Abstract
Although global health is a recommended content area for the future of education in public health, no standardized global health competency model existed for master-level public health students. Without such a competency model, academic institutions are challenged to ensure that students are able to demonstrate the knowledge, skills, and attitudes (KSAs) needed for successful performance in today's global health workforce. The Association of Schools of Public Health (ASPH) sought to address this need by facilitating the development of a global health competency model through a multistage modified-Delphi process. Practitioners and academic global health experts provided leadership and guidance throughout the competency development process. The resulting product, the Global Health Competency Model 1.1, includes seven domains and 36 competencies. The Global Health Competency Model 1.1 provides a platform for engaging educators, students, and global health employers in discussion of the KSAs needed to improve human health on a global scale.
Introduction
Health is at the center of many important global issues, including economic development, global security, effective governance, and human rights promotion.1 As the field of global health rapidly changes, academic public health institutions are increasingly engaged in defining the scope of the university mission in this area, collaborating with multiple partners to solve multisectoral, systems-based population health problems, and responding to global health challenges with evidence-based research, teaching, and service.1,2 The Institute of Medicine's report on “Who Will Keep the Public Healthy,” highlighted global health as a recommended content area for the future of public health education,3 while interest in global health has exploded among college students.4,5
Schools and programs of public health have great potential to meet the demand for global health professionals to fill positions such as public health advisors, planners, analysts, epidemiologists, health educators, and health communicators (Hiland J, unpublished presentation). However, the lack of clearly defined competencies in master's-level global health education challenges the ability of academic institutions to ensure that students are able to demonstrate the knowledge, skills, and attitudes (KSAs) needed for successful performance in today's global health workforce. Although 25 of the then 40 Association of Schools of Public Health (ASPH, now the Association of Schools and Programs of Public Health, or ASPPH)-member schools reported using competencies to guide their global health education programs in 2009, an analysis of the competency sets received from 20 of the schools indicate considerable variation in expectations for their graduates.6
Competencies, composed of KSAs, serve as educational tools or benchmarks that assist educators in preparing students to demonstrate how they would contribute effectively to the workforce upon graduation. Without such an educational framework, students might be unprepared for the complex challenges they will encounter in the field.7 Global health competencies have been developed for medicine and nursing students,7 yet, until recently, no standardized global health competency model existed for master-level students in public health. Various groups and individuals have recommended the need for such competencies and improved global health training and education, in general.1,8–10
Given the expertise in global health among faculty at schools and programs of public health, the growing number of tracks in global health, and the growing interest in global health from students at schools and programs of public health and elsewhere, the ASPH Global Health Committee sought to address this need by facilitating consensus development of a global health competency model. The goal of the ASPH global health competency development project was to “promote population health, safety, and well-being at local and global levels by enhancing the global health competence of students in schools of public health and related global health educational programs.”11 The primary target audience for this initiative was students specializing in global health upon graduation from a master's level program of study, inclusive of globalized curricula where the entire program of study is relevant to global public health. This work describes the methodology used to arrive at the model, presents the model as well as its potential uses, and discusses some of the ways in which these competencies may influence education and practice.
Methods
Participants.
The ASPH Global Health Committee selected both practitioners and academic global health experts to provide leadership and guidance throughout the competency development process. The leadership group, chaired by Pierre Buekens, consisted of 11 global health experts who guided the project by delineating the scope and shaping the aims for the model. Project staff solicited experts to populate workgroups, which formed around each of the seven thematic areas (domains) considered relevant to the nascent competency framework. Two experts in global health practice and research, one to represent academia and one to represent practice, co-chaired each of the seven domain workgroups. (The domain workgroup co-chairs, recruited individually for their expertise, led the domain workgroups through the model development process.)
Each domain workgroup consisted of both a core workgroup and a resource workgroup. Core workgroups for each domain consisted of ∼10 subject matter experts in the respective thematic areas who would participate in the entire competency development process. Resource workgroups consisted of ∼10–20 subject matter experts in the respective thematic areas who would participate in only certain stages of the competency development process to provide additional expert engagement.
