Abstract
Previous research has shown that exposure to parental verbal aggression is common and associated with increased levels of depression, anxiety, dissociation, and drug use. A key question that has not been addressed is whether verbal affection from the same or opposite parent can attenuate the effects of verbal aggression. This cross-sectional study examined the effects of parental verbal aggression and affection during childhood on measures of psychopathology and wellbeing in a community sample of 2,518 individuals (18–25 years). Data were analyzed for moderating influences using mixed effect models and for direct and indirect effects using structural equation models. The moderation analysis suggested that high levels of exposure to verbal affection did not mitigate the effects of verbal aggression from the same parent, and high levels of verbal affection from another parent did not generally result in a significant attenuation of the effects of verbal aggression. Structural equation models showed that verbal aggression was predominantly associated with effects on psychiatric symptoms scores, whereas verbal affection was primarily associated with effects on measures of wellbeing. These findings highlight the relatively independent effects of verbal aggression and verbal affection and suggest that the latter may be particularly important in establishing a foundation for emotional and physical wellbeing. These findings also suggest that ridicule, disdain, and humiliation cannot be easily counteracted by praise and warmth from the same or another parent.
Keywords: verbal aggression, verbal affection, depression, wellbeing, parent
Introduction
Parental verbal interactions with their children can be a source of comfort and care or ridicule and abuse. Along with other types of neglectful or abusive childhood experiences, emotional abuse in the form of verbally aggressive parenting has been shown to have lasting effects on brain development (see Belsky & de Haan, 2011, for a thorough review). Teicher and colleagues have provided preliminary data showing that exposure to parental verbal aggression is associated with alterations in white matter pathways involved in language processing (Choi, Jeong, Rohan, Polcari, & Teicher, 2009) and in gray matter alterations in the auditory cortex (Tomoda, et al., 2011). Furthermore, exposure to parental verbal aggression has been shown to exert enduring adverse psychiatric effects, comparable in magnitude to other forms of childhood adversity such as witnessing domestic violence and extra- familial sexual abuse (Teicher, Samson, Polcari, & McGreenery, 2006). Johnson et al. (2001) found evidence that individuals who experienced maternal verbal aggression during childhood were more than 3 times as likely as those who did not to have borderline, narcissistic, obsessive-compulsive, and paranoid personality disorders during adolescence or early adulthood (Johnson et al., 2001).
Parental verbal aggression is often characterized as a component or form of emotional maltreatment. Leading authors in the field have studied the verbal aspects of emotional harm from parents (Iwaniec, Larkin, & McSherry, 2007), parental psychological unresponsiveness or hostility (Shaffer, Yates, & Egeland, 2009), verbal threats and gestures (Moore & Pepler, 2006), and emotional neglect (Egeland, 2009) within the construct of emotional abuse. The study of positive parenting has focused on parenting styles (Rossman & Rea, 2005), parent mental health (Johnson, Cohen, Kasen, Ehrensaft, & Crawford, 2006), praise and feedback (Jack, Mikami, & Calhoun 2011), encouragement (Kelly, 2002), and parental involvement (De Kemp, Overbeek, De Wied, Engels, & Scholte, 2007), within the construct of responsiveness to the emotional needs of the child.
Purpose of the Study
Understanding parenting effects in the normal range can aid our understanding of other parental influences beyond adversity (Belsky & de Haan, 2011). In the current study, we sought to distinguish the effects of verbal interactions from other aspects of parental practices in childhood and to evaluate the effects of two components of parental practices – verbal aggression and verbal affection – on self-reported measures of psychopathology and well-being in young adulthood.
There were two primary objectives for the study. The first objective was to determine the statistical associations between self-reported exposure to parental verbal aggression and verbal affection in childhood on ratings of psychiatric symptoms and mental and physical wellbeing in young adulthood from a large community sample of young adults. The second objective was to determine whether positive factors such as verbal praise and affection could undo some of the consequences of exposure to harmful verbal interactions.
On the one hand, it is plausible that such signs of affection delivered by the same person, or by another parent, may be a protective factor that softens the impact of the verbal aggression. It is just as plausible that the combination of affectionate and abusive verbal statements within the household could create an uncertain and inconsistent environment that might do more harm than good. Examination of the roles of parental verbal affection and verbal aggression within the same sample could add to our understanding of the differential effects of each and answer questions about the potentially mitigating effect of affection in the individual’s life.
Methods
Participants and Procedures
Data were collected from 2004 to 2013 as part of a pooled prescreening effort to recruit for larger studies involving neuroimaging investigations. The overarching aim of each of the larger studies was to assess the association between self-reported exposure to childhood maltreatment and measures of brain morphometry, function, and psychopathology. Our strategy was to recruit potential participants from the general population based on their exposure history, without regard to psychiatric diagnosis, to obtain a sample with both psychiatrically susceptible and resilient individuals that would provide a more representative assessment of the overall consequences of exposure than recruitment of psychiatric or high-risk samples. Further, potential participants were only informed that we were assessing the influence of early experience on brain development and were not told about our interest in any specific types of maltreatment. Thus, the sample would not be biased towards any specific set of experiences. Also, this prescreening approach allowed us to recruit participants who could not knowingly fabricate histories or symptoms to gain enrollment. Participants responded to posted or published advertisements entitled Memories of Childhood. The questionnaires and prescreening methodologies underwent Institutional Review Board review and approval by McLean Hospital.
We chose to study 18–25 year olds because this represents the youngest age range in which parental consent is not required and because there is no mandated reporting requirement for child abuse and neglect of the participant. In addition, the shorter length of time between childhood events and assessment allowed for fewer intervening events than might be observed in older populations and more recent memories of the maltreatment.
Respondents to our advertisement phoned the office and were given a URL and password to link them to our HIPAA-compliant online enrollment system. Once logged in, the respondents electronically signed the informed consent to complete multiple survey instruments about childhood history, development, and current symptomatology. Respondents were paid $20, regardless of further eligibility for subsequent studies.
The computerized program was easy to use, and respondents could exit and return at their convenience until the information was complete, thereby reducing study demand. Participants received phone contact information for a clinician who was available 24/7 in case they experienced significant distress; however, we did not receive a single distress call. The participants controlled the submission of their information by selecting the submit button when complete. Entries were reviewed by hand, and appropriate candidates were invited to the laboratory for further evaluation, and if eligible, for enrollment in subsequent imaging studies.
The prescreening strategy during recruitment for the neuroimaging studies created a rich cross-sectional database derived from a communitywide convenience sample of young adults, which contained important developmental history on the timing and potency of potential risk and protective factors that could influence the emergence of psychiatric symptoms during late adolescence and early adulthood. Information from the prescreening database has been used to assess the differential influences of exposure to specific types of maltreatment on psychiatric symptom scores (Teicher, Samson, Sheu, Polcari, & McGreenery, 2010; Teicher & Vitaliano, 2011). This prescreening database is relatively unique in that approximately 40% of the individuals who completed the initial surveys were screened further to determine eligibility for the neuroimaging studies and underwent an elaborate face-to-face evaluation that included structured diagnostic interviews by a licensed mental health professional, a semi-structured trauma interview, neuropsychological testing, interviewer-based ratings of depression, anxiety and post-traumatic stress plus additional self-report measures. Any additional data collected was used in the current report to augment instrument psychometrics only. The current report analyzes the data from all survey participants, regardless of whether the individuals pursued or enrolled in the neuroimaging studies.
