Abstract
A previous randomized controlled trial (RCT) by Schiffman et al. (2007)15 compared four treatments strategies for temporomandibular joint (TMJ) disc displacement without reduction with limited mouth opening (closed lock). In this parallel group RCT, 106 patients with magnetic resonance imaging (MRI)-confirmed TMJ closed lock were randomized between medical management, non-surgical rehabilitation, arthroscopic surgery, and arthroplasty. Surgical groups also received rehabilitation post-surgically. The current paper reassesses the effectiveness of these four treatment strategies using outcome measures recommended by the International Association of Oral and Maxillofacial Surgeons (IAOMS). Clinical assessments at baseline and at follow-up (3, 6, 12, 18, 24, and 60 months) included intensity and frequency of TMJ pain, mandibular range of motion, TMJ sounds, and impairment of chewing. TMJ MRIs were performed at baseline and 24 months, and TMJ tomograms at baseline, 24 and 60 months. Most IAOMS recommended outcome measures improved significantly over time (P ≤ 0.0003). There was no difference between treatment strategies relative to any treatment outcome at any follow-up (P ≥ 0.16). Patient self-assessment of treatment success correlated with their ability to eat, with pain-free opening ≥35 mm, and with reduced pain intensity. Given no difference between treatment strategies, non-surgical treatment should be employed for TMJ closed lock before considering surgery.
Keywords: temporomandibular joint, closed lock, surgery, randomized effectiveness study, treatment success criteria
Dentists routinely provide patients with initial medical management for their temporomandibular disorders (TMD). When patients are refractory to medical management, triaging them for further care is challenging due to the lack of evidence-based guidelines. This is particularly true for patients with temporomandibular joint (TMJ) disc displacement without reduction and with limited opening (i.e., closed lock), a chronic, persistent disorder1–3 that can cause significant jaw pain, limited jaw movement, and functional impairment, affecting among other capacities, the ability to eat. This condition has been postulated to lead to TMJ degenerative joint disease2,4–6 (DJD).
Although case series involving surgical treatment of closed lock7–9 suggest that surgery could have better outcomes than non-surgical rehabilitation therapy, clinical trials3 to confirm such claims are limited. Reviews10–13 of the literature, including one meta-analysis, have not demonstrated any differences between physical therapy, arthrocentesis, arthroscopic surgery, and disc repair/repositioning surgery relative to outcomes such as maximum mouth opening, jaw pain, and jaw function. A more recent randomized clinical trial (RCT) comparing arthroscopy to open-joint surgery14 showed that both treatments were effective for symptomatic closed lock patients. Our 5-year RCT for patients with closed lock15 demonstrated that medical management and non-surgical rehabilitation improved pain and dysfunction as effectively as either arthroscopic surgery with rehabilitation, or arthroplasty (open joint surgery) with rehabilitation. Finally, the conclusion of the 2011 Cochrane Collaboration review on arthroscopy16 is that arthroscopy is less effective than open surgery for pain reduction at 12 months postoperatively. Arthroscopy is associated with greater improvement than arthrocentesis for maximum mouth opening at 12 months, and both arthroscopy and non-surgical treatments reduce pain at 6 months. This review states also that the study by Schiffman et al.15 is one of the best RCTs assessing the treatment for TMJ closed lock.
The current paper complements the 2007 report by Schiffman et al.15 in which treatment success was defined by two primary outcome study measures: the Symptom Severity Index (SSI)17–19 to assess TMJ pain, and the Craniomandibular Index (CMI)20,21 to assess jaw dysfunction. For this study, we used the International Association of Oral and Maxillofacial Surgeons (IAOMS) recommended criteria for success22 to assess the relative effectiveness of medical management, rehabilitation, arthroscopic surgery, and arthroplasty. This will allow for comparisons of the study outcomes with those of other studies using IAOMS recommended outcomes. In addition, this report compares these treatment strategies for a closed lock disorder relative to patient satisfaction, treatment costs, and selected radio-graphic outcomes, including TMJ disc status observed at 24 months and TMJ hard tissue status observed at 60 months post-treatment.
Patients and methods
Study design and study population
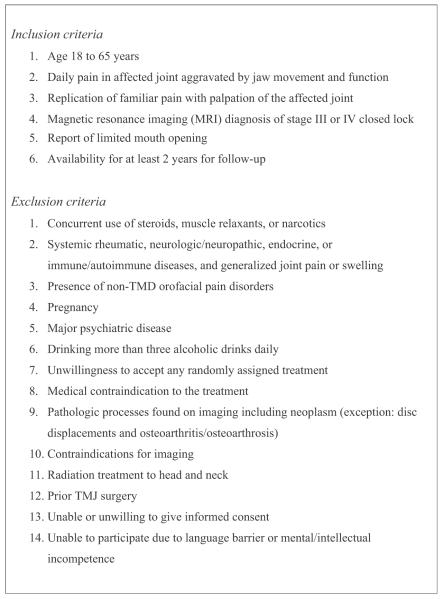
This parallel group RCT was conducted from June 1992 to June 2004. The sources of the study subjects, informed consent procedures, institutional review board (IRB) approval for conducting the study, the potential limitations of such a scientific inquiry, and the CONSORT checklist and flow-chart have been reported previously.15 We also received approval for this ongoing data analysis. The authors have read the Declaration of Helsinki and followed the guidelines for this investigation. Inclusion and exclusion criteria are summarized in Fig. 1. The diagnosis of TMJ disc displacement without reduction (i.e., closed lock)9 was confirmed using TMJ magnetic resonance imaging (MRI). Other inclusion criteria included daily joint pain (arthralgia) affected by jaw function, replication of joint pain with palpation, and limited mouth opening. A concurrent diagnosis of masticatory myofascial pain was also allowed for these study patients.
Fig. 1.
Inclusion and exclusion criteria.
Randomization and treatments
This RCT assessed four treatment strategies with each strategy labelled in terms of its initial treatment modality: (1) medical management, (2) rehabilitation, (3) arthroscopy with rehabilitation, and (4) arthroplasty with rehabilitation. These treatment strategies were designed to represent treatment choices occurring in clinical practice. The initial treatment randomization was concealed from patients and care provider(s) until the enrollment procedure was completed. The randomized allocation employed two strata: ‘non-chronic’ disorder (duration of limited mouth opening <6 months) and ‘chronic’ disorder (duration of limited mouth opening <6 months). This ensured that each group would be balanced with regard to chronicity of limited mouth opening.
