Abstract
Purulent pericarditis is rarely encountered in the antibiotherapy era, mainly in immunosupressed patients, after cardiac operations, in septicemia. Diagnosis of purulent pericarditis is based upon the analysis of pericardial drainage, obtained through pericardiocentesis or preferably, through a surgical approach. The reported case has following peculiarities: clinical signs of false acute surgical abdomen; altered clinical and biological response to infection; Optimal treatment is early, efficient pericardial drainage, with low risk of tissue contamination and of pericardial constriction; Surgical subxyphoid pericardial drainage is prefered in patients with affected general status. Antero-(lateral) thoracic approach with associated anterior pericardiectomy ensures an efficient pericardial drainage and prevents pericardial constriction, with low risks for pleural contamination.
Keywords: purulent pericardial effusion, cardiac tamponade, diagnosis, treatment
Introduction
Pericardial effusions are rather frequently encountered syndromes in the medical practice. The etiology involved in the genesis of pericardial effusion syndrome (PEs) is extremely varied. Thus, doctors of different specialties may deal with this pathology which, apart from the cardiac decompression therapy, requires a therapy of the main affection generating PEs. The etiological variety of PEs explains the difference in medical prognosis for the affected patients.
By using traditional medical treatment, the internist or cardiologist may succeed in regressing the pericardial effusions, however, very often, it is necessary to use an invasive medical technique either for diagnosis (obtain pericardial fluid or pericardial tissue fragments for additional lab tests) or for therapeutic purposes (pericardial drainage for the decompression of the heart). The guidelines for using these invasive strategies, as well as for the lab tests on the intraprocedurally collected specimen, have been partially established by the European Society of Cardiology Guidelines, published in 2004.
There are many controversial aspects referring to the PEs diagnosis and therapy, as there are not so far randomized evidence-based prospective studies to state clear recommendations for different diagnostic and therapeutic methods.
Moreover, new techniques have appeared (percutaneous balloon pericardiostomy, percutaneous pericardiostomy), but they are used in very few medical centers in the world. They require special medical equipment and a certain learning curve and their results are difficult to interpret and to reproduce „d’ emblee”.
Very often a pericardiocenthesis is performed by the cardiologist for diagnostic and/or therapeutic purposes. And very frequently, the cardiovascular and thoracic surgeons are consulted in order to decide upon the necessity, the moment of the operation, the surgical procedure of pericardial drainage and contingently upon a different therapy (resection of a lung tumor, usually for bioptic purposes, pericardiectomy, etc).
The surgeon finds himself facing many controversies and often having a patient with an associated frame of significant comorbidities. Nowadays, there are variable results in the use of various techniques of pericardial drainage (mini-invasive or invasive ones) which may be associated with local intrapericardial treatment (sclerotherapy, chemotherapy), with pericardial biopsy guided by pericardioscopy, and rarely, with the performance of a pericardiectomy (total or partial) in order to avoid the PES recurrence or a possible evolution towards constrictive pericardial syndrome.
Case Report
34 year-old patient, D.C, urgently admitted in the Clinic of Cardiology-Craiova, in 2008
Reasons for hospitalization
False surgical acute abdominal, dyspnea at rest, tachypnea, low fever and asthenia.
History
A patient undergoing oncological treatment for the Hodgkin disease, diagnosed a month before admission, was urgently transferred from Craiova Hematology Clinic for progressive epigastric and retrosternal pain in last few days, progressive dyspnea in the last week, presently with dyspnea at rest and tachypnea, accompanied by asthenia for the last 2 months. The patient had had fever (38.9° C) five days before (cultures from blood and urine were collected and treatment with broad-spectrum antibiotics initiated until a definitive antibiogram result). Yet, the culture tests were negative.
