Abstract
Introduction
Sepsis refers to the host’s deleterious and non-resolving systemic inflammatory response to microbial infections, and represents the leading cause of death in the intensive care unit. The pathogenesis of sepsis is complex, but partly mediated by a newly identified alarmin molecule, the high mobility group box 1 (HMGB1).
Areas covered
Here we review the evidence that support extracellular HMGB1 as a late mediator of experimental sepsis with a wider therapeutic window, and discuss the therapeutic potential of HMGB1-neutralizing antibodies and small molecule inhibitors (herbal components) in experimental sepsis.
Expert opinion
It will be important to evaluate the efficacy of HMGB1-targeting strategies for the clinical management of human sepsis in the future.
Keywords: innate immune cells, cytokines, sepsis, antibodies, HMGB1, herbal component, PKR
1. Introduction
Cohabitating with various microbes, animals have developed multiple strategies to deal with microbial infections. The epithelial barriers serve as the first layer of defense by limiting the access and/or growth of many pathogens. If they are breached, the host’s innate immune system mounts an immediate biological response, termed “inflammation” (“set on fire”, in Greek), to confine and remove the invading pathogens [1]. If successful, the inflammatory process resolves to restore immunologic homeostasis; otherwise the invading pathogens can leak into the blood stream, triggering a widespread, systemic inflammatory response termed “sepsis” (Figure 1). Sepsis refers to the host’s deleterious and non-resolving systemic inflammatory response to microbial infection [2], and represents the leading cause of death in the intensive care unit. As a continuum of increasing clinical severity, “severe sepsis” is often associated with one or more acute organ dysfunctions [3]. Despite recent advances in antibiotic therapy and intensive care, the overall mortality rate of severe sepsis remains high (28.6%) [4], claiming 215,000 lives annually in the U.S. alone. Current therapies for sepsis are still largely supportive and limited to a few clinical interventions including antibiotics, steroidal anti-inflammatory drugs (e.g., hydrocortisone) and early goal directed therapies (EGDT). Unfortunately, these supportive therapies are often ineffective, prompting the on-going search for novel therapeutic strategies for human sepsis. Here we review the accumulating evidence that support the therapeutic potential of several HMGB1-targeting agents in animal models of sepsis.
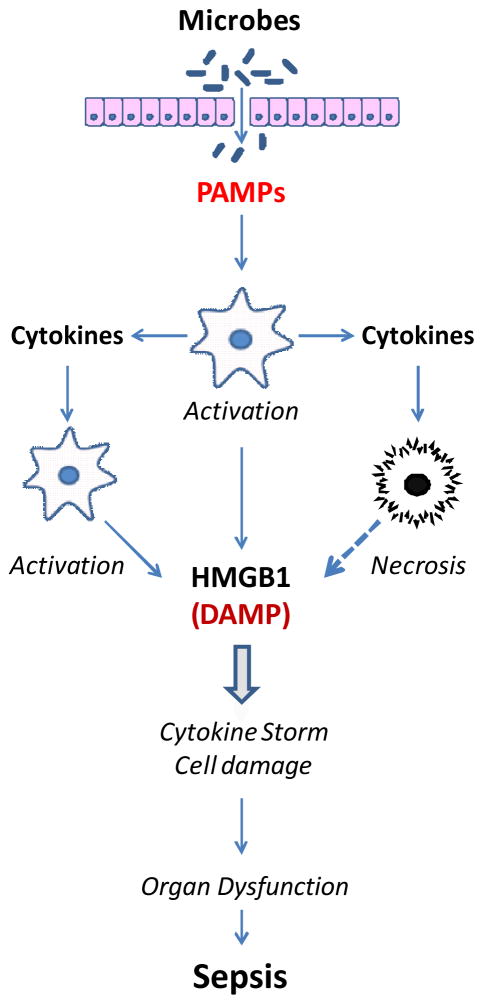
Figure 1. A microbial infection can trigger a systemic inflammatory response.
The disruption of epithelial barrier allows invasion of microbial pathogens, which elicit an innate immune response through liberating pathogen-associated molecular patterns (PAMPs). In immune-compromised hosts, the excessive accumulation of PAMPs causes cytokine storm and accompanying cell injury during the early stage of sepsis. Subsequently, damage-associated molecular patterns (DAMPs, such as HMGB1, mtDNA, and ATP) are released from injured tissue, and further amplify the cytokine storms and cell damages, resulting in organ dysfunction and sepsis.
2. Pathogenesis of Sepsis
The pathogenesis of sepsis is rather complex, but partly attributable to dys-regulated systemic inflammatory responses propagated by innate immune cells including macrophages and monocytes. While continuously patrolling the body to search for invading pathogens or damaged tissues, monocytes immediately infiltrate into the infected/injured tissues upon detecting microbial products (termed pathogen-associated molecular patterns, PAMPs) or damage-associated molecular patterns (DAMPs) [5]. Upon reaching extravascular tissues, these monocytes are differentiated into tissue-specific resident macrophages, which are responsible for ingesting and eliminating invading pathogens in alliance with other phagocytes (e.g., neutrophils) [6].
Additionally, macrophages/monocytes are equipped with receptors [such as the Toll-like receptors (TLRs) TLR2, TLR3, TLR4, and TLR9] [7–11] specific for various PAMPs (e.g., bacterial peptidoglycan, ds-RNA, endotoxin, and CpG-DNA) [12;13]. The engagement of PAMPs with respective receptors triggers the sequential release of early (e.g., TNF, IL-1 and IFN-γ) and late (e.g., HMGB1) proinflammatory mediators (Figure 1) [14–16]. Early mediators, individually or in combination, contribute to the pathogenesis of lethal systemic inflammation. For instance, neutralizing antibodies against an early cytokine, TNF [17], reduce lethality in animal models of endotoxemic/bacteremic shock. However, the early kinetics of systemic TNF accumulation makes it difficult to target in clinical settings [17], prompting a search for other late mediators (e.g., HMGB1) that may offer wider therapeutic windows.
3. HMGB1 as a late mediator of experimental sepsis
HMGB1 is constitutively expressed to maintain a large “pool” of pre-formed protein in the nucleus of most cells [18;19]. It contains two internal repeats of positively charged domains (“HMG boxes” known as “A box” and “B box”) in the N-terminus, and a continuous stretch of negatively charged (aspartic and glutamic acid) residues in the C-terminus. These HMG boxes enable HMGB1 to bind chromosomal DNA, and fulfill its nuclear functions such as maintaining the nucleosomal structure and stability and regulating gene expression [20].
3.1. Active Release
In response to PAMPs (e.g., ds-RNA, CpG-DNA and endotoxin) [16;21], DAMPs (e.g., ATP) [22], or cytokines [e.g., interferon (IFN)-γ] [23], macrophages/monocytes actively release HMGB1 in a dose- and time-dependent manner (Figure 1). Lacking a leader signal sequence, HMGB1 cannot be actively secreted via the classical ER-Golgi secretory pathway [16]. Instead, activated macrophages/monocytes acetylated HMGB1 at the nuclear localization sequences, leading to sequestration of HMGB1 within cytoplasmic vesicles and extracellular release [19;23;24]. Accumulating evidence has suggested an essential role for inflammasome activation in the regulation of LPS/ATP-induced HMGB1 release [22;25], because genetic disruption of key inflammasome components (e.g., caspase 1 or Nalp3) completely impaired the LPS/ATP-induced HMGB1 release. Furthermore, the double-stranded RNA-activated protein kinase R (PKR) functions as the key regulator of the inflammasome activation and HMGB1 release (Figure 2) [22].
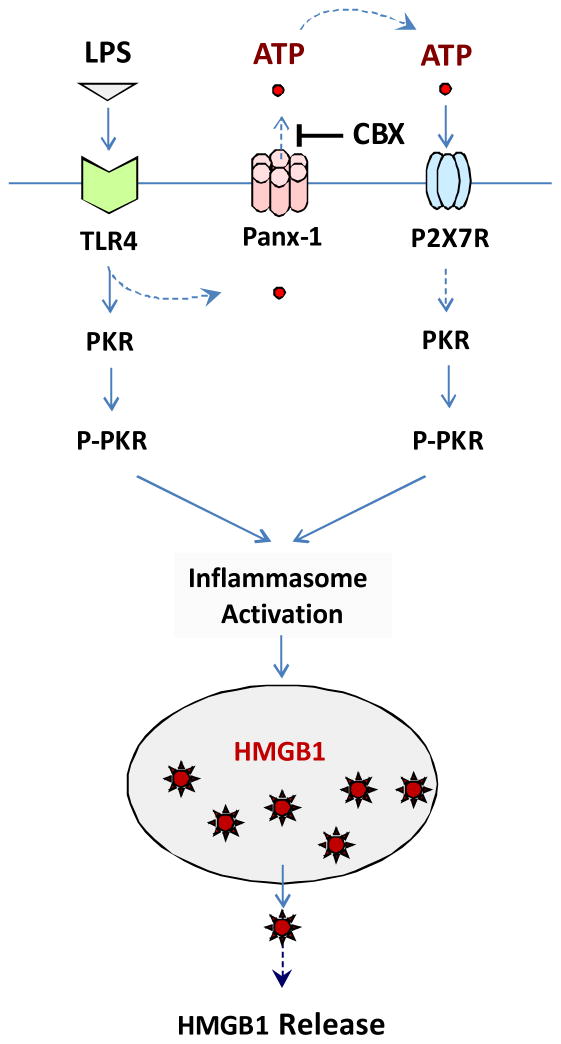
Figure 2. CBX inhibits LPS-induced HMGB1 release by preventing PKR activation.
