Abstract
Purpose.
To evaluate, by receiver operating characteristic (ROC) analysis, the ability of noncycloplegic retinoscopy (NCR), Retinomax Autorefractor (Retinomax), and SureSight Vision Screener (SureSight) to detect significant refractive errors (RE) among preschoolers.
Methods.
Refraction results of eye care professionals using NCR, Retinomax, and SureSight (n = 2588) and of nurse and lay screeners using Retinomax and SureSight (n = 1452) were compared with masked cycloplegic retinoscopy results. Significant RE was defined as hyperopia greater than +3.25 diopters (D), myopia greater than 2.00 D, astigmatism greater than 1.50 D, and anisometropia greater than 1.00 D interocular difference in hyperopia, greater than 3.00 D interocular difference in myopia, or greater than 1.50 D interocular difference in astigmatism. The ability of each screening test to identify presence, type, and/or severity of significant RE was summarized by the area under the ROC curve (AUC) and calculated from weighted logistic regression models.
Results.
For detection of each type of significant RE, AUC of each test was high; AUC was better for detecting the most severe levels of RE than for all REs considered important to detect (AUC 0.97–1.00 vs. 0.92–0.93). The area under the curve of each screening test was high for myopia (AUC 0.97–0.99). Noncycloplegic retinoscopy and Retinomax performed better than SureSight for hyperopia (AUC 0.92–0.99 and 0.90–0.98 vs. 0.85–0.94, P ≤ 0.02), Retinomax performed better than NCR for astigmatism greater than 1.50 D (AUC 0.95 vs. 0.90, P = 0.01), and SureSight performed better than Retinomax for anisometropia (AUC 0.85–1.00 vs. 0.76–0.96, P ≤ 0.07). Performance was similar for nurse and lay screeners in detecting any significant RE (AUC 0.92–1.00 vs. 0.92–0.99).
Conclusions.
Each test had a very high discriminatory power for detecting children with any significant RE.
Keywords: vision screening, refractive error, children's vision
This study showed that noncycloplegic retinoscopy, Retinomax Autorefractor, and SureSight Vision Screener each had a very high power for detecting preschool children with significant refractive errors.
Introduction
Significant refractive errors are the most prevalent and treatable vision problems in preschool children.1 A high prevalence of refractive error in young children has been established.2–10 Previous literature and clinical practice guidelines have identified an association between significant refractive error and amblyopia and strabismus.8,11–18 Research has also revealed educational and cognitive implications of uncorrected hyperopia.19–22 Therefore, significant refractive error is important to detect with vision screening.23–26
The Vision In Preschoolers (VIP) Study Group showed that screening tests of refraction (noncycloplegic refraction [NCR], Retinomax autorefractor [Retinomax], and SureSight Vision Screener [SureSight]) had excellent testability and performed best in identifying preschool children with VIP-targeted vision disorders, including significant refractive error, strabismus, and amblyopia.23 Furthermore, the VIP Study Group has shown that the Retinomax and SureSight can be used by trained eye care professionals, nurse screeners, or lay screeners to detect significant refractive errors.23–25
Although previous studies have evaluated detection of refractive error in preschool children using the Retinomax23–25,27–38 or SureSight,23–25,36–43 age range often varies amongst studies and the majority of studies focus on agreement between autorefraction and a gold standard measure of refraction. Few studies have performed receiver operating characteristic (ROC) curve analysis to examine the ability of NCR, Retinomax, or SureSight to detect or screen for specific types of refractive error. Because there is not complete agreement regarding the best specificity level for use in screening, ROC curve analysis is helpful to compare the performance of screening tests over the complete range of specificity levels.44 Using ROC analysis, Ying et al.45 showed that NCR, Retinomax, and SureSight had similar and high accuracy in detecting preschoolers enrolled in the VIP Study with any targeted vision disorders (amblyopia, strabismus, and significant refractive error) including the most severe conditions. However, the ability of these screening procedures to detect refractive error alone has not yet been evaluated in the VIP Study. Some screening programs may need to know the ability of a screening test of refraction to detect specific types of refractive error and significant refractive error overall because (1) prevalence and type of refractive error vary across race, ethnicity,3,10 and age, and (2) detection of specific refractive errors may vary with type of refractive error and instrument.36,46,47
Cordonnier and De Maertelaer38 used ROC curve analysis to evaluate the ability of SureSight and Retinomax to detect hyperopia greater than 3.0 diopters (D), myopia greater than 3.0 D, astigmatism greater than or equal to 2.0 D, and anisometropia greater than or equal to 1.5 D as determined by cycloplegic retinoscopy or autorefraction in 98 children ages 6 months to 16.5 years. They concluded that with the use of specific referral criteria both instruments were adequate for vision screening.38 However, the ability of these screening tests of refraction to identify preschool children with specific types of significant refractive error has not been investigated using ROC analysis in a large group of children. The purpose of this study is to evaluate the ability of NCR, Retinomax, and SureSight to detect specific refractive errors (hyperopia, myopia, astigmatism, and anisometropia) when used by different types of screeners, among the large number of preschool children enrolled in the VIP Study.
Methods
This is a secondary data analysis of the VIP data. The VIP Study methods have been published in detail previously.23–25 The relevant methods are described briefly below.
Subjects
During the VIP Study, 3- to 5-year-old Head Start preschool children (n = 4040) were enrolled at one of five VIP clinical centers (New England College of Optometry, Boston, MA; Northeastern State University Oklahoma College of Optometry, Tahlequah, OK; The Ohio State University College of Optometry, Columbus, OH; Pennsylvania College of Optometry at Salus University, Philadelphia, PA; and University of California Berkeley School of Optometry, Berkeley, CA). The proportion of children with vision problems was enriched in the VIP Study by recruiting all children who failed the local Head Start vision screening and a random sample of children who passed the screening. The VIP Study adhered to the tenets of the Declaration of Helsinki and was approved by the appropriate local institutional review boards associated with each VIP center. Parents or legal guardians of participating children provided written informed consent/parental permission prior to testing.