Matherial and Method
Nineteen million people have died of AIDS since the discovery of HIV in the 1980s. In 1999 alone, 5.4 million people were newly infected with HIV (ref. 1 and http://www.unaids.org/epidemicupdate/report/Epireport.html). (For brevity, HIV-1 is referred to as HIV in this paper.) Sub-Saharan Africa has been hardest hit, with more than 20% of the general population HIV-positive in some countries (2, 3). In comparison, heterosexual epidemics in developed, market-economy countries have not reached such severe levels. Factors contributing to the severity of the epidemic in economically developing countries abound, including economic, health, and social differences such as high levels of sexually transmitted diseases and a lack of prevention programs. However, the staggering rate at which the epidemic has spread in sub-Saharan Africa has not been adequately explained. The rate and severity of this epidemic also could indicate a greater underlying susceptibility to HIV attributable not only to sexually transmitted disease, economics, etc., but also to other more ubiquitous factors such as host genetics (4, 5).
Clinical examination: skin and mucosal pallor, normal weight, low fever (37.9° C), reduced adipose tissue, right latero-cervical and axillary poliadenopathy; respiratory system without clinical modifications; cardiovascular/circulatory system - tachycardic heart sounds, heart rate (HR) = 110 beats/minute, grade 3 jugular turgescence, TA: 85/60 mmHg; digestive system – epigastrial and right hypochondrial pain on palpation with muscle defense, grade 1 splenomegaly, normal liver on palpation; painless flanks; neurologically - without modifications on objective examination.
The peripheral vascular access has been obtained via two veins and usual blood samples were collected for lab tests. The oxygen therapy was implemented (4l/min O2). The hemodynamic (BP, pulse, ECG) and respiratory (SO2 established by skin pulse oxymetry) monitoring started. The broad spectrum antibiotics scheme was modified.
Paraclinical tests:
The biochemical examination: ESR=52 mm/h, Fibrinogen=400 mg/dl, CRP=12.5 mg.l, Hb=11.4 g/dl, thrombocytes= 190000/mm³, leucocytes= 15.200/ mm³, unsegmented neutrophils=2%, segmented neutrophils= 75%, lymphocytes= 17%, monocytes= 4%, eosinophils= 1%, Na=127.3 mmol/l, K= 3.35 mmol/l, Cl= 91 mmol/l, Ca= 0.709 mmol/l. The rest of the biochemical tests are normal.
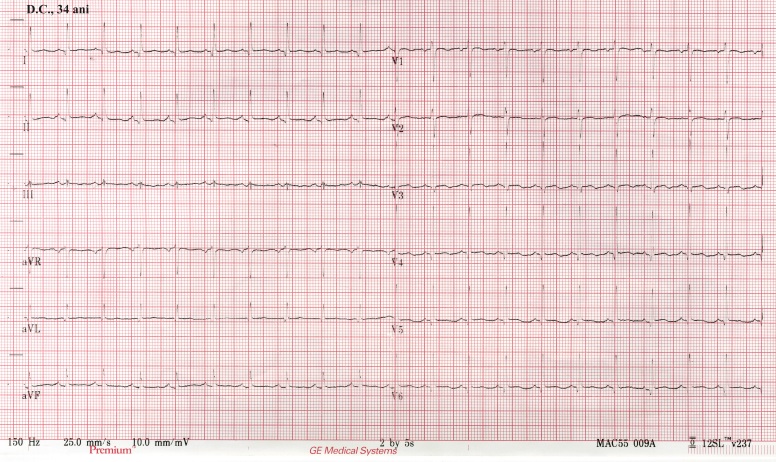
ECG: electric alternance of the QRS complex, synus tachycardia, +30° QRS axis, without T wave alternance (Fig. 1).
Figure 1.
ECG 12 derivations, early re-polarization with electrical alternance, diffuse low voltage.
Echocardiography: pericardial fluid 33 mm posterior to the LV and 33 mm anterior to the RV; VCI=30 mm. Normal LV function. Total collapse of the RA and RV (Fig. 2)
Figure 2.
