Abstract
Alcohol and marijuana use are thought to increase sexual risk taking, but event-level studies conflict in their findings and often depend on reports from a limited number of people or on a limited number of sexual events per person. With event-level data from 1856 sexual intercourse events provided by 297 college women (Mage = 18 years; 71% White), we used multilevel modeling to examine associations between alcohol and marijuana use and condom use as well as interactions involving sexual partner type and alcohol-sexual risk expectancies. Controlling for alternative contraception use, partner type, regular levels of substance use, impulsivity and sensation-seeking, and demographics, women were no more or less likely to use condoms during events involving drinking or heavy episodic drinking (HED) than during those without drinking. However, for drinking events, there was a negative association between number of drinks consumed and condom use; additionally, women with stronger alcohol-sexual risk expectancies were marginally less likely to use condoms when drinking. Although there was no main effect of marijuana use on condom use, these data suggest that marijuana use with established romantic partners may increase risk of unprotected sex. Intervention efforts should target expectancies and emphasize the dose-response relationship of drinks to condom use.
Young people between the ages of 15 and 24 account for 50% of all new HIV infections (Wilson, Wright, Safrit, & Rudy, 2010) and are also at elevated risk for other sexually transmitted infections (STIs; CDC, 2009). Condom use is an important method for reducing the risk of STIs as well as unplanned pregnancy (CDC, 2010). However, most young people use condoms inconsistently, or not at all (American College Health Association, 2012; Eaton et al., 2012). Alcohol use and marijuana use are thought to increase sexual risk taking (Cooper, 2006), and many cross-sectional studies find associations between substance use and risky sex (Cooper, 2002; Leigh & Stall, 1993). However, the picture is less clear when the focus is on event-level associations between substance use and condom use (for review, see Cooper, 2002; Weinhardt & Carey, 2000). Conflicting results have emerged as a function of sexual partner type, and few studies have considered marijuana use specifically. Methodologically, research has often depended on reports from a limited number of people or on a limited number of sexual events per person. To address these gaps and methodological limitations in prior research, we use data collected from a large sample of college women across a full year to examine associations between alcohol and marijuana use and condom use while including detailed assessments of sexual partner type and considering several relevant control variables.
Substance Use and Sexual Risk-Taking
Theoretical explanations for ties between substance use and risky sex
There are a number of theoretical explanations for ties between alcohol use and risky sexual behavior. First, alcohol intoxication may cause one to take sexual risks. According to alcohol myopia theory (Steele & Josephs, 1990), alcohol disinhibits behavior by affecting information processing. When under the influence of alcohol, highly salient, instigating cues (e.g., arousal) continue to be processed, while more distal and complex cues that would ordinarily inhibit behavior (e.g., concerns about STIs or pregnancy) are no longer adequately processed.
Second, expectancy theories (e.g., Lang, 1985) also provide an explanation for the associations between substance use and sexual risk behavior. According to these models, individuals’ behavior after drinking is driven by beliefs about alcohol’s effects on behavior. Thus, those individuals who believe that alcohol leads to sexual risk taking may be more likely to exhibit risky behavior when under the influence. Expectancy theories are supported by studies finding that individuals who believe they have consumed alcohol who also hold strong expectancy beliefs report greater sexual arousal and perceive interaction partners as more sexually disinhibited (George, Stoner, Norris, Lopez, & Lehman, 2000).
Finally, it is also possible that alcohol does not affect sexual risk taking, but that other variables lead to both. For example, personality traits such as sensation-seeking or impulsivity (Charnigo et al., 2013; Leigh & Stall, 1993), or environmental characteristics such as living in a sorority or fraternity (Baer, 1994) may encourage both drinking and sexual behavior. Impulsivity (the tendency to make decisions without attending to the consequences of one’s actions; Hoyle, Fejfar, & Miller, 2000) and sensation seeking (the desire for novel and exciting experiences; Zuckerman, Buchsbaum, & Murphy, 1980) have been of particular interest in past research given their associations with both substance use (e.g., Hittner & Swickert, 2006; Verdejo-García, Lawrence, & Clark, 2008) and sexual risk taking (e.g., Kahn, Kaplowitz, Goodman, & Emans, 2002; Spitalnick et al., 2007). Indeed, some studies have found that sensation-seeking completely accounts for the association between drinking and risky sexual behavior (Justus, Finn, & Steinmetz, 2000; Kalichman, Heckman, & Kelly, 1996).
