Abstract
Objective
Few studies have examined brain changes in response to effective weight loss; none have compared different methods of weight-loss intervention. We compared functional brain changes associated with a behavioral weight loss intervention to those associated with bariatric surgery.
Methods
15 obese participants were recruited prior to adjustable gastric banding surgery and 16 obese participants were recruited prior to a behavioral diet intervention. Groups were matched for demographics and amount of weight lost. fMRI scans (visual food motivation paradigm while hungry and following a meal) were conducted before, and 12 weeks after surgery/behavioral intervention.
Results
When compared to bariatric patients in the pre-meal analyses, behavioral dieters showed increased activation to food images in right medial PFC and left precuneus following weight loss. When compared to behavioral dieters, bariatric patients showed increased activation in in bilateral temporal cortex following the weight loss.
Conclusions
Behavioral dieters showed increased responses to food cues in medial PFC – a region associated with valuation and processing of self-referent information – when compared to bariatric patients. Bariatric patients showed increased responses to food cues in brain regions associated with higher level perception—when compared to behavioral dieters. The method of weight loss determines unique changes in brain function.
Keywords: functional MRI, bariatric surgery, neuroscience, weight loss, neuroimaging
Introduction
Benefits of weight-loss and body fat reduction in obese people include decreased blood pressure and triglycerides, and improved cholesterol ratio and glucose tolerance (1, 2) Although behavioral interventions that modify diet and or physical activity are common, the short term effects (weight loss) and longer term effects (weight maintenance) of these approaches are variable (3). Bariatric surgery is also an effective method for weight loss yielding long-term outcomes superior to behavioral methods (4), though the enduring effectiveness has not been established. Laparoscopic adjustable gastric banding (LAGB) is one form of bariatric surgery that has become a favored procedure with mild to moderately obese individuals (5). With faster recovery and lower risk of complications compared to gastric bypass surgery, it is very successful. People who undergo LAGB achieve 30% excess weight loss 6 months post-surgery, 40% 1 year post-surgery, and 50% 2 years post-surgery (6, 7). The majority of successful LAGB patients experience reduced hypertension, hyperlipidemia, sleep apnea, diabetes, and depression (8, 9).
There has been recent interest in characterizing the brain's role in appetite, food motivation, and obesity. Functional magnetic resonance imaging (fMRI) studies provide evidence that the brains of obese and healthy weight individuals differ in their responses to visual food cues in regions associated with reward (striatum, orbitofrontal cortex, insula), homeostatic regulation (hypothalamus), and cognitive control (prefrontal cortex (PFC), cingulate cortex) (10). One study examined brain responses to visual food stimuli in individuals who had successfully maintained long-term weight loss. They found that successful weight-loss maintainers showed greater functional activation in left superior frontal and right middle temporal cortex (11). Cross-sectional studies have determined that post-obese individuals demonstrate greater activation in dorsolateral PFC when exposed to food cues, a pattern of activation that is most consistently found among lean individuals (12, 13). Taken together, these findings suggest that higher neural activation in regions associated with cognitive control or “rational” decision-making is associated with successful weight loss. This may serve as one mechanism by which healthy choices are made, and weight loss is achieved and maintained.
Few studies have employed a longitudinal approach to examine the effects of behavioral weight loss on the brain. Rosenbaum and colleagues induced a 10% weight loss in an inpatient setting with a liquid diet, and used fMRI to demonstrate increased activations in PFC (inferior frontal gyrus), parahippocampus, middle temporal gyrus, lingual gyrus, and brainstem (14). Conversely, the same study demonstrated decreases in activation in hypothalamus, cingulate, and middle frontal gyrus. A study examining brain changes associated with an outpatient behavioral weight loss intervention reported decreased activation to food versus control pictures in medial prefrontal cortex, inferior parietal lobule, precuneus, posterior cingulate, premotor cortex and angular gyrus (15). This study only examined a fasted state, did not include a control group comparison, and did not collect data on a post-meal state, and the authors encouraged future studies to examine both fasted and fed appetite states. The changes observed in these studies may be due to the weight loss itself or due more specifically to the nature of the intervention (i.e. inpatient liquid diet or outpatient behavioral intervention). To our knowledge, no study has examined the how behavioral weight loss interventions change brain function when controlling for the type of weight loss intervention.
A few published studies have examined the effects of bariatric surgical interventions on brain function. Specifically, our group examined LAGB and found increased activation in anterior PFC, and decreased activity in insula, parahippocampal gyrus, and medial PFC (16).
