Abstract
Diabetes affects a large and growing segment of the US population. Ethnic and racial minorities are at disproportionate risk for diabetes, with Hispanics and non-Hispanic blacks showing a near doubling of risk relative to non-Hispanic whites. There is an urgent need to identify low cost, effective, and easily implementable primary and secondary prevention approaches, as well as tertiary strategies that delay disease progression, complications, and associated deterioration in function in patients with diabetes. The Chronic Care Model provides a well-accepted framework for improving diabetes and chronic disease care in the community and primary care medical home. A number of community-based diabetes programs have incorporated this model into their infrastructure. Diabetes programs must offer accessible information and support throughout the community and must be delivered in a format that is understood, regardless of literacy and socioeconomic status. This article will discuss several successful, culturally competent community-based programs and the key elements needed to implement the programs at a community or health system level. Health systems together with local communities can integrate the elements of community-based programs that are effective across the continuum of the care to enhance patient-centered outcomes, enable patient acceptability and ultimately lead to improved patient engagement and satisfaction.
Keywords: diabetes, nurse care management, peer education, promotora, community based, integrated delivery network, care coordination
Introduction
Chronic illnesses including diabetes affect a large and growing segment of the US population. In 2009, 145 million US residents were living with one or more chronic conditions, and 1 in 4 had more than one (1). Increases in diabetes rates reflect a myriad of influences including higher life expectancy, population aging, more aggressive screening practices, and marked increases in obesity and related behavioral risk factors (2). Chronic disease treatment and management have been estimated to consume 84% of national health care expenditures (1). Thus, there is an urgent need to identify low cost, effective, and easily implementable primary and secondary prevention approaches, as well as tertiary strategies that delay disease progression, complications, and associated deterioration in function in patients with diabetes. The Chronic Care Model provides a well-accepted framework for improving diabetes and chronic disease care in the community and primary care medical home.(3,4) Patient self-management, delivery system design (including information systems and decision support) and community resources are some critical components of this approach. Substantial research shows that programs consistent with the Chronic Care Model improve health outcomes and reduce costs among many chronic disease populations.(5) Unfortunately, comprehensive implementation of the model components remains low in many communities and primary care settings and practices.(6,7) Scripps Whittier Diabetes Institute (SWDI) has developed community-based care coordination and self-management education programs relying heavily on the role of the peer educator as a bridge between the medical system and community. The peer educator role has facilitated improved communications between patient, physician and health system, lowered barriers and clarified myths related to cultural beliefs in diabetes management and ultimately improved patient “internal locus of control” defined as the patient’s perception that the individual can make a difference in the outcome of their own health. Over the last 15 years, SWDI has demonstrated that this partnership with peer educators allows hospitals, communities and physician partners to achieve better health, better healthcare, and lower cost for patients with diabetes.
Although diabetes occurs across all ages, ethnic and racial minorities are at disproportionate risk for diabetes, with Hispanics and non-Hispanic blacks showing a near doubling of risk relative to non-Hispanic whites. Therefore, it is critical for community-based programs to be delivered in a format that is understood, regardless of literacy, cultural beliefs and socioeconomic status. Prevalence of diagnosed and undiagnosed diabetes combined is 70–80% higher in non-Hispanic blacks and Hispanics than in non-Hispanic white subjects. (8,9) More than half of Hispanics and non-Hispanic black adults had diabetes or prediabetes in 2005–2006. (8) Hispanics and non-Hispanic blacks with diabetes also show poorer glycemic control, more complications, and a higher hospitalization rate than non-Hispanic whites. (10–12) Moreover, Latinos and African Americans who are hospitalized with diabetes are at higher risk for readmission than non-Latino whites. (13,14) Many factors, including lack of insurance, transportation and caregiving barriers, distrust, language and cultural barriers, and healthcare system inefficiencies may contribute to these patterns. (15,16)
If community-based diabetes programs are to make a difference in reducing the rates of developing diabetes and improving the control of existing disease they must be able to offer information and support throughout the community where it is accessible to all and delivered in a format that is understood, regardless of literacy, cultural beliefs and socioeconomic status. Several programs and key components for implementation will be described in this article.
Community-based diabetes programs-What has been done in the past?
A number of community-based programs that employ components consistent with the Chronic Care Model have demonstrated success and value in improving diabetes specific outcomes. (5,17–21) Patient self-management, delivery system design (including information systems and decision support) and community resources are some critical components in these approaches. The American Diabetes Association includes many of these components in its annual recommendations for delivering the basic standards of care to individuals detected with diabetes and pre-diabetes. (22). Self management education, one of the key components of the Chronic Care Model, is associated with improved knowledge, self-care behavior (23), and improved clinical outcomes such as lower A1C (24,25,27,28,29–32), lower self-reported weight (23), improved quality of life (26,30,33), healthy coping (34), and lower costs (35) in patients with diabetes. Additionally, many studies have supported the role of community health workers and peer (36–42) and lay leaders (43) in delivering diabetes self management education in conjunction with the primary care team (44,45) A recent systematic review and meta-analysis of DSME interventions identified an average reduction in HbA1C of .8% across 12–14 mo. (46) Consistent with the newly developing requirements and goals in the Affordable Care Act, diabetes self management education is associated with increased use of primary and preventive services (35,47) and lower use of acute, inpatient hospital services (35). Patients who participate in diabetes education are more likely to follow best practice treatment recommendations, particularly among the Medicare population, and have lower Medicare and commercial claim costs (48,49).
Approaches using self management education can also apply to the education and support of people at risk for diabetes, in particular in efforts to prevent the onset of diabetes. The strategies for supporting successful behavior change and the healthy behaviors recommended for people at risk for diabetes are similar to those for people with diabetes. Translating evidence-based programs such as the Diabetes Prevention Program into a community-based format can assist people at risk for diabetes in developing and maintaining behaviors that can prevent or delay the onset of diabetes. (50–52).
