Abstract
Background
Social engagement has many demonstrated benefits for aging non-Hispanic Whites in the U.S. This study examined data from the U.S. Health and Retirement Study to determine whether these benefits were similar among American Indians and Alaska Natives older than 50 years.
Methods
Linear regression techniques were used to examine the associations between level of social engagement, scores for memory and mental status, and self-reported health among 203 American Indian and Alaska Native elders who participated in the Health and Retirement Study and had data available between 1998 and 2010.
Results
Level of social engagement was significantly associated with memory, mental status, and self-reported health. However, only the association of social engagement with mental status and self-reported health remained significant (p=0.04 and p=0.05, respectively) after adjusting for sociodemographic variables, number of known health conditions, and scores on the Center for Epidemiologic Studies Depression scale. Level of social engagement was not associated with patterns of decline across time in cognitive or physical health.
Conclusion
Higher levels of social engagement are associated with better physical and cognitive functioning in American Indian and Alaska Native elders. Future studies should examine whether this association acts through cognitive stimulation, increase in physical activity resulting from social engagement, or access to resources that support physical and cognitive health.
Keywords: American Indians, Alaska Natives, elders, social engagement, cognition, memory, aging, retirement, health
BACKGROUND
Physical and mental health among older adults is influenced by a complex set of biological, behavioral, and lifestyle factors (Goins & Pilkerton 2010). Although much of our current understanding of healthy aging in non-Hispanic White elders should also be relevant for American Indian and Alaska Native (AI/AN) elders, limited literature is available on potential associations between psychosocial factors and cognitive and physical health in this population. This scarcity is particularly unfortunate, since the number of AI/AN elders is growing rapidly. Relative to non-Hispanic Whites, this population includes a disproportionate number of people who now or will soon experience significant disability or require full-time assistance or care (Goins & Pilkerton 2010).
Physical activity is recognized as an important feature in the maintenance of health during natural aging in the general population (Chodzko-Zajko et al. 2009) as well as in older AI/ANs (Sawchuk et al. 2008). Putative mechanisms supporting the protective effects of physical activity on cognition, such as increased production of growth hormone and neurotrophic factor, are fairly well understood (Miller et al. 2012). However, several recent reports highlight the importance of psychosocial variables in healthy aging (Ruthig et al. 2011; Tumminello et al. 2011; Ailshire & Crimmins 2011; Lee et al. 2012). For example, emotional well-being, most notably a low or undetectable level of depression, is associated with better cognitive health among elders, whereas depression is independently associated with cognitive difficulties (Ferraro et al. 1997; Bassuk et al. 1998; Ailshire & Crimmins 2011).
Social engagement has also been identified as a potentially protective factor for successful cognitive aging (Bassuk et al. 1999; Ertel et al. 2008; Lee et al. 2012). Its effects appear to be independent of other factors. A recent study from the National Social Life, Health, and Aging Project found that participation in “congregant,” “diverse,” or “friends” social networks (as opposed to “restricted” or “family” networks) was significantly associated with good mental health in later life, especially with avoidance of depressive symptoms and their potential to impair cognition. However, in the same analysis, physical activity did not independently predict good mental health (Litwin 2012). Another recent study showed that low social support and low religiosity independently predicted endorsement of depressive symptoms and major depressive episodes by older adults who accessed aging services (Richardson et al. 2012). Social engagement by itself was associated with quality of life among the oldest old in a recent analysis of data from the University of Michigan Health and Retirement Study (HRS) (Ailshire & Crimmins 2011). Findings suggested that social interactions may play an important role in maintaining physical and mental health in older age. This body of research underscores the potentially vital importance of social integration for good cognitive functioning in later years (Bassuk et al. 1999; Ertel et al. 2008).
