Abstract
Introduction: Real time-sonoelastography (RTE) is a new developed technique that reveals the physical properties of the tissue by characterizing the difference in hardness between diseased tissue and surrounding tissue. Elasticity measurements have been already reported to be useful for the diagnosis and differentiation of many tumors: breast lesions, prostate cancer, lymph nodes and pancreatic masses but there are only few studies for the focal liver lesions. The aim of the study was to analyze whether computer enhanced dynamic analysis of elastography images is able to better characterize and differentiate benign and malignant liver lesions. Material and methods: The study group included, in total thirty nine liver tumors. RTE was performed by EUS or transabdominal ultrasound. ROC analysis for the mean hue obtained through histogram analysis of the region of interest (liver lesion) after averaging individual pixels over a 10-second elastography movies was used to assess the color information inside the region of interest and to consequently differentiate benign and malignant liver lesions. Based on a cutoff of 170 for the mean hue histogram values recorded on the region of interest, the sensitivity, specificity, and accuracy of differentiation of benign and malignant masses were 92.5%, 88.8%, and 88.6%, respectively. The positive and negative predictive values were 86.7% and 92.3%, respectively. In conclusion, real time sonoelastography is a promising technique that might improve the characterization and differentiation between benign and malignant focal liver lesions visualized during transabdominal or endoscopic ultrasound.
Keywords: real-time sonoelastography, focal liver lesions, hepatocellular carcinoma
Introduction
Text Real time sonoelastography (RTE) is a new sonographic/ imaging method used for the appreciation of the physical characteristics of the tissues. The method differentiates between the hardness of the diseased tissue and of the surrounding one. Malignant tumors are harder compared to benign ones and about 100 times harder than the surrounding tissue. Because of their reduced elasticity, malignant tumors can change their shape less than the benign ones and the latter less than the surrounding tissue. By means of the ability to appreciate the elasticity of the tissues, the real time sonoelastography can make the difference between benign and malignant tumors. It has already been proved that measuring elasticity is useful in the differential diagnosis of some tumoral lesions, especially breast, prostate, lymph [1, 2], and pancreatic [3] lesions. However, the role of RTE in differentiating liver lesions is approached in few studies only [4-6]
The purpose of this paper is to appreciate if the dynamic computer analysis of the sonoelastography is able to characterize and differentiate between the benign and malignant liver lesions.
Matherial and Method
The study was a retrospective one and included patients with focal liver lesions examined by means of the RTE between 2007 and 2010. The sonoelastography was performed by a Hitachi 6500 with an RTE module: Hitachi Medical Systems Europe Holding AG, Zug, Switzerland. It was a transabdominal approach with a linear probe of 6,5 MHz or an endoscopic ultrasound one. The final diagnosis was made by considering both the sonographic/imaging and histopathological data and/or recheck after 6 months.
Each sonoelastography film was subjected to computer analysis by using a java instrument to process the image-ImageJ-developed at the National Institute of Health, Bethesda, Maryland, for which a special dynamic analysis plug-in was created. To minimize the subjectivity given by the examining doctor, all the digital postprocessing analyses were performed by the IT Center of the University of Medicine and Pharmacy in Craiova, the IT team unaware of the clinical and laboratory data of the patients. For each sonoelastography film, 10 seconds long (about 125 frames), only the color frames were automatically selected, which contain elastography information, for which the histograms were calculated. The final numeric value attributed to each examination was calculated as the average of individual histograms of each elastography frame.
The ROC analysis of the average color obtained from the direct analysis of the histograms of the concerned region (the liver tumor), after averaging the individual pixels from the 10-second-long elastography film, was used to evaluate the color information about the concerned region for the purpose of differentiating between the benign and the malignant liver lesions.
Results
We included 31 patients having an average age of 58.64±11.99. In all, 39 focal liver lesions have been studied: 30 malignant and 9 benign tumors. Out of the 30 malignant tumors, 6 were hepatocellular carcinoma, 2 cholangiocarcinoma, and 22 liver metastases. The 9 benign tumors were liver haemangioma. The sonoelastographic examination was performed during the endoscopic ultrasound (2 cholangiocarcinoma, 8 liver metastases, and 2 haemangioma) or transabdominal ultrasound (6 hepatocellular carcinoma, 7 haemangioma, 14 liver metastases). Out of the studied tumors, the cholangiocarcinoma were the hardest [Fig.1], followed by the liver metastases [Fig.2], the hepatocellular carcinoma and the liver haemangioma [Fig.3].
Fig.1.
