Abstract
Background
Mother-to-child transmission (MTCT) of Human immunodeficiency virus (HIV) through breastfeeding remains the most significant route infection among children. Although the current guideline is recommending continued breastfeeding for HIV exposed infants, significant proportion of infants have been subjected to early weaning to prevent HIV transmission. However the predictors of breastfeeding cessation among HIV positive mothers were not documented in Ethiopia. Therefore the objective of this study was to determine the predictors of breastfeeding cessation among HIV-infected women in Southern Ethiopia.
Methods
A facility based cross sectional study was conducted in Southern Ethiopia. The samples were selected by cluster sampling technique. The Kaplan-Meier curve was used to describe the survival time of breastfeeding and a step-wise multivariable Cox-proportional hazards regression model were used to identify the predictors of breastfeeding cessation. Both crude and adjusted hazard ratio were determined and p<0.05 was considered as statistically significant.
Result
The mean duration of breastfeeding among HIV positive mothers was 13.79 [95% CI: (12.97–14.59)] months. The Kaplan-Meier estimate showed that proportions of women who were breastfeeding at 6, 9, 12 and 17 months were 89.3%, 75.3%, 66% and 17%, respectively. Those mothers having a monthly income of ≤500 ETB [AHR = 0.16, 95% CI :(0.03–0.76)], having a family size of three and below [AHR = 0.12, 95%CI: (0.02–0.68), four and above [AHR = 0.07, 95%CI: (0.01–0.35)] and bottle feeding [AHR = 3.95, 95%CI: (1.64–9.51)] were also independent factors associated with breastfeeding cessation.
Conclusion
Above one third of HIV positive mothers stopped breastfeeding before 12 months. Monthly income, bottle feeding and family size were the independent predictors of breastfeeding cessations. Strengthening the current counseling and promotion modality on avoidance of bottle feeding and continued breastfeeding is recommended for improved HIV free survival.
Introduction
Mother-to-child transmission (MTCT) of HIV has remained the most significant route of HIV infection among children [1]. In the absence of interventions during pregnancy and delivery, HIV transmission through breastfeeding could be responsible for over a third of all childhood HIV infections [2], [3]. Breast milk can be a source of HIV, but on the other hand, infants, particularly those in low-income settings, are at increased risk of malnutrition, diarrhea, acute respiratory infection, and death if they are not breastfed [4].
Multiple studies in low-income countries have documented increased morbidity and mortality associated with early cessation of breastfeeding compared to continued breastfeeding among HIV exposed children. Early cessation of breastfeeding to prevent HIV transmission would increase the risk of severe morbidities and mortality associated among HIV exposed infants who were weaned early (at 4–6 months of age), compared with those who breastfed (BF) for longer periods [5], [6], [7], [8].
A study from Zambia revealed that breastfeeding cessation is associated with malnutrition which showed a significant decrease in weight-for-age Z-scores among HIV exposed infants who stopped breastfeeding early (at 4 months) compared to those who breastfed continuously [9]. Although the risk of HIV transmission increased as breastfeeding continues, HIV free survival of HIV exposed infants who breastfed beyond 6 months was similar to those of infants who ceased breastfeeding at 6th months [10], [11].
According to the revised national PMTCT guideline, HIV positive mothers are recommended to breastfeed exclusively for the first six months of life, followed by introduction of appropriate complementary feedings at sixth months with continued breastfeeding until 12–18 months [12]. However, there is a paucity of studies which show predictors of breastfeeding cessation among HIV positive mothers in Ethiopia. Identifying predictors of breastfeeding cessation among HIV infected women is important for targeting the education and counseling message to groups of women at risk for shorter breastfeeding which helps to increased HIV-free survival. The objective of this study is to assess the predictors of breastfeeding cessation among HIV positive mothers in Sidama Zone, Southern Ethiopia.
Methods
Ethics statement
Ethical approval was received from Hawassa University Institutional Review Board (IRB). Official letter of cooperation was also obtained from Sidama Zonal Health Department. The objective of the study was explained for the administrative body of the selected health institution and permission was obtained from the administration. The study objectives and procedures were explained and informed written consent was obtained from the respondents.