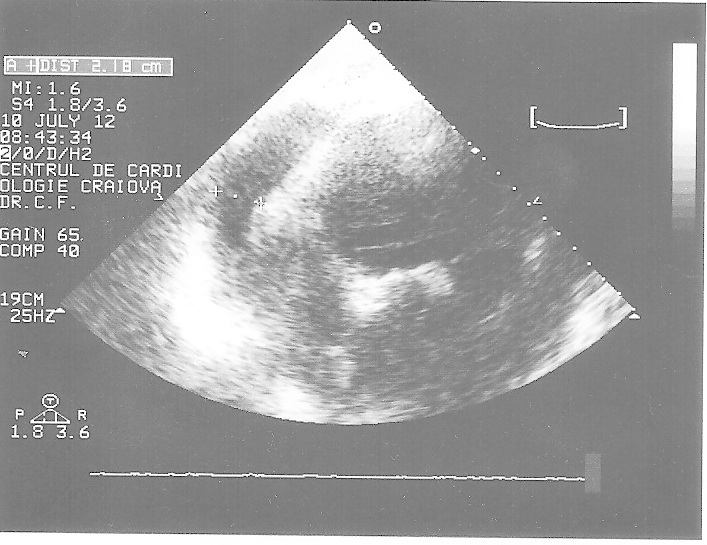
Echocardiography, 4 chambers apical view, early depolarization, large PEs with diastolic collapse of the right cavities.
Stage diagnosis: pericardial effusion with cardiac tamponade. Hodgkin disease under chemotherapy.
An emergency subxyfoid pericardial puncture was performed, under asepsia and local anesthesia with xylocaine: 50 ml of frank purulent fluid could be extracted. The patient respiratory and hemodynamic status is relatively stable under oxygen therapy and volume replacement solutions (Ringer-lactate) at an average flow without inotropic or vasoactive support.
Diagnosis: purulent pericarditis with cardiac tamponade, Hodgkin disease
Emergency thoracic surgical consultation was asked for.
A pericardial drainage was decided upon and subsequently performed through a left anterior thoracotomy. On entering the pleural cavity, the intense erythematous and under tension pericardium could be observed. A minimum incision is made in the pericardium anterior to the phrenic nerve and the aspirator is introduced. Approximately 100 ml frank purulent fluid is aspirated, and then fluid is collected for the bacteriological, cytological and biochemical testing. A 7x7 cm pleuro-pericardial window is created and the pericardium section is sent for the histopathological examination. The rest of the purulent fluid from the pericardial cavity is aspirated and the digital lysis of the false membrane is performed. The pericardial and the pleural cavity are washed with physiological saline solution at body temperature. In the end, gentamicin is administered intrapericardially and intrapleurally. 2 drainage tubes are inserted into the pericardial and pleural cavities respectively, and exteriorized separately though a counter-incision in the inferior intercostal space and connected to low aspiration. Approximately 600 ml frank purulent pericardial fluid has been drained.
The biochemical examination of the pericardial fluid shows: proteins =5.2 g/dl, a positive Rivalta reaction, glucose= 80 mg/dl.
The cytological examination of the pericardial fluid: frequent polymorphonuclear leucocytes, rare lymphocytes and rare erythrocytes.
The bacteriological examination of the pericardial fluid for TB and unspecified germs: no germs developed.
After surgery, the patient has been treated in the intensive care unit for 4 days. General therapeutic measures have been applied: hydroelectrolytic balance, analgesics, general antibiotherapy- Oxacillin IV 2g q6h, Ceftriaxone IV 2g q12h, Gentamicin IV 80 mg q8h.
The pericardial cavity has been continually irrigated with physiological saline solution and gentamicin, intrapleurally and intrapericardially, 3-4 times a day, for the first 3 days. Removal of drainage took place on the 7th postoperative day, with subsequent immediate radiological control and another control prior to discharge.
The clinical postoperative evolution was favorable, with normal echocardiographic aspect. The patient was discharged 2 weeks after the operation, with signs of normal wound healing, in order to continue the specific treatment of the main disease.