Although alcohol myopia theory and expectancy theory are specific to alcohol use, they might also be applied to marijuana use. Tetrahydrocannabinol (THC), the active physiological ingredient in marijuana, may have detrimental effects on memory, inhibition, and decision-making (Lane, Cherek, Tcheremissine, Lieving, & Pietras, 2005; Skosnik, Spatz-Glenn, & Park, 2001); lab studies have found that acute marijuana use is associated with increases in risky decision-making (Lane et al., 2005). Studies have also shown that young people hold sex-related marijuana expectancies, and that these expectancies function similarly to alcohol expectancies (Hendershot, Magnan, & Bryan, 2010). Additionally, impulsivity and sensation-seeking are associated with marijuana use in addition to alcohol use (Donohew et al., 2000).
Alcohol use and condom use
Although reviews of studies using event-level methodology (Cooper, 2002, 2006; Weinhardt & Carey, 2000) conclude that, overall, people who use condoms when sober also tend to use them when drinking, studies have found that heavy drinking may reduce condom use under some specific circumstances. However, evidence regarding these circumstances is conflicting. Some studies have suggested that drinking is associated with a lower probability of condom use with steady (romantic) partners only (e.g., Scott-Sheldon, Carey, & Carey, 2010), while other studies have suggested that drinking is associated with a lower probability of condom use with casual partners only (e.g., Brown & Vanable, 2007; Kiene, Barta, Tennen, & Armeli, 2009; LaBrie, Earleywine, Schiffman, Pedersen, & Marriot, 2005). Several studies have found no associations between alcohol consumption and safer sex regardless of partner type (e.g., Bailey, Gao, & Clark, 2006; Schroder, Johnson, & Wiebe, 2009).
In addition to conflicting findings related to partner type, studies have measured alcohol use in different ways, with many studies using dichotomous indicators of drinking (e.g., Brown & Vanable, 2007; Schroder et al., 2009; Scott-Sheldon et al., 2009; Shrier, Walls, Lops, Kendall, & Blood, 2012), and others using dichotomous indicators of heavy drinking (Cousins, McGee, & Layte, 2010; Scott-Sheldon, et al., 2010; for exceptions, see Bailey, et al., 2006; Kiene, et al., 2009; Parks, Hsieh, Collins, & Levonyan-Radloff, 2011). Reviews have suggested that it may be important to consider not only use, but also level of use (Weinhardt & Carey, 2000).
Alcohol expectancies play an important role in explaining associations between drinking and condom use, with several studies finding a stronger relationship between alcohol consumption and unprotected sex for those with high alcohol expectancies (Corbin & Fromme, 2002; Dermen & Cooper, 2000; Dermen, Cooper, & Agocha, 1998; LaBrie et al., 2005). However, the majority of these studies have found this interaction only for specific sexual events, such as first intercourse or first intercourse with one’s most recent partner (Corbin & Fromme, 2002; Dermen & Cooper, 2000; Dermen et al., 1998). Because of the relatively small number of studies and conflicting results, expectancies warrant further exploration.
Marijuana use and condom use
As compared to alcohol use, the influence of event-level marijuana use has been much less frequently studied. At the global level, young people who use marijuana tend to engage in riskier sexual activities (Bellis et al., 2008; Guo et al., 2005; Yan, Chiu, Stoesen, & Wang, 2007) and be at a higher risk of STIs (Smith et al., 2010; Wu, Ringwalt, Patkar, Hubbard, & Blazer, 2009). Results related to condom use are mixed, but marijuana use is related to a reduced frequency of condom use in most studies (Adefuye, Abiona, Balogun, & Lukobo-Durrell, 2009; Bellis et al., 2008; Guo et al., 2005; Yan et al., 2007).