Study setting and sample
In Sidama Zone, there were 18 health institutions which provide ART and PMTCT services. Four heath institutions were excluded because they had no eligible study subjects. Hence, the remaining eligible fourteen health institutions were considered as clusters. From the eligible 14 health institutions, ten health institutions (clusters) were selected randomly. A facility based cross sectional study was conducted in randomly selected 10 government health institutions (3 hospitals and 7 health centers) providing ART and PMTCT services in Sidama Zone Southern Ethiopia [13]. Considering the power of the study and sample adequacy, all (n = 184) HIV positive mothers who have HIV exposed infants aged 6–17 months found in the randomly selected health institutions were included.
Data collection process and quality
Data were collected from all mother infant pairs found in the selected health institutions. The data were collected by health professionals recruited from respective health institutions and trained for two days on data collection techniques. The data collection process was closely supervised and the collected data were checked for completeness and consistency in the field.
Bottle feeding practices was measured by a 24-hour recall as recommended by WHO [14] and it was asked as “Did [Child Name] drink anything from a bottle with a nipple yesterday during the day or night time?”. Breastfeeding duration was assessed by asking the time lapse from date of birth to the time that a mother stopped breastfeeding. Those mothers who could not recall the month when they had stopped breastfeeding were excluded from the analysis.
Statistical analysis
After the data collection was completed, data were checked for completeness and consistency; the data were entered, cleaned, and coded. Data analysis was carried out by SPSS for windows version 20 (IBM® SPSS® Statistics, IBM Corp, New York). Descriptive statistics were computed for all continuous and categorical variables. The Kaplan Meier (KM) curve with log rank test was used to describe the survival time of breastfeeding, probability of breastfeeding cessation and to compare survival curves by monthly income, family size and bottle feeding. Univariate and multivariable forward stepwise Cox-proportional hazards regression models were used. Those statistically significant variables (p<0.05) in univariate analysis were entered in to multivariable forward stepwise Cox proportional hazards regression model to identify the independent predictors of breastfeeding cessation. Both crude and adjusted hazard ratio (HR) with calculated 95% confidence interval were reported and p<0.05 was considered as statistically significant.
Results
Socio-demographic characteristics
The mean (+SD) age of mothers was 28.85 (+5.41) years while the mean (±SD) age of infants were 10.42(±3.49) months. Above thirty seven percent (37.5%) and 24.5% of the infants were in the age group of 6–8 months and 9–11 months respectively. Fifty seven percent (57%) of the infants were male by sex. Most of the mothers (77.7%) had an educational status of primary level and below. Majority of the mothers (85.9%) had disclosed their sero status at least to their husbands. More than two third (67.2%) of the mothers were on ART treatment while 32.8% of the mothers were on the pre-ART phase. One quarter of the infants had introduced complementary food before 6 months. Above eighty four (84.2%) and 64.7% of HIV positive mothers had ANC follow up and health institution delivery respectively ( Table 1 ).
Table 1. Characteristics of HIV positive mother's infant pairs in Sidama Zone, Southern Ethiopia, 2012.