Prolonged stimulation with crude LPS may lead to panx-1 hemichannel-mediated ATP efflux, and up-regulation of PKR expression. Extracellular ATP then binds to P2X7R and activates the ATP-gated P2X7R and panx-1 channels, leading to PKR phosphorylation and subsequent inflammasome-dependent HMGB1 release. CBX may block LPS-induced ATP efflux through Panx-1, thereby impairing ATP/P2X7R-mediated PKR activation, and subsequent inflammasome-dependent HMGB1 release.
Interestingly, ultra-pure LPS (free from contaminating bacterial proteins and nucleic acids) fails to trigger HMGB1 release unless the initial LPS (10 μg/ml) priming is accompanied by a second stimulus (e.g., ATP) [22;25]. Similarly, ATP itself is unable to induce HMGB1 release without prior LPS exposure [25], even though it can induce PKR phosphorylation [22] and inflammasome activation [26–28]. In contrast, prolonged stimulation with crude LPS (containing trace amounts of bacterial proteins and nucleic acids) triggered dramatic HMGB1 release [16], as well as an up-regulation of PKR expression (> 2-folds) and phosphorylation (> 8-fold) in macrophages. It is plausible that the crude LPS activates inflammasomes initially through triggering the release of ATP, which then binds to the purinergic P2X7 receptor (P2X7R) [29], thereby inducing feed-forwarding ATP release, and subsequent inflammasome activation (Figure 2) [26–28].
3.2. Passive Leakage
In addition, HMGB1 can be passively released from damaged cells [30] following sterile tissue injury resulting from ischemia/reperfusion [31–33], non-penetrating trauma [34–36], or exposure of toxic chemicals to the liver [37–41]. As a DAMP, extracellular HMGB1 passively released by necrotic cells allows innate immune cells to respond to sterile injury (Figure 1) [42;43]. In fact, the sterile tissue injury-elicited systemic inflammatory response syndrome (SIRS) is indistinguishable from microbial infection-induced sepsis [2;44]. Thus, seemingly unrelated conditions such as infection and injury can converge on a common process - inflammation [42], which is orchestrated by HMGB1 and other proinflammatory mediators (e.g., mitochondrial DNA) released both by activated innate immune cells and by damaged tissues [42–45] (Figure 1). Similarly, HMGB1 can be passively released by cells infected by various viruses (e.g., West Nile, Salmon anemia, Dengue, and influenza viruses) [46–48] or mycobacteria [49;50], suggesting HMGB1 as a pathogenic mediator of viral infection-elicited inflammatory diseases [51].
3.3. Extracellular HMGB1 as an alarmin
Once released, extracellular HMGB1 functions as an alarmin signal to alert, recruit, and activate innate immune cells [52;53]. For instance, HMGB1 is capable of stimulating the migration of monocytes, dendritic cells [54;55] and neutrophils [56], functioning as a chemokine to facilitate the recruitment of innate immune cells to the sites of infection or injury [57;58]. Furthermore, HMGB1 binds to various PAMPs (e.g., CpG-DNA or LPS), thereby facilitating their recognition by respective receptors [59], and consequently augmenting the PAMPs-induced inflammatory responses [59]. In addition, HMGB1 can bind to multiple cell surface receptors including RAGE [59], TLR2, TLR4 [60–62], TLR9 [21;59], cluster of differentiation 24 (CD24)/Siglec-10 [63], Mac-1 [56], thrombomodulin [64], as well as single transmembrane domain proteins (e.g., syndecans) [65]. Consequently, it can activate macrophages [60;66–69] and endothelial cells [70;71] to produce proinflammatory cytokines, chemokines, and adhesion molecules.
Intriguingly, recent studies have suggested that chemical modification may affect the cytokine or chemokine activities of HMGB1. For instance, it was shown that reactive oxygen species (ROS) may oxidize HMGB1 to form intra-molecular disulfide bond between thiol group of Cys106 and Cys23 or Cys 45, and consequently abolish HMGB1-mediated immunostimulatory activities [72]. Furthermore, it has been suggested that only the fully reduced (“all-thiol” ) HMGB1 has chemokine-like activities; the Cys23-Cys45 disulfide form has cytokine activities; whereas the fully oxidized HMGB1 lost both chemokine and cytokine activities [73–75]. Considered together, these studies suggest extracellular HMGB1 as an alarmin signal to recruit, alert, and activate innate immune cells, thereby sustaining a potentially injurious inflammatory response during sepsis.
3.4. Pathogenic role of HMGB1 in sepsis
Experimentally, sepsis is routinely induced by several techniques including the infusion of exogenous bacterial toxins (endotoxemia), as well as the disruption of host epithelial barrier to induce microbial translocation (such as the cecal ligation and puncture, CLP). Each model has particular strengths and weaknesses with respect to their ability to mimic the clinical progression of human sepsis [76]. Endotoxemia is generally considered as a model of septic shock, and has been widely used to investigate the roles of various cytokines in lethal systemic inflammation. In contrast, CLP allows bacteria spillage into the peritoneal cavity, mimicking the human clinical conditions of perforated appendicitis or diverticulitis. The severity of sepsis, as reflected by the eventual mortality rates, can be controlled surgically by varying the size of the needle used for cecal puncture. Thus, the CLP model is considered as the most clinically relevant experimental model for human sepsis [77].
In murine models of endotoxemia and CLP-sepsis, HMGB1 is first detected in the circulation eight hours after the disease onset, and subsequently increased to plateau levels from 16 to 32 hours [16;78]. This late appearance of circulating HMGB1 parallels with the onset of animal lethality from endotoxemia or sepsis, and distinguishes itself from TNF and other early proinflammatory cytokines [79]. The pathogenic role of HMGB1 in endotoxemia was inferred from studies using HMGB1-neutralizing antibodies, which conferred a dose-dependent protection against endotoxin-induced tissue injury and lethality [16;80]. In a more clinically relevant animal model of sepsis (induced by CLP), delayed administration of HMGB1-specific neutralizing antibodies beginning 24 h after CLP, dose-dependently rescued rodents from lethal sepsis [78;81;82]. Taken together, these experimental data establish extracellular HMGB1 as a critical late mediator of experimental sepsis, which can be therapeutically targeted within wider therapeutic windows than other early cytokines.
4. Therapeutic potential of HMGB1-inhibiting agents
Currently, there is no effective therapy for the treatment of sepsis, although a number of interventions are routinely employed in clinical settings. For instance, appropriate broad-spectrum antibiotics are often given to patients to facilitate the elimination of bacterial pathogens [3]. However, the disruption of bacteria may be accompanied by the liberation of PAMPs (such as endotoxin or CpG-DNA) that adversely stimulate innate immune cells to produce proinflammatory cytokines. Thus, various anti-inflammatory steroids (such as hydrocortisone, methylprednisolone, dexamethasone, fludrocortisone) are frequently used to modulate the excessive inflammatory response, despite the lack of reproducible efficacy in the treatment of human sepsis [83–85]. As a supportive intervention, the ‘early goal directed therapy’ employs extremely tight control of a number of physiological parameters (such as central venous pressure, mean arterial blood pressure, central venous oxygen saturation, and hematocrit) with discrete, protocol driven interventions of crystalloid fluid, vasopressors, and blood transfusions. It is not yet conclusive whether this simple intervention significantly reduces the mortality of patients with sepsis or septic shock [86;87], prompting the search for HMGB1-targeting agents for the treatment of human sepsis.