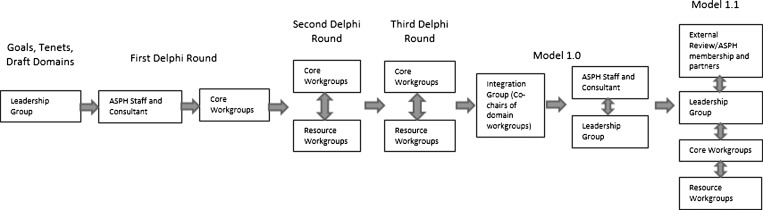
Core workgroup members identified the preliminary list of competencies before the first Delphi round, completed all Delphi rounds, and were invited to provide comments after the first full model, Model 1.0, was released. Resource workgroup members completed only the second and third Delphi rounds and were also invited to provide comments on the full model. Model 1.0 was also made broadly available to ASPH membership and partners and the public through an external review process. The flow of recommendations among the various participants throughout the initiative is depicted in Figure 1.
Figure 1.
Flow of recommendations among participants throughout the initiative.
Staff recruited members of the domain core and resource workgroups through the weekly, electronic ASPH Friday Letter and by e-mails targeted at stakeholder groups and schools of public health. Individuals were placed into workgroups based on their experience, interest, and availability. Diversity of the domain core and resource workgroups was considered beyond practice/academic designations to include gender, race, ethnicity, type of workplace (e.g., non-governmental organization (NGO), foundation, government), and national affiliation. Employers of global health master's graduates were strongly encouraged to participate in the resource groups. Project staff coordinated all efforts, and ASPH secured the services of a consultant to assist the core workgroups in the competency development process.
Procedures.
Some of the methodology implemented early in the project has been previously described.6 The project formation began with the identification of leadership group members and other key participants in the spring and summer of 2009. The ASPH then launched the initiative in September 2009 by conducting a 2-day Global Health Competency Development Project Consensus Conference at the University of Minnesota. End-products of the conference included draft tenets, draft domains, and an outline of processes to guide the effort.11
After reaching agreement on the initiative's goals, the leadership group endorsed the following seven tenets to guide the workgroups:
-
1.
Approach global health as public health;
-
2.
Keep in mind the inter-relatedness of health, development, security, and governance;
-
3.
Build upon the Master of Public Health (MPH) core competencies;12
-
4.
Draw from existing frameworks and models;
-
5.
Ensure the competencies are both practice- and application-oriented, as well as measurable;
-
6.
Think 3 to 5 years ahead; and
-
7.
Examine linkages across disciplines and schools (e.g., anthropology, business, and joint degrees).
Three essential guiding tenets were emphasized to the workgroups as they began their efforts and, thus, are described as follows. First, in recognition of the considerable overlap between global health and public health, and to avoid duplication, the leadership group concluded that the global health competencies would be built upon the foundation provided by ASPH's MPH Core Competency Model.12 Second, although the competencies were aimed at academe, their intent is to improve the practice of global health across all entrants into the global health workforce. Third, in recognition of the increasing complexity and the constantly shifting global health challenges (e.g., anticipated demographic and climate changes), the competencies needed to be developed with the future in mind.
To ensure the competency model would be informed by evidence, the consultant developed draft thematic domains from existing frameworks, models, and literature (e.g., Global Health Competency Project Resource Guide) and external resources.13,14 The discussion at the Consensus Conference led to the revision of some of the draft domains, with seven domains eventually identified as critical to global health (Table 1). Proposed domains were provided to the leadership group as a starting place and, upon approval, were used to constitute the workgroups.
Table 1.
Domain names
| Domain | Proposed domain name | Final domain name |
|---|---|---|
| 1 | Capacity building | Capacity strengthening |
| 2 | Collaboration and partnering | Collaborating and partnering |
| 3 | Ethical reasoning and professional practice | Ethical reasoning and professional practice |
| 4 | Health equity and social justice leadership | Health equity and social justice |
| 5 | Project and process management | Program management |
| 6 | Socio-cultural and political awareness | Socio-cultural and political awareness |
| 7 | Strategic analysis and evaluation | Strategic analysis |
From November 2009 through April 2010, staff coordinated the recruitment of individuals to participate in the model development process at various levels of involvement. From April through June of 2010, staff arranged an orientation teleconference for workgroup co-chairs and subsequent orientation teleconferences for each workgroup.
