Abstract
Background
Enthesopathy is an evolving area for applied clinical research. MRI is the gold standard in the diagnosis of elbow joint pathology, but recent reports indicate that ultrasound imaging is more sensitive and accurate than MRI in detecting enthesopathy of the heels and knees. Too many patients are under-diagnosed and/or misdiagnosed because the early pathological changes of enthesitis in the different types of seronegative arthropathies are not detected.
Objectives
This study was undertaken to describe the ultrasound features of elbow enthesitis in patients with seronegative arthropathies.
Methods
We studied 38 diseased elbows in 38 patients with spondyloarthropathies (26 men and 12 women, mean age 32 years). All had elbow enthesopathy without typical conventional radiographic findings. Patients with histories of degenerative changes and/or local steroid injections were excluded. An HDI 3000 ATL ultrasound machine was used with a 5–12 MHz linear transducer to examine the affected elbow joints. The elbows of 10 normal healthy individuals were examined as normal controls. The patients were examined in the supine position with the elbow flexed 30°–50°. Longitudinal and transverse scans were obtained of the radiohumeral joint, the ulnahumeral joint, and the olecranon fossa. Two independent observers unaware of the clinical diagnosis read the ultrasound images and assessed the collateral ligaments, intratendinous echogenicity, tendon calcification, tendon thickness, presence of fluid, synovial proliferation, and bony changes. The reliability of the sonographic images was assessed by review of video recordings of the ultrasound examinations.
Results
Ultrasound revealed loss of the fibrillar echopattern (100 %), lack of a homogenous pattern with loss of the tightly packed echogenic dots (100 %), peritendinous edema with flaring of the tendon margins (84.2 %), irregular fusiform tendon thickening (100 %), and hyperechoic intratendinous lesions with ill-defined focal defects (18.4 %). Ultrasound also detected intratendinous calcifications of both the common extensor and common flexor tendons (52.6 %). Bony erosions were seen at the tendon insertions into the lateral epicondyles (13.15 %).
Conclusion
Ultrasonographic features of elbow enthesitis differed from those described in knee and heel enthesitis. Ultrasound clearly showed early signs of tendon calcification, tendon edema, peritendinitis, and bony entheseal erosions. However, in elbow enthesitis the early bone erosion was associated with bone marrow edema, and the common extensor tendon was diffusely thickened. Ultrasound is a reliable, reproducible bedside imaging procedure. It improves the documentation of disease activity, progression, and treatment responses in patients with spondyloarthropathies. We recommend its use for the diagnosis and post-treatment follow-up of patients with enthesitis and seronegative spondyloarthropathies.
Keywords: Ultrasound, Elbow enthesitis, Seronegative arthropathies
Riassunto
Background
Recenti report hanno dimostrato che l’esame ecografico è più sensibile e accurato di altre tecniche di imaging nel rilevare le entesopatie dei talloni e delle ginocchia.
Obiettivi
Descrivere le caratteristiche ecografiche dell’entesite del gomito in pazienti affetti da artropatie sieronegative.
Metodi
Abbiamo studiato 38 gomiti affetti di 38 pazienti con diagnosi di spondiloartropatie (26 uomini e 12 donne), di età media di 32 anni. Tutti i pazienti avevano un’entesopatia del gomito senza i tipici reperti con la radiografia tradizionale. Sono stati esaminati i gomiti di 10 individui sani come controllo normale. Tre regioni sono state esaminate con scansioni longitudinali e trasversali; l’articolazione radio-omerale, l’articolazione ulno-omerale e la fossa olecranica.
Risultati
L’esame ecografico ha rivelato la perdita dell’ecostruttura fibrillare (100%), la mancanza di una struttura omogenea con perdita dei punti ecogeni fitti (100%), l’edema peritendineo con slargamento dei margini tendinei (84,2%), l’ispessimento irregolare fusiforme del tendine (100%) e le lesioni iperecogene intratendinee con difetto focale mal definito (18,4%). Inoltre, l’ecografia rileva calcificazioni intratendinee sia del tendine estensore comune sia dei flessori comuni (52,6%). Abbiamo rilevato erosioni ossee a livello dell’inserzione dei tendini negli epicondili laterali (13,15%).
Conclusione
L’ecografia è una procedura d’imaging affidabile e riproducibile in pazienti affetti da entesite e spondiloartiti sieronegative.