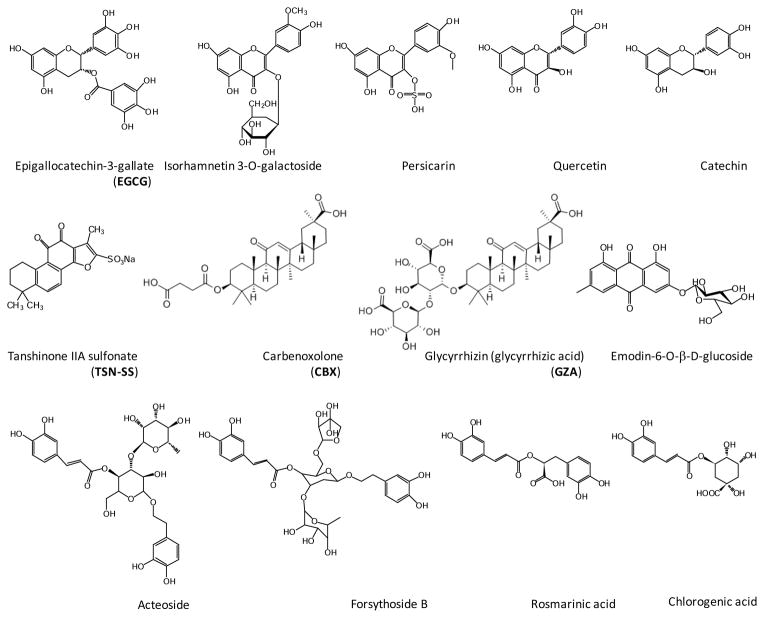
Since our seminal discovery of HMGB1 as a late mediator of lethal endotoxemia [16], a growing list of agents has been tested for activities in inhibiting HMGB1 release, and efficacy for protecting against lethal endotoxemia or sepsis (Table 1). The HMGB1-inhibiting agents range from intravenous immunoglobulin (IVIG) [88], anti-coagulant agents (antithrombin III, thrombomodulin, danaparoid sodium) [64;89], acute phase proteins (e.g., fetuin-A) [90], endogenous hormones (e.g., insulin, vasoactive intestinal peptide, ghrelin) [91;92;92;93], to endogenous small molecules (e.g., acetylcholine, stearoyl lysophosphatidylcholine, glutamine) [18;94–96]. In addition, a number of herbal extracts (e.g., Danggui, Mung bean, and Prunella vulgaris) [97–99] and components (e.g., nicotine, EGCG, tanshinone, glycyrrhizin, chlorogenic acid, Emodin-6-O-β-D-glucoside, Rosmarinic acid, isorhamnetin-3-O-galactoside, Persicarin, Forsythoside B, chloroquine, acteroside ) [100–111] have been proven effective in inhibiting endotoxin-induced HMGB1 release (Figure 3). Nevertheless, various herbal components appear to utilize distinct mechanisms to prevent HMGB1 release by activated macrophages/monocytes. For instance, a major green tea component, EGCG, prevents the LPS-induced HMGB1 release strategically by destroying it in the cytoplasm via a cellular degradation process – autophagy [112]. In contrast, a derivative of tanshinone IIA, TSN-SS selectively inhibits HMGB1 release by facilitating endocytosis of exogenous HMGB1, leading to subsequent degradation via a lysosome-dependent pathway [113]. A pannexin-1 channel blocker, carbenoxolone (CBX), attenuates LPS-induced HMGB1 release by preventing the expression and phosphorylation of PKR, a newly identified regulator of inflammasome activation and HMGB1 release (Figure 2) [22;114].
Table 1.
Potential HMGB1-targeting therapeutic agents.
| Agents | Models of Sepsis | ↓ HMGB1 |
|---|---|---|
|
| ||
| Neutralizing antibodies | Endotoxemia/Sepsis | Activity |
| Anti-coagulant agents | ||
| Anti-thrombin III | Endotoxemia | Release |
| Thrombomodulin | Endotoxemia | Activity |
| Acute phase proteins | ||
| Fetuin-A | Endotoxemia/Sepsis | Release |
| Endogenous hormones | ||
| Insulin | Endotoxemia | Release |
| Vasoactive intestinal peptide | Sepsis | Release |
| Ghrelin | Sepsis | Release |
| Intravenous immunoglobulin | Sepsis | Release |
| Stearoyl lysophosphatidylcholine | Endotoxemia/Sepsis | Release |
| Herbal extract | ||
| Danggui | Endotoxemia/Sepsis | Release |
| Mung bean | Endotoxemia/Sepsis | Release |
| Prunella vulgaris | Sepsis | Release |
| Herbal components | ||
| Nicotine | Endotoxemia/sepsis | Release |
| Danshen (TSN-SS) | Endotoxemia/sepsis | Release/Activity |
| Green tea (EGCG) | Endotoxemia/sepsis | Release/Activity |
| Carbenoxolone | Sepsis | Release |
| heme-oxygenase-1 (HO-1)-derived carbon monoxide (CO) | Endotoxemia/sepsis | Release |
| Chloroquine | Endotoxemia/Sepsis | Release |
| Acteoside, an active phenylethanoid glycoside | Sepsis | Release |
| Glycyrrhizin | Endotoxemia | Release |
| Chlorogenic acid | Endotoxemia/Sepsis | Release |
| Emodin-6-O-β-D-glucoside | Sepsis | Release |
| Rosmarinic acid (RA) | Endotoxemia/Sepsis | Release |
| Isorhamnetin-3-O-galactoside | Endotoxemia/Sepsis | Release |
| Persicarin | Endotoxemia/Sepsis | Release |
| Forsythoside B | Sepsis | Release |
Figure 3.
Chemical structures of HMGB1-inhibiting herbal components.
In light of the capacity of herbal ingredients in preventing endotoxin-induced HMGB1 release, we explored their efficacy in animal models of lethal endotoxemia. Consistent with previous report [115;116], we found that the intraperitoneal administration of EGCG (4.0 mg/kg) at −0.5, +24, and +48 h post onset of endotoxemia significantly improved animal survival from 50% to 76% [101]. To further explore its therapeutic potential, we employed the clinically relevant animal model of CLP-induced sepsis. Given the late and prolonged kinetics of HMGB1 accumulation in experimental sepsis [78], the first dose of EGCG was given 24 h after the onset of sepsis - a time point when mice developed clear signs of sepsis including lethargy, diarrhea, and piloerection. Repetitive intraperitoneal administration of EGCG (at 24, 48, and 72 h post CLP) significantly increased animal survival rates from 53% to 82% [101]. Even when given orally, EGCG still rescued mice from lethal sepsis, significantly increasing animal survival rates from 16% to 44% [112]. As predicted, delayed administration of EGCG did not affect the circulating levels of early cytokines, but significantly attenuated systemic accumulation of HMGB1 [101]. Furthermore, it attenuated circulating levels of IL-6 (by 75%) and KC (by 60%) - two reliable surrogate markers of lethal sepsis [117;118]. Intriguingly, we found that EGCG facilitated bacterial elimination in selective organs (e.g., the liver and lung) in an animal model of sepsis [111]. It is not yet known whether these antibacterial properties are attributable to the possibilities that EGCG directly kill microbes by altering microbial protein conformations and functions [111], or indirectly by modulating macrophage-associated innate immune responses. Considered together, these experimental data indicate that EGCG protects mice against lethal sepsis partly by attenuating systemic HMGB1 accumulation, and partly by facilitating bacterial elimination.
Similarly, repeated administration of CBX or TSN-SS beginning 24 h after the onset of sepsis (followed by additional doses at 48 and 72 h post CLP) conferred a dose-dependent and significant protection against lethal sepsis [102;119], supporting a therapeutic potential for herbal components in experimental sepsis. Furthermore, both CBX and TSN-SS significantly reduced HMGB1 levels not only systemically in the circulation [102], but also locally in the peritoneal lavage fluid, suggesting that CBX and TSN-SS confers protection against lethal sepsis possibly by attenuating local and systemic HMGB1 accumulation. In addition, a growing list of HMGB1 inhibitors has been proven protective by attenuating systemic HMGB1 release or action (Table 1), stimulating further interests in possible future clinical studies.
5. Conclusions
-
5.1
Sepsis is the host’s deleterious and non-resolving systemic inflammatory response to microbial infection, and is partly mediated by various proinflammatory mediators (e.g., HMGB1).
-
5.2
HMGB1 is secreted by activated macrophages/monocytes through complex mechanisms dependent on the activation of PKR and inflammasomes.
-
5.3
HMGB1 can also be passively released by necrotic cells following ischemia-reperfusion, trauma, and injury, thereby functioning as a DMAP molecule to orchestrate the injury-elicited inflammatory responses.
-
5.4
Extracellular HMGB1 functions as an alarmin signal to alert, recruit, and activate innate immune cells, thereby serving as a late mediator of lethal sepsis with a wider therapeutic window.
-
5.5
A number of endogenous macromolecules (e.g., intravenous immunoglobulin, anti-coagulants, acute phase proteins, and hormones) or small molecules (e.g., acetylcholine, stearoyl lysophosphatidylcholine, glutamine) have been found to be effective in inhibiting HMGB1 release, and protecting against lethal endotoxemia or sepsis.
-
5.6
Many herbal components have been proven effective in inhibiting HMGB1 release through divergently distinct mechanisms, ranging from inducing autophagic degradation, stimulating endocytic uptake, to preventing PKR activation.
-
5.7
Many herbal extracts and components have been proven protective in animal models of experimental sepsis.