Project Dulce-Bringing together the components of the Chronic Care Model into one community-based diabetes program
Project Dulce is an American Diabetes Association (ADA)-recognized care management program developed in 1997 by the Scripps Whittier Diabetes Institute (SWDI) in collaboration with San Diego County, federally qualified health centers, and San Diego State University (SDSU), to improve health and access to care of underserved, ethnically diverse people with type 2 diabetes mellitus (T2DM). Project Dulce is founded in the Chronic Care Model (5,53), which recognizes that the majority of chronic care management takes place outside of formal healthcare settings. Project Dulce uses a team-based approach, with nurse care managers overseeing care, and peer educators providing culturally appropriate, group-based diabetes self-management education (DSME), cornerstone of effective diabetes management. (54) Peers are specially trained laypersons that serve as a trusted bridge between patients and the healthcare system. Peer-led education and intervention is an evidence-based method that has been shown to promote self management and health behavior change and improve outcomes in diabetes and other conditions, and is thought to be an effective model for reducing health disparities. (55–60) Tailoring of the Project Dulce DSME for diverse ethnic communities includes a focus on cultural beliefs, an emphasis on the family context, and a discussion of ways to stay healthy while on a budget. The curriculum is suitable for broad literacy levels and relies substantially on graphic content. Content was developed with input from Hispanic, non-Hispanic Whites, non-Hispanic Blacks, Vietnamese and Filipino patient focus groups and meetings with providers to gather information on the beliefs, and barriers that affect care in these patient populations. The curriculum acknowledges these beliefs but also creates methods to direct patients to optimal self-management.
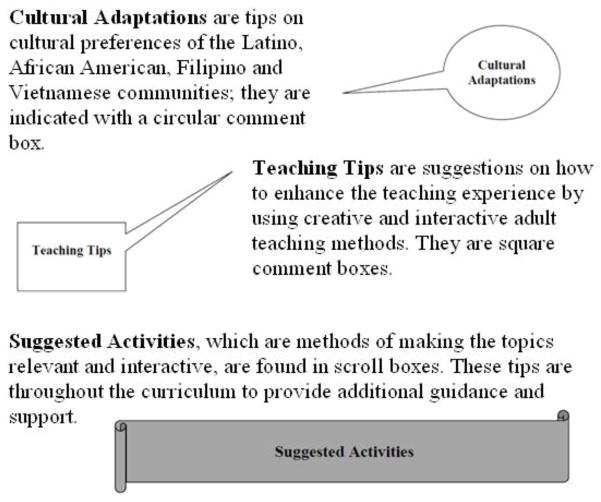
Studies evaluating Project Dulce have demonstrated positive effects on clinical, behavioral, and cost outcomes, including decreased emergency room and hospital utilization.(61–65) A study testing the peer DSME component alone showed that it was effective in improving clinical outcomes including HbA1C, blood pressure, and lipids in low income Latinos with poorly controlled diabetes. (64) To date, Project Dulce has served more than 20,000 patients in federally qualified health centers across San Diego County, and has been disseminated to other health systems across the nation and in Tijuana, Mexico. An example of the approaches used to enhance the training manual and curriculum is noted in the Figure 1.
Figure 1.
Community-based adaptations to training manuals.
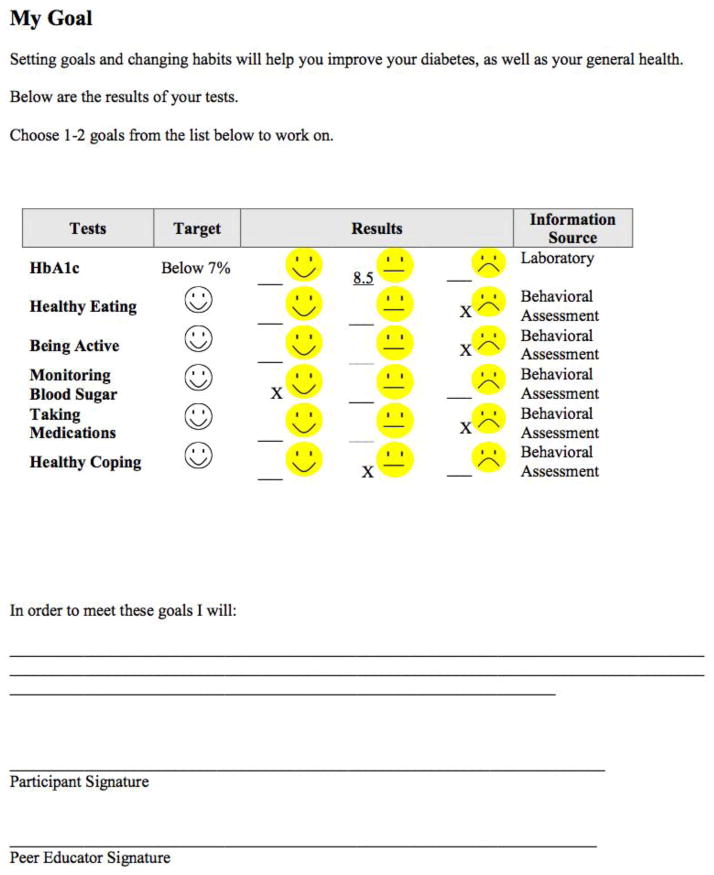
Providing step by step instructions for the peer leaders is part of the training program provided prior to integrating the programs into the community. Peer leaders, once identified, undergo 40 hours of training that includes learning curriculum content, group management skills, behavioral motivation techniques, electronic medical record navigation and workplace skills Competencies must be met before peers can be placed in a community teaching environment. Each section of the curriculum guides the peer educator to provide the necessary information while allowing the flexibility to have group discussions and exchange of personal experiences among the participants. A sample session for basic nutrition will include teaching goals such as: the basics of nutrition; how carbohydrates and fats affect blood sugar levels; use of the food labels; use of an action plan to set a personal goal. Culturally tailored handouts are included at the end of the lesson plan such as traditional foods that are high in carbohydrates/fats, types of fat, the “plate method”, heart healthy eating, read the food label, dining out, weight loss tips, alcohol and diabetes, estimating portion sizes and “my goal”. Finally recommended materials are suggested for each session such as lab results to share and discuss, graphic examples (posters/models of food items), measuring cups, spoons and standards of care cards (available from Scripps Whittier Diabetes Institute, American Diabetes Association, American Heart Association). An example of a patient friendly standard of care card with goals is noted in Figure 2.