The treatment strategy randomization also employed unequal blocks to increase the number of patients assigned to ‘medical management’ because we anticipated a priori that such requests would be greatest in this group. By design, we intended to honour requests by patients for a change in treatment just as occurs in actual clinical practice.
The four treatment strategies are described as follows and are described in more detail in the appendix of our prior manuscript.15 ‘Medical management’ included education about the patient’s condition, with optimistic counselling, a self-help programme,23 and a 6-day regimen of oral methylprednisolone followed by prescription non-steroidal anti-inflammatory drugs (NSAIDS) for up to 6 weeks. Although patient preference for specific NSAIDs was honoured, ibuprofen 800 mg three times daily was used most often. Initially, concurrent short-term use of a muscle relaxant was used as needed, and the medication was typically cyclobenzaprine, 10 mg at bedtime. After this course of medication management, over-the-counter analgesics were used as needed. All medications, including over-the-counter analgesics, were monitored at monthly appointments by one orofacial pain dentist (ELS), with the goal of minimizing unnecessary use of medications. Medical management was also provided to patients in the other three treatment groups.
The rehabilitation24 team included an orofacial pain dentist, a physical therapist, and a health psychologist. They implemented medical management as described above, plus an intraoral orthotic, physical therapy, and cognitive-behavioural therapy. Patients were randomly assigned to one of the two treating orofacial pain dentists (ELS, JRF) who inserted and monitored the use of an orthotic at monthly appointments for 6 months, and then as needed. Patients who continued to use an orthotic after the first 6 months were seen at least one time per year to monitor its effects. The orthotic typically had a flat plane design (i.e., stabilization splint). A registered physical therapist performed outcome-based physical therapy designed to decrease pain, increase function for eating and talking, and increase pain-free active range of motion. Mobilization of the jaw and modalities were used as indicated, combined with a home exercise programme. When active physical therapy was completed, the recorded improvements in pain and function were monitored monthly for 6 months, and then as needed. A licensed clinical psychologist implemented and monitored a cognitive-behavioural programme usually consisting of self-help and oral habit reversal techniques. Patients were typically seen three times by the clinical psychologist.
Arthroscopy consisted of a standardized procedure described by Moses and Poker25 that was performed by one of two participating oral surgeons (JQS or RBT) who were randomly assigned. Following general anaesthesia, the superior joint space was injected with bupivacaine and infused with heparinized lactated Ringer’s solution. After the needle was removed, a cannula was inserted at the same entry site, and a sharp trocar was used to puncture the joint capsule. A blunt trocar was then employed to enter the superior joint space and to lyse intracapsular adhesions. Debris and blood were cleared with Ringer’s solution using a secondary needle, as needed, as an outflow port for the irrigation. Beta-methasone was then injected into the capsule, and the mandible was manually moved to maximize the patient’s range of motion.
Arthroplasty was an open joint surgery that was performed under general anaesthesia by Dr. Clyde Wilkes in accordance with his published protocol.9 Briefly, the goal was to do a disc repositioning procedure (discoplasty) when feasible. However, if the surgeon determined that a discoplasty was not indicated, a disc removal procedure (i.e., discectomy) was performed with joint debridement and hard tissue recontouring as needed. Intra-articular steroids were not used with any of the arthroplasties.
Patients were seen at least once per month over the first 6 months by the treating surgeons, and then as needed. All surgical patients saw the same physical therapists and the psychologist who treated the rehabilitation group. In addition, if an orthotic was judged to be indicated, then this was inserted postoperatively and monitored by one orofacial pain dentist (ELS), as described above.
Follow-up data collections
Clinical examinations and questionnaires were completed at baseline and at the 3-, 6-, 12-, 18-, 24-, and 60-month follow-ups. One examiner (PAL), who was blinded to treatment assignments, performed all clinical examinations. When patients presented for their clinical evaluation, a research coordinator administered questionnaires and reminded them not to discuss treatment with the examiner. Tape was placed over both pre-auricular areas to conceal the presence or absence of a surgical scar, and patients were paid $200 at each follow-up visit.
Radiographic data collections were based on imaging studies performed at Hennepin County Medical Centre, Minneapolis. Study patients received TMJ MRI at baseline and at their 24-month follow-up. TMJ tomogram studies were performed at baseline, 24 months and 60 months. A board-certified radiologist (QNA) did all imaging interpretations.
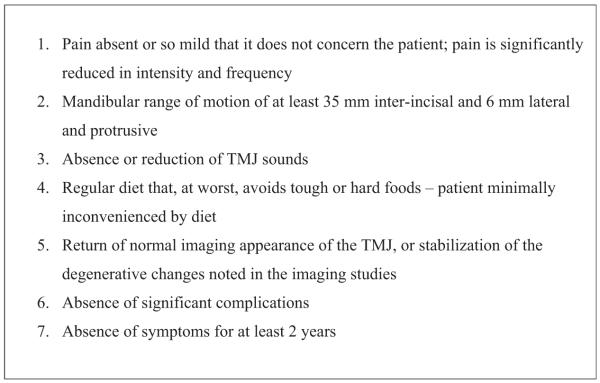
Fig. 2 lists the IAOMS recommended criteria for evaluating TMJ surgical treatment outcomes. Since the IAOMS did not provide operational definitions for these outcome measures, the measurement methods used in this data collection are explained below under ‘Data collection specifications’. This report also takes into consideration both jaw joint pain and jaw muscle pain. Two other important outcome measures defined under ‘Data collection specifications’ are patient satisfaction with their treatment, and treatment cost.
Fig. 2.
Treatment outcome measures recommended by the International Association of Oral and Maxillofacial Surgeons for assessment of treatment success.