Modified Delphi process.
This project was intended to build consensus on what constitutes global health competencies, and to provide guidance to faculty so education could be consistent and comparable across schools and programs, regardless of the pedagogical approach.15,16 Using Bloom's Taxonomy as a framework for competency development,17 the consultant and staff managed and oversaw a modified Delphi process implemented in three rounds. They used a survey to identify the key sets of skills required of global health professionals, i.e., what must professionals know (knowledge), do (skills), and feel (attitudes) to improve health around the world? Once delineated, these KSAs would constitute the essential competencies recommended for students specializing in global health practice upon completion of a master's level program of study.
Originally, the competencies in the survey were preceded by a stem: “In order to protect and promote population health, safety, and well-being at local and global levels, as well as eliminate health and social disparities worldwide, every graduate of a master's program in global health should be able to…;” however, this text was dropped later as it was considered too cumbersome. After each competency was presented for each round of the modified Delphi survey, respondents had four potential responses: accept, accept with changes, reject, or consider an alternative. The options for “accept with changes” and “consider an alternative” were both appended with an open-ended question that allowed respondents to elaborate. In all surveys, respondents were invited to provide further comments and competencies. In the third of three rounds, an additional item was included, soliciting comments on the domain definition.
Staff sent potential respondents e-mails with an embedded Survey Monkey link to complete each survey round. In August 2010, the first survey was administered to core workgroup members within their respective domains. Each workgroup was given 2 weeks to complete its survey. Workgroup members then discussed the resultant data by teleconference and e-mail. In January 2011, core and resource workgroup members completed the second modified Delphi round. Adding resource group members allowed for greater numbers of stakeholders to provide electronic input on the draft sets of domains and competencies specific to their area of expertise. Subsequently, workgroup members again discussed the resultant data from their workgroups by teleconference and e-mail. The third and final modified Delphi round was completed by core and resource workgroup members in March 2011, the results of which were again discussed within the specific workgroups.
Finally, in April 2011, a two-day integration meeting was held in Washington, DC for co-chairs of the domain workgroups to distill the global health competencies into one model. Until that point, workgroups had independently been developing their domain definitions and competencies, and although staff and the consultant had alerted workgroup co-chairs to content that overlapped among the seven workgroups, this was the co-chairs' first opportunity to view the model in a holistic manner. Co-chairs of each of the seven domain workgroups presented their deliberations and then refined the draft slate of competencies. Based upon the co-chairs' consensus for the model's preamble and domain names, definitions, and competencies, project staff and the consultant, with input from the Leadership Group, prepared a final draft model for dissemination during the external review process.
In addition to the hundreds of global health experts who assisted in the development and vetting of the model, additional stakeholders were afforded multiple opportunities to offer feedback throughout the development process. These opportunities included a panel presentation at the 2010 American Public Health Association annual meeting, panel presentations at the 2010 and 2011 Global Health Council annual meetings, reports to the ASPH Global Health Committee, reports to the ASPH Education Committee, e-mails with the deans of ASPH member schools, and an open electronic comment period announced through the ASPH Friday Letter. During the open electronic comment period, or external review, frequently asked questions were developed to assist in the dissemination and understanding of the model. Based on responses from the external review, Model Version 1.0 was revised into the final Model Version 1.1.
Results
The modified Delphi rounds generated a response rate of 100%, 87%, and 72% for rounds one, two, and three, respectively (Table 2). Of the 149 workgroup participants, 70% (N = 105) reported being academics, and 30% (N = 44) reported being practitioners; 9% reportedly resided outside of the United States.
Table 2.