-
5.8
Unlike neutralizing antibodies, the herbal components may confer protection against lethal sepsis by inhibiting HMGB1 as well as other potential off-targets. For instance, at the doses that completely prevented HMGB1 release, TSN-SS also partially inhibited endotoxin-induced release of nitric oxide, IL-1α (by 50 ± 7%), platelet factor 4 (PF-4, by 35 ± 6%) and MCP-5 (by 25 ± 5%) [102], although it did not affect most other cytokines (e.g., TNF, IL-6, IL-12) and chemokines (e.g., KC, MCP-1, MIP-1α, MIP-2).
6. Expert opinion
For complex systemic inflammatory syndromes, it might be difficult to translate successful animal studies into clinical applications. For instance, various therapeutic strategies against bacterial endotoxin including neutralizing antibodies [120] and binding proteins [121] failed to improve survival in sepsis clinical trials. Similarly, agents blocking endotoxins from binding to the TLR4 receptor (e.g., Eritoran) also did not show benefit in a recent clinical trial [122], raising questions about the feasibility of TLR4-blocking agents in the treatment of human sepsis. Notably, the innate recognition system [consisting of LPS-binding protein (LBP), CD14, and TLR4] is essential for macrophages/monocytes to effectively recognize and respond to minute amounts of endotoxins. If presented at high levels, endotoxins can be internalized into macrophage cytoplasmic compartments, thereby activating the release of inflammasome-dependent cytokines via TLR4-independent signaling pathways [123;124]. Thus, if endotoxins reach critical concentrations during sepsis, aberrant cytoplasmic localization may occur to trigger inflammasome-dependent release of HMGB1 and other pathogenic mediators in TLR4-independent mechanisms. There, it may be important to use detectable endotoxemia as a precondition for enrollment of septic patients in respective TLR4-targeting sepsis trials.
Although neutralizing antibodies against early cytokines (e.g., TNF) [17;125] are protective in animal models of endotoxemia or bacteremia, these agents also failed in sepsis clinical trials [126]. This failure partly reflected the complexity of the underlying pathogenic mechanisms of sepsis, and the consequent heterogeneity of the patient population [1;3]. It may also be attributable to pitfalls in the selection of non-feasible therapeutic targets or non-realistic clinical outcome measures (such as survival rates) [1]. Nevertheless, the investigation of pathogenic cytokines in animal models of diseases has led to the development of successful cytokine-targeting therapeutic strategies. For instance, chimeric anti-TNF monoclonal antibody (infliximab) and a soluble TNF receptors-Fc fusion protein (sTNF-R-Fc, etanercept) have been approved for patients with debilitating chronic inflammatory diseases, such as rheumatoid arthritis (RA) [127]. It is thus necessary and hopeful to continue the search for clinically feasible therapeutic target and drugs for clinical management of human sepsis.
The discovery of HMGB1 as a late mediator of experimental sepsis has stimulated a great interest in developing neutralizing antibodies for clinical management of human sepsis. In the animal model of sepsis, monoclonal antibodies effectively rescued mice from the lethal sequelae even when given 24 h post the onset of sepsis. It is not yet known whether HMGB1 can ever be a clinically feasible therapeutic target for human sepsis until HMGB1-neutralizing antibodies are tested in clinical trials. Humanized anti-HMGB1 antibodies have been commercially developed by MedImmune, but the company has decided not to conduct sepsis clinical trials after strategic merge with AstraZeneca in 2007. In addition to business-related reasons, it may also relate to the frustrating difficulties encountered by the MedImmune while attempting to develop reliable bioassays for screening HMGB1-neutralizing antibodies. Specifically, the cytokine or chemokine activities of recombinant HMGB1 protein were found to be paradoxically unstable. Subsequently, it was discovered that the redox status of HMGB1 protein affected its cytokine- or chemokine-like activities in a dramatically divergent fashion [73–75]. Of course, the failure of previous sepsis trials may have similarly discouraged many investigators from believing that a single therapeutic target will ever be feasible for a complex syndrome like sepsis. Moreover, many investigators believe that some patients with sepsis die from immunosuppression rather than exaggerated inflammation, even though the excessive inflammation may still be a prerequisite of the subsequent immunosuppression. Interestingly, it has been shown that HMGB1 can: i) enhance the regulatory T cell-mediated immunosuppression [128;129]; ii) induce immunological tolerance [72;130;131]; and iii) impair phagocytic elimination of microbes [132;133] and apoptotic cells [134]. Given the relative wider therapeutic window for HMGB1 in experimental sepsis, it is important to pre-determine circulating HMGB1 levels in their circulation before anti-HMGB1 therapy is given to septic patients. Currently, humanized anti-HMGB1 antibodies are being developed by major pharmaceutical companies to treat inflammatory autoimmune diseases (such as lupus). Future clinical studies are expected in the coming years to test the efficacy of HMGB1-neutralizing antibodies in the clinical management of human inflammatory diseases.
Notably, humanized monoclonal antibodies (mAb) are manufactured in low-yield and time-consuming mammalian cells, and are thus tremendously more expensive than developing small molecule chemical drugs. For example, the recommended dose for frequent injections of Humira (TNF mAb) to treat rheumatoid arthritis is 40 mg every two weeks, totaling > 1 gram (> $16,000) per year. It is thus essential to develop cost-effective small molecule drugs for the clinical management of human sepsis. We and others have found a number of small molecules that effectively prevented HMGB1 release, and conferred protection against lethal endotoxemia and sepsis. Extensive pre-clinical toxicology and safety studies are needed before testing these HMGB1 inhibitors for efficacy in clinical studies.
Will any HMGB1 inhibitors also become therapeutic agents for human sepsis? One of the most selective HMGB1 inhibitor, TSN-SS, has already been used in China as a medicine for patients with cardiovascular disorders [135]. Even in septic animals, TSN-SS reduced total peripheral vascular resistance, and yet increased cardiac stroke volume and cardiac output [102]. The dual effects of TSN-SS in attenuating late inflammatory response and improving cardiovascular function make it a promising therapeutic agent for sepsis. The capacity to facilitate endocytic HMGB1 uptake by professional phagocytes may provide basis for the treatment of both infection- and injury-elicited inflammatory diseases. Several lines of evidence have supported the feasibility of developing TSN-SS as potential therapies for human sepsis. These include the lack of drug toxicity in the clinical management of other cardiovascular diseases with TSN-SS; and the effectiveness of TSN-SS in reducing lethality in animal models of sepsis. The advantages of TSN-SS over many other sepsis drugs in development are: 1) fewer side effects are expected, because it has been prescribed in China as a cardiovascular drug for many years; and 2) the low cost of purification of this drug should reduce sepsis therapy costs significantly, enabling treatments to become more accessible. Of course, it is not yet known whether a better protection could be achieved by combinational therapy with several anti-HMGB1 agents. It is thus important to further explore the therapeutic potential of these HMGB1-inhibiting agents in future studies.
Acknowledgments
We are grateful to the peer reviewers for their critical and constructive comments. Work in authors’ laboratory was supported by grants from the National Center of Complementary and Alternative Medicine (NCCAM, R01AT005076) and the National Institute of General Medical Sciences (NIGMS, R01GM063075).