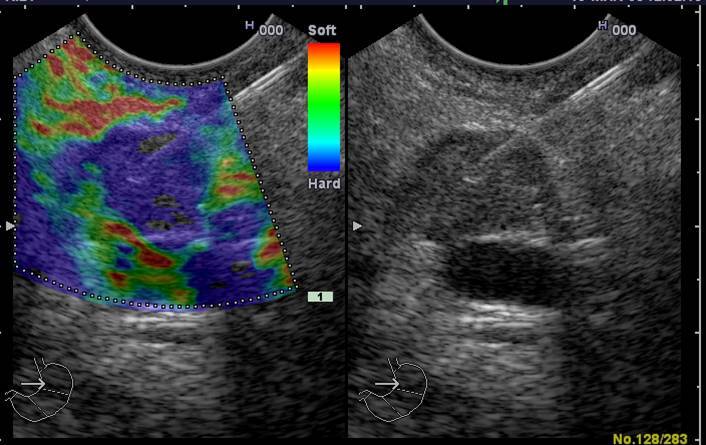
Real time transabdominal sonoelastography to a patient 65 years old with cholangiocarcinoma. The aspects in RT-E examination is predominant blue (average histogram= 221.81) suggest a hardness of the lesion. Figure take a elastography image during fine needle aspiration guided by endoscopic ultrasound
Fig.2.
Appearance of liver metastases in RT-E by transabdominal approach (2a) and endoscopic ultrasound (2b). The images illustrate the hard aspect of lesions predominantly blue. In Fig 2a RT-E demarcates very well a liver metastasis which was very difficult visible in standard ultrasound
a.
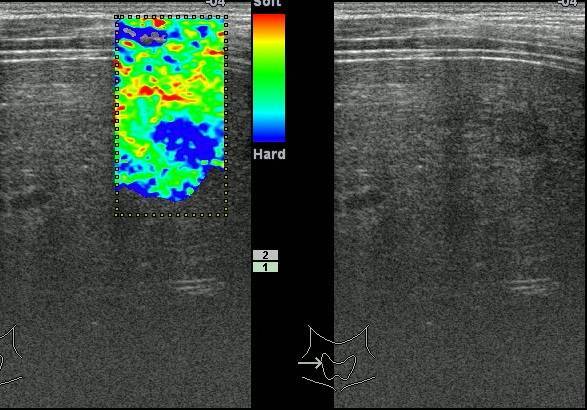
b.
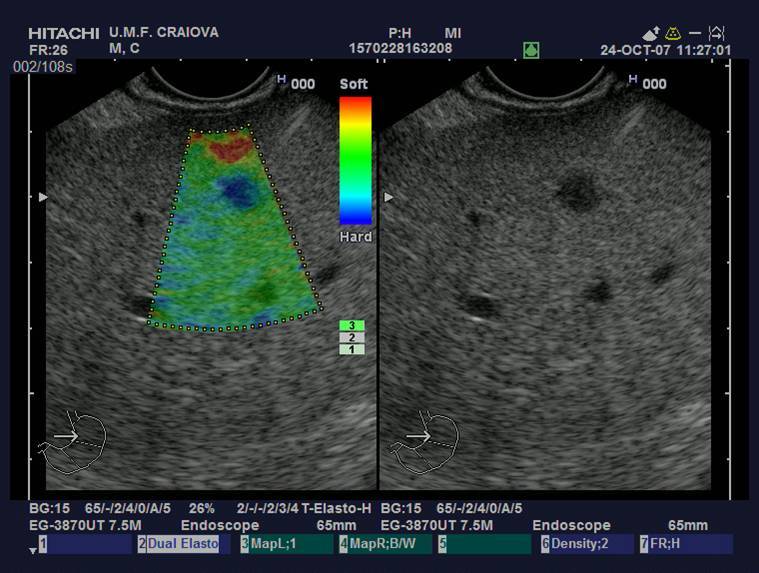
Fig.3.

Haemangioma to a young patient. RT-E reveal inhomogeneous pattern with dominant green areas. Average histogram was in this case 147.73
The average histogram obtained by analyzing the sonoelastographic films, on types of tumors, was: haemangioma 161.42±26.72; hepatocellular carcinoma 187,71±24,72; cholangiocarcinoma 208.93±18.22 and liver metastasis 204.29±16,99 [Figure 4]. The difference between the four groups was statistically significant (p<0.001). Moreover, the difference was statistically significant between the value of the average histogram for the benign and malignant tumors [Figure 5].
Fig.4.
