Abstract
Victims of electrical burns account for approximately 5% of admissions to major burn centers. The first case of visceral injury caused by electrical burns was described in 1927 by Simonin, who reported perforation of the small intestine. Other rare cases were reported over the following years. The colon and small intestine were the organs most frequently affected. Less frequently involved organs were the heart, esophagus, stomach, pancreas, liver, gallbladder, lung, and kidney. We highlight the potential fatal visceral injuries after the electrical trauma. This study provides a review on this topic and proposes a management flowchart that should be adopted by the multidisciplinary team to treat these patients. Conclusion: Visceral injuries are rare in electrical burns victims, but it can be severe and are associated with high rates of morbidity and mortality, sometimes requiring a more interventional approach.
Keywords: Electrical burn, pancreatic injuries, visceral injuries, electrical shock
Introduction
Victims of electrical burns account for approximately 5% of admissions to major burn centers [1,2]. Traumas due to high-voltage currents (>1,000 V, 50 Hz) are generally associated with work accidents in which the worker comes into direct contact with the energy source, or indirectly through conductive materials or equipment [3].
The damage caused by electrical burns is the result of heat and of the electrical current passing through tissues, causing coagulative necrosis and cell membrane rupture. The resistance of tissue to the passage of an electrical current is variable and is lower for nerves and vessels and higher for fat and bones. An electrical current of the same intensity can cause variable damage depending on the susceptibility of each individual and the quality of care provided at the site of the accident [4].
Survivors of electrical burns have injuries at the entrance and exit site of the electrical current and potential visceral injuries whose severity is generally disproportional to the body surface burned [5,6]. Visceral lesions are rare, but potentially severe. They are associated with high morbidity and mortality and sequelae of variable magnitude, and often require more interventional approaches. Therefore, visceral injuries should always be remembered in the case of electrical burns and should be managed adequately by a multidisciplinary team.
The first case described of visceral injury caused by electrical burns was in 1927 by Simonin, who reported perforation of the small intestine [7,8]. Other rare cases were reported over the following years. The colon and small intestine were the organs most frequently affected. Less frequently involved organs were the heart, esophagus, stomach, pancreas, liver, gallbladder, lung, and kidney [3,9-11]. In 1945, Glazer reported three cases of pancreatic necrosis diagnosed during autopsy of two patients hit by lightning and one patient after electrocution [12].
The severity of electrical burns is determined by the voltage, amperage and type of current (alternating or continuous), direction of flow, duration of contact, resistance at the entrance point, and individual susceptibility. Tissue injuries are caused by a combination of thermal and non-thermal mechanisms. As it passes through tissues, electricity generates heat according to Joule’s law: heat (Joule, J) = I² (current) × R (resistance). The increase in temperature causes the denaturation of macromolecules which is usually irreversible [13]. Also, the electrical current alters the transmembrane potential and muscle fibers and nerves are the most susceptible structures.
Electroporation can induce cell necrosis in the absence of heat [14-16]. Transmembrane protein molecules contain polar amino acid residues that may alter their orientation in response to the passage of an electrical current. This effect, known as electro conformational denaturation of membrane proteins, is usually irreversible and represents another mechanism of non-thermal injury [17].
Management of electrical burns according to the Advanced Trauma Life Support (ATLS), Advanced Burn Life Support (ABLS) and Advanced Cardiac Life Support (ACLS) guidelines is fundamental. Ventricular fibrillation is a known cause of sudden death after electrical burn injury and cardiac monitoring is therefore critical during the first 24 h after trauma [18].
Electrical burns and visceral injuries
Although rare, visceral injuries resulting from electrical burns should be taken into account, investigated, and treated adequately. Approximately 15% of these patients have other associated traumatic injuries resulting from falls, bodily collisions with objects and tetanic contractions due to shock, which must not be neglected [4].