Figure 2.
Patient-friendly standards of care and goals.
Extending the community-based peer education model to other populations
A number of excellent protocols have been established and tested that demonstrate benefit in preventing diabetes or reducing rates of readmissions in individuals hospitalized with diabetes. These protocols were conducted using intensive interventions that many times were staffed with highly skilled nurses, dietitians and psychologists to deliver the programs. In the era of cost containment in delivering health related interventions it is reasonable to identify methods in which the interventions can be adapted and delivered effectively in patient centric, community-based formats. The success of using peer educators within Project Dulce has resulted in a bidirectional effect within SWDI and Scripps as a whole, to ensure that the health system builds and develops more culturally sensitive and effective programs whether they are based in the community, or at Scripps. This is reflected in the subsequent development of two additional programs focused on prevention and reducing hospital readmissions both of which are key initiatives for health systems today. SWDI has piloted these two approaches that suggest incorporating peer-led components into the programs are acceptable to patients and can be integrated into the existing health system to optimize health care delivery, and potentially reduce costs.
Peer-led diabetes prevention in high risk women with a history of gestational diabetes (GDM)
Women with a history of gestational diabetes mellitus (GDM) have a 7-fold likelihood of future type 2 diabetes mellitus (T2DM) relative to those with normoglycemic pregnancies (66). Latinas have the highest birth rate among all U.S. racial/ethnic groups (67) and are at high risk for GDM (68) and T2DM (9) when compared with non-Latino whites. Lifestyle interventions, such as the Diabetes Prevention Program (DPP), can delay or prevent T2DM onset in post-GDM and other high-risk groups (69,70). To address the specific needs and barriers encountered in the Latino community SWDI adapted the DPP publically available curriculum with the Project Dulce community-based approach and conducted a single-group pilot study to evaluate the effectiveness and acceptability of a group-format, peer-educator administered translation of the DPP in reducing type 2 diabetes risk among Latinas with prior GDM-Dulce Mothers. Seventy-six Latinas, 18–45 years, with recent GDM underwent an 8-week, peer-educator led, DPP-based group intervention, with adaptations for Latino culture and recent mothers. Risk factors were assessed at baseline, month 3, and month 6.
Participants showed significant improvements in lipids, blood pressure, physical activity, dietary fat intake, and fatalistic and culturally-driven diabetes beliefs (ps<.05). (71) Formative evaluation suggested that the program was acceptable to participants. The conclusions from the pilot indicted that low-cost, peer-led, culturally appropriate DPP adaptation reduced clinical and other indicators of diabetes risk in Latinas with GDM. Based on the preliminary results and feedback from the participants additional modifications to the program will focus on diet and caloric balance to achieve greater weight loss.
Peer-led diabetes care coordination-Discharge to home
Hospitalizations with diabetes as a primary or secondary diagnosis increased from 2.8 million in 1988 to nearly 5.5 million in 2009. (72) Individuals with diabetes accounted for 26% of all hospital inpatient days in 2012, and these hospitalizations accounted for more than half of the $176 billion in healthcare costs attributed to diabetes in this same year. (73) As noted earlier, ethnic minorities with diabetes suffer more complications, a higher hospitalization rate, higher risk for readmission and an increased mortality rate relative to their non-Hispanic white counterparts. (10,11,13,14, 74). These failures in diabetes care have an enormous impact on patient quality and quantity of life.
The term care transition describes the process by which a patient’s care shifts from one setting to another, e.g., hospital to home. Poorly coordinated care transitions are a major factor in hospital readmissions, complications, and worsening health. (75,76) Failures of care coordination including poor care transitions accounted for up to $45 billion in wasted healthcare spending in 2011. (77) Further, three quarters of short-term hospital readmissions are potentially preventable. (78) Care transitions have thus been identified as a critical target for improving healthcare quality. (76) Indeed, the Affordable Care Act will fund implementation of evidence-based care transitions services for Medicare patients at high risk for readmissions (Section 3026 of HR 3590). In addition, under the Affordable Care Act, Medicare recently began financially penalizing hospitals that have higher-than-expected 30-day readmissions rates for some conditions. A recent systematic review of 24 studies testing structured discharge programs showed positive effects on readmissions and length of stay, with some studies suggesting improved patient satisfaction with care. (79) Research concerning the effects of such programs on other patient relevant health outcomes (e.g., functional status, well-being, perceived health, quality of life) and on clinical control was noted to be very limited, highlighting an important gap in evidence. Indeed, the review highlighted the need for additional, rigorous research examining such programs. Further, their reliance on nurses, pharmacists, or other professionals, means that the programs reviewed entail a resource intensive commitment in new staff or set aside time for existing staff. Moreover, such programs may not adequately address the specific needs of low-income, ethnic minority patients, or patients with diabetes, who are at especially high risk for readmissions. A recent report that gathered perspectives of leaders from state and local hospitals and improvement teams noted that many hospitals have eschewed discharge planning programs because they do not view the benefits as outweighing the costs, and they feel that there is inadequate evidence regarding cost-effective interventions to guide improvement. (80) Additional research is needed to fill these evidence gaps and better guide provision of care and care improvement for the highest risk populations.