Ochner and colleagues reported similar findings associated with Roux-en-Y gastric bypass surgery (17, 18). Specifically, they noted reduced activations in both reward (striatum) and inhibitory regions (ventromedial and dorsolateral PFC) in a fasted state, but no significant changes in a fed state.
The goal of the current study was to examine brain activation changes associated with successful weight loss in dieters and bariatric patients in both hungry and fed states. It was hypothesized that diet and bariatric participants would exhibit different functional brain changes from pre to post weight loss. Specifically, it was predicted that in both hungry and fed states, dieters would exhibit greater increases in brain activation in regions associated with cognitive control when compared to bariatric patients. In contrast, bariatric patients were expected to show greater decreases in food motivation and reward brain regions in both hungry and fed states when compared to diet participants.
Methods and Procedures
Participants
Diet participants
16 diet participants (5 males) were selected from a larger behavioral weight-loss intervention study (120 participants) [NIH DK080090] that recruited using advertisements placed in local news outlets, broadcast emails, and a university-based weight management center (Table 1). Obese participants with a BMI between 30-45 kg/m2 were recruited to participate in a three-month weight loss and six-month maintenance intervention that involved behavioral strategies, moderate calorie restriction, and titrated physical activity. Exclusion criteria included participation in a research project involving weight loss or physical activity in the previous six months, smoking, special diets (i.e. vegetarian, Atkins), use of appetite or metabolic medications (i.e. thyroid, beta blockers, Meridia), or the inability to exercise (i.e. walk). Participants' age range was 23-52 years, M = 40.6, SD = 7.1). Fourteen of the dieting participants had attended college. Participants were selected for this study, blind to imaging data, based solely on demographic criteria.
Table 1. Participant demographics.
| Diet Group | Total N | Sex | Age (years) x̄, σ | Attended college | % weight lost |
|---|---|---|---|---|---|
| Behavioral | 16 | 5 males | 40.6, 7.1 | 14 | 10.8% |
| Bariatric | 15 | 3 males | 41.4, 9.8 | 11 | 9.3% |
Surgical participants
15 pre-surgical participants (3 males) were identified at two surgical sites in the Kansas City area. Obese participants who had decided to undergo adjustable gastric banding weight loss surgery (LapBand®) were recruited for the study (Table 1). As the majority of participants seeking bariatric surgery in the recruited BMI range had a history of diabetes, patients who had well-controlled diabetes and were not taking insulin (most recent hemoglobin A1c < 7) were included. Participants' age range was 21-56 years, M = 41.4, SD = 9.8). Eleven of the bariatric patients had attended college.
Exclusion criteria for both groups included current eating disorder, current major depression, history of neurological disease, pregnancy within the past 6 months, planning a pregnancy within 12 months, cancer, recent cardiac event (heart attack), and internal metal objects that pose risks in a strong magnetic field. Individuals with a BMI ≥ 46 kg/m2 were also excluded, as these individuals were unable to comfortably lie in the MRI scanner. Individuals were ineligible if they reported use of insulin, appetite suppressants, and stimulants. In contrast, given the prevalence of subclinical depression among patients seeking bariatric surgery, participants taking psychotropic medications not directly targeting the mesolimbic dopamine system (selective serotonin reuptake inhibitors) were included in the bariatric study.
No statistically significant differences between the diet and bariatric groups were observed for age [t(29) = 0.27; p = .79], education [χ2 = -1.89; p = .60], sex [χ2 = 0.51; p = .47], pre-intervention BMI [t(29) = 1.59; p = .12], post-intervention BMI [t(29) = 1.71; p = .10], or percent of weight lost [9.3% bariatric vs. 10.8% diet; t(29) = 1.02; p = .32].
Design and Procedure
We scanned 31 obese participants at two time points: once before commencing weight loss intervention and once 12 weeks after completing the intervention (16 following the behavioral intervention; 15 following LAGB surgery). At each time point, participants were scanned while hungry (following at least a 4-hour fast) and after eating a small standardized meal. Prior to scanning, participants were weighed and their height was recorded. Immediately prior to each of the scans (premeal and postmeal), participants were asked to rate their hunger on a visual analog scale (VAS) ranging from 1 to 100. The study was approved by the Human Subjects Committee of the University of Kansas Medical Center and the Institutional Review Board at the University of Missouri-Kansas City. All participants provided written informed consent.
fMRI Food motivation paradigm
The block experimental paradigm is detailed in previous reports (19, 20). Participants viewed pictures of food, animals, and blurred baseline images during two scanning sessions 1) after fasting for at least four hours (pre-meal condition) and 2) immediately after eating a small uniform meal (post-meal) that was standardized for energy [Kcal = 500] and micronutrient content (e.g., a weighed lean meat [turkey or ham] sandwich, carrot sticks, a piece of fruit, and skim milk). The order of sessions (pre-meal, post-meal) was counterbalanced across subjects. The caloric and macro-nutrient contents of the meals were matched across diet and surgical groups pre-intervention. The format of the foods (i.e., wraps vs. sandwiches) was different for the bariatric participants so they could adhere to post-surgical dietary guidelines.
