Abstract
From 2006 to 2012, the South Sudan Guinea Worm Eradication Program reduced new Guinea worm disease (dracunculiasis) cases by over 90%, despite substantial programmatic challenges. Program logistics have played a key role in program achievements to date. The program uses disease surveillance and program performance data and integrated technical–logistical staffing to maintain flexible and effective logistical support for active community-based surveillance and intervention delivery in thousands of remote communities. Lessons learned from logistical design and management can resonate across similar complex surveillance and public health intervention delivery programs, such as mass drug administration for the control of neglected tropical diseases and other disease eradication programs. Logistical challenges in various public health scenarios and the pivotal contribution of logistics to Guinea worm case reductions in South Sudan underscore the need for additional inquiry into the role of logistics in public health programming in low-income countries.
Introduction
As early as 2002, global disease eradication campaigners understood that South Sudan would likely be a last bastion of dracunculiasis,1 commonly known as Guinea worm disease (GWD). During the 23-year civil war, GWD eradication surveillance and interventions in South Sudan were supported through a loose consortium of non-governmental organizations with limited success because of lack of a strong central governmental coordinating body, weak information and logistical systems, poor infrastructure, heavy seasonal rains coinciding with peak disease transmission, and rampant insecurity. The 2005 Comprehensive Peace Agreement allowed the newly created Ministry of Health, Republic of South Sudan to launch the South Sudan Guinea Worm Eradication Program (SSGWEP). (South Sudan gained full independence from Sudan in July of 2012, becoming the Republic of South Sudan.) In 2006, the program reported 20,582 new GWD cases from 3,137 villages in 7 of 10 states and 39 of 80 counties. South Sudan then accounted for 82% of cases globally.2 In 2012, the program reported 521 new cases, a 97% reduction since 2006 (Ministry of Health, Republic of South Sudan, unpublished data).
Logistics provide the means to make the right thing possible at the right place and time.3,4 Defined by the Council of Supply Chain Management Professionals (2010) as “the process of planning, implementing, and controlling procedures for the efficient and effective transportation and storage of goods … from the point of origin to the point of consumption,” logistics are a primary reason for the 97% reduction in GWD annual incidence. For public health practitioners, useful logistical guidelines exist. (The John Snow, Inc/U.S. Agency for International Development [USAID] Deliver Project provides an array of useful practical guides and policy papers, including The Logistics Handbook, a Practical Guide for Supply Chain Managers in Family Planning and Health Programs [available at http://deliver.jsi.com]. Another useful handbook, written for logistics in humanitarian disasters, is McGuire's Handbook of Humanitarian Health Care Logistics [available at www.humanitarianhealthcarelogistics.com].) However, a search for publically available, peer-reviewed literature on the role of logistics in global health (generally) and disease eradication (specifically) reveals limited available sources. Logistical challenges have negatively impacted, to name a few, efforts to combat lymphatic filariasis,5 trachoma,6 polio,7 smallpox,3 malaria, tuberculosis, and human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS)8; however, related literature on effective logistical system design and management approaches is sparse. This paper is intended for public health practitioners and policy-makers working in low-income countries. It discusses the key role of logistics in GWD eradication in South Sudan and its contribution to the how of disease eradication, including logistical system design considerations, characteristics, management approaches, and key lessons learned.
Design Considerations: Strategy And Tactics
“Logistics comprises the means and arrangements which work out the plans of strategy and tactics” (General Antoine Henri Jomini, Precis de l'Art de la Guerre, 1838).
Disease eradication requires effective and efficient technical, logistical, and administrative support structures.9 GWD eradication strategy and tactics, designed around disease epidemiology in South Sudan and associated contextual considerations, shape SSGWEP support structures and associated management approaches.
GWD eradication strategy.
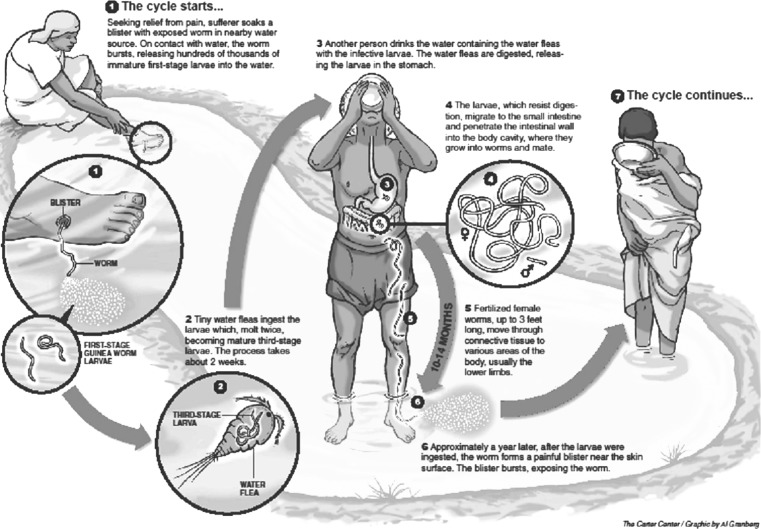
Eradication campaigns require a level of intervention delivery and surveillance substantially surpassing the level of disease control programs.10 Eradication programs must interrupt disease transmission everywhere as rapidly as possible. Therefore, case containment and sensitive and specific surveillance are fundamental to the strategy and foundational for program interventions. The SSGEWP attempts to detect every case (defined as a person with one or more worms emerging from his/her body in a calendar year) and contain every worm. Case containment prevents a worm from releasing its larvae into a water source (Figure 1). Containment requires detection within 24 hours of worm emergence, case management every 24 hours, and supervisory confirmation of containment within 7 days.