Measures
Verbal Abuse Scale (VAS)
Ratings of exposure to maternal or paternal verbal aggression were assessed using the Verbal Abuse Scale (VAS; Teicher, Samson, Polcari, & McGreenery, 2006). The VAS consists of 15 items that are rated from 0–7 based on frequency of occurrence (i.e., never, once/twice, once/year, a few times/year, monthly, weekly, a few times/week, daily) of the parental verbal offense which could have occurred at any point during childhood. Participants rated mother (or mother figure) and father (or father figure) separately. The original psychometric evaluation of the VAS was undertaken with a nonclinical sample of 554 individuals (384 female, 170 male) who ranged in age from 18 to 23 years (Navalta, Polcari, Webster, Boghossian, & Teicher, 2006). Item-total correlations were computed separately for the 15-item VAS for mothers and fathers. All items met minimum criterion item-total level of .30. The standardized Cronbach’s alpha for the scale was .96 for the mother version and .97 for the father version. Confirmatory principal components analysis with Varimax rotation, using eigenvalues > 1.0, resulted in identical two-factor solutions for both parent versions. Factor 1 included 12 items of criticism, threats, humiliation, insults, and blame. Factor 2 included three items of raising voice, yelling, and scolding. The maternal VAS two-factor solution accounted for 73.3% of the initially extracted variance (Factor 1, 65.8% and Factor 2, an additional 7.5%). The paternal VAS two-factor solution accounted for 75.3% of the initially extracted variance (Factor 1, 67.5% and Factor 2, an additional 7.8%).
Parental Bonding Instrument (PBI)
For criterion validity, both mother and father versions of the scale were then correlated with an established instrument used to assess how an individual feels about their parent, the PBI (Parker, Tupling, & Brown, 1979). As expected, the scores on the maternal VAS were highly negatively correlated with the maternal PBI caring subscale, r = −.71, p < .0001. Similarly, the scores on the paternal VAS were negatively correlated with the paternal PBI caring subscale, r = −.58, p < .0001.
A new psychometric evaluation was conducted from the current study participants, and the results were nearly identical to the original psychometrics. The same two factors accounted for 61% and 8% of the variance for mothers and 62% and 8% of the variance for fathers. Even though in both samples some factor loadings suggested two subscales, all 15 items define the construct. Theoretically, raised voice, yelling, or scolding could be considered a somewhat common occurrence in households, however these behaviors, if frequent and added to the more derisive ones, define verbally aggressive parenting practices. The higher the score, the more frequent the experiences of verbally abusive parenting (range: 0–105; Teicher, Samson, Polcari, & McGreenery, 2006). For any analysis requiring a cut-off score, we have determined that a score of >40 characterized verbal aggression from parents (Teicher, Samson, Polcari, & McGreenery, 2006).
Supplemental respondent data was evaluated for test-retest reliability for participants who completed online and a second in-person pen-and-paper VAS about 1–2 months later. The VAS showed high stability, r = .82, 95% CI [.778, .854], p < .001, n = 290. Furthermore, the participants’ mood and anxiety ratings assessed in-person in the office using Hamilton Depression Scale (HAM-D; Hamilton, 1960) and Hamilton Anxiety Scale (HAM-A; Hamilton & White, 1959) had no significant influence on the VAS retest scores (multiple regression analysis HAM-D: t = 0.348, df = 97, p = 0.73; HAM-A: t = 1.48, df = 97, p = 0.14) and accounted for 1.4% and 2.1% of the variance in test-retest scores, respectively based on variance decomposition (Lindeman et al. 1980; Grömping, 2007) demonstrating minimal state influences on remembrance of verbal experiences with a parent.
Verbal Affection Questionnaire (VAFF)
Ratings of exposure to verbal affection were assessed using the Verbal Affection Questionnaire (Polcari & Teicher, 2007, unpublished, included as supplementary material). Created to measure positive verbal parenting, the VAFF was modeled after the pre-existing VAS using the same 0–7 frequency of occurrence (i.e., never, once/twice, once/year, a few times/year, monthly, weekly, a few times/week, daily). The VAFF is a 12-item scale to assess the frequency of parental verbal positive interactions. Items included a parent saying she/he loved you, offering praise, providing verbal comfort, expressing affection through stories or singing for younger children, and engaging in meaningful conversations for an older child, across three stages of childhood (i.e., infant/toddler, latency, and adolescence). In 2003, a panel of expert clinicians endorsed the items as indicators of the construct of verbal affection.
Psychometric analysis was conducted from the current study participants (Polcari & Teicher, 2007) and showed that the VAFF has high internal consistency. Item-total correlations were computed separately for mothers and fathers and all items met minimum criterion item-total level of .30 (Mertler & Vannatta, 2013). The standardized Cronbach’s alpha for the scale was .95 for the mother version and .97 for the father version. Confirmatory principal components analysis with Varimax rotation, using eigenvalues >1.0 resulted in a two-factor solution for the mother version and a single factor for the father version. Maternal factor analysis identified two factors that accounted for 75% of the variance. The first factor was the verbal love and praise from infancy through childhood that accounted for 66% variance. The second factor was the praise, verbal comfort, and engaging in meaningful talks during adolescence, that accounted for an additional 9% of the variance. The paternal VAFF factor analysis yielded a single factor that accounted for 73% of the variance. All 12-items were used to define the construct of verbal affection. Participants rated mother (or mother figure) and father (or father figure) separately. The possible range was 0 to 84, and a maximum score of 84 denoted daily experiences throughout childhood to all affection items.
As reported earlier, the verbal aggression measure negatively correlated with an existing measure of parental caring, the PBI (Parker, Tupling, & Brown, 1979). We performed a regression analysis on a subset of this sample (n = 721) from the additional prescreening data to understand the relationship between verbal affection and aggression to parental caring. Maternal verbal measures accounted for 66% of the variance in maternal caring (37% aggression and 28.9% affection; r2 = .66, p < .001). Paternal verbal measures accounted for 59.8% of the variance in paternal caring (16.5% aggression and 43.3% affection; r2 = .60, p < .001). This psychometric analysis provided convergent validity and further supported the use of this measure as a valid and reliable instrument to measure parental verbal affection.