Introduction
The term enthesis refers to the attachment to the bone of a tendon, muscle, ligament, or joint capsule. Histologically, this area can be divided into four identifiable zones, which blend into each other and represent the transition of the tendons at their insertion into bones. The first zone includes the actual tendon or ligament, the second and third consist of unmineralized and mineralized fibrocartilage, respectively, and the fourth comprises the bone itself [1].
Enthesopathy is an evolving area for applied clinical research. Inflammation of the enthesis is the hallmark of the seronegative arthropathies. The diagnosis of enthesitis in clinical practice is difficult, and conventional radiography is almost always negative. Too many patients are under-diagnosed and/or misdiagnosed because X-rays fail to detect the early pathological changes of enthesitis in seronegative arthropathies.
There is now accumulating evidence that ultrasound improves the clinical diagnosis of enthesitis and that it is superior to the clinical examination alone in the diagnosis and localization of joint and bursal effusion and synovitis. Recent clinical studies addressing the use of ultrasound in the evaluation of synovial inflammation and joint damage confirm that physical examination of the joint and plain X-rays are insensitive diagnostic tools in this setting [2–6]. Kamel et al. [7, 8] showed that ultrasound imaging is more sensitive and accurate than other imaging modalities in detecting definite features of enthesopathy involving the heels and knees. Thickened enthesitis, erosion, enthesophytes, and adjacent bursitis are common findings on ultrasound [9].
To our knowledge, few studies have focused on the ultrasound features of elbow enthesopathy. The objective of the present study was to describe in detail the ultrasound features of elbow enthesitis in patients with seronegative arthropathies.
Patients and methods
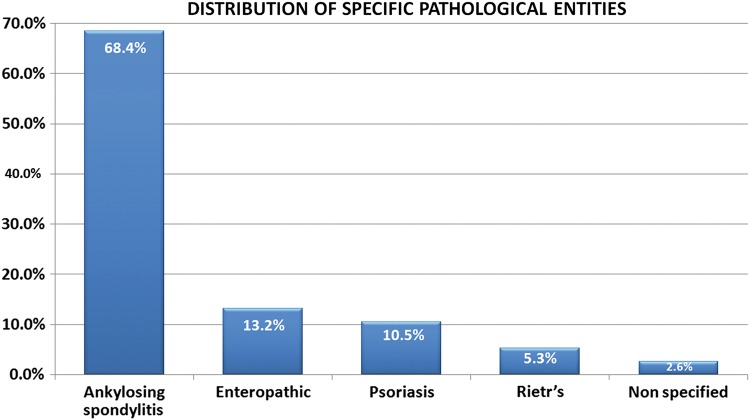
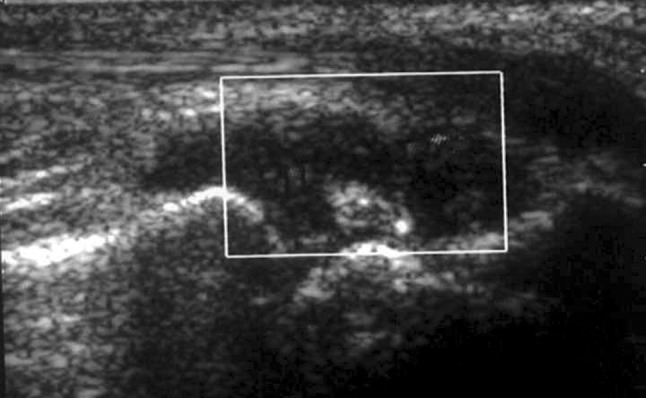
In this study, we examined the elbow joints of 38 patients (22 men and 16 women; mean age 32 years) with established diagnoses of seronegative spondyloarthropathies. All had elbow enthesopathy (Fig. 1) without typical radiographic findings. Lesions were unilateral in 26 (68.4 %) patients and bilateral in 12 (31.6 %). Patients were excluded if they had a history of degenerative changes and/or had received local steroid injections. The elbows of 10 normal healthy individuals were examined as controls.
Fig. 1.
Distribution of specific pathological entities
The entheses of the affected elbow joints were examined with an HDI 3000 ATL ultrasound machine equipped with a 5–12 MHz linear transducer. The patient was placed in the supine position with the affected elbow flexed 30–50°. In all patients, we examined the contralateral elbow for comparison purposes. Three regions were examined with longitudinal and transverse scans: the radiohumeral and ulnahumeral joints and the olecranon fossa.