Discussion
The purulent pericarditis is rare nowadays due to the development of antibiotherapy; it may appear in patients whose immune system is compromised (leukemia, lymphoma, chronic liver diseases, chronic kidney diseases, diabetes, alcoholism, during the imunosupresive/cytostatic treatment), after cardiothoracic surgery, in patients with infective endocarditis or septicemia.
The presented case has the following characteristics:
• purulent pericarditis in a patient having Hodgkin disease under treatment with cytostatic medication. Patients with Hodgkin disease have a lower cell immunity characterized by anergy to the skin tests [1] and reverse ratio CD4/CD8;
• presence of abdominal epigastric pain (false acute surgical abdomen) in the acute hypodiastolic syndrome. The abdominal pain in the pericardial effusion with cardiac tamponade appears in 20-40 % of the cases [1], being determined by the distention of the liver capsule during the hypodiastolic syndrome with liver stasis;
• clinical and biological response to infection and inflammation is altered. The cytokines and their antagonists are involved in the response to the infection and inflammation; the antagonists of the inter-leukin 1 receptors and the TNF alpha-receptors are very high for old people or patients with immunodeficiency. These modifications inhibit the fever reaction and the elevation in the non-specific inflammatory markers [2].
For almost 50-60% of the cases having purulent pericarditis, the cultures remain positive, while for the rest of the cases they are negative [3]. For the case presented above, the cultures were not positive, possibly because of the antibiotic treatment the patient had received prior to the bacteriological tests.
The evolution of the presented case was favorable due to the early diagnosis and the implementation of specific therapy. The purulent pericarditis diagnosed too late or without specific treatment evolves to toxico-septic complications and death [3].
In the specialty literature, the adequate choice of pericardial drainage methods for purulent pericarditis is controversial. Several methods of managing the pericardial drainage are described:
• subxyphoid pericardiocentesis by placing a drainage tube intrapericardially and irrigating it periodically with physiological saline solution and, if needed, with antibiotics or fibrinolytic drugs. Pericardiocentesis is a minimally-invasive procedure, yet, sometimes it cannot evacuate the thick purulent liquid from a pericardial cavity, false membranes often not allowing an efficient drainage. There have been reported about exceptional cases of improved pericardial drainage and implicitly of recovery by leaving a catheter in the pericardial cavity and administering local fibrinolytic treatment [4]. There are raports of efficient drainage in purulent pericarditis with the new method of percutaneous balloon pericardiostomy, but there is little experience with it [5];
• the classic surgical subxiphoid pericardial drainage is preferred, as the surgical trauma is minimal and it avoids the risk of sternal or pleural cavity contamination, risks associated with the median sternotomy and thoracotomy. The disadvantage is that it cannot evacuate posterior fluid loculations and does not allow an extended pericardiectomy, reasons why some authors recommend it only for patients in critical condition, to whom a thoracotomy or a median sternotomy would be too aggressive [6]. Concomitant use of intraoperative pericardioscopy would probably outset this disadvantage [7];
• the pleuro-pericardial window by anterior thoracotomy or VATS is an efficient pericardial drainage method. However, there is the risk of another body cavity contamination. There are authors who mention relative contraindications [8] but there are other authors who report satisfactory results [9];
• the external pericardial window by median sternotomy. It has the advantage of an excellent pericardial exposure, facilitating the lysis of adhesions and the evacuation of loculated purulent fluid. Nevertheless, there is the risk of sternal contamination which may cause high post-surgery morbidity;
• in cases with a local tendency to fibrosis and high fibrin content in the pericardial fluid, the pericardiectomy is sometimes recommended in order to avoid the evolution towards a pericardial constriction. Performing the pericardiectomy and the pericardial drainage simultaneously is controversial. It implies an antero-lateral thoracic approach (thoracoscopic video-assisted also possible) or though a median sternotomy [7,9,10]. If both procedures are performed simultaneously, they associate the risk of pleural or sternal contamination (more fearful), as well as the risk of a more aggressive intervention (longer operative time and a greater risk of bleeding).