SWDI recently developed and piloted a novel care transitions program for high-risk patients hospitalized with diabetes. The Dulce Transitions program assigns specially trained peer educators (“peer transitions coaches”) to follow patients discharged from the hospital, connect them with outpatient health and other community resources, and activate them to effectively manage their disease within their own environment and cultural context by developing necessary knowledge skills, self-efficacy, and resources, and overcoming barriers (Figure 3). The pilot program reached 200 patients between October 2010 and February 2012. An internal evaluation revealed a reduced 30-day readmissions rate for these patients of 11% versus 16% in similar patients who were not included in the program during the same period. This 31% reduction in readmissions is comparable to that achieved in nurse led programs, such as the successful care transitions program developed by Coleman and colleagues (81) and the “Re-Engineered Discharge” program. (82) Clinical and other patient relevant outcomes were not tracked in this pilot. Patients and peer providers were surveyed to obtain their impressions of the program’s strengths and areas for improvement. One patient from Scripps Mercy Hospital Chula Vista reported being hospitalized up to 2 times per month prior to participating in the Dulce Transitions pilot. The peer-led diabetes self-management program resulted in knowledge gained by the patient and a positive outlook towards her health and future.
Figure 3.
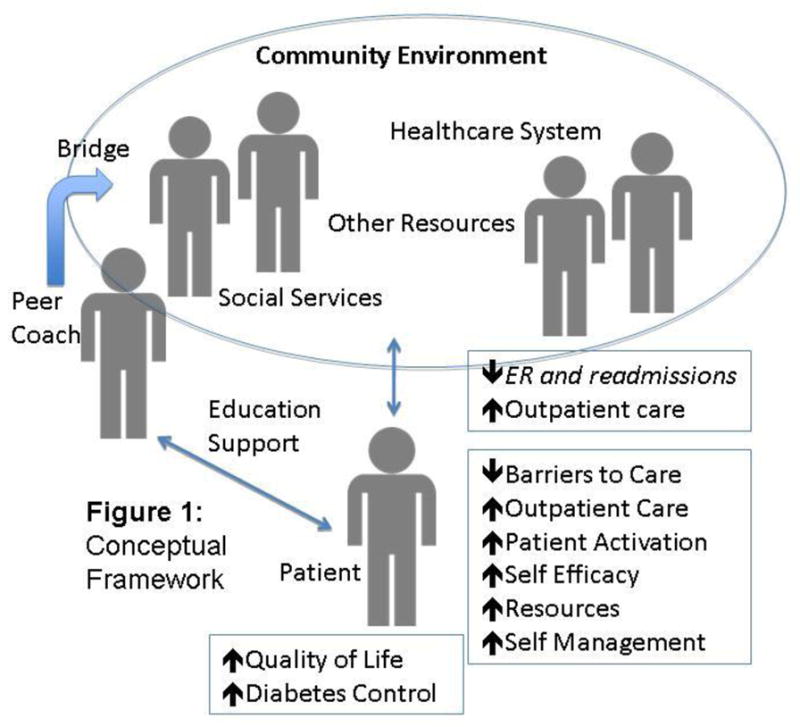
Peer-led model for “discharge to home” care coordination.
In both examples further studies will be required to formally test the effectiveness of community–based peer led models in improving clinical and patient centered outcomes (e.g., quality of life) compared to a nurse-led discharge support intervention or other models of prevention programs. Optimally this should be developed in a partnership model that integrates patients and other stakeholders from inception to dissemination.
Key strategies for implementing community-based diabetes programs
Consistent with the Chronic Care Model, key components must be in place in order to successfully implement a community-based diabetes program into specific communities. The key elements of the underlying infrastructure might be considered a “checklist” that must be completed before deployment can occur.
Key elements include the following:
Data collection and tracking system-The system must collect and report on the outcomes that the community or health system would like to manage to achieve improvement. The most common elements include glucose (HbA1c), lipid (LDL) and blood pressure control, but can also include vaccination requirements (influenza, pneumonia, hepatitis B), smoking status, aspirin use, depression and diabetes distress scores, and other self care management scores. Other long term outcomes that may need to be tracked and reported includes annual costs related to specialist visits, emergency and urgent care visits and hospitalizations. The data tracking and reporting system can be a simple registry specific for diabetes outcomes or a more sophisticated data analytics program that is tied to the electronic medical record or to a health information exchange that captures the required elements from all sources of patient care and interaction.
Staffing-A community-based program must have clinical and operational leadership to develop and sustain an ongoing program. A physician champion who is either an endocrinologist or primary care physician knowledgeable in the diabetes standards and literature can take on the role of medical leadership. They will provide guidance and support for the clinical decision support tools and be available as back up for complicated clinical situations. One or more certified diabetes educators will provide oversight for maintaining the integrity of the clinical interventions and the self management education programs. A program manager will have oversight responsibilities for staffing, program location, integration with existing community and health system services, distribution of tracking reports and communication between program staff, health system, community and patients on the program progress. Underlying support services may be required from finance, human resources and information technology to maintain smooth operations of the program. The program leadership will need to decide what type of staff mix will be needed to deliver the program content such as nurses, dietitians, health coaches or peer educators.
Training-It is important to ensure that all who that will be participating in the program delivery are appropriately trained. Physicians, health system operations staff and community leaders involved in the program should be knowledgeable in the basic concepts of the Chronic Care Model and team-based care. Staff who are directly responsible for the development and implementation of the program should be trained in the basic operations requirements, job descriptions and competencies to conduct each role. Staff who will be delivering the content must have training in the content delivery and provided with ancillary materials for patient education that is appropriate for the language, literacy and culture of the community where the program will operate.
Health systems integration-A community-based program must ensure that it can share summary reports, labs and other data with the local health systems and physician offices that it will be serving. A shared electronic medical system can facilitate this process but is not always easily available therefore other communication plans must be established.
Local resource identification-Identifying additional community resources that will assist patients in achieving their clinical and behavioral goals are critical since these systems may be more easily available to patients in their neighborhoods. Community resources can include local community health centers, county health resources, senior centers and YMCAs.
Ongoing communication among all parties-Regular meetings should be planned to resolve any operational and clinical issues, to discuss outcomes and to ensure that there is bidirectional dialogue between all the constituents of the program including patients and community leaders for recommendations and ongoing improvements.