Figure 1.
Guinea worm lifecycle.
The village is the basic unit of surveillance. The program maintains an updated list of villages under active surveillance and a complete line list of all detected cases. Generally, villages remain under active surveillance until reporting no cases for 3 consecutive years and no established population movements with known endemic villages. The SSGWEP logistical system must support continuous daily active surveillance among households in villages under active surveillance and delivery of other interventions in all endemic villages. Program logistics must also support the necessary supervisory structures.
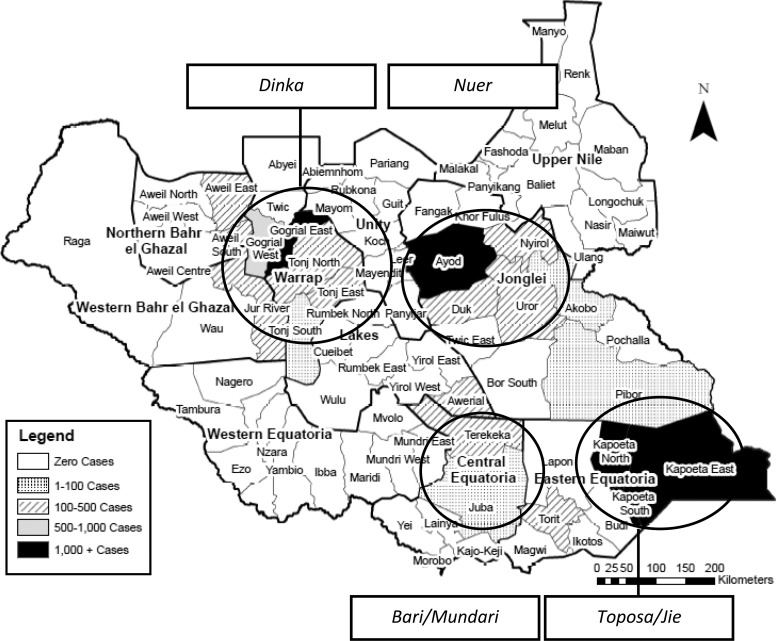
The epidemiology and programmatic environment in South Sudan dictate the design of program logistics. In 2006, based on data that would be subsequently validated over years of active surveillance, the SSGWEP understood that transmission took place in four foci (Figure 2). In endemic areas, GWD transmission typically occurs in rainy season settlements located on relatively higher and drier ground compared with dry season settlements. Because of heavy population movement and low safe water coverage, the level of transmission risk across villages within a county remains relatively static. The physical environment in endemic areas, such as Warrap and Lakes states, largely consists of seasonal swamps, restricting transport of supplies and making transport, when possible, slow and expensive.
Figure 2.
GWD-endemic focal areas and ethnic groups in 2006.
SSGWEP tactics.
GWD eradication deploys a complementary intervention package applied simultaneously that is appropriate to the different stages of the transmission cycle. Program interventions include cloth and pipe filters (with a 100×100-μm mesh; Vestergaard, Lausanne, Switzerland), which remove the intermediate host of Guinea worm, called copepods, from drinking water. Chemical vector control using the larvicide ABATE temephos (BASF Corporation, Florham Park, NJ) controls copepod populations in unsafe water sources. Health education and behavior change efforts bolster community uptake of program interventions.
Logistical impact of person, place, and time on GWD eradication in South Sudan.
The village is the primary unit of surveillance, because it is the main location where targeted populations reside. In South Sudan, different ethnic groups populate endemic areas, but all communities are pastoralist. Villages can be, in whole or part, depopulated during the driest months, because whole families migrate with their cattle, only to return when the rains and planting season begin. Surveillance must track mobile populations throughout the year, and logistical support must enable surveillance in all places that target communities inhabit throughout the year.
Generally, the annual peak transmission season corresponds with the rainy season from April to September (Table 1). The timing and severity of the seasonal rains and resulting flooding are primary determinants for logistical system design. The program defines logistical coverage areas for support bases to mitigate poor road accessibility to endemic villages. The rainy season necessitates decentralization of materials and execution of technical and logistics activities according to a seasonal implementation calendar.
Table 1.
Precipitation, transmission, and program activities (2006–2012)
| Month | Rainfall | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dry | Rains | Dry | ||||||||||
| January | February | March | April | May | June | July | August | September | October | November | December | |
| Total new GWD cases 2006–2012 by month | 252 | 309 | 725 | 4,009 | 7,069 | 6,886 | 6,186 | 4,273 | 3,295 | 1,839 | 867 | 285 |
| Technical activities | Surveillance and supervision | |||||||||||
| Planning, mapping, village volunteer training | Volunteer training, health education, prepare for onset transmission | Intensified supervision, case containment, and intervention delivery | Microplanning and mapping | |||||||||
| Training supervisors and annual review meeting | ||||||||||||
| Logistical activities | Procurement; shipping to field offices; field office construction/maintenance | Limited movement of materials/staff | Limited movement of materials/staff; develop logistics plans for next transmission season 11and materials requiring production; procurement; finalize shipping plan | Procurement; shipping origin to warehouses; construction of new offices and stores | ||||||||
| Vehicle preventative maintenance | ||||||||||||
SSGWEP Logistical Design
Locating logistical resources.
