Abstract
Background
Navigators can facilitate timely access to cancer services but there are little data on their economic impact.
Methods
We conduct a cost-consequence analysis of navigation vs. usual care among 10,521 individuals with abnormal breast, cervix, colorectal or prostate cancer screening results who enrolled in the Patient Navigation Research Program study from January 1 2006 to March 31 2010. Navigation costs included diagnostic evaluation, patient and staff time, materials, and overhead. Consequences or outcomes were time to diagnostic resolution and probability of resolution. Differences in costs and outcomes were evaluated using multi-level, mixed-effects regression adjusting for age, race/ethnicity, language, marital status, insurance, cancer, and site clustering.
Results
Most individuals were minority (70.7%) and un- or publically-insured (72.7%). Diagnostic resolution was higher for navigation vs. usual care at 180 (56.2% vs. 53.8%, p=0.008) and 270 days: 70.0% vs. 68.2%, p<0.001). While there were no differences in average days to resolution (110 vs. 109 days, p=.63), the probability of ever having diagnostic resolution was higher for navigation vs. usual care (84.5% vs. 79.6%, p <0.001). The added cost of navigation vs. usual care was $275 per patient (95% CI $260 – $290, p <0.001). There was no significant difference in stage distribution among the 12.4% of navigated vs. 11% of usual care patients diagnosed with cancer.
Conclusions
Navigation adds costs and modestly increases the probability of diagnostic resolution among patients with abnormal screening tests. Navigation is only likely to be cost-effective if improved resolution translates into earlier cancer stage at diagnosis.
Keywords: cancer, navigation, cost, outcomes, abnormal cancer screening
Introduction
Despite improvements in cancer care there are persistent disparities in stage at presentation, access to treatment, and survival between minority and socioeconomically disadvantaged populations compared to their white and/or more advantaged counterparts.1, 2 Inadequate follow-up after an abnormal screening test or a cancer diagnosis are potential contributors to these disparate outcomes since less than 75% of disadvantaged individuals with an abnormal cancer screening examination receive timely diagnostic care.3–6 Patient navigation programs were developed to reduce such gaps in care by improving access to, and timeliness of, cancer services.7, 8
While patient navigation programs hold promise as a means of reducing disparities in cancer screening follow-up, the evidence supporting their efficacy in decreasing mortality or economic impact is limited. Studies showing that navigation programs increase participation in cancer screening and adherence to diagnostic follow-up have lacked control groups or have had relatively small sample sizes8, 9 Only a single modeling-based economic evaluation of navigation for breast cancer has been published.10
The Patient Navigation Research Program (PNRP) study was designed to examine the benefits of navigation for minority/underserved patients with abnormal breast, cervical, colorectal, or prostate cancer screening results.11,12 We conducted an economic evaluation alongside the PNRP to estimate the short-term costs and outcomes of navigation from receipt of an abnormal screening exam to diagnostic resolution (benign or cancer).
Materials and Methods
Setting, Population, and Intervention
The PNRP was a multisite, prospective study that evaluated the impact of navigation for individuals aged 18 to 98 years from underserved populations with abnormal breast, prostate, colorectal or cervical cancer screening tests. Underserved populations included African Americans, Hispanics, Asians, and American Indians/Native Alaskans or low income populations.11 The study was conducted at nine sites between January 1 2006 and March 31 2010. While all sites shared a common definition of patient navigation, common methods for data collection, enrollment and follow-up periods, each implemented navigation in the real-world context of their community and health care setting. This resulted in varied research designs for comparing navigation to usual care: two sites used an individually- randomized trial design, two employed a group-randomized trial design, and five used quasi-experimental designs with nonrandom allocation into groups. This approach allowed for the needs of community-based participatory research, as well as the traditional multi-center clinical trials analysis.13–19 Usual care consisted of standard diagnostic follow-up for an abnormal screening without navigator support.11 Navigation added provision of support and guidance for timely access to the cancer care system, addressing barriers, and facilitating quality care.11, 20 Navigators were professional health workers and/or lay persons (e.g., cancer survivors or community volunteers).21 In addition to site-specific training, all navigators participated in a national training.22
Economic Evaluation
We conducted an economic evaluation of navigation vs. usual care using the societal perspective, including health sector and patient costs.23–25 We focused on the primary PNRP study outcome: time to diagnostic resolution. Because the time horizon of the PNRP was less than 365 days for 92% of participants, we only consider events occurring within the study period without discounting future costs or effects.26 Results are presented in a cost-consequence format12, 27 in 2011 US dollars (USD).34 All data collection procedures were approved by the respective PNRP site Institutional Review Boards.
Data Collection
Data on direct medical resources for diagnostic follow-up tests and services following an abnormal screen were based on PNRP study records. To estimate the fixed and variable costs related to providing patient navigation services,12, 28 we surveyed PNRP program managers about the resources used to establish and maintain each navigation program. Information from navigator tracking logs was used to measure average time spent providing navigation from abnormal screen to diagnostic resolution (cancer or non-cancer) in the periods where the program was in a steady state (i.e., excluding study start-up and training periods).