| Socio-demographic characteristics | Frequency | Percentage |
| Age of the mother(years) | ||
| ≤24 | 28 | 15.6 |
| 25–29 | 73 | 40.8 |
| ≥30 | 78 | 43.6 |
| Educational status | ||
| Primary education and below | 143 | 77.7 |
| Secondary and above | 41 | 22.3 |
| Presence of animal milk at home | ||
| Yes | 33 | 82.1 |
| No | 151 | 17.9 |
| ART status | ||
| Pre ART | 60 | 32.8 |
| On ART | 123 | 67.2 |
| HIV sero status disclosure | ||
| Yes | 158 | 85.9 |
| No | 26 | 14.1 |
| Current marital status | ||
| Married | 158 | 85.9 |
| Not married | 26 | 14.1 |
| Place of residence | ||
| Urban | 134 | 72.8 |
| Rural | 50 | 27.2 |
| Stigma and discrimination | ||
| Yes | 167 | 90.8 |
| No | 17 | 9.2 |
| ANC attendance | ||
| Yes | 155 | 84.2 |
| No | 29 | 15.8 |
| $Monthly income (n = 116) | ||
| ≤500 | 67 | 57.8 |
| 501–1000 | 29 | 25 |
| ≥1001 | 20 | 17.2 |
| Family size(n = 182) | ||
| ≤3 | 50 | 27.5 |
| 4–5 | 103 | 56.6 |
| ≥6 | 29 | 15.9 |
| Birth order(n = 176) | ||
| 1 | 54 | 30.7 |
| 2–3 | 94 | 53.4 |
| ≥4 | 28 | 15.9 |
| When know sero status | ||
| Before birth | 156 | 84.8 |
| After birth | 28 | 15.2 |
| Place of delivery | ||
| Health institution | 119 | 64.7 |
| Home | 65 | 35.3 |
| Age of introduction complementary feeding | ||
| Before 6 months | 135 | 75.8 |
| At 6 months and after | 43 | 24.2 |
| Age of infants (n = 184) | ||
| 6–8 months | 69 | 37.5 |
| 9–11 months | 45 | 24.5 |
| 12–17 months | 70 | 38 |
- Exchange rate 1 USD = 17.87 Ethiopian Birr (ETB).
Survival analysis for breastfeeding cessation
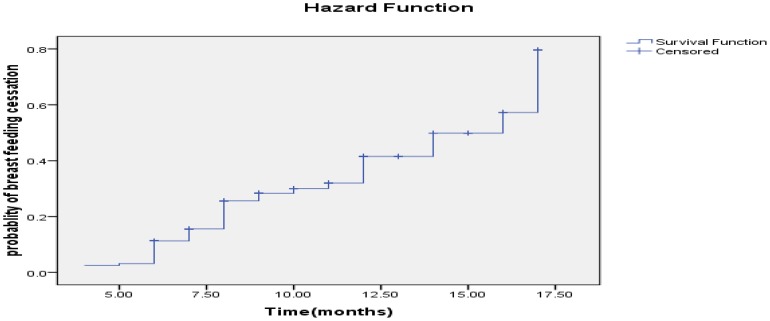
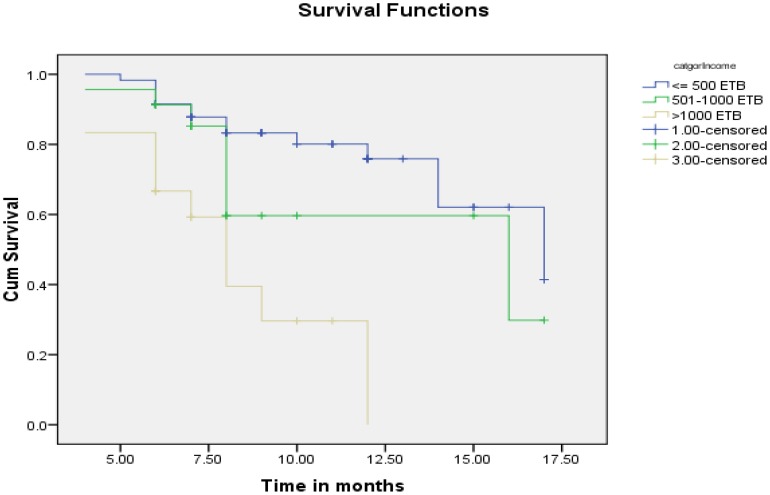
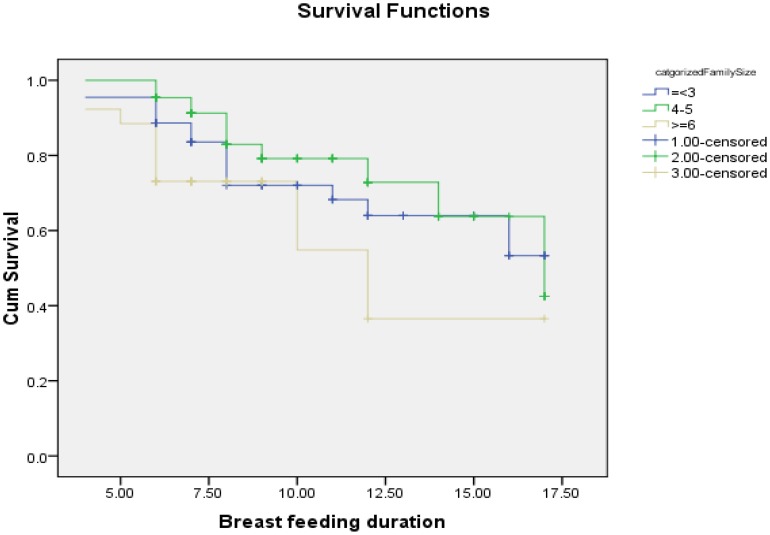
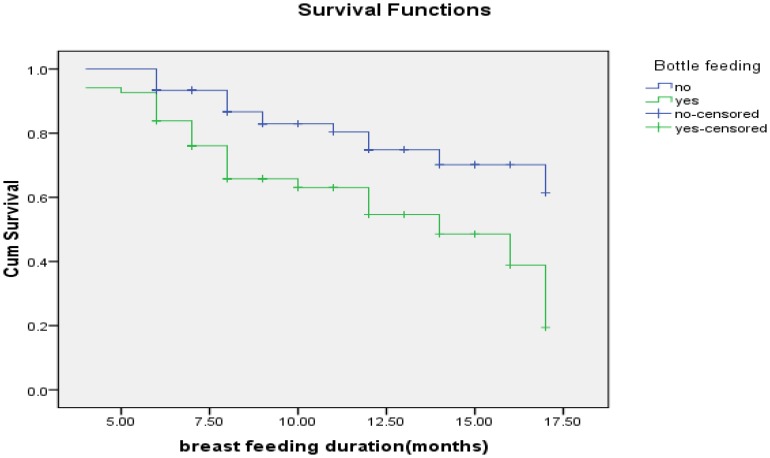