Data from the Americans’ Changing Lives survey show that, in a nationally representative sample, older people with high levels of social engagement have lower levels of physical and cognitive limitations over time (Thomas 2011). Other work has shown that continued physical, mental, and social activity in older age may also mitigate the rate and extent of cognitive changes (Fratiglioni et al. 2004). However, all these investigations have focused primarily on non-Hispanic Whites. Their results may not be applicable to populations outside the majority culture, given findings that the size of social networks and the degree of social engagement likely differ across racial groups (Barnes et al. 2004). While social engagement appears to have a positive association with maintenance of cognitive ability in older Americans in general, some findings suggest that race may play an important role in this relationship. For example, the Chicago Health and Aging Study found that Blacks had smaller social networks and lower levels of social engagement than Whites (Barnes et al. 2004). In contrast, a study of community-dwelling elders in New Haven, Connecticut, found that non-Whites (not otherwise specified) were slightly more likely than Whites to be socially engaged (Bassuk et al. 1999).
No studies to date have examined the association between social engagement and physical and cognitive health among AI/ANs. Social engagement may play a larger role for Native elders than it does for elderly Whites, given the importance of family relationships in AI/AN culture (Jervis 2010) and the high rates of comorbid medical problems observed among older AI/ANs, who may face barriers to social activities (Goins & Pilkerton 2010). Our study examines the relationship between social engagement and physical and cognitive health among AI/ANs who participated in the HRS between 1998 and 2010.
METHODS
The University of Michigan HRS, launched in 1992, is a longitudinal survey of a representative sample of more than 26,000 Americans over the age of 50. Interviews are conducted every two years and include 332 AI/AN participants who were first interviewed before 2008. However, the survey items that we needed to construct a measure of social engagement were not available before 1998, so we restricted our analysis to the 203 AI/ANs who provided data on cognitive health and social engagement for the 1998 interview. Our analysis used 1998 data for social engagement, sociodemographic factors, and lifestyle and health characteristics. For cognitive and physical health, we included longitudinal measures across seven waves of data collection, from 1998 through 2010. Since unmasked data on race are not publicly available, we obtained this information through a data use and confidentiality agreement with the University of Michigan. Our analysis was approved by the University of Washington Institutional Review Board.
Measures
We used public-use, imputed datasets to extract the variables necessary for our analyses whenever possible. Pre-processed datasets included the Cross-Wave: Imputation of Cognitive Functioning Measures 1992–2010 (v3.0), RAND HRS Data File (v.L), and 1998 HRS Core Fat Files (Final) RAND (v.B). The raw core family data file (v.2.3) was used to create certain components of the social engagement index. Unmasked race, which allowed us to identify AI/ANs, was available through a restricted-use data file. Our dataset included no missing values because we only used imputed variables prepared by the RAND Center for the Study of Aging.
Cognitive and physical health
The HRS measures cognitive functioning by using the Telephone Interview for Cognitive Status (TICS). We used two resulting summary scores: a memory index and a mental status score. The memory index consisted of both immediate and delayed recall of words in a list. Possible scores ranged from 0 to 20, with higher scores indicating better memory. The mental status score was a composite measure of orientation to time, backward counting, object naming, and serial sevens (Herzog & Wallace 1997). Possible scores ranged from 0 to 15, with higher scores indicating better mental status. Physical health status was assessed by a single question: “Would you say your health is excellent (1), very good (2), good (3), fair (4), or poor (5)?” This item has been previously shown to predict all-cause mortality (Giltay et al. 2012).
Social engagement
Our social engagement index is similar to the one used by Ertel and colleagues (Ertel et al. 2008). It is a composite scale derived from measures of relationship status, volunteer activities, and contact with family and neighbors. Participants received one point each for 1) being married or living with a partner, 2) volunteering for religious, educational, health-related, or other charitable organizations at least one hour in the past year, 3) having weekly or greater contact with any parent, including in-laws, 4) having weekly or greater contact with offspring, and 5) having weekly or greater contact with neighbors. Participants without living parents or offspring were coded as 0 for those domains. The composite index scores range from 0 to 5. The sample was divided into those with low (scores 0–1), moderate (scores 2–3), or high (scores 4–5) levels of social engagement.
Covariates
Sociodemographic covariates included sex, age in 1998, years of education, and total household income in 1998. Income in U.S. dollars was categorized into quartiles ($0–8,580; $8,581–19,312; $19,313–35,330; and >$35,330). Lifestyle and health covariates included score on the Center for Epidemiologic Studies Depression (CES-D) scale, number of self-reported health conditions (high blood pressure, diabetes, stroke, cancer, lung disease, heart problems, arthritis), the presence of at least one self-reported vascular condition (high blood pressure, diabetes, stroke), and physical activity. Physical activity was captured by a single yes/no item asking respondents if, on average over the last 12 months, they participated in vigorous physical activity or exercise three times a week or more.