Each ultrasound study was reviewed by two consultant radiologists with more than 15 years’ experience in musculoskeletal radiology. The following aspects were examined:
A: Tendons
Alterations involving the common extensor tendon or common flexor tendon, including loss of the fibrillar pattern, tendon thickening, intrasubstance tears, and intratendinous calcifications (Fig. 2).
Loss of the fibrillar pattern was diagnosed when the tendon displayed heterogeneous echogenicity.
Fusiform thickening was considered present when the thickness of the affected tendon was greater than that of the contralateral tendon.
A linear intrasubstance tear was defined as a hypoechoic band within the substance of the tendon associated with discontinuity of the tendon fibers.
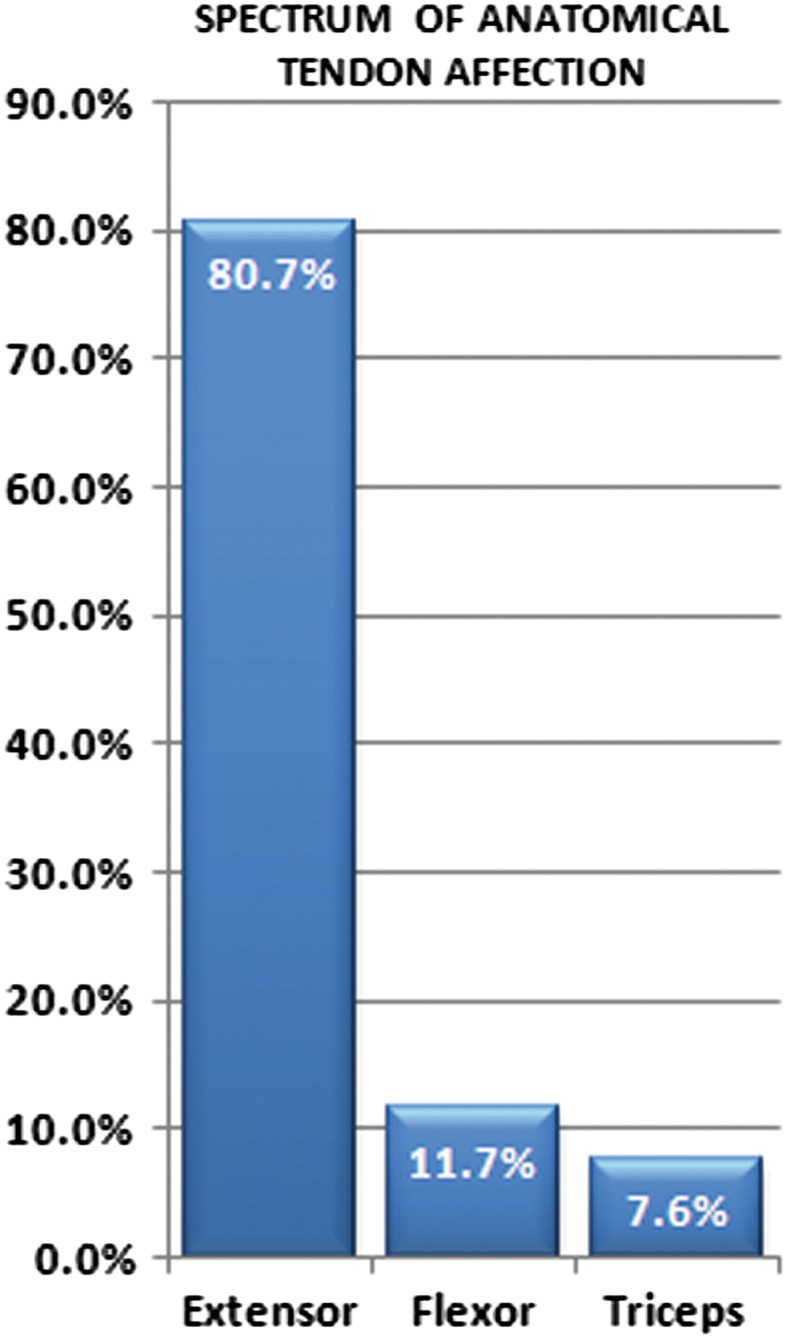
Peritendinous fluid was postulated when anechoic fluid was observed along the superficial aspect of the tendon (Fig. 3).
Calcific tendonitis was diagnosed when the tendon presented internal foci of high-density echoes with posterior shadowing.
Fig. 2.