However, only a few studies have assessed whether using marijuana in conjunction with sexual activity influences condom use. These studies have generally found that marijuana use before sex predicts a decrease in the likelihood of condom use (Bryan, Schmiege, & Magnan, 2012; Hendershot et al., 2010; Kingree & Betz, 2003; Kingree, Braithwaite, & Woodring, 2000). One study has suggested these associations occur primarily for new partners (Bryan et al., 2012), though most studies have not included detailed measures of partner type.
The role of partner type
Partner type has often been considered as a control or moderating variable when considering the effects of substance use on condom use. There are theoretical reasons to anticipate differences in the effects of alcohol or marijuana dependent upon partner type. Research has shown that partner familiarity lessens perceptions of HIV and STI risk (Swann, Silvera, & Proske, 1995; Williams et al., 1992). More known partners are perceived as safer, possibly because individuals use incorrect heuristics (such as perceiving familiar others as similar to the self; Robbins & Krueger, 2005) to estimate sexual partners’ HIV risks. Research has suggested that even modest familiarity may be enough to decrease risk appraisals (Swann et al., 1995). Alcohol myopia models (Steele & Josephs, 1990) would suggest that familiarity may act as a particularly salient impelling cue encouraging unprotected sex when intoxicated.
Although familiarity may be a strong impelling cue, research has also suggested that established romantic partners often negotiate a stable pattern of sexual behavior and condom use, often replacing the use of condoms with hormonal contraception as their relationship progresses (Civic, 2000; Hammer, Fisher, Fitzgerald, & Fisher, 1996). In these cases, due to established patterns of condom (non-)use, alcohol or marijuana use may have little impact on whether use occurs. Finally, research has suggested that levels of substance use in conjunction with sexual activity differ across partner types, with substance use being more common with newer or less known partners (LaBrie et al., 2005). Although many studies of alcohol or marijuana use and condom use have considered only two or three partner categories (i.e., steady, casual, and/or new partners), the functions of both familiarity and established behavior patterns suggest that the role of partner type might be more complex. Specifically, we might anticipate the strongest influence of substance use on condom use with new romantic and known casual partners (e.g., friends), given that these partners are familiar, that patterns of sexual protection may not be established, and that substance use may be common.
The role of gender
Past studies have suggested that associations between alcohol use and condom use differ based on gender. Specifically, several studies have identified negative associations between drinking and condom use for women, but not men (Bryan, Ray, & Cooper, 2007; Dermen & Cooper, 2000; Scott-Sheldon et al., 2010; Scott-Sheldon et al., 2009). Because of gender-based power differentials present in sexual encounters (Bryan, Aiken, & West, 1997; Wingood & DiClemente, 2000), women may have less control over condom use than do men (Campbell, 1995; Pearson, 2006), and more self-regulation and greater skills in negotiation may be necessary for women to influence the use of condoms. Drinking or drug use may impair women’s abilities to negotiate condom use (e.g., Maisto, Carey, Carey, Gordon, & Schum, 2004). Research has also suggested that alcohol use and partner type may interact for women but not men (Scott-Sheldon et al., 2010; Scott-Sheldon et al., 2009). Because of these gender differences in associations between substance use and unprotected sex, we chose to conduct a focused, systematic analysis of substance use and condom use among women.