Direct Medical Care Costs
Tests and services were matched to their corresponding Healthcare Common Procedure Coding System (HCPCS) codes29 and valued based on 2011 Medicare fee schedules published by the Centers for Medicare and Medicaid Services (CMS).30, 31
To estimate the cost of establishing navigation services, the cost of navigator recruitment was based on time for secretarial staff to produce and post advertisements and for managers to review resumes (the cost of the advertisements were excluded). Navigator training costs included time for adapting national PNRP navigator training and teaching materials to the local site and the time for navigators and their direct supervisor/s to attend training. Based on the PNRP training standards, we assumed supervisors received one day of training and navigators received three days of training.22 While PNRP training was provided at no cost by the American Cancer Society in partnership with the National Cancer Institute,22 we estimated that training costs were $100 per day.32 Initial recruitment and training costs were annuitized over the working half-life of navigators.33 The cost to purchase office furnishings and equipment was converted to 2011 dollars and then applied as a five year annuitized cost for the duration of the study period at a discount rate of 10%.
The estimated fixed cost to maintain navigation services included the cost of additional office space for navigation staff valued using the published national average adjusted to 2011 USD.35 Costs associated with navigator travel (e.g., taxi, bus and train fares) and navigation materials (e.g., office supplies and telephone and mail charges) were based on costs reported by program managers. Navigator mileage was valued based on the IRS standard mileage rate for 2011.36 Time required for supervising, providing administrative support to navigators, and receiving ongoing training were estimated based on average time requirements reported by program managers and valued using the respective national wage rate. The direct cost of providing navigation services was based on staff time recorded in navigator logs based on median times for the 15-minute time intervals recorded. Times to visit termination were recorded per patient and were truncated at 90-minutes for scheduling time and 240-minutes for direct care for all patients. Navigation services provided by professional navigators were valued using median national wage rates for registered nurses.37 Lay navigator rates were based on the median hourly wage for nursing aides, orderlies, and attendants. Services that used a mix of professional and lay navigators used the average of the two wage groups. Wage rates were inflated to 2011 USD using the consumer price index medical services component38 with a 30% fringe rate.39
Navigator turnover observed in the PNRP study was 26% per year. We valued the cost of replacing navigators based on estimated recruitment and training costs plus the cost of lost productivity.40
Patient time and travel costs
Patient time associated with seeking care included time spent traveling to health care services and time spent using these services. Information on patient home and clinic zip codes and corresponding centroid data were used to calculate the approximate distance traveled to receive services. Travel costs were estimated using the IRS standard mileage rate for 2011.36 Time spent obtaining medical care related to the abnormal screening test was estimated based on expert clinical opinion plus a 20% wait time. Time was valued using PNRP census region-specific wage rates from the Bureau of Labor Statistics for individuals matched by their age and gender.
Consequence (Outcome) of Navigation
The primary PNRP study outcome was time from abnormal finding to diagnostic resolution (cancer or non-cancer). This was analyzed via a meta-analysis comparing adjusted proportional hazards ratios of patient navigation vs. usual care for each cancer type across each site. A two-part approach was used to estimate: 1) the mean number of days to resolution among those who were observed through to the point of diagnostic resolution, and 2) the probability of patients completing follow-up by different time points – 60 days, 90 days, 180 days, 270 days, and ever. We also performed sub-group analyses evaluating the mean number of days to diagnostic resolution for those diagnosed with cancer and those diagnosed with early stage neoplasia (CIN2/CIN3/stage 0 and stage I) versus more advanced cancers (stage II to IV).
Analysis
Categorical patient characteristics were compared using independent χ2-tests. We tested for differences in total costs and consequences between navigation vs. usual care23, 24, 26 using multilevel mixed-effects linear regression modeling. Consequences included the mean probability of resolution by 60 days, 90 days, 180 days, 270 days and ever (yes vs. no) and being diagnosed with early versus late stage among those with cancer. Since the navigated and usual care groups were not balanced, all analyses were adjusted for a priori set of defined covariates including age (in decades), race/ethnicity (Black, White, Hispanic, or other), language (English, Spanish, or other), marital status (never married, married, or other), insurance status (uninsured, public, or private), and cancer site. Clustering was accounted for at the site level by including site as a random effect in the mixed-effect models. To incorporate uncertainty surrounding the estimates of the cost of providing navigation services, we used results from probabilistic modeling with 1,000 simulations41 for each site in all analyses.
Less than 5% of item-level patient survey information was missing; patients were missing <10% of data for demographic or clinical characteristics. Missing survey data were replaced using the Schonlau implementation of the hotdeck multiple imputation procedure42 and missing patient data were imputed using chained equations.43
The cost analysis and probabilistic modeling were completed in Microsoft® Excel 2007 (Microsoft Corporation).44 Zip code centroid data and distance approximation used SAS® (SAS Institute Incorporated version 9.2) and statistical analyses were completed in Stata 12.1 (StataCorp 2009).