War and neglect left South Sudan with a programmatic environment characterized by poor road networks, a weak primary healthcare system, and regular insecurity. Since 2006, South Sudanese primary healthcare structures have developed slowly, with limited extension services in endemic communities. The SSGWEP could not rely on or effectively integrate its efforts with nascent primary healthcare structures, because those structures were too weak to reliably support intervention delivery at the level necessary to break transmission. For the same reasons, the program could not rely on other government or private sector capabilities. Thus, the SSGWEP designed and built its own logistical (and surveillance and intervention delivery) system to meet technical requirements and overcome environmental challenges.
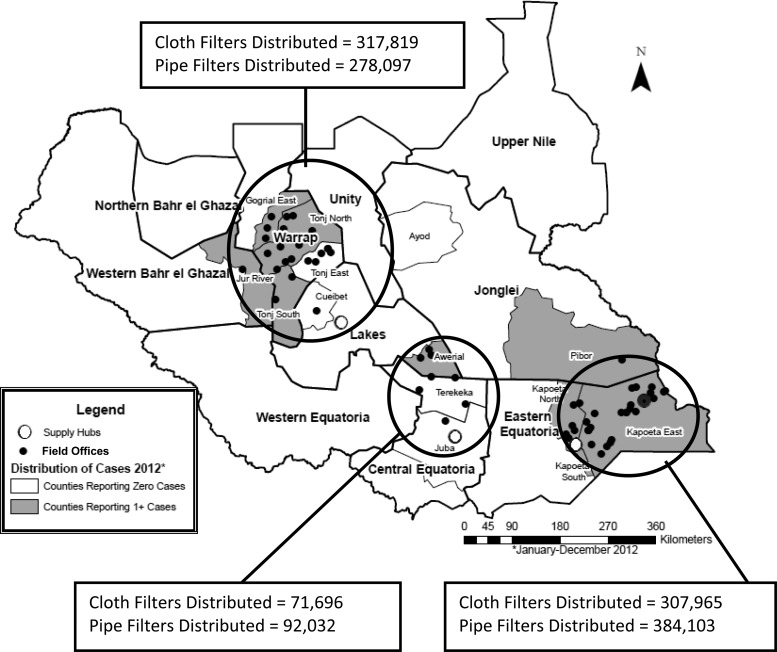
The SSGWEP uses a hub-and-spoke logistical model designed to meet the needs of the implementation environment.11 Covering defined regions, there are three central hubs serving as logistical foci (Figure 3): Kapoeta, Rumbek, and Juba. Hubs are part of a network geographically placed to facilitate connectivity between themselves, procurement locations, and satellite distribution points (i.e., spokes).12 Each hub is located on an all-weather road accessible by a heavy truck from the primary procurement point: Nairobi, Kenya. Field offices serve a similar, although less comprehensive, function as logistical support bases for field stores within payams (subdistricts) and by extension, the villages within a defined coverage area.
Figure 3.
Logistical hubs and field offices with cloth and pipe filters distributed by logistical hubs in 2012.
As part of the hub-and-spoke model, SSGWEP uses decentralized warehousing4,13 to position materials as close as possible to targeted villages. The approach maximizes availability and minimizes transport costs, especially during the rainy season when intervention materials, such as cloth and pipe filters, are most needed. Cloth filters flow from procurement locations to hubs to field offices to field stores to villages. Village volunteers distribute them to households and maintain a small stock for replacement purposes.
Systemic approaches to controlling logistical flows.
Through hub-and-spoke and warehousing systems, the SSGWEP uses two approaches to determine procurement and material flows.14 First, during annual allocations, the Secretariat uses previous year epidemiologic data to dictate materials, quantities, delivery times, and destinations and pushes them to the peripheral locations. As shown in Table 2, non-endemic villages under active surveillance and endemic villages receive different pre-defined intervention packages based on levels of transmission risk. Endemic villages (reporting indigenous cases during the current or previous year) are more likely to experience transmission, and thus, they are a higher priority than other villages under active surveillance.
Table 2.
Interventions in endemic and non-endemic villages under active surveillance
| Endemic villages | Non-endemic village under active surveillance |
|---|---|
| Surveillance: Two or more trained village volunteers, daily house-to-house surveillance by volunteer, daily visits by supervisor | Surveillance: one trained village volunteer, daily house-to-house surveillance, supervisor visits weekly |
| Cloth filters (four times per year) | Cloth filter (one time per year) |
| Pipe filters (80% of population) | |
| All water sources associated with current or previous year cases treated with ABATE | |
| Medical supplies for case management and containment |
Second, in a subordinate requisition or pull system, SSGWEP field offices request materials, destinations, delivery timing, and quantities from an assigned hub. Requisitions meet unforeseen needs, such as when field staff identify new villages requiring surveillance. Pull typically happens during the transmission (rainy) season, when movements are more complicated, costly, and slower. A well-developed hub-and-spoke system is key to supporting both logistics flows.
To maximize vehicle availability, the program emphasizes scheduled preventative maintenance. Trained mechanics and a fully functional automotive workshop are in each hub (Table 3). Mechanics travel regularly to field sites. Decentralized stocks of automotive spare parts further minimize mechanical downtime.15 Decentralized maintenance reduces the time that it takes to repair non-operating mechanical assets. Additionally, the vehicle fleet consists of similar vehicle models, reducing time and expense by facilitating easy bulk procurement of spare parts and easing the burden on program mechanics.
Table 3.
SSGWEP transport and maintenance resources in 2012
| Resource | Quantity |
|---|---|
| Vehicles (4×4) | 49 |
| Heavy trucks | 10 |
| Motorcycles | 198 |
| Mechanics | 6 |
| Automotive workshops | 3 |
Management approaches to improve logistical functioning.