Measurement of Refractive Error
Each child's vision was screened using two tests of refraction. Testing was performed by pediatric licensed eye care professionals in mobile medical units in Phase I and by nurse and lay screeners in a school screening setting in Phase II. The VIP Study personnel were trained and certified in each procedure. In Phase 1, year 01, NCR and Retinomax (in automatic mode) (Right Manufacturing, Virginia Beach, VA) were performed. The eye care professional performed NCR using a streak retinoscope and retinoscopy lens rack or handheld trial lenses while the child watched an animated target on a video screen. The child wore retinoscopy spectacles, corresponding to the screener's working distance, to control accommodation. In Phase 1, year 02 and in Phase 2, the Retinomax and SureSight Vision Screener (in child mode) (Welch Allyn, School Health Corp., Hanover Park, IL) were used. As part of a comprehensive eye examination, cycloplegic retinoscopy was performed on all children on a later day by a different pediatric licensed eye care professional who was trained and certified in the procedures and who was masked to the screening results. Cycloplegic retinoscopy was performed 30 to 40 minutes after instillation of drops including 1% cyclopentolate.
Definitions of Vision Disorders and Classification of Children
Results from cycloplegic retinoscopy were used to classify children with respect to the presence or absence of each type of significant refractive error. If either or both eyes had significant refractive error, the child was considered to have significant refractive error. Hyperopia and myopia were defined as greater than 3.25 D or 2.00 D, respectively, in any meridian in either eye. Children with greater than 1.50 D difference between principal meridians were classified as having astigmatism. Anisometropia was defined as greater than 1.00 D interocular difference in hyperopia (most hyperopic meridian), or greater than 3.00 D interocular difference in myopia (most myopic meridian), or greater than 1.50 D interocular difference in astigmatism. Each type of significant refractive error was further classified into a hierarchy of groups or levels of severity (Table 1).
Table 1.
Definitions of Significant Refractive Errors in the VIP Study
|
|
Group 1 |
Groups 1 and 2 |
Groups 1, 2, and 3 |
| Hyperopia | ≥+5.0 D | >+3.25 D with IOD in SE of ≥+0.5 D | >+3.25 D with IOD in SE of <+0.5 D |
| Myopia | ≥6.0 D | ≥4.0 D | >2.0 D |
| Astigmatism | ≥2.5 D | >1.5 D | N/A |
| Anisometropia (IOD) | >2.0 D hyperopia, >3.0 D astigmatism, or >6.0 D myopia | >1.0 D hyperopia, >1.5 D astigmatism, or >3.0 D myopia | N/A |
IOD, intraocular difference; N/A, not applicable.
Children were classified as a screening pass or fail based upon the child's worse eye and using the following results for each screening test of refraction: most positive meridian for hyperopia, most negative meridian for myopia, cylinder for astigmatism, and maximum interocular difference for anisometropia.
Statistical Analysis
We assessed the accuracy of each screening test for detecting any significant refractive error and each type of refractive error (hyperopia, myopia, astigmatism, and anisometropia) using ROC curve analysis. The details of ROC curve analysis applied to the VIP Study data have been described previously by Ying et al.45 with respect to the performance of NCR, Retinomax, and SureSight in detecting preschoolers with one or more targeted vision disorders (amblyopia, strabismus, and significant refractive error).45 An ROC curve plots the sensitivity against the false positive rate (i.e., 1-specificity), in which each point reflects values obtained at a different cutpoint value from a continuous or ordinal measure. By calculating the area under the curve (AUC), the ROC analysis provides a summary of the discriminative ability for a screening test, and allows a quick comparison of discriminative ability among different screening tests. The AUC has a value from 0.0 to 1.0. An AUC greater than 0.9 is considered excellent, greater than 0.8 to 0.9 very good, 0.7 to 0.8 good, 0.6 to 0.7 average, and less than 0.6 poor.48
Although NCR, Retinomax, and SureSight provide measures of refractive error (sphere, cylinder, and axis for NCR and Retinomax, sphere and cylinder for SureSight) for each eye, the present ROC analysis is child-specific. As in real screening settings, if either eye fails the screening, the child is referred for a comprehensive eye examination. In the VIP Study, children who had failed the Head Start vision screening were preferentially recruited into the VIP study and therefore over represented. To take the sampling weights into account in the ROC analysis, we used weighted logistic regression, with the weights calculated as the inverse sampling probability specific to each clinical center. The empirical AUC and its 95% confidence interval (CI) were then calculated using ROC analysis functions available in the Logistic Regression Procedure in SAS v9.2 (SAS Institute, Inc., Cary, NC). When the AUC was compared between screening tests (NCR, Retinomax, SureSight) or between types of vision screeners performed on the same children, the statistical method described by Delong et al.49 was used to accommodate the correlation between the AUC estimates. All the statistical analyses were performed in SAS v9.2 (SAS Institute, Inc.), and a two-sided P value less than 0.05 was considered to be statistically significant.
Results
Table 2 shows the characteristics of the study population, including the number of children who met the criterion for each type of refractive error. In Phase 1, year 1, 1142 children were enrolled, in Phase 1 year 2, 1446 children were enrolled, and in Phase II, 1452 children were enrolled. In this group of children enriched for vision disorders, the proportion of children with any significant refractive error ranged from 21% to 26% (Table 2). The mean spherical equivalent (±SD) as measured with cycloplegic retinoscopy for the 8077 eyes of 4040 children was 1.41 D (±1.52 D), with a range from −20 D to +16.5 D. Spherical equivalent could not be calculated for three eyes because a sphere or cylinder measurement was not obtained.
Table 2.