Symptom Questionnaire (SQ)
Self-reported ratings of psychiatric symptoms and wellbeing during the one week prior to starting the surveys were obtained using the SQ, a 92-item yes/no instrument (Kellner, 1987). In the SQ, psychiatric symptoms fall in the four domains of depression, anxiety, anger-hostility, and somatization, each with a 17-item subscale. Depression includes sad, feeling unworthy, feel like crying, thoughts of death or dying, and feeling of hopelessness. Anxiety includes nervous, scared, worried, jumpy, and tense. Anger-hostility includes angry, annoyed, losing temper easily, enraged, and resentful. Somatization includes cramps, headaches, heavy arms or legs, breathing difficulty, and nauseated/sick to stomach. The SQ also provides four wellbeing subscales (content, relaxed, friendly, and somatic well-being), each with six items. Contented includes cheerful, happy, feeing well and looking forward to the future. Relaxed includes feeling calm, feeling peaceful, self-confident and relaxed. Friendly includes patient, feeling kind toward people, feeling warm toward people, and feeling friendly. Somatic wellbeing includes feeling healthy, feeling fit, no unpleasant feeling in head or body, and no aches anywhere.
The SQ was developed to detect therapeutic response to psychotropic medications and is very sensitive to subtle differences from normal (Kellner, 1987). The SQ asks questions about state not trait, thereby making it a measure of the symptoms an individual is currently experiencing rather than how he/she usually feels or thinks. As such, it has demonstrated excellent sensitivity to detect clinical changes in response to treatment that might have been missed with typical measures, such as clinical impressions used to assess remission of depression (Fava, 2003). Using the supplemental available data from the participants, we established convergent validity of the SQ self-report to standardized office evaluation of depression and anxiety (Hamilton & White, 1959; Hamilton, 1960). Depressive symptoms on the SQ correlated strongly with HAM-D, r = .57, 95% CI [.439, .680], p < .001, n = 290. Odds of meeting diagnostic criteria for depression on interview were increased by 4.3-fold, 95% CI [2.1, 8.6], p < .001, if their previous SQ depression subscale score was greater than 12, a common indicator of clinically significant symptoms on this instrument. Similarly, self-report SQ anxiety scores correlated strongly with HAM-A scores, r = .56, 95% CI [0.425, 0.676], p < .001. Odds of meeting clinical criteria for an anxiety disorder were increased by 2.98-fold, 95% CI [1.44, 6.14], p < .002, if their previous SQ anxiety subscale was greater than 12. Our findings support the use of the SQ subscales to reflect clinically meaningful symptoms.
Maltreatment and Abuse Chronology of Exposure (MACE) Scale
The MACE was designed by Teicher and Parigger (Parigger, 2012) as an extensive research instrument to retrospectively assess severity and developmental timing of exposure to 10 forms of childhood maltreatment (sexual abuse, parental physical abuse, parental verbal aggression, parental nonverbal emotional abuse, witnessing interparental violence, witnessing violence toward siblings, peer physical abuse, peer verbal aggression, physical neglect, and emotional neglect). The MACE consists of 75-items identifying specific experiences, which the subject can endorse, and it provides 18 boxes for each item to indicate the years when the experienced occurred. The scale was developed using item responses theory and has excellent psychometric properties (e.g., test-retest reliability, n = 64, r = .894). MACE scales were available on a subset of this current analysis (n = 1,007). However, for the current study, we only made use of the subjects’ ratings of exposure to parental verbal aggression across age (MACE-PVA). The MACE-PVA score is based on response to five items that include name-calling, humiliation, screaming, and saying things that make the individual feel frightened. Unlike the VAS, the MACE-PVA score does not provide separating measures for mothers and fathers. Although the young childhood scoring of parental verbal aggression includes ages 1 through 5, the score most likely represents recalled memories from ages 4 and 5. Our data are consistent with Multhaup, Johnson, and Tetirick (2005) who demonstrated autobiographical recollected memories can be recalled from around 4 or 5 years old.
Report of Abuse
Self-reported exposure to sexual abuse was considered yes if a participant reported a parent had sexual contact with the sexual parts of their body or his/her body, on one or more occurrence, even if the participant was too young to understand the meaning of what was happening to them. Exposure to physical abuse by a parent was considered yes if a participant reported a parent physically hurt or attacked him/her (i.e., being struck, kicked, bitten, pushed, or otherwise physically hurt) on more than 4 occurrences, or if only one occurrence was severe enough to result in medical treatment or permanent injury or scar. Domestic violence was considered yes if a participant responded affirmatively to having ever witnessed serious domestic violence where a family member was harmed. These brief survey definitions for abuse experiences were derived from an adaptation of the Life Experiences Questionnaire (Bryer, Nelson, Miller, & Krol, 1987), an established, reliable means to elicit report of an abuse history as part of a screening or intake (Dill, Chu, Grob, & Eisen, 1991).
Perceived Financial Sufficiency
Participants were asked to characterize their financial sufficiency during childhood rather than the dollar amount of family income. The scale ranged from 1 (much less than enough money to meet our needs) to 5 (much more than enough money to meet our needs). We included this indicator of family finances for several reasons: participants were often uncertain of their parent’s income, family income could vary across their childhood, and family income could mean very different things depending on geographic locale, family size, and parental spending habits (Teicher, Samson, Polcari, & McGreenery, 2006).
Moderation Analysis Procedure
A moderator is a variable that affects the direction and/or strength of the relation between an independent or predictor variable and a dependent or criterion variable. In analysis of variance (ANOVA) terms, a moderator effect can be represented as an interaction between a focal independent variable and a variable that specifies how this relationship varies across conditions (Baron & Kenny, 1986). To test for the moderating influence of verbal affection on the relationship between verbal affection and symptom scores, we divided respondents into four verbal affection exposure groups. These consisted of those respondents who experienced: (1) low verbal affection from both parents, (2) high verbal affection from mother but not father, (3) high verbal affection from father but not mother, and (4) high verbal affection from both parents.
Cut scores for high or low verbal affection were determined using k-means cluster analysis to maximize statistical differences between these groups in verbal affection scores. The maternal cut score was 55 while the cut score for high paternal verbal affection was 45. Linear mixed effect nested models (R packages lme4 and LMERConvenienceFunctions) were used to assess the potential moderating effects of verbal affection grouping on the direct relationship between maternal and paternal verbal aggression scores and symptom ratings.
Structural Equation Modeling Procedure
Structural equation modeling (SEM) was used to assess direct and indirect (i.e., mediated) influences of maternal and paternal verbal aggression and affection ratings on psychiatric symptoms and wellbeing scores. To detect potential mediating effects, we subdivided verbal affection and verbal aggression scores into separate time periods so that the directionality of the relationship could be specified. We restricted the division to two time periods (early childhood vs. latency-adolescence) to minimize colinearity. The VAS provided separate ratings for ages 1–5, 6–12, and 13–17 years. Hence, we used verbal affection ratings for ages 1–5 for time period 1 and the average of the 6–12 and 13–17 ratings for time period 2. For verbal aggression, we used the average of MACE-PVA scores for 1–5 years for time period 1 and the respondents’ 15-item maternal and paternal verbal aggression scores as the time period 2 estimate. This approach was justified as the degree of exposure to MACE-PVA at 1–5 years correlated only −.01 and −.08 with 15-item paternal and maternal VAS scores, respectively, when extent of MACE-PVA at 6–17 years was partialled out. In contrast, MACE-PVA at 6–17 years correlated .52 and .57 with paternal and maternal VAS scores when extent of MACE=PVA at 0–5 years was partialled out. Hence, the 15-item VAS scores are much more reflective of exposure to parental verbal aggression during latency-adolescence than early childhood.
