Abstract
Purpose
Fatigue is a commonly reported symptom by prostate cancer survivors and is associated with significant distress and declines in quality of life. Qigong is a mind-body activity that consists of both physical activity and meditative aspects. This 12-week Randomized Controlled Trial (RCT) examined the feasibility and efficacy of a Qigong intervention for improving older prostate cancer survivors’ levels of fatigue and distress.
Methods
Forty older (Mdn age=72, range=58–93), fatigued (cut-off value of ≥ 1 on the CTCAEv4.0, >20 on a fatigue grading scale), and sedentary (<150 minutes of moderate exercise/week) prostate cancer survivors were randomized to 12-weeks of Qigong or Stretching classes. Primary outcomes were feasibility (i.e., retention & class attendance rates), and fatigue (FACIT-Fatigue), and secondary outcome was distress (Brief Symptom Inventory-18, BSI-18).
Results
Study retention rates did not significantly differ between study groups (Qigong=80%, Stretching=65%, p=0.48). The Qigong group had significantly higher class attendance than the Stretching group (p=0.04). The Qigong group had significantly greater improvements in the FACIT-Fatigue (p=0.02) and distress (i.e., BSI-18 Somatization, Anxiety, & Global Severity Index, p’s<0.05), than the Stretching group.
Conclusions
This 12-week Qigong intervention was feasible and potentially efficacious in improving senior prostate cancer survivors’ levels of fatigue and distress levels. Future, larger definitive randomized controlled trials are needed to confirm these benefits in older prostate cancer survivors, and in racially and ethnically diverse populations.
Implications for Cancer Survivors
Qigong may be an effective nonpharmacological intervention for the management of senior prostate cancer survivors’ fatigue and distress.
Keywords: Senior Prostate Cancer Survivors, Qigong, Randomized Controlled Trial, Fatigue, Distress
Introduction
Prostate cancer accounts for 25% of newly diagnosed cancers in U.S. males, and it is the second leading cause of cancer-related deaths cancer in men [1, 2]. Prostate cancer is an older man’s disease, with a median diagnosis age of 67 years [2]. Severe fatigue is one of the most common cancer-related symptoms reported by cancer survivors, particularly for prostate cancer survivors receiving androgen deprivation therapy (ADT) [3]. Yet, it is one of the least understood symptoms by both patients and providers [4]. The prevalence of cancer-related fatigue ranges from 17% to 21% (using ICD-10 diagnostic criteria) and 33% to 53% when a graded fatigue scale is used (0 – 10 fatigue) [5]. It is defined as a subjective sense of physical, emotional, or cognitive tiredness, but the underlying causes of cancer-related fatigue are not well understood and are likely multifactorial [5]. Alleged contributing factors include cancer treatments (i.e., ADT, chemotherapy, radiation), anemia, psychological distress, pain, medications, sleep disturbance, decreased functional status, nutritional deficit, and comorbidities (e.g., cardiac, endocrine, or pulmonary dysfunction) [5]. Fatigue may persist for months or years following treatment and greatly diminish survivors’ quality of life by limiting their ability to perform daily living activities and generating significant distress [6, 7].
Distress is another commonly reported symptom by survivors and rates are higher (17% to 25%) in cancer survivors than in healthy populations (3%) [8]. A large number of older survivors have untreated significant levels of distress [9, 10], which is cause for concern because distress is a risk factor for poor adherence to cancer treatment, surveillance guidelines, and risk-reducing health behaviors [10]. Older survivors with poor physical functioning, comorbidities, and cancer-related physical symptoms are the most prone to high levels of distress [4, 11–13]. Both fatigue and distress have significant negative implications for survivors’ quality of life, therefore it is imperative for researchers to find effective interventions for the management of these symptoms.
Physical activity is a nonpharmacological intervention that has been recommended for the management of cancer-related fatigue and is also associated with reductions in distress [14, 5, 15, 16]. Mind-body activities such as Qigong combine physical activity with stress reduction elements [17, 18]. Specifically, the practice of Qigong consists of slow, flowing movements, coordinated with deep breathing, and a meditative focus to balance the flow of ‘Qi’ or life energy for overall well-being [17]. Qigong may be a feasible modality of physical activity for older cancer survivors because it is performed at a slow pace, not overly physically exertive, and is easily accessible (i.e., can be performed sitting).
A 2012 review [19] on the effectiveness of Qigong in supportive cancer care revealed that only two randomized controlled trials (RCT) had assessed distress outcomes and one RCT had examined fatigue outcomes. These studies generally indicated improvements in fatigue and distress for cancer survivors of different cancer types. Since this review, two additional Qigong RCTs with depressed chronically ill elderly adults and breast cancer survivors undergoing radiation therapy have been conducted. These trials were associated with reductions in depressive symptoms [20, 21] and improvements in fatigue for breast cancer survivors with elevated depressive symptoms at baseline [21]. However, Qigong RCTs have not specifically targeted older prostate cancer survivors for improving fatigue and distress, and this is an important group of survivors to intervene with [4].
We are not aware of any RCTs that have examined the efficacy of Qigong for improving fatigue and distress in senior prostate cancer survivors. The purpose of this 12-week RCT was to assess its feasibility in senior prostate cancer survivors and examine its efficacy for improving fatigue (primary outcome) and distress (secondary outcome) compared to an active control (i.e., stretching exercise group). We hypothesized that the Qigong intervention would be associated with larger improvements in fatigue and distress compared to a stretching exercise control group. The results can be used to inform the development of a larger definitive RCT for helping older prostate cancer survivors effectively manage levels of fatigue and distress.