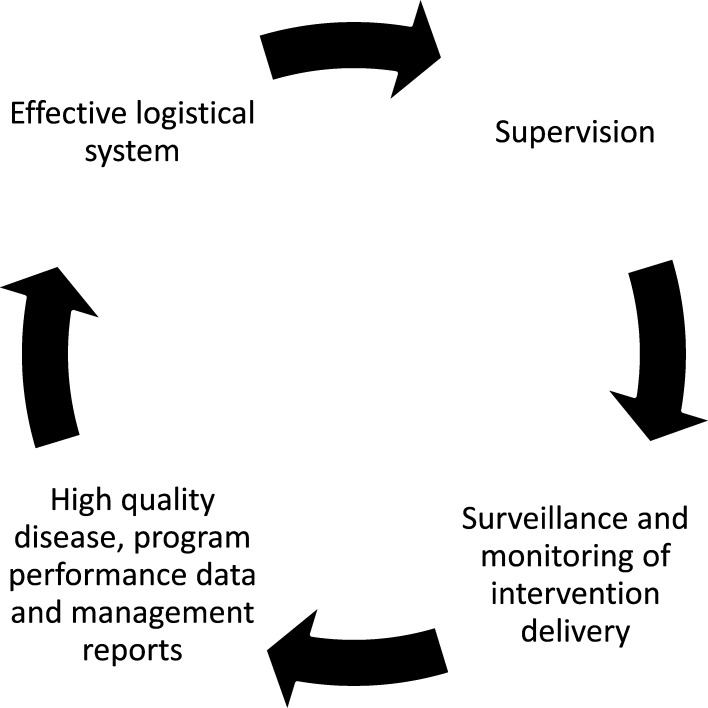
Logistical system design, no matter how well-suited to programmatic demands and environment, does not necessarily translate into an effective and efficient system. The program uses disease surveillance and program performance data together with integrating logistical and technical responsibilities to ensure logistical effectiveness.
Data-driven planning.
The SSGWEP collects and validates surveillance and performance data through regular documented supervision at all program levels (Figure 4). Supervision extends to every village under active surveillance. The program conducts systematic data quality checks and cleaning as data are transferred from the village to the national Secretariat. Supervisors confirm the existence of villages, their physical locations (including geographic coordinates), demographic data, and epidemiologic information. Therefore, supervision strengthens disease surveillance and monitoring of intervention delivery, improves data quality, and reinforces rational logistical planning and resource deployment (Figure 4). This process is not possible without significant initial and ongoing investment in logistics.
Figure 4.
Continuous quality improvement cycle for SSGWEP logistical system.
Data quality since 2006 improved alongside the logistical capacity supporting data collection and supervision. By 2008, surveillance data from the three Kapoeta counties showed relatively early transmission beginning annually in March. Thus, the program put logistical support and surge capacity in place by February. From 2008 to 2009, timely delivery of logistical support helped boost case containment (54–73%; Kapoeta counties reported 1,350 and 675 cases in 2008 and 2009, respectively), endemic village chemical vector control coverage (69–72%), and endemic village cloth filter coverage (84–99%), and cases declined (–50%).
Data-driven planning is instrumental to an effective and efficient logistical system. Field managers, known as technical advisors (TAs), oversee program surveillance, interventions, and logistical support in a defined geographic area. They create annual microplans identifying forecasted technical and logistical needs for their respective areas. By planning logistics for the coming year immediately after the recently concluded transmission season in August/September, the program maximizes the time between knowing what and how much logistical support is needed and when it must be delivered (before the next transmission season). Microplans capture the logistical and technical support required to implement interventions at a level necessary to break GWD transmission in the coming year. The planning process results in the total forecasted logistical needs of a given TA program area for the coming year. The program uses a mathematical forecasting model14 based on disease burden (numbers of cases as well as endemic and at-risk villages), demographics (population and households), and intervention coverage required to break transmission. For example, data-driven planning allowed the program in 2009 to successfully pre-position cloth filters in Warrap State. The state then had 193,453 targeted households in 5,119 endemic and at-risk villages. The program-defined intervention package required availability of four cloth filters for every targeted household to maintain a viable filter throughout the year. In 2009, the program pre-positioned over 800,000 filters and distributed 787,425 before (initial distribution) and during (replacement distributions) the rainy/transmission season. Successful pre-positioning of cloth filters in Warrap State led to 99% coverage of endemic villages and contributed to a 43% decrease in cases (Warrap reported 1,193 and 675 cases in 2009 and 2010, respectively).
Functional integration.
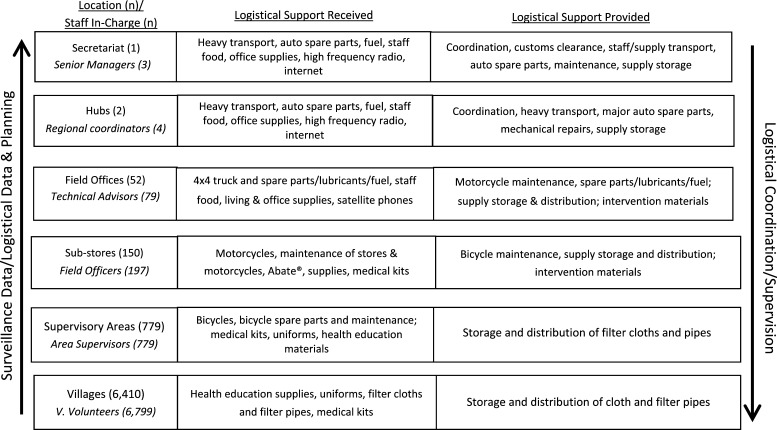
The SSGWEP integrates logistical and technical management (Figure 5). Such integration has proven effective in other public health efforts, including eradication programs.3 Field officers, TAs, and to an extent, village-based volunteers manage technical implementation, enabling logistical support in their respective coverage areas.