SEM was used to test the fit of a parsimonious model that hypothesized that exposure to verbal aggression would directly influence symptom ratings, whereas verbal affection would directly influence ratings of wellbeing. We also hypothesized that measures of verbal affection during time period 1 for one parent would directly influence time period 2 ratings of verbal affection for the same parent, but not the opposite parent. SQ ratings of anxiety, depression, somatization, and anger-hostility were used as external measures of the psychiatric symptoms latent variable, while relaxed, contented, friendly, and physically well feeling were used as external measures of the wellbeing latent variable.
SEMs were developed in R (Package OpenMx). These models were developed and tested on the full data set. We then tested the hypothesized and empirically-derived model separately for males and females, to test whether the hypothetical or empirical models provided a satisfactory fit across genders.
Scores for verbal affection and verbal aggression with SQ ratings were used as continuous variables and z-transformed (Glaser, 2011). The associative weight between the psychiatric symptom latent variable and SQ-anxiety scores was set equal to one, as was the weighting between wellbeing and SQ-relaxed scores. Goodness of fit was evaluated using a combination of absolute fit and relative fit indices to minimize Type I and Type II errors (Hu, Bentler, & Kano, 1992). Absolute fit was evaluated by root mean square error of approximation (RMSEA) and standardized root mean square residual (SRMR). SRMR values less than .08 are indicative of a good fit (Hu, Bentler, & Kano, 1992). Currently, RMSEA values less than or equal to .06 (Hu & Bentler, 1999) or .07 (Steiger, 2007) are used as indicators of acceptable fit. Chi-square was not used as these values are strongly influenced by sample size, and in models with this many subjects chi-square will usually lead to the unwarranted rejection of acceptable models (Hu, Bentler, & Kano, 1992). Relative fit indices include the Tucker-Lewis Index (TLI), Comparative Fit Index (CFI), and Incremental Fit Index (IFI), with the later being the least sensitive to sample size (Hu, Bentler, & Kano, 1992). Relative fit indices with values greater than .95 are indicative of good fits.
Finally, the Akaike information criterion (AIC) and Bayesian information criterion (BIC) were used to compare models. Both metrics balance model fit and parsimony, but BIC places a stronger emphasis on parsimony.
Results
Description of the Sample
The sample consisted of 2,518 consecutively enrolled participants (948 males, 1,570 females; Mage 21.80 ± 2.02 years) who completed the screening instruments. As shown in Table 1, participants were predominantly female (62%), Caucasian (75%), and Non-Hispanic (90%). They were recruited from a community with many nearby universities (40% of participants had some college, 41% completed college, and an additional 8% attended graduate school). Respondents’ characterized the financial sufficiency of their households during childhood as mostly stable with only 15% of the respondents reporting their family as having less or much less money than needed during childhood, 49% reporting enough for their needs, and 34% reporting having more or much more money wealth.
Table 1.
Respondent Characteristics
| Characteristic | Total Cohort (n=2,518) |
|---|---|
| Age in years (Mean + SD) | 21.80 ± 2.02 |
| 18 | 175 (7) |
| 19 | 196 (8) |
| 20 | 331 (13) |
| 21 | 381 (15) |
| 22 | 469 (19) |
| 23 | 370 (15) |
| 24 | 332 (13) |
| 25 | 264 (10) |
| Sex | |
| Female | 1,570 (62) |
| Male | 948 (38) |
| Race | |
| African American/Black | 188 (7) |
| Asian | 203 (8) |
| Caucasian | 1,893 (75) |
| Native American | 20 (1) |
| Other | 169 (7) |
| Not Reported | 45 (2) |
| Ethnicity | |
| Hispanic | 190 (8) |
| Non-Hispanic | 2,265 (90) |
| Not Reported | 63 (2) |
| Education Level of Respondents | |
| <12 years of education | 44 (2) |
| High school graduate | 182 (7) |
| Some college or enrolled now | 996 (40) |
| College graduate | 1,037 (41) |
| Graduate School | 213 (8) |
| Not Reported | 46 (2) |
| Financial Sufficiency | |
| Much less than enough money | 55 (2) |
| Less than enough money | 319 (13) |
| Enough money | 1,229 (49) |
| More than enough money | 782 (31) |
| Much more than enough money | 73 (3) |
| Not Reported | 60 (2) |
| Physical Abuse History | |
| Yes | 730 (29) |
| No | 1,487 (59) |
| Not Reported | 301 (12) |
| Physically Abused by a Parent | |
| Yes | 301 (12) |
| No | 1,916 (76) |
| Not Reported | 301 (12) |
| Domestic Violence History | |
| Yes | 437 (17) |
| No | 1,804 (72) |
| Not Reported | 277 (11) |
| Sexual Abuse History | |
| Yes | 396 (16) |
| No | 1,803 (71) |
| Not Reported | 319 (13) |
| Sexually Abused by A Parent | |
| Yes | 23 (1) |
| No | 2,176 (86) |
| Not Reported | 319 (13) |
Note. Values represent N (%)
Table 2 shows a summary of the verbal aggression, verbal affection, and psychiatric symptoms and wellbeing ratings for males and females. In general, the two groups were similar in age, financial sufficiency, parental education, and exposure to parental affection. Females rated maternal verbal aggression as significantly higher (M = 28.86) than males (M = 25.99). Females also rated symptoms of depression, anxiety, and somatization significantly higher than males. Males rated feelings of relaxation and physical wellbeing as significantly higher than females. Ratings of contentment, anger-hostility, and friendliness were not significantly different between groups.
Table 2.