At SWDI we have found that integrating peer educators into the glucose management team as part of community-based diabetes programs has been a key to successfully breaking down cultural and socio-economic barriers to improved care. Appropriate, standardized training is required to ensure the highest caliber of program delivery. In return for the significant effort made by the peer in training a stipend is offered after completing their basic training. Competencies must be met before peers can be placed in a community teaching environment. Once the peer educators complete the training and competencies they are considered eligible for employment and are compensated to conduct the Project Dulce DSME programs. Type of employment can vary and may be contracted or full-time. Peer educators can be hired by the health system, community health centers or other community based organizations to conduct programs depending on the needs of the individual community. At SWDI peer educators are integrated into the health system glucose management teams so that on-going support is provided with licensed professionals.
Conclusions
The population that requires knowledge and access to diabetes programs is growing worldwide. We must be able to offer information and support throughout the community where it is accessible to all and delivered in a format that is understood, regardless of literacy and socioeconomic status if we expect to make a difference in reducing the rates of developing diabetes and improving the control of existing disease. The Chronic Care Model offers a framework for creating and implementing community-based programs. The American Diabetes Association Standards of Care provides additional recommendations and guidelines to support program development. (22) Strategies such as explicit goal setting with patients; identifying and addressing language, numeracy, or cultural barriers to care; integrating evidence-based guidelines and clinical information tools into the process of care; and incorporating care management teams including nurses, pharmacists, and other providers have each been shown to optimize provider and team behavior and thereby catalyze reduction in A1C, blood pressure, and LDL. At SWDI, our community programs have been anchored by peer educators who have been trained to deliver content and serve a bidirectional role in strengthening the intervention as well as delivering it. Finally, scaling and replicating local programs that have been tested and evaluated can offer options for integrating community-based programs across the continuum of integrated delivery networks to enhance patient-centered outcomes and enable patient acceptability ultimately leading to improved patient engagement and satisfaction. (83–92)
Footnotes
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Athena Philis-Tsimikas and Linda C. Gallo declare that they have no conflict of interest.
Contributor Information
Athena Philis-Tsimikas, Email: tsimikas.athena@scrippshealth.org, Scripps Whittier Diabetes Institute, 9894 Genesee Ave, Suite 316, La Jolla, CA 92037, Telephone : 858-626-5628, Fax : 858-626-5680.
Linda C. Gallo, Email: lgallo@mail.sdsu.edu, San Diego State University, Department of Psychology, 9245 Sky Park Court Suite 115, San Diego, CA 92123, Telephone: (619) 594-4833, Fax: (619) 594-6780.
References
- 1.Anderson G. Chronic care: Making the case for ongoing care. Princeton, NJ: 2010. [Google Scholar]
- 2.Thorpe KE, Philyaw M. The medicalization of chronic disease and costs. Annual Review of Public Health. 2012;33:409–423. doi: 10.1146/annurev-publhealth-031811-124652. [DOI] [PubMed] [Google Scholar]
- 3.Wagner EH, Austin BT, Von Korff M. Improving outcomes in chronic illness. Manag Care Q. 1996;4(2):12–25. [PubMed] [Google Scholar]
- 4.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving Chronic Illness Care: Translating Evidence Into Action. Health Aff (Millwood) 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 5.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Affairs (Millwood) 2009;28:75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rittenhouse DR, Shortell SM, Gillies RR, et al. Improving chronic illness care: findings from a national study of care management processes in large physician practices. Medical Care Research and Review. 2010;67:301–320. doi: 10.1177/1077558709353324. [DOI] [PubMed] [Google Scholar]
- 7.Committee on Quality of Health Care in America and Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington D.C: 2001. [Google Scholar]
- 8.Center for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 9.Cowie CC, Rust KF, Ford ES, et al. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988–1994 and 2005–2006. Diabetes Care. 2009;32(2):287–294. doi: 10.2337/dc08-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lanting LC, Joung IM, Mackenbach JP, Lamberts SW, Bootsma AH. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients: a review. Diabetes Care. 2005 Sep;28(9):2280–2288. doi: 10.2337/diacare.28.9.2280. [DOI] [PubMed] [Google Scholar]
- 11.Peek ME, Cargill A, Huang ES. Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev. 2007 Oct;64(5 Suppl):101S–156S. doi: 10.1177/1077558707305409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kirk JK, Passmore LV, Bell RA, et al. Disparities in A1C Levels Between Hispanic and Non-Hispanic White Adults With Diabetes: A meta-analysis. Diabetes Care. 2008 Feb 1;31(2):240–246. doi: 10.2337/dc07-0382. [DOI] [PubMed] [Google Scholar]
- 13.Jiang HJ, Andrews R, Stryer D, Friedman B. Racial/ethnic disparities in potentially preventable readmissions: the case of diabetes. Am J Public Health. 2005 Sep;95(9):1561–1567. doi: 10.2105/AJPH.2004.044222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim H, Ross JS, Melkus GD, Zhao Z, Boockvar K. Scheduled and unscheduled hospital readmissions among patients with diabetes. Am J Manag Care. 2010 Oct;16(10):760–767. [PMC free article] [PubMed] [Google Scholar]