Food and animal images were obtained from professional stock photography and matched to baseline images on brightness, resolution, and size. Animal (non-food) images were used to control for general interest and visual richness. In a pilot image validation study, food and animal images were rated based on the extent to which they were appetizing, exciting (arousal), and pleasant (valence), using established methods (21). Selected food images were significantly more appetizing than selected animal images (p < .001). No significant difference existed between the food and animal image groups with regard to valence (p = .55) or arousal (p = .96). These food and animal images were blurred so as to be unrecognizable with a phase randomized Fast Fourier Transform in MATLAB (The MathWorks, Inc., Natick, MA) program. Blurred images were used as baseline visual comparison stimuli to control for visual cortex activation during the paradigm. All images were presented once to each subject. Each functional scan involved three repetitions of each block of each stimulus condition type (i.e., food or animal), alternated between blocks of blurred images). This well-validated food motivation paradigm has been described in several published studies (19, 22, 23). Visual stimuli were projected from the stimuli-generating software (Presentation, Neurobehavioral Systems, Inc., Albany, CA) onto a screen. Stimulus presentation time was 2.5 seconds, with an interstimulus interval (ISI) of 0.5 seconds. Within each of the two functional scans there was a total of 13 blocks of stimuli presentation; within each block, 10 images were presented. The order of category presentation was counterbalanced across subjects.
Image Acquisition
Scanning was performed at the Hoglund Brain Imaging Center on a 3 Tesla head-only Siemens Allegra scanner (Siemens, Erlangen, Germany) fitted with a quadrature head coil. Participants' heads were immobilized with head cushions. Following automated scout image acquisition and shimming to optimize field homogeneity, a structural scan was completed. T1-weighted anatomic images were acquired with a 3D magnetization prepared rapid acquisition gradient echo (MPRAGE) sequence (TR/TE = 23/3.06 ms, flip angle = 8°, field of view [FOV] = 192 × 100 mm, matrix = 192 × 192, slice thickness = 1 mm) used for slice localization for the functional scans, Talairach transformation, and coregistration with fMRI data. After structural scans, two gradient echo BOLD scans were acquired in 43 contiguous oblique axial slices at a 40° angle (repetition time/echo time [TR/TE] = 3000/30 ms, flip angle = 90°, field of view [FOV] = 220 mm, matrix =64×64, slice thickness =3 mm, .5 skip, in-plane resolution = 3×3 mm, 130 data pts).
Data Analysis
Preprocessing steps included trilinear 3D motion correction, sinc-interpolated slice scan time correction, 3D spatial smoothing with 4-mm Gaussian filter, and high pass filter temporal smoothing. Functional images were realigned to the anatomic images obtained within each session and normalized to Talairach and Tournoux's stereotaxic atlas (24). Runs containing motion of more than 4 mm along any axis (x, y, or z) were discarded.
Whole Brain Statistical Analyses
Activation maps were generated using statistical parametric methods (25) and random effects in Brain Voyager QX (Brain Innovation, Maastricht, Netherlands, 2004). Statistical contrasts were conducted using multiple regression analysis with the general linear model, allowing multiple predictors to be built into the model. Regressors representing experimental conditions of interest were modeled with a hemodynamic response filter and entered into the multiple regression analysis. Contrasts between conditions of interest were assessed with t-statistics. Voxel values were considered significant if the activation survived a statistical cluster-based threshold (α < .05 [p < .01, k = 7 voxels]), determined by Monte Carlo simulation (26, 27) to correct for multiple comparisons across whole brain. The results from one bariatric participant in the fed condition were removed due to motion on two runs in excess of 4 mm. Separate 3-way ANOVAs (Group × Condition × Stimulus) were performed for the hungry and fed conditions. First, analyses were conducted pre-meal while participants (diet vs. bariatric) were hungry using a Condition (Pre-weight loss, Post-weight loss) × Stimulus (Food, Nonfood) repeated measures ANOVA model. Next, analyses were conducted post-meal (diet vs. bariatric) after participants had been fed also using a Condition (Pre-weight loss, Post-weight loss) × Stimulus (Food, Nonfood) repeated measures ANOVA model. Statistical parametric maps were overlaid on three-dimensional renderings of an averaged-group brain.