We recently treated in our hospital a rare case of polytrauma after high-voltage electrical current injuries associated with a pancreatic electrocution. The medical report stated cardiopulmonary arrest caused by ventricular fibrillation for thirty min, which was reversed after maneuvers recommended by the Advanced Cardio-vascular Life Support (ACLS). Already intubated, the patient was admitted to the Trauma Room of the Emergency Unit of Hospital das Clínicas de Ribeirão Preto, University of São Paulo (HCRP-USP). The patient had non-circumferential third-degree burns on the hands, predominantly on the dorsal surface from the right index to ring finger and on the palmar surface of the left index and middle fingers, and second-degree burns on the forearms and chest, corresponding to 15% of TBSA. The first tests showed signs of rhabdomyolysis (metabolic acidosis; serum creatinine = 1.8 mg/dl; CPK = 4,188 U/l) and hyperamylasemia (1,087 U/l). An abdominal computed tomography scan was suspicious of gastric bleeding, pancreatic laceration (AAST grade III), lacerations in the left kidney (AAST grade III), left adrenal hemorrhage, hemoperitoneum, and a left retroperitoneal hematoma (Figure 1). The patient was submitted to exploratory laparotomy by the general surgical team, which showed a moderate volume of blood in the abdominal cavity, a perforation with charred borders in the mesentery of the transverse colon without intestinal ischemia, and a left perirenal hematoma extending to the left parietocolic gutter. In addition, there was serosal injury in the posterior gastric wall and a charred laceration in the distal third of the pancreas, compromising half of its transverse diameter (Figure 2). Caudal pancreatectomy and splenectomy were performed. A three-way vesical catheter was installed for intra-abdominal pressure monitoring at intervals of 4 h. A febrile plateau and worsening of renal function were observed over the next days that were not correlated with alterations in intra-abdominal pressure, which ranged from 12 to 20 mmHg. Hemodialysis and antibiotics were initiated. Renal failure was attributed to nephrotoxicity resulting from empirical antibiotic therapy initiated after the onset of fever. On day 15 of hospitalization, the patient presented massive hematemesis and worsening of hemodynamic parameters. Upper gastrointestinal endoscopy revealed esophagitis and adherent blood clots in the fundus and gastric body. Twenty days after laparotomy, the abdominal wall was resutured due to evisceration and examination of the abdominal cavity showed no relevant findings. Laboratory testing of the intra-abdominal fluid revealed normal amylase and culture was positive for Gram-negative rods. The patient remained hospitalized in the ICU in serious condition. Amputation of the ring finger and rotation of a local flap to cover the right middle finger were indicated, but the patient’s clinical conditions did not permit the procedure. The general condition of the patient worsened and he died one month after admission. Anatomopathological examination confirmed the suspicion of electrical burns in the pancreas (Figure 3A and 3B).
Figure 1.
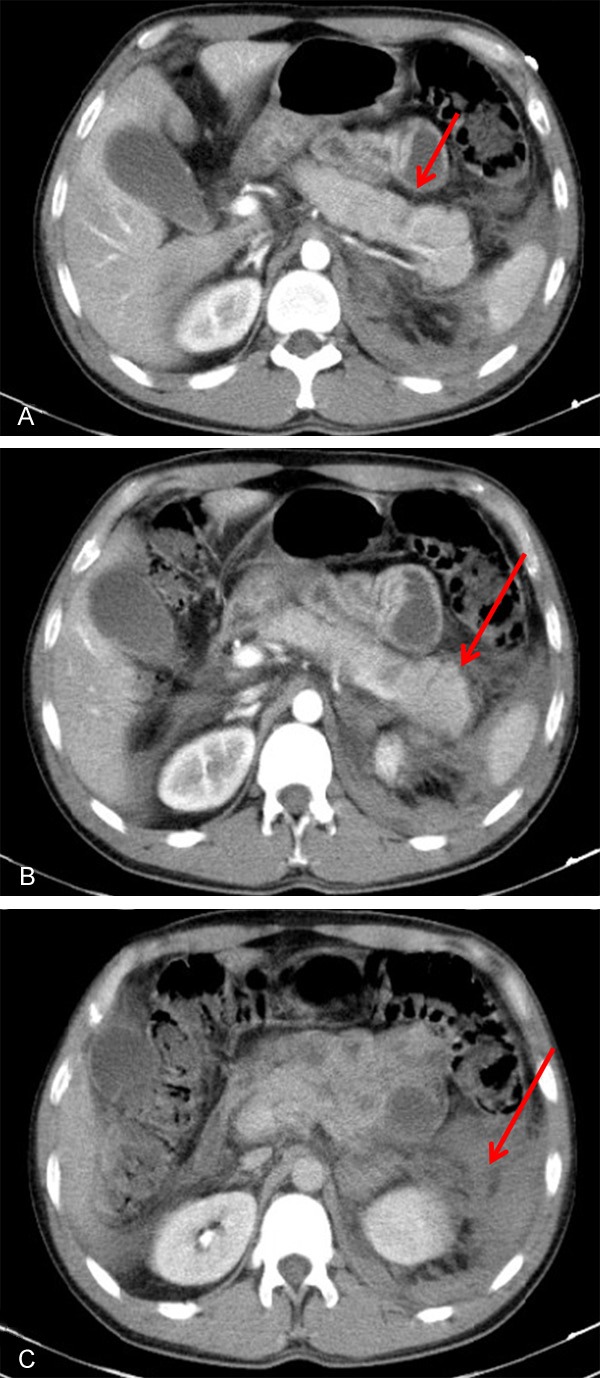