Summary of Scores by Sex
| Males | Females | T-value | df* | p-value | |
|---|---|---|---|---|---|
| Age | 22.24 ± 2.07 | 22.34 ± 2.01 | 1.26 | 1940.83 | p > .21 |
| Maternal Verbal Aggression | 25.99 ± 20.05 | 28.86 ± 22.60 | 3.29 | 2134.84 | p < .001 |
| Paternal Verbal Aggression | 21.40 ± 19.43 | 19.89 ± 19.78 | −1.82 | 1899.97 | p < .07 |
| Maternal Verbal Affection | 65.69 ± 16.59 | 64.88 ± 18.54 | −1.12 | 2131.17 | p > .26 |
| Paternal Verbal Affection | 53.69 ± 21.65 | 55.04 ± 22.49 | 1.46 | 1943.20 | p > .14 |
| Anxiety | 4.96 ± 3.92 | 5.78 ± 4.16 | 4.86 | 2025.56 | p < .001 |
| Relaxed | 4.75 ± 1.50 | 4.43 ± 1.65 | −5.04 | 2109.85 | p < .001 |
| Depressed | 4.81 ± 4.39 | 5.49 ± 4.57 | 3.68 | 1996.51 | p < .001 |
| Contented | 5.27 ± 1.16 | 5.29 ± 1.21 | 0.51 | 2021.65 | p > .61 |
| Somatization | 3.03 ± 3.28 | 4.05 ± 3.64 | 7.12 | 2082.03 | p < .001 |
| Physical Wellbeing | 3.86 ± 1.70 | 3.57 ± 1.84 | −3.96 | 2059.66 | p < .001 |
| Anger-Hostility | 4.47 ± 4.14 | 4.81 ± 4.08 | 1.94 | 1901.22 | p < .06 |
| Friendliness | 4.80 ± 1.47 | 4.83 ± 1.43 | 0.52 | 1905.65 | p > .60 |
| Parental Education | 15.81 ± 2.74 | 15.72 ± 2.94 | −0.74 | 2050.96 | p > .46 |
| Financial Sufficiency | 3.24 ± 0.74 | 3.18 ± 0.81 | −1.91 | 2069.12 | p < .06 |
Note. Values represent mean ± SD;
Welch T test assuming variance
Moderation Analysis
Mixed effect models identified robust main effects of maternal and paternal verbal aggression ratings on symptom measures (e.g., SQ-anxiety: MVAS F = 176.82, df = 1, 2275, p < .001; FVAS F = 33.37, df = 1, 2275, p < .001), with the effects of maternal verbal aggression being even more reliable than the effects of paternal verbal aggression. In addition, for all symptom ratings there was at least one significant interaction between maternal or paternal verbal aggression scores and the respondent’s group-level exposure to parental verbal affection. The significance and nature of these interactions are summarized in Tables 3 and 4.
Table 3.
Moderating Effects of Verbal Affection on the Influence of Verbal Aggression on Symptom Ratings
| Symptom Ratings | Influence of Verbal Aggression from: | Verbal Affection Exposure Groupings
|
|||
|---|---|---|---|---|---|
| Low Maternal Low Paternal (N=421) | High Maternal Low Paternal (N=379) | Low Maternal High Paternal (N=169) | High Maternal High Paternal (N=1,579) | ||
| Anxiety | Mother | .041*** | .026 ∘ | .024 ∘ | .049*** |
| Father | .014 | .019 ∘ | .022 | .041*** | |
| Depression | Mother | .043*** | .022 | .019 | .052*** |
| Father | .015 | .014 | .054** | .039*** | |
| Somatization | Mother | .033*** | .028* | .008 | .043*** |
| Father | .023** | .003 | .058*** | .020*** | |
| Anger-Hostility | Mother | .038*** | .022 | .007 | .049*** |
| Father | .026* | .016 | .093*** | .034*** | |
Note. Values indicate slope of the linear regression between maternal and paternal verbal aggression in groups differing in extent of maternal and paternal verbal affection;
.1,
.05,
.01,
.001
Table 4.
Moderating Effects of Verbal Aggression on the Influence of Verbal Affection on Measures of Wellbeing
| Ratings of Wellbeing | Influence of Verbal Affection from: | Verbal Aggression Exposure Groupings
|
|||
|---|---|---|---|---|---|
| Low Maternal Low Paternal (N=1,713) | High Maternal Low Paternal (N=330) | Low Maternal High Paternal (N=227) | High Maternal High Paternal (N=278) | ||
| Relaxation | Mother | .000 | .012* | .024** | .005 |
| Father | .009*** | .006 | −.002 | .002 | |
| Contented | Mother | .007** | .013** | .009 | .007 |
| Father | .007*** | .009* | .006 ∘ | .003 | |
| Physically Well | Mother | −.002 | .012* | .023* | .003 |
| Father | .010*** | .003 | −.002 | .000 | |
| Friendly | Mother | .006 ∘ | .012** | .018* | .008 |
| Father | .007*** | .005 | .004 | .004 | |
Note. Values indicate slope of the linear regression between maternal and paternal verbal affection on wellbeing in groups differing in extent of exposure to maternal and paternal verbal aggression;
.1,
.05,
.01,
.001
There were significant interactions between verbal affection exposure and maternal verbal aggression on symptoms of depression and anxiety and trend-level interactions between verbal affection and paternal verbal aggression. For somatization, there was a significant interaction between verbal affection grouping and paternal verbal aggression, and for anger-hostility, there were significant interactions involving verbal affection grouping and both maternal and paternal verbal aggression.
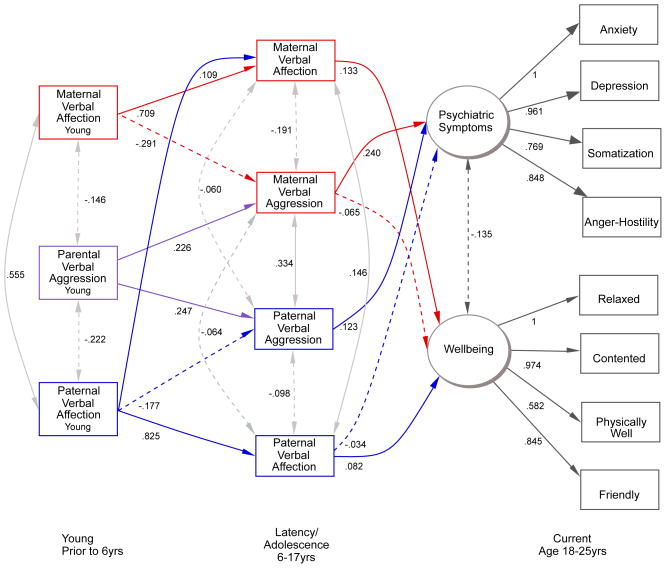
The nature of these interactions on ratings of depression as an example is shown in Figure 1. there was a strong regressive relationship between maternal verbal aggression scores and ratings of depression in respondents with low exposure to verbal affection from both parents, β = 0.043, r = .26, p < .001, and in respondents with high levels of verbal affection from both parents, β = 0.052, r = .23, p < .001, but not in respondents who experienced verbal affection from only one parent (e.g., high paternal affection, β = 0.019, r = .18, p < .08). Conversely, paternal verbal aggression only appeared to have a marked effect on depression measures in the groups of respondents exposed to high levels of paternal verbal affection.
Figure 1.
Moderation interactions on ratings of depression.