Results
Self-reported Hunger Ratings
We conducted independent samples t-tests for the VAS hunger ratings taken prior to the pre-meal scans. Behavioral diet and bariatric groups did not differ significantly on VAS hunger ratings taken prior to the pre-meal scans (p > .1, t -test). We conducted independent samples t-tests for the VAS hunger ratings prior to the post-meal (fed) scans as well. Again, behavioral and bariatric groups were not significantly different (p >. 1). In contrast, both groups reported substantially decreased hunger following the meal (p 's<.001).
When participants were collapsed across treatment groups (diet, bariatric), independent samples t-tests revealed that before the weight loss intervention there were group differences in hunger ratings before the pre-meal scan between those who had the pre-meal scan first (M = 60.4) vs. those who had the postmeal scan first (M = 30.6); [t(28) = 3.5; p = .002]. However, the percentage of participants in each of the groups (premeal scan first, postmeal scan first) did not differ by treatment group,[χ2 = .29, p = .59]. There were no significant group differences before the weight loss intervention between hunger ratings before the post-meal scan. Further, there were no significant differences after the weight loss intervention in hunger ratings pre-meal or post-meal.
Hungry: Diet vs. Bariatric x Pre to Post Weight loss Interaction
In the pre-meal Condition (Pre-, Post-weight loss) x Stimulus type (Food, Nonfood) interaction, diet participants showed significantly greater changes in right medial prefrontal cortex (Figure 2) and left precuneus. Bariatric participants showed no significantly greater changes in brain activation from pre- to post-weight loss than diet participants (Table 2).
Figure 2.

Regions showing significantly greater change in the behavioral diet group vs. the bariatric group in right medial prefrontal cortex, and left precuneus to food versus nonfood pictures in the premeal condition.
Table 2.
Regions reaching significance for the contrasts between food and non-food stimuli categories between groups (α < 0.05, corrected, random effects).
| Contrast and Region | Coordinates | Extent of Activation (mm3) | |||
|---|---|---|---|---|---|
| x | y | z | t | ||
| Pre-meal (Hungry) | |||||
| Diet patients > Bariatric patients | |||||
| Right Medial prefrontal cortex BA 9 | 6 | 50 | 19 | 3.72 | 216 |
| Left Precuneus BA 19 | -30 | -67 | 40 | 4.04 | 567 |
| Bariatric patients > Diet patients | |||||
| None | |||||
| Post-meal (Fed) | |||||
| Diet patients > Bariatric patients | |||||
| None | |||||
| Bariatric patients > Diet patients | |||||
| Right Middle Temporal gyrus | 48 | -55 | 7 | 3.98 | 216 |
| Left Inferior temporal gyrus/occipital | -42 | -64 | -2 | 4.82 | 783 |
Fed: Diet vs. Bariatric Changes x Pre to Post Weight loss interaction
In the Postmeal Condition (Pre-, Post-weight loss) x Stimulus type (Food, Nonfood) interaction, bariatric participants showed significantly greater changes in bilateral temporal cortex. Diet participants showed no significantly greater changes pre-to post weight loss than bariatric participants (Table 2).
Discussion
We compared brain activation changes associated with weight loss in individuals who underwent behavioral diet intervention vs. laparoscopic banding surgery. This study provides the first evidence of the neural mechanisms supporting weight loss in two distinct methods of successful, intentional weight loss. Both diet and surgical participants have altered brain activations in response to visual food cues following weight loss. However, changes in activation patterns were different in the two treatment groups.
Consistent with our hypotheses, we observed significant activation changes for behavioral diet weight loss participants compared to surgical participants in brain regions associated with self-referential processing and valuation when participants were hungry. Interestingly, not only did diet weight loss participants demonstrate increases in medial prefrontal cortex, the bariatric weight loss participants demonstrated decreases in medial prefrontal cortex. This could be due to the behavioral dieters experiencing greater salience and importance on food cues. Behavioral and recent neuroimaging data demonstrate that if one voluntarily restricts one's intake of food, the reward value, attentional bias, and salience of food cues increase (28). The bariatric participants, on the other hand, showed decreases in medial prefrontal cortex, which supports the notion that surgical weight loss patients undergo a “forced” dietary restriction in avoiding discomfort that renders food cues to be less rewarding and less salient. This may be evident in our observed decreases in medial prefrontal cortex activation in surgical participants. Bariatric participants may be also more disconnected from the self-referent experience of hunger. In Hare and colleagues' study (29), healthy weight individuals who were classified as “self-controllers” had greater activation in medial prefrontal cortex, consistent with our findings. It may be that the bariatric participants have the salience of food and self-referential thought decreased through the surgically placed laparoscopic band. Converging evidence from Ochner and colleagues (17) demonstrated decreased activations in ventromedial and dorsolateral prefrontal cortex in a fasted state after Roux-en-Y surgical participants had lost weight.