Statistical analyses
We used linear regression in a four-step process to examine the longitudinal association of cognitive and physical health with baseline social engagement. Cognitive health and physical health were used as dependent variables. First, we fit models that included a three-level social engagement measure and time (measured as HRS data collection wave) as independent variables. We used dummy variables for the social engagement measure, with low social engagement as the reference. We also fit models with continuous social engagement to assess trend. For simplicity, time was fit as a continuous variable, since initial inspection of the data showed a linear trend in outcomes across time. These models allowed us to examine the association of cognitive and physical health with social engagement, averaged across time. We were also able to assess whether cognitive and physical health changed across time. Second, we extended our models to include an interaction term between social engagement and time. These models allowed us to examine whether the trend in cognitive or physical health across time differed according to level of social engagement. We dropped the interaction term from further modeling if it was not significant at the 0.05 level. Third, we added baseline sociodemographic covariates to the models. Fourth, we added covariates for lifestyle and health characteristics. Random effects models were used to account for the correlation between repeated measures from the same individual. All analyses were conducted by using Stata/SE for Windows version 10.1 (StataCorp LP, College Station, TX). Inferential models included the 1998 sample weight provided by HRS as a covariate to adjust parameter estimates for the complex survey sample design.
RESULTS
Data on cognitive health and social engagement were available for 203 AI/ANs in 1998. This group constituted our full sample; we analyzed data on the same participants, subject to availability, in each wave of data collection. By 2010, 11% of the sample had contributed to one wave of data collection, 18% contributed to two or three waves, 27% contributed to four to six waves, and 44% contributed to all seven waves. As shown in Table 1, social engagement was higher in younger participants than in older participants. People with high social engagement had an average age of 56 years in 1998, while those with low social engagement had an average age of 70 years in the same year. Women represented 59% of the full sample, 77% of the low engagement sample, and 61% of the high engagement sample. Social engagement tended to be higher among people with higher income. Forty-four percent of participants with low social engagement were in the lowest income quartile, whereas only 11% of those with high social engagement were in the lowest income quartile. Those with high social engagement also had lower depression scores, fewer health conditions, and higher levels of physical activity.
Table 1.
Sociodemographic, lifestyle, and health characteristics according to level of social engagement in American Indians and Alaska Natives from the Health and Retirement Study in 1998
| Characteristic | Social engagement
|
||
|---|---|---|---|
| Low (N=43) | Moderate (N=132) | High (N=28) | |
| Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | |
| Sociodemographic | |||
| Age in years (in 1998) | 69.7 (11.1) | 62.3 (8.6) | 56.0 (7.4) |
| Female | 77 | 53 | 61 |
| Years of education | 9.1 (4.4) | 9.8 (4.0) | 11.7 (4.7) |
| Income quartile: | |||
| <$8,581 | 44 | 22 | 11 |
| $8,581–19,312 | 26 | 24 | 29 |
| $19,313–35,330 | 19 | 28 | 21 |
| >$35,330 | 12 | 26 | 39 |
| Lifestyle and health | |||
| Depression (CES-D)a | 2.7 (2.2) | 2.2 (2.2) | 1.1 (1.5) |
| Number of health conditionsb | 2.3 (1.5) | 1.9 (1.4) | 1.6 (1.6) |
| ≥ 1 vascular health conditionc | 68 | 55 | 57 |
| Vigorous physical activity ≥ 3 times/week |
35 | 38 | 61 |
CES-D = Center for Epidemiologic Study Depression scale;
hypertension, diabetes, stroke, cancer, lung disease, heart problems, and arthritis;
hypertension, diabetes, stroke.
Social engagement and memory functioning
Figure 1 shows a modest but significant decline in memory functioning across time in all levels of social engagement (p<0.001). We found no evidence that this decline differed according to social engagement (p=0.43). However, in an unadjusted model, participants with higher levels of social engagement had higher mean scores on memory functioning than did participants with lower levels of social engagement (p<0.001). This association became non-significant after adjustment for age and other sociodemographic, lifestyle, and health characteristics (p=0.30, Table 2).