Response rates by core and resource workgroup members by domain and round
| Domain | Round 1 | Round 2 | Round 3 | ||||
|---|---|---|---|---|---|---|---|
| No. in workgroup | No. completed | No. in workgroup | No. completed | No. in workgroup | No. completed | ||
| 1 | Capacity strengthening | 9 | 9 | 27 | 23 | 27 | 21 |
| 2 | Collaborating and partnering | 10 | 10 | 24 | 19 | 24 | 16 |
| 3 | Ethical reasoning and professional practice | 9 | 9 | 17 | 15 | 17 | 13 |
| 4 | Health equity and social justice | 9 | 9 | 19 | 16 | 19 | 15 |
| 5 | Program management | 7 | 7 | 17 | 16 | 17 | 13 |
| 6 | Socio-cultural and political awareness | 10 | 10 | 18 | 16 | 18 | 13 |
| 7 | Strategic analysis | 8 | 8 | 27 | 24 | 27 | 17 |
| Total | 62 | 62 | 149 | 129 | 149 | 108 | |
| Response rate | 100% | 87% | 72% | ||||
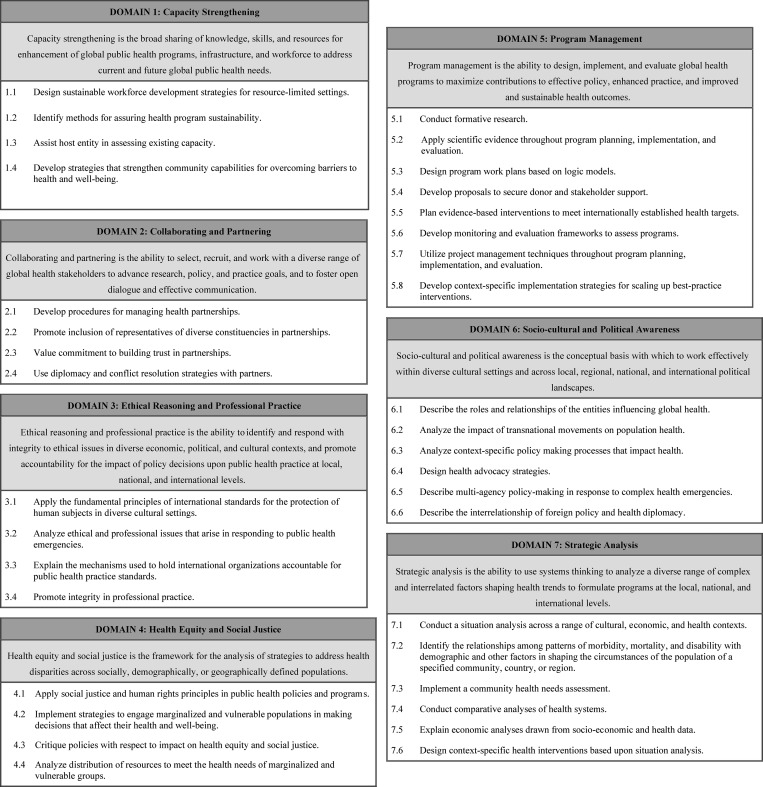
Respondents to each of the rounds contributed to significantly reducing the number of competencies (N = 793 in the first round) and clarifying remaining competencies (Table 3). Model 1.1, released in November 2011 (Figure 2), 36 competencies (Table 3) under the seven domains (Table 1).
Table 3.
Number of competencies at each stage of process
| Domain | Delphi 1 | Delphi 2 | Delphi 3 | Integration meeting | Model 1.0 | Model 1.1 | |
|---|---|---|---|---|---|---|---|
| No. of comps | No. of comps | No. of comps | No. of comps | No. of comps | No. of comps | ||
| 1 | Capacity strengthening | 129 | 52 | 24 | 7 | 4 | 4 |
| 2 | Collaborating and partnering | 124 | 33 | 29 | 9 | 6 | 4 |
| 3 | Ethical reasoning and professional practice | 68 | 35 | 17 | 7 | 4 | 4 |
| 4 | Health equity and social justice | 95 | 65 | 32 | 10 | 4 | 4 |
| 5 | Program management | 154 | 36 | 24 | 9 | 8 | 8 |
| 6 | Socio-cultural and political awareness | 115 | 59 | 27 | 12 | 6 | 6 |
| 7 | Strategic analysis | 108 | 58 | 31 | 10 | 4 | 6 |
| Total | 793 | 338 | 184 | 64 | 36 | 36 |
Figure 2.
Global Health Competency Model 1.1.