Also in the hungry condition, we observed significant changes in the precuneus, parallel to the medial prefrontal cortex changes. The diet weight loss participants showed increases in precuneus activity after losing weight whereas the bariatric participants showed decreases. The decreased activity in precuneus demonstrated by bariatric participants is consistent with a study by Murdaugh and colleagues (15), showing decreased activation to food pictures in precuneus post-weight loss. The precuneus is associated with the fronto-parietal network of theory of mind and mental representations of the self (30, 31), therefore making the changes similar to medial PFC. Precuneus and posterior cingulate have been shown in other studies to be associated with the salience and relevance of stimuli, independent of valence (32, 33). The medial PFC and precuneus may be working together to facilitate both increased valuation and salience of food-related cues in the behavioral diet group of participants.
Results did not support our hypothesis that participants would exhibit differential significant changes in reward-processing regions of the brain for diet participants or for surgical weight loss participants in hungry or fed states. This is consistent with Murdaugh and colleagues (15) who did not find changes in traditional reward brain regions in dieting participants. However, this is contrary to other findings in Roux-en-Y surgical patients, who demonstrated reduced activation in striatum (18). However, their patients may have experienced greater levels of hunger and higher food motivation, as they were in a fasted state of 12 hours, whereas we only requested patients to fast for 4 hours to reflect a more typical, ecologically valid eating schedule. If we had scanned participants after a longer fasted state or during delivery of a rewarding food stimulus, we may have observed reduced brain activation in reward regions. We did not observe brain activation changes in any reward or self-control regions, which is similar to Ochner et al (17), who reported no brain activation changes in reward or self-control regions after weight loss when patients were in a fed state.
Findings post-meal indicated increases in bilateral temporal cortex in bariatric participants compared to behavioral diet participants. Activations in middle temporal cortex are commonly reported in studies of food motivation and are associated with higher level perception including visual and semantic processing, and semantic memory (34, 35). Rosenbaum and colleagues (14) reported increases in middle temporal cortex in patients who underwent an inpatient liquid diet weight loss program. Increases in temporal cortex have also been reported in studies using positron emission tomography (PET) following food deprivation (36). It is possible that food cues evoke more semantic processing for those who have undergone a more drastic weight loss procedure (such as a surgery or an inpatient liquid diet) but further research is needed.
This is the first study of brain changes associated with two different methods of weight loss. Using two successful weight loss strategies, a behavioral weight loss intervention and a laparoscopic banding surgical intervention, we demonstrated that the functional brain changes observed may not be due to decreased body mass alone, but appear to be associated with the process by which weight loss is achieved. One of the major strengths of the study is that the participants in two different weight loss interventions were matched on demographics and on the percent of weight lost during the 12 week period. Though we found evidence of neural change in areas associated with food motivation and reward after weight loss, our sample size was relatively small, and we are unable to fully dissect the mechanism of this change. One limitation is that participants were not randomized to treatment group. Another limitation is the lack of a control group, which should be included in future work. Although the standardized meals differed in that bariatric participants received a wrap instead of the bread eaten by diet participants, because the groups were matched on BMI, the percentage of daily caloric needs was consistent across groups. In addition, we found that hunger ratings in both the hungry and fed states were not significantly different. Diet and bariatric groups did not report different hunger levels before or after eating the provided meal. We did observe differences in the hunger ratings in the premeal scan based on the order of scans, such that participants who were assigned to the premeal scan first reported greater hunger than those who had the premeal scan second. This effect, however, was minimized due to the equal division of scan order across the diet and bariatric groups.
There were also some differences in baseline characteristics between the groups. Some bariatric patients had well-controlled diabetes whereas none of the dieters had a diabetes diagnosis. Although dieters included in the study reported that they had not lost weight in the six months prior to intervention, bariatric patients frequently dieted prior to surgery. Finally, some of the bariatric group used anti-depressant medication. It should be noted that the aforementioned differences between the groups are those of which we are aware. Individuals who seek out and submit to an obesity intervention like laparoscopic banding surgery may have a longer history with weight problems and may possess more diverse psychological characteristics than those enrolling in a dieting weight loss intervention. However, the matching on demographic characteristics and percent of weight lost during the 12-week intervention helped control for some of the potential differences. Longitudinal research that includes matched obese controls and measures of behavior and hormonal change may better elucidate the mechanisms associated with brain changes following gastric banding and behavioral weight loss
This fMRI study is the first to examine the longitudinal effects of diet versus surgical weight loss on brain function. It provides evidence not only that brain responses are altered in response to weight loss, but that the brain responses might be specific to the method of weight loss. Results suggest that weight loss differentially changes brain functioning, specifically in areas known to be related to food motivation, the experience of hunger, and other aspects of self-referent processing. Findings have potential clinical implications, including using obesity interventions to target specific brain activation changes. Some experts have called for the development of “knifeless” pharmacological and/or behavioral treatments for the prevention and treatment of obesity (37). Ultimately, this knowledge may be used to improve the effectiveness of interventions for health behavior change.