Figure 1.
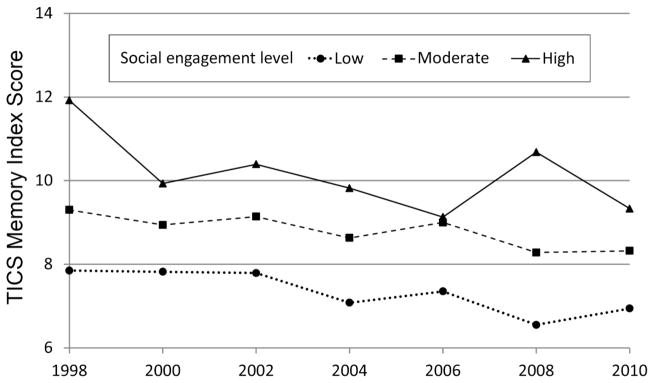
Telephone Interview for Cognitive Status memory index score by level of social engagement from 1998 to 2010
Table 2.
Adjusted mean outcome and 95% confidence intervals according to level of social integration in American Indians who participated in the Health and Retirement Study
| Social integration level | Model 1b | Model 2b | ||
|---|---|---|---|---|
|
| ||||
| Mean | (95% CI) | Mean | (95% CI) | |
| TICS memory indexa | ||||
| Low | 8.1 | (7.4 – 8.8) | 8.3 | (7.7 – 9.0) |
| Moderate | 8.7 | (8.3 – 9.1) | 8.8 | (8.3 – 9.2) |
| High | 9.0 | (8.3 – 9.7) | 8.9 | (8.2 – 9.7) |
| Ptrend | 0.07 | 0.30 | ||
| TICS mental status score | ||||
| Low | 10.3 | (9.6 – 10.9) | 10.2 | (9.6 – 10.9) |
| Moderate | 10.7 | (10.3 – 11.1) | 10.8 | (10.4 – 11.1) |
| High | 11.4 | (10.4 – 12.4) | 11.5 | (10.5 – 12.4) |
| Ptrend | 0.07 | 0.04 | ||
| Self-reported physical health | ||||
| Low | 3.7 | (3.3 – 4.1) | 3.5 | (3.2 – 3.9) |
| Moderate | 3.3 | (3.1 – 3.5) | 3.3 | (3.2 – 3.5) |
| High | 2.8 | (2.4 – 3.2) | 3.0 | (2.6 – 3.3) |
| Ptrend | <0.01 | 0.05 | ||
Memory index ranges from 0 to 20, with higher scores indicating better memory; mental status score ranges from 0 to 15, with higher scores indicating better mental status; self-reported health ranges from 1 to 5, with higher scores indicating worse health.
Model 1 adjusts for sample weight, time, sex, age, education, and income; Model 2 additionally adjusts for number of health conditions, presence of ≥1 vascular health condition (diabetes, hypertension, stroke), physical activity, and Center for Epidemiologic Studies Depression (CES-D) scale score.
Social engagement and mental status
Figure 2 shows a small but significant decline in mental status across time in all levels of social engagement (p=0.01). We found no evidence that the association between mental status and time differed according to social engagement (p=0.06). As in memory functioning, an unadjusted model indicated a monotonic increasing trend in mental status score with increasing level of social engagement (p<0.001). Unlike memory functioning, this association remained significant after adjustment for age and other sociodemographic, lifestyle, and health characteristics (p=0.04, Table 2).
Figure 2.