Frequency Distribution of Significant Refractive Error by Hierarchy
|
Group 1 Only
n (%) |
Groups 1 and 2
n (%) |
Groups 1, 2, and 3
n (%) |
|
| VIP Phase 1, year 1, N = 1142 | |||
| Any significant refractive error | 123 (10.8) | 222 (19.4) | 240 (21.0) |
| Myopia | 8 (0.7) | 13 (1.1) | 28 (2.5) |
| Hyperopia | 56 (4.9) | 96 (8.4) | 122 (10.7) |
| Astigmatism | 64 (5.6) | 131 (11.5) | 131 (11.5) |
| Anisometropia | 10 (0.9) | 49 (4.3) | 49 (4.3) |
| VIP Phase 1, year 2, N = 1446 | |||
| Any significant refractive error | 146 (10.1) | 262 (18.1) | 299 (20.7) |
| Myopia | 7 (0.5) | 9 (0.6) | 25 (1.7) |
| Hyperopia | 67 (4.6) | 116 (8.0) | 168 (11.6) |
| Astigmatism | 82 (5.7) | 156 (10.8) | N/A |
| Anisometropia | 10 (0.7) | 47 (3.3) | N/A |
| VIP Phase II, N = 1452 | |||
| Any significant refractive error | 198 (13.6) | 337 (23.2) | 380 (26.2) |
| Myopia | 9 (0.6) | 11 (0.8) | 39 (2.7) |
| Hyperopia | 80 (5.5) | 124 (8.5) | 182 (12.5) |
| Astigmatism | 114 (7.9) | 218 (15.0) | N/A |
| Anisometropia | 19 (1.3) | 56 (3.9) | N/A |
Receiver operating characteristic curves and the areas under the ROC curve for any significant refractive error, myopia, hyperopia, astigmatism, and anisometropia are shown in Figures 1 to 5, respectively. Supplementary Tables S1 through S5 show the AUC for any significant refractive error, myopia, hyperopia, astigmatism, and anisometropia, respectively, by hierarchy (groups or levels of severity) and for each type of test and screener. For the detection of any significant refractive error overall, the AUC of each screening test was high. The AUC ranged from 0.97 to 1.00 for detecting the most severe (highest) levels of RE, and ranged from 0.92 to 0.93 for detecting any significant refractive error (Fig. 1, Supplementary Table S1). The AUCs were highest for myopia (NCR: 0.99; SureSight: 0.97–0.98; Retinomax: 0.97–0.98; Fig. 2, Supplementary Table S2), and astigmatism (NCR: 0.90–0.96; SureSight: 0.95–0.99; Retinomax: 0.95–0.99; Fig. 4, Supplementary Table S4). The AUCs were next highest for hyperopia (NCR: 0.92–0.99, SureSight: 0.85–0.94; Retinomax: 0.90–0.98), with the AUC ranging from 0.92 to 0.99 for the most severe (highest) level of hyperopia and from 0.85 to 0.94 for any hyperopia greater than 3.25 D (Fig. 3, Supplementary Table S3). The AUCs were somewhat lower for anisometropia (NCR: 0.82–0.92; SureSight: 0.85–1.00; Retinomax: 0.76–0.96), with higher AUCs for the most severe (highest) level of anisometropia (0.88–1.00) as compared with any significant anisometropia (0.76–0.91; Fig. 5, Supplementary Table S5).
Figure 1.
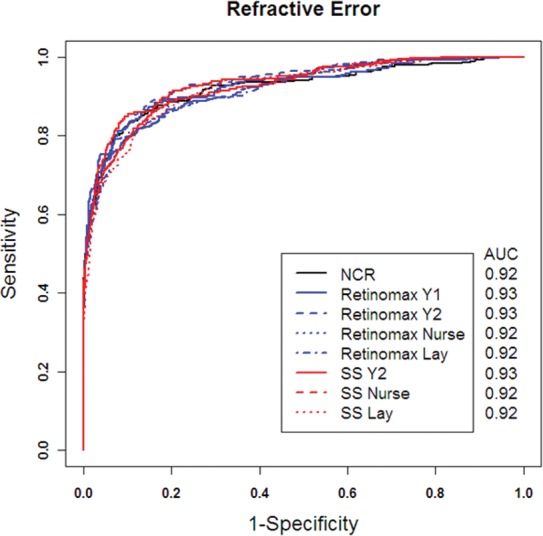
Receiver operating characteristic curves for overall refractive error.
Figure 5.
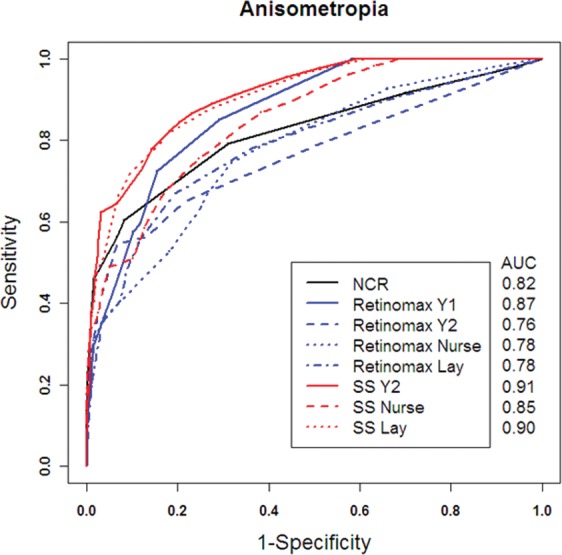
Receiver operating characteristic curves for anisometropia.
Figure 2.
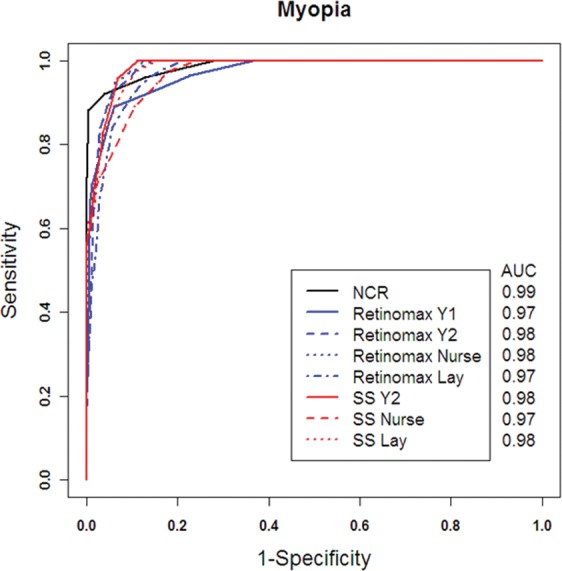
Receiver operating characteristic curves for myopia.