Figure 5.
SSGWEP logistical and technical management structure in 2012 (Ministry of Health, Republic of South Sudan, unpublished data).
Each program level requires logistical support and in turn, provides logistical support to subordinate levels. Again, using the example of microplans, after TAs forecast their needs, the Secretariat verifies and allocates an intervention and logistical package. Using surveillance data collected from village volunteers and verified by TAs, the Secretariat identifies program areas requiring more or less logistical support than requested in the plans. It then compiles all microplans to create program-wide procurement and shipping plans.
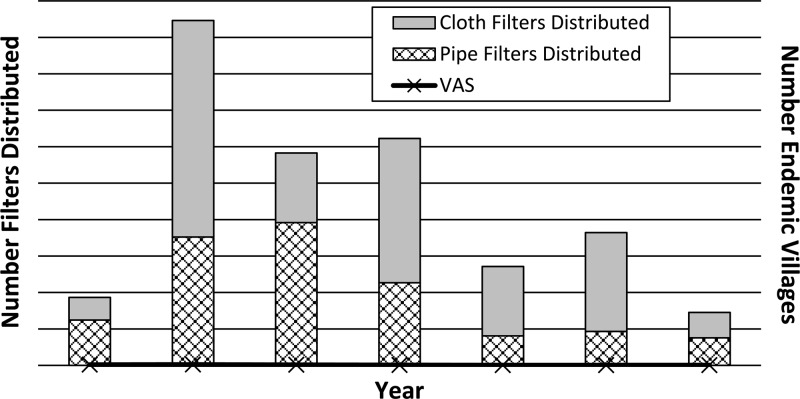
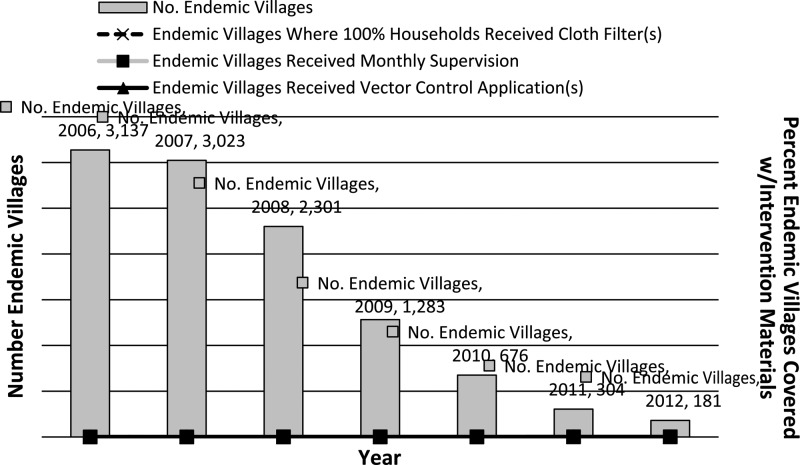
Logistical capacities.
From 2006 to 2012, SSGWEP logistical capacity consistently increased: technical advisors increased from 16 to 79, suboffice warehouses increased from 11 to 49, and 4×4 vehicles increased from 29 to 49. Increased capacity translated to increased outputs. The number of filters distributed generally corresponds to the evolving number of villages under active surveillance (Figure 6), but the program focused first on filter (and other intervention) coverage in endemic villages (Figure 7). In 2007, with over 22,000 villages under active surveillance, the peak number of filters was distributed (approximately 9.5 million). The number of water source treatments also increased from 263 in 2006 to 12,591 in 2012. The program showed marked progress in terms of improving surveillance, reducing endemic villages, and increasing intervention coverage.
Figure 6.
Total pipe and cloth filters distributed and villages under active surveillance from 2006 to 2012 (Ministry of Health, Republic of South Sudan, unpublished data).
Figure 7.
New GWD cases by year and endemic village annual intervention coverage rates from 2006 to 2012 (Ministry of Health, Republic of South Sudan, unpublished data).
Intervention coverage is expressed as a proportion of endemic villages receiving the intervention according to program norms. Coverage changes yearly depending on interventions reaching endemic villages (numerator) in the prescribed manner and total number of endemic villages (denominator). Endemic villages were supplied pre-rainy season to ensure availability before cases occurred, because during and after rainy season distribution was impossible. Reductions in endemic villages (denominator) were a function of improving surveillance sensitivity and specificity as well as successes in breaking transmission within them—none of which would have been possible without a robust logistical system. For the numerator, increased intervention coverage was a direct result of increased logistical capacity.
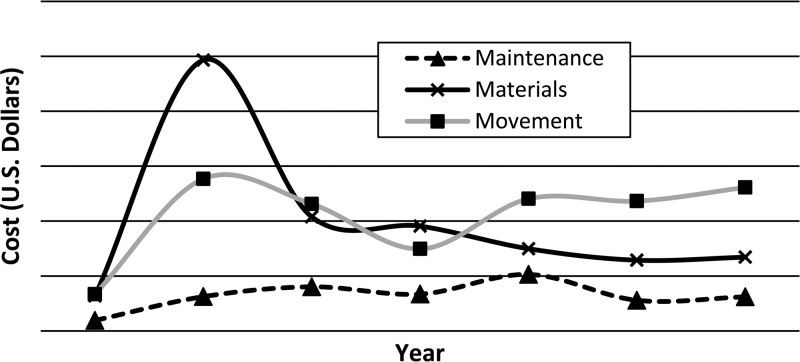
Logistical costs.