Figure 1.
fMRI Cognitive activation paradigm (block design) of visual stimuli: food, animals, and blurred baseline images.
Figure 3.
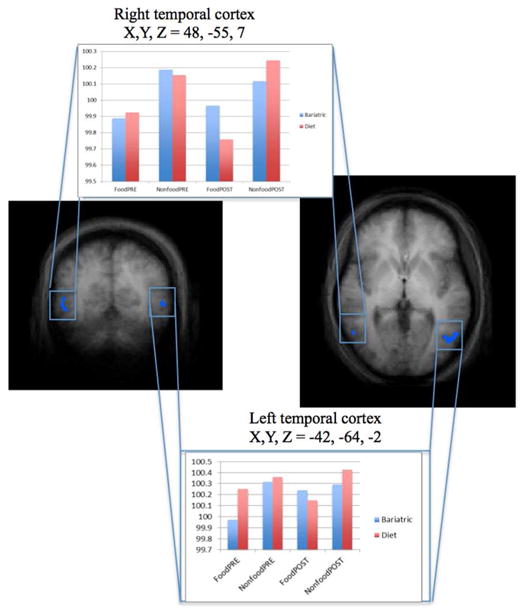
Postmeal, the bariatric group showed significantly greater change to food versus nonfood images in bilateral temporal cortex compared to the diet group.
What is already known about this subject:
Functional magnetic resonance imaging (fMRI) studies have shown that the brains of obese and healthy weight individuals differ in their responses to visual food cues.
Research has shown that obese patients exhibit increased activation in areas related to food motivation and decreased activation in regions associated with inhibition and cognitive control in comparison to healthy weight controls in response to visual food cues.
Findings suggest that higher neural activation in regions associated with valuation associated with behavioral compared to surgical weight loss.
What this study adds:
Information regarding brain activation changes associated with successful weight loss in dieters and bariatric patients in both hungry and fed states.
When hungry, behavioral dieters showed increased responses to food cues in medial PFC when compared to bariatric patients.
This is the first study to show that different methods of weight loss are associated with unique changes in brain function from pre to post-intervention.
Acknowledgments
This work was supported in part by a Pilot Studies Grant to Amanda Bruce from Frontiers: The Heartland Institute for Clinical and Translational Research (CTSA UL1TR000001 grant to University of Kansas Medical Center), the University of Missouri Research Board to Jared Bruce, and NIH R01DK080090 to Cary Savage. Dietary meals were provided by Health Management Resources, Boston, MA. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or any individual institute. All authors were involved in writing the paper and had final approval of the submitted and published versions.
Abbreviations
- fMRI
functional magnetic resonance imaging
- BMI
body mass index
- OFC
orbitofrontal cortex
- PFC
prefrontal cortex
- MPFC
medial prefrontal cortex
- ACC
anterior cingulate cortex
- ROI
region of interest
Footnotes
Conflicts of Interest: I hereby claim that my research staff and I have no significant financial interests or any other conflicts of interest as specified in the Public Health Service (PHS) conflict of interest regulations (42 CFR Part 50 Subpart F, 45 C.F.R. Part 94).