Data collection specifications
Pain outcomes
The IAOMS recommended pain intensity and frequency measures are subscales of the reliable and valid SSI.17–19 These data were available for analysis since the SSI was one of the primary outcome measures used in the initial report15 of this RCT. Given that IAOMS recommendations were for postoperative assessment of TMJ surgery, it is assumed that their recommended pain intensity and frequency measures were intended for assessment of pain in the TMJ. TMJ pain intensity was measured based on the question, “How intense is your usual level of jaw joint pain in the past month?” The response was assessed as a categorical measure on a 5-point scale: (1) no pain, (2) mild pain, (3) moderate pain, (4) severe pain, and (5) most pain imaginable. TMJ pain frequency was measured by six frequency categories including: (1) never, (2) once monthly, (3) once weekly, (4) once daily, (5) once hourly, and (6) constantly. Since muscle pain is also a frequent problem associated with TMJ closed lock, parallel questions were queried regarding jaw muscle pain intensity and frequency.
Jaw range of motion and TMJ sounds
The IAOMS recommended measures for jaw range of motion and TMJ sounds are components of the second primary outcome measure used in the initial report15 of this RCT, i.e., the CMI.20,21 This is a reliable and valid instrument designed to globally assess TMD signs including TMJ pain, dysfunction, and joint sounds. Since the CMI operationalizes measurement of jaw range of motion (ROM) on a continuous scale (mm), our data were readily reanalyzed according to IAOMS recommendations. Maximum unassisted opening without pain was dichotomized as: no limitation (≥35 mm) and limitation (<35 mm). Lateral excursive movements and protrusive movements were categorized as: no limitation (≥6 mm) and limitation (<6 mm). TMJ sounds were assessed based on three repetitions of each jaw movement including opening, closing, right and left lateral excursion, and protrusion of the jaw. Joint noise response categories were measured separately for joint clicks and crepitus. Disc clicks were recorded in four categories: no click, or clicking occurring during 1, 2, or all 3 repetitions for each jaw movement. Crepitus sounds were recorded as none, fine crepitus, or coarse crepitus.
Mandibular function impairment
Mandibular function impairment was assessed using the question, “In general, when chewing foods, what types of foods cause pain in your jaw and/or jaw joint?” The response options included: (1) no pain when eating any foods, (2) pain only when eating chewy (resistant) foods, (3) pain when eating most foods, (4) pain even when eating soft foods, and (5) pain when eating anything. Per IAOMS recommendations requiring minimal inconvenience associated with eating, the ability to chew was dichotomized as 1 or 2 = acceptable, versus 3–5 = not acceptable.
Radiographic imaging assessments
Tomograms were scored according to four specified assessments evaluating changes in either shape or bone density that affected either the glenoid fossa or the condyle. Each item was scored as: 0 = normal; 1 = mild change; 2 = moderate change; 3 = severe change. Scores of 1 and 2 were considered as various stages of remodelling (i.e., sclerosis and/or flattening) and a score of 3 was considered frank DJD26 (i.e., osteophytes, subcortical cysts, generalized sclerosis, and surface erosion). The overall tomogram score for a given joint was based on the greatest score observed: 0 indicating that no score among the four assessments was greater than 0; 1 representing a worst score no greater than 2; and 2 representing a worst score of 3, i.e., DJD. MRIs, performed at baseline and at 24 months, were scored regarding disc position with 1 = normal, 2 = a reducing disc, and 3 = a non-reducing disc. The radiologist’s intra-rater reliability for the interpretation of the TMJ tomograms and MRIs was assessed at baseline, mid-study, and at the study end, resulting in kappa values ranging from 0.88 to 0.93. The radiologist had no contact with patients and was blind to their treatment group assignment.
Satisfaction with the treatment
The Group Health Association of America (GHAA) Consumer Satisfaction Survey was employed to assess the patients’ satisfaction with their treatment outcome. Self-reported treatment outcomes included: (1) poor, (2) fair, (3) good, (4) very good, and (5) excellent. A finding of treatment success required a self-report of 4 or 5; scores of 1–3 were considered as less-than-optimum in this study. This survey was administered only at the 60-month follow-up visit and can be obtained from GHAA (Department of Research and Analysis, Group Health Association of America, Inc., 1129 Twentieth St. NW, Suite 600, Washington, DC 20036, USA).
Cost of treatment
The cost of treatment was determined after the 60-month follow-up by record reviews for all patients, including costs of orthotics, physical therapy modalities, and cognitive-behaviour treatments. The cost of the TMJ MRIs and tomograms were not included in the cost estimates since they were the same for all treatment strategies. Additional costs pertinent to surgical groups were the cost of unilateral or bilateral TMJ surgeries. Applicable surgery costs were also accounted to the medical management and comprehensive rehabilitation treatment strategies for any patient from one of these groups who opted for surgery at some time after the 3-month follow-up visit.
Statistical analyses
The analysis of data for this study was specified a priori as ‘intention-to-treat’, meaning that, for the primary analysis, all patient data would be analyzed according to each patient’s randomized initial treatment strategy assignment. Consequently, patients who requested a change in treatment modality (after their 3-month follow-up) were not reassigned to a different treatment for the analysis. Likewise, intention-to-treat studies, often referred to as effectiveness studies, commonly include in the final analysis the results of dropouts, i.e., study participants who refuse their treatment and drop out of the study after learning of their randomized treatment allocation. The primary data analysis for this study includes the dropouts, while a secondary data analysis was also performed that was limited to those patients who received a study treatment. P-values were not adjusted for multiple comparisons.
Each IAOMS recommended outcome was measured at the beginning of the study and tested for differences between groups at baseline using Fisher’s exact test, as shown in Table 1. Treatment success based on the IAOMS criteria shown in Fig. 2 was assessed for each patient’s data at each follow-up, with ‘success = yes’ if all conditions were satisfied and ‘success = no’ otherwise. Table 2 shows rates of success for each treatment strategy at each follow-up time, and Fisher’s exact test was used to test differences between these rates (see P-value for between-group differences).
Table 1.