References
- 1.Wang H, Zhu S, Zhou R, et al. Therapeutic potential of HMGB1-targeting agents in sepsis. Expert Rev Mol Med. 2008;10:e32. doi: 10.1017/S1462399408000884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2*.Vincent JL, Opal SM, Marshall JC, et al. Sepsis definitions: time for change. Lancet. 2013;381:774–5. doi: 10.1016/S0140-6736(12)61815-7. These authors proposed a new definition for sepsis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock. Crit Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 4.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Luster AD, Alon R, von Andrian UH. Immune cell migration in inflammation: present and future therapeutic targets. Nat Immunol. 2005;6:1182–90. doi: 10.1038/ni1275. [DOI] [PubMed] [Google Scholar]
- 6.Liles WC. Immunomodulatory approaches to augment phagocyte-mediated host defense for treatment of infectious diseases. Semin Respir Infect. 2001;16:11–17. doi: 10.1053/srin.2001.22724. [DOI] [PubMed] [Google Scholar]
- 7.Ha T, Lu C, Liu L, et al. TLR2 ligands attenuate cardiac dysfunction in polymicrobial sepsis via a phosphoinositide 3-kinase-dependent mechanism. Am J Physiol Heart Circ Physiol. 2010;298:H984–H991. doi: 10.1152/ajpheart.01109.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gao M, Ha T, Zhang X, et al. Toll-like receptor 3 plays a central role in cardiac dysfunction during polymicrobial sepsis. Crit Care Med. 2012;40:2390–9. doi: 10.1097/CCM.0b013e3182535aeb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brightbill HD, Libraty DH, Krutzik SR, et al. Host defense mechanisms triggered by microbial lipoproteins through toll-like receptors. Science. 1999;285:732–6. doi: 10.1126/science.285.5428.732. [DOI] [PubMed] [Google Scholar]
- 10.Poltorak A, He X, Smirnova I, et al. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science. 1998;282:2085–8. doi: 10.1126/science.282.5396.2085. [DOI] [PubMed] [Google Scholar]
- 11.Hemmi H, Takeuchi O, Kawai T, et al. A Toll-like receptor recognizes bacterial DNA. Nature. 2000;408:740–5. doi: 10.1038/35047123. [DOI] [PubMed] [Google Scholar]
- 12.Akira S, Takeda K. Toll-like receptor signalling. Nat Rev Immunol. 2004;4:499–511. doi: 10.1038/nri1391. [DOI] [PubMed] [Google Scholar]
- 13.Baggiolini M, Loetscher P. Chemokines in inflammation and immunity. Immunol Today. 2000;21:418–20. doi: 10.1016/s0167-5699(00)01672-8. [DOI] [PubMed] [Google Scholar]
- 14.Chan ED, Riches DW. IFN-gamma + LPS induction of iNOS is modulated by ERK, JNK/SAPK, and p38(mapk) in a mouse macrophage cell line. Am J Physiol Cell Physiol. 2001;280:C441–C450. doi: 10.1152/ajpcell.2001.280.3.C441. [DOI] [PubMed] [Google Scholar]
- 15.Wizemann TM, Gardner CR, Laskin JD, et al. Production of nitric oxide and peroxynitrite in the lung during acute endotoxemia. J Leukoc Biol. 1994;56:759–68. doi: 10.1002/jlb.56.6.759. [DOI] [PubMed] [Google Scholar]
- 16**.Wang H, Bloom O, Zhang M, et al. HMG-1 as a late mediator of endotoxin lethality in mice. Science. 1999;285:248–51. doi: 10.1126/science.285.5425.248. These authors made the seminal discovery on the important role of extracellular HMG-1 (now called HMGB1) as a late mediator of lethal systemic inflammation. [DOI] [PubMed] [Google Scholar]
- 17**.Tracey KJ, Fong Y, Hesse DG, et al. Anti-cachectin/TNF monoclonal antibodies prevent septic shock during lethal bacteraemia. Nature. 1987;330:662–4. doi: 10.1038/330662a0. These authors first reported a pathogenic role of proinflammatory cytokine in the pathogenesis of lethal infection. [DOI] [PubMed] [Google Scholar]
- 18.Chen G, Li J, Qiang X, et al. Suppression of HMGB1 release by stearoyl lysophosphatidylcholine:an additional mechanism for its therapeutic effects in experimental sepsis. J Lipid Res. 2005;46:623–7. doi: 10.1194/jlr.C400018-JLR200. [DOI] [PubMed] [Google Scholar]
- 19.Bonaldi T, Talamo F, Scaffidi P, et al. Monocytic cells hyperacetylate chromatin protein HMGB1 to redirect it towards secretion. EMBO J. 2003;22:5551–60. doi: 10.1093/emboj/cdg516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bustin M. At the crossroads of necrosis and apoptosis: signaling to multiple cellular targets by HMGB1. Sci STKE. 2002;2002:E39. doi: 10.1126/stke.2002.151.pe39. [DOI] [PubMed] [Google Scholar]
- 21.Ivanov S, Dragoi AM, Wang X, et al. A novel role for HMGB1 in TLR9-mediated inflammatory responses to CpG-DNA. Blood. 2007;110:1970–81. doi: 10.1182/blood-2006-09-044776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22**.Lu B, Nakamura T, Inouye K, et al. Novel role of PKR in inflammasome activation and HMGB1 release. Nature. 2012;488:670–4. doi: 10.1038/nature11290. These authors made a breakthrough progress in uncovering the molecular mechanisms underlying the regulation of HMGB1 release. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23**.Rendon-Mitchell B, Ochani M, Li J, et al. IFN-gamma Induces High Mobility Group Box 1 Protein Release Partly Through a TNF-Dependent Mechanism. J Immunol. 2003;170:3890–7. doi: 10.4049/jimmunol.170.7.3890. These authors first reported the important role of early cytokines in stimulating HMGB1 release. [DOI] [PubMed] [Google Scholar]
- 24.Gardella S, Andrei C, Ferrera D, et al. The nuclear protein HMGB1 is secreted by monocytes via a non-classical, vesicle-mediated secretory pathway. EMBO Rep. 2002;3:955–1001. doi: 10.1093/embo-reports/kvf198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25**.Lamkanfi M, Sarkar A, Vande WL, et al. Inflammasome-dependent release of the alarmin HMGB1 in endotoxemia. J Immunol. 2010;185:4385–92. doi: 10.4049/jimmunol.1000803. These authors first reported the important role of inflammasome in the regulation of endotoxin-induced HMGB1 release. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mehta VB, Hart J, Wewers MD. ATP-stimulated release of interleukin (IL)-1beta and IL-18 requires priming by lipopolysaccharide and is independent of caspase-1 cleavage. J Biol Chem. 2001;276:3820–6. doi: 10.1074/jbc.M006814200. [DOI] [PubMed] [Google Scholar]
- 27.Griffiths RJ, Stam EJ, Downs JT, Otterness IG. ATP induces the release of IL-1 from LPS-primed cells in vivo. J Immunol. 1995;154:2821–8. [PubMed] [Google Scholar]
- 28.Perregaux DG, McNiff P, Laliberte R, et al. ATP acts as an agonist to promote stimulus-induced secretion of IL-1 beta and IL-18 in human blood. J Immunol. 2000;165:4615–23. doi: 10.4049/jimmunol.165.8.4615. [DOI] [PubMed] [Google Scholar]
- 29.Surprenant A, Rassendren F, Kawashima E, et al. The cytolytic P2Z receptor for extracellular ATP identified as a P2X receptor (P2X7) Science. 1996;272:735–8. doi: 10.1126/science.272.5262.735. [DOI] [PubMed] [Google Scholar]
- 30**.Scaffidi P, Misteli T, Bianchi ME. Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Nature. 2002;418:191–5. doi: 10.1038/nature00858. These authors first reported that HMGB1 can be released by damaged cells. [DOI] [PubMed] [Google Scholar]
- 31**.Tsung A, Sahai R, Tanaka H, et al. The nuclear factor HMGB1 mediates hepatic injury after murine liver ischemia-reperfusion. J Exp Med. 2005;201:1135–43. doi: 10.1084/jem.20042614. These authors first reported the extracellular role of HMGB1 as a damage-associated molecular pattern (DAMP) molecule. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qiu J, Nishimura M, Wang Y, et al. Early release of HMGB-1 from neurons after the onset of brain ischemia. J Cereb Blood Flow Metab. 2008;28:927–38. doi: 10.1038/sj.jcbfm.9600582. [DOI] [PubMed] [Google Scholar]
- 33.Andrassy M, Volz HC, Igwe JC, et al. High-mobility group box-1 in ischemia-reperfusion injury of the heart. Circulation. 2008;117:3216–26. doi: 10.1161/CIRCULATIONAHA.108.769331. [DOI] [PubMed] [Google Scholar]
- 34.Cohen MJ, Brohi K, Calfee CS, et al. Early release of high mobility group box nuclear protein 1 after severe trauma in humans: role of injury severity and tissue hypoperfusion. Crit Care. 2009;13:R174. doi: 10.1186/cc8152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peltz ED, Moore EE, Eckels PC, et al. HMGB1 is markedly elevated within 6 hours of mechanical trauma in humans. Shock. 2009;32:17–22. doi: 10.1097/shk.0b013e3181997173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Manganelli V, Signore M, Pacini I, et al. Increased HMGB1 expression and release by mononuclear cells following surgical/anesthesia trauma. Crit Care. 2010;14:R197. doi: 10.1186/cc9316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhou RR, Liu HB, Peng JP, et al. High mobility group box chromosomal protein 1 in acute-on-chronic liver failure patients and mice with ConA-induced acute liver injury. Exp Mol Pathol. 2012;93:213–9. doi: 10.1016/j.yexmp.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 38.Takano K, Shinoda M, Tanabe M, et al. Protective effect of high-mobility group box 1 blockade on acute liver failure in rats. Shock. 2010;34:573–9. doi: 10.1097/SHK.0b013e3181df0433. [DOI] [PubMed] [Google Scholar]