Methods
Study Design and Participants
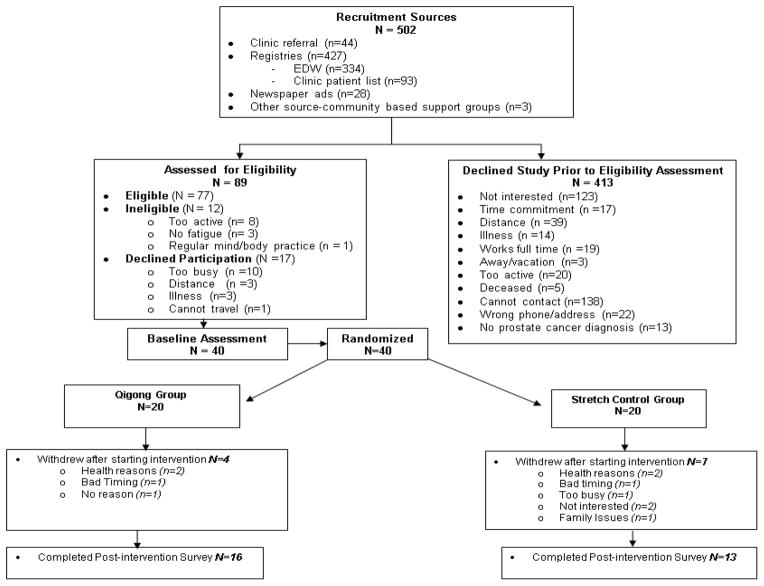
This was a two-armed, parallel group, feasibility RCT guided by the Consolidated Standards of Reporting Trials (CONSORT) statement (Figure 1) [22]. A single-blinded design was not used because informed consent procedures required that participants be informed that they would be randomly assigned to either Qigong or Stretching classes; statisticians were blinded to study group allocation. The study was approved by the University of Utah Institutional Review Board and registered at ClinicalTrials.gov (NCT01564394). Power calculations indicated that, with a sample size of 24 participants in each study group and a standard deviation of 9.0, a change in FACIT –Fatigue score could be estimated to within ±3.6 units using a two-sided 95% confidence interval, with 80% power to detect a 7.5 unit difference between the groups at 5% significance level. The purpose of this pilot trial was to determine the feasibility of a Qigong intervention in senior prostate cancer survivors and to provide data for estimating effect size required for a larger more definitive trial.
Figure 1.
Consort diagram of the 12-week Qigong randomized controlled trial.
Senior prostate cancer survivors were recruited via Huntsman Cancer Institute (HCI) clinics, cancer registries, and community-based strategies (Figure 1). Survivors’ family members (i.e., a spouse, adult child, or sibling) were invited to participate in the classes to aid in enrollment and retention. A research coordinator contacted potential participants to discuss study details and to assess their eligibility for enrollment. Inclusion criteria consisted of: 1) Age ≥ 55 years; 2) significant fatigue as assessed during eligibility screening with the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAEv4.0) using a fatigue cut-off value of ≥ 1 or a general fatigue grading scale (i.e. fatigue currently and in the past week from a scale of 0 to 100) with a cut off value of >20; 3) sedentary as defined by <150 minutes of moderate-intensity exercise/week per Centers for Disease Control and Prevention guidelines [23]; 4) resided within 60 miles of HCI and able to travel; 5) spoke and read English fluently; 6) physician’s medical release; and 7) willing to be randomized to study group. Exclusion criteria included: 1) Evidence of metastatic disease other than elevated Prostate-Specific Antigen levels [24]; 2) current practice of Qigong, Tai Chi, or similar type of Complementary and Alternative Medicine exercise; 3) inability to pass the Folstein Mini Mental Status Exam (score ≤23); and 4) health conditions (i.e., respiratory, cardiovascular or neurological problems) that could interfere with intervention. We recruited fatigued and sedentary prostate cancer survivors because they may derive the most benefit from the Qigong intervention by improving their vitality and physical activity levels (i.e., fatigue was the primary outcome). All participants provided informed consent prior to enrollment in study.
Intervention
After completion of the baseline survey, HCI’s Research Informatics Shared Resource randomized participants to study group (Qigong or Stretching) using blocks of varying sizes (2–4) to minimize predictability of assignment. The Qigong and non-aerobic stretching exercise classes were 60 minutes in duration, held two days per a week for 12 weeks at Huntsman Cancer Institute’s Survivorship & Wellness Center, and supplemented with home-based practice. The intervention period was set at 12 weeks to be an acceptable length in this senior sample for whom time commitment (i.e., time required to attend classes and for traveling) is a barrier to engaging in physical activity [25]. The sessions were twice per a week, rather than more frequent weekly sessions, based on participants’ suggestions from a prior RCT of Tai Chi Chih in older female survivors [26] and most physical activity interventions for cancer survivors are held for 2 to 3 days a week for 10 to 24 weeks [27]. Trained research staff attended each session to ascertain participant attendance. Make-up classes were not offered. However, to encourage home-based practice both groups were provided with a DVD (Qigong or Stretching) that consisted of progressive sessions of each intervention performed by the respective instructors. Additionally, the research coordinator reminded participants each week to maintain home practice. Participants were asked not to begin other new physical activities during the study.
The Qigong classes were led by a Qigong Master and his certified instructors. Sessions began with a five-minute meditative focus on the breath, followed by sitting exercises, then standing movements, and ended with a final five-minute meditative focus on the breath. Examples of the sitting exercises include: 1) Opening of the nine gates, 2) muscle change exercises, and 3) cavity presses. Examples of the standing exercises include: 1) Collecting Energy of Heaven and Earth, 3) Rocking chair, 4) Tai Chi Ruler, 6) Hands skimming on water, 7) Pushing and pulling space, and 8) Cloud hands. As the study progressed, a larger proportion of time was spent performing the standing movements than the sitting exercises.
We also integrated an eccentrically-biased muscular focus into the Qigong standing movements (e.g., Rocking chair, Tai Chi Ruler, etc) to increase the intensity of the intervention, while maintaining a level of safety for these older adults. Eccentrically-biased movements use the body weight as resistance and target eccentric muscle contractions where the muscle lengthens. This entailed using deeper squatting positions in the Qigong standing movements. For instance, during the Rocking Chair movement, participants were instructed to focus on squatting as low as they could during the movement. Eccentric muscle activity can produce the highest forces, maximizing the muscle and mobility responses at the lowest energetic cost to the individual. This is ideal for older prostate cancer survivors who may be experiencing muscle wasting and weakness, and fatigue as a result of cancer treatments. Research with older cancer survivors has shown that eccentrically-biased muscular movement is associated with increased muscle size and strength, and improved mobility compared to non-exercise usual care [28].