References
- 1.Lalonde L, Gray-Donald K, Lowensteyn I, Marchand S, Dorais M, Michaels G, et al. Comparing the benefits of diet and exercise in the treatment of dyslipidemia. Prev Med. 2002;35:16–24. doi: 10.1006/pmed.2002.1052. [DOI] [PubMed] [Google Scholar]
- 2.Flechtner-Mors M, Ditschuneit HH, Johnson TD, Suchard MA, Adler G. Metabolic and weight loss effects of long-term dietary intervention in obese patients: four-year results. Obes Res. 2000;8:399–402. doi: 10.1038/oby.2000.48. [DOI] [PubMed] [Google Scholar]
- 3.Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755–1767. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 4.O'Brien PE, Dixon JB, Laurie C, Skinner S, Proietto J, McNeil J, et al. Treatment of mild to moderate obesity with laparoscopic adjustable gastric banding or an intensive medical program: a randomized trial. Ann Intern Med. 2006;144:625–633. doi: 10.7326/0003-4819-144-9-200605020-00005. [DOI] [PubMed] [Google Scholar]
- 5.O'Brien PE, Dixon JB. Lap-band: outcomes and results. J Laparoendosc Adv Surg Tech A. 2003;13:265–270. doi: 10.1089/109264203322333593. [DOI] [PubMed] [Google Scholar]
- 6.Chapman AE, Kiroff G, Game P, Foster B, O'Brien P, Ham J, et al. Laparoscopic adjustable gastric banding in the treatment of obesity: a systematic literature review. Surgery. 2004;135:326–351. doi: 10.1016/S0039-6060(03)00392-1. [DOI] [PubMed] [Google Scholar]
- 7.Chau WY, Schmidt HJ, Kouli W, Davis D, Wasielewski A, Ballantyne GH. Patient characteristics impacting excess weight loss following laparoscopic adjustable gastric banding. Obes Surg. 2005;15:346–350. doi: 10.1381/0960892053576811. [DOI] [PubMed] [Google Scholar]
- 8.Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–1737. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 9.Ponce J, Haynes B, Paynter S, Fromm R, Lindsey B, Shafer A, et al. Effect of Lap-Band-induced weight loss on type 2 diabetes mellitus and hypertension. Obes Surg. 2004;14:1335–1342. doi: 10.1381/0960892042583932. [DOI] [PubMed] [Google Scholar]
- 10.Carnell S, Gibson C, Benson L, Ochner CN, Geliebter A. Neuroimaging and obesity: current knowledge and future directions. Obes Rev. 13:43–56. doi: 10.1111/j.1467-789X.2011.00927.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCaffery JM, Haley AP, Sweet LH, Phelan S, Raynor HA, Del Parigi A, et al. Differential functional magnetic resonance imaging response to food pictures in successful weight-loss maintainers relative to normal-weight and obese controls. Am J Clin Nutr. 2009;90:928–934. doi: 10.3945/ajcn.2009.27924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Le DS, Pannacciulli N, Chen K, Del Parigi A, Salbe AD, Reiman EM, et al. Less activation of the left dorsolateral prefrontal cortex in response to a meal: a feature of obesity. Am J Clin Nutr. 2006;84:725–731. doi: 10.1093/ajcn/84.4.725. [DOI] [PubMed] [Google Scholar]
- 13.Le DS, Pannacciulli N, Chen K, Salbe AD, Del Parigi A, Hill JO, et al. Less activation in the left dorsolateral prefrontal cortex in the reanalysis of the response to a meal in obese than in lean women and its association with successful weight loss. Am J Clin Nutr. 2007;86:573–579. doi: 10.1093/ajcn/86.3.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosenbaum M, Sy M, Pavlovich K, Leibel RL, Hirsch J. Leptin reverses weight loss-induced changes in regional neural activity responses to visual food stimuli. J Clin Invest. 2008;118:2583–2591. doi: 10.1172/JCI35055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murdaugh DL, Cox JE, Cook EW, 3rd, Wesller RE. fMRI reactivity to high-calorie food pictures predicts short- and long-term outcome in a weight-loss program. Neuroimage. 59:2709–2721. doi: 10.1016/j.neuroimage.2011.10.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bruce JM, Hancock L, Bruce A, Lepping RJ, Martin L, Lundgren JD, et al. Changes in brain activation to food pictures after adjustable gastric banding. Surg Obes Relat Dis. 2012;8:602–608. doi: 10.1016/j.soard.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 17.Ochner CN, Kwok Y, Conceicao E, Pantazatos SP, Puma LM, Carnell S, et al. Selective reduction in neural responses to high calorie foods following gastric bypass surgery. Ann Surg. 2011;253:502–507. doi: 10.1097/SLA.0b013e318203a289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ochner CN, Laferrere B, Afifi L, Atalayer D, Geliebter A, Teixeira J. Neural responsivity to food cues in fasted and fed states pre and post gastric bypass surgery. Neurosci Res. 2012;74:138–143. doi: 10.1016/j.neures.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bruce AS, Holsen LM, Chambers RJ, Martin LE, Brooks WM, Zarcone JR, et al. Obese children show hyperactivation to food pictures in brain networks linked to motivation, reward and cognitive control. Int J Obes (Lond) 2010;34:1494–1500. doi: 10.1038/ijo.2010.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martin LE, Holsen LM, Chambers RJ, Bruce AS, Brooks WM, Zarcone JR, et al. Neural mechanisms associated with food motivation in obese and healthy weight adults. Obesity (Silver Spring) 2009;18:254–260. doi: 10.1038/oby.2009.220. [DOI] [PubMed] [Google Scholar]