Figure 4.
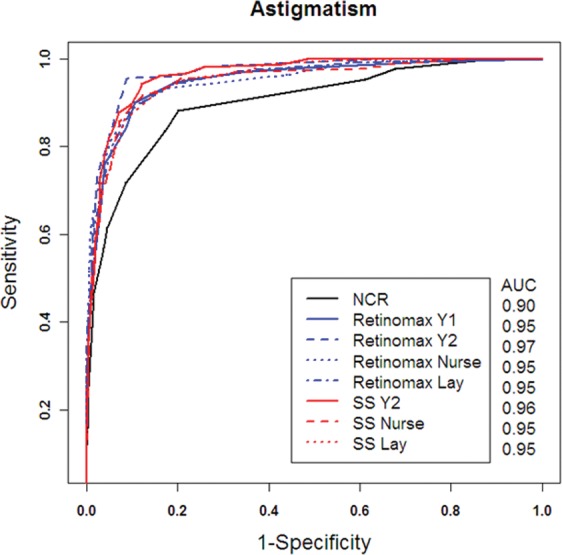
Receiver operating characteristic curves for astigmatism.
Figure 3.
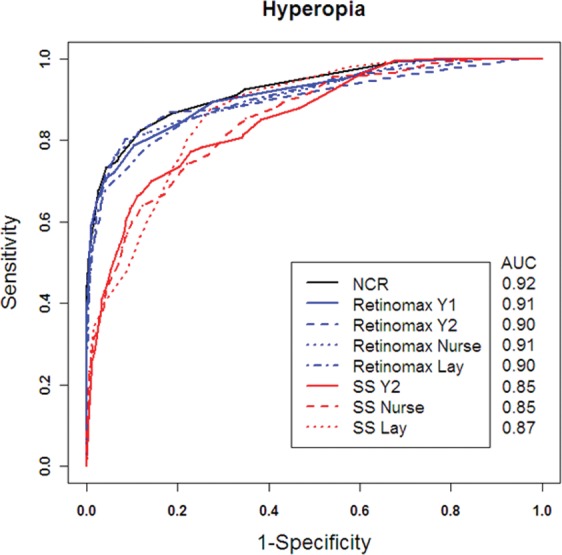
Receiver operating characteristic curves for hyperopia.
The Retinomax performed better than NCR for the detection of astigmatism greater than 1.50 D (AUC 0.95 vs. 0.90, P = 0.01; Fig. 4, Supplementary Table S4). The detection of hyperopia was better for NCR and Retinomax than for SureSight (AUC NCR: 0.92–0.99 and Retinomax: 0.90–0.98 versus SureSight: 0.85–0.94, P ≤ 0.02 for Retinomax versus SureSight). The differences between Retinomax and SureSight reached statistical significance for all three types of screeners for one or more severity levels of hyperopia (Fig. 3, Supplementary Table S3). The detection of anisometropia was better for SureSight than for Retinomax (AUC 0.85–1.00 vs. 0.76–0.96, P ≤ 0.07), with differences reaching statistical significance for nurse and lay screeners at both severity levels of anisometropia and for licensed eye care professionals for any significant anisometropia (Fig. 5, Supplementary Table S5).
For significant refractive error overall, performance was similar for nurse and lay screeners (AUC 0.92–1.00 vs. 0.92 to 0.99), with generally small, nonsignificant differences. NCR, Retinomax, and SureSight all had very high discriminatory power for detecting children with any significant refractive error when administered by pediatric licensed eye care professionals, pediatric nurse screeners, or lay screeners (Fig. 1, Supplementary Table S1). Differences in the AUC for the detection of each type of refractive error for pediatric nurse and lay screeners also were small and generally nonsignificant.
To provide the failure criteria that maximize the sensitivity for detecting presence of any significant refractive error by each screening test, we pooled data from all VIP phases because of the similarity in the ROC across all phases and determined the sensitivities at several specificity levels ranging from 50% to 90%. The sensitivities for detecting any significant refractive error, the most severe (group 1) level of refractive error, and each specific type of refractive error are provided in Supplementary Table S6. The corresponding failure criteria for detection of any significant refractive error are also provided in Supplementary Table S6. The cutoffs for failure criteria for detecting any significant refractive error differed among screening tests, depending on the type of refractive error. For example, for detection of significant refractive error overall at 90% specificity, the referral criteria varied from −1.00 D (SureSight) to −1.75 D (NCR) to −2.75 D (Retinomax) for myopia, from 1.50 D (Retinomax) to 2.5 D (NCR) to 3.75 D (SureSight) for hyperopia, from 1.50 D (NCR) to 1.75 D (SureSight, Retinomax) for astigmatism, and from 1.50 D (NCR) to 2.50 D (SureSight) or 2.75 D (Retinomax) for anisometropia.
Discussion
Detection of significant refractive error overall was excellent for NCR, Retinomax, and SureSight with similar areas under the curve for each of these tests of refractive error. When myopia or astigmatism was considered, all three tests showed excellent performance. Detection of the most severe (highest) levels of hyperopia (group 1) was excellent and detection of any hyperopia greater than 3.25 D was very good to excellent. Detection of severe anisometropia was very good to excellent with all three tests and detection of any significant anisometropia was good to excellent. For hyperopia, Retinomax and NCR performed better than SureSight, while detection of anisometropia was better with SureSight than with Retinomax. Although the test distance for the SureSight is further from the child than that of the Retinomax, we found significantly better detection of hyperopia with Retinomax. Therefore, the Retinomax target may provide better relaxation of accommodation. However, the SureSight showed better detection of anisometropia than the Retinomax, indicating there was apparently more consistent accommodation between the two eyes perhaps due to either the more remote test distance or differences in the fixation targets. Identification of astigmatism was better with the Retinomax than with NCR. An association has previously been shown among hyperopia and anisometropia and astigmatism,4 which may in part explain the excellent performance for all three tests for detection of overall significant refractive error despite differences among the tests for detection of specific levels and types of refractive error.