The non-aerobic stretching classes were led by instructors from the University of Utah’s Department of Exercise and Sport Science. This group served as an active control (i.e., physical activity in group setting) and consisted of light stretching exercises, while avoiding relaxation techniques that would be similar to meditation. The exercises included upper and lower body stretching exercises that targeted main muscle groups, and were performed seated and standing. As the study progressed, the intensity and duration of the stretching exercises were progressively increased.
Measures
The intervention’s feasibility was assessed with retention and class attendance rates. Our primary and secondary outcomes of improvement in fatigue and distress were assessed at baseline and one-week post-intervention with the Functional Assessment Chronic Illness Therapy (FACIT)-Fatigue scale [29] and the Brief Symptom Inventory-18 (BSI-18) [30]. The FACIT-Fatigue Scale assesses levels of fatigue during usual activities over the past seven days, with higher scores indicating less fatigue (score range= 0 – 52). Very good internal consistency has been reported (α = 0.86 to 0.87) [31]. The BSI-18 assesses psychological distress from the past seven days, and produces a Global Severity Index (GSI) and dimension scores for somatization (SOM), anxiety (ANX), and depression (DEP). Raw scores were converted to T-scores based on gender-specific oncology norms, with lower scores indicating less distress. Good to very good internal consistency has been reported (GSI α = 0.89, SOM α = 0.74, ANX α = 0.79, DEP α = 0.84) [30]. To measure intervention intensity, participants reported their rate of perceived exertion with the Borg scale [32] on a biweekly basis to keep respondent burden low. Home practice was self-reported weekly.
Data Analysis
Comparisons of the two study groups’ sociodemographics at baseline were assessed with Pearson Chi-square tests for categorical data (Fisher’s Exact Tests if expected cell count n <5) and Wilcoxon tests for continuous data. Comparison of changes (post – baseline) in FACIT-Fatigue and BSI-18 among the study groups were assessed with Wilcoxon tests. Wilcoxon non-parametric tests were used because the data were appreciably skewed. Statistical significance was based on an alpha of 0.05. Per protocol analyses were conducted on participants with complete data at baseline and post-intervention with statistical program SPSS v.17. Intent-to-treat analyses were not employed because we did not have post-intervention data on participants who withdrew from the study to conduct complete case analysis and our sample size was too small to conduct multiple imputation techniques.
Results
Feasibility
We invited 502 senior prostate cancer survivors to participate through clinic referrals, the cancer registry, or community advertisements (Figure 1). We assessed 89 survivors for eligibility and randomized 40 eligible and interested survivors to either the Qigong or Stretching group (n=20 in each study group). The most common reasons that survivors gave for declining the eligibility assessment or enrollment into the trial were a lack of interest in the study or time constraints (i.e., work full time, too busy, not willing to make time commitment). Twenty-nine participants completed the 12-week intervention (Qigong n=16, Stretching n=13). The retention rates (i.e., the number of participants who remained enrolled and completed post-intervention measures) did not significantly differ between the study groups (Qigong = 80%, Stretching = 65%, p = 0.48).
One possibility is that survivors who had family members attending classes were more likely to remain enrolled (i.e., there were 10 family members in each study group). We tested this with Fisher’s Exact test by comparing retention rates for survivors who withdrew or remained enrolled by those who had a family member enrolled. These results were nonsignificant (59% had a family member attend & remained enrolled, whereas 41% had no family member attend & remained enrolled; p=0.15), indicating that participants’ choice to remain enrolled in the study did not depend on having a family member enrolled. However, these results should be interpreted with caution as the small sample size limits our ability to draw firm conclusions of the effects of enrolled family members on participants’ retention.
We next compared class attendance rates (i.e., number of classes attended/number of total classes*100) among the study groups and found that the Qigong group had significantly higher attendance than the Stretching group (Qigong Mdn = 85%, Interquartile range (IQR)= 68%; Stretching Mdn = 43%, IQR = 67%, p = 0.04). Additionally, we found that the class attendance rates did not differ according to whether survivors had a family member enrolled or not (p =0.30).
Sociodemographics
The study arms did not differ significantly with respect to baseline sociodemographic data (Table 1). The median age of participants was 72 years (range 58 to 93 years), diagnosed with prostate cancer a median of 5 years prior (range 0 to 26). Forty-eight percent were currently on ADT. We also compared the participants who completed the intervention to those who withdrew on sociodemographic variables (i.e., age, marital status, education, income, current ADT use, & cancer stage), FACIT-Fatigue, and the BSI-18 scales (i.e., DEP, ANX, SOM, & GSI), and found no significant differences (p’s>.05).
Table 1.