Discussion
Global Health Competency Model 1.1 proposes skills that are specific to global health practice, regardless of context, location, or scale of the work. It reflects the diversity of infrastructural, socio-cultural, and political environments in which practitioners must be able to perform the global health competencies. These skills are useful in settings both domestic and outside the borders of one's host country. Similarly, the competencies are specifically designed to be applied within and across any country or countries. Although the manner of application will vary by circumstance, they are broad enough to be applicable in any setting.
Experts identified the global health literature and the ASPH MPH Core Competency Model as foundations upon which global health competencies should be constructed. Indeed, the MPH competencies are considered foundational to the global health competencies, building upon and complementing, rather than replacing them. As such, the goal of this project, to promote population health, safety, and well-being at local and global levels by enhancing students' global health competence, suggests the competencies are positioned at what, in practice, is an interesting confluence of global health and public health. An ASPPH task force, working on a project called “Framing the Future: The Second 100 Years of Public Health,” is reviewing the full spectrum of public health education and is considering this global health competency model as it explores delivering new recommendations to update the MPH for the 21st century.18
The model's competencies are almost evenly split between the higher (e.g., analysis, synthesis, and evaluation) and lower (e.g., remember, understand, and apply) strata of the cognitive domain in Bloom's taxonomy, which reflect the development of one's abilities and skills.17,19 However, a few of the competencies reside in Bloom's affective domain (e.g., valuing), which describes one's interests, attitudes, values, and are critical both to improving students' academic performance20 and heightening the efficacy of students' learning experiences.21
The proposed model is not prescriptive; it serves as a framework regarding expectations of graduates entering the workforce. As such, it may stimulate conversations at both school and program levels regarding a consistency in building and achieving educational goals. It is anticipated that graduates from schools and programs that successfully implement and use this model would be adequately prepared to contribute to global health.
A challenge for faculty is that competencies are action-based, thus requiring less passive approaches to student-learning.6 Because each faculty's experience in competency-based education is variable, development of competency-based educational pedagogy and curriculum development skills are recommended for faculty, in conjunction with promoting use of the model.
In addition, faculty may be faced with personal content gaps in some areas included among the competencies, such as in 1.1 “Design sustainable workforce development strategies for resource-limited settings” (Figure 2). Although an instructor may be experienced in competency-based teaching, he or she may not have immediate knowledge of the appropriate material for use in teaching to a particular competency. The authors support increasing resources for faculty development to enhance educators' teaching, as called for by Frenk and colleagues in a recent report.22
Although competency models provide useful guides in pedagogy, they have little value without the dedicated effort to match the model to a school mission or program/departmental objectives and, subsequently aligning the model with sub-competencies, learning objectives, educational experiences, and assessments. This process usually requires mapping the competency model to existing coursework which, in many cases, exposes deficiencies in the curricula. When discovered, the missing content needs to be reconciled with the overall aims of the educational program so that, indeed, the school is delivering what it promises to both students and future employers.
Limitations.
This project's modified-Delphi process, which engaged nearly 150 global health experts to identify and come to consensus about the fundamental elements that constitute global health, was transparent, open, and well-communicated with the stakeholders. The grounding of the model in theory and evidence, as supplied by the broad range of practice and academic contributors to its development, including employers of the target audience in the competency model, will, however, need to be validated against the broad practice of global public health. Evaluation of students' proficiency in performing the proposed competencies is required to affirm or adjust the model to optimize its value to producing successful graduates for the global health workforce.
With regard to methods, midway through the competency development project, ASPH changed consultants. The second consultant, with approval of the project chairs, tweaked the methodology, thus facilitating workgroups to focus on streamlining the final two rounds of competency refinement and distilling the resulting competencies to their clearest possible meanings.
Conclusions
The Global Health Competency Model 1.1 provides a platform for engaging educators, students, and global health employers in discussion of the KSAs needed to improve human health on a global scale. The model may be used by graduate-level educators, in part or in full, to better prepare students in schools and programs of public health and global health education programs for the workforce. The competency model is also applicable to those implementing a broader public health curriculum that integrates global health throughout the curriculum. Furthermore, the model will assist faculty in preparing students from a variety of global health programs across institutions such as international relations/affairs, health profession schools, law schools, business schools, and social and biologic sciences. As such, students able to demonstrate the full array of knowledge, skills, and attitudes as depicted in the model will be better prepared for a wide variety of global workforce positions.