Results
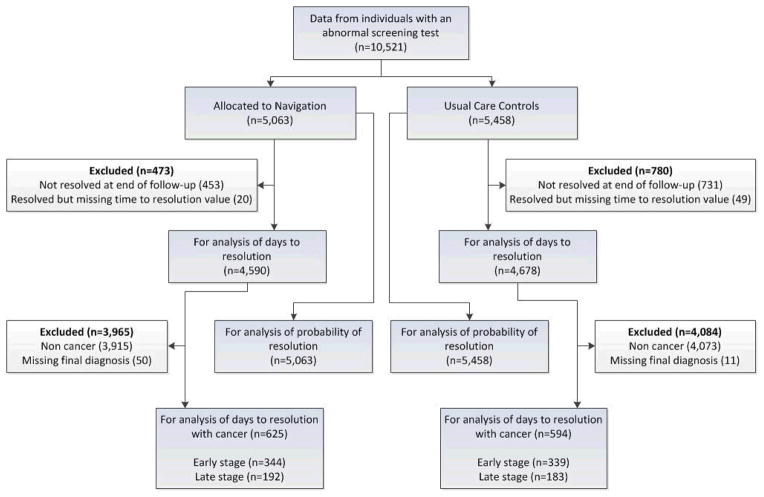
The PNRP included 10,521 patients (5,063 patients in the navigation group and 5,458 in the usual care group) (Table 1). Twelve hundred and fifty-three patients (11%) were excluded from the days to resolution analysis because they did not resolve before the end of study follow-up (365 days) or were missing time to resolution data (<1%) (Figure 1). A high proportion of participants were either Hispanic (39%) or black (32%). Forty percent were publically insured. Only 11% of usual care patients and 12.4% of navigated patients were diagnosed with cancer.
Table 1.
Characteristics of the Population in the Patient Navigation Research Program
| Characteristics | Total % (n) | Navigation % (n) | Usual Care % (n) | p-value |
|---|---|---|---|---|
| 100 (10,521) | 48.1 (5,063) | 51.9 (5,458) | ||
| Age (years) | ||||
| <30 | 18.6 (1,958) | 22.0 (1,115) | 15.4 (843) | <0.001 |
| 30–39 | 13.8 (1,451) | 16.6 (841) | 11.2 (610) | |
| 40–49 | 28.4 (2,988) | 26.5 (1,340) | 30.2 (1,648) | |
| 50–59 | 20.4 (2,146) | 19 (950) | 21.9 (1,196) | |
| 60–69 | 12.5 (1,313) | 11 (560) | 13.8 (753) | |
| 70–79 | 4.8 (507) | 4 (217) | 5.3 (290) | |
| 80+ | 1.2 (125) | 0.5 (27) | 1.8 (98) | |
| Missing | 0.3 (33) | 0.3 (13) | 0.4 (20) | |
| Gender | ||||
| Female | 91.9 (9,671) | 92.1 (4,665) | 91.7 (5,006) | 0.471 |
| Male | 8.1 (849) | 7.9 (398) | 8.3 (451) | |
| Missing | <0.1 (1) | 0 (0) | <0.1 (1) | |
| Race | ||||
| Black | 31.7 (3,330) | 29.4 (1,487) | 33.8 (1,843) | <0.001 |
| White | 24.7 (2,594) | 24.2 (1,224) | 25.1 (1,370) | |
| Hispanic | 39 (4,106) | 42.3 (2,142) | 36 (1,964) | |
| Other | 3.7 (392) | 4.1 (207) | 3.4 (185) | |
| Missing | 0.9 (99) | 0.1 (3) | 1.8 (96) | |
| Primary Language | ||||
| English | 59.7 (6,286) | 62.4 (3,159) | 57.3 (3,127) | <0.001 |
| Spanish | 24.5 (2,576) | 29.9 (1,515) | 19.4 (1,061) | |
| Other | 5.6 (594) | 6.2 (312) | 5.2 (282) | |
| Missing | 10.1 (1,065) | 1.5 (77) | 18.1 (988) | |
| Marital Status | ||||
| Single/Never Married | 41 (4,317) | 43.1 (2,180) | 39.2 (2,137) | <0.001 |
| Married/Living as Married | 31.9 (3,360) | 35 (1,772) | 29.1 (1,588) | |
| Divorced/Separated | 13.3 (1,397) | 15.5 (784) | 11.2 (613) | |
| Widowed | 4.3 (457) | 3.9 (197) | 4.8 (260) | |
| Missing | 9.4 (990) | 2.6 (130) | 15.8 (860) | |
| Insurance | ||||
| Uninsured | 32.2 (3,385) | 36.3 (1,837) | 28.4 (1,548) | <0.001 |
| Public | 40.5 (4,259) | 38.9 (1,969) | 42 (2,290) | |
| Private | 26.6 (2,801) | 23.7 (1,202) | 29.3 (1,599) | |
| Missing | 0.7 (76) | 1.1 (55) | 0.4 (21) | |
| Cancer Screening Test | ||||
| Breast | 63.9 (6,726) | 60.9 (3,083) | 66.7 (3,643) | <0.001 |
| Cervix | 25.5 (2,681) | 28.7 (1,455) | 22.5 (1,226) | |
| Colorectal | 4.7 (497) | 4.3 (219) | 5.1 (278) | |
| Prostate | 5.9 (617) | 6 (306) | 5.7 (311) | |
| Diagnosis | ||||
| No cancer | 76.5 (8,050) | 77.7 (3,934) | 75.4 (4,116) | <0.001 |
| Cancer | 11.7 (1,226) | 12.4 (626) | 11 (600) | |
| Missing | 11.8 (1,245) | 9.9 (503) | 13.6 (742) | |
| Stage | ||||
| Stage 0 | 11.5 (141) | 7.5 (47) | 15.7 (94) | <0.001 |
| Stage I | 18.9 (232) | 18.1 (113) | 19.8 (119) | |
| Stage II | 20.7 (254) | 19.6 (123) | 21.8 (131) | |
| Stage III | 7.3 (89) | 7.8 (49) | 6.7 (40) | |
| Stage IV | 2.9 (35) | 3.2 (20) | 2.5 (15) | |
| CIN2 or CIN3 | 25.4 (311) | 29.6 (185) | 21 (126) | |
| Missing | 13.4 (164) | 14.2 (89) | 12.5 (75) | |
Figure 1.