- 15.Caballero AE. Understanding the Hispanic/Latino patient. The American Journal of Medicine. 2011;124(10, Supplement):S10–S15. doi: 10.1016/j.amjmed.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 16.Cusi K, Ocampo GL. Unmet Needs in Hispanic/Latino Patients with Type 2 Diabetes Mellitus. The American Journal of Medicine. 2011;124(10, Supplement):S2–S9. doi: 10.1016/j.amjmed.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 17**.Stellefson M, Dipnarine K, Stopka C. The Chronic Care Model and Diabetes Management in US Primary Care Settings: A Systematic Review. Prev Chronic Dis. 2013;10:120180. doi: 10.5888/pcd10.120180. http://dx.doi.org/10.5888/pcd10.120180. Good discussion on the use of the Chronic Care Model specifically with diabetes care in primary care environments. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siminerio LM, Piatt G, Zgibor JC. Implementing the chronic care model for improvements in diabetes care and education in a rural primary care practice. Diabetes Educ. 2005;31(2):225–34. doi: 10.1177/0145721705275325. [DOI] [PubMed] [Google Scholar]
- 19.Piatt GA, Orchard TJ, Emerson S, Simmons D, Songer TJ, Brooks MM, et al. Translating the chronic care model into the community: results from a randomized controlled trial of a multifaceted diabetes care intervention. Diabetes Care. 2006;29(4):811–7. doi: 10.2337/diacare.29.04.06.dc05-1785. [DOI] [PubMed] [Google Scholar]
- 20.Siminerio LM, Piatt GA, Emerson S, Ruppert K, Saul M, Solano F, et al. Deploying the chronic care model to implement and sustain diabetes self-management training programs. Diabetes Educ. 2006;32(2):253–60. doi: 10.1177/0145721706287156. [DOI] [PubMed] [Google Scholar]
- 21.Smith SA, Shah ND, Bryant SC, Christianson TJ, Bjornsen SS, Giesler PD, Krause K, Erwin PJ, Montori VM Evidens Research Group. Chronic care model and shared care in diabetes: randomized trial of an electronic decision support system. Mayo Clin Proc. 2008;83(7):747–57. doi: 10.4065/83.7.747. [DOI] [PubMed] [Google Scholar]
- 22.American Diabetes Association. Standards of Medical Care in Diabetes 2013. Diabetes Care January. 2013;36(1):S11–S66. [Google Scholar]
- 23.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 24.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159–1171. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 25.Gary TL, Genkinger JM, Guallar E, Peyrot M, Brancati FL. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educ. 2003;29:488–501. doi: 10.1177/014572170302900313. [DOI] [PubMed] [Google Scholar]
- 26.Steed L, Cooke D, Newman S. A systematic review of psychosocial outcomes following education, self-management and psychological interventions in diabetes mellitus. Patient Educ Couns. 2003;51:5–15. doi: 10.1016/s0738-3991(02)00213-6. [DOI] [PubMed] [Google Scholar]
- 27.Ellis SE, Speroff T, Dittus RS, Brown A, Pichert JW, Elasy TA. Diabetes patient education: a meta-analysis and meta-regression. Patient Educ Couns. 2004;52:97–105. doi: 10.1016/s0738-3991(03)00016-8. [DOI] [PubMed] [Google Scholar]
- 28.Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med. 2004;164:1641–1649. doi: 10.1001/archinte.164.15.1641. [DOI] [PubMed] [Google Scholar]
- 29.Barker JM, Goehrig SH, Barriga K, et al. DAISY study. Clinical characteristics of children diagnosed with type 1 diabetes through intensive screening and follow-up. Diabetes Care. 2004;27:1399–1404. doi: 10.2337/diacare.27.6.1399. [DOI] [PubMed] [Google Scholar]
- 30.Heinrich E, Schaper NC, de Vries NK. Self-management interventions for type 2 diabetes: a systematic review. Eur Diabetes Nurs. 2010;7:71–76. [Google Scholar]
- 31.Frosch DL, Uy V, Ochoa S, Mangione CM. Evaluation of a behavior support intervention for patients with poorly controlled diabetes. Arch Intern Med. 2011;171:2011–2017. doi: 10.1001/archinternmed.2011.497. [DOI] [PubMed] [Google Scholar]
- 32.McGowan P. The efficacy of diabetes patient education and self-management education in type 2 diabetes. Can J Diabetes. 2011;35:46–53. [Google Scholar]
- 33.Cochran J, Conn VS. Meta-analysis of quality of life outcomes following diabetes self-management training. Diabetes Educ. 2008;34:815–823. doi: 10.1177/0145721708323640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fisher EB, Thorpe CT, Devellis BM, Devellis RF. Healthy coping, negative emotions, and diabetes management: a systematic review and appraisal. Diabetes Educ. 2007;33:1080–1103. doi: 10.1177/0145721707309808. discussion 1104–1106. [DOI] [PubMed] [Google Scholar]
- 35.Robbins JM, Thatcher GE, Webb DA, Valdmanis VG. Nutritionist visits, diabetes classes, and hospitalization rates and charges: the Urban Diabetes Study. Diabetes Care. 2008;31:655–660. doi: 10.2337/dc07-1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heisler M, Vijan S, Makki F, Piette JD. Diabetes control with reciprocal peer support versus nurse care management: a randomized trial. Ann Intern Med. 2010;153:507–515. doi: 10.7326/0003-4819-153-8-201010190-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heisler M. Different models to mobilize peer support to improve diabetes self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future research. Fam Pract. 2010;27(Suppl 1):i23–i32. doi: 10.1093/fampra/cmp003. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 38.Long JA, Jahnle EC, Richardson DM, Loewenstein G, Volpp KG. Peer mentoring and financial incentives to improve glucose control in African American veterans: a randomized trial. Ann Intern Med. 2012;156:416–424. doi: 10.1059/0003-4819-156-6-201203200-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tang TS, Funnell MM, Gillard M, Nwankwo R, Heisler M. The development of a pilot training program for peer leaders in diabetes: process and content. Diabetes Educ. 2011;37:67–77. doi: 10.1177/0145721710387308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tang T, Ayala GX, Cherrington A, Rana G. A review of volunteer-based peer support interventions in diabetes. Diabetes Spectrum. 2011;24:85–98. [Google Scholar]
