Abstract
Black-pigmented sputum, also called “melanoptysis,” is a symptom that may be observed in certain pathologies such us coal workers’ pneumoconiosis (anthracosis). The cavitation and liquefaction of a fibrosed mass by an infectious process (tuberculosis, infections by anaerobes, etc.) or by ischemic necrosis may cause expectoration of a blackish secretion. We report the case of a patient with labor precedents as a coal worker, from whom abundant black sputum was obtained in the course of an incidental expectoration. Cyto-histological findings are shown and a differential diagnosis is established.
Keywords: Anthracosis, black-pigmented sputum, melanoptysis
Black-pigmented sputum, also called “melanoptysis,” is a symptom that may be observed in certain pathologies such us coal workers’ pneumoconiosis (anthracosis),[1] a professional lung disease caused by inhalation of coal dust that is then deposited on the pulmonary parenchyma. Progressive deposit of this material causes pigmented nodular lesions formed by loaded macrophages with anthracotic material, and conjunctive tissue. In the course of the disease, the nodules tend to come together and produce masses of progressive massive fibrosis (the complicated form of the disease). The cavitation and liquefaction of a fibrosed mass by an infectious process (tuberculosis, infections by anaerobes, etc.) or by ischemic necrosis, and the consequent drainage into the lumen of a bronchus may cause expectoration of a blackish secretion.[2]
The images shown here correspond to a 58-year-old patient of chronic obstructive pulmonary disease (COPD), who was a smoker and with labor precedents as a coal worker for more than 25 years and was being evaluated for persistent cough. Abundant black sputum was obtained in the course of an incidental expectoration. After this incident, chest radiograph, computed tomography (CT) scan, and pulmonary function tests performed did not show significant alterations corresponding to his pathologic process (pulmonary anthracosis).
Macroscopic (gross) examination of the abundant expectoration showed the presence of a consistent blackish material interspersed with saliva [Figure 1a]. After macroscopic examination of the sample, sputum smears and cell block sections were carried out. Smears were fixed in 96% ethanol and stained by the Papanicolaou method. Cell block microtome sections were stained with hematoxylin — eosin (H and E) and Pearl's iron stain.
Figure 1.
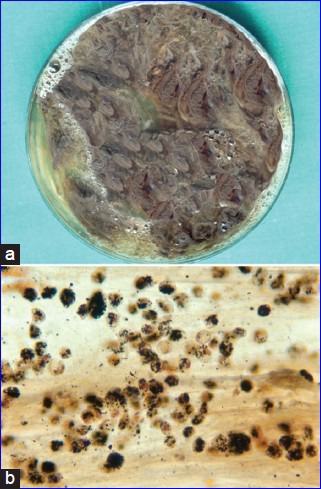
(a) Black-pigmented expectoration. Macroscopic (gross) appearance. (b) Black-pigmented expectoration. Cytological smear (Pap, ×200)
Cytological imaging of the smear [Figure 1b] showed a large amount of anthracotic material in the background and phagocyted by numerous macrophages, which was responsible for the pigmentation of the expectoration. In the H and E cell block sections also, the same anthracotic material was observed [Figure 2a], and the Pearl's stain for iron was positive [Figure 2b]. Because hemoptysis is a common symptom in COPD patients, the presence of iron among the anthracotic pigments phagocyted by macrophages could be due to the concomitant existence of hemosiderin.
Figure 2.
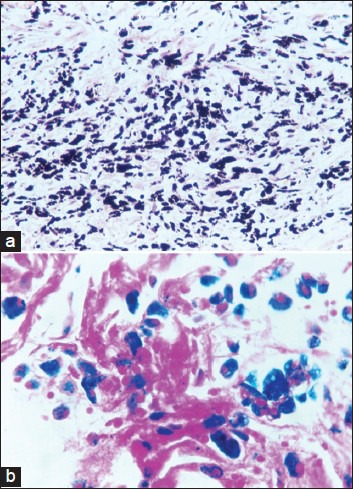
(a) Black-pigmented expectoration. Cell block section (H and E, ×200). (b) Black-pigmented expectoration. Cell block section (Pearl's stain, ×400)
This case illustrates black-pigmented sputum observed in coal workers’ pneumoconiosis (anthracosis) in the course of an incidental expectoration. As a result of a cavitation and liquefaction of a fibrosed mass in the course of a pulmonary anthracosis, a profuse black expectoration may be occasionally observed. An active infection or partial vascular stenosis is probably responsible for the patches of colliquative necrosis. Extension of the necrotic process to involve a patent bronchus allows the liquefied material to be expectorated. In some cases, findings strongly suggest that bronchial stenosis or obliteration with anthracotic pigmentation in the mucus may be caused by a fibrotic response to active or old tuberculosis infection. In this case, it was not possible to demonstrate the association of tuberculosis and anthracosis.
Black-pigmented sputum must be also distinguished from the expectoration of melanic pigment in cases of bronchopulmonary melanoma[3] and from certain uncommon fungal infections caused by the black yeast Exophiala dermatitidis, especially in patients suffering from cystic fibrosis,[4] and by Aspergillus niger in case of COPD.[5] Special stains for melanin (S-100, HMB 45, Melan-A) and fungi [Grocott's methenamine silver, periodic acid Schiff (PAS)] and fungal cultures may help to establish the diagnosis.
On the other hand, excessive carbonaceous material, in the case of crack smokers,[6] may be responsible for the blackened appearance of both bronchoalveolar lavage fluid and sputum samples.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kirchner J, Kirchner EM. Melanoptysis: Findings on CT and MRI. Br J Radiol. 2001;74:1003–6. doi: 10.1259/bjr.74.887.741003. [DOI] [PubMed] [Google Scholar]
- 2.Haro M, Nuñez A, Gozález G, Vizcaya M. Black sputum and progressive cavitary lung lesion in a coal miner. Chest. 1997;111:808–9. doi: 10.1378/chest.111.3.808. [DOI] [PubMed] [Google Scholar]
- 3.Eide J. Pathogenesis of generalized melanosis with melanuria and melanoptysis secondary to malignant melanoma. Histopathology. 1981;5:285–94. doi: 10.1111/j.1365-2559.1981.tb01787.x. [DOI] [PubMed] [Google Scholar]
- 4.Griffard EA, Guajardo JR, Cooperstock MS, Scoville CL. Isolation of Exophiala dermatitidis from pigmented sputum in a cystic fibrosis patient. Pediatr Pulmonol. 2010;45:508–10. doi: 10.1002/ppul.21187. [DOI] [PubMed] [Google Scholar]
- 5.Kimmerling E, Fedrick J, Tenholder M. Invasive Aspergillus niger with fatal pulmonary oxalosis in chronic obstructive pulmonary disease. Chest. 1992;101:870–2. doi: 10.1378/chest.101.3.870. [DOI] [PubMed] [Google Scholar]
- 6.Greenebaum E, Copeland A, Grewal R. Blackened bronchoalveolar lavage fluid in crack smokers. A preliminary study. Am J Clin Pathol. 1993;100:481–7. doi: 10.1093/ajcp/100.5.481. [DOI] [PubMed] [Google Scholar]