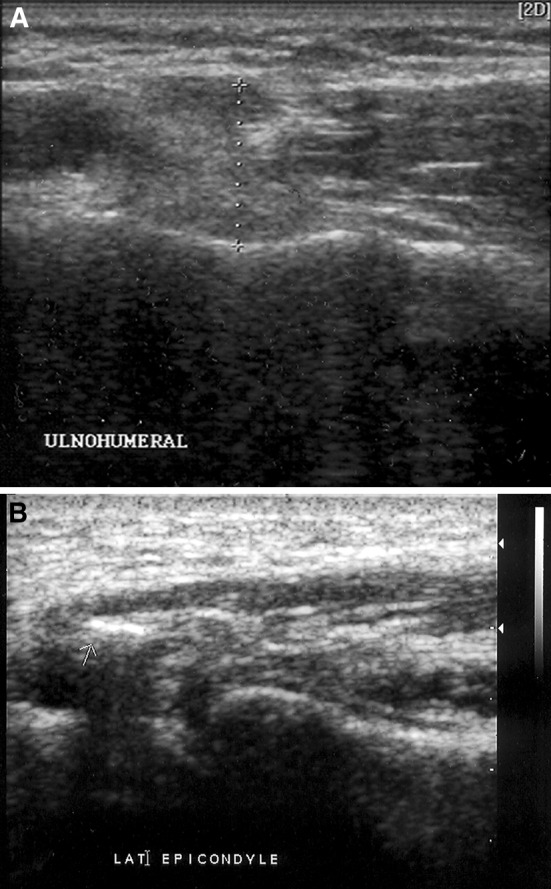
a, b Ultrasound (5–12 MHz). Coronal images of lateral epicondyles of two different patients, showing thickened common extensor tendons, loss of the fibrillar echo pattern, and calcific foci (arrows)
Fig. 3.
Ultrasound (5–12 MHz). Coronal image of the lateral epicondyle showing thickening of the common extensor tendon and a hypoechoic area representing a peritendinous fluid collection
B: Ligaments
Both the medial and lateral collateral ligaments were scanned for laxity and/or thickening.
C: Bones
Both the medial and lateral epicondyles of the humerus were examined for erosions, periosteal reaction, and the presence of enthesophytes at the tendon insertion site (Fig. 4).
Fig. 4.

Ultrasound (5–12 MHz). Coronal image of the lateral epicondyle showing focal cortical erosion (arrow). The common extensor tendon also presents fusiform thickening and loss of the fibrillar echo pattern
D: Bursa
The scan included examination of the olecranon fossa for evidence of bursitis.
Each of the two consultant radiologists reviewed the scan images separately and with no knowledge of the clinical diagnosis. To minimize the interobserver errors, we recorded only the concordant judgments. When discordant judgments emerged, the findings were sent to a third radiologist, who reviewed the images using the cine loop. The findings confirmed by the third observer were considered positive [10, 11].
The contralateral elbow was scanned in all patients and controls to obtain internal reference data for measurements of tendon and ligament thickness and to rule out subclinical enthesitis in the apparently unaffected elbow.
Within 1 week of the ultrasound examination, all patients underwent MRI examination of the affected elbow, with axial, coronal, and sagittal T1-weighted, T2-weighted, and STIR sequences [5, 6].
Imaging data were tabulated and subjected to statistical analysis using the Kappa test. Tests of significance were applied to estimate the accuracy of the ultrasound diagnosis, using MRI as the gold standard.
All elbows were treated conservatively with oral anti-inflammatory drugs, physiotherapy, and/or local injection of corticosteroids. No biopsies or surgical interventions were performed.
All patients had follow-up ultrasound or MRI examinations after completion of the treatment protocol. All findings related to the acute inflammatory reaction subsided completely.
Results
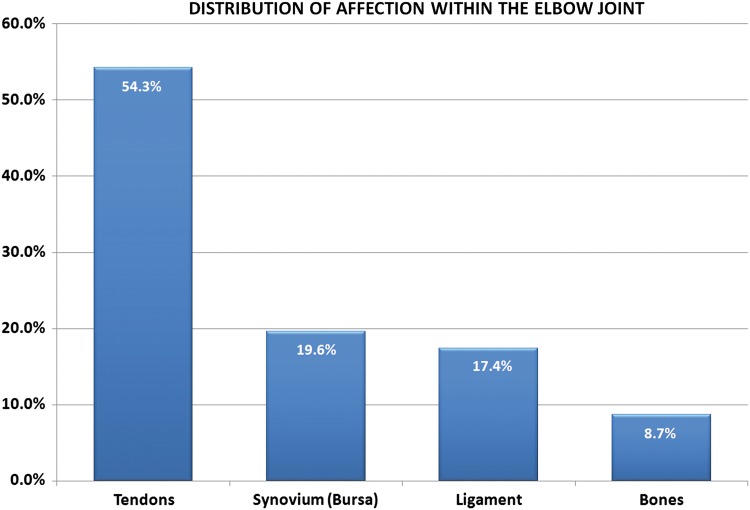
The 38 elbows we examined presented a broad spectrum of changes, which involved the tendons, ligaments, bursa, and cortical bone. Four of the patients were found to have bilateral involvement (Fig. 5).