Baseline Sociodemographics and Clinical Variables by Study Groups
| Qigong n=16 |
Stretching n=13 |
p-value | |
|---|---|---|---|
| Age, years Mdn (range) | 72 yrs (58 – 90) | 73 yrs (61 – 93) | 0.81 |
|
| |||
| Ethnicity n (%) | 0.45 | ||
| Non-Latino | 16 (100%) | 12 (92%) | |
| Latino | 0 (0%) | 1 (8%) | |
|
| |||
| Race n (%) | 0.19 | ||
| White | 16 (100%) | 11 (85%) | |
| Non-white | 0 (0%) | 2 (15%) | |
|
| |||
| Marital Status n (%) | 0.34 | ||
| Married/living as married | 12 (75%) | 12 (92%) | |
| Not Marrieda | 4 (25%) | 1 (8%) | |
|
| |||
| Education n (%) | 0.70 | ||
| High School, some vocational school or college | 5 (31%) | 3 (23%) | |
| College degree/Post-grad | 11 (69%) | 10 (77%) | |
|
| |||
| Religion n (%) | 0.68 | ||
| Latter Day Saints/Mormon | 9 (56%) | 5 (39%) | |
| Other religion | 5 (31%) | 6 (46%) | |
| Not religious | 2 (13%) | 2 (15%) | |
|
| |||
| Employment n (%) | 0.67 | ||
| Employed | 3 (19%) | 4 (31%) | |
| Not employed | 13 (81%) | 9 (69%) | |
|
| |||
| Incomeb n (%) | 1.00 | ||
| <$50,000 | 5 (31%) | 4 (36%) | |
| ≥$50,000 | 11 (69%) | 7 (64%) | |
|
| |||
| Cancer Stagec n (%) | 0.11 | ||
| Stage I – II | 8 (53%) | 2 (18%) | |
| Stage III – IV | 7 (47%) | 9 (82%) | |
|
| |||
| Years since diagnosis Mdn (range) | 5.50 yrs (2 – 22) | 4.00 yrs (0 – 26) | 0.83 |
|
| |||
| Current ADT Use n (%) | 0.27 | ||
| Yes | 6 (38%) | 8 (61%) | |
| No | 10 (62%) | 5 (39%) | |
|
| |||
| Cancer Treatmentd n (%) | |||
| Open radical prostatectomy | 5 (31%) | 6 (46%) | 0.46 |
| DaVinci prostatectomy | 1 (6%) | 1 (8%) | 1.00 |
| Surgery | 2 (12%) | 1 (8%) | 1.00 |
| External beam radiation | 4 (25%) | 0 (0%) | 0.11 |
| Radiation | 2 (12%) | 3 (23%) | 0.63 |
| Brachytherapy | 5 (31%) | 0 (0%) | 0.05 |
| Chemotherapy | 0 (0%) | 2 (15%) | 0.19 |
|
| |||
| Chronic Diseases n (%) | |||
| Diabetes | 5 (31%) | 4 (31%) | 1.00 |
| Arthritis | 6 (38%) | 6 (46%) | 0.72 |
| Hypertension | 9 (56%) | 10 (77%) | 0.43 |
| Depression | 5 (31%) | 4 (31%) | 1.00 |
| Myocardial Infarction | 3 (19%) | 3 (23%) | 1.00 |
| COPD | 1 (6%) | 0 (0%) | 1.00 |
Note. Medians (Mdn) were reported for skewed data and Wilcoxen tests conducted. Categorical data were analyzed with Pearson Chi-square tests; data with cell n< 5 used Fisher’s Exact tests.
COPD = Chronic Obstructive Pulmonary Disease.
Includes divorced, separated, never married, widowed.
Two participants declined to report income.
Cancer stage was not reported for three participants (Qigong n=1, Stretch n=2).
One participant reported watchful waiting and one reported immunotherapy.
Intervention Intensity
We compared the study groups on their rate of perceived exertion (i.e., Borg scale) during the Qigong and Stretching classes with Wilcoxon tests. The range of this scale is 0 (feel no exertion or breathlessness) to 10 (the most effort one can possibly give). The Qigong group had significantly higher rates of perceived exertion (Mdn=4.3, range= 1.8 – 8.4) than the Stretching group (Mdn=2.6, range 1.0 – 4.0; p=.002). The Qigong group’s Borg scale value indicated that they felt the classes were of “somewhat strong” exertion, whereas the Stretching group felt the classes were of “weak” to “moderate” exertion.
Fatigue
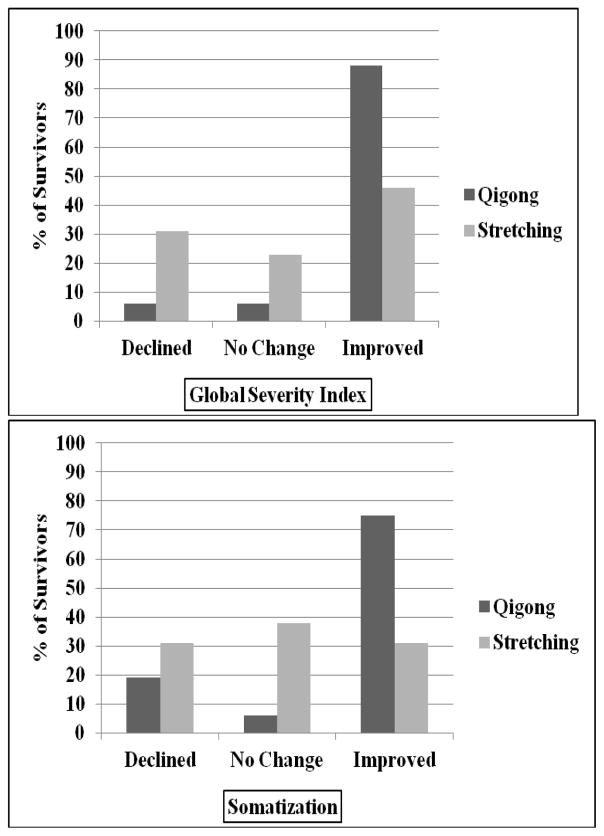
At baseline, the Qigong and Stretching groups did not differ by clinical levels of fatigue using the FACIT-Fatigue cut-off ≤43 (Cella, 2002), with 55% (n=12) in the Qigong group and 45% (n=10) in the Stretching group. This also indicated that the majority of our sample was clinically fatigued (i.e., 22 out of 29 participants). For our primary outcome of fatigue, we compared the study groups on their change (post – baseline) in the FACIT-Fatigue with Wilcoxon tests. As hypothesized, the Qigong group had significantly greater improvement than the Stretching group (Qigong Mdn = 5.0, range = −3 to 30; Stretching Mdn = 0, range = −22 to −9, p= 0.02, Table 2). Additionally, 69% (n=11) in the Qigong group and 38% (n=5) in the Stretching group had a minimally important difference of three points or more (Cella, 2002). See Figure 2 for the percentage of survivors in each group who improved, declined (worsened), or had no change in the FACIT-Fatigue.
Table 2.