Research Objectives
Mixed results in the literature indicate the need for further exploration of associations between substance use and condom use at the event level. Five features of the current study allow it to make a novel contribution to this research area. First, many previous studies using event-level data have included few participants or few events per participant, have required participants to recall multiple events from the past several months, or have depended on reports of unique sexual events (e.g., first intercourse or the first time with a new partner). To improve upon these, we collected 12 monthly reports on most recent sexual events with both romantic and casual partners from a large sample of women. In this way, participants provided multiple reports on unique events (up to 24 per participant) but had to recall only recent (i.e., past month) events. Spacing these reports one month apart also reduced the chances of reactivity due to daily reporting. Second, we included a detailed assessment of partner type as a moderator of the association between substance use and condom use. Third, we assessed levels of alcohol use as well as categorical alcohol use as a predictor to improve upon prior work that has used more limited, dichotomous measures of alcohol use. Fourth, we assessed the relationship between marijuana use and condom use in college women. Few event-level studies have explored associations between marijuana use and safe sex (cf, Bryan et al., 2012; Hendershot et al., 2010; Shrier et al., 2012), and these studies have primarily focused on high-risk adolescents rather than college students. Fifth, we assessed alcohol expectancies as a potential moderating variable and also considered important control variables not always accounted for, including event-level use of alternative contraception and the personality characteristics impulsivity and sensation-seeking.
Using event-level data from a large sample of first-year college women, we addressed the following research questions:
Are event-level drinking (yes/no), heavy episodic drinking (HED; yes/no), or number of drinks consumed associated with condom use during sexual encounters involving intercourse? Based on the theories presented, we hypothesized that any drinking, HED, and number of drinks consumed within a drinking event would be negatively related to condom use even after controlling for regular levels of HED, impulsivity, sensation seeking, partner type, alternative contraception use, and demographic controls.
Is marijuana use associated with condom use during sexual encounters involving intercourse? Based on limited previous research and knowledge of the pharmacological effects of marijuana, we hypothesized that marijuana use would be negatively related to condom use even after controlling for regular levels of marijuana use, impulsivity, sensation seeking, partner type, alternative contraception use, and demographic controls.
Do associations between substance use and condom use vary based on partner type? We compared long-term romantic partners to new romantic partners, known casual partners (friends and ex-boyfriends), and unknown casual partners (strangers and acquaintances). We predicted that substance use would have the largest associations with condom use for new romantic and known casual partners, given that these partners are familiar (an instigating cue) but that patterns of sexual protection may not yet be established.
Do alcohol expectancies moderate associations between drinking, HED, and number of drinks and condom use? Based on expectancy theories, we hypothesized that drinking, HED, and number of drinks consumed would be more negatively related to condom use for those with strong alcohol-sexual risk expectancies.
Method
Participants
Participants came from a pool of 483 female first-year college students (Mage = 18, SDage = 0.21) at a Northeastern university who participated in a year-long study of health behaviors and relationships. The larger study explored a variety of health behaviors (e.g., substance use, diet, exercise, sleep) as well as sexual behavior and psychosocial adjustment (Fielder, Carey, & Carey, 2013; Walsh, Fielder, Carey, & Carey, 2012). The women included in the current study (N = 297, 61% of the total sample) all reported at least one episode of intercourse with a romantic or casual partner during their first year of college. Most participants were Caucasian (71%); other self-identified racial/ethnic identities included African American (13%), Asian (8%), and other (7%); 11% identified as Latina. The ethnic distribution of the sample was representative of the incoming first-year female students at the university in Fall 2009.
Procedures
This research was approved by the university’s Institutional Review Board. Participants were recruited via a mass mailing sent to incoming first-year female students. Campus flyers, word of mouth, and the psychology department participant pool were also used to bolster recruitment. Interested students attended an orientation session, after which they provided informed consent and completed the initial survey. Subsequently, participants completed monthly online assessments for one year; surveys were completed during the first week of each month reporting on the previous month. For each survey, participants received $10 to $20, depending on survey length.
Measures
Event-level
During each of the 12 monthly follow-up surveys, women who reported having engaged in either oral or vaginal sex during the past month reported on their most recent encounter involving oral, vaginal, or anal sex with both a romantic and a casual partner. Thus, each participant could describe between 0 and 2 events per month, or between 0 and 24 events total. Events were included in analysis only if participants reported that (1) the event had occurred during the month immediately preceding each data collection and (2) the event involved either vaginal or anal sex.