Total logistical costs peaked in 2007 at over $8.6 million and since then, averaged over $4.5 million annually. With the exception of the push in 2007 to rapidly build the SSGWEP logistical system (and the relatively large number of villages under active surveillance), with corresponding one-time large capital expenditures, logistical costs have remained relatively stable (Figure 8). Logistical costs broken down by the major logistical components of maintenance/construction, materials/warehousing, and shipping/transport show that material costs decreased along with the number of endemic villages.
Figure 8.
SSGWEP non-personnel logistical costs by type (2006–2012).
Discussion
In past disease eradication efforts, logistical support contributed to success, such as with smallpox,3 and failure, such as with the aborted malaria eradication efforts in the mid-20th century.16 The program learned numerous lessons in the process of establishing and strengthening program logistics, some of which will be relevant to other public health efforts in low-resource environments.
Lessons learned from SSGWEP logistical implementation.
Lesson 1: logistical systems are costly in eradication programs.
Even with decreasing caseloads and endemic villages, logistical costs remain substantial. Since the 2007 peak in costs and villages under active surveillance, staff, suboffices, and vehicles have increased, translating to substantial ongoing costs for maintenance and shipping/transport to reach remote locations. Overall costs for materials have decreased, because endemic villages, which receive the bulk of intervention materials, have decreased substantially.
Logistical costs have, however, remained substantial for two reasons. First, from a management perspective, the program enhanced supervisory structures to increase momentum to elimination by improving the quality of surveillance and intervention delivery. Supervisory structures require transport, supplies, and maintenance. To increase the rate of case reductions, since 2006, the program expanded its logistical capability, despite successive reductions in cases and endemic villages.
Second, since 2010, logistical costs remain substantial, because the number of villages under active surveillance has remained largely static. The SSGWEP sacrifices cost savings from reductions in numbers of villages targeted to increase surveillance sensitivity. Weak existing primary healthcare structures and highly mobile populations in endemic areas necessitate maintaining active surveillance in thousands of villages with no documented transmission in the past 3 years. Adequate financing allows the prioritization of impact over cost. However, programmatic complacency or reinfection of non-endemic villages could result in substantial opportunity and long-term direct costs, far outweighing upfront capital costs given the 1-year incubation period/lifecycle for dracunculiasis. Despite the investment necessary for such comprehensive geographic coverage, several financially and programmatically costly outbreaks have temporarily set the program back, a dynamic that would have been exacerbated had there not been the investment in the system to detect and respond quickly and effectively to outbreaks.
Lesson 2: management approaches are key to effective logistics.
SSGWEP logistical and technical systems are intrinsically linked. Technical–logistical integration combine participatory and directive decision-making. As a result, the program benefits from the efficiency of directive decision-making and high levels of commitment that are characteristic of participatory approaches.17,18 Despite the added burden on technical staff, integration ultimately improves surveillance, supervision, and intervention delivery. Those individuals tasked with technical implementation are also responsible for logistical implementation and decision-making. Technical and logistical implementers/decision-makers are regularly in targeted villages directly assessing whether logistical support is sufficient to achieve eradication, thereby maximizing efficiencies at the village level. Additionally, technical–logistical integration creates a horizontal organizational structure, which further improves efficiency. Integration maintains program focus on the organizational goal18 of eradicating GWD. Integrated structures minimize competing priorities and inefficient action.
Lesson 3: disease surveillance and program performance data are an effective basis of logistical planning and execution.
Businesses use profits to measure effectiveness; the SSGWEP uses case numbers and key performance indicators. As the program increased supervision, surveillance and program data quality improved, facilitating more effective logistical and technical forecasting, planning, and implementation. In Kapoeta in 2008, the enhanced understanding of transmission seasonality permitted appropriate timing of supply deliveries, ensuring that intervention materials were in place before transmission season.
Additionally, as in any complex public health program, priorities compete. However, quality surveillance data allow for effective prioritization. Supervisors must analyze field staff and volunteer demands for supplies during monthly refresher trainings held with thousands of community volunteers. A simple but accurate list of villages ranked by previous year cases allows TAs to predict the likely location and timing of current year cases and thus, dynamically prioritize who gets what supplies at what times.
Evidence-based planning allows for rational program implementation. It also reduces logistical workload. The Secretariat can accurately forecast logistical needs and allocate resources to maximize impact where transmission occurs. Need-based planning allows for effective pre-positioning of program supplies, thus minimizing requests and associated time wastage from demand-driven or pull logistical support. Surveillance data also provide a verifiable basis to control resource wastage and prevent urgent requests for resupply resulting from misuse.
An inherent challenge from reliance on a non-logistical data collection system to guide logistical implementation is that, as the logistical system matured, the program often lacked microlevel data common to logistical planners that are used to identify logistical bottlenecks. For example, only after 2012 could the program accurately track delivery times for all ordered supplies and vehicle indicators, such as fleet miles covered or fleet fuel consumption.
Lesson 4: flexibility is essential to success.
Regardless of the quality of planning and implementation, unexpected needs arise, and program managers must be able to respond. Just as it was crucial to smallpox eradication,19 logistical flexibility has been a key feature of the SSGWEP. The approaches of technical–logistical integration and data-driven planning produce a flexible logistical system capable of dealing with a dynamic epidemiologic and programmatic environment.