International Association of Oral and Maxillofacial Surgeons (IAOMS) recommended outcome variables by group at baseline.
| Treatment group | Vertical range of motiona |
Lateral and protrusive movementb |
Impaired mandibular functionc |
Excessive jaw muscle pain frequencyd |
Excessive jaw muscle pain intensitye |
Excessive joint pain frequencyf |
Excessive joint pain intensityg |
Tomogram score (worst side)h |
Joint clicking |
Joint crepitus |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <35 | ≥35 | <6 | ≥6 | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | 0 | 1 | 2 | Yes | No | Yes | No | |
| Medical management | 27 | 2 | 13 | 16 | 15 | 11 | 25 | 4 | 21 | 8 | 28 | 1 | 24 | 5 | 2 | 26 | 0 | 13 | 16 | 3 | 26 |
| Non-surgical rehabilitation | 22 | 2 | 10 | 14 | 9 | 7 | 21 | 2 | 16 | 7 | 23 | 0 | 20 | 3 | 2 | 22 | 0 | 9 | 16 | 1 | 24 |
| Arthroscopic surgery | 21 | 4 | 8 | 17 | 12 | 10 | 25 | 1 | 22 | 4 | 26 | 0 | 25 | 1 | 1 | 24 | 1 | 8 | 18 | 7 | 19 |
| Arthroplasty (open joint) | 23 | 3 | 7 | 19 | 12 | 8 | 24 | 2 | 22 | 3 | 25 | 1 | 24 | 1 | 2 | 23 | 1 | 9 | 17 | 4 | 22 |
| Total subjects | 104 | 104 | 84 | 104 | 103 | 104 | 103 | 104 | 106 | 106 | |||||||||||
|
P-value for between-group differencei |
P = 0.76 | P = 0.51 | P = 0.99 | P = 0.69 | P = 0.32 | P = 1.0 | P = 0.29 | P = 0.95 | P = 0.75 | P = 0.123 | |||||||||||
Vertical range of motion: <35 = limitation; ≥35 = no limitation.
Lateral and protrusive movement: <6 = limitation; ≥6 = no limitation.
Impaired mandibular function: yes = impaired chewing; no = no impairment or only when chewing the most resistant foods.
Excessive jaw muscle pain frequency: yes = excessive frequency; no = never or at most once monthly.
Excessive jaw muscle pain intensity: yes = excessive intensity; no = no pain or at most mild pain.
Excessive joint pain frequency: yes = excessive frequency; no = never or at most once monthly.
Excessive joint pain intensity: yes = excessive intensity; no = no pain or at most mild pain.
Tomogram score (worst side): 0 = normal osseous status; 1 = mild to moderate osseous changes; 2 = severe changes, i.e., osteoarthritis.
Using Fisher’s exact test.
Table 2.
Rates of treatment success based on International Association of Oral and Maxillofacial Surgeons (IAOMS) criteria by group and by follow-up.
| Treatment group Successa |
3-month follow-up |
6-month follow-up |
12-month follow-up |
18-month follow-up |
24-month follow-up |
60-month follow-up |
60-month self-report of treatment success |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | |
| Medical management | 28 | 1 | 26 | 1 | 27 | 2 | 23 | 2 | 24 | 2 | 25 | 2 | 7 | 18 |
| Non-surgical rehabilitation | 22 | 1 | 20 | 1 | 18 | 4 | 19 | 3 | 21 | 1 | 21 | 2 | 4 | 17 |
| Arthroscopic surgery | 22 | 1 | 22 | 0 | 21 | 2 | 21 | 0 | 22 | 0 | 24 | 1 | 5 | 16 |
| Arthroplasty (open joint) | 18 | 2 | 16 | 3 | 17 | 3 | 18 | 3 | 20 | 1 | 22 | 2 | 3 | 15 |
| Total subjects followed up | 95 | 89 | 94 | 89 | 91 | 99 | 85 | |||||||
| P-value for between-group differenceb | P = 0.81 | P = 0.16 | P = 0.56 | P = 0.31 | P = 0.84 | P = 0.91 | P = 0.84 | |||||||
| Overall success ratio (%) | 5/95 (5.3%) |
5/89 (5.6%) |
11/94 (11.7%) |
8/89 (9.0%) |
4/91 (4.4%) |
7/99 (7.1%) |
66/85 (77.6%) |
|||||||
Postoperative treatment success at 3, 6, 12, and 18 months took into account vertical opening, lateral and protrusive range of motion, mandibular function, jaw muscle pain frequency and intensity, joint pain frequency and intensity, and joint noises. Imaging was not repeated at these follow-ups. Treatment success at 24 months postoperatively took into account the clinical findings above as well as MRI and tomogram results. Treatment success at 60 months was based on the clinical findings plus the tomogram data. The 60-month self-report column (far right) represents the patient’s own appraisal of the treatment’s success: yes = a successful treatment outcome; no = a treatment failure based on any rating inferior to ‘very good’. The 99 participants examined at the 60-month follow-up included 90 patients who were treated in the study and nine participants who dropped out after randomization.
Using Fisher’s exact test.
Further investigation into what might constitute treatment success was focused on the concerns often expressed by TMD patients: their ability to eat, to open their mouth, and to have pain-free TMJs and jaw muscles. Therefore, the examination and questionnaire data collected at 60 months were used to explore limited success algorithms based just on these variables relative to their correlation with self-reported success at 60 months by the patients. These latter findings are summarized in the ‘Results’ section.
Finally, each individual IAOMS outcome measure was assessed for its improvement over the entire follow-up period, and the four treatment strategies were compared for the relative improvement associated with each of these measures (Table 3). This separate analysis for each treatment outcome measure was performed using a generalized estimating equations (GEE) procedure. All but one outcome was binary (yes, no), according to whether the outcome met the IAOMS criterion for success or not. For a given binary outcome (dependent variable), e.g., vertical range of motion, an observation (‘case’) was a person measured at a follow-up time. Thus in the GEE analysis, a person formed a cluster and the working correlation was autoregressive. The logit link was employed for these analyses.
Table 3.
Analyses of International Association of Oral and Maxillofacial Surgeons (IAOMS) recommended outcome variables by groups and by time effect.
| Effects | Vertical range of motion |
Lateral and protrusive range of motion |
Mandibular function (eating) |
Jaw muscle pain frequency |
Jaw muscle pain intensity |
Joint pain frequency |
Joint pain intensity |
Joint clicking |
Joint crepitus |
Tomogram score (worst score) |
|---|---|---|---|---|---|---|---|---|---|---|
|
P-value for group effecta |
P = 0.23 | P = 0.11 | P = 0.19 | P = 0.10 | P = 0.48 | P = 0.47 | P = 0.86 | P = 0.78 | P = 0.09 | P = 0.20 |
|
P-value for time effectb |
P < 0.0001 | P = 0.0003 | P < 0.0001 | P < 0.0001 | P < 0.0001 | P < 0.0001 | P < 0.0001 | P = 0.25 | P = 0.23 | P = 0.0004 |
GEE, generalized estimating equations.