Sequential computed tomograph scans of the abdomen showing pancreatic laceration (A: arrow), edema of the pancreatic tail (B: arrow), and a left retroperitoneal hematoma (C: arrow).
Figure 2.

Intraoperative image after exposure of the pancreas showing the laceration with charred edges at the body-tail transition.
Figure 3.

A: Gross inspection: note the blackened areas on the surface of the pancreatic parenchyma specimen, corresponding to coagulative necrosis. B: Microscopic analysis (100x magnification): area of coagulative necrosis in the upper half of the image compared to normal parenchyma in the lower half.
The present patient was initially evaluated as a polytraumatized electrical burn victim. The general surgery and trauma team opted to perform an exploratory laparotomy in view of the hemodynamic instability of the patient and visceral injuries identified by computed tomography, considering blunt abdominal trauma. Until then, these injuries could be explained by passage of the electrical current or biomechanical mechanisms related to trauma. The suspicion of visceral damage due to electrical current was supported by the intraoperative findings of carbonization of the mesentery of the transverse colon and pancreatic laceration, inferring that the electrical current had entered through the left hand, passed through the base of the thorax and upper abdomen, and left through the right hand. This suspicion was confirmed by anatomopathological analysis of a pancreatic fragment obtained by caudal pancreatectomy, which revealed coagulative necrosis associated with initial hyperamylasemia.
The clinical and radiologic findings did not permit to establish the true mechanism of injury to the left kidney due to the association with fall from a height. There was no need for surgical exploration since the injury was classified as AAST grade III. On the other hand, the development of cardiac arrhythmia as a result of ventricular fibrillation suggests heart damage that may have also been caused by passage of the electrical current.
Pancreatic involvement in burn patients is described indirectly in the literature as acute pancreatitis. In a retrospective study of adult patients with major burns, Ryan et al [19] found that 40% of the patients had hyperamylasemia and hyperlipasemia which were temporarily associated with infections, inhalation injury, trauma, and escharotomy. However, in a thorough search of the Pubmed-Medline database we found no explicit cases of pancreatic burns due to electrical current other than the postmortem cases reported by Glazer [12].
In a retrospective review of severe complications in electrical burns that included 1,065 patients and comprised a period of 13 years, Haberal et al [9] reported two cases of gastrointestinal bleeding and one case of gastric perforation. The present patient also had gastrointestinal bleeding suggested by the initial abdominal tomography scan and exteriorized through hematemesis during hospitalization. Endoscopy was nonspecific in terms of the etiology of bleeding. Care was taken since that patient had been admitted in order to prevent Curling ulcer by adequate clinical management and intravenous administration of proton pump inhibitors. However, gastric mucosal injury caused by the electrical current could not be ruled out as a possible etiology of gastrointestinal hemorrhage.