FACIT-Fatigue and BSI-18 Baseline and Change Values for Study Groups
| Qigong Median (range) n=16 |
Stretch Median (range) n=13 |
p-value | |
|---|---|---|---|
| FACIT-Fatigue | |||
| Baseline | 34.0 (14 – 46) | 38.0 (18–49) | .56 |
| Change (Post–Baseline) | 5.0 (−3 – 30) | 0 (−22 – 9) | .02 |
|
| |||
| BSI-18 Depression | |||
| Baseline | 57.5 (42–78) | 60.0 (42–67) | .65 |
| Change (Post–Baseline) | −6.5 (−20 −2) | 0.0 (−12 – 19) | .09 |
|
| |||
| BSI-18 Somatization | |||
| Baseline | 54.0 (40–69) | 54.0 (40–64) | .76 |
| Change (Post–Baseline) | −6.5 (−17 − 7) | 0.0 (−10 – 11) | .048 |
|
| |||
| BSI-18 Anxiety | |||
| Baseline | 47.0 (39–71) | 48.0 (39–67) | .65 |
| Change (Post–Baseline) | −7.5 (−23 −9) | 0.0 (−9 −26) | .003 |
|
| |||
| BSI-18 Global Severity Index | |||
| Baseline | 52.0 (48–71) | 57.0 (41–68) | .91 |
| Change (Post–Baseline) | −7.0 (−18 −5) | 0.0 (−10 −20) | .002 |
Note. BSI-18 subscale data are T-scores based on male Oncological norms. Analyses included participants with complete post-intervention data and were conducted with Wilcoxon tests. BSI-18 = Brief Symptom Inventory-18, FACIT-Fatigue = Functional Assessment of Chronic Illness Therapy-Fatigue. Positive change values for FACIT-Fatigue indicate improvement. Negative change values for BSI-18 scales indicate improvement.
Figure 2.
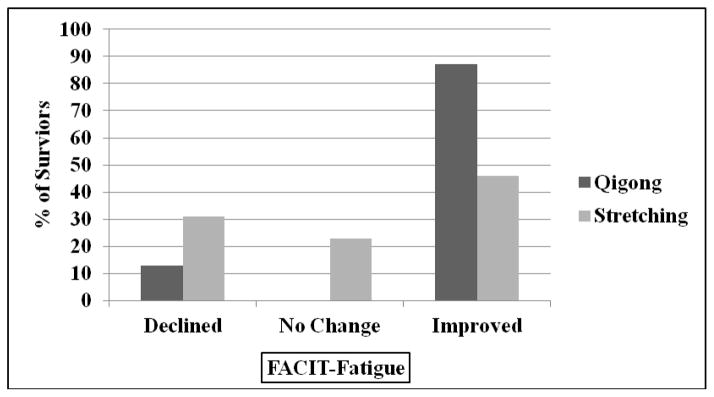
Percentage of survivors in each study group who declined, had no change, or improved in FACIT-Fatigue.
Distress
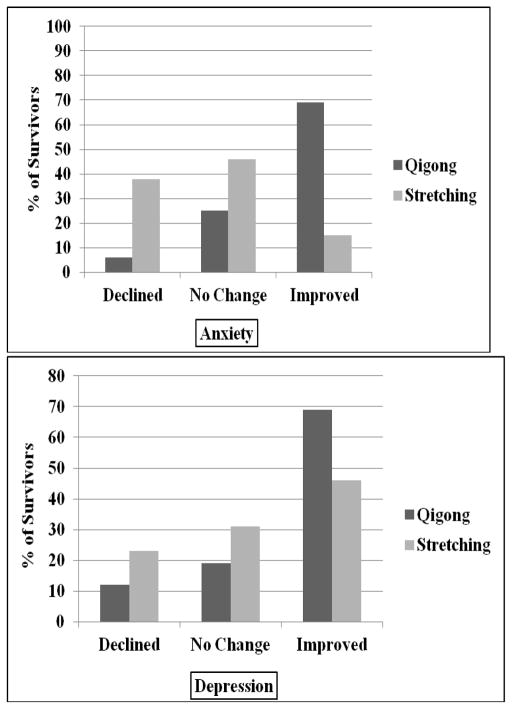
At baseline, the Qigong and Stretching groups did not significantly differ on the DEP, SOM, ANX, and GSI levels (Table 2). We compared the groups on their change (post-baseline) in the BSI-18 with Wilcoxon tests and found that the Qigong group had more significant improvements than the Stretching group in the SOM, ANX, and GSI scales (p’s<.05; see Table 2 for medians and ranges). We did not assess minimally important differences in the BSI-18 because there are not published guidelines on what such a difference would be for the BSI-18. Using Cohen’s d, we calculated effect sizes for comparing the changes between study groups (Small effect = 0.2, Medium effect = 0.5, Large effect = 0.8) and found these to be associated with large effect sizes (i.e., ANX d = −1.1, SOM d = −0.8, GSI d= −1.2, DEP d = −0.8). See Figure 3 for the percentage of survivors in each group who improved, declined (worsened), or had no change in GSI, SOM, ANX, and DEP.
Figure 3.
Percentage of survivors in each study group who declined, had no change, or improved in the BSI-18 scales.
Home Practice
The Qigong and the Stretching group reported a median home practice of 1.25 (range = 0 to 2.75) and 0.75 (range = 0 to 3.33) times a week, respectively, which did not significantly differ from one another (Wilcoxon test p=.80). We also conducted bivariate Pearson correlations to examine whether the frequency of home practice was associated with changes in the FACIT-Fatigue and BSI-18 scales for each of the study groups. These tests did not reveal any significant associations (all p’s >.05). However, the home practice results should be interpreted with caution because the study groups had low compliance for reporting on the frequency of their home practice. Therefore, we may not have an accurate record of how much home practice was actually engaged in.
Discussion
In this 12-week RCT, we demonstrated that a Qigong intervention is feasible in a population of senior prostate cancer survivors. Retention and class attendance rates for the Qigong intervention were good. In a prior RCT of Tai Chi Chih for older female cancer survivors [26], the study retention rate was 86% and class attendance rate was 81%, which is comparable to our sample of older prostate cancer survivors. We did not find that the participation of a family member significantly effected retention or attendance rates, although survivors with an attending family member were 18% more likely to remain enrolled than those without a family member. Research indicates that spousal or family support can facilitate engagement in health behaviors that help manage chronic illnesses [33, 34]. Future larger studies are warranted to better ascertain the effects of family participation on older male survivors’ retention in behavioral intervention trials.
Importantly, we found that the Qigong intervention was associated with significantly larger improvements in fatigue and distress than the Stretching group. Not only did we see significant improvement in the Qigong participants’ fatigue, but a large proportion (69%) of the Qigong participants had a minimally important difference of three points or more in fatigue [29], whereas 31% of the Stretching participants did. We did not assess minimally important differences in distress because there are not published guidelines on what such a difference would be for the BSI-18; however, we did find large effect sizes for the improvements in distress. Fatigue and distress are common symptoms among cancer survivors that can lead to declines in quality of life, and poor adherence to cancer treatment and surveillance guidelines [10, 5]. For older survivors, fatigue and distress can become debilitating as these survivors are also attempting to manage cancer treatment side effects, age-related comorbidities, and declines in physical functioning. The joint effect of these may create a downward spiral towards poor health and functioning, and threaten their ability to maintain their independence into late life [9].