From GEE analysis; a non-significant group effect (P > 0.05) indicates no difference between treatment groups.
From GEE analysis; the highly significant time effect is associated with improvement over time for outcome variables measuring mandibular range of motion, mandibular function (eating), jaw muscle pain frequency and intensity, and joint pain frequency and intensity. In contrast, joint clicking and crepitus were unchanged, and tomogram scores increased significantly over time (i.e., higher prevalence of osteoarthritis).
The exception to the description above was for the tomogram results, which were not binary but multinomial: 0 = normal osseous status; 1 = sclerosis/flattening (slight, mild, moderate); 2 = frank osteoarthrosis. The correlation structure for the tomogram results was specified as independent and the cumulative logit link was used. All such computations used the GENMOD procedure in the SAS system (version 9.1; SAS Institute Inc., Cary, NC, USA). The ‘group effect’ row in Table 3 shows P-values that represent the statistical probability of a difference between any of the treatment strategies. By convention, a P-value > 0.05 suggests that an observed treatment difference is not statistically significant and, therefore, likely due to chance. For each outcome variable, the P-values in the ‘time effect’ row indicate the statistical significance of the improvement in the outcome over time from its baseline level.
Results
One hundred and six subjects were randomly assigned to the four treatment strategy groups. These groups did not differ significantly (P ≥ 0.12) at baseline for any of the IAOMS recommended outcome measures (Table 1, n = 106). Ten of the subjects dropped out of the study after their treatment strategy was made known to them. The 96 patients who accepted their treatment assignment included 29 in medical management, 23 in rehabilitation, 23 in arthroscopy, and 21 in arthroplasty. Table 2 shows the success rates for each treatment strategy group, determined by using algorithms based on the IAOMS recommended criteria for success. The primary analysis for the 60-month follow-up in Table 2 shows 99 patients.
Consistent with intention-to-treat, we planned to re-examine all available subjects who were randomized. Ninety out of 96 treated patients were seen for this follow-up, as well as nine out of the 10 subjects who had dropped out. Relative success rates associated with each of the treatment strategies did not differ significantly at any of the follow-ups. This was true for the 3-month follow-up when all patients were still undergoing their initial treatment modalities (P = 0.81), and at all subsequent follow-ups (P ≥ 0.16). The secondary analysis comparing results among the 90 treated patients at the final (60-month) follow-up showed success ratios to be: 2/27 for medical management, 2/21 for non-surgical rehabilitation, 1/22 for arthroscopy, and 1/20 for arthroplasty. Thus, six of 90 treated patients (6.7%) experienced a successful outcome based on IAOMS criteria. There was no statistical difference between groups regarding these success rates (P = 0.95, Fisher’s exact test). There was also no difference in success rates between the n = 90 who received treatment (6.7% success) when compared to the n = 99 patients who included dropouts (7.1% success, Table 2).
The crossover rate was greatest among patients assigned to the medical management strategy, where 46% (13/28) underwent either rehabilitation (n = 12) or arthroscopic surgery (n = 1) after 3 months of care. Also, one rehabilitation patient had arthroplasty surgery after 3 months of care. Although patients assigned to either arthroscopic or arthroplastic surgery received post-surgical rehabilitation, two arthroscopy patients and one arthroplasty patient also requested and received repeat surgeries. Arthroscopy was performed on 32 joints. Arthroplasty was performed on 34 joints, including 23 discoplasties and 11 discectomies. Most surgical patients required an orthotic post-surgically; the only exceptions were two of the arthroscopy patients and five of the arthroplasty patients.
Given that Table 2 shows no statistical difference in success rates between treatments (all P-values ≥ 0.16), we combined the entire study sample to estimate overall success rates determined by using IAOMS success criteria. These success rates, shown in the last row of Table 2, ranged from a maximum of 11/94 (12%) patients at 12 months when no radiographic findings were included in the analysis, dropping to 4/91 (4%) at 24 months when MRI and tomogram criteria were added to the success algorithm, and increasing to 7/99 (7%) at 60 months when the final tomogram results were included in the analysis.
In contrast, Table 2 also shows that 66/85 (78%) patients reported at 60 months that they had experienced a ‘very good’ or ‘excellent’ outcome. The large discrepancy at 60 months between success rates based on patient judgement (78%) and on IAOMS criteria (7%) highlights the need for further study as to which IAOMS recommended criteria, measured at 60 months, best match the patients’ self-reported success. Unimpaired mandibular function was the most highly associated with patient-reported success (94% agreement), followed by pain-free maximum opening (85%), jaw muscle pain intensity (83%), excursive ROM (80%), and jaw joint pain intensity (74%). More moderate agreement between clinical outcome and self-report of success was observed for jaw muscle pain frequency (67% agreement) and osseous status per the tomograms (67%). Outcomes that were poor to marginal indicators for patient-reported success were jaw joint pain frequency (47% agreement), presence of joint clicks (41%), and presence of joint crepitus (14%).
Success rates corresponding to the concerns commonly expressed by closed lock patients were as follows: If the ability to eat most foods were the only measure for success, 86/99 (87%) had a successful outcome at 60 months. Adding to this the ability to open one’s mouth to 35 mm reduced the proportion of successful outcomes to 76/99 (77%). The success rate dropped to 53/99 (54%) when adding the requirement that the patient would also be relatively pain-free.
Considering the improvement over time analysis, Table 3 shows seven clinical outcomes with highly significant improvements over the follow-up period. The time effects showing statistically significant improvement include vertical opening, lateral and protrusive ROM, mandibular function, jaw muscle pain frequency and intensity, and joint pain frequency and intensity (all P ≥ 0.0003). Joint clicking and joint crepitus changed little over time (P = 0.25 and P = 0.23, respectively, Table 3). Treatment strategies did not differ for any of the outcomes (P ≥ 0.09; see group effect, Table 3).
One outcome in Table 3, the osseous changes scored from the tomograms, showed significant worsening over time (P = 0.0004). Table 4 is therefore added to describe the overall increase in DJD from two cases at baseline to 13 cases at 60 months. The number of new cases of DJD not present at baseline was four within the 23 patients of the arthroplasty group (17%). This rate of incident DJD was similar for the arthroscopy group in which 4/24 (17%) new cases occurred. By comparison, medical management had 2/27 (7%) new cases of DJD, and rehabilitation had 1/23 (4%). The 97 patients re-imaged at the 60-month follow-up (Table 4) included eight patients who had refused their treatment allocation and dropped out. In a secondary analysis limited to the 89 treated patients, the osseous outcome frequencies were: one normal, 75 mild to moderate remodelling, and 13 severe remodelling (DJD).