These results support the conclusions of two previous studies. Specifically, Cordonnier and De Maertelaer38 showed that both SureSight and Retinomax were useful instruments for vision screening, with the use of unique referral criteria. Second, an analysis of the VIP Study data by Ying et al.45 showed that NCR, noncycloplegic Retinomax, and noncycloplegic SureSight had similar and high accuracy in detecting preschoolers with one or more targeted vision disorders including the most severe conditions. Referral criteria for detection of one or more targeted vision disorders for each test of refraction have been reported by Ying et al.45 This study shows similar performance of each test of refraction for the detection of specific types of refractive error and overall refractive error and adds to the findings of Ying et al.,45 which showed comparable performance between tests for detection of significant vision disorders overall.
Each of the three tests of refraction evaluated in this study are among the best performing screening tests23–25 and each may be used as a stand-alone vision screening procedure. Because many strabismic children have significant refractive error, these screening tests of refraction identify many children with strabismus. However, a test of refraction also may be combined with a test of eye alignment/stereopsis in order to attain some improvement in sensitivity for detection of strabismus.50 These findings suggest that other differences such as personnel needed, ease of use/interpretation, cost, and testing time may be considered in selecting which of these tests to use for screening. Both Retinomax and SureSight may be performed by eye care professionals, trained nurses, or lay screeners,25 while NCR requires more extensive training. Differences in the detection of significant refractive error between pediatric nurse and lay screeners were small. However, it is important to note that these results apply to the use of these tests of refraction by comparably trained personnel.23,25 Software is available for the SureSight (when used in minus cylinder format) which incorporates the VIP referral criteria (School Health Corp.) and displays an asterisk on the printout for each child who meets the VIP referral criteria, thus facilitating interpretation of the results. Manual interpretation of Retinomax results is needed as similar software is not available.25
Noncycloplegic retinoscopy, Retinomax, and SureSight have been shown to perform somewhat better than screening tests of monocular acuity for detection of one or more visual disorders, the most severe visual disorders and significant refractive error.23 Because the recommended vision screening for children is frequently a screening test of monocular acuity alone, future research should compare the sensitivities of screening tests of monocular acuity alone with that of screening using combinations of tests (i.e., one of the best tests of monocular acuity and one of the best tests of refraction) in order to determine whether adding a screening test of noncycloplegic refraction to a test of monocular visual acuity improves detection of visual disorders including significant refractive error.
The strengths of this study include the standard training of screeners and application of screening protocols and standardized cycloplegic refractive error measurements performed by study-certified optometrists and ophthalmologists on all participating children. In addition, VIP Study participants were Head Start preschool children who were geographically, racially, and ethnically diverse.10,23–25 The enriched sample over representing preschool children with vision disorders provided a large number of preschool children with significant refractive error. However, a limitation of the study is the small number of children with myopia. Although children recruited to participate in the VIP Study include a higher percentage of children who failed an initial Head Start screening, and were thus more likely to have vision disorders, the analysis of detection of refractive error overall and for specific types of refractive error by NCR, Retinomax, and SureSight is generalizable to other preschool children.
In conclusion, AUC was excellent for the most severe (highest) levels of each type of refractive error and very good to excellent for the detection of any significant refractive error. Each test had a very high power for detecting preschool children with any significant refractive error.
Acknowledgments
The authors thank Velma Dobson, PhD, who passed away in 2010, for her invaluable contributions to the VIP Study.
Supported by National Eye Institute/National Institutes of Health DHHS Grants U10EY12644, U10EY12547, U10EY12545, U10EY12550, U10EY12534, U10EY12647, U10EY12648, and R21EY018908. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure: M.T. Kulp, None; G.-S. Ying, None; J. Huang, None; M. Maguire, None; G. Quinn, None; E.B. Ciner, None; L.A. Cyert, None; D.A. Orel-Bixler, None; B.D. Moore, None
Appendix
The Vision in Preschoolers Study Group
Executive Committee: Paulette Schmidt, OD, MS (Chair); Agnieshka Baumritter, MA; Elise Ciner, OD; Lynn Cyert, PhD, OD; Velma Dobson, PhD; Beth Haas; Marjean Taylor Kulp, OD, MS; Maureen Maguire, PhD; Bruce Moore, OD; Deborah Orel-Bixler, PhD, OD; Ellen Peskin, MA; Graham Quinn, MD, MSCE; Maryann Redford, DDS, MPH; Janet Schultz, RN, MA, CPNP; Gui-shuang Ying, PhD.
Participating Centers
AA, administrative assistant; BPC, back-up project coordinator; GSE, gold standard examiner for comprehensive vision examinations; LPS, LEP screener; LS, lay screener; NS, nurse screener; PI, principal investigator; PC, Project Coordinator; PL, parent liaison; PR, programmer; VD, van driver; NHC, nurse/health coordinator.
Berkeley, CA: University of California Berkeley School of Optometry
Deborah Orel-Bixler, PhD, OD (PI/GSE/LPS); Pamela Qualley, MA (PC); Dru Howard (BPC/PL); Lempi Miller Suzuki (BPC); Sarah Fisher, PhD, OD (GSE/LPS); Darlene Fong, OD (GSE); Sara Frane, OD (GSE/LPS); Cindy Hsiao-Threlkeld, OD (GSE); Selim Koseoglu, MD (GSE); A. Mika Moy, OD (GSE); Sharyn Shapiro, OD (GSE); Lisa Verdon, OD (GSE); Tonya Watson, OD (GSE); Nina Friedman, OD, MS (LPS); Jennifer Seino, OD (LPS); Sean McDonnell (LS/VD); Erika Paez (LS); Darlene Sloan (LS); Evelyn Smith (LS); Leticia Soto (LS); Robert Prinz (LS); Joan Edelstein, RN (NS); Beatrice Moe, RN (NS).