- 39.Yang R, Zhang S, Cotoia A, et al. High mobility group B1 impairs hepatocyte regeneration in acetaminophen hepatotoxicity. BMC Gastroenterol. 2012;12:45. doi: 10.1186/1471-230X-12-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Antoine DJ, Dear JW, Lewis PS, et al. Mechanistic biomarkers provide early and sensitive detection of acetaminophen-induced acute liver injury at first presentation to hospital. Hepatology. 2013;58:777–87. doi: 10.1002/hep.26294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Seo YS, Kwon JH, Yaqoob U, et al. HMGB1 recruits hepatic stellate cells and liver endothelial cells to sites of ethanol induced parenchymal cell injury. Am J Physiol Gastrointest Liver Physiol. 2013 doi: 10.1152/ajpgi.00151.2013. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Andersson U, Tracey KJ. HMGB1 is a therapeutic target for sterile inflammation and infection. Annu Rev Immunol. 2011;29:139–62. doi: 10.1146/annurev-immunol-030409-101323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhu S, Li W, Ward MF, et al. High mobility group box 1 protein as a potential drug target for infection- and injury-elicited inflammation. Inflamm Allergy Drug Targets. 2010;9:60–72. doi: 10.2174/187152810791292872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sursal T, Stearns-Kurosawa DJ, Itagaki K, et al. Plasma bacterial and mitochondrial DNA distinguish bacterial sepsis from sterile systemic inflammatory response syndrome and quantify inflammatory tissue injury in nonhuman primates. Shock. 2013;39:55–62. doi: 10.1097/SHK.0b013e318276f4ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45**.Zhang Q, Raoof M, Chen Y, et al. Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature. 2010;464:104–7. doi: 10.1038/nature08780. These authors first reported mtDNA functions as a DAMP molecule that orchestrate injury-elicited inflammatory responses. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46**.Chen LC, Yeh TM, Wu HN, et al. Dengue virus infection induces passive release of high mobility group box 1 protein by epithelial cells. J Infect. 2008;56:143–50. doi: 10.1016/j.jinf.2007.10.008. These authors first reported the passive release of HMGB1 from virus infected cells. [DOI] [PubMed] [Google Scholar]
- 47.Alleva LM, Budd AC, Clark IA. Systemic release of high mobility group box 1 protein during severe murine influenza. J Immunol. 2008;181:1454–9. doi: 10.4049/jimmunol.181.2.1454. [DOI] [PubMed] [Google Scholar]
- 48.Whilding LM, Archibald KM, Kulbe H, et al. Vaccinia Virus Induces Programmed Necrosis in Ovarian Cancer Cells. Mol Ther. 2013;10 doi: 10.1038/mt.2013.195. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hofner P, Seprenyi G, Miczak A, et al. High mobility group box 1 protein induction by Mycobacterium bovis BCG. Mediators Inflamm. 2007;2007:53805. doi: 10.1155/2007/53805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grover A, Taylor J, Troudt J, et al. Mycobacterial infection induces the secretion of high-mobility group box 1 protein. Cell Microbiol. 2008;10:1390–404. doi: 10.1111/j.1462-5822.2008.01135.x. [DOI] [PubMed] [Google Scholar]
- 51.Wang H, Ward MF, Fan XG, et al. Potential role of high mobility group box 1 in viral infectious diseases. Viral Immunol. 2006;19:3–9. doi: 10.1089/vim.2006.19.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhu S, Ashok M, Li J, et al. Spermine protects mice against lethal sepsis partly by attenuating surrogate inflammatory markers. Mol Med. 2009;15:275–282. doi: 10.2119/molmed.2009.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53**.Andersson U, Wang H, Palmblad K, et al. High Mobility Group 1 Protein (HMG-1) Stimulates Proinflammatory Cytokine Synthesis in Human Monocytes. J Exp Med. 2000;192:565–70. doi: 10.1084/jem.192.4.565. These authors first reported the proinflammatory activities of extracellular HMGB1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54**.Yang D, Chen Q, Yang H, et al. High mobility group box-1 protein induces the migration and activation of human dendritic cells and acts as an alarmin. J Leukoc Biol. 2007;81:59–66. doi: 10.1189/jlb.0306180. These authors first reported the chemokine activities of extracellular HMGB1. [DOI] [PubMed] [Google Scholar]
- 55.Dumitriu IE, Bianchi ME, Bacci M, et al. The secretion of HMGB1 is required for the migration of maturing dendritic cells. J Leukoc Biol. 2007;81:84–91. doi: 10.1189/jlb.0306171. [DOI] [PubMed] [Google Scholar]
- 56.Orlova VV, Choi EY, Xie C, et al. A novel pathway of HMGB1-mediated inflammatory cell recruitment that requires Mac-1-integrin. EMBO J. 2007;26:1129–1139. doi: 10.1038/sj.emboj.7601552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Degryse B, Bonaldi T, Scaffidi P, et al. The high mobility group (HMG) boxes of the nuclear protein HMG1 induce chemotaxis and cytoskeleton reorganization in rat smooth muscle cells. J Cell Biol. 2001;152:1197–1206. doi: 10.1083/jcb.152.6.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Degryse B, de Virgilio M. The nuclear protein HMGB1, a new kind of chemokine? FEBS Lett. 2003;553:11–17. doi: 10.1016/s0014-5793(03)01027-5. [DOI] [PubMed] [Google Scholar]
- 59**.Tian J, Avalos AM, Mao SY, et al. Toll-like receptor 9-dependent activation by DNA-containing immune complexes is mediated by HMGB1 and RAGE. Nat Immunol. 2007;8:487–496. doi: 10.1038/ni1457. These authors first reported that HMGB1 amplified inflammation by facilitating innate recognition of microbial CpG-DNA. [DOI] [PubMed] [Google Scholar]
- 60.Yu M, Wang H, Ding A, et al. HMGB1 signals through Toll-like receptor (TLR) 4 and TLR2. Shock. 2006;26:174–9. doi: 10.1097/01.shk.0000225404.51320.82. [DOI] [PubMed] [Google Scholar]
- 61.Ha T, Xia Y, Liu X, et al. Glucan phosphate attenuates myocardial HMGB1 translocation in severe sepsis through inhibiting NF-kappaB activation. Am J Physiol Heart Circ Physiol. 2011;301:H848–55. doi: 10.1152/ajpheart.01007.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xiang M, Shi X, Li Y, et al. Hemorrhagic shock activation of NLRP3 inflammasome in lung endothelial cells. J Immunol. 2011;187:4809–17. doi: 10.4049/jimmunol.1102093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63**.Chen GY, Tang J, Zheng P, Liu Y. CD24 and Siglec-10 selectively repress tissue damage-induced immune responses. Science. 2009;323:1722–5. doi: 10.1126/science.1168988. These authors first reported CD24 as another potential cell surface receptor for HMGB1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64**.Abeyama K, Stern DM, Ito Y, et al. The N-terminal domain of thrombomodulin sequesters high-mobility group-B1 protein, a novel antiinflammatory mechanism. J Clin Invest. 2005;115:1267–74. doi: 10.1172/JCI22782. These authors first reported the presence of endogenous HMGB1-binding protein that functions as HMGB1-inhibiting agent. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65**.Salmivirta M, Rauvala H, Elenius K, et al. Neurite growth-promoting protein (amphoterin, p30) binds syndecan. Exp Cell Res. 1992;200:444–51. doi: 10.1016/0014-4827(92)90194-d. These authors first reported the presence of HMGB1 outside of the nucleus (on the cytoplasmic membrane) [DOI] [PubMed] [Google Scholar]
- 66.Park JS, Svetkauskaite D, He Q, et al. Involvement of TLR 2 and TLR 4 in cellular activation by high mobility group box 1 protein (HMGB1) J Biol Chem. 2004;279:7370–7. doi: 10.1074/jbc.M306793200. [DOI] [PubMed] [Google Scholar]
- 67.Park JS, Gamboni-Robertson F, He Q, et al. High mobility group box 1 protein interacts with multiple Toll-like receptors. Am J Physiol Cell Physiol. 2006;290:C917–C924. doi: 10.1152/ajpcell.00401.2005. [DOI] [PubMed] [Google Scholar]
- 68.Kokkola R, Andersson A, Mullins G, et al. RAGE is the Major Receptor for the Proinflammatory Activity of HMGB1 in Rodent Macrophages. Scand J Immunol. 2005;61:1–9. doi: 10.1111/j.0300-9475.2005.01534.x. [DOI] [PubMed] [Google Scholar]