Table 4.
Tomogram-disclosed TMJ osseous changes over 5 years of follow-up.a
| Intervention | Baseline |
24 months |
60 monthsb |
||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 n (%) |
I n (%) |
IIc n (%) |
0 n (%) |
I n (%) |
II n (%) |
0 n (%) |
I n (%) |
IIc n (%) |
|
| Medical management (%) | 2 (7) | 26 (93) | 0 (0) | 1 (4) | 24 (96) | 0 (0) | 0 (0) | 25 (93) | 2 (7) |
| Non-surgical rehabilitation (%) | 1 (4) | 22 (96) | 0 (0) | 0 (0) | 16 (84) | 3 (16) | 0 (0) | 22 (96) | 1 (4) |
| Arthroscopic surgery (%) | 1 (4) | 24 (92) | 1 (4) | 0 (0) | 18 (86) | 3 (14) | 1 (4) | 18 (75) | 5 (21) |
| Arthroplasty surgery (%) | 2 (8) | 23 (88) | 1 (4) | 1 (5) | 17 (81) | 3 (14) | 1 (4) | 17 (74) | 5 (22) |
| Total n (%) | 6 (6) | 95 (92) | 2 (2) | 2 (2) | 75 (87) | 9 (10) | 2 (2) | 82 (85) | 13 (13) |
A score of 0 = normal; I = mild to moderate osseous remodelling; II = severe remodelling (osteoarthritis).
The total of 97 persons re-imaged at the 60-month follow-up included 89 patients who received study treatments and eight dropouts who refused treatment.
Net increases in osteoarthritis (II) over 5 years of follow-up: (1) medical management: from 0 to 2 cases = 2/27 = 7.4%; (2) non-surgical rehabilitation: from 0 to 1 case = 1/23 = 4.3%; (3) arthroscopic surgery: from 1 to 5 cases = 4/24 = 16.7%; (4) arthroplasty surgery: from 1 to 5 cases = 4/23 = 17.4%.
Regarding MRI results, all patients had TMJ disc displacement without reduction at baseline on the side of their chief complaint, and this finding was confirmed for all surgical cases. Changes in disc status were measured by MRI only at 24 months. At this follow-up, baseline non-reducing discs persisted in all but three involved joints among the 25 patients in medical management who were re-imaged. One of these discs was reported to have normal position, while two discs were diagnosed as being a disc displacement with reduction. Among the 20 rehabilitation patients receiving an MRI at 2 years, non-reducing discs persisted in all but three joints that now showed disc displacement with reduction. Of the 32 joints that had arthroscopy, 29 had follow-up MRIs. Two non-reducing discs at baseline were reported by the radiologist to have normal disc position at follow-up and five had disc displacement with reduction. All 23 joints that received discoplasty were re-imaged with MRI at 2 years. Five non-reducing discs at baseline were reported to have normal disc position and nine joints showed disc displacement with reduction. Disc position was not normal for 56/63 (89%) surgical joints imaged at 2 years.
Patients randomized to the medical management strategy incurred significantly lower average costs ($1385, range $410–$3555) than rehabilitation ($2379, range $1375–$5240), arthroscopic surgery ($7890, range $5830–$15,940), and arthroplasty ($13,128, range $11,085–$15,280) patients. These costs do not include MRI and tomogram costs, which were the same for all patients.
Discussion
Using the IAOMS success criteria, we found no clinically significant difference between treatment strategies that utilized as the initial treatment any of the following approaches: medical management, rehabilitation, arthroscopic surgery with rehabilitation, and arthroplasty with rehabilitation (P ≥ 0.16). We have previously reported15 the absence of an imbalance between treatment strategy groups at baseline regarding depression, somatization, age, gender, education, and family income. We also found no difference between these treatment strategies15 using other reliable and valid global measures for pain and dysfunction. These consistent findings support a stepped approach to managing patients with symptomatic closed lock, starting with medical management. As previously reported,15 medical management alone was sufficient for a successful outcome in more than half of patients assigned to this treatment strategy. If a patient desires additional care, comprehensive non-surgical rehabilitation, as described for this RCT, should be implemented.
Since improvements over time were unrelated to the initial treatment strategy (Table 3), we concur with the IAOMS recommendation22 to defer surgery for typically 6 months. This allows time for healing to occur, and also for implementation of comprehensive rehabilitation, if that is needed. The practice of evidence-based medicine27 is an integration of the clinician’s experience, the best research evidence, and the patient’s beliefs and expectations. In the current study, one medical management patient and one rehabilitation patient requested and received surgery. Therefore, TMJ surgery is not necessary to manage the vast majority of patients with closed lock. When surgery is considered, arthroscopic surgery is recommended over arthroplasty since it is equally effective with regard to reducing pain and dysfunction, and it costs less.
Review of the literature
The ultimate goal of treatment is to improve on the outcome that would have occurred if no treatment were performed. When education is the only intervention offered, the natural history of closed lock28–30 is to typically improve with time alone. However, one RCT31 has shown that providing palliative treatment, consistent with the medical management offered in the current study, has a better short-term outcome than providing just education about the disorder. These same authors concluded that the addition to medical management of an orthotic and mobilization did not improve outcomes at 2-, 4-, and 8-week follow-ups. Therefore, educating the patient, providing home-based self-care instructions and, when desired by the patient, providing medication for palliative relief of symptoms is the appropriate initial care. In addition, this study suggests that a multi-modal treatment approach with physical therapy, cognitive-behavioural therapy, and orthotics can provide additional support for healing.
Another RCT3 found no difference between physical therapy with or without arthroscopic surgery. In addition, a meta-analysis of different surgeries11 concluded that there was no overall difference between arthrocentesis, arthroscopic surgery, and discectomy, although one RCT32 reported that arthroscopic surgery improved ROM better than arthrocentesis. Arthrocentesis was not assessed in the current study. But, given the results of the RCT mentioned above, it could be considered instead of arthroscopic surgery in cases where ROM is not limited.