Boston, MA: New England College of Optometry
Bruce Moore, OD (PI/GSE/LPS); Joanne Bolden (PC); Sandra Umaña (PC/LS/PL); Amy Silbert (BPC); Nicole Quinn, OD (GSE/LPS); Heather Bordeau, OD (GSE); Nancy Carlson, OD (GSE/LPS); Amy Croteau, OD (GSE); Micki Flynn, OD (GSE); Barry Kran, OD (GSE); Jean Ramsey, MD (GSE); Melissa Suckow, OD (GSE/LPS); Erik Weissberg, OD (GSE); Daniel Kurtz, PhD, OD (LPS); Daniel Laby, MD (LPS); Stacy Lyons, OD (LPS); Marthedala Chery (LS/PL); Maria Diaz (LS); Leticia Gonzalez (LS/PL); Edward Braverman (LS/VD); Rosalyn Johnson (LS/PL); Charlene Henderson (LS/PL); Maria Bonila (PL); Cathy Doherty, RN (NS); Cynthia Peace-Pierre, RN (NS); Ann Saxbe, RN (NS); Vadra Tabb, RN (NS).
Columbus, OH: The Ohio State University College of Optometry
Paulette Schmidt OD, MS (PI); Marjean Taylor Kulp, OD, MS (Co-Investigator/GSE/LPS); Molly Biddle, MA (PC); Jason Hudson (BPC); Melanie Ackerman, OD (GSE); Sandra Anderson, OD (GSE); Michael Earley, OD, PhD (GSE/LPS); Kristyne Edwards, OD, MS (GSE/LPS); Nancy Evans, OD (GSE); Heather Gebhart, OD (GSE/LPS); Jay Henry, OD, MS (GSE); Richard Hertle, MD (GSE); Ann Hickson, OD, MS (GSE/LPS); Jeffrey Hutchinson, DO (GSE); LeVelle Jenkins, OD (GSE/LPS); Andrew Toole, OD, MS (GSE); Sherry Crawford, OD, MS (LPS); Kathy Reuter, OD (LPS); Keith Johnson (LS/VD); Richard Shoemaker (VD); Rita Atkinson (LS); Fran Hochstedler (LS); Tonya James (LS); Tasha Jones (LS); June Kellum (LS); Denise Martin (LS); Christina Dunagan, RN (NS); Joy Cline, RN (NS); Sue Rund, RN (NS).
Philadelphia, PA: Pennsylvania College of Optometry
Elise Ciner, OD (PI/GSE/LPS); Angela Duson (PC/LS); Lydia Parke (BPC); Mark Boas, OD (GSE/LPS); Shannon Burgess, OD (GSE/LPS); Penelope Copenhaven, OD (GSE/LPS); Ellie Francis, PhD, OD (GSE/LPS); Michael Gallaway, OD (GSE/LPS); Sheryl Menacker, MD (GSE/LPS); Graham Quinn, MD, MSCE (GSE/LPS); Janet Schwartz, OD (GSE/LPS); Brandy Scombordi-Raghu, OD (GSE/LPS); Janet Swiatocha, OD (GSE/LPS); Edward Zikoski, OD (GSE/LPS); Jennifer Lin, MD (GSE); Leslie Kennedy (LS/PL); Rosemary Little (LS/PL); Geneva Moss (LS/PL); Latricia Rorie (LS); Shirley Stokes (LS/PL); Jose Figueroa (LS/VD); Eric Nesmith (LS); Gwen Gold (BPC/NHC/PL); Ashanti Carter (PL); David Harvey (LS/VD); Sandra Hall, RN (NS); Lisa Hildebrand, RN (NS); Margaret Lapsley, RN (NS); Cecilia Quenzer, RN (NS); Lynn Rosenbach, RN (NHC/NS).
Tahlequah, OK: Northeastern State University College of Optometry
Lynn Cyert, PhD, OD (PI/GSE/LPS); Linda Cheatham (PC/VD); Anna Chambless (BPC/PL); Colby Beats, OD (GSE); Jerry Carter, OD (GSE); Debbie Coy, OD (GSE); Jeffrey Long, OD (GSE); Shelly Rice, OD (GSE); James Dunn, OD (LPS); Elisabeth Harrington, OD (LPS); Leslie Trimble, OD (LPS); Shelly Dreadfulwater, (LS/PL); Cindy McCully (LS/PL); Rod Wyers (LS/VD); Ramona Blake (LS/PL); Jamey Boswell (LS/PL); Anna Brown (LS/PL); Jeff Fisher, RN (NS); Jody Larrison, RN (NS).
Study Center, Columbus, OH: The Ohio State University College of Optometry
Paulette Schmidt, OD, MS (PI); Beth Haas (Study Coordinator).
Coordinating Center, Philadelphia, PA: University of Pennsylvania, Department of Ophthalmology
Maureen Maguire, PhD (PI); Agnieshka Baumritter, MA (Project Director); Mary Brightwell-Arnold (Systems Analyst); Christine Holmes (AA); Andrew James (PR); Aleksandr Khvatov (PR); Lori O'Brien (AA); Ellen Peskin, MA (Project Director); Claressa Whearry (AA); Gui-shuang Ying, PhD (Biostatistician).
Bethesda, MD: National Eye Institute
Maryann Redford, DDS, MPH.
Advisory Committee (Voting Members)
Roy Beck (Chair); Susan Cotter; Jonathan Holmes; Melvin Shipp; Sheila West.