Mixed model analyses assessing the interactive effects of verbal aggression on separate maternal and paternal verbal affection groups identified significant interactions between paternal verbal aggression and paternal verbal affection on depression, F1, 2294 = 5.741, p < .02, somatization, F1, 2278 = 5.20, p < .03 and anger-hostility, F1, 2286 = 10.83, p = .001, with high verbal affection from both parents significantly increasing the effect of exposure to paternal verbal aggression. High levels of maternal verbal affection were associated with stronger effects of maternal verbal aggression on anxiety scores, F1,2291 = 3.98, p < .05. The remaining verbal affection-verbal aggression same-parent comparisons showed nonsignificant worsening, with no evidence for a significant attenuating affect of verbal affection on verbal aggression for any measure.
Cross-parent comparisons showed a marginal attenuating influence of high maternal verbal affection on the association between paternal verbal aggression and somatization, F1,2278 = 3.34, p < .07. Nonsignificant attenuations were seen for high maternal verbal affection on depression and anger-hostility and for high paternal verbal affection on somatization and anger-hostility. In summary, high levels of verbal affection from one parent did not increase the impact of verbal aggression from the other parent, but also did not generally result in a significant attenuation of the effects of verbal aggression.
Structural Equation Modeling
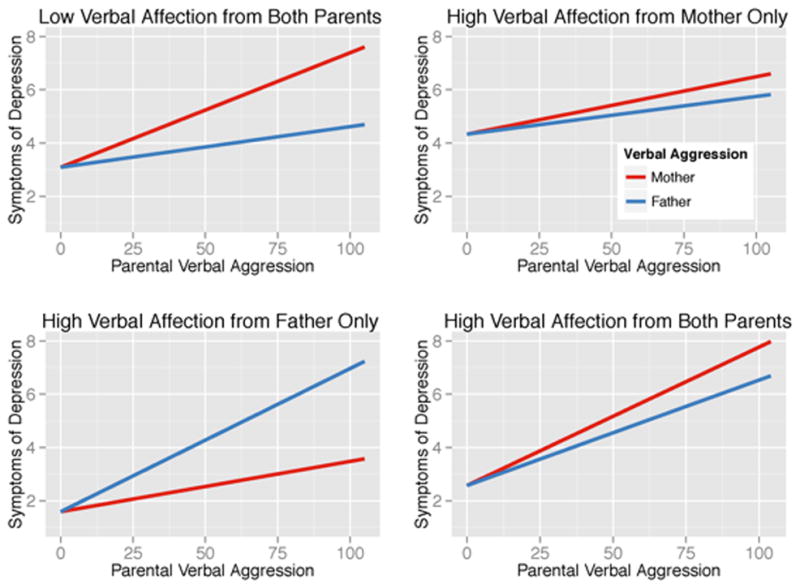
A structural equation analysis was conducted to determine the potential causal associations between exposure to maternal and paternal verbal affection and aggression during early childhood prior to age 6 (time 1) and latency-adolescence (time 2) on latent variable measures of psychiatric symptomatology and wellbeing. The initial model provided a reasonably good fit to the empirical data based on RMSEA, SRMR, IFI and CFI criteria. However, it fell a little short by TLI (0.942) criteria. Tests of the missing paths in the initial model indicated that three additional paths would significantly contribute to the model (paternal verbal affection-time 1 on maternal verbal affection-time 2, maternal verbal aggression on wellbeing and paternal verbal affection-time 2 on symptomatology). The revised model is presented in Figure 2. This model fit the empirical data better than the original model as indicated by lower AIC and BIC measures, even though the empirical model was less parsimonious than the hypothetical model. All path coefficients were significant at the .05 level. Separate analyses of males and females showed that the empirical model provided a good fit to the data for both sexes as shown in Table 5. The direct, indirect, and total causal effects on the latent variables of the revised model are presented in Table 6. The original model was designed to test the hypothesis that psychiatric symptomatology was directly affected by parental verbal aggression, but not verbal affection, and conversely that wellbeing was directly affected by parental verbal affection but not verbal aggression. Although this model provided a reasonable fit to the data, overall fit was improved by including a modest influence of maternal verbal aggression on wellbeing and a weak influence of paternal verbal affection on symptomatology. Altogether, parental verbal aggression accounted for 92% of the direct effect on psychiatric symptoms accounted for by the model. Similarly, parental verbal affection accounted for 76% of the direct effect on wellbeing explained by the model.
Figure 2.
Final Model of the associations between exposure to maternal and paternal verbal affection and aggression during early childhood, and latency-adolescence, on latent variable measures of psychiatric symptomatology and wellbeing.
Table 5.
Absolute, Relative And Comparative Indices Of Fit Of The Structural Equation Models To The Empirical Data.
| Model | N | df | RMSEA | SRMR | TLI | IFI | CFI | AIC | BIC | |
|---|---|---|---|---|---|---|---|---|---|---|
| All | Hypothetical | 2518 | 84 | 0.060 | 0.070 | 0.942 | 0.954 | 0.954 | 678.06 | 188.24 |
| Empirical | 2518 | 81 | 0.058 | 0.064 | 0.946 | 0.958 | 0.958 | 607.98 | 135.65 | |
| Females | Hypothetical | 1570 | 84 | 0.059 | 0.071 | 0.965 | 0.972 | 0.972 | 378.68 | −71.46 |
| Empirical | 1570 | 81 | 0.059 | 0.064 | 0.966 | 0.974 | 0.974 | 355.30 | −78.77 | |
| Males | Hypothetical | 945 | 84 | 0.063 | 0.074 | 0.976 | 0.981 | 0.981 | 231.96 | −175.54 |
| Empirical | 945 | 81 | 0.059 | 0.069 | 0.979 | 0.984 | 0.984 | 185.08 | −207.86 |
Note: AIC - Akaike information criterion, BIC - Bayesian information criterion, CFI - Comparative Fit Index, IFI - Incremental Fit Index, RMSEA - root mean square error of approximation, SRMS - standardized root mean square residual, TLI - Tucker-Lewis Index
Table 6.
Direct, Indirect And Total Causal Effects On The Latent Variables Of The Revised Model
| Outcome | Determinant |
|
||
|---|---|---|---|---|
| Causal Effects
| ||||
| Direct | Indirect | Total | ||
| Psychiatric Symptoms R2= .352 |
MVAGG Ages 6–17 | .236*** | .236 | |
| PVAGG Ages 6–17 | .125*** | .125 | ||
| PVAFF Ages 6–17 | −.032* | −.032 | ||
| MVAFF Ages 0–5 | −.069 | −.069 | ||
| Parental VAGG 0–5 | .082 | .082 | ||
| PVAFF Ages 0–5 | −.049 | −.049 | ||
| Wellbeing R2= .177 |
MVAFF Ages 6–17 | .129*** | .129 | |
| PVAFF Ages 6–17 | .084*** | .084 | ||
| MVAGG Ages 6–17 | −.066** | −.066 | ||
| MVAFF Ages 0–5 | .110 | .110 | ||
| Parental VAGG 0–5 | −.015 | −.015 | ||
| PVAFF Ages 0–5 | .017 | .017 | ||
Discussion
In the current study, we examined the statistical associations of both verbally aggressive and affectionate experiences in the same group of respondents on ratings for symptoms and wellbeing. We found that parenting practices of both mother and father influence symptom scores. Structural equation models showed that verbal aggression was predominantly associated with effects on psychiatric symptoms scores, whereas verbal affection was primarily associated with effects on measures of wellbeing. Our findings are consistent with the well-established role of adverse childhood experiences in adult psychopathology (Edwards, Holden, Felitti, & Anda, 2003; MacMillan et al., 2001). Meties, Ingram, and Siegle (2012) found lower scores for maternal caring were associated with negative self-beliefs, negative interpersonal interactions, feeling fatigue, and generalized fearfulness while lower scores for paternal caring were related to negative interactions with others (Meties et al., 2012).