In the presented case, it was decided upon a pericardial drainage by left anterior thoracotomy with simultaneous partial anterior pericardiectomy to avoid the risk of an evolution towards a pericardial constriction and to be able to perform an efficient “under view”, open drainage, with the lysis of the pericardial adhesions. A month after surgery, the patient was received in the ambulatory: no recurrence of empyema, sound wound healing, good general status.
The surgery was performed under general anesthesia with selective bronchial intubation. There was the risk of a cardiovascular decompensation at anesthesia induction, but the patient remained hemodynamically stable, using only the volume replacement therapy. The following drugs should be avoided in the pericardial effusion with cardiac tamponade: vasodilators, drugs decreasing the heart rate and drugs decreasing plasma volume (furosemide). The positive-pressure mechanical ventilation and the positive PEEP is recommended to be performed cautiously, as, by increasing the intrathoracic pressure, the preload is decreased and hypotension may supervene, with shock and death. The positive inotropic agents are used for treating the hypotension installed before or after pericardial drainage together with drugs that restore the plasma volume.
References
- 1.Fauci Anthony S., Braunwald Eugene, Kasper Dennis L., Hauser Stephen L., Longo Dan L., Jameson J. Larry, Loscalzo Joseph, et al. Harrison's Principles of Internal Medicine. 17. New York City, U.S.: Mcgraw-Hill Publ.Comp.; 2008. pp. 1073–1078. [Google Scholar]
- 2.Catania H. Takayasu arteritis. Medicina Internă. 2009;48:1073–1078. [Google Scholar]
- 3.Lorell BH. Pericardial diseases. In: Braunwald E, editor. Heart Disease: A Textbook of Cardiovascular Medicine. 5. Philadelphia, Pa: WB Saunders; 1997. pp. 1478–1534. [Google Scholar]
- 4.Ustünsoy H, Celkan MA, Sivrikoz MC, Kazaz H, Kilinç M. Intrapericardial fibrinolytic therapy in purulent pericarditis. Eur J Cardiothorac Surg. 2002;22(3):373–376. doi: 10.1016/s1010-7940(02)00258-0. [DOI] [PubMed] [Google Scholar]
- 5.Aqel R, Mehta D, Zoghbi GJ. Percutaneous balloon pericardiotomy for the treatment of infected pericardial effusion with tamponade. J Invasive Cardiol. 2006;18(7):E194–E197. [PubMed] [Google Scholar]
- 6.Miller JI, Mansour KA, Hatcher CR Jr. Pericardiectomy: current indications, concepts, and results in a university center. Ann Thorac Surg. 1982;34(1):40–45. doi: 10.1016/s0003-4975(10)60850-8. [DOI] [PubMed] [Google Scholar]
- 7.B Maisch. Interventional Pericardiology. Berlin Heidelberg: Springer; 2011. pp. 111–121. [Google Scholar]
- 8.Sellke Frank., editor. Sellke: Sabiston and Spencer's Surgery of the Chest, 8th ed. Philadelphia: Saunders, an imprint of Elsevier Inc.; 1997. [Google Scholar]
- 9.Tan EC, Rieu PN, Nijveld A, Backx AP, Meis JF, Severijnen RS. Pericarditis as complication of appendicitis. Ann Thorac Surg. 2004;78(3):1086–1088. doi: 10.1016/S0003-4975(03)01432-2. [DOI] [PubMed] [Google Scholar]
- 10.DeValeria PA, Baumgartner WA, Casale AS, Greene PS, Cameron DE, Gardner TJ, Gott VL, Watkins L Jr, Reitz BA. Current indications, risks, and outcome after pericardiectomy. Ann Thorac Surg. . 1991;52(2):219–224. doi: 10.1016/0003-4975(91)91339-w. [DOI] [PubMed] [Google Scholar]