Electrical burns and abdominal compartment syndrome
The development of abdominal compartment syndrome in patients with major burns is generally related to the extent of injury and oversupply of the resuscitation fluid volume administered. Associated abdominal trauma represents an additional risk factor for the development of this condition. The negative impact of a progressive increase in intra-abdominal pressure and consequent abdominal compartment syndrome has been recognized in intensive care units and surgical units. Surgical decompression continues to be the gold standard for the rapid and definitive treatment of this condition. Patients with an intra-abdominal pressure ≥ 25 mmHg associated with organ dysfunction or failure should be submitted immediately to surgical decompression [20,21].
In view of the impact of medical care on the survival of abdominal electrical burn victims, we propose a guideline for the monitoring and treatment of these patients after initial resuscitation (Figure 4).
Figure 4.

Guideline proposal for the management of patients with severe electrical burns. IAP: intra-abdominal pressure; ECG: electrocardiogram; CT: computed tomography; ATLS: Advanced Trauma Life Support; ABLS: Advanced Burn Life Support; ACLS: Advanced Cardiac Life Support.
Conclusion
The adequate treatment of patients with electrical burns requires the availability of an intensive care unit and surgical center, a multidisciplinary team including clinicians, intensivists, nephrologists, plastic surgeons, general surgeons, trauma surgeons, and orthopedists, as well as other professionals involved in the treatment and rehabilitation of these patients such as qualified nurses and practical nurses, physiotherapists, psychologists, occupational therapists, nutritionists, and nutrition experts.
After initial resuscitation, additional damage should be prevented in abdominal electrocution by an early diagnosis of segmental or abdominal compartment syndrome, and tissue necrosis. Electrocardiographic, hemodynamic and intra-abdominal pressure monitoring is fundamental, as is maintenance of water balance and adequate management of rhabdomyolysis to prevent renal and heart failure. Potential visceral injuries should always be suspected in polytraumatized patients with electrical burns and detailed analysis of the mechanism of trauma is necessary. Thorough physical examination combined with imaging methods and laboratory tests permits the early diagnosis of severe injuries, reducing morbidity and mortality by enabling early intervention. The path of the electrical current through the body cannot be determined accurately and can often only be suggested based on the detection of abdominal visceral injuries by exploratory laparotomy or laparoscopy. In the case of pancreatic injuries, involvement of the major pancreatic duct is the main prognostic factor and requires immediate surgical treatment to reduce complications and the length of hospital stay.
Although rare, abdominal trauma produced by electrical currents is associated with high morbidity and mortality. This paper proposes a treatment guideline designed to permit early intervention, the prevention of additional damage and late complications, and progressive improvement in the prognosis of these patients.
Disclosure of conflict of interest
None.