The potential effects of parental affection and aggression appeared to be more independent then interactive in our model. The dichotomy between verbal aggression appearing to influence symptom scores and verbal affection appearing to influence wellbeing ratings emerged as a potentially powerful finding. The significant associations between verbal affection scores and measures of wellbeing are also intriguing and worthy of further exploration. Hence, we have made this scale freely available (see supplementary material). The potential capacity of verbal affection to exert an enduring beneficial effect on measures of wellbeing suggests that verbal affection may be more than the absence of a risk factor or the presence of a protective factor. Rather, it seems to be an important component of healthy development.
Although we found that verbal interactions of both mother and father influence symptoms, the moderation analysis suggested that the adverse consequences of high levels of exposure to parental verbal aggression cannot be easily overcome, neither by the verbally affectionate ministrations of the offending parent nor the verbal affection of the non-offending parent. High levels of exposure to verbal affection did not mitigate the effects of verbal aggression from the same parent. High levels of verbal affection from another parent did not generally result in a significant attenuation of the effects of verbal aggression. Effects of exposure to verbal aggression on measures of depression, anger, and somatic symptoms were as strong for individuals who experienced high levels of affection from both parents, as for those who experienced low levels from both parents. The strongest effect was for individuals who experienced high verbal aggression and affection from father, and low verbal affection from mother (see Table 3). This observation lends further support to efforts to better inform parents about the potentially deleterious consequences of ridicule, disdain, and scorn of their children (Iwaniec, Larkin, & McSherry, 2007).
Verbal affection has not been generally studied as a single factor. Although we believe that it is useful to isolate and analyze it in this way, it is important to note that verbal affection is one component of healthy parental responsiveness to the emotional needs of the child. Maternal and paternal verbal affection may, however, be an intrinsic and internally consistent component that can be used to take the exploration of early parental experience and brain development from studies of adversity into the range of normal development (Belsky & de Haan, 2011).
Limitations
The current study relies on retrospective self-report and self-reported symptoms. As such, questions can arise about the lack of external assessment (Shaffer et al., 2008). We addressed this potential concern related to the study design in the description of the psychometrics of our measures. We found consistent reporting of childhood parental frequency of occurrence of verbal aggression on the VAS (Teicher, Samson, Polcari, & McGreenery, 2006), with high correlation between in-person office reports and the online survey reports. We also established that the online report of depressed and anxious symptomatology with the SQ (Kellner, 1987) reflects clinically meaningful information about the individuals.
Although we were able to demonstrate childhood influence on adult symptomatology, these analyses used cross-sectional data in a retrospective design. It would be ideal to follow prospectively a large group of children over time in a longitudinal study to measure any intervening influences that might influence exposure to parental verbal aggression and affection and any later effects on symptomatology. In addition, as with any community sample recruited through advertisement for participants, self-selection bias may have been introduced by both the participant’s initial interest in the study and the decision to complete the prescreening surveys.
It is possible that individual temperament for some individuals who are subjected to parental aggression is a large contributing factor (Belsky & de Haan, 2011) and thus some had difficulty in the family or were more sensitive to the effects of poor parenting practices. It is also conceivable that individuals receiving high levels of parental affection were particularly easy to parent, or have attributes that help elicit positive parental interactions in some way. Individuals differ in their susceptibility to conditions that both undermine wellbeing and enhance it (Belsky & de Haan, 2011).
Alternate contextual explanations should be considered, mostly related to the complexity of studying the outcomes of parenting practices. We have considered if the items in our measure (expressions of affection, declaring love, praise, verbal comfort, reading or singing for younger children, and engaging in meaningful conversations for older children) have an impact for other contextual reasons such as physical proximity or more likely, an overall atmosphere of haven and comfort in the home. Cultural beliefs that influence family life also add to the complexity of understanding parenting practices (Fiese, Tomcho, Douglas, Josephs, Poltrock, & Baker, 2002) and therefore, any single study should be viewed with caution.
Conclusion
Exposure to parental verbal aggression may be a largely underestimated factor with lasting adverse consequences that has confounded our understanding of mood and behavioral symptoms. Exposure to parental verbal affection may be an underestimated contributor to healthy development. Children with less exposure to verbal affection from parents may be missing a chance during development to foster feelings of wellbeing, contentment, and friendliness that extend into adulthood. The potential for parental verbal affection in childhood to launch a lifetime of feeling more contented and well in adulthood are promising. Future studies should explore the mechanisms or underlying processes by which these childhood experiences influence adult wellbeing. Studies should also explore other positive parental behaviors such as physical affection to better measure the influence of feeling loved and cared for by your parents.