Flow of Patient Data Included in the Economic Evaluation
The average cost to hire and train a patient navigator was $2,460; ongoing maintenance costs for each navigator, exclusive of wages, was $24,140 annually (Table 2). Participants in the navigation group received more than 14,000 hours of navigation at an estimated average total cost of $190 per patient (Table 3).
Table 2.
Estimated Costs to Establish and Maintain Navigation, Excluding Wages
| Mean (SE) 2011 US$* | |
|---|---|
| Establishment | |
| Hiring | 800 (140) |
| Equipment | 710 (100) |
| Training | 1,200 (40) |
| TOTAL COST | $2,460 (180) |
| Maintenance | |
| Office space | 5,160 (840) |
| Supervision | 15,940 (6,090) |
| Administrative support | 2,060 (440) |
| Office supplies | 420 (130) |
| Mailing | 360 (110) |
| Telephone | 1,030 (360) |
| Parking and travel | 1,070 (610) |
| Ongoing training | 670 (210) |
| ANNUALIZED TOTAL COST | $24,140 (6,350) |
Average per single navigator based on surveys from site managers; excludes wages.
Table 3.
Time and Associated Adjusted Costs of Providing Navigation to Diagnostic Resolution of Abnormal Cancer Screening Tests
| Screening test | Number navigated to diagnostic resolution | Total navigation time | Average navigation time per person | Average value of navigator time per person Mean (95% CI)1 |
Average total costs per person Mean (95% CI)2 |
|---|---|---|---|---|---|
| % (n) | % (n) Hours | Hours | 2011 USD | 2011 USD | |
| Breast | 57 (2,468) | 73 (10,344) | 4.2 | 150 (50 – 460) | 210 (100 – 560) |
| Cervical | 31 (1,358) | 14 (2,043) | 1.5 | 70 (40 – 120) | 130 (60 – 230) |
| Colorectal | 5 (214) | 9 (1,220) | 5.7 | 210 (140 – 450) | 300 (180 – 530) |
| Prostate | 7 (290) | 4 (508) | 1.8 | 110 (70 – 190) | 200 (160 – 260) |
| Total | 100 (4,330) | 100 (14,114) | 3.3 | 130 (60 – 450) | 190 (80 – 540) |
Includes navigator wages and fringe benefit cost
Total costs of navigation include navigator time costs and ongoing maintenance costs (Table 2).
CI = Confidence Interval
The average value of navigator time per person, including wages and benefits, was $130 (95% CI: $60 – $450). Navigated patients had higher adjusted mean diagnostic follow-up costs ($400 vs. $320) and patient time costs ($70 vs. $18) than patients in usual care. Considering all costs, the total adjusted incremental cost of navigation vs. usual care was $275 (95% CI: $260 to $ 290) (Table 4). Unadjusted results and results, excluding imputed cost data, had little impact on this result (mean $284, 95% CI: $265 to $300).
Table 4.