The estimated KM proportions of women who were breastfeeding at 6, 9, 12 and 17 months were 89.3%, 75.3%, 66% and 17%, respectively ( Figure 1 ). The mean duration of breastfeeding among HIV positive mothers was 13.79 [95% CI: (12.97–14.59) months. The median survival time for breastfeeding was 17 months. Twenty seven percent (27.7%) of HIV positive mothers had ceased breastfeeding at the time of the study. A test for comparing the equality of survival distribution between the different categories of income showed that there was a statistically significant difference in the survival distribution between different categories of income (Log Rank (Mantel-Cox)) test, chi squire = 19.266, Df = 2 p value = 0.001) ( Figure 2 ). Figure 3 and 4 shows the survival distribution of breastfeeding stratified based different categories of family size and bottle feeding respectively.
Figure 1. Probability of breastfeeding cessation of HIV positive mothers in Sidama Zone, Southern Ethiopia, 2012.
Figure 2. Survival function of breastfeeding duration stratified based on monthly income among HIV positive mothers in Sidama Zone, Southern Ethiopia, 2012.
Figure 3. Survival function of breastfeeding duration stratified based on bottle feeding practices of HIV positive mothers in Sidama Zone, Southern Ethiopia, 2012.
Figure 4. Survival function of breastfeeding duration stratified based on family size among HIV positive mothers in Sidama Zone, Southern Ethiopia, 2012.
The univariate analysis showed that mothers having animal(owned cows) milk at home, HIV status disclosure of the mother, educational status of mothers, monthly income, age of the mother, family size, infant age at initiation of complementary food, bottle feeding, place of residence and BMI(kg/m2) were significantly associated with cessation of breastfeeding (p<0.05).
Those HIV positive mothers having a monthly income of ≤500 ETB(Exchange rate 1 USD = 17 Ethiopian Birr (ETB)) [AHR = 0.16, 95% CI :(0.03–0.76)], having a family size of three and below [AHR = 0.12, 95%CI: (0.02–0.68), four and above [AHR = 0.07, 95%CI: (0.01–0.35)] and bottle feeding [AHR = 3.95, 95%CI: (1.64–9.51)] were also independent factors associated with breastfeeding cessation ( Table 2 ).