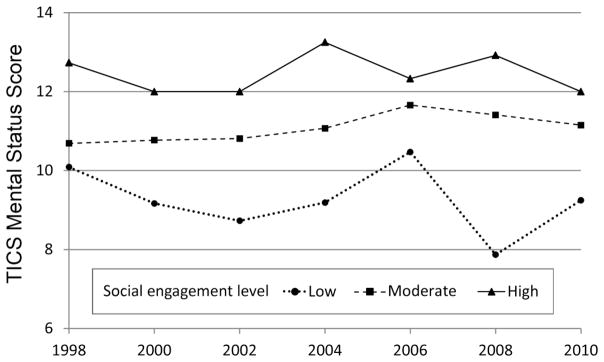
Telephone Interview for Cognitive Status mental status score by level of social engagement from 1998 to 2010
Social engagement and self-reported physical health
Figure 3 shows a small but significant decrease in self-reported health across time at all levels of social engagement (p=0.02). We found no evidence that the association between self-reported health and time differed according to social engagement (p=0.74). In an unadjusted model, self-reported levels of health were uniformly higher at higher levels of social engagement (p<0.01; lower values indicate better health). This association remained marginally significant after adjustment for age and other sociodemographic, lifestyle, and health characteristics (p=0.05, Table 2).
Figure 3.
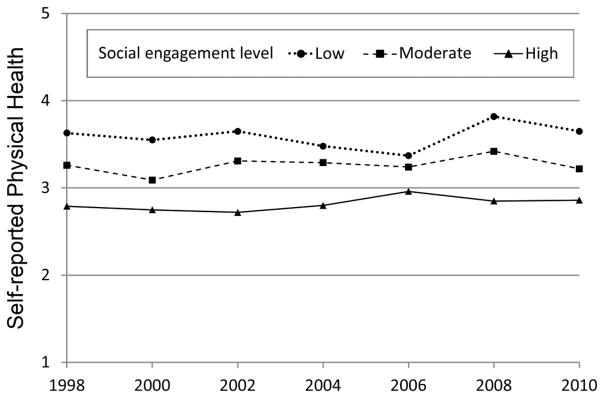
Self-reported physical health by level of social engagement from 1998 to 2010
DISCUSSION
Our analysis took advantage of the HRS, a large-scale investigation of the health status of a representative sample of older U.S. adults, to examine associations between social engagement and cognitive and physical health in an understudied population. Our findings suggest that AI/ANs benefit from some of the advantages of higher levels of social engagement that were demonstrated by Ertel and colleagues for non-Hispanic Whites (Ertel et al. 2008).
Our descriptive analysis found that social engagement tended to be higher among younger members of the sample, with social engagement decreasing with increasing age. This correlation likely reflects decreasing access to social activities for older people, who are more likely to have functional disabilities that can limit mobility. Consistent with this interpretation, we found that higher levels of social engagement corresponded to lower levels of depression and fewer self-reported health conditions. An alternative explanation might be that older AI elders have more traditional beliefs and lifestyles, and may therefore avoid the kinds of social activities measured here. However, this explanation cannot be evaluated with the available HRS data.
Higher levels of social engagement were also more common in participants with higher income. This is consistent with the notion that people with more resources generally have better access to social events or to environments with more opportunities for social interaction.
Overall, the findings of our inferential analyses suggest that social engagement is just as important for the cognitive and physical health of AI/AN elders as it is for elders in other racial and ethnic groups (Bassuk et al. 1999; Barnes et al. 2004; Thomas 2011). Although we were unable to detect any protective effects over time resembling those reported in previous studies – for example, less cognitive and physical decline in participants who were highly socially engaged (Ertel et al. 2008) – we believe that this null result stems from the fact that HRS does not oversample AI/ANs. Without oversampling, the number of AI/ANs for whom data were available was too small to permit more precise inference. In Figures 1 and 2, a slight difference in the slope of the declines is apparent on visual inspection, but our analysis was likely underpowered to detect the interaction effect of time by level of social integration. While we saw a trend toward significance (p=0.06) for the interaction effect of mental status after adjusting for these factors, this trend was likely due to the increased variance associated with the scores of participants in the lowest social engagement group in 2008, rather than to any systematic interaction over the long term.