References
- 1. Ciner EB, Schmidt PP, Orel-Bixler D, et al. Vision screening of preschool children: evaluating the past, looking toward the future. Optom Vis Sci. 1998; 75: 571–584 [DOI] [PubMed] [Google Scholar]
- 2. Giordano L, Friedman DS, Repka MX, et al. Prevalence of refractive error among preschool children in an urban population: the Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009; 116: 739–746, 746.e1–e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Multi-Ethnic Pediatric Eye Disease Study Group Prevalence of myopia and hyperopia in 6- to 72-month-old African American and Hispanic children: the Multi-Ethnic Pediatric Eye Disease Study. Ophthalmology. 2010; 117: 140–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. O'Donoghue L, McClelland JF, Logan NS, Rudnicka AR, Owen CG, Saunders KJ. Profile of anisometropia and aniso-astigmatism in children: prevalence and association with age, ocular biometric measures, and refractive status. Invest Ophthalmol Vis Sci. 2013; 54: 602–608 [DOI] [PubMed] [Google Scholar]
- 5. Fozailoff A, Tarczy-Hornoch K, Cotter S, et al. Prevalence of astigmatism in 6- to 72-month-old African American and Hispanic children: the Multi-Ethnic Pediatric Eye Disease Study. Ophthalmology. 2011; 118: 284–293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Harvey EM, Dobson V, Clifford-Donaldson CE, Green TK, Messer DH, Miller JM. Prevalence of astigmatism in Native American infants and children. Optom Vis Sci. 2010; 87: 400–405 [DOI] [PubMed] [Google Scholar]
- 7. Huynh SC, Wang XY, Ip J, et al. Prevalence and associations of anisometropia and aniso-astigmatism in a population based sample of 6 year old children. Br J Ophthalmol. 2006; 90: 597–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ip JM, Robaei D, Kifley A, Wang JJ, Rose KA, Mitchell P. Prevalence of hyperopia and associations with eye findings in 6- and 12-year-olds. Ophthalmology. 2008; 115: 678–685, e671 [DOI] [PubMed] [Google Scholar]
- 9. Wen G, Tarczy-Hornoch K, McKean-Cowdin R, et al. Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: Multi-Ethnic Pediatric Eye Disease Study. Ophthalmology. 2013; 120: 2109–2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ying G, Maguire M, Cyert L, et al. Prevalence of vision disorders by racial and ethnic group among children participating in Head Start [ published online ahead of print October 31, 2013]. Ophthalmology. doi:10.1016/j.ophtha.2013.09.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cotter SA, Varma R, Tarczy-Hornoch K, et al. Risk factors associated with childhood strabismus: the Multi-Ethnic Pediatric Eye Disease and Baltimore Pediatric Eye Disease Studies. Ophthalmology. 2011; 118: 2251–2261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dobson V, Miller JM, Clifford-Donaldson CE, Harvey EM. Associations between anisometropia, amblyopia, and reduced stereoacuity in a school-aged population with a high prevalence of astigmatism. Invest Ophthalmol Vis Sci. 2008; 49: 4427–4436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Multi-Ethnic Pediatric Eye Disease Study Group Prevalence and causes of visual impairment in African-American and Hispanic preschool children: the Multi-Ethnic Pediatric eye Disease Study. Ophthalmology. 2009; 116: 1990–2000, e1991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pascual M, Huang J, Maguire M, et al. Risk factors for amblyopia in the Vision in Preschoolers (VIP) Study [ published online ahead of print October 13, 2013]. Ophthalmology. doi: 10.1016/j.ophtha.2013.08.040 [Google Scholar]
- 15. Robaei D, Rose K, Ojaimi E, Kifley A, Huynh S, Mitchell P. Visual acuity and the causes of visual loss in a population-based sample of 6-year-old Australian children. Ophthalmology. 2005; 112: 1275–1282 [DOI] [PubMed] [Google Scholar]
- 16. Robaei D, Rose KA, Kifley A, Cosstick M, Ip JM, Mitchell P. Factors associated with childhood strabismus: findings from a population-based study. Ophthalmology. 2006; 113: 1146–1153 [DOI] [PubMed] [Google Scholar]
- 17. Tarczy-Hornoch K, Varma R, Cotter SA, et al. Risk factors for decreased visual acuity in preschool children: the Multi-Ethnic Pediatric Eye Disease and Baltimore Pediatric Eye Disease Studies. Ophthalmology. 2011; 118: 2262–2273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ying GS, Huang J, Maguire MG, et al. Associations of anisometropia with unilateral amblyopia, interocular acuity difference, and stereoacuity in preschoolers. Ophthalmology. 2013; 120: 495–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shankar S, Evans MA, Bobier WR. Hyperopia and emergent literacy of young children: pilot study. Optom Vis Sci. 2007; 84: 1031–1038 [DOI] [PubMed] [Google Scholar]
- 20. Simons K. Hyperopia, accommodative dysfunction and reading. Binocul Vis Strabismus Q. 2004; 19: 69–70 [PubMed] [Google Scholar]
- 21. Rosner J, Rosner J. The relationship between moderate hyperopia and academic achievement: how much plus is enough? J Am Optom Assoc. 1997; 68: 648–650 [PubMed] [Google Scholar]
- 22. Williams WR, Latif AH, Hannington L, Watkins DR. Hyperopia and educational attainment in a primary school cohort. Arch Dis Child. 2005; 90: 150–153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vision In Preschoolers Study Group Comparison of preschool vision screening tests as administered by licensed eye care professionals in the Vision in Preschoolers Study. Ophthalmology. 2004; 111: 637–650 [DOI] [PubMed] [Google Scholar]
- 24. Vision In Preschoolers Study Group Sensitivity of screening tests for detecting vision in preschoolers-targeted vision disorders when specificity is 94%. Optom Vis Sci. 2005; 82: 432–438 [DOI] [PubMed] [Google Scholar]