- 69.Pedrazzi M, Patrone M, Passalacqua M, et al. Selective proinflammatory activation of astrocytes by high-mobility group box 1 protein signaling. J Immunol. 2007;179:8525–32. doi: 10.4049/jimmunol.179.12.8525. [DOI] [PubMed] [Google Scholar]
- 70.Fiuza C, Bustin M, Talwar S, et al. Inflammation-promoting activity of HMGB1 on human microvascular endothelial cells. Blood. 2003;101:2652–60. doi: 10.1182/blood-2002-05-1300. [DOI] [PubMed] [Google Scholar]
- 71**.Treutiger CJ, Mullins GE, Johansson AS, et al. High mobility group 1 B-box mediates activation of human endothelium. J Intern Med. 2003;254:375–85. doi: 10.1046/j.1365-2796.2003.01204.x. These authors first reported that HMGB1 activates non-immune cells. [DOI] [PubMed] [Google Scholar]
- 72.Kazama H, Ricci JE, Herndon JM, et al. Induction of immunological tolerance by apoptotic cells requires caspase-dependent oxidation of high-mobility group box-1 protein. Immunity. 2008;29:21–32. doi: 10.1016/j.immuni.2008.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yang H, Lundback P, Ottosson L, et al. Redox modification of cysteine residues regulates the cytokine activity of high mobility group box-1 (HMGB1) Mol Med. 2012;18:250–9. doi: 10.2119/molmed.2011.00389. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 74**.Venereau E, Casalgrandi M, Schiraldi M, et al. Mutually exclusive redox forms of HMGB1 promote cell recruitment or proinflammatory cytokine release. J Exp Med. 2012;209:1519–28. doi: 10.1084/jem.20120189. These authors further examined the effects of the redox status of HMGB1 affects its cytokine activities. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tang D, Billiar TR, Lotze MT. A Janus tale of two active high mobility group box 1 (HMGB1) redox states. Mol Med. 2012;20;18:1360–2. doi: 10.2119/molmed.2012.00314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wichterman KA, Baue AE, Chaudry IH. Sepsis and septic shock--a review of laboratory models and a proposal. J Surg Res. 1980;29:189–201. doi: 10.1016/0022-4804(80)90037-2. [DOI] [PubMed] [Google Scholar]
- 77.Li W, Zhu S, Zhang Y, et al. Use of animal model of sepsis to evaluate novel herbal therapies. J Vis Exp. 2012:3926. doi: 10.3791/3926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78**.Yang H, Ochani M, Li J, et al. Reversing established sepsis with antagonists of endogenous high-mobility group box 1. Proc Natl Acad Sci U S A. 2004;101:296–301. doi: 10.1073/pnas.2434651100. These authors first reported the extracellular role of HMGB1 as a late mediator of lethal sepsis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang H, Yang H, Czura CJ, et al. HMGB1 as a Late Mediator of Lethal Systemic Inflammation. Am J Respir Crit Care Med. 2001;164:1768–73. doi: 10.1164/ajrccm.164.10.2106117. [DOI] [PubMed] [Google Scholar]
- 80.Abraham E, Arcaroli J, Carmody A, et al. HMG-1 as a mediator of acute lung inflammation. J Immunol. 2000;165:2950–4. doi: 10.4049/jimmunol.165.6.2950. [DOI] [PubMed] [Google Scholar]
- 81.Qin S, Wang H, Yuan R, et al. Role of HMGB1 in apoptosis-mediated sepsis lethality. J Exp Med. 2006;203:1637–42. doi: 10.1084/jem.20052203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Suda K, Kitagawa Y, Ozawa S, et al. Anti-high-mobility group box chromosomal protein 1 antibodies improve survival of rats with sepsis. World J Surg. 2006;30:1755–62. doi: 10.1007/s00268-005-0369-2. [DOI] [PubMed] [Google Scholar]
- 83.Lefering R, Neugebauer EA. Steroid controversy in sepsis and septic shock: a meta-analysis. Crit Care Med. 1995;23:1294–303. doi: 10.1097/00003246-199507000-00021. [DOI] [PubMed] [Google Scholar]
- 84.Annane D, Sebille V, Charpentier C, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA. 2002;288:862–71. doi: 10.1001/jama.288.7.862. [DOI] [PubMed] [Google Scholar]
- 85.Sprung CL, Annane D, Keh D, et al. Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008;358:111–24. doi: 10.1056/NEJMoa071366. [DOI] [PubMed] [Google Scholar]
- 86.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 345:1368–77. doi: 10.1056/NEJMoa010307. 200. [DOI] [PubMed] [Google Scholar]
- 87.Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 358:877–87. doi: 10.1056/NEJMoa067373. 200. [DOI] [PubMed] [Google Scholar]
- 88.Hagiwara S, Iwasaka H, Hasegawa A, et al. High-dose intravenous immunoglobulin G improves systemic inflammation in a rat model of CLP-induced sepsis. Intensive Care Med. 2008;34:1812–9. doi: 10.1007/s00134-008-1161-1. [DOI] [PubMed] [Google Scholar]
- 89.Hagiwara S, Iwasaka H, Matsumoto S, Noguchi T. High dose antithrombin III inhibits HMGB1 and improves endotoxin-induced acute lung injury in rats. Intensive Care Med. 2008;34:361–7. doi: 10.1007/s00134-007-0887-5. [DOI] [PubMed] [Google Scholar]
- 90.Li W, Zhu S, Li J, et al. A hepatic protein, fetuin-A, occupies a protective role in lethal systemic inflammation. PLoS ONE. 2011;6:e16945. doi: 10.1371/journal.pone.0016945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hagiwara S, Iwasaka H, Hasegawa A, et al. Effects of hyperglycemia and insulin therapy on high mobility group box 1 in endotoxin-induced acute lung injury in a rat model. Crit Care Med. 2008;36:2407–13. doi: 10.1097/CCM.0b013e318180b3ba. [DOI] [PubMed] [Google Scholar]
- 92.Chorny A, Delgado M. Neuropeptides rescue mice from lethal sepsis by down-regulating secretion of the late-acting inflammatory mediator high mobility group box 1. Am J Pathol. 2008;172:1297–307. doi: 10.2353/ajpath.2008.070969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chorny A, Anderson P, Gonzalez-Rey E, Delgado M. Ghrelin Protects against Experimental Sepsis by Inhibiting High-Mobility Group Box 1 Release and by Killing Bacteria. J Immunol. 2008;180:8369–8377. doi: 10.4049/jimmunol.180.12.8369. [DOI] [PubMed] [Google Scholar]
- 94.Wang H, Yu M, Ochani M, et al. Nicotinic acetylcholine receptor alpha7 subunit is an essential regulator of inflammation. Nature. 2003;421:384–388. doi: 10.1038/nature01339. [DOI] [PubMed] [Google Scholar]
- 95.Wang H, Czura CJ, Tracey KJ. Lipid unites disparate syndromes of sepsis. Nat Med. 2004;10:124–125. doi: 10.1038/nm0204-124. [DOI] [PubMed] [Google Scholar]
- 96.Hu YM, Pai MH, Yeh CL, et al. Glutamine administration ameliorates sepsis-induced kidney injury by downregulating the high-mobility group box protein-1-mediated pathway in mice. Am J Physiol Renal Physiol. 2012;302:F150–F158. doi: 10.1152/ajprenal.00246.2011. [DOI] [PubMed] [Google Scholar]
- 97**.Wang H, Li W, Li J, et al. The aqueous extract of a popular herbal nutrient supplement, Angelica sinensis, protects mice against lethal endotoxemia and sepsis. J Nutr. 2006;136:360–365. doi: 10.1093/jn/136.2.360. This is the first report showing that herbal extract inhibited HMGB1 release and protected against lethal sepsis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhu S, Li W, Li J, et al. It Is Not Just Folklore: The Aqueous Extract of Mung Bean Coat Is Protective against Sepsis. Evid Based Complement Alternat Med. 2012;2012:498467. doi: 10.1155/2012/498467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jun MS, Kim HS, Kim YM, et al. Ethanol extract of Prunella vulgaris var. lilacina inhibits HMGB1 release by induction of heme oxygenase-1 in LPS-activated RAW 264. 7 cells and CLP-induced septic mice. Phytother Res. 2012;26:605–12. doi: 10.1002/ptr.3613. [DOI] [PubMed] [Google Scholar]
- 100.Wang H, Liao H, Ochani M, et al. Cholinergic agonists inhibit HMGB1 release and improve survival in experimental sepsis. Nat Med. 2004;10:1216–21. doi: 10.1038/nm1124. [DOI] [PubMed] [Google Scholar]
- 101.Li W, Ashok M, Li J, et al. A Major Ingredient of Green Tea Rescues Mice from Lethal Sepsis Partly by Inhibiting HMGB1. PLoS ONE. 2007;2:e1153. doi: 10.1371/journal.pone.0001153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Li W, Li J, Ashok M, et al. A cardiovascular drug rescues mice from lethal sepsis by selectively attenuating a late-acting proinflammatory mediator, high mobility group box 1. J Immunol. 2007;178:3856–64. doi: 10.4049/jimmunol.178.6.3856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wang W, Zhao F, Fang Y, et al. Glycyrrhizin protects against porcine endotoxemia through modulation of systemic inflammatory response. Crit Care. 2013;17:R44. doi: 10.1186/cc12558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lee CH, Yoon SJ, Lee SM. Chlorogenic acid attenuates high mobility group box 1 (HMGB1) and enhances host defense mechanisms in murine sepsis. Mol Med. 2013;18:1437–48. doi: 10.2119/molmed.2012.00279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lee W, Ku SK, Kim TH, Bae JS. Emodin-6-O-beta-D-glucoside inhibits HMGB1-induced inflammatory responses in vitro and in vivo. Food Chem Toxicol. 2013;52:97–104. doi: 10.1016/j.fct.2012.10.061. [DOI] [PubMed] [Google Scholar]