Summary of Adjusted Societal Perspective Costs and Consequences of Navigation to Diagnostic Resolution of Abnormal Cancer Screening Tests1
| Navigation | Usual Care | Incremental Change | p-value | |
|---|---|---|---|---|
| COSTS 2011 USD (95% CI) | ||||
| Navigation costs | $190 (80 – 540) | - | - | - |
| Medical care costs | ||||
| Diagnostic follow-up | $400 (380 – 410) | $320 (260 – 380) | $ 80 (60 – 90) | <0.001 |
| Patient costs | ||||
| Time | $70 (66 – 72) | $18 (2 – 34) | $51 (48 – 54) | <0.001 |
| Travel | $7 (5 – 9) | $8 (3 – 12) | $-1 (−3 – 1) | 0.191 |
| Total cost | $635 (620 – 650) | $360 (260 – 460) | $275 (260 – 290) | <0.001 |
| CONSEQUENCES (OUTCOMES) | ||||
| Days to diagnostic resolution, mean (95% CI) | ||||
| 110 days (106 – 115) | 109 days (90 – 128) | 1.0 days (−3 – 6) | 0.630 | |
| Probability of diagnostic resolution, mean (95% CI) | ||||
| By 60 days | 43.6% (41.7 – 45.5%) | 42.3% (34.4 – 50.2%) | 1.3% (−0.5 – 3.2%) | 0.165 |
| By 90 days | 52.3% (50.4 – 54.1%) | 51.0% (42.1 – 59.9%) | 1.3% (−0.6 – 3.1%) | 0.195 |
| By 180 days | 56.2% (53.2 – 57.9%) | 53.8% (44.2 – 63.3%) | 2.4% (0.6 – 4.1%) | 0.008 |
| By 270 days | 70.0 % (60.7 – 71.5%) | 67.2% (57.9 – 76.6%) | 2.8% (1.3 – 4.3%) | <0.001 |
| Ever vs. never | 84.5% (83.3 – 85.7%) | 79.6% (75.5 – 83.7%) | 4.9% (3.7 – 6.2%) | <0.001 |
| Patients diagnosed with cancer - days to diagnostic resolution, mean (95% CI) | ||||
| 106 days (96 – 116) | 104 days (49 – 158) | 2.0 days (−8 – 12) | 0.666 | |
| Patients diagnosed with cancer - stage at diagnosis, mean (95% CI) | ||||
| Early vs. late2 | 57.9% (52.7 – 63.1%) | 52.2% (35.7 – 68.7%) | 5.7% (0.5 – 10.9%) | 0.074 |
| Patients diagnosed with early stage cancer - days to diagnostic resolution, mean (95% CI) | ||||
| 90 days (79 – 102) | 86 days (55 – 117) | 4.0 days (−7 – 16) | 0.468 | |
| Patients diagnosed with late stage cancer - days to diagnostic resolution, mean (95% CI) | ||||
| 91 days (68 – 113) | 81 days (7 – 153) | 10.0 days (−13 – 32) | 0.416 | |
CI = Confidence Interval
Multi-level mixed-effects regression, adjusting for age, race/ethnicity, language, marital status, insurance status, cancer, and site clustering.
Early defined as CIN2/CIN3/stage 0 and stage I; late defined as stage II to IV cancer.
Navigation increased the probability of diagnostic resolution after 180 and 270 days. The adjusted probability of ever having diagnostic resolution was higher in navigation than usual care (84.5% vs. 79.6%; 4.9% increase, 95% CI 3.7% to 6.2%, p <0.001); unadjusted results are similar (not shown). Among patients who obtained diagnostic resolution, the adjusted mean time to resolution was 110 days (95% CI: 106 to 115 days) in the navigation group and 109 days (95% CI: 90 to 128 days) in the usual care group (p=0.630) (Table 3). For those that were diagnosed with cancer, the adjusted mean time to resolution was 106 days (95% CI: 96 to 116 days) for navigated patients and 104 days (95% CI: 49 to 158 days) for patients in the usual care group (p=0.66). With adjustment, here was also no significant difference among pre-cancers and early stage versus late stage diagnoses (57.9% navigated vs. 52.2% usual care group, p=0.074), days to diagnosis for those with early stage disease (90 days navigated vs. 86 days usual care, p=0.468), or days to diagnosis for those with late stage disease (91 days navigated vs. 81 days usual care, p=0.416). Imputation of missing covariate data had no impact on these results.
Discussion
This is the first study to examine the costs of navigation alongside an evaluation of its impact in a large national program evaluating navigation for largely underserved patients with abnormal cancer screening findings. Our results indicate that navigation yields a small but significant increase in the probability of diagnostic resolution after 180 and 270 days following an abnormal cancer screening test at an added incremental cost of $275 per person compared to usual care. However, the added costs of navigation services did not translate into downstaging of cancer among the 11–12% of patients with abnormal tests diagnosed with cancer.
The relatively short time horizon for this study prevents estimation of longer term outcomes such as cancer mortality. However, the small differences in outcomes and relatively large incremental costs observed for navigated patients suggest that general patient navigation programs among low income and underserved populations with abnormal cancer screening tests are unlikely to be cost-effective (either expressed as cost per life year gained or quality adjusted life year gained) using commonly cited thresholds for cost-effectiveness (e.g., $50,000 or $100,000). In this study, navigated patients were more likely to be younger, minority race, not have English as primary language, single or divorced, and uninsured. If patients with these characteristics were more likely to need and benefit from navigation, this should have biased the study in favor of seeing an effect. When we remove adjustment for these factors, the results differ little from the adjusted results in magnitude or significance (data available upon request).
One previous study investigating the cost-effectiveness of patient navigation extended data from mammography follow-up from a single institution in a decision analysis model.10 The analysis assumed a six-month difference in the time to diagnostic resolution between navigation and usual care. Under this optimistic assumption, navigation cost $114,800 per life-year saved (LYS) (adjusted to 2011 USD). If there was a three-month difference, costs increased to $235,280 per LYS. Navigation was only cost-effective ($43,520 per LYS) under the combination of the most favorable assumptions, including a six-month earlier time of diagnosis, a 15% higher probability of obtaining follow-up resolution, and supposing that those lost to follow-up present at more advanced stages of cancer.