- 25. Vision In Preschoolers Study Group Preschool vision screening tests administered by nurse screeners compared with lay screeners in the vision in preschoolers study. Invest Ophthalmol Vis Sci. 2005; 46: 2639–2648 [DOI] [PubMed] [Google Scholar]
- 26. Donahue SP, Arnold RW, Ruben JB. Preschool vision screening: what should we be detecting and how should we report it? Uniform guidelines for reporting results of preschool vision screening studies. J AAPOS. 2003; 7: 314–316 [DOI] [PubMed] [Google Scholar]
- 27. Harvey EM, Miller JM, Wagner LK, Dobson V. Reproducibility and accuracy of measurements with a hand held autorefractor in children. Br J Ophthalmol. 1997; 81: 941–948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cordonnier M, Dramaix M. Screening for abnormal levels of hyperopia in children: a non-cycloplegic method with a hand held refractor. Br J Ophthalmol. 1998; 82: 1260–1264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. el-Defrawy S, Clarke WN, Belec F, Pham B. Evaluation of a hand-held autorefractor in children younger than 6. J Pediatr Ophthalmol Strabismus. 1998; 35: 107–109 [DOI] [PubMed] [Google Scholar]
- 30. Cordonnier M, Dramaix M. Screening for refractive errors in children: accuracy of the hand held refractor Retinomax to screen for astigmatism. Br J Ophthalmol. 1999; 83: 157–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Harvey EM, Miller JM, Dobson V, Tyszko R, Davis AL. Measurement of refractive error in Native American preschoolers: validity and reproducibility of autorefraction. Optom Vis Sci. 2000; 77: 140–149 [DOI] [PubMed] [Google Scholar]
- 32. Wesemann W. Dick B. Accuracy and accommodation capability of a handheld autorefractor. J Cataract Refract Surg. 2000; 26: 62–70 [DOI] [PubMed] [Google Scholar]
- 33. Barry JC, Konig HH. Non-cycloplegic screening for amblyopia via refractive findings with the Nikon Retinomax hand held autorefractor in 3 year old kindergarten children. Br J Ophthalmol. 2001; 85: 1179–1182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Liang CL, Hung KS, Park N, Chan P, Juo SH. Comparison of measurements of refractive errors between the hand-held Retinomax and on-table autorefractors in cyclopleged and noncyclopleged children. Am J Ophthalmol. 2003; 136: 1120–1128 [DOI] [PubMed] [Google Scholar]
- 35. Cordonnier M, Kallay O. Non-cycloplegic screening for refractive errors in children with the hand-held autorefractor Retinomax: final results and comparison with non-cycloplegic photoscreening. Strabismus. 2001; 9: 59–70 [DOI] [PubMed] [Google Scholar]
- 36. Suryakumar R, Bobier WR. The manifestation of noncycloplegic refractive state in pre-school children is dependent on autorefractor design. Optom Vis Sci. 2003; 80: 578–586 [DOI] [PubMed] [Google Scholar]
- 37. Steele G, Ireland D, Block S. Cycloplegic autorefraction results in pre-school children using the Nikon Retinomax Plus and the Welch Allyn SureSight. Optom Vis Sci. 2003; 80: 573–577 [DOI] [PubMed] [Google Scholar]
- 38. Cordonnier M, De Maertelaer V. Comparison between two hand-held autorefractors: the Sure-Sight and the Retinomax. Strabismus. 2004; 12: 261–274 [DOI] [PubMed] [Google Scholar]
- 39. Schimitzek T, Schworm HD. Wave-front analysis as screening technique for amblyogenic ametropia with and without cycloplegia. Strabismus. 2003; 11: 133–143 [DOI] [PubMed] [Google Scholar]
- 40. Buchner TF, Schnorbus U, Grenzebach UH, Busse H. Examination of preschool children for ametropia: first experiences using a new hand-held autorefractor. Strabismus. 2004; 12: 111–117 [DOI] [PubMed] [Google Scholar]
- 41. Iuorno JD, Grant WD, Noel LP. Clinical comparison of the Welch Allyn SureSight handheld autorefractor versus cycloplegic autorefraction and retinoscopic refraction. J AAPOS. 2004; 8: 123–127 [DOI] [PubMed] [Google Scholar]
- 42. Kemper AR, Keating LM, Jackson JL, Levin EM. Comparison of monocular autorefraction to comprehensive eye examinations in preschool-aged and younger children. Arch Pediatr Adolesc Med. 2005; 159: 435–439 [DOI] [PubMed] [Google Scholar]
- 43. Rowatt AJ, Donahue SP, Crosby C, Hudson AC, Simon S, Emmons K. Field evaluation of the Welch Allyn SureSight vision screener: incorporating the vision in preschoolers study recommendations. J AAPOS. 2007; 11: 243–248 [DOI] [PubMed] [Google Scholar]
- 44. Metz CE. Basic principles of ROC analysis. Semin Nucl Med. 1978; 8: 283–298 [DOI] [PubMed] [Google Scholar]
- 45. Ying GS, Maguire M, Quinn G, Kulp MT, Cyert L; VIP Study Group. ROC analysis of the accuracy of Noncycloplegic retinoscopy, Retinomax Autorefractor, and SureSight Vision Screener for preschool vision screening. Invest Ophthalmol Vis Sci. 2011; 52: 9658–9664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Schaeffel F, Mathis U, Bruggemann G. Noncycloplegic photorefractive screening in pre-school children with the “PowerRefractor” in a pediatric practice. Optom Vis Sci. 2007; 84: 630–639 [DOI] [PubMed] [Google Scholar]
- 47. Rajavi Z, Parsafar H, Ramezani A, Yaseri M. Is noncycloplegic photorefraction applicable for screening refractive amblyopia risk factors? J Ophthalmic Vis Res. 2012; 7: 3–9 [PMC free article] [PubMed] [Google Scholar]
- 48. Choi BC. Slopes of a receiver operating characteristic curve and likelihood ratios for a diagnostic test. Am J Epidemiol. 1998; 148: 1127–1132 [DOI] [PubMed] [Google Scholar]
- 49. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44: 837–845 [PubMed] [Google Scholar]
- 50. Vision In Preschoolers Study Group Does assessing eye alignment along with refractive error or visual acuity increase sensitivity for detection of strabismus in preschool vision screening? Invest Ophthalmol Vis Sci. 2007; 48: 3115–3125 [DOI] [PMC free article] [PubMed] [Google Scholar]