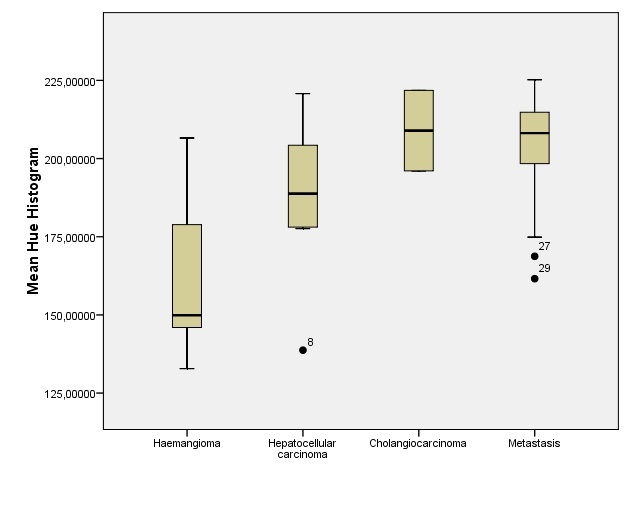
Graph shows box plots of average histogram to type of tumors. From examined tumors cholangiocarcinoma and liver metastases had the highest hardness
Fig.5.
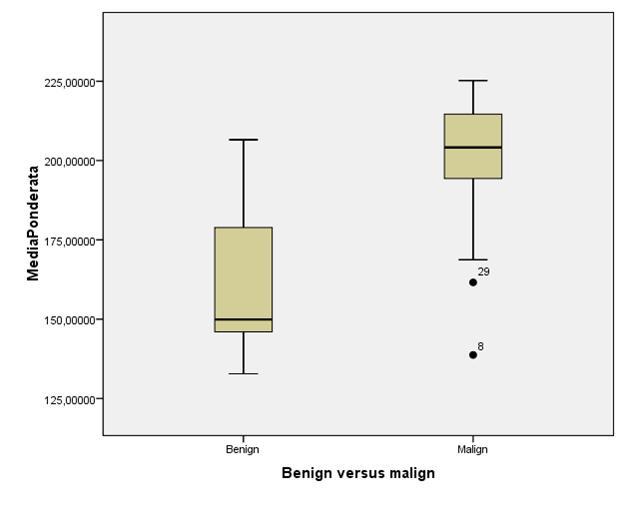
Graph shows box plots of average histogram for benign versus malignant tumors
For a cutoff value of 170 of the average histogram obtained from the concerned region, the sensitivity, specificity and accuracy of the differentiation between the benign and malignant liver lesions, was 92.5%, 88.8% and respectively 88.6% [Figure 6]. The positive predictive value was 86.7% and the negative predictive value was 92.3%.
Fig.6.
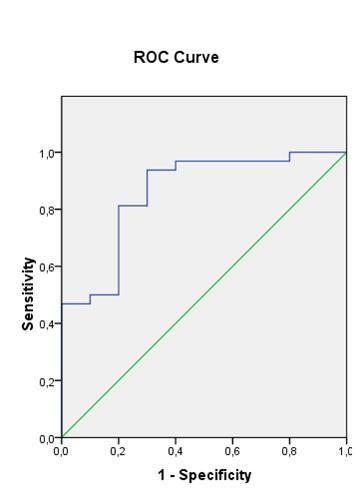
ROC analysis used for the differentiation between benign and malignant focal liver lesions based on pattern analysis of elastography images
Discussion
Taking into account the risks of the liver biopsy, lately there have been attempts to find other noninvasive methods to help the doctor differentiate between the benign and the malignant liver lesions. The sonoelastography, by its ability to appreciate the elasticity of tissues, can be one of the noninvasive sonographic/imaging methods of diagnosis. The RTE was the first elastographic method appeared on the market. It is, in fact, a soft attached to a highly professional ultrasound system. That is why, the RTE is performed immediately after the discovery of a focal lesion by means of the standard ultrasound, using the same machine and saving time for both the doctor and the patient.
Studies have shown that the RTE is really accurate in differentiating breast, thyroid, prostate, pancreas tumors or adenopathies [1 - 3, 7 - 12]. For the focal liver lesions, however, there are few studies published. The study conducted by L. Gheorghe has proven that the RTE is accurate enough in differentiating the regenerating hepatocarcinoma nodules. The study has been conducted on patients with cirrhosis with small, under 3 centimetres, subcapsular nodules [4].
The article published by Kato K. [5] and his collaborators has also shown good results of the RTE in differentiating hepatocarcinoma metastases. The authors have divided the tumors according to a new system called elasticity type of liver tumour (ETLT). According to this, most hepatocarcinoma were included into the type B, while most metastases were included into type C and D.
Another role of the RTE was demonstrated by the team led by Inoue Y., namely the discovery of small lesions which are hardly visible at the standard ultrasound [6].
Unlike the previous articles which analysed images of static RTE, our study had as a protocol, the recording and analysis of an elastography film which comprised at least 125 frames. The film was analysed by the IT Department of the University represented by an independent researcher. Thus, we eliminated the subjectivity of the first examiner who has information about the patient, which might influence the diagnosis.