Navigation of patients with abnormal cancer screening results may provide value to consumers in other domains. For instance, it may lessen the anxiety associated with having an abnormal test result and negotiating the medical care system, enhance patient satisfaction, and/or improve health-related quality of life.46 Analysis of PNRP patient satisfaction surveys showed no significant difference in the crude satisfaction scores of navigated and usual care patients.47, 48 Navigation might also improve the efficiency of clinical services by ensuring that scheduled follow-up appointments are not missed, decreasing gaps in provider productivity. It could also assist patients in obtaining screening coverage through federal or local programs, reducing the burden to health systems of uncompensated care.45, 50 Positive navigation experiences could also lead to improved adherence to subsequent regular screening.
Given the very modest effects of the navigation program evaluated in this study, other strategies to improve timeliness of and access to follow-up care in underserved populations should be considered. For example, focusing navigation programs towards individuals who have no record of follow-up care 180 days after an abnormal result, or those with more severely abnormal findings could reduce resource needs for programs while targeting those who may benefit most from the services.
There are several caveats that should be considered in interpreting our results. Although research costs were not included in our calculations, the overall efficiency of the PNRP navigation programs could have been reduced due to research data collection activities. Our results may not represent the full range of costs or outcomes across the country or in settings or reimbursement models not represented within the PNRP sites. The study took a short-term perspective and did not include quality-adjusted life years saved.12, 23, 24 If new data emerge on the effectiveness of navigation, then future economic evaluations could extend our analysis to address these longer term outcomes.12, 23 Our economic data are intended to be a source of evidence for decision-makers in health care delivery systems, public and private insurance plans, and government and nongovernmental organizations about the economic impact of patient navigation. However, decisions about deployment of navigation will ultimately depend on the setting and needs of the population served, resources available, and public health priorities.
Acknowledgments
Financial support: Funding was provided by the National Cancer Institute through its Center to Reduce Cancer Health Disparities Contract 263-FQ-612391; by National Institutes of Health Grants U01 CA116892 (PI Karen Freund), U01 CA 117281 (PI Richard Roetzheim), U01CA116903 (PI Peter Raich), U01CA116937 (PI Steven Patierno), U01CA116924 (PI Kevin Fiscella), U01CA116885 (PI Donald Dudley), U01CA116875 (PI Steven Rosen, Elizabeth Calhoun), U01CA116925 (PI Victoria Warren-Mears), and American Cancer Society #SIRSG-05-253-01 (PI Electra Paskett). Dr. Mandelblatt’s work was supported in part by NCI grants U01 CA88283, U01CA152958, U01CA114593 and KO5CA96940. Dr. McKoy was supported by the Center to Reduce Cancer Health Disparities (1K01CA134554-01).
Footnotes
Conflicts of Interest: None declared
References
- 1.Shavers VL, Fagan P, McDonald P. Health disparities across the cancer continuum. J Health Care Poor Underserved. 2007 Nov;18(4 Suppl):1–5. doi: 10.1353/hpu.2007.0122. [DOI] [PubMed] [Google Scholar]
- 2.Laiyemo AO, Doubeni C, Pinsky PF, et al. Race and colorectal cancer disparities: health-care utilization vs different cancer susceptibilities. J Natl Cancer Inst. 2010 Apr 21;102(8):538–546. doi: 10.1093/jnci/djq068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yabroff KR, Washington KS, Leader A, Neilson E, Mandelblatt J. Is the promise of cancer-screening programs being compromised? Quality of follow-up care after abnormal screening results. Med Care Res Rev. 2003 Sep;60(3):294–331. doi: 10.1177/1077558703254698. [DOI] [PubMed] [Google Scholar]
- 4.Baig N, Myers RE, Turner BJ, et al. Physician-reported reasons for limited follow-up of patients with a positive fecal occult blood test screening result. American Journal of Gastroenterology. 2003 Sep;98(9):2078–2081. doi: 10.1111/j.1572-0241.2003.07575.x. [DOI] [PubMed] [Google Scholar]
- 5.Morris JB, Stellato TA, Guy BB, Gordon NH, Berger NA. A critical analysis of the largest reported mass fecal occult blood screening program in the United States. American Journal of Surgery. 1991 Jan;161(1):101–105. doi: 10.1016/0002-9610(91)90368-n. discussion 105–106. [DOI] [PubMed] [Google Scholar]
- 6.Burack RC, Simon MS, Stano M, George J, Coombs J. Follow-up among women with an abnormal mammogram in an HMO: is it complete, timely, and efficient? American Journal of Managed Care. 2000 Oct;6(10):1102–1113. [PubMed] [Google Scholar]
- 7.Li ST, Chi P. Optimizing the Efficacy of First-Line Chemotherapy plus Bevacizumab in Metastatic Colorectal Cancer Analysis of Multiple Methods. Biodrugs. 2011;25(1):43–50. doi: 10.2165/11584680-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Wells K, Battaglia T, Dudley D, et al. Patient navigation: state of the art or is it science? Cancer. 2008;113(8):1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robinson-White S, Conroy B, Slavish K, Rosenzweig M. Patient navigation in breast cancer: a systematic review. Cancer Nurs. 2010;33(2):127–140. doi: 10.1097/NCC.0b013e3181c40401. [DOI] [PubMed] [Google Scholar]