- 106.Yang EJ, Ku SK, Lee W, et al. Barrier protective effects of rosmarinic acid on HMGB1-induced inflammatory responses in vitro and in vivo. J Cell Physiol. 2013;228:975–82. doi: 10.1002/jcp.24243. [DOI] [PubMed] [Google Scholar]
- 107.Kim TH, Ku SK, Bae JS. Anti-inflammatory activities of isorhamnetin-3-O-galactoside against HMGB1-induced inflammatory responses in both HUVECs and CLP-induced septic mice. J Cell Biochem. 2013;114:336–45. doi: 10.1002/jcb.24361. [DOI] [PubMed] [Google Scholar]
- 108.Kim TH, Ku SK, Bae JS. Persicarin is anti-inflammatory mediator against HMGB1-induced inflammatory responses in HUVECs and in CLP-induced sepsis mice. J Cell Physiol. 2013;228:696–703. doi: 10.1002/jcp.24214. [DOI] [PubMed] [Google Scholar]
- 109.Jiang WL, Yong X, Zhang SP, et al. Forsythoside B protects against experimental sepsis by modulating inflammatory factors. Phytother Res. 2012;26:981–7. doi: 10.1002/ptr.3668. [DOI] [PubMed] [Google Scholar]
- 110.Yang M, Cao L, Xie M, et al. Chloroquine inhibits HMGB1 inflammatory signaling and protects mice from lethal sepsis. Biochem Pharmacol. 2013;10 doi: 10.1016/j.bcp.2013.05.013. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Seo ES, Oh BK, Pak JH, et al. Acteoside improves survival in cecal ligation and puncture-induced septic mice via blocking of high mobility group box 1 release. Mol Cells. 2013;35:348–54. doi: 10.1007/s10059-013-0021-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Li W, Zhu S, Li J, et al. EGCG stimulates autophagy and reduces cytoplasmic HMGB1 levels in endotoxin-stimulated macrophages. Biochem Pharmacol. 2011;81:1152–63. doi: 10.1016/j.bcp.2011.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zhang Y, Li W, Zhu S, et al. Tanshinone IIA sodium sulfonate facilitates endocytic HMGB1 uptake. Biochem Pharmacol. 2012;84:1492–500. doi: 10.1016/j.bcp.2012.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lu B, Wang H, Andersson U, et al. Regulation of HMGB1 release by inflammasomes. Protein Cell. 2013;4:163–7. doi: 10.1007/s13238-012-2118-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Yang F, de Villiers WJ, McClain CJ, Varilek GW. Green tea polyphenols block endotoxin-induced tumor necrosis factor-production and lethality in a murine model. J Nutr. 1998;128:2334–40. doi: 10.1093/jn/128.12.2334. [DOI] [PubMed] [Google Scholar]
- 116.Ichikawa D, Matsui A, Imai M, et al. Effect of various catechins on the IL-12p40 production by murine peritoneal macrophages and a macrophage cell line, J774. 1. Biol Pharm Bull. 2004;27:1353–8. doi: 10.1248/bpb.27.1353. [DOI] [PubMed] [Google Scholar]
- 117.Osuchowski MF, Welch K, Siddiqui J, Remick DG. Circulating cytokine/inhibitor profiles reshape the understanding of the SIRS/CARS continuum in sepsis and predict mortality. J Immunol. 2006;177:1967–74. doi: 10.4049/jimmunol.177.3.1967. [DOI] [PubMed] [Google Scholar]
- 118.Heuer JG, Sharma GR, Gerlitz B, et al. Evaluation of protein C and other biomarkers as predictors of mortality in a rat cecal ligation and puncture model of sepsis. Crit Care Med. 2004;32:1570–8. doi: 10.1097/01.ccm.0000129488.54282.1a. [DOI] [PubMed] [Google Scholar]
- 119.Li W, Li J, Sama AE, et al. Carbenoxolone Blocks Endotoxin-Induced Protein Kinase R (PKR) Activation and High Mobility Group Box 1 (HMGB1) Release. Mol Med. 2013;19:203–11. doi: 10.2119/molmed.2013.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ziegler EJ, Fisher CJ, Jr, Sprung CL, et al. Treatment of gram-negative bacteremia and septic shock with HA-1A human monoclonal antibody against endotoxin. A randomized, double-blind, placebo-controlled trial. The HA-1A Sepsis Study Group. N Engl J Med. 1991;324:429–436. doi: 10.1056/NEJM199102143240701. [DOI] [PubMed] [Google Scholar]
- 121.Levin M, Quint PA, Goldstein B, et al. Recombinant bactericidal/permeability-increasing protein (rBPI21) as adjunctive treatment for children with severe meningococcal sepsis: a randomised trial. rBPI21 Meningococcal Sepsis Study Group. Lancet. 2000;356:961–7. doi: 10.1016/s0140-6736(00)02712-4. [DOI] [PubMed] [Google Scholar]
- 122.Opal SM, Laterre PF, Francois B, et al. Effect of eritoran, an antagonist of MD2-TLR4, on mortality in patients with severe sepsis: the ACCESS randomized trial. JAMA. 2013;309:1154–62. doi: 10.1001/jama.2013.2194. [DOI] [PubMed] [Google Scholar]
- 123**.Hagar JA, Powell DA, Aachoui Y, et al. Cytoplasmic LPS activates caspase-11: implications in TLR4-independent endotoxic shock. Science. 2013;341:1250–3. doi: 10.1126/science.1240988. These authors first reported a TLR4-independent cytoplasmic signaling pathway for endotoxin-mediated inflammasome activation and cytokine release. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124**.Kayagaki N, Wong MT, Stowe IB, et al. Noncanonical inflammasome activation by intracellular LPS independent of TLR4. Science. 2013;341:1246–9. doi: 10.1126/science.1240248. These authors first reported a cytoplasmic signaling pathway involved in endotoxin-mediated inflammasome activation and cytokine release. [DOI] [PubMed] [Google Scholar]
- 125**.Beutler B, Milsark IW, Cerami AC. Passive immunization against cachectin/tumor necrosis factor protects mice from lethal effect of endotoxin. Science. 1985;229:869–71. doi: 10.1126/science.3895437. These authors first reported a pathogenic role of TNF in lethal endotoxemia. [DOI] [PubMed] [Google Scholar]
- 126.Abraham E, Wunderink R, Silverman H, et al. Efficacy and safety of monoclonal antibody to human tumor necrosis factor alpha in patients with sepsis syndrome. A randomized, controlled, double-blind, multicenter clinical trial. TNF-alpha MAb Sepsis Study Group. JAMA. 1995;273:934–41. [PubMed] [Google Scholar]
- 127.Feldmann M, Maini RN. Anti-TNF alpha therapy of rheumatoid arthritis: what have we learned? Annu Rev Immunol. 2001;19:163–96. doi: 10.1146/annurev.immunol.19.1.163. [DOI] [PubMed] [Google Scholar]
- 128.Zhang Y, Yao YM, Huang LF, et al. The potential effect and mechanism of high-mobility group box 1 protein on regulatory T cell-mediated immunosuppression. J Interferon Cytokine Res. 2011;31:249–57. doi: 10.1089/jir.2010.0019. [DOI] [PubMed] [Google Scholar]
- 129.Wild CA, Bergmann C, Fritz G, et al. HMGB1 conveys immunosuppressive characteristics on regulatory and conventional T cells. Int Immunol. 2012;24:485–494. doi: 10.1093/intimm/dxs051. [DOI] [PubMed] [Google Scholar]
- 130.Aneja RK, Tsung A, Sjodin H, et al. Preconditioning with high mobility group box 1 (HMGB1) induces lipopolysaccharide (LPS) tolerance. J Leukoc Biol. 2008;84:1326–34. doi: 10.1189/jlb.0108030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Robert SM, Sjodin H, Fink MP, et al. Preconditioning with high mobility group box 1 (HMGB1) induces lipoteichoic acid (LTA) tolerance. J Immunother. 2010;33:663–71. doi: 10.1097/CJI.0b013e3181dcd111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132**.Entezari M, Weiss DJ, Sitapara R, et al. Inhibition of high-mobility group box 1 protein (HMGB1) enhances bacterial clearance and protects against Pseudomonas Aeruginosa pneumonia in cystic fibrosis. Mol Med. 2012;18:477–85. doi: 10.2119/molmed.2012.00024. These author first reported the extracellular role of HMGB1 in the impairment of bacterial elimination by macrophages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Patel VS, Sitapara RA, Gore A, et al. High Mobility Group Box-1 mediates hyperoxia-induced impairment of Pseudomonas aeruginosa clearance and inflammatory lung injury in mice. Am J Respir Cell Mol Biol. 2013;48:280–7. doi: 10.1165/rcmb.2012-0279OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Liu G, Wang J, Park YJ, et al. High mobility group protein-1 inhibits phagocytosis of apoptotic neutrophils through binding to phosphatidylserine. J Immunol. 2008;181:4240–6. doi: 10.4049/jimmunol.181.6.4240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ji XY, Tan BK, Zhu YZ. Salvia miltiorrhiza and ischemic diseases. Acta Pharmacol Sin. 2000;21:1089–94. [PubMed] [Google Scholar]