Despite the limited sample size, we found clear associations between levels of social engagement and both mental status and physical health, even when controlling for sociodemographic variables, self-reported health problems, and depression. The attenuation of the association between social engagement and memory by these covariates may be related to the heightened risk of cerebrovascular disease in people with cardiovascular disease (Kuller et al. 2004; Lopez et al. 2005; Dufouil et al. 2005). Consistent with this hypothesis, we found that self-reported physical health showed a small but significant trend toward decline with increasing age. Disproportionately high levels of cardiovascular disease are regularly reported among AI/ANs, with potentially serious implications for memory functioning in older age (Longstreth 1998; Elkins et al. 2004; Harwell et al. 2005). White matter hyperintensities associated with cerebrovascular disease accompany memory dysfunction as well as depression in older adults; both of these conditions are also likely to affect various domains of social engagement (O’Brien et al. 2006; Herrmann et al. 2007; Richardson et al. 2012), especially since depression by itself can compromise cognition in elderly people (Bassuk et al. 1998). A larger sample size would be helpful to disentangle this potentially complex set of relationships in AI/AN elders. Unfortunately, such an analysis is impossible with available data.
The likely mechanisms underlying the relationships between social engagement and both cognitive and physical health are a potentially fruitful area of inquiry. Future studies could examine whether the association acts through cognitive stimulation, increase in physical activity resulting from social engagement, or material support in the form of access to resources that can maintain and improve physical and cognitive health. This is an important research question, because an understanding of the mechanisms at work will inform future interventions in AI/AN communities.
Our study has several limitations. While our work demonstrated a strong association between social engagement and cognitive and physical health, secondary data analyses such as this one cannot constrain the direction of the relationship. It is possible that elders with higher levels of cognitive and physical health remain socially engaged, while elders with deteriorating functioning in these domains become more reclusive. Such outcomes might be particularly likely for people who live in rural areas, as do many AI/AN elders. Long travel times and limited options for transportation in these areas may present barriers to participating in social gatherings. A second major limitation was the lack of oversampling of AI/ANs in the HRS. As a result, our study sample was relatively small and our analytic power was restricted, preventing us from detecting potential interaction effects of social engagement with rates of cognitive decline. The routine adoption of oversampling in the design of large, population-based studies would yield substantial benefits for health disparities research in general.
A further limitation might be our use of TICS, a simple measure of general cognitive functioning, to estimate cognitive health (Herzog & Wallace 1997). More complex measures can provide richer information about functioning across a larger number of cognitive domains, since social engagement may be more strongly associated with some domains than others. For example, the dynamic nature of social interaction may be more helpful in maintaining domains of fluid intelligence than such crystallized functions as memory. Some types of social interaction are also more protective than others (e.g., playing bridge versus joining others in watching a play).
Finally, our analysis treated social engagement as a static variable, even though it likely changes over time. However, the data needed to examine the potentially dynamic nature of this factor were not collected by the HRS. A finer measure of social networks may be a fruitful addition to the HRS, because such networks are probably significant for health in older adults.
The reliability and consistency across domains of the associations between social engagement, physical health, and cognitive health suggest that interventions to increase social activities can improve the health and well-being of AI/AN elders. Such a strategy seems especially pertinent for this population, since many Native elders reside in remote rural areas with few opportunities for social interaction (Lee et al. 2012). Simply increasing access to social activities could have beneficial effects on cognitive and physical health (Bassuk et al. 1999; Lee et al. 2012).
In summary, we found that higher levels of social engagement were associated with better functioning in both cognitive and physical health domains among older AI/ANs in the University of Michigan HRS. Although we found no evidence for a protective effect of social engagement on decline in cognitive or physical health, this null result may stem from our small sample size and the resulting limits on analytic power. Understanding the relationships between cognitive health and a broad array of social activities will assist in designing future interventions.
Acknowledgments
We would like to thank Dr. Karen A. Ertel for providing us with the social engagement scoring algorithm. Her assistance made these analyses possible. This work was supported by National Institutes of Health grant 5 P60 MD5000507, Research Center of Excellence (EXPORT).