Acknowledgments
Funding provided by RO1 grants MH066222, DA017846, DA016934, and MH091391 to MHT.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Belsky J, de Haan M. Annual research review: Parenting and children’s brain development: The end of the beginning. Journal of Child Psychology & Psychiatry. 2011;52:409–428. doi: 10.1111/j.1469-7610.2010.02281.x. [DOI] [PubMed] [Google Scholar]
- Bryer JB, Nelson BA, Miller JB, Krol PA. Childhood sexual abuse and physical abuse as factors in adult psychiatric illness. American Journal of Psychiatry. 1987;144:1426–1430. doi: 10.1176/ajp.144.11.1426. [DOI] [PubMed] [Google Scholar]
- Choi J, Jeong B, Rohan ML, Polcari AM, Teicher MH. Preliminary evidence for white matter tract abnormalities in young adults exposed to parental verbal abuse. Biological Psychiatry. 2009;65:227–34. doi: 10.1016/j.biopsych.2008.06.022. Epub 2008 Aug 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeKemp R, Overbeek G, DeWied M, Engels R, Scholte R. Early adolescent empathy, parental support, and antisocial behavior. The Journal of Genetic Psychology. 2007;168:5–18. doi: 10.3200/GNTP.168.1.5-18. [DOI] [PubMed] [Google Scholar]
- Dill LD, Chu JA, Grob MC, Eisen S. The reliability of abuse history reports: A comparison of two inquiry formats. Comprehensive Psychiatry. 1991;32:166–169. doi: 10.1016/0010-440x(91)90009-2. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. American Journal of Psychiatry. 2003;160:1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Egeland B. Taking stock: Childhood emotional maltreatment and developmental psychopathology. Child Abuse & Neglect. 2009;33:22–26. doi: 10.1016/j.chiabu.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Fava M. Depression with physical symptoms: Treating to remission. Journal of Clinical Psychiatry. 2003;64(suppl 7):24–28. [PubMed] [Google Scholar]
- Fiese BH, Tomcho TJ, Douglas M, Josephs K, Poltrock S, Baker T. A review of 50 years of research on naturally occurring family routines and rituals: Cause for celebration? Journal of Family Psychology. 2002;16:381–390. doi: 10.1037//0893-3200.16.4.381. [DOI] [PubMed] [Google Scholar]
- Glaser D. How to deal with emotional abuse and neglect—Further development of a conceptual framework (FRAMEA) Child Abuse & Neglect. 2011;35:866–875. doi: 10.1016/j.chiabu.2011.05.013. Epub 2011 Oct 19. [DOI] [PubMed] [Google Scholar]
- Grömping U. Estimators of relative importance in linear regression based on variance decomposition. The American Statistician. 2007;61:139–147. [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M, White JM. Clinical syndromes in depressive states. Journal of Mental Science. 1959;105:985–998. doi: 10.1192/bjp.105.441.985. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM, Kano Y. Can test statistics in covariance structure analysis be trusted? Psychological Bulletin. 1992;112:351–362. doi: 10.1037/0033-2909.112.2.351. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Iwaniec D, Larkin E, McSherry D. Emotionally harmful parenting. Child Care in Practice. 2007;13:203–220. [Google Scholar]
- Jack A, Mikami A, Calhoun C. The moderating role of verbal aggression on the relationship between parental feedback and peer status among children with ADHD. Journal of Abnormal Child Psychology. 2011;39:1059–1071. doi: 10.1007/s10802-011-9521-7. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Ehrensaft MK, Crawford TN. Associations of parental personality disorders and axis I disorders with childrearing behavior. Psychiatry: Interpersonal & Biological Processes. 2006;69:336–350. doi: 10.1521/psyc.2006.69.4.336. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Smailes EM, Skodol AE, Brown J, Oldham JM. Childhood verbal abuse and risk for personality disorders during adolescence and early adulthood. Comprehensive Psychiatry. 2001;42:16–23. doi: 10.1053/comp.2001.19755. [DOI] [PubMed] [Google Scholar]
- Kellner R. A symptom questionnaire. Journal of Clinical Psychiatry. 1987;48:268–273. [PubMed] [Google Scholar]
- Kelly FD. The effects of locus of control, gender, and grade upon children’s preference for praise or encouragement. Journal of Individual Psychology. 2002;58:197–207. [Google Scholar]
- Lindeman RH, Merenda PF, Gold RZ. Introduction to bivariate and multivariate analysis. Glenview, IL: Scott Foresman; 1980. [Google Scholar]
- MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, Beardslee WR. Childhood abuse and lifetime psychopathology in a community sample. The American Journal of Psychiatry. 2001;158:1878–1883. doi: 10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- Meites TM, Ingram RE, Siegle GJ. Unique and shared aspects of affective symptomatology: The role of parental bonding in depression and anxiety symptom profiles. Cognitive Therapy and Research. 2012;36:173–181. [Google Scholar]
- Mertler CA, Vannatta RA. Advanced and multivariate statistical methods practical application and interpretation. 5. Glendale, CA: Pyrczak; 2013. [Google Scholar]
- Moore TE, Pepler DJ. Wounding words: Maternal verbal aggression and children’s adjustment. Journal of Family Violence. 2006;21:89–93. doi: 10.1007/s10896-005-9007-x. [DOI] [Google Scholar]
- Multhaup KS, Johnson MD, Tetirick JC. The Wane of childhood amnesia for autobiographical and public event memories. Memory. 13:161–173. doi: 10.1080/09608210344000652. [DOI] [PubMed] [Google Scholar]
- Navalta CP, Polcari A, Webster DM, Boghossian A, Teicher MH. Effects of childhood sexual abuse on neuropsychological and cognitive function in college women. Journal of Neuropsychiatry and Clinical Neurosciences. 2006;18:45–53. doi: 10.1176/jnp.18.1.45. [DOI] [PubMed] [Google Scholar]
- Parker G, Tupling H, Brown LB. A parental bonding instrument. British Journal of Medical Psychology (Now: Psychology and Psychotherapy) 1979;52:1–10. doi: 10.1111/j.2044-8341.1979.tb02487.x. Article first published online: 14 Jul 2011. [DOI] [Google Scholar]
- Polcari A, Teicher MH. Effects of parent verbal abuse and affection on psychiatric symptomatology. Abstract presented at the 54th annual meeting of the American Academy of Child and Adolescent Psychiatry Conference; Boston, MA. 2007. Oct, p. 206. [Google Scholar]
- Parigger A. Thesis: Development of a Modified Adverse Childhood Experience (MACE) Scale. Wissenschaftliche Arbeitzur Erlangung des Grades einer Diplom-Psychologin im Fachbereich Psychologie der Universitat Konstanz; 2012. May, 2012. [Google Scholar]
- R Development Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2010. [Google Scholar]
- Rossman B, Rea J. The relation of parenting styles and inconsistencies to adaptive functioning for children in conflictual and violent families. Journal of Family Violence. 2005;20:261–277. [Google Scholar]
- Shaffer A, Huston L, Egeland B. Identification of child maltreatment using prospective and self-report methodologies: A comparison of maltreatment incidence and relation to later psychopathology. Child Abuse & Neglect. 2008;32:682–692. doi: 10.1016/j.chiabu.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger JH. Understanding the limitations of global fit assessment in structural equation modeling. Personality and Individual Differences. 2007;42:893–898. [Google Scholar]
- Teicher MH, Samson JA, Polcari A, McGreenery CE. Sticks, stones, and hurtful words: Relative effects of various forms of childhood maltreatment. American Journal of Psychiatry. 2006;163:993–1000. doi: 10.1176/appi.ajp.2010.10010030. Epub 2010 Jul 15. [DOI] [PubMed] [Google Scholar]
- Teicher MH, Samson JA, Sheu YS, Polcari A, McGreenery CE. Hurtful words: Association of exposure to peer verbal abuse with elevated psychiatric symptom scores and corpus callosum abnormalities. American Journal of Psychiatry. 2010;167:1464–1471. doi: 10.1176/appi.ajp.2010.10010030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, Vitaliano GD. Witnessing violence toward siblings: An understudied but potent form of early adversity. PLoS One. 2011;6(12):e28852. doi: 10.1371/journal.pone.0028852. Epub 2011 Dec 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomoda A, Sheu YS, Rabi K, Suzuki H, Navalta CP, Polcari A, Teicher MH. Exposure to parental verbal abuse is associated with increased gray matter volume in superior temporal gyrus. Neuroimage. 2011;54(Suppl 1):S280–286. doi: 10.1016/j.neuroimage.2010.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]