References
- 1.Lee RC. Injury by electrical forces: pathophysiology, manifestations and therapy. Curr Probl Surg. 1997;34:677–764. doi: 10.1016/s0011-3840(97)80007-x. [DOI] [PubMed] [Google Scholar]
- 2.Esselman PC, Thombs BD, Magyar-Russell G, Fauerbach JA. Burn rehabilitation: state of the science. Am J Phys Med Rehabil. 2006;85:383–418. doi: 10.1097/01.phm.0000202095.51037.a3. [DOI] [PubMed] [Google Scholar]
- 3.Masanés MJ, Gourbiére E, Prudent J, Lioret N, Febvre M, Prévot S, Lebeau B. A high voltage electrical burn of lung parenchyma. Burns. 2000;26:659–63. doi: 10.1016/s0305-4179(00)00035-8. [DOI] [PubMed] [Google Scholar]
- 4.Arnoldo BD, Purdue GF. The diagnosis and management of electrical injuries. Hand Clin. 2009;25:469–79. doi: 10.1016/j.hcl.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 5.GourbieÁre E, Corbut JP, Brazin Y. Functional consequence of electrical injury. Electrical injury: a multidisciplinary approach to therapy, prevention and rehabilitation. Ann N Y Acad Sci. 1994;720:259–71. doi: 10.1111/j.1749-6632.1994.tb00285.x. [DOI] [PubMed] [Google Scholar]
- 6.Bingham H. Electrical burns. Clin Plast Surg. 1986;13:75–85. [PubMed] [Google Scholar]
- 7.Williams DB, Karl RC. Intestinal injury associated with low-voltage electrocution. J Trauma. 1981;21:246–50. doi: 10.1097/00005373-198103000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Branday JM, DuQuesnay DR, Yeesing MT, Duncan ND. Visceral complications of electrical burn injury. West Indian Med J. 1989;38:110–13. [PubMed] [Google Scholar]
- 9.Haberal M, UQar K, Bayraktar O, Oner R. Severe complications in electrical burns (including visceral complications) Ann Burns and Fire Disaster. 1996;9:149–53. [Google Scholar]
- 10.Velho AV, Strappazzon JL, Giabatti G. Trauma abdominal penetrante consecutive a corrente elétrica industrial. Rev Col Bras Cir. 2010;27:287–89. [Google Scholar]
- 11.Azevedo MA, Oliveira LAM, Tardelli HC, Farina JA Jr. Queimadura elétrica com trauma renal: relato de um caso. Rev Bras Queimaduras. 2008;7:42–44. [Google Scholar]
- 12.Glazer AM. Pancreatic necrosis in electric shock. Arch Pathol. 1945;39:9–10. [Google Scholar]
- 13.Tuttnauer A, Mordzynski SC, Wess YG. Electrical and lightning injuries. Contemp Crit Care. 2006;7:1–10. [Google Scholar]
- 14.Lee RC, Zhang D, Hanning J. Biophysical injury mechanisms in electrical shock trauma. Ann Rev Biomed Eng. 2000;2:477–509. doi: 10.1146/annurev.bioeng.2.1.477. [DOI] [PubMed] [Google Scholar]
- 15.Block TA, Aarswold JN, Matthews KL, Mintzer RA, River LP, Capelli-Schellpfeffer M, Wollmann RL, Tripathi S, Chen CT, Lee RC. The 1995 Lindberg Award. Nonthermally mediated muscle injury and necrosis in electrical trauma. J Burn Care Rehabil. 1995;16:581–8. [PubMed] [Google Scholar]
- 16.DeBono R. A histological analysis of a high voltage electric current injury to an upper limb. Burns. 1999;25:541–7. doi: 10.1016/s0305-4179(99)00029-7. [DOI] [PubMed] [Google Scholar]
- 17.Chen W, Lee RC. Altered ion channel conductance and ionic selectivity induced by large imposed membrane potential pulse. Biophys J. 1994;67:603–12. doi: 10.1016/S0006-3495(94)80520-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geddes LA, Bourland JD, Ford G. The mechanism underlying sudden death from electric shock. Med Instrum. 1986;20:303–15. [PubMed] [Google Scholar]
- 19.Ryan CM, Sheridan RL, Schoenfeld DA, Warshaw AL, Tompkins RG. Postburn pancreatitis. Ann Surg. 1995;222:163–170. doi: 10.1097/00000658-199508000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bersani AL, Gomes JO, Braga ILS, Guimaraes HP, Lopes RD. Síndrome compartimental abdominal. Rev Bras Clin Med. 2009;7:313–321. [Google Scholar]
- 21.World Society of the Abdominal Compartment Syndrome (WSACS) Intra-abdominal hypertension (IAH)/Abdominal Compartment Syndrome (ACS) management algorithm. 2007. Available at: http://www.wsacs.org/algorithms.php (accessed September 1, 2013)