References
- Ailshire J, Crimmins E. Psychosocial Factors Associated with Longevity in the United States: Age Differences Between the Old and the Oldest-Old in the Health and Retirement Study. Journal of Aging Research. 2011;2011:Article ID 530534. doi: 10.4061/2011/530534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes L, Mendes De Leon C, Bienias J, Evans D. A Longitudinal Study of Black-White Differences in Social Resources. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2004;59:S146–153. doi: 10.1093/geronb/59.3.s146. [DOI] [PubMed] [Google Scholar]
- Bassuk SS, Berkman LF, Wypij D. Depressive Symptomatology and Incident Cognitive Decline in an Elderly Community Sample. Archives of General Psychiatry. 1998;55:1073–1081. doi: 10.1001/archpsyc.55.12.1073. [DOI] [PubMed] [Google Scholar]
- Bassuk SS, Glass TA, Berkman LF. Social Disengagement and Incident Cognitive Decline in Community-Dwelling Elderly Persons. Annals of Internal Medicine. 1999;131:165–173. doi: 10.7326/0003-4819-131-3-199908030-00002. [DOI] [PubMed] [Google Scholar]
- Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ, Skinner JS. Exercise and Physical Activity for Older Adults. Medicine and Science in Sports and Exercise. 2009;41:1510–1530. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- Dufouil C, Chalmers J, Coskun O, Besancon V, Bousser MG, Guillon P, Macmahon S, Mazoyer B, Neal B, Woodward M, Tzourio-Mazoyer N, Tzourio C. Effects of Blood Pressure Lowering on Cerebral White Matter Hyperintensities in Patients with Stroke: The PROGRESS (Perindopril Protection Against Recurrent Stroke Study) Magnetic Resonance Imaging Substudy. Circulation. 2005;112:1644–1650. doi: 10.1161/CIRCULATIONAHA.104.501163. [DOI] [PubMed] [Google Scholar]
- Elkins JS, O’Meara ES, Longstreth WT, Jr, Carlson MC, Manolio TA, Johnston SC. Stroke risk factors and loss of high cognitive function. Neurology. 2004;63:793–799. doi: 10.1212/01.wnl.0000137014.36689.7f. [DOI] [PubMed] [Google Scholar]
- Ertel KA, Glymour MM, Berkman LF. Effects of Social Integration on Preserving Memory Function in a Nationally Representative US Elderly Population. American Journal of Public Health. 2008;98:1215–1220. doi: 10.2105/AJPH.2007.113654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro F, Bercier B, Chelminski I. Geriatric Depression Scale-Short Form (GDS-SF) performance in Native American elderly adults. Clinical Gerontologist. 1997;18:52–55. [Google Scholar]
- Fratiglioni L, Paillard-Borg S, Winblad B. An Active and Socially Integrated Lifestyle in Late Life Might Protect Against Dementia. The Lancet Neurology. 2004;3:343–353. doi: 10.1016/S1474-4422(04)00767-7. [DOI] [PubMed] [Google Scholar]
- Giltay EJ, Vollaard AM, Kromhout D. Self-rated Health and Physician-rated Health as Independent Predictors of Mortality in Elderly Men. Age and Ageing. 2012;41:165–171. doi: 10.1093/ageing/afr161. [DOI] [PubMed] [Google Scholar]
- Goins R, Pilkerton C. Comorbidity among Older American Indians: The Native Elder Care Study. Journal of Cross-Cultural Gerontology. 2010;25:343–354. doi: 10.1007/s10823-010-9119-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harwell TS, Oser CS, Okon NJ, Fogle CC, Helgerson SD, Gohdes D. Defining Disparities in Cardiovascular Disease for American Indians: Trends in Heart Disease and Stroke Mortality among American Indians and Whites in Montana, 1991 to 2000. Circulation. 2005;112:2263–2267. doi: 10.1161/CIRCULATIONAHA.105.560607. [DOI] [PubMed] [Google Scholar]
- Herrmann LL, Lemasurier M, Ebmeier KP. White Matter Hyperintensities in Late Life Depression: A Systematic Review. Journal of Neurology, Neurosurgery, and Psychiatry. 2007;79(6):619–624. doi: 10.1136/jnnp.2007.124651. [DOI] [PubMed] [Google Scholar]