- 41.Tang TS, Nwankwo R, Whiten Y, Oney C. Training peers to deliver a church-based diabetes prevention program. Diabetes Educ. 2012;38:519–525. doi: 10.1177/0145721712447982. [DOI] [PubMed] [Google Scholar]
- 42**.Dale JR, Williams SM, Bowyer V. What is the effect of peer support on diabetes outcomes in adults? A systematic review. Diabet Med. 2012;29:1361–1377. doi: 10.1111/j.1464-5491.2012.03749.x. Recent review of the current evidence of peer led support for diabetes outcomes. [DOI] [PubMed] [Google Scholar]
- 43.Foster G, Taylor SJ, Eldridge SE, Ramsay J, Griffiths CJ. Self-management education programmes by lay leaders for people with chronic conditions. Cochrane Database Syst Rev. 2007;(4):CD005108. doi: 10.1002/14651858.CD005108.pub2. [DOI] [PubMed] [Google Scholar]
- 44.Norris SL, Chowdhury FM, Van Le K, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med. 2006;23:544–556. doi: 10.1111/j.1464-5491.2006.01845.x. [DOI] [PubMed] [Google Scholar]
- 45*.Rosal MC, Ockene IS, Restrepo A, et al. Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income Latinos: Latinos en Control. Diabetes Care. 2011;34:838–844. doi: 10.2337/dc10-1981. There are very few peer-led SME randomized controlled studies with clinical outcomes documented. This study had clinical data as one of its outcomes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Deakin T, McShane CE, Cade JE. Review: group-based education in self management strategies improves outcomes in type 2 diabetes mellitus. Evidence Based Medicine. 2005;10(6):173–173. doi: 10.1136/ebn.8.4.111. [DOI] [PubMed] [Google Scholar]
- 47.Johnson TM, Murray MR, Huang Y. Associations between self-management education and comprehensive diabetes clinical care. Diabetes Spectrum. 2010;23:41–46. [Google Scholar]
- 48.Duncan I, Birkmeyer C, Coughlin S, Li QE, Sherr D, Boren S. Assessing the value of diabetes education. Diabetes Educ. 2009;35:752–760. doi: 10.1177/0145721709343609. [DOI] [PubMed] [Google Scholar]
- 49.Duncan I, Ahmed T, Li QE, et al. Assessing the value of the diabetes educator. Diabetes Educ. 2011;37:638–657. doi: 10.1177/0145721711416256. [DOI] [PubMed] [Google Scholar]
- 50.Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the diabetes prevention program into the community: The DEPLOY pilot study. Am J Prev Med. 2008;35(4):357–63. doi: 10.1016/j.amepre.2008.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lipscomb ER, Finch EA, Brizendine E, Saha CK, Hays LM, Ackermann RT. Reduced 10-year risk of coronary heart disease in patients who participated in a community-based diabetes prevention program: the DEPLOY pilot study. Diabetes Care. 2009;32(3):394–6. doi: 10.2337/dc08-1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kramer MK, McWilliams JR, Chen HY, Siminerio LM. A community-based diabetes prevention program: evaluation of the group lifestyle balance program delivered by diabetes educators. Diabetes Educ. 2011;37:659–668. doi: 10.1177/0145721711411930. [DOI] [PubMed] [Google Scholar]
- 53.Wagner E, Grothaus L, Sandhu N, et al. Chronic care clinics for diabetes in primary care. Diabetes Care. 2001;24(4):695. doi: 10.2337/diacare.24.4.695. [DOI] [PubMed] [Google Scholar]
- 54.Funnell MM, Brown TL, Childs BP, et al. National Standards for Diabetes Self-Management Education. Diabetes Care. 2012 Jan 1;35(Supplement 1):S101–S108. doi: 10.2337/dc12-s101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Educators AAoD. Community Health Workers American Association of Diabetes Educators (AADE) Position Statement. 2011 [Google Scholar]
- 56.Norris SL, Chowdhury FM, Van Le K, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med. 2006 May;23(5):544–556. doi: 10.1111/j.1464-5491.2006.01845.x. [DOI] [PubMed] [Google Scholar]
- 57.Davis KL, O'Toole ML, Brownson CA, Llanos P, Fisher EB. Teaching how, not what: the contributions of community health workers to diabetes self-management. Diabetes Educ. 2007 Jun;33 (Suppl 6):208S–215S. doi: 10.1177/0145721707304133. [DOI] [PubMed] [Google Scholar]
- 58.Foster G, Taylor SJ, Eldridge SE, Ramsay J, Griffiths CJ. Self-management education programmes by lay leaders for people with chronic conditions. Cochrane Database Syst Rev. 2007;(4):CD005108. doi: 10.1002/14651858.CD005108.pub2. [DOI] [PubMed] [Google Scholar]
- 59.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Self-monitoring and other non-pharmacological interventions to improve the management of hypertension in primary care: a systematic review. Br J Gen Pract. 2010 Dec;60(581):e476–488. doi: 10.3399/bjgp10X544113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Steinsbekk A, Rygg L, Lisulo M, Rise MB, Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res. 2012;12:213. doi: 10.1186/1472-6963-12-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gilmer TP, Philis-Tsimikas A, Walker C. Outcomes of Project Dulce: a culturally specific diabetes management program. Ann Pharmacother. 2005 May;39(5):817–822. doi: 10.1345/aph.1E583. [DOI] [PubMed] [Google Scholar]
- 62.Gilmer TP, Roze S, Valentine WJ, et al. Cost-effectiveness of diabetes case management for low-income populations. Health Serv Res. 2007 Oct;42(5):1943–1959. doi: 10.1111/j.1475-6773.2007.00701.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gilmer TP, Walker C, Johnson ED, Philis-Tsimikas A, Unutzer J. Improving treatment of depression among Latinos with diabetes using project Dulce and IMPACT. Diabetes Care. 2008 Jul;31(7):1324–1326. doi: 10.2337/dc08-0307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Philis-Tsimikas A, Fortmann A, Lleva-Ocana L, Walker C, Gallo LC. Peer-led diabetes education programs in high-risk Mexican Americans improve glycemic control compared with standard approaches: a Project Dulce promotora randomized trial. Diabetes Care. 2011 Sep;34(9):1926–1931. doi: 10.2337/dc10-2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Philis-Tsimikas A, Walker C, Rivard L, et al. Improvement in diabetes care of underinsured patients enrolled in project dulce: a community-based, culturally appropriate, nurse case management and peer education diabetes care model. Diabetes Care. 2004 Jan;27(1):110–115. doi: 10.2337/diacare.27.1.110. [DOI] [PubMed] [Google Scholar]