This study suggests that disc displacement without reduction can be improved by surgery, and perhaps rarely by non-surgical intervention. An improvement from non-reducing status to disc displacement with reduction was still present at 2 years post-surgery in five joints treated by arthroscopy and in nine joints treated with discoplasty. Normal disc position was achieved surgically for seven non-reducing discs. We have no data to show whether these improvements may have persisted up to 5 years, but in general our 2-year data support prior reports33,34 that any treatment for TMJ closed lock, including surgery, typically results in persistent disc displacement without reduction, or, in the case of discectomy, no disc remaining. We may also conclude that surgically improved disc position did not result in higher success rates for the surgical groups at 2 years (Table 2), and that surgical intervention in patients with closed lock did not ultimately decrease the occurrence of TMJ DJD at 5 years (Table 4).
Defining a successful treatment outcome
It is difficult to claim a successful outcome if success is based on fulfilling all the IAOMS recommended criteria. More importantly, the IAOMS definition of success differed significantly from the patients’ report of improvement. A patient’s subjective impression of success may be more aligned with the least stringent success measures assessed in this paper: the ability to eat most foods, to open one’s mouth pain-free to at least 35 mm, and to have reduced pain intensity – and in that order. Further research on the most appropriate measures of success is recommended.
In summary, more than half of the closed lock patients treated with medical management responded as positively as patients assigned to the other treatment strategies, and additional rehabilitation was as effective as either surgery. This study suggests that clinicians need to educate patients with TMJ closed lock to the reality that immediate relief using any of these treatment strategies does not occur often, and that all treatment strategies result in similar improvement over time.
Acknowledgments
We acknowledge Dr. Clyde Wilkes (surgeon); Drs. Gary Anderson, Mike John, Kate Hathaway, Jana (Wagner) Reinhart, and Greg Pelletier, as well as Constance Bromaghim, Bruce Lindgren, Mary Brazil, Kathleen Olson, and Cynthia Kiecker from the University of Minnesota; Amanda Jackson from the Clinical Dental Research Centre at the University of Minnesota; and Andy Nelson and Dr. Brad Rindal from HealthPartners.
Funding This study was supported by NIH/NIDCR grants R29DEO8668, P30-DEO9737, N01-DE22635, R01 DE13421, NIDCR’s TMJ Implant Registry and Repository (N01-DE-22635), and by HealthPartners of Minnesota, Medica, and by the University of Minnesota School of Dentistry Dental Research Institute and Clinical Dental Research Centre. The costs of the radiological services were offset by Hennepin County Medical Centre in Minneapolis, Minnesota. The radiological and treatments costs were paid, in part, by Medica, HealthPartners of Minnesota, Blue Cross Blue Shield of Minnesota, and the University of Minnesota’s School of Dentistry.
Footnotes
Competing interests No conflict of interest exists between any of the authors or their academic institution with other people or organizations that could influence the conduct of this research being reported or any of the resulting conclusions.
Ethical approval Approval for reanalysis of data was confirmed by the University of Minnesota Research Subjects’ Protection Programme, Human Subjects Code Number: 8709M02208.
References
- 1.Schiffman EL, Ohrbach R, Truelove EL, Feng T, Anderson GC, Pan W, et al. The revised research diagnostic criteria for temporomandibular disorders: methods used to establish and validate revised axis I diagnostic algorithms. J Orofac Pain. 2010;24:63–78. [PMC free article] [PubMed] [Google Scholar]
- 2.de Leeuw JR. Orofacial pain: guidelines for assessment, diagnosis, and management. Quintessence; Chicago, IL: 2008. [Google Scholar]
- 3.Stegenga B, de Bont LG, Dijkstra PU, Boering G. Short-term outcome of arthroscopic surgery of temporomandibular joint osteoarthrosis and internal derangement: a randomized controlled clinical trial. Br J Oral Maxillofac Surg. 1993;31:3–14. doi: 10.1016/0266-4356(93)90089-f. [DOI] [PubMed] [Google Scholar]
- 4.de Leeuw R, Boering G, Stegenga B, de Bont L. Temporomandibular joint osteoarthrosis: clinical and radiographic characteristics 30 years after nonsurgical treatment: a preliminary report. Cranio. 1993;11:15–24. doi: 10.1080/08869634.1993.11677936. [DOI] [PubMed] [Google Scholar]
- 5.Rasmussen OC. Description of population and progress of symptoms in a longitudinal study of temporomandibular arthropathy. Scand J Dent Res. 1981;89:196–203. doi: 10.1111/j.1600-0722.1981.tb01671.x. [DOI] [PubMed] [Google Scholar]
- 6.Rasmussen OC. Clinical findings during the course of temporomandibular arthropathy. Scand J Dent Res. 1981;89:283–8. doi: 10.1111/j.1600-0722.1981.tb01684.x. [DOI] [PubMed] [Google Scholar]
- 7.Dimitroulis G. The role of surgery in the management of disorders of the temporomandibular joint: a critical review of the literature. Part 2. Int J Oral Maxillofac Surg. 2005;34:231–7. doi: 10.1016/j.ijom.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 8.Mercuri LG, Laskin DM. Indications for surgical treatment of internal derangements of the temporomandibular joint. Oral Maxillofac Surg Clin North Am. 1994;6:223–7. [Google Scholar]
- 9.Wilkes CH. Surgical treatment of internal derangements of the temporomandibular joint. A long-term study. Arch Otolaryngol Head Neck Surg. 1991;117:64–72. doi: 10.1001/archotol.1991.01870130070019. [DOI] [PubMed] [Google Scholar]