Table 2. Univariate and multivariable analysis of the predictors of breastfeeding cessation among HIV positive mothers in Sidama Zone, Southern Ethiopia, 2012.
| Variable | Crude HR [95%CI] | P-value | Adjusted HR[95%CI] | P value |
| Family size | ||||
| ≤3 | 0.59[0.25–1.38] | 0.22 | 0.12[0.02–0.68] | 0.017 |
| 4–5 | 0.45[0.20–0.98] | 0.047 | 0.07[0.01–0.35] | 0.001 |
| ≥6 | 1 | |||
| Bottle feeding | ||||
| Yes | 2.48[1.35–4.57] | 0.004 | 3.95[1.64–9.51] | 0.002 |
| No | 1 | 1 | ||
| Monthly income (ETB) *$ | ||||
| ≤500 | 0.19[0.09–0.45] | ≤0.001 | 0.16[0.03–0.76] | 0.021 |
| 501–1000 | 0.33[0.13–0.87] | 0.025 | 0.93[0.29–3.03] | 0.910 |
| ≥1001 | 1 | 1 | ||
| Age of the mother(years) | ||||
| ≤24 | 0.37[0.14–0.98] | 0.044 | 0.64[0.14–2.99] | 0.575 |
| 25–29 | 0.39[0.19–0.79] | 0.010 | 1.67[0.47–5.99] | 0.433 |
| ≥30 | 1 | |||
| Presence of animal milk at home | ||||
| Yes | 2.84[1.02–7.94] | 0.04 | 3.87[0.41–36.47] | 0.237 |
| No | 1 | 1 | ||
| HIV status disclosed | ||||
| Yes | 1 | |||
| No | 0.19[0.046–0.79] | 0.02 | ||
| Educational status of mothers | ||||
| Primary and bellow | 2.16[1.02–4.57] | 0.04 | ||
| Secondary and above | 1 | |||
| Age at introduction of complementary food | ||||
| Before 6 months | 1.99[1.03–3.85] | 0.04 | 0.86[0.23–3.23] | 0.822 |
| At 6 months and after | 1 | |||
| Place of residence | ||||
| Urban | 2.15[0.91–5.08] | 0.08 | ||
| Rural | 1 | |||
| BMI((kg m−2) | ||||
| <18.5 | 0.44[0.17–1.11] | 0.08 | ||
| 18.5–24.9 | 0.39[0.17–1.08] | 0.05 | ||
| ≥25 | 1 | |||
| Getting any food or cash support | ||||
| Yes | 1 | |||
| No | 0.92[0.46–1.83] | 0.82 | ||
| ART status | ||||
| Pre ART | 0.69[0.35–1.37] | 0.28 | ||
| On ART | 1 | |||
| Current marital status | ||||
| Married | 0.99[0.47–2.11] | 0.99 | ||
| Not married | 1 | |||
| When you know your sero status | ||||
| Before birth | 0.20[0.72–5.66] | 0.18 | ||
| After birth | 1 | |||
Discussion
Optimizing HIV free survival for infants born from HIV infected mothers is a major challenge in sub-Saharan Africa, where prevalence of HIV infection remains high among reproductive age women. The current WHO guideline emphasizes the importance of continued breastfeeding to improve HIV free survival in resource limited areas [5].
In this study, 66% of HIV positive mothers were breastfed their HIV exposed infants for 12 months. This is very low as compared to the study from Tanzania which report that 95% of HIV positive mothers breast fed at 12 months [15]. But a study from Brazil revealed that only 33.7% of HIV positive mothers breast fed their infants at 12 months which is lower as compared to our finding [16]. The mean breastfeeding duration of this study was shorter as compared to the study done in Tanzania [15].