- 66.Bellamy L, Casas JP, Hingorani AD, Williams D. T2DM mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373(9677):1773–1779. doi: 10.1016/S0140-6736(09)60731-5. [DOI] [PubMed] [Google Scholar]
- 67.US Center for Health Statistics. Births: final data for 2008. Natl Vital Stat Rep. 2010:59. [PubMed] [Google Scholar]
- 68.Ferrara A. Increasing prevalence of gestational diabetes mellitus. Diabetes Care. 2007;30(S2):S141–S146. doi: 10.2337/dc07-s206. [DOI] [PubMed] [Google Scholar]
- 69.Ratner RE, Christophi CA, Metzger BE, Dabelea D, Bennett PH, Pi-Sunyer X, et al. Prevention of diabetes in women with a history of gestational diabetes: Effects of metformin and lifestyle interventions. J Clin Endocrinol Metab. 2008;93(12):4774–9. doi: 10.1210/jc.2008-0772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ferrara A, Hedderson MM, Albright CL, Ehrlich SF, Quesenberry CP, Jr, Peng T, et al. A pregnancy and postpartum lifestyle intervention in women with gestational diabetes mellitus reduces diabetes risk factors: a feasibility randomized control trial. Diabetes Care. 2011;34(7):1519–25. doi: 10.2337/dc10-2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dharkar-Surber Sapna, Fortmann Adelaide, Euyoque Johanna, Ruiz Monica, Hernandez Magdalena, Araujo Rachel, Schultz James, Gallo Linda, Philis-Tsimikas Athena. American Diabetes Association Professional Scientific Sessions. Philadelphia: 2012. Results of Peer-Led DM Prevention Program for High Risk Latino Women with GDM; p. 769-P. [Google Scholar]
- 72.Centers for Disease Control and Prevention (CDC), Division of Health Care Statistics. [Accessed May 6, 2013.];Number (in Thousands) of Hospital Discharges with Diabetes as Any-Listed Diagnosis, United States, 1988–2009. 2009 http://www.cdc.gov/diabetes/statistics/dmany/fig1.htm.
- 73.American Diabetes Association. Economic Costs of Diabetes in the U.S. in 2012. Diabetes Care. 2013 Apr 1;36(4):1033–1046. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vega WA, Rodriguez MA, Gruskin E. Health disparities in the Latino population. Epidemiol Rev. 2009;31(1):99–112. doi: 10.1093/epirev/mxp008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cook CB, Seifert KM, Hull BP, et al. Inpatient to outpatient transfer of diabetes care: planing for an effective hospital discharge. Endocr Pract. 2009 Apr;15(3):263–269. doi: 10.4158/EP.15.3.263. [DOI] [PubMed] [Google Scholar]
- 76.Burton R. Health Policy Brief: Care Transitions. Health Aff (Millwood) 2012 Sep 13; [Google Scholar]
- 77.Berwick DM, DHA ELiminating waste in us health care. JAMA. 2012;307(14):1513–1516. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- 78.Hackbarth G, Reischauer R, Miller M. Report to Congress: Medicare Payment Policy. Washington D.C: Medicare Payment Advisory Committee; 2007. [Google Scholar]
- 79.Shepperd S, Lannin NA, Clemson LM, McCluskey A, Cameron ID, Barras SL. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2013;1:CD000313. doi: 10.1002/14651858.CD000313.pub4. [DOI] [PubMed] [Google Scholar]
- 80.Laderman M, Loehrer S, McCarthy D. State Action on Avoidable Rehospitalizations (STAAR) Issue Brief: The Effect of Medicare Readmissions Penalties. Cambridge, MA: Institute for Healthcare Improvement; 2013. Feb, [Google Scholar]
- 81.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006 Sep;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 82.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009 Feb 3;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163:83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 84.Osborn CY, Cavanaugh K, Wallston KA, et al. Health literacy explains racial disparities in diabetes medication adherence. J Health Commun. 2011;16(Suppl 3):268–278. doi: 10.1080/10810730.2011.604388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rothman R, Malone R, Bryant B, Horlen C, DeWalt D, Pignone M. The relationship between literacy and glycemic control in a diabetes disease-management program. Diabetes Educ. 2004;30:263–273. doi: 10.1177/014572170403000219. [DOI] [PubMed] [Google Scholar]
- 86.O’Connor PJ, Sperl-Hillen JM, Rush WA, et al. Impact of electronic health record clinical decision support on diabetes care: a randomized trial. Ann Fam Med. 2011;9:12–21. doi: 10.1370/afm.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Garg AX, Adhikari NK, McDonald H, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA. 2005;293:1223–1238. doi: 10.1001/jama.293.10.1223. [DOI] [PubMed] [Google Scholar]
- 88.Smith SA, Shah ND, Bryant SC, et al. Evidens Research Group. Chronic care model and shared care in diabetes: randomized trial of an electronic decision support system. Mayo Clin Proc. 2008;83:747–757. doi: 10.4065/83.7.747. [DOI] [PubMed] [Google Scholar]
- 89.McLean DL, McAlister FA, Johnson JA, et al. SCRIP-HTN Investigators. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: Study of Cardiovascular Risk Intervention by Pharmacists Hypertension (SCRIP-HTN) Arch Intern Med. 2008;168:2355–2361. doi: 10.1001/archinte.168.21.2355. [DOI] [PubMed] [Google Scholar]
- 90.Wubben DP, Vivian EM. Effects of pharmacist outpatient interventions on adults with diabetes mellitus: a systematic review. Pharmacotherapy. 2008;28:421–436. doi: 10.1592/phco.28.4.421. [DOI] [PubMed] [Google Scholar]
- 91.Davidson MB, Ansari A, Karlan VJ. Effect of a nurse-directed diabetes disease management program on urgent care/emergency room visits and hospitalizations in a minority population. Diabetes Care. 2007;30:224. doi: 10.2337/dc06-2022. [DOI] [PubMed] [Google Scholar]
- 92.Stone RA, Rao RH, Sevick MA, et al. Active care management supported by home telemonitoring in veterans with type 2 diabetes: the DiaTel randomized controlled trial. Diabetes Care. 2010;33:478–484. doi: 10.2337/dc09-1012. [DOI] [PMC free article] [PubMed] [Google Scholar]