- 10.Kropmans TJ, Dijkstra PU, Stegenga B, de Bont LG. Therapeutic outcome assessment in permanent temporomandibular joint disc displacement. J Oral Rehabil. 1999;26:357–63. doi: 10.1046/j.1365-2842.1999.00417.x. [DOI] [PubMed] [Google Scholar]
- 11.Reston JT, Turkelson CM. Meta-analysis of surgical treatments for temporomandibular articular disorders. J Oral Maxillofac Surg. 2003;61:3–10. doi: 10.1053/joms.2003.50000. [DOI] [PubMed] [Google Scholar]
- 12.Holmlund AB, Axelsson S, Gynther GW. A comparison of discectomy and arthroscopic lysis and lavage for the treatment of chronic closed lock of the temporomandibular joint: a randomized outcome study. J Oral Maxillofac Surg. 2001;59:972–7. doi: 10.1053/joms.2001.25818. [DOI] [PubMed] [Google Scholar]
- 13.Miyamoto H, Sakashita H, Miyata M, Goss AN. Arthroscopic surgery of the temporomandibular joint: comparison of two successful techniques. Br J Oral Maxillofac Surg. 1999;37:397–400. doi: 10.1054/bjom.1999.0129. [DOI] [PubMed] [Google Scholar]
- 14.Politi M, Sembronio S, Robiony M, Costa F, Toro C, Undt G. High condylectomy and disc repositioning compared to arthroscopic lysis, lavage, and capsular stretch for the treatment of chronic closed lock of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:27–33. doi: 10.1016/j.tripleo.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 15.Schiffman EL, Look JO, Hodges JS, Swift JQ, Decker KL, Hathaway KM, et al. Randomized effectiveness study of four therapeutic strategies for TMJ closed lock. J Dent Res. 2007;86:58–63. doi: 10.1177/154405910708600109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rigon M, Pereira LM, Bortoluzzi MC, Loguercio AD, Ramos AL, Cardoso JR. Arthoscopy for temporomandibular disorders. Cochrane Database Syst Rev. 2011;5:CD006385. doi: 10.1002/14651858.CD006385.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Fricton JR, Nelson A, Monsein M. IMPATH: microcomputer assessment of behavioral and psychosocial factors in craniomandibular disorders. Cranio. 1987;5:372–81. doi: 10.1080/08869634.1987.11678214. [DOI] [PubMed] [Google Scholar]
- 18.Fricton JR. Musculoskeletal measures of orofacial pain. Anesth Prog. 1990;37:136–43. [PMC free article] [PubMed] [Google Scholar]
- 19.Nixdorf DR, John MT, Wall MM, Fricton JR, Schiffman EL. Psychometric properties of the modified Symptom Severity Index (SSI) J Oral Rehabil. 2010;37:11–20. doi: 10.1111/j.1365-2842.2009.02017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fricton JR, Schiffman EL. The craniomandibular index: validity. J Prosthet Dent. 1987;58:222–8. doi: 10.1016/0022-3913(87)90181-8. [DOI] [PubMed] [Google Scholar]
- 21.Fricton JR, Schiffman EL. Reliability of a craniomandibular index. J Dent Res. 1986;65:1359–64. doi: 10.1177/00220345860650111701. [DOI] [PubMed] [Google Scholar]
- 22.Goss AN. Toward an international consensus on temporomandibular joint surgery. Report of the Second International Consensus Meeting, April 1992, Buenos Aires, Argentina. Int J Oral Maxillofac Surg. 1993;22:78–81. doi: 10.1016/s0901-5027(05)80807-0. [DOI] [PubMed] [Google Scholar]
- 23.Wright EF, Schiffman EL. Treatment alternatives for patients with masticatory myofascial pain. J Am Dent Assoc. 1995;126:1030–9. doi: 10.14219/jada.archive.1995.0281. [DOI] [PubMed] [Google Scholar]
- 24.Fricton JR, Hathaway KM, Bromaghim C. Interdisciplinary management of patients with TMJ and craniofacial pain: characteristics and outcome. J Craniomandib Disord. 1987;1:115–22. [PubMed] [Google Scholar]
- 25.Moses JJ, Poker ID. TMJ arthroscopic surgery: an analysis of 237 patients. J Oral Maxillofac Surg. 1989;47:790–4. doi: 10.1016/s0278-2391(89)80035-7. [DOI] [PubMed] [Google Scholar]
- 26.Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove E, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:844–60. doi: 10.1016/j.tripleo.2009.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strauss SE, Richardson WS, Glasziou P, Hayes RB. Evidence-based medicine: how to practice and teach EBM. Elsevier/Churchill Livingstone; New York: 2005. [Google Scholar]
- 28.Sato S, Goto S, Kawamura H, Motegi K. The natural course of nonreducing disc displacement of the TMJ: relationship of clinical findings at initial visit to outcome after 12 months without treatment. J Orofac Pain. 1997;11:315–20. [PubMed] [Google Scholar]
- 29.Sato S, Kawamura H, Nagasaka H, Motegi K. The natural course of anterior disc displacement without reduction in the temporomandibular joint: follow-up at 6, 12, and 18 months. J Oral Maxillofac Surg. 1997;55:234–8. doi: 10.1016/s0278-2391(97)90531-0. [DOI] [PubMed] [Google Scholar]
- 30.Kurita K, Westesson PL, Yuasa H, Toyama M, Machida J, Ogi N. Natural course of untreated symptomatic temporomandibular joint disc displacement without reduction. J Dent Res. 1998;77:361–5. doi: 10.1177/00220345980770020401. [DOI] [PubMed] [Google Scholar]
- 31.Minakuchi H, Kuboki T, Matsuka Y, Maekawa K, Yatani H, Yamashita A. Randomized controlled evaluation of non-surgical treatments for temporomandibular joint anterior disk displacement without reduction. J Dent Res. 2001;80:924–8. doi: 10.1177/00220345010800031501. [DOI] [PubMed] [Google Scholar]
- 32.Goudot P, Jaquinet AR, Hugonnet S, Haefliger W, Richter M. Improvement of pain and function after arthroscopy and arthrocentesis of the temporomandibular joint: a comparative study. J Craniomaxillofac Surg. 2000;28:39–43. doi: 10.1054/jcms.1999.0103. [DOI] [PubMed] [Google Scholar]
- 33.Montgomery MT, Gordon SM, Van Sickels JE, Harms SE. Changes in signs and symptoms following temporomandibular joint disc repositioning surgery. J Oral Maxillofac Surg. 1992;50:320–8. doi: 10.1016/0278-2391(92)90389-h. [DOI] [PubMed] [Google Scholar]
- 34.Montgomery MT, Van Sickels JE, Harms SE. Success of temporomandibular joint arthroscopy in disk displacement with and without reduction. Oral Surg Oral Med Oral Pathol. 1991;71:651–9. doi: 10.1016/0030-4220(91)90268-h. [DOI] [PubMed] [Google Scholar]