Central to flexibility and dictated by the quality of active surveillance and supervision is the need in disease eradication to quickly address identified technical gaps.3 Flexibility requires readily available personnel, materials, maintenance, and transport capacity to act when and where needed.19 Thus, the program uses decentralized warehousing and the hub-and-spoke model.
In 2010, the program detected an outbreak in Bakder, Tonj South County, a village not previously under active surveillance. Decentralized warehousing allowed for rapid usage of nearby resources. Cases were first detected in late June, and by July, the program achieved 100% cloth and pipe filter coverage and treated all unsafe water sources. The program contained 85% of all cases and thus, achieved an 86% case reduction the next year.
The SSGWEP invests heavily in transport and maintenance capabilities to ensure optimal flexibility. It is essential to move staff and materials when needed, including in the rainy/transmission season when movement by foot is sometimes the only option. By 2012, the program had eight military-grade trucks suitable for rainy season transport. To increase transport availability, the SSGWEP invests substantially in decentralized preventative maintenance. Between 2006 and 2012, maintenance-dedicated staff grew from zero to eight, and the SSGWEP can now monitor and verify daily preventative maintenance performed on each vehicle.
Regular direct communication between field staff and senior managers without necessarily immediately involving a direct supervisor was one key to the success of small pox eradication in India.9 Level jumping is an important means for field staff to efficiently communicate needs to the Secretariat. However, conflicts can arise when information flows regularly or unnecessarily bypasses direct supervisors, negating necessary oversight. Consistent lack of adherence to program structures by field staff has, at times, undermined the hierarchical structure necessary to coordinate and supervise such a complex program. Senior supervisors only allow and encourage level jumping in specific situations, such as when an outbreak occurs or there is breakdown in logistical support. In such situations, a TA can efficiently communicate with the Secretariat, who in turn, can ensure appropriate resource mobilization.
Because of the need to respond effectively to cases within a challenging physical environment, speed and decentralization of logistical resources can undermine logistical controls. Logistical resources, especially in remote field offices, have, at times, been misused, undermining program effectiveness. The decision in 2009 to cease decentralization of specific expensive vehicle spare parts unnecessary for routine preventative maintenance sought to balance maintaining logistical flexibility with not foregoing basic controls. Additionally, field personnel have occasionally acted independently, contrary to technical guidelines. Such actions have been exacerbated by the ability to deploy logistical capacities without prior approval. On-site supervision and robust monthly reporting can detect and mitigate inappropriate actions, but they require constant programmatic attention (and logistics).
Broader implications of logistical lessons learned in public health programming.
The debate on the long-term benefits of vertical public health programs and how to effectively integrate existing vertical structures into horizontal health systems continues.20–22 Because of the intensity of eradication programs, associated logistical investments are higher than in disease control programs. However, vertical programs can serve as building blocks for health systems development.23 Some of the infrastructure, processes, approaches, and personnel could be adapted and adopted to establish and/or strengthen community-based disease surveillance, monitor public health interventions, and generally, document public health outcomes. Specifically, programs requiring significant community-level interaction (for example, mass drug administration for neglected tropical diseases, routine immunization campaigns, and disease eradication programs) could benefit from the logistical approaches and system designs addressed in this paper. Integrated technical–logistical staffing reduces personnel needs, because one person covers logistical and technical responsibilities. It also ensures strong linkages between health outcomes and the strategies and tactics used to achieve said outcomes. Surveillance data-driven logistical planning improves temporal and geographic pre-positioning of public health resources. Furthermore, implementers can adapt decentralized warehousing, maintenance, and transport networks to support relevant public health programs.
Conclusion
Because logistics play an essential role in many public health efforts, the amount of investment required (when done effectively), and the limited availability of related peer-reviewed research, the study of logistics in public health deserves additional attention. As GWD elimination in South Sudan approaches, there is an opportunity to adapt some aspects of the SSGWEP logistical system into the emerging public health system before transmission is interrupted nationwide (for example, in areas where active surveillance must be maintained but where there are no currently endemic villages). Careful consideration should be given in this process to carefully select the logistical design and approaches relevant to national public health priorities while not jeopardizing Guinea worm eradication achievements to date. If the Republic of South Sudan, with donor help, can leverage existing SSGEWP logistical capabilities, a legacy of strengthened public health logistics would be a meaningful additional benefit to the end of GWD.
ACKNOWLEDGMENTS
For their invaluable contributions to the Guinea worm eradication campaign in South Sudan, the authors thank the Ministry of Health, Republic of South Sudan; The Carter Center; the World Health Organization; United Nations Children's Fund (UNICEF); the Bill and Melinda Gates Foundation; the United Kingdom's Department for International Development; program technical advisors; and the thousands of local volunteers who are making Guinea worm eradication in South Sudan a reality in their new nation.
Footnotes
Authors' addresses: Alexander H. Jones, P. Craig Withers, Ernesto Ruiz-Tiben, Donald R. Hopkins, and David Stobbelaar, Health Programs, The Carter Center, Atlanta, GA, E-mails: jonesahj@yahoo.com, cwither@emory.edu, eruizt@emory.edu, sdsulli@emory.edu, and resadv@cartercenter-ssudan.com. Steven Becknell, Division of Public Health Systems and Workforce Development, Centers for Disease Control and Prevention, Atlanta, GA, E-mail: ziq1@ug.cdc.gov. Samuel Yibi Makoy, Directorate of Public Health, Ministry of Health, Republic of South Sudan, Juba, South Sudan, E-mail: makoy@cartercenter-ssudan.com.