ACKNOWLEDGMENTS
We are grateful for the assistance of Joanne Russell, Director of the Center for Global Health at the University of Pittsburgh Graduate School of Public Health, who provided valuable feedback during the development of this manuscript. We acknowledge Judith Calhoun at the University of Michigan, for her role in helping plan and design the initial structure for the project. Finally, we acknowledge the more than 150 global health professionals who participated in the ASPH Global Health Competency Development Project. The American Society of Tropical Medicine and Hygiene assisted with publication expenses.
Footnotes
Authors' addresses: Elizabeth Ablah, Department of Preventive Medicine and Public Health, University of Kansas School of Medicine-Wichita, Wichita, KS, E-mail: eablah@kumc.edu. Dorothy A. Biberman, Global Health, Association of Schools and Programs of Public Health, Washington, DC, E-mail: dbiberman@aspph.org. Elizabeth M. Weist, Special Projects, Association of Schools and Programs of Public Health, Washington, DC, E-mail: eweist@aspph.org. Pierre Buekens, Office of the Dean, Tulane University School of Public Health and Tropical Medicine, New Orleans, LA, E-mail: pbuekens@tulane.edu. Margaret E. Bentley, Associate Dean for Global Health, University of North Carolina at Chapel Hill Gillings School of Global Public Health, Chapel Hill, NC, E-mail: pbentley@unc.edu. Donald Burke, Office of the Dean, University of Pittsburgh Graduate School of Public Health, Pittsburgh, PA, E-mail: donburke@pitt.edu. John R. Finnegan, Jr., University of Minnesota School of Public Health, Minneapolis, MN, E-mail: sphdean@umn.edu. Antoine Flahault, Descartes School of Medicine, Sorbonne Paris Cité - Hôtel-Dieu, Paris, France, E-mail: antoine.flahault@parisdescartes.fr. Julio Frenk, Office of the Dean, Harvard School of Public Health, Boston, MA, E-mail: jfrenk@hsph.harvard.edu. Audrey R. Gotsch, Department of Health Education and Behavioral Science, School of Public Health, Rutgers, The State University of New Jersey, Piscataway, NJ, E-mail: audrey.gotsch@rutgers.edu. Michael J. Klag, Office of the Dean, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, E-mail: mklag@jhsph.edu. Mario Henry Rodriguez Lopez, Instituto Nacional de Salud Pública, Ahucatitian, Cuernavaca, Mexico, E-mail: mhenry@correo.insp.mx. Philip Nasca, University at Albany SUNY School of Public Health, Rensselaer NY, E-mail: pnasca@albany.edu. Stephen Shortell, University of California Berkeley School of Public Health, Berkeley, CA, E-mail: shortell@berkeley.edu. Harrison C. Spencer, President and CEO, Association of Schools and Programs of Public Health, Washington, DC, E-mail: hspencer@aspph.org.