- 10.Markossian TW, Calhoun EA. Are breast cancer navigation programs cost-effective? Evidence from the Chicago Cancer Navigation Project. Health Policy. 2011;99:52–59. doi: 10.1016/j.healthpol.2010.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freund K, Battaglia T, Calhoun E, et al. National Cancer Institute Patient Navigation Research Program: methods, protocol, and measures. Cancer. 2008;113(12):3391–3399. doi: 10.1002/cncr.23960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramsey S, Whitley E, Mears V, et al. Evaluating the cost-effectiveness of cancer patient navigation programs: conceptual and practical issues. Cancer. 2009;115(23):5394–5403. doi: 10.1002/cncr.24603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paskett ED, Katz ML, Post DM, et al. The Ohio Patient Navigation Research Program: Does the American Cancer Society Patient Navigation Model Improve Time to Resolution in Patients with Abnormal Screening Tests? Cancer Epidemiol Biomarkers Prev. 2012 Oct;21(10):1620–1628. doi: 10.1158/1055-9965.EPI-12-0523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raich PC, Whitley EM, Thorland W, Valverde P, Fairclough D for the Denver Patient Navigation Research P. Patient Navigation Improves Cancer Diagnostic Resolution: An Individually Randomized Clinical Trial in an Underserved Population. Cancer Epidemiol Biomarkers Prev. 2012 Oct;21(10):1629–1638. doi: 10.1158/1055-9965.EPI-12-0513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dudley DJ, Drake J, Quinlan J, et al. Beneficial effects of a combined navigator/promotora approach for Hispanic women diagnosed with breast abnormalities. Cancer Epidemiol Biomarkers Prev. 2012 Oct;21(10):1639–1644. doi: 10.1158/1055-9965.EPI-12-0538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Battaglia TA, Bak SM, Heeren T, et al. Boston patient navigation research program: the impact of navigation on time to diagnostic resolution after abnormal cancer screening. Cancer Epidemiol Biomarkers Prev. 2012 Oct;21(10):1645–1654. doi: 10.1158/1055-9965.EPI-12-0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoffman HJ, Laverda NL, Young HA, et al. Patient navigation significantly reduces delays in breast cancer diagnosis in the district of columbia. Cancer Epidemiol Biomarkers Prev. 2012 Oct;21(10):1655–1663. doi: 10.1158/1055-9965.EPI-12-0479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wells KJ, Lee JH, Calcano ER, et al. A cluster randomized trial evaluating the efficacy of patient navigation in improving quality of diagnostic care for patients with breast or colorectal cancer abnormalities. Cancer Epidemiol Biomarkers Prev. 2012 Oct;21(10):1664–1672. doi: 10.1158/1055-9965.EPI-12-0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Markossian TW, Darnell JS, Calhoun EA. Follow-up and timeliness after an abnormal cancer screening among underserved, urban women in a patient navigation program. Cancer Epidemiol Biomarkers Prev. 2012 Oct;21(10):1691–1700. doi: 10.1158/1055-9965.EPI-12-0535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Cancer Institute. [Accessed July 17, 2012];Patient Navigation Research Program RFA-CA005-019. 2008 http://grants.nih.gov/grants/guide/rfa-files/RFA-CA-05-019.html.
- 21.Haylock P, Murph P. Oncology Nursing Society, the Association of Oncology Social Work, and the National Association of Social Workers Joint Position on the Role of Oncology Nursing and Oncology Social Work in Patient Navigation; Pittsburgh, PA. June 26–27; Oncology Nursing Society; 2009. [Google Scholar]
- 22.Calhoun E, Whitley E, Esparza A, et al. A national patient navigator training program. Health Promot Pract. 2010;11(2):205–215. doi: 10.1177/1524839908323521. [DOI] [PubMed] [Google Scholar]
- 23.Drummond M, Sculpher M, Torrance G, O’Brien B, Stoddart G. Methods for the economic evaluation of health care programmes. 3. Oxford: Oxford University Press; 2005. [Google Scholar]
- 24.Gold M, Siegel J, Russell L, Weinstein M, editors. Cost-Effectiveness in Health and Medicine. Oxford: Oxford University Press; 1996. [Google Scholar]
- 25.Ramsey S, Wilke R, Briggs A, et al. Good research practice for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA task force report. Value in Health. 2005;8:521–533. doi: 10.1111/j.1524-4733.2005.00045.x. [DOI] [PubMed] [Google Scholar]
- 26.Glick H, Doshi J, Sonnad S, Polsky D. Economic evaluation in clincial trials. Oxford: Oxford University Press; 2007. [Google Scholar]
- 27.Coast J. Is economic evaluation in touch with society’s health values? BMJ. 2004;329:1233–1236. doi: 10.1136/bmj.329.7476.1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Whitley E, Valverde P, Wells K, Williams L, Teschner T, Shih Y-CT. Establishing common cost measures to evaluate the economic value of patient navigation programs. Cancer. 2011;117(15 Suppl):3616–3623. doi: 10.1002/cncr.26268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Medicare and Medicaid Services (CMS) [Accessed February 10, 2012];Healthcare Common Procedure Coding System Release and Code Set Quarterly Update. 2012 https://www.cms.gov/HCPCSReleaseCodeSets/02_HCPCS_Quarterly_Update.asp#TopOfPage.