Fig. 5.
Distribution of affected structures within the elbow joint
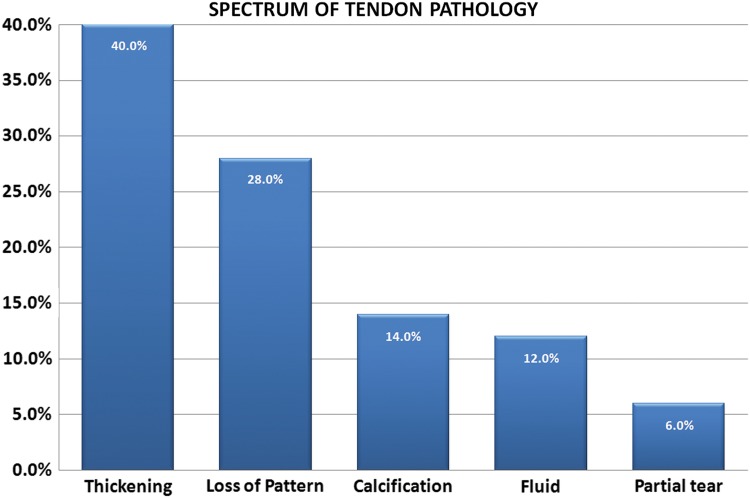
Tendon pathology Tendon involvement was by far the most common finding encountered on sonography: 25 (65.8 %) of the 38 elbows showed positive findings. The most common alterations were irregular fusiform thickening of the tendons (20/38 elbows; 52.8 %) and loss of the fibrillar pattern, which was seen in 14 (36.8 %) elbows. Calcific tendonitis was detected in seven (18.7 %.) elbows, peritendinous fluid was seen in six (15.7 %), and partial tears were found in three (7.8 %) elbows. Complete tendon tears were not seen in any of our patients (Fig. 6).
Fig. 6.
Spectrum of tendon pathologies
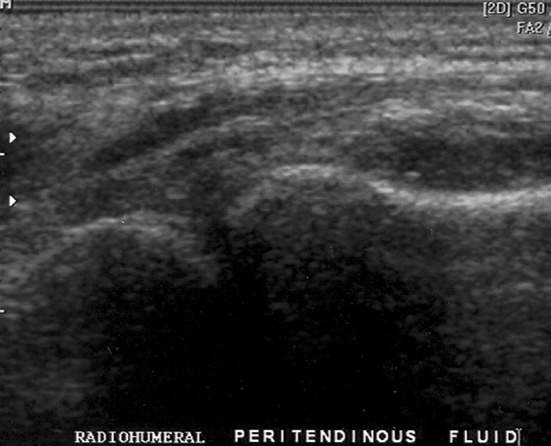
In terms of distribution, the common extensor tendon was by the far the most common tendon affected (21/38 elbows; 55.3 %), followed by the triceps tendon were affected in three (12 %) patients. Lesions of the common flexor tendon were encountered in two (8 %) patients. In four patients, involvement of more than one tendon group was observed (Fig. 7).
Fig. 7.
Tendons affected
Changes involving the medial and lateral collateral ligaments (thickening, laxity, or both) were identified in eight (21 %) elbows. Bone involvement (erosion or spur formation) was detected in four (10.5 %) elbows. Synovial thickening, with or without bursitis, was seen in nine (23.6 %) elbows, while olecranon bursitis was present in eight (21 %).