Condom use
For events involving vaginal sex, participants reported whether they and their partner used a condom during vaginal sex (0 = no, 1 = yes). For events involving anal sex, participants reported whether they and their partner used a condom during anal sex (0 = no, 1 = yes). Given that anal sex was rare (n = 79, 3% of events), these measures were combined to indicate any condom use during an event.
Alcohol use and HED
Participants reported whether they drank alcohol before each event (0 = no, 1 = yes). Those participants who did consume alcohol reported the number of drinks they consumed; participants were coded as engaging in HED if they had consumed 4 or more drinks (Wechsler, Dowdall, Davenport, & Rimm, 1995). Number of drinks was positively skewed and was normalized with a natural log transformation.
Marijuana use
Participants reported whether they used drugs other than alcohol before each event (0 = no, 1 = yes). Those participants who had used drugs reported which drugs they had used (“marijuana,” “another drug,” or “both marijuana and another drug”). We coded whether participants had used marijuana.
Partner type
For those events with a casual partner, participants reported who their partner was for the event. Response options included “a stranger,” “an acquaintance,” “a friend,” “an ex-boyfriend or ex-girlfriend,” and “other.” For some analyses, casual partner types were classified as “unknown” (strangers and acquaintances) and “known” (friends and exes). Answers of “other” were rare (n = 57, 2% of events) and were coded as missing.
Relationship length
Participants who were involved in romantic relationships reported the length of their current relationship in months. Current relationship length was recoded to indicate if a romantic relationship was new (≤ 3 months) or established (> 3 months). Women who reported engaging in intercourse with a romantic partner but indicated they were dating but not in a committed relationship were considered to be in new romantic relationships.
Alternative contraception
Participants reported what method(s) of birth control they and their partner had used (e.g., “nothing,” “male condom,” or “withdrawal”). Participants who reported use of the birth control pill, patch, or vaginal ring; an injectable hormone (Luelle, Depo Provera); or an intrauterine device (IUD) were coded as using alternative, reliable contraception.
Person-level
Person-level variables were assessed only once during the year.
Average HED
Each month, participants reported the number of days they had consumed 4 or more drinks on one occasion. This variable was recoded to indicate any HED, and months were averaged to indicate a proportion of months during the first year of college in which HED occurred.
Average marijuana use
Each month, participants reported the number of times they had used marijuana. This variable was recoded to indicate any marijuana use and months averaged to indicate a proportion of months during the first year of college in which marijuana use occurred.
Alcohol-sexual risk expectancies
At four points during the year (T1, T5, T9, and T13), sexually active participants completed 3 items from the sexual risk subscale of Dermen and Cooper’s (1994) measure of sex-related alcohol expectancies. Participants reported their level of agreement with statements related to practicing safer sex after drinking (e.g., “After a few drinks of alcohol, I am less likely to use birth control”) on a scale from 1 (“strongly disagree”) to 6 (“strongly agree”). Items were averaged at each time point, with higher scores indicating stronger expectancies that alcohol consumption leads to unsafe sex (αs = .86). The four summary scores obtained during the year were averaged (α = .79); this positively-skewed average was normalized with a natural log transformation.
Impulsivity
At baseline, impulsivity was measured using six items (Magid, MacLean, & Colder, 2007) from the impulsiveness subscale of the Impulsiveness—Monotony Avoidance Scale (Schalling, 1978). Participants indicated how well each item (e.g., “I often throw myself too hastily into things”) applied to them on a Likert scale from 1 (not at all like me) to 4 (very much like me). Scores were summed to create a total score (α = .82).
Sensation-seeking
At baseline, sensation-seeking was measured using six items (Magid et al., 2007) from the monotony avoidance subscale of the Impulsiveness—Monotony Avoidance Scale (Schalling, 1978). Participants indicated how well each item (e.g., “I like doing things just for the thrill of it”) applied to them on a Likert scale from 1 (not at all like me) to 4 (very much like me). Scores were summed to create a total score (α = .82).