Our study findings are consistent with other Qigong RCTs for cancer survivors and depressed, chronically ill older adults. A 10-week Qigong RCT with different types of cancer survivors and genders was associated with improved fatigue, distress, cognitive functioning, quality of life, and inflammation (C-Reactive Protein) compared to a usual care control [35, 36]. In older depressed adults living with chronic illness, a 12-week Qigong intervention reduced depressive symptoms relative to a reading control group [20]. Similarly, in breast cancer survivors receiving radiation therapy, Qigong (i.e., 5 classes during 5 to 6 weeks of radiation therapy) was associated with fewer depressive symptoms, and improvements in fatigue and quality of life in those with elevated baseline levels of depression [21]. Finally, in patients with chronic fatigue, a 4-month Qigong intervention helped improve fatigue symptoms and mental functioning [37].
Our study extends on these studies in a few ways. First, the prior studies demonstrated the efficacy of Qigong in cancer survivors of different ages and cancer types, and in chronically ill adults. We have demonstrated Qigong’s efficacy for improving fatigue and distress in older prostate cancer survivors. We targeted older prostate cancer survivors because this is an understudied group of survivors, despite being the second largest group of cancer survivors. Furthermore, the prevalence of fatigue is high among those receiving ADT [5], and as mentioned prior, older cancer survivors are a particularly vulnerable group [4].
Secondly, we incorporated eccentrically-biased-muscular movements into the Qigong protocol for the purpose of increasing the exercise intensity (i.e., deeper squatting movements) without compromising safety. Research has shown that eccentrically biased exercises can improve muscular and mobility functioning in older cancer survivors [28]. Furthermore, exercise is associated with reductions in cancer-related fatigue [16, 38] and is recommended for older adults to maintain physical functioning and quality of life [39]. Future trials should continue to examine the benefits of including an eccentrically-biased muscular focus in the Qigong movements through objective assessments of physical functioning.
Finally, Qigong RCTs, such as those described previously, have compared a Qigong intervention with a usual care control or a wait-list control (i.e., exception of Tsang, 2013 who used a reading control). The limitations of these control groups is that the participants’ outcome expectancies between treatment and control groups may differ, and these types of control groups do not control for active (i.e., physical activity) components of the Qigong intervention [40]. On the contrary, we used an active control group that controlled for engagement in physical activity (i.e., stretching) and was structurally equivalent to the Qigong intervention by having a similar class format (i.e., length of time, frequency, & same weekdays; group format), both study group’s classes consisted of sitting and standing exercises, and were provided DVDs to encourage home practice. Additionally, we attempted to establish treatment credibility by promoting both study groups as providing a benefit for participants. We think the use of a stretching control group helps lend greater confidence to the validity of our study’s findings.
There are a few limitations of our study to take note of. First, the mechanisms responsible for our fatigue and distress outcomes are not known. The improvements in fatigue and distress may have been a result of increased physical activity, the meditative aspects of the Qigong intervention, or the combination of both. Although we used a control group that included physical activity, the Qigong participants reported a higher rate of perceived exertion (i.e., Borg scale) than the Stretching participants did. In support of the meditative mechanisms, yoga and mindfulness-based stress-reduction interventions have demonstrated benefits for a variety of cancer-related symptoms, including fatigue and distress [41, 42]. However, we did not assess mindfulness or meditative aspects and future trials would benefit from including these. It may be that the effective management of fatigue and distress in older cancer survivors entails both meditative and physical activity strategies as provided by mind-body activities such as Qigong. Furthermore, Qigong may be an appealing form of physical activity to older sedentary cancer survivors because it is not overly physically exertive and is considered safe in elderly populations [17].
A second limitation of our study is that our study sample was racially and ethnically homogenous (i.e., mainly non-Latino White). We do not know if these outcomes would occur with other racial or ethnic groups of cancer survivors. For example, a recent study [43] demonstrated that physical activity was associated with reductions in prostate cancer risk for White men, but not for African American men, despite having equivalent levels of physical activity. Future studies are needed to investigate the efficacy of Qigong for other racially/ethnically diverse populations of older survivors and potential biological mechanisms that may underline differential outcomes.
Additionally, attrition bias is a threat to the validity of our study if the participants who withdrew systematically differed from those who remained enrolled. To examine this, we compared the baseline sociodemographic variables, FACIT-Fatigue, and BSI-18 scores for participants who withdrew and those who remained enrolled. We found that the groups did not significantly differ in their baseline levels, therefore we felt more confident that attrition bias was not a large threat to our study.
Another limitation is that our screening of potential participants’ fatigue was assessed with fatigue measures (i.e., CTCAE & general fatigue grading scale) other than the FACIT-Fatigue scale that we used to measure the fatigue outcome. We did this to decrease the respondent burden of the screening eligibility questions and the CTCAE is widely used in clinic settings to assess patients’ levels of fatigue. As aforementioned, we found that a large proportion of our participants had clinical levels of fatigue at baseline (Qigong=55%, Stretching=45%) using the FACIT-Fatigue scale.
Finally, we do not know what the long-term benefits of Qigong may be as the purpose of this study was to assess acute outcomes of fatigue and distress. Future trials should include longer follow-up periods to assess whether older cancer prostate cancer survivors continue to practice Qigong and are able to effectively manage symptoms of fatigue and distress.
Despite these limitations, our study is the first Qigong RCT that we are aware of to target older prostate cancer survivors and to demonstrate the efficacy of a Qigong intervention for improving fatigue and distress. As mentioned prior, older cancer survivors are a vulnerable group of survivors because they may be experiencing cancer treatment late effects, alongside age related declines in physical functioning and comorbidities [8]. Furthermore, prostate cancer survivors, especially those receiving ADT, are prone to severe fatigue [3, 5]. With the high survival rate and treatment side effects that accompany this disease, prostate cancer survivors are in need of interventions that will help alleviate treatment side effects and contribute to good quality of life into late life. We believe our study findings help support the utilization of Qigong in the supportive cancer care of older prostate cancer survivors for alleviating fatigue and distress. Future, larger definitive randomized controlled trials are needed to confirm these benefits in older prostate cancer survivors of racially/ethnically diverse populations, for longer follow-up periods, and to examine the potential mechanisms.