The results obtained in this study are quite promising. The RTE had 88.6% accuracy in differentiating between the benign and malignant lesions. Moreover, the results match those of previous studies that is the significant hardness of cholangiocarcinoma, followed by hepatocarcinoma, while the liver haemangioma have proved the least hard.
Perspectives
The present study included a smaller number of patients with cholangiocarcinoma and included no patients with adenoma or hepatic nodular hyperplasia. In the future all types of liver tumor are intended to be studied and an increasing number of patients included. The RTE might be used as a noninvasive method to diagnose liver tumor, as well as the ultrasound with contrast (CEUS). It would be interesting to find out if the CEUS combined with RTE would have higher accuracy as compared to CEUS as the only method of diagnosis.
In conclusion, the RTE is a sonographic/imaging method with promising results in the characterization and differentiation of focal liver lesions visualized transabdominally or endoscopically ultrasound.
Acknowledgments
This work was supported by research grant Partnership – PN II of the ANCS, CNDI – UEFISCDI, project number 2011-3,2-0503.
References
- 1.Saftoiu A, Vilmann P, Hassan H, et al. Analysis of endoscopic ultrasound elastography used for characterization and differentiation of benign and malignant lymph nodes. Ultraschall Med. 2006;27:535–542. doi: 10.1055/s-2006-927117. [DOI] [PubMed] [Google Scholar]
- 2.Saftoiu A, Vilmann P, Ciurea T, et al. Dynamic analysis of endoscopic ultrasound (EUS) elastography used for the differentiation of benign and malignant lymph nodes. Gastrointest Endosc. 2007;66:291–300. doi: 10.1016/j.gie.2006.12.039. [DOI] [PubMed] [Google Scholar]
- 3.Săftoiu A, Vilmann P, Gorunescu F, et al. Neural network analysis of dynamic sequences of EUS elastography used for the differential diagnosis of chronic pancreatitis and pancreatic cancer. Gastrointest Endosc. 2008 Dec;68(6):1086–1094. doi: 10.1016/j.gie.2008.04.031. [DOI] [PubMed] [Google Scholar]
- 4.Gheorghe L, Iacob S, Iacob R, Dumbrava M, Becheanu G, Herlea V, Gheorghe C, Lupescu I, Popescu I. Real time elastography - a non-invasive diagnostic method of small hepatocellular carcinoma in cirrhosis. J Gastrointestin Liver Dis. 2009 Dec;18(4):439–446. [PubMed] [Google Scholar]
- 5.Kato K, Sugimoto H, Kanazumi N, Nomoto S, Takeda S, Nakao A. Intra-operative application of real-time tissue elastography for the diagnosis of liver tumours. Liver Int. 2008 Nov;28(9):1264–1271. doi: 10.1111/j.1478-3231.2008.01701.x. [DOI] [PubMed] [Google Scholar]
- 6.Inoue Y, Takahashi M, Arita J, Aoki T, Hasegawa K, Beck Y, Makuuchi M, Kokudo N. Intra-operative freehand real-time elastography for small focal liver lesions: "visual palpation" for non-palpable tumors. Surgery. 2010 Nov;148(5):1000–1011. doi: 10.1016/j.surg.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 7.Itoh A, Ueno E, Tohno E, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006;239:341–350. doi: 10.1148/radiol.2391041676. [DOI] [PubMed] [Google Scholar]
- 8.Thomas A, Fischer T, Frey H, et al. Real-time elastography – an advanced method of ultrasound: first results in 108 patients with breast lesions. Ultrasound Obstet Gynecol. 2006;28:335–340. doi: 10.1002/uog.2823. [DOI] [PubMed] [Google Scholar]
- 9.Lyshchik A, Higashi T, Asato R, et al. Thyroid gland tumor diagnosis at US elastography. Radiology. 2005;237:202–211. doi: 10.1148/radiol.2363041248. [DOI] [PubMed] [Google Scholar]
- 10.Rago T, Santini F, Scutari M, Pinchera A, Vitti P. Elastography: new developments in ultrasound for predicting malignancy in thyroid nodules. J Clin Endocrinol Metab. 2007;92:2917–2922. doi: 10.1210/jc.2007-0641. [DOI] [PubMed] [Google Scholar]
- 11.Miyanaga N, Akaza H, Yamakawa M, et al. Tissue elasticity imaging for diagnosis of prostate cancer: a preliminary report. Int J Urol. 2006;13:1514–1518. doi: 10.1111/j.1442-2042.2006.01612.x. [DOI] [PubMed] [Google Scholar]
- 12.Tsutsumi M, Miyagawa T, Matsumura T, et al. The impact of real-time tissue elasticity imaging (elastography) on the detection of prostate cancer: clinicopathological analysis. Int J Clin Oncol. 2007;12:250–255. doi: 10.1007/s10147-007-0669-7. [DOI] [PubMed] [Google Scholar]