- 30.Centers for Medicare and Medicaid Services (CMS) [Accessed February 10, 2012];Physician Fee Schedule. 2012 https://www.cms.gov/PhysicianFeeSched/
- 31.Centers for Medicare and Medicaid Services (CMS) [Accessed February 10, 2012];Hospital Outpatient Prospective Payment System. 2012 https://www.cms.gov/HospitalOutpatientPPS/
- 32.Colorado Patient Navigator Training Program. [Accessed February 10, 2012];Patient Navigator Training. http://patientnavigatortraining.org/website/courses.htm.
- 33.Netten A, Knight LJ. Annuitizing the human captila investment costs of health service professionals. Health Econ. 1999;8:245–255. doi: 10.1002/(sici)1099-1050(199905)8:3<245::aid-hec430>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 34.Consumer price index all urban consumers (CPI-U) January 1913 to December 2011. Washington, DC: Bureau of Labor Statistics U.S. Department of Labor; 2012. [Google Scholar]
- 35.Office space across the world: Global office market report. New York: Cushman and Wakefield Research; 2011. [Google Scholar]
- 36.Internal Revenue Service. [Accessed 10 Februrary, 2012];IRS Announces 2010 Standard Mileage Rates. 2010 http://www.irs.gov/privacy/index.html.
- 37.Bureau of Labor Statistics. [Accessed February 10, 2012];Career guide to industries. 2008 2010–2011 Edition. http://www.bls.gov/oco/cg/cgs035.htm.
- 38.Consumer price index medical (CPI-M) January 1947 to December 2011. Washington, DC: Bureau of Labor Statistics U.S. Department of Labor; 2012. [Google Scholar]
- 39.Bureau of Labor Statistics. [Accessed April 25, 2012];Employer costs for employee compensation - March 2012. 2012 www.bls.gov/news.release/pdf/ecec.pdf.
- 40.Jones CB. The costs of nurse turnover: part 1: an economic perspective. J Nurs Adm. 2004 Dec;34(12):562–570. doi: 10.1097/00005110-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Briggs A, Claxton K, Sculpher M. Decsion modelling for health economic evaluation. Oxford: Oxford University Press; 2006. [Google Scholar]
- 42.Schnonlau M. [Accessed August 25, 2011];Stata software package, hotdeckvar.pkg, for hotdeck imputation. 2006 http://www.schonlau.net/stata/
- 43.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011 Feb 20;30(4):377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 44.Microsoft Excel version 12 [computer program] Redmond, WA: Microsoft Corporation; 2007. [Google Scholar]
- 45.Haideri NA, Moormeier JA. Impact of patient navigation from diagnosis to treatment in an urban safety net breast cancer population. Journal of Cancer. 2011;2:467–473. doi: 10.7150/jca.2.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Campbell C, Craig J, Eggert J, Bailey-Dorton C. Implementing and Measuring the Impact of Patient Navigation at a Comprehensive Community Cancer Center. Oncology Nursing Forum. 2010 Jan;37(1):61–68. doi: 10.1188/10.ONF.61-68. [DOI] [PubMed] [Google Scholar]
- 47.Fiscella K. Impact of patient navigation on satisfaction with cancer related health care. American Association for Cancer Research (AACR) International Conference on the Science of Cancer Health Disparities. Cancer Epidemiol Biomarkers Prev. 2011 doi: 10.1158/1055-9965.DISP-1111-PL1106-1104. [DOI] [Google Scholar]
- 48.Hendren S, Griggs JJ, Epstein R, et al. Randomized controlled trial of patient navigation for newly diagnosed cancer patients. Cancer Epidemiol Biomarkers Prev. 2012 Oct;21(10):1682–1690. doi: 10.1158/1055-9965.EPI-12-0537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979 May;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 50.Freeman HP, Rodriguez RL. History and principles of patient navigation. Cancer. 2011 Aug;117(15 Suppl):3539–3542. doi: 10.1002/cncr.26262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carroll JK, Winters PC, Purnell JQ, Devine K, Fiscella K. Do navigators’ estimates of navigation intensity predict navigation time for cancer care? Journal of Cancer Education. 2011 Dec;26(4):761–766. doi: 10.1007/s13187-011-0234-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thorne S, Truant T. Will designated patient navigators fix the problem? Oncology nursing in transition. Canadian Oncology Nursing J. 2010 Summer;20(3):116–128. doi: 10.5737/1181912x203116121. [DOI] [PubMed] [Google Scholar]
- 53.Robinson-White S, Conroy B, Slavish KH, Rosenzweig M. Patient navigation in breast cancer: A systematic review. Cancer Nursing. 2010 Mar-Apr;33(2):127–140. doi: 10.1097/NCC.0b013e3181c40401. [DOI] [PubMed] [Google Scholar]