Acknowledgments
A portion of this manuscript’s preparation was funded by a National Institutes of Health National Center for Complementary and Alternative Medicine (NCCAM) Research Fellowship in Complementary and Alternative Medicine (T-32 AT003378) at the University of North Carolina for the first author (R.A. Campo). The Qigong project was funded by a University of Utah Center on Aging Pilot Award to A.Y. Kinney and by the Huntsman Cancer Foundation. Additional support was provided by the Shared Resources (P30 CA042014) and the Linda B. and Robert B. Wiggins Wellness-Survivorship Center at Huntsman Cancer Institute. This content is solely the responsibility of the authors and does not necessarily represent the official views of the funding and supporting agencies. The authors have no conflicts of interest to report.
References
- 1.Society AC. Cancer Facts & Figures 2010. Atlanta: American Cancer Society; 2010. [Google Scholar]
- 2.Altekruse SFKC, Krapcho M, Neyman N, Aminou R, Waldron W, Ruhl J, Howlader N, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Cronin K, Chen HS, Feuer EJ, Stinchcomb DG, Edwards BK. SEER Cancer Statistics Review. National Cancer Institute; 2009. 2011. [Google Scholar]
- 3.Joly F, Alibhai SM, Galica J, Park A, Yi QL, Wagner L, et al. Impact of androgen deprivation therapy on physical and cognitive function, as well as quality of life of patients with nonmetastatic prostate cancer. J Urol. 2006;176(6 Pt 1):2443–7. doi: 10.1016/j.juro.2006.07.151. S0022-5347(06)01932-X [pii] [DOI] [PubMed] [Google Scholar]
- 4.Rao A, Cohen HJ. Symptom management in the elderly cancer patient: fatigue, pain, and depression. J Natl Cancer Inst Monogr. 2004;(32):150–7. doi: 10.1093/jncimonographs/lgh0312004/32/150. [pii] [DOI] [PubMed] [Google Scholar]
- 5.National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Cancer-Related Fatigue. Verson 1.2013. Fort Washington, PA: National Comprehensive Cancer Network; 2012. [Google Scholar]
- 6.Curt GA, Breitbart W, Cella D, Groopman JE, Horning SJ, Itri LM, et al. Impact of cancer-related fatigue on the lives of patients: new findings from the Fatigue Coalition. Oncologist. 2000;5(5):353–60. doi: 10.1634/theoncologist.5-5-353. [DOI] [PubMed] [Google Scholar]
- 7.Hofman M, Ryan JL, Figueroa-Moseley CD, Jean-Pierre P, Morrow GR. Cancer-related fatigue: the scale of the problem. Oncologist. 2007;12 (Suppl 1):4–10. doi: 10.1634/theoncologist.12-S1-4. [DOI] [PubMed] [Google Scholar]
- 8.Rao AV, Demark-Wahnefried W. The older cancer survivor. Crit Rev Oncol Hematol. 2006;60(2):131–43. doi: 10.1016/j.critrevonc.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 9.Avis NE, Deimling GT. Cancer survivorship and aging. Cancer. 2008;113(12 Suppl):3519–29. doi: 10.1002/cncr.23941. [DOI] [PubMed] [Google Scholar]
- 10.National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Distress Management. 2012. [Google Scholar]
- 11.Ganz PA, Guadagnoli E, Landrum MB, Lash TL, Rakowski W, Silliman RA. Breast cancer in older women: quality of life and psychosocial adjustment in the 15 months after diagnosis. J Clin Oncol. 2003;21(21):4027–33. doi: 10.1200/JCO.2003.08.097. [DOI] [PubMed] [Google Scholar]
- 12.Stanton AL. What happens now? Psychosocial care for cancer survivors after medical treatment completion. J Clin Oncol. 2012;30(11):1215–20. doi: 10.1200/JCO.2011.39.7406. [DOI] [PubMed] [Google Scholar]
- 13.Deimling GT, Bowman KF, Sterns S, Wagner LJ, Kahana B. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology. 2006;15(4):306–20. doi: 10.1002/pon.955. [DOI] [PubMed] [Google Scholar]
- 14.Mustian KM, Sprod LK, Palesh OG, Peppone LJ, Janelsins MC, Mohile SG, et al. Exercise for the management of side effects and quality of life among cancer survivors. Curr Sports Med Rep. 2009;8(6):325–30. doi: 10.1249/JSR.0b013e3181c2232400149619-200911000-00013. [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cramp F, Byron-Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2012;11:CD006145. doi: 10.1002/14651858.CD006145.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Puetz TW, Herring MP. Differential effects of exercise on cancer-related fatigue during and following treatment: a meta-analysis. Am J Prev Med. 2012;43(2):e1–24. doi: 10.1016/j.amepre.2012.04.027. [DOI] [PubMed] [Google Scholar]
- 17.Rogers CE, Larkey LK, Keller C. A review of clinical trials of tai chi and qigong in older adults. West J Nurs Res. 2009;31(2):245–79. doi: 10.1177/0193945908327529. 31/2/245 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larkey L, Jahnke R, Etnier J, Gonzalez J. Meditative movement as a category of exercise: implications for research. J Phys Act Health. 2009;6(2):230–8. doi: 10.1123/jpah.6.2.230. [DOI] [PubMed] [Google Scholar]
- 19.Chan CL, Wang CW, Ho RT, Ng SM, Chan JS, Ziea ET, et al. A systematic review of the effectiveness of qigong exercise in supportive cancer care. Support Care Cancer. 2012;20(6):1121–33. doi: 10.1007/s00520-011-1378-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsang HW, Tsang WW, Jones AY, Fung KM, Chan AH, Chan EP, et al. Psycho-physical and neurophysiological effects of qigong on depressed elders with chronic illness. Aging & mental health. 2013;17(3):336–48. doi: 10.1080/13607863.2012.732035. [DOI] [PubMed] [Google Scholar]