- Herzog AR, Wallace RB. Measures of Cognitive Functioning in the AHEAD Study. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 1997;52B:37–48. doi: 10.1093/geronb/52b.special_issue.37. [DOI] [PubMed] [Google Scholar]
- Jervis LL. American Indian family caregivers’ experiences with helping elders. Journal of Cross-Cultural Gerontology. 2010;25:355–369. doi: 10.1007/s10823-010-9131-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuller LH, Longstreth WT, Jr, Arnold AM, Bernick C, Bryan RN, Beauchamp NJ., Jr White Matter Hyperintensity on Cranial Magnetic Resonance Imaging: A Predictor of Stroke. Stroke. 2004;35:1821–1825. doi: 10.1161/01.STR.0000132193.35955.69. [DOI] [PubMed] [Google Scholar]
- Lee CT, Yeh CJ, Lee MC, Lin HS, Chen VCH, Hsieh MH, Yen CH, Lai TJ. Social Support and Mobility Limitation as Modifiable Predictors of Improvement in Depressive Symptoms in the Elderly: Results of a National Longitudinal Study. Archives of Gerontology and Geriatrics. 2012;55(3):530–538. doi: 10.1016/j.archger.2012.03.002. [DOI] [PubMed] [Google Scholar]
- Litwin H. Physical Activity, Social Network Type, and Depressive Symptoms in Late Life: An Analysis of Data from the National Social Life, Health and Aging Project. Aging and Mental Health. 2012:1–9. doi: 10.1080/13607863.2011.644264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longstreth WT., Jr Brain Abnormalities in the Elderly: Frequency and Predictors in the United States (the Cardiovascular Health Study). Cardiovascular Health Study Collaborative Research Group. Journal of Neural Transmission Supplementum. 1998;53:9–16. doi: 10.1007/978-3-7091-6467-9_2. [DOI] [PubMed] [Google Scholar]
- Lopez OL, Kuller LH, Becker JT, Jagust WJ, Dekosky ST, Fitzpatrick A, Breitner J, Lyketsos C, Kawas C, Carlson M. Classification of Vascular Dementia in the Cardiovascular Health Study Cognition Study. Neurology. 2005;64:1539–1547. doi: 10.1212/01.WNL.0000159860.19413.C4. [DOI] [PubMed] [Google Scholar]
- Miller DI, Taler V, Davidson PSR, Messier C. Measuring the Impact of Exercise on Cognitive Aging: Methodological Issues. Neurobiology of Aging. 2012;33:622. doi: 10.1016/j.neurobiolaging.2011.02.020. [DOI] [PubMed] [Google Scholar]
- O’Brien JT, Firbank MJ, Krishnan MS, Van Straaten EC, Van Der Flier WM, Petrovic K, Pantoni L, Simoni M, Erkinjuntti T, Wallin A, Wahlund LO, Inzitari D. White Matter Hyperintensities Rather Than Lacunar Infarcts Are Associated with Depressive Symptoms in Older People: The LADIS Study. American Journal of Geriatric Psychiatry. 2006;14:834–841. doi: 10.1097/01.JGP.0000214558.63358.94. [DOI] [PubMed] [Google Scholar]
- Richardson T, Friedman B, Podgorski C, Knox K, Fisher S, He H, Conwell Y. Depression and its Correlates among Older Adults Accessing Aging Services. American Journal of Geriatric Psychiatry. 2012;20:346–54. doi: 10.1097/JGP.0b013e3182107e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruthig J, Hanson B, Pedersen H, Weber A, Chipperfield J. Later Life Health Optimism, Pessimism and Realism: Psychosocial Contributors and Health Correlates. Psychology & Health. 2011;26:835–853. doi: 10.1080/08870446.2010.506574. [DOI] [PubMed] [Google Scholar]
- Sawchuk CN, Charles S, Wen Y, Goldberg J, Forquera R, Roy-Byrne P, Buchwald D. A Randomized Trial to Increase Physical Activity among Native Elders. Preventive Medicine. 2008;47:89–94. doi: 10.1016/j.ypmed.2008.03.011. [DOI] [PubMed] [Google Scholar]
- Thomas PA. Trajectories of Social Engagement and Limitations in Late Life. Journal of Health and Social Behavior. 2011;52:430–443. doi: 10.1177/0022146511411922. [DOI] [PubMed] [Google Scholar]
- Tumminello M, Miccichè S, Dominguez LJ, Lamura G, Melchiorre MG, Barbagallo M, Mantegna RN. Happy Aged People Are All Alike, While Every Unhappy Aged Person Is Unhappy in its Own Way. PLoS ONE. 2011;6:e23377. doi: 10.1371/journal.pone.0023377. [DOI] [PMC free article] [PubMed] [Google Scholar]