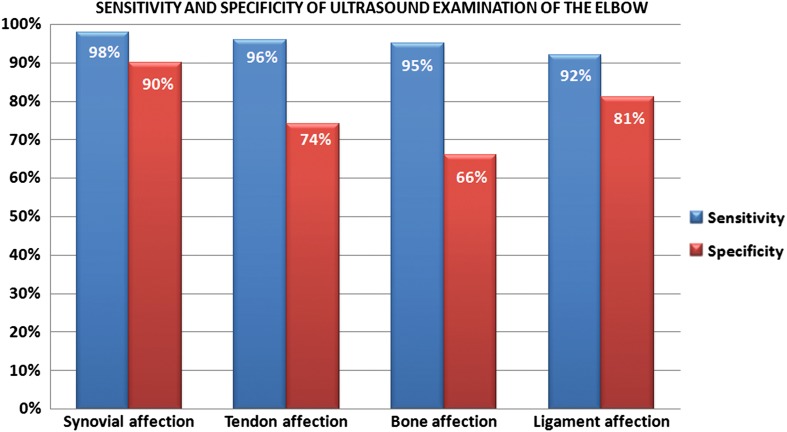
MRI was performed in all cases (Fig. 8). Ultrasound showed equivalent sensitivity to MRI in detecting all the above changes, and it was more sensitive than MRI in detecting calcific tendinitis and cortical bone erosion.
Fig. 8.

MRI coronal (a) and axial (b) images of the elbow using fat suppression sequence. The ill-defined area of signal hyperintensity in the medullary bone of the lateral epicondyle reflects bone edema (osteitis)
Discussion
Ultrasound examination of the elbow has many potential advantages, including its ability to produce clear images of the ultra-fine pathological changes involving the bones, bursa, tendons, ligaments, synovial tissue, and articular cartilage with high sensitivity and specificity (Fig. 9).
Fig. 9.
Sensitivity and specificity of ultrasound examination of the elbow
Many publications have addressed the advantages of ultrasound imaging over X-ray in the evaluation of diseases involving the elbow joint, such as rheumatoid synovial inflammation (Fig. 10) [4, 12].
Fig. 10.
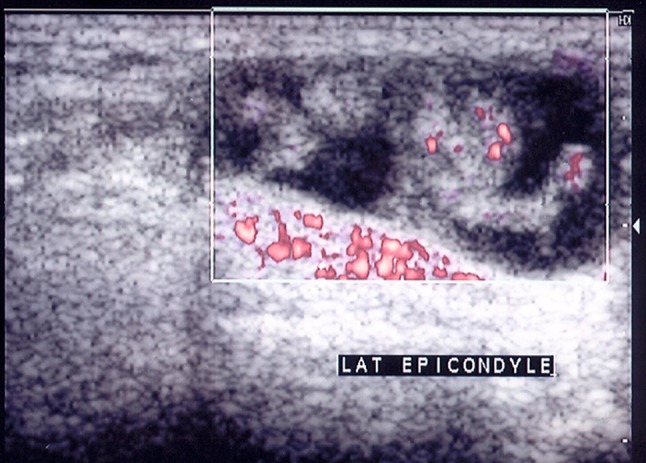
Power Doppler ultrasound image (5–12 mHz) of the olecranon fossa showing lobulated synovial thickening surrounded by hypoechoic fluid. The active Doppler signal confirms the presence of active inflammation
Clinical examination of the joint and plain X-rays are relatively insensitive tools in the setting of chronic disease of the elbow joint. In patients with seronegative arthropathy, the main targets of the inflammatory process are the synovial lining of the joint, the tendons and ligaments, and the subjacent bones. We have shown that ultrasound can detect pathological involvement of these structures with high accuracy [13].
The common extensor tendon was affected more frequently than other tendon groups in the elbow. This finding can be explained by the common extensor tendon’s natural exposure to frequent micro-trauma. The spectrum of findings within the tendon in seronegative arthropathy included thickening, altered echogenicity, peritendinous, flaring, partial tears, and calcification (Fig. 11). This wide variety reflects different phases of disease involvement, i.e., initial, chronic, healing, and irreversible. Interestingly, the incidence of tendon calcification was significantly higher in the elbow than in heels and knees [7, 8, 14].
Fig. 11.
Power Doppler ultrasound image (5–12 mHz) of the olecranon fossa showing a distended olecranon bursa. Hypoechoic fluid with focal synovial thickening and focal calcification are also seen. No active flow is noted on the Doppler image
This finding is consistent with those of Kamel et al. [10, 11], who reported a higher incidence of calcific tendinopathy around the elbow than in the knee.
Our findings show that involvement of the elbow joint in seronegative arthropathy has a slightly different pattern of manifestations compared with that of other conditions. Bone erosions were found to occur early in the elbow region of our patients, whereas in tennis elbow, bone erosion is rarely encountered. This might be a differentiating feature since seronegative arthropathy displays special predilections for the bony attachment, as in sacroiliac joint involvement [4, 15–17].