References
- 1.Hopkins DR, Ruiz-Tiben E, Diallo N, Withers C, Maguire J. Dracunculiasis eradication: and now, Sudan. Am J Trop Med Hyg. 2002;67:415–422. doi: 10.4269/ajtmh.2002.67.415. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Progress toward global eradication of Dracunculiasis, January 2005–May 2007. MMWR Morb Mortal Wkly Rep. 2007;56:813–817. [PubMed] [Google Scholar]
- 3.Wickett J, Carrasco P. Logistics in smallpox: the legacy. Vaccine. 2011;29((Suppl 4)):D131–D134. doi: 10.1016/j.vaccine.2011.06.043. [DOI] [PubMed] [Google Scholar]
- 4.Ghiana G, Laporte G, Musmanno R. Introduction to Logistical Systems Planning and Control. West Sussex, UK: John Wiley & Sons Ltd; 2004. [Google Scholar]
- 5.World Health Organization Conclusions of the meeting of the Technical Advisory Group on the Global Elimination of Lymphatic Filariasis, November 2007. Wkly Epidemiol Rec. 2008;83:345. [PubMed] [Google Scholar]
- 6.Kolaczinski JH, Robinson E, Finn TP. The cost of antibiotic mass drug administration for trachoma control in a remote area of South Sudan. PLoS Negl Trop Dis. 2011;5:e1362. doi: 10.1371/journal.pntd.0001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mushtaq M, Majrooh M, Ullah M, Akram J, Siddiqui AM, Shad MA, Waqas M, Abdullah HM, Ahmad W, Shahid U, Khurshid U. Are we doing enough? Evaluation of the Polio Eradication Initiative in a district of Pakistan's Punjab province: a LQAS study. BMC Public Health. 2010;10:60. doi: 10.1186/1471-2458-10-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Travis P, Bennett S, Haines A, Pang T, Bhutta Z, Hyder AA, Pielemeier NR, Mills A, Evans T. Overcoming health-systems constraints to achieve the Millennium Development Goals. Lancet. 2004;364:900–906. doi: 10.1016/S0140-6736(04)16987-0. [DOI] [PubMed] [Google Scholar]
- 9.Brilliant L. The Management of Smallpox Eradication in India. Ann Arbor, MI: University of Michigan Press; 1985. pp. 77–143. [Google Scholar]
- 10.Hopkins D, Ruiz-Tiben E. Strategies for Dracunculiasis eradication. Bull World Health Organ. 1991;69:533–540. [PMC free article] [PubMed] [Google Scholar]
- 11.Zapfel G, Wasner M. Planning and optimization of hub-and-spoke transportation networks of cooperative third-party logistics providers. Int J Prod Econ. 2002;78:207–220. [Google Scholar]
- 12.O'Kelly M. A geographer's analysis of hub-and-spoke networks. J Transp Geogr. 1998;6:171–186. [Google Scholar]
- 13.Hugos M. Essentials of Supply Chain Management. 3rd Ed. Hoboken, NJ: John Wiley & Sons; 2011. [Google Scholar]
- 14.John Snow Inc. Programs That Deliver: Logistics' Contributions to Better Health in Developing Countries. Arlington, VA: US Agency for International Development; 2000. [Google Scholar]
- 15.Collins CD, Myers G, Nicholson N. A successful transport scenario for the health sector in developing countries. World Hosp. 1992;28:9–14. [PubMed] [Google Scholar]
- 16.Krogstad DJ. Malaria as a reemerging disease. Epidemiol Rev. 1996;18:77–89. doi: 10.1093/oxfordjournals.epirev.a017918. [DOI] [PubMed] [Google Scholar]
- 17.Wysocki RK. Effective Project Management: Traditional, Agile, Extreme. Indianapolis, IN: Wiley Publishing; 2009. [Google Scholar]
- 18.Frakel EG. Quality Decision Management—The Heart of Effective Futures-Oriented Management: A Primer for Effective Decision-Based Management. New York, NY: Springer Science & Business Media; 2008. pp. 5–6. [Google Scholar]
- 19.Henderson DA. Principles and lessons of the smallpox eradication campaign. Bull World Health Organ. 1987;65:535–546. [PMC free article] [PubMed] [Google Scholar]
- 20.Windisch R, Waiswa P, Neuhann F, Scheibe F, De Savigny D. Scaling up antiretroviral therapy in Uganda: using supply chain management to appraise health systems strengthening. Global Health. 2011;7:25. doi: 10.1186/1744-8603-7-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Travis P, Bennett S, Haines A, Pang T, Bhutta Z, Hyder AA, Pielemeier NR, Mills A, Evans T. Overcoming health-systems constraints to achieve the Millennium Development Goals. Lancet. 2004;364:900–906. doi: 10.1016/S0140-6736(04)16987-0. [DOI] [PubMed] [Google Scholar]
- 22.Atun RA, Bennett S, Duran A. When Do Vertical (Stand-Alone) Programmes Have a Place in Health Systems? 2008. http://www.who.int/management/district/services/WhenDoVerticalProgrammesPlaceHealthSystems.pdf Available at. Accessed March 31, 2012. [Google Scholar]
- 23.Melgaard B, Creese A, Aylward B, Olive JM, Maher C, Okow-Bele JM, Lee JW. Disease eradication and health systems development. MMWR Morb Mortal Wkly Rep. 1999;48:28–35. [PMC free article] [PubMed] [Google Scholar]