References
- 1.Frenk J. The global health system: strengthening national health systems as the next step for global progress. PLoS Med. 2010;375:e1000089. doi: 10.1371/journal.pmed.1000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fried LP, Bentley ME, Buekens P, Burke DS, Frenk JJ, Klag MJ, Spencer HC. Global health is public health. Lancet. 2010;375:535–537. doi: 10.1016/S0140-6736(10)60203-6. [DOI] [PubMed] [Google Scholar]
- 3.Gebbie KM, Rosenstock L, Hernandez LM. Who Will Keep the Public Healthy: Educating Public Health Professionals for the 21st Century. Washington, DC: National Academies Press; 2003. http://www.nap.edu/openbook.php?record_id=10542&page=R1 Available at. Accessed December 19, 2011. [PubMed] [Google Scholar]
- 4.Fischer K, Glenn D. Five college majors on the rise. Chronicle of Higher Education. 2009 http://chronicle.com/article/5-College-Majors-On-the-Rise/48207 Available at. Accessed September 10, 2011. [Google Scholar]
- 5.Rosenstock L, Helsing K, Rimer BK. Public health education in the United States: then and now. Public Health Rev. 2011;33:39–65. doi: 10.1007/BF03391620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calhoun JG, Spencer HC, Buekens P. Competencies for global health graduate education. Infect Dis Clin North Am. 2011;25:575–592. doi: 10.1016/j.idc.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 7.Arthur MA, Battat R, Brewer TF. Teaching the basics: core competencies in global health. Infect Dis Clin North Am. 2011;25:347–358. doi: 10.1016/j.idc.2011.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Finch TH, Chae SR, Shafaee MN, Siegel KR, Ali MK, Tomei R, Panjabi R, Kishore SP. Role of students in global health delivery. Mt Sinai J Med. 2011;78:373–381. doi: 10.1002/msj.20254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hagopian A, Spigner C, Gorstein JL, Mercer MA, Pfeiffer J, Frey S, Benjamin L, Gloyd S. Developing competencies for a graduate school curriculum in international health. Public Health Rep. 2008;123:408–414. doi: 10.1177/003335490812300325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Finberg HV, Hunter DJ. A global view of health: an unfolding series. N Engl J Med. 2013;368:78–79. doi: 10.1056/NEJMe1208801. [DOI] [PubMed] [Google Scholar]
- 11.ASPHa . Association of Schools of Public Health; 2012. Global Health Competency Model.http://www.asph.org/document.cfm?page=1084 Available at. Accessed May 25, 2012. [Google Scholar]
- 12.ASPHb . Association of Schools of Public Health; 2012. MPH Core Competency Model.http://www.asph.org/document.cfm?page=851 Available at. Accessed October 3, 2012. [Google Scholar]
- 13.ASPHc . Association of Schools of Public Health; 2012. Global Health Competency Development – ASPH Resources.http://www.asph.org/document.cfm?page=1098 Available at. Accessed May 25, 2012. [Google Scholar]
- 14.ASPHd . Association of Schools of Public Health; 2012. Global Health Competency Development – External Resources.http://www.asph.org/document.cfm?page=1099 Available at. Accessed May 25, 2012. [Google Scholar]
- 15.Battat R, Seidman G, Chadi N, Chanda MY, Nehme J, Hulme J, Li A, Faridi N, Brewer TF. Global health competencies and approaches in medical education: a literature review. BMC Med Educ. 2010;10:94. doi: 10.1186/1472-6920-10-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brewer TF, Saba N, Clair V. From boutique to basic: a call for standardized medical education in global health. Med Educ. 2009;43:930–933. doi: 10.1111/j.1365-2923.2009.03458.x. [DOI] [PubMed] [Google Scholar]
- 17.Bloom BS, Engelhart MD, Furst EJ, Hill WH, Krathwohl DR. Taxonomy of Educational Objectives: The Classification of Educational Goals. Handbook I: Cognitive Domain. New York: David McKay; 1956. [Google Scholar]
- 18.ASPHe . Association of Schools of Public Health; 2012. Framing the Future: The Second 100 Years of Education for Public Health.http://www.asph.org/document.cfm?page=1218 Available at. Accessed October 25, 2013. [Google Scholar]
- 19.ASPHf . Association of Schools of Public Health; 2012. Anderson & Krathwohl's Revised Bloom's Taxonomy Classifications Applied to Global Health Core Competency Model 1.1.http://www.asph.org/UserFiles/GHComps-Version1.1_Taxonomy.pdf Available at. Accessed on May 25, 2012. [Google Scholar]
- 20.Elias MJ, Zins JE, Weissberg RP, Frey KS, Greenberg MT, Haynes NM, Kessler R, Schwab-Stone ME, Shriver TP. Promoting Social and Emotional Learning: Guidelines for Educators. Alexandria, VA: Association for Supervision & Curriculum Development; 1997. http://www.ascd.org/Publications/Books/Overview/Promoting-Social-and-Emotional-Learning.aspx Available at. [Google Scholar]
- 21.Liff SB. Social and emotional intelligence: applications for developmental education. J Dev Educ. 2003;26:28–34. [Google Scholar]
- 22.Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, Fineberg H, Garcia P, Ke Y, Kelley P, Kistnasamy B, Meleis A, Naylor D, Pablos-Mendez A, Reddy S, Scrimshaw S, Sepulveda J, Serwadda D, Zurayk H. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]