Breastfeeding cessation was associated with presence of animal milk at home (milk from owned cows). This might be due to the fact that mothers who have animal milk at home provide cow milk as a replacement of breast milk and stop breastfeeding earlier due to the fear of HIV transmission through breastfeeding. Similarly, monthly income was also independent predictor of early breastfeeding cessation. This might be due to the fact that those mothers who have relatively better monthly income would have the capacity to afford complementary food. Similar studies from South Africa and Uganda have revealed that mothers who were economically better-off were more likely to introduce complementary food for their infants at an early age compared with economically poor mothers [17], [18], [19]. In this study, having larger family size is protective of early breastfeeding cessation. This might be related to the economic capacity of the household to afford other foods to replace breast milk to prevent mother to child transmission of the virus through breastfeeding.
This study found that introduction of food before 6 months was not a predictor of breastfeeding cessation in the multivariable model. However other studies in both developing and developed countries which showed introduction of cow's/powdered milk and infant formula were associated with earlier cessation of breastfeeding [15], [20], [21], [22].
Our study did not show statistically significant association between mothers' educational status with early cessation of breastfeeding. But disclosure of HIV status was statistically associated with breastfeeding cessation. In these regards a study done in Kisumu showed that the educated mothers are more likely to stopped breastfeeding [23].
The study from Tanzania reported that instrumental and material support (which included help with domestic chores, monetary assistance, transportation, etc.) was associated with delayed cessation of breastfeeding [15]. However this study did not find any statistically significant association between getting any food or cash support and cessation of breastfeeding.
Limitations
There are two major limitations in this study. The study design was institutional based cross sectional study so that the breastfeeding duration was determined by asking the mother to recall the time when she had stopped breastfeeding and this study did include HIV exposed infants of age only 6 months and above. This would introduce recall bias and selection bias respectively.
Conclusion
Above one third of HIV positive mothers stopped breastfeeding before 12 months. The estimated KM proportions of women who were breastfeeding at 6, 9, 12 and 17 months were 89.3%, 75.3%, 66% and 17%, respectively. Monthly income, bottle feeding and family size were the independent predictors of breastfeeding cessations. In this study having low monthly income and having larger family size were associated with decreased risk of cessation while bottle feeding was associated with increased risk of breastfeeding cessation. Therefore, strengthening current counseling modality on avoidance of bottle feeding and continued breastfeeding for improved HIV free survival and further research are recommended.
Funding Statement
Funding provided by HENNA (Higher Education Network for Applied Human Nutrition between Eastern Africa and Europe) (http://hennaproject.org) project funded this study. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.WHO/UNAIDS/UNICEF (2009) Towards Universal Access: Scaling up HIV priority interventions in the health sector. Progress Report.
- 2. Coovadia H, Rollins N, Bland R, Little K, Bennish M, et al. (2007) Mother-to-child transmission of HIV-1 infection during exclusive breastfeeding in the first 6 months of life: an intervention cohort study. Lancet 369: 1107–1116. [DOI] [PubMed] [Google Scholar]
- 3. Breastfeeding and HIV International Transmission Study Group (2004) Late postnatal transmission of HIV-1 in breast-fed children: an individual patient data meta-analysis. Journal of infectious diseases 189: 2154–2166. [DOI] [PubMed] [Google Scholar]
