use disorder treatment. Alcohol. Clin. Exp. Res. 2007;31:1–8. doi: 10.1111/j.1530-0277.2007.00348.x. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Bohnert AS, Ignacio RV, McCarthy JF, Valenstein MM, Kim HM, Blow FC. Psychiatric diagnoses and risk of suicide in veterans. Arch. Gen. Psychiatry. 2010;67:1152–1158. doi: 10.1001/archgenpsychiatry.2010.129. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Burnette ML, Conner KR, Czyz E, Murray R, Chermack S. The association between violence and lifetime suicidal thoughts and behaviors in individuals treated for substance use disorders. Addict. Behav. 2010a;35:111–115. doi: 10.1016/j.addbeh.2009.09.010. [DOI] [PubMed] [Google Scholar]
- Jacobson IG, Ryan MAK, Hooper TI, Smith TC, Amoroso PJ, Boyko EJ, Gackstetter GD, Wells TS, Bell NS. Alcohol use and alcohol-related problems before and after military combat deployment. JAMA. 2008;300:663–675. doi: 10.1001/jama.300.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakupcak M, Cook J, Imel Z, Fontana A, Rosenheck R, McFall M. Posttraumatic stress disorder as a risk factor for suicidal ideation in Iraq and Afghanistan war veterans. J. Trauma Stress. 2009;22:303–306. doi: 10.1002/jts.20423. [DOI] [PubMed] [Google Scholar]
- Joiner T. Why People Die by Suicide. Harvard University Press; Cambridge, MA: 2005. [Google Scholar]
- Kang HK, Bullman TA. Is there an epidemic of suicides among current and former U.S. Military Personnel? Ann. Epidemiol. 2009;19:757–760. doi: 10.1016/j.annepidem.2009.05.004. [DOI] [PubMed] [Google Scholar]
- Kang HK, Bullman TA. Risk of suicide among US Veterans after returning from the Iraq or Afghanistan war zones. JAMA. 2008;300:652–653. doi: 10.1001/jama.300.6.652. [DOI] [PubMed] [Google Scholar]
- Kang HK, Bullman TA. Mortality among US Veterans of the Persian Gulf War: 7-Year Follow-up. Am. J. Epidemiol. 2001;154:399–405. doi: 10.1093/aje/154.5.399. [DOI] [PubMed] [Google Scholar]
- Kang HK, Bullman TA. Mortality among US Veterans of the Persian Gulf War. N. Eng. J. Med. 1996;335:1498–1504. doi: 10.1056/NEJM199611143352006. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, McFarland B, Huguet N. Firearm suicide among veterans in the general population: findings from the National Violent Death Reporting System. J. Trauma. 2009;67:503–507. doi: 10.1097/TA.0b013e3181b36521. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, McFarland BH, Newsom JT. Suicide among male veterans: a prospective population based study. J. Epidemiol. Community Health. 2007;61:619–624. doi: 10.1136/jech.2006.054346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, McFarland BH, Newsom JT. Correction: Suicide among male veterans: a prospective population-based study. J. Epidemiol. Commun. Health. 2007;61:751. doi: 10.1136/jech.2006.054346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimerling R, Street AE, Pavao J, Smith MW, Cronkite RC, PhD, Holmes, Frayne SM. Military-related sexual trauma among Veterans Health Administration patients returning from Afghanistan and Iraq. Am. J. Pub. Health. 2010;100:1409–1412. doi: 10.2105/AJPH.2009.171793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lande RG, Marin BA, Chang AS, Lande GR. Gender differences and alcohol use in the U.S. Army. J. Am. Osteopath. Assoc. 2007;107:401–407. [PubMed] [Google Scholar]
- Leeies M, Pagura J, Sareen J, Bolton JM. The use of alcohol and drugs to self-medicate symptoms of posttraumatic stress disorder. Depress. Anxiety. 2010;27:731–736. doi: 10.1002/da.20677. [DOI] [PubMed] [Google Scholar]
- Maynard C, Boyko EJ. Differences in cause of death of Washington State veterans who did and did not use Department of Veterans Affairs healthcare services. J. Rehabil. Res. Dev. 2006;43:825–830. doi: 10.1682/jrrd.2006.01.0004. [DOI] [PubMed] [Google Scholar]
- McCarthy JF, Valenstein M, Kim HM, Ilgen M, Zivin K, Blow FC. Suicide mortality among patients receiving care in the Veterans Health Administration health system. Am. J. Epidemiol. 2009;169:1033–1038. doi: 10.1093/aje/kwp010. [DOI] [PubMed] [Google Scholar]