Ultrasound depicted early bone erosion-like changes in patients with enthesitis as decortication defects, a few millimeters in length, at the points of synovial attachment. These lesions were found to be associated with bone marrow edema on the MRI examination. Therefore, the presence of bone erosion on ultrasound can be considered indirect evidence of marrow edema.
Other investigators [18] observed a striking association between the presence of bone erosion and increased intra-articular blood flow in the metacarpophalangeal joint on color Doppler flow imaging. The presence of marrow edema on MRI is an indicator of active bone resorption. Ejbjerg et al. [19] concluded that the presence of bone marrow edema is a reflection of a true pathologic event. However, bone marrow edema is not disease-specific: indeed, it is a well-known finding in osteoarthritis, post-traumatic conditions, and rheumatoid arthritis (RA). Bone erosion and bone marrow edema are very specific markers for distinguishing arthritic joints from normal joints.
Signs of bone marrow edema are rarely found in healthy controls. This sign may thus prove to be a specific tool for distinguishing between arthritic disease and other conditions. In RA, bone marrow edema is a frequent finding, and in patients with early disease it is associated with an increased risk (up to 6.4-fold) of developing erosive changes [20]. It is also a well-known finding in osteoarthritis and trauma. Musculoskeletal ultrasound can detect up to seven times more erosions than plain film radiography in early RA [4].
Ultrasound was found to be more sensitive than MRI in detecting early changes of enthesopathy of the heels and knees. We have shown that ultrasound was more sensitive than MRI in detecting early changes of enthesopathy of the heels and knees [5, 6]. The present study describes sensitive ultrasound features of elbow enthesitis. The finding showed a peculiar pattern of enthesitis involving the elbow joint. Bone erosions were found to occur early in the elbow [7, 8].
Intratendinous calcifications were also more prevalent in the elbow than in the heels and knees. Furthermore, the increased thickness of the common extensor tendon was uniform with full-length involvement of the enthesitic area. Edema was a frequent finding in patients with rheumatoid arthritis and was associated with an increased risk (up to 6.4-fold) of developing erosive changes in patients with early rheumatoid arthritis. Sonographic features of rheumatoid epicondylitis include outward bowing of the common flexor tendon, presence of hypoechoic fluid adjacent to the common tendon, tendon thickening, decreased echogenicity, and common tendons with ill-defined margins. These features are non-specific and were reported in several studies [21].
Conclusions
Ultrasound images clearly documented early signs of tendon calcification, tendon edema, peritendinitis, and bony entheseal erosions. In elbow enthesitis, early bone erosions are associated with bone marrow edema and diffuse thickening of the common extensor tendon. Ultrasound is a reliable, reproducible bedside imaging procedure. In patients with spondyloarthropathies, it improves the documentation of disease activity, progression, and response to treatment. We recommend performing ultrasound examination for the diagnosis and post-treatment follow-up of patients with enthesitis and seronegative spondyloarthropathies. The fundamental ultrasound signs that could be identified in these patients were enthesopathy, tendinitis, peritendinitis, bursitis, and intramuscular hematoma.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 [5].