- 21.Chen Z, Meng Z, Milbury K, Bei W, Zhang Y, Thornton B, et al. Qigong improves quality of life in women undergoing radiotherapy for breast cancer: Results of a randomized controlled trial. Cancer. 2013 doi: 10.1002/cncr.27904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg. 2011;9(8):672–7. doi: 10.1016/j.ijsu.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 23.CDC. Fact sheet for health professionals on physical activity guidelines for older adults. Atlanta: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 24.Hussain M, Tangen CM, Higano C, Schelhammer PF, Faulkner J, Crawford ED, et al. Absolute prostate-specific antigen value after androgen deprivation is a strong independent predictor of survival in new metastatic prostate cancer: data from Southwest Oncology Group Trial 9346 (INT-0162) J Clin Oncol. 2006;24(24):3984–90. doi: 10.1200/JCO.2006.06.4246. 24/24/3984 [pii] [DOI] [PubMed] [Google Scholar]
- 25.Schutzer KA, Graves BS. Barriers and motivations to exercise in older adults. Prev Med. 2004;39(5):1056–61. doi: 10.1016/j.ypmed.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 26.Campo RA, O’Connor K, Light KC, Nakamura Y, Lipschitz DL, Lastayo PC, et al. Feasibility and Acceptability of a Tai Chi Chih Randomized Controlled Trial in Senior Female Cancer Survivors. Integr Cancer Ther. 2013 doi: 10.1177/1534735413485418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Galvao DA, Newton RU. Review of exercise intervention studies in cancer patients. J ClinOncol. 2005;23(4):899–909. doi: 10.1200/JCO.2005.06.085. [DOI] [PubMed] [Google Scholar]
- 28.LaStayo PC, Marcus RL, Dibble LE, Smith SB, Beck SL. Eccentric exercise versus usual-care with older cancer survivors: the impact on muscle and mobility--an exploratory pilot study. BMC Geriatr. 2011;11:5. doi: 10.1186/1471-2318-11-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cella D, Lai JS, Chang CH, Peterman A, Slavin M. Fatigue in cancer patients compared with fatigue in the general United States population. Cancer. 2002;94(2):528–38. doi: 10.1002/cncr.10245. [DOI] [PubMed] [Google Scholar]
- 30.Derogatis LR. BSI 18 Brief Symptom Inventory 18, Administration, Scoring, and Procedures Manual. Minneapolis, MN: NCS Pearson, INC; 2000. [Google Scholar]
- 31.Cella D, Yount S, Sorensen M, Chartash E, Sengupta N, Grober J. Validation of the Functional Assessment of Chronic Illness Therapy Fatigue Scale relative to other instrumentation in patients with rheumatoid arthritis. J Rheumatol. 2005;32(5):811–9. 0315162X-32-811 [pii] [PubMed] [Google Scholar]
- 32.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–81. [PubMed] [Google Scholar]
- 33.Khan CM, Stephens MA, Franks MM, Rook KS, Salem JK. Influences of Spousal Support and Control on Diabetes Management Through Physical Activity. Health Psychol. 2012 doi: 10.1037/a0028609. [DOI] [PubMed] [Google Scholar]
- 34.Pettee KK, Brach JS, Kriska AM, Boudreau R, Richardson CR, Colbert LH, et al. Influence of marital status on physical activity levels among older adults. Med Sci Sports Exerc. 2006;38(3):541–6. doi: 10.1249/01.mss.0000191346.95244.f7. [DOI] [PubMed] [Google Scholar]
- 35.Oh B, Butow PN, Mullan BA, Clarke SJ, Beale PJ, Pavlakis N, et al. Effect of medical Qigong on cognitive function, quality of life, and a biomarker of inflammation in cancer patients: a randomized controlled trial. Support Care Cancer. 2012;20(6):1235–42. doi: 10.1007/s00520-011-1209-6. [DOI] [PubMed] [Google Scholar]
- 36.Oh B, Butow P, Mullan B, Clarke S, Beale P, Pavlakis N, et al. Impact of medical Qigong on quality of life, fatigue, mood and inflammation in cancer patients: a randomized controlled trial. Ann Oncol. 2010;21(3):608–14. doi: 10.1093/annonc/mdp479. mdp479 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ho RT, Chan JS, Wang CW, Lau BW, So KF, Yuen LP, et al. A randomized controlled trial of qigong exercise on fatigue symptoms, functioning, and telomerase activity in persons with chronic fatigue or chronic fatigue syndrome. Ann Behav Med. 2012;44(2):160–70. doi: 10.1007/s12160-012-9381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvao DA, Pinto BM, et al. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010;42(7):1409–26. doi: 10.1249/MSS.0b013e3181e0c11200005768-201007000-00023. [pii] [DOI] [PubMed] [Google Scholar]
- 39.Morey MC, Sloane R, Pieper CF, Peterson MJ, Pearson MP, Ekelund CC, et al. Effect of physical activity guidelines on physical function in older adults. J Am Geriatr Soc. 2008;56(10):1873–8. doi: 10.1111/j.1532-5415.2008.01937.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mohr DC, Spring B, Freedland KE, Beckner V, Arean P, Hollon SD, et al. The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychother Psychosom. 2009;78(5):275–84. doi: 10.1159/000228248. [DOI] [PubMed] [Google Scholar]
- 41.Garland SN, Tamagawa R, Todd SC, Speca M, Carlson LE. Increased Mindfulness Is Related to Improved Stress and Mood Following Participation in a Mindfulness-Based Stress Reduction Program in Individuals With Cancer. Integr Cancer Ther. 2012 doi: 10.1177/1534735412442370. [DOI] [PubMed] [Google Scholar]
- 42.Bower JE, Woolery A, Sternlieb B, Garet D. Yoga for cancer patients and survivors. Cancer Control. 2005;12(3):165–71. doi: 10.1177/107327480501200304. [DOI] [PubMed] [Google Scholar]
- 43.Singh AA, Jones LW, Antonelli JA, Gerber L, Calloway EE, Shuler KH, et al. Association between exercise and primary incidence of prostate cancer: does race matter? Cancer. 2013;119(7):1338–43. doi: 10.1002/cncr.27791. [DOI] [PubMed] [Google Scholar]