- McFarland BH, Kaplan MS, Huguet N. Self-inflicted deaths among women with U.S. Military service: a hidden epidemic? Psychiatr. Serv. 2010;61:12. doi: 10.1176/ps.2010.61.12.1177. [DOI] [PubMed] [Google Scholar]
- Murdoch M, Bradley A, Mather SH, Klein RE, Turner CL, Yano EM. Women and war: what physicians should know. J. Gen. Intern. Med. 2006;21:s5–10. doi: 10.1111/j.1525-1497.2006.00368.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunnink SE, Goldwaser G, Heppner PS, Pittman JOE, Nievergelt CM, Baker DG. Female veterans of the OEF/OIF conflict: concordance of PTSD symptoms and substance misuse. Addict. Behav. 2010;35:655–659. doi: 10.1016/j.addbeh.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Pfeiffer PN, Ganoczy D, Ilgen M, Zivin K, Valenstein M. Comorbid anxiety as a suicide risk factor among depressed veterans. Depress. Anxiety. 2009;26:752–757. doi: 10.1002/da.20583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rand Corporation Pentagon announces plans to integrate women in combat. [October 5, 2013];The Rand Blog. 2013 Jun 18; http://www.rand.org/blog/2013/06/pentagon-announces-plans-to-integrate-women-in-combat.html.
- Rich CL, Young D, Fowler RC. San Diego suicide study: young vs. old subjects. Arch. Gen. Psychiatry. 1986;43:577–582. doi: 10.1001/archpsyc.1986.01800060071009. [DOI] [PubMed] [Google Scholar]
- Seal CH, Cohen G, Waldrop A, Cohen BE, Maguen BE. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001-2010: implications for screening diagnosis and treatment. Drug Alcohol Depend. 2011;116:93–101. doi: 10.1016/j.drugalcdep.2010.11.027. [DOI] [PubMed] [Google Scholar]
- Serras A, Saules KK, Cranford JA, Eisenberg D. Self-injury, substance use, and associated risk factors in a multi-campus probability sample of college students. Psychol. Addict. Behav. 2010;24:119–128. doi: 10.1037/a0017210. [DOI] [PubMed] [Google Scholar]
- Shen Y-C, Arkes J, Williams TV. Effects of Iraq/Afghanistan deployments on major depression and substance use disorder: analysis of active duty personnel in the US military. Am. J. Public Health. 2012;102:s80–s87. doi: 10.2105/AJPH.2011.300425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street AE, Vogt D, Dutra L. A new generation of women veterans: stressors faced by women deployed to Iraq and Afghanistan. Clin. Psych. Rev. 2009;29:685–694. doi: 10.1016/j.cpr.2009.08.007. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . The NSDUH Report: Serious Psychological Distress and Substance Use Disorder among Veterans. Office of Applied Studies; Rockville, MD: 2007. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2006 National Survey on Drug Use and Health: National Findings. Office of Applied Studies; Rockville, MD: 2007a. [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol. Bull. 2006;132:959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- US Army . Army Health Promotion, Risk Reduction, Suicide Prevention: Report. Department of the US Army; Washington D.C.: 2010. [June 3, 2012]. On-line: http://www.army.mil/article/42934/. [Google Scholar]
- Vogt DS, Pless AP, King LA, King DW. Deployment stressors, fender, and mental health outcomes among Gulf War I veterans. J. Trauma Stress. 2005;18:115–127. doi: 10.1002/jts.20018. [DOI] [PubMed] [Google Scholar]
- Weiner J, Richmond TS, Conigliaro J, Wiebe DJ. Military veteran mortality following a survived suicide attempt. BMC Public Health. 2011;11:374–383. doi: 10.1186/1471-2458-11-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 2004;76s:s11–s19. doi: 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Zivin K, Kim M, McCarthy JF, Austin KL, Hoggart KJ, Walters H, Valenstein M. Suicide mortality among individuals receiving treatment for depression in the Veterans Affairs Health System: associations with patient and treatment setting characteristics. Am. J. Public Health. 2007;97:2193–2198. doi: 10.2105/AJPH.2007.115477. [DOI] [PMC free article] [PubMed] [Google Scholar]