- 21.Lang PJ, Bradley MM, Cuthbert BN. International Affective Picture System (IAPS): Technical manual and affective ratings. 1997 [Google Scholar]
- 22.Martin LE, Holsen LM, Chambers RJ, Bruce AS, Brooks WM, Zarcone JR, et al. Neural mechanisms associated with food motivation in obese and healthy weight adults. Obesity (Silver Spring) 18:254–260. doi: 10.1038/oby.2009.220. [DOI] [PubMed] [Google Scholar]
- 23.Holsen LM, Zarcone JR, Thompson TI, Brooks WM, Anderson MF, Ahluwalia JS, et al. Neural mechanisms underlying food motivation in children and adolescents. Neuroimage. 2005;27:669–676. doi: 10.1016/j.neuroimage.2005.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Talairach JTP. Co-planar stereotaxic atlas of the human brain. Thieme medical publishers; New York: 1988. [Google Scholar]
- 25.Friston KJ, Frith CD, Frackowiak RS, Turner R. Characterizing dynamic brain responses with fMRI: a multivariate approach. Neuroimage. 1995;2:166–172. doi: 10.1006/nimg.1995.1019. [DOI] [PubMed] [Google Scholar]
- 26.Lieberman MD, Cunningham WA. Type I and Type II error concerns in fMRI research: re-balancing the scale. Soc Cogn Affect Neurosci. 2009;4:423–428. doi: 10.1093/scan/nsp052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goebel R, Espozito F, Formisano ER. Analysis of functional image analysis contest (FIAC) data with Brain Voyager QX: from single-subject ot cortically aligned group general linear model analysis and self-organizing group independent component analysis. Human Brain Mapping. 2006;27:392–401. doi: 10.1002/hbm.20249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stice E, Burger K, Yokum S. Caloric deprivation increases responsivity of attention and reward brain regions to intake, anticipated intake, and images of palatable foods. Neuroimage. 67:322–330. doi: 10.1016/j.neuroimage.2012.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hare TA, Camerer CF, Rangel A. Self-Control in Decision-Making Involves Modulation of the vmPFC Valuation System. Science. 2009;324:646–648. doi: 10.1126/science.1168450. [DOI] [PubMed] [Google Scholar]
- 30.Lamm C, Decety J, Singer T. Meta-analytic evidence for common and distinct neural networks associated with directly experienced pain and empathy for pain. Neuroimage. 2011;54:2492–2502. doi: 10.1016/j.neuroimage.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 31.Legrand D, Ruby P. What is self-specific? Theoretical investigation and critical review of neuroimaging results. Psychol Rev. 2009;116:252–282. doi: 10.1037/a0014172. [DOI] [PubMed] [Google Scholar]
- 32.Maddock RJ. The retrosplenial cortex and emotion: new insights from functional neuroimaging of the human brain. Trends Neurosci. 1999;22:310–316. doi: 10.1016/s0166-2236(98)01374-5. [DOI] [PubMed] [Google Scholar]
- 33.Small DM, Zatorre RJ, Dagher A, Evans AC, Jones-Gotman M. Changes in brain activity related to eating chocolate: from pleasure to aversion. Brain. 2001;124:1720–1733. doi: 10.1093/brain/124.9.1720. [DOI] [PubMed] [Google Scholar]
- 34.DelParigi A, Pannacciulli N, Le DN, Tataranni PA. In pursuit of neural risk factors for weight gain in humans. Neurobiology of Aging. 2005;26(Supplement):50–55. doi: 10.1016/j.neurobiolaging.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 35.Binder JR, Desai RH, Graves WW, Conant LL. Where is the semantic system? A critical review and meta-analysis of 120 functional neuroimaging studies. Cereb Cortex. 2009;19:2767–2796. doi: 10.1093/cercor/bhp055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang GJ, Volkow ND, Telang F, Jayne M, Ma J, Rao M, et al. Exposure to appetitive food stimuli markedly activates the human brain. Neuroimage. 2004;21:1790–1797. doi: 10.1016/j.neuroimage.2003.11.026. [DOI] [PubMed] [Google Scholar]
- 37.Shin AC, Berthoud HR. Food reward functions as affected by obesity and bariatric surgery. Int J Obes (Lond) 2011;35(Suppl 3):S40–44. doi: 10.1038/ijo.2011.147. [DOI] [PMC free article] [PubMed] [Google Scholar]