References
- 1.Danda D, Shyam Kumar NK, Cherian R, et al. Enthesopathy: clinical recognition and significance. Natl Med J India. 2001;14:90. [PubMed] [Google Scholar]
- 2.Kane D, Grassi W, Sturrock R, et al. Musculoskeletal Ultrasound- a state of the art review in rheumatology. Part 2: clinical indications for musculoskeletal ultrasound in rheumatology. Rheumatology. 2004;43:829. doi: 10.1093/rheumatology/keh215. [DOI] [PubMed] [Google Scholar]
- 3.Grassi W, Filippucci E, Farina A, et al. Ultrasonography in the evaluation of bone erosions. Ann Rheum Dis. 2001;60:98. doi: 10.1136/ard.60.2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wakefield RJ, Gibbon WW, Pease C, et al. The value of Sonography in the detection of bone erosions in patients with Rheumatoid arthritis: a comparison with conventional radiography. Arthritis Rheum. 2000;43:2762. doi: 10.1002/1529-0131(200012)43:12<2762::AID-ANR16>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 5.Kamel M, Eid H, Mansour R. Ultrasound detection of heel enthesitis: a comparison with magnetic resonance imaging. J Rheumatol. 2003;30:774. [PubMed] [Google Scholar]
- 6.Kamel M, Eid H, Mansour R. Ultrasound detection of knee patellar enthesitis: a comparison with magnetic resonance imaging. Ann Rheum Dis. 2004;63:213. doi: 10.1136/ard.2003.010314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kamel M, Moghazy K. Ultrasonographic detection of enthesitis: a comparison with MRI. Arthritis Rheum. 2001;44(suppl 9):95. [Google Scholar]
- 8.Kamel M, Mansour R, Eid H. Ultrasound detection of patellar enthesitis: a comparison with MRI. Arthritis Rheum. 2002;46(Suppl 9):S104. doi: 10.1136/ard.2003.010314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.D’Agostino MA, Said-Nahal R, Hacquard-Bouder C, et al. Assessment of peripheral enthesitis in the spondylarthropathies by ultrasonography combined with power Doppler: a cross-sectional study. Arthritis Rheum. 2003;48:523. doi: 10.1002/art.10812. [DOI] [PubMed] [Google Scholar]
- 10.Kamel M, Kotob H. High frequency ultrasonogrphic findings in planter fascitis and assessment of local steroid injection. J Rheumatol. 2000;27:2139. [PubMed] [Google Scholar]
- 11.Kamel M, Kotob H. Ultrasonographic assessment of local steroid injection in Tietze’s syndrome. Br J Rheumatol. 1997;36:547. doi: 10.1093/rheumatology/36.5.547. [DOI] [PubMed] [Google Scholar]
- 12.Grassi W, Filippucci E, Farina A, et al. Ultrasonography in the evaluation of bone erosions. Ann Rheum Dis. 2001;60:98. doi: 10.1136/ard.60.2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.du Toit C, Stieler M, Saunders R, et al. Diagnostic accuracy of power Doppler ultrasound in patients with chronic tennis elbow. Br J Sports Med. 2008;42:872. doi: 10.1136/bjsm.2007.043901. [DOI] [PubMed] [Google Scholar]
- 14.Coombes BK, Bisset L, Vicenzino B. A new integrative model of lateral epicondylalgia. Br J Sports Med. 2009;43:252. doi: 10.1136/bjsm.2008.052738. [DOI] [PubMed] [Google Scholar]
- 15.Benjamin M, McGonagle D. The anatomical basis for disease localisation in seronegative spondyloarthropathy at entheses and related sites. J Anat. 2001;199:503. doi: 10.1046/j.1469-7580.2001.19950503.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McGonagle D, Wakefield RJ, Tan AL, et al. Distinct topography of erosion and new bone formation in achilles tendon enthesitis: implications for understanding the link between inflammation and bone formation in spondylarthritis. Arthritis Rheum. 2008;58:2694. doi: 10.1002/art.23755. [DOI] [PubMed] [Google Scholar]
- 17.Benjamin M, Toumi H, Suzuki D, et al. Microdamage and altered vascularity at the enthesis-bone interface provides an anatomic explanation for bone involvement in the HLA-B27-associated spondylarthritides and allied disorders. Arthritis Rheum. 2007;56:4. doi: 10.1002/art.22291. [DOI] [PubMed] [Google Scholar]
- 18.Taylor PC, Steuer A, Gruber J, et al. Comparison of ultrasonographic assessment of synovitis and joint vascularity with radiographic evaluation in a randomized placebo-controlled study of infliximab therapy in early rheumatoid arthritis. Arthritis Rheum. 2004;50:1107. doi: 10.1002/art.20123. [DOI] [PubMed] [Google Scholar]
- 19.Ejbjerg B, Narvestad E, Rostrup E, et al. Magnetic resonance imaging of wrist and finger joints in healthy subjects, occasionally shows changes resembling erosions and synovitis as seen in rheumatoid Arthritis. Arthritis Rheum. 2004;50:1097. doi: 10.1002/art.20135. [DOI] [PubMed] [Google Scholar]
- 20.McQueen FM, Stewart N, Crabbe J, et al. MRI of the wrist in early rheumatoid arthritis reveals progression of erosions despite clinical improvement. Ann Rheum Dis. 1999;58:156. doi: 10.1136/ard.58.3.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller TT, Shapiro MA, Schultz E, et al. Comparison of Sonography and MRI for Diagnosing Epicondylitis. J Clin Ultrasound. 2002;30:193. doi: 10.1002/jcu.10063. [DOI] [PubMed] [Google Scholar]