- 4. Young SL, Mbuya MNN, Chantry CJ, Geubbels EP, Israel-Ballard K, et al. (2011) Current Knowledge and Future Research on Infant Feeding in the Context of HIV: Basic, Clinical, Behavioral, and Programmatic Perspectives. Adv Nutr 2: 225–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Taha TE, Hoover DR, Chen S, Kumwenda NI, Mipando L, et al. (2011) Effects of Cessation of Breastfeeding in HIV-1 Exposed, Uninfected Children in Malawi. Clinical Infectious Diseases 53: 388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Onyango-Makumbi C, Bagenda D, Mwatha A, Omer SB, Musoke P, et al. (2010) Early weaning of HIV-exposed uninfected infants and risk of serious gastroenteritis: findings from two perinatal HIV prevention trials in Kampala, Uganda. J Acquir Immune Defic Syndr 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Creek T, Kim A, Lu L, Bowen A, Masunge J, et al. (2010) Hospitalization and mortality among primarily non-breastfed children during a large outbreak of diarrhea and malnutrition in Botswana. J Acquir Immune Defic Syndr 53: 14–19. [DOI] [PubMed] [Google Scholar]
- 8. Kuhn L, Aldrovandi GM, Sinkala M, Kankasa C, Semrau K, et al. (2008) Effects of Early, Abrupt Weaning on HIV-free Survival of Children in Zambia. N Engl J Med 359: 130–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Arpadi S, Fawzy A, Aldrovandi G, Kankasa C, Sinkala M, et al. (2009) Growth faltering due to breastfeeding cessation in uninfected children born to HIV-infected mothers in Zambia. American Journal of Clininical Nutrition 90: 344–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kagaayi J, Gray RH, Brahmbhatt H, Kigozi G, Nalugoda F, et al. (2008) Survival of infants born to HIV-positive mothers, by feeding modality, in Rakai, Uganda. PLoS ONE 3: e3877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thior I, Lockman S, Smeaton L, Shapiro R, Wester C, et al. (2006) Breastfeeding plus infant zidovu-dine prophylaxis for 6 months vs formula feeding plus infant zidovudine for 1 month to reduce mother-to-child HIV transmission in Botswana: a randomized trial: the Mashi Study. JAMA 296: 794–805. [DOI] [PubMed] [Google Scholar]
- 12.HAPCO/FMOH (2007) Guidelines For Prevention of Mother-to-Child Transmission of HIV in Ethiopia MOH: Addis Ababa.
- 13.Ethiopia CCSA (2007) Summary and Statistical Report of the 2007 Population and Housing Census, Population Census Commission, Addis Ababa, Federal Democratic Republic of Ethiopia.
- 14.WHO U, IFPRI, UC Davis, USAID FANTA (2008) Indicators for assessing infant and young child feeding practices. Geneva, Switherland World Health Organization. Available: (http://wwwwhoint/hild_adolescent_health/documents/9789241596664/en/indexhtml). Accessd 2011 May 25.
- 15. Petraro P, Duggan C, Msamanga G, Peterson KE, Spiegelman D, et al. (2011) Predictors of breastfeeding cessation among HIV-infected women in Dar es Salaam,Tanzania. Maternal and Child Nutrition 7: 273–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chaves RG, Lamounie JA, César CC (2007) Factors associated with duration of breastfeeding. J Pediatr (Rio J) 83: 241–246. [DOI] [PubMed] [Google Scholar]
- 17. Doherty T, Sanders D, Jackson D, Swanevelder S, Lombard C, et al. (2012) Early cessation of breastfeeding amongst women in South Africa: an area needing urgent attention to improve child health. BMC Pediatrics 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fadnes LT, Engebretsen IM, Wamani H, Semiyaga NB, Tylleskär T, et al. (2009) Infant feeding among HIV-positive mothers and the general population mothers: comparison of two cross-sectional surveys in Eastern Uganda. BMC Public Health 9 http://www.biomedcentral.com/1471-2458/1479/1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ghuman M, Saloojee H, Morris G (2009) Infant feeding practices in a high HIV prevalence rural district of KwaZulu-Natal, South Africa. South African Journal of Clinical Nutrition 22: 74–77. [Google Scholar]
- 20. Berra S, Sabulsky J, Rajmil L, Passamonte R, Pronsato J, et al. (2003) Correlates of breastfeeding duration in an urban cohort from Argentina. Acta Paediatrica 92: 952–957. [DOI] [PubMed] [Google Scholar]
- 21. Hornell A, Hofvander Y, Kylberg E (2001) Solids and formula: association with pattern and duration of breastfeeding. Pediatrics 107: E38. [DOI] [PubMed] [Google Scholar]
- 22. Agboado G, Michel E, Jackson E, Verma A (2010) Factors associated with breastfeeding cessation in nursing mothers in a peer support programme in Eastern Lancashire. BMC Pediatrics 10 http://www.biomedcentral.com/1471-2431/1410/1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Morgan M, Masaba R, Nyikuri M, Thomas T (2010) Factors affecting breastfeeding cessation after discontinuation of antiretroviral therapy to prevent mother-to-child transmission of HIV. AIDS Care 22: 866–873. [DOI] [PubMed] [Google Scholar]