Control variables
Several variables were included as demographic controls. Dummy variables indicated whether participants self-identified as African-American, Asian/Asian-American, or Latina. Socioeconomic status (SES) was assessed using a 10-point ladder (Adler, Epel, Castellazzo, & Ickovics, 2000), on which participants ranked their family relative to other American families. Participants reported to what extent they considered themselves religious (from “not religious” to “very religious”) and their frequency of attending religious services (from “never” to “more than once a week”). These items were averaged, with higher scores on a 0-to-3 scale indicating greater religiosity (α = .80). Finally, participants indicated their high school grade point average (GPA) on a 4.0 scale.
Data Management and Analysis
Missing data
Completion rates for monthly surveys ranged from 82% (T11) to 100% (T1), with the average participant completing 11.82 months of data collection (SD = 2.24). Data on individual person-level variables were missing for between 0 and 11% of participants. There was also a small amount of missing data related to reported events (1.5% or less for all variables). Women with missing data had lower high school GPAs, t(294) = 3.03, p < .01, and more pre-college sexual partners, t(294) = −5.15, p < .001. Additionally, they were more likely to be African American, χ2(1) = 9.15, p < .01, less likely to be Asian or Asian American, χ2(1) = 7.69, p < .01, and more likely to have used marijuana in the month before entering college, χ2(1) = 9.13, p < .01. However, there were no differences in other demographic variables (i.e., age, religiosity, or SES), or in initial levels of condom use or pre-college alcohol or tobacco use. In order to maintain the entire sample, multiple imputation (MI) was used to replace missing values (Rubin, 1996; Schafer, 1997). MI is a modern method for dealing with missing data that avoids biases associated with using only complete cases or with single imputations (Schafer, 1999). We imputed 100 complete datasets (Graham, Olchowski, & Gilreath, 2007) using the R program Amelia (Honaker, King, & Blackwell, 2011) by first imputing 10 complete datasets at the person level and then imputing 10 event-level datasets for each imputed person-level dataset. This is the preferred method for imputing event-level data. All study variables were included in the imputation. Analyses were conducted with all 100 datasets, and parameter estimates were pooled using the imputation algorithms in Mplus 7 (Muthén & Muthén, 1998–2013).
Analysis plan
We used multilevel modeling in Mplus 7 (Muthén & Muthén, 1998–2013) to analyze the data. Sexual events (N = 1856) were nested within people (N = 297), and we examined both event-level predictors (i.e., substance use, partner type, and alternative contraception use) and person-level predictors (i.e., demographics, average substance use, impulsivity, sensation-seeking, and expectancies). We originally tested which control variables were associated with event-level condom use, so that we could control for the most relevant factors. We controlled for any variables significant at the p < .10 level. Following this, the first set of models explored uncontrolled associations between substance-use variables (event-level drinking, HED, number of drinks, and marijuana use) and condom use. We also report associations between drinking, HED, number of drinks, and marijuana use and condom use controlling for partner type alone (given strong associations between partner type and both substance use and condom use).
Proceeding from these simpler models, we constructed full models including (1) substance use, (2) partner type, (3) interactions between partner type and substance use (to test whether associations between substance use and condom use varied across partner types), and (4) all relevant control variables as predictors of event-level condom use. Finally, to explore the role of alcohol-sexual risk expectancies (for alcohol use models only), a random effect of alcohol use on condom use was modeled, and we explored whether this association was stronger for those women with stronger expectancies (i.e., we tested the interaction between expectancies and substance use). The model examining number of drinks included only those events with alcohol use (n = 371 events from n = 144 women). Across all models, we compared models including all women to models including only those women who varied in their pre-event substance use (i.e., those women who reported drinking or using marijuana before some but not all sexual events) to assure that estimates of the substance use-condom use association did not differ; results were consistent across models, so we report results for the full sample. Coefficients for variables that were highly non-significant (T < 1) were constrained to zero to increase model parsimony and stabilize estimates (Bentler & Mooijaart, 1989). Odds ratios (ORs) or unstandardized coefficients (Bs) as well as 95% confidence intervals (CIs) are reported throughout.
Results
Rates of Drinking, HED, Marijuana Use, and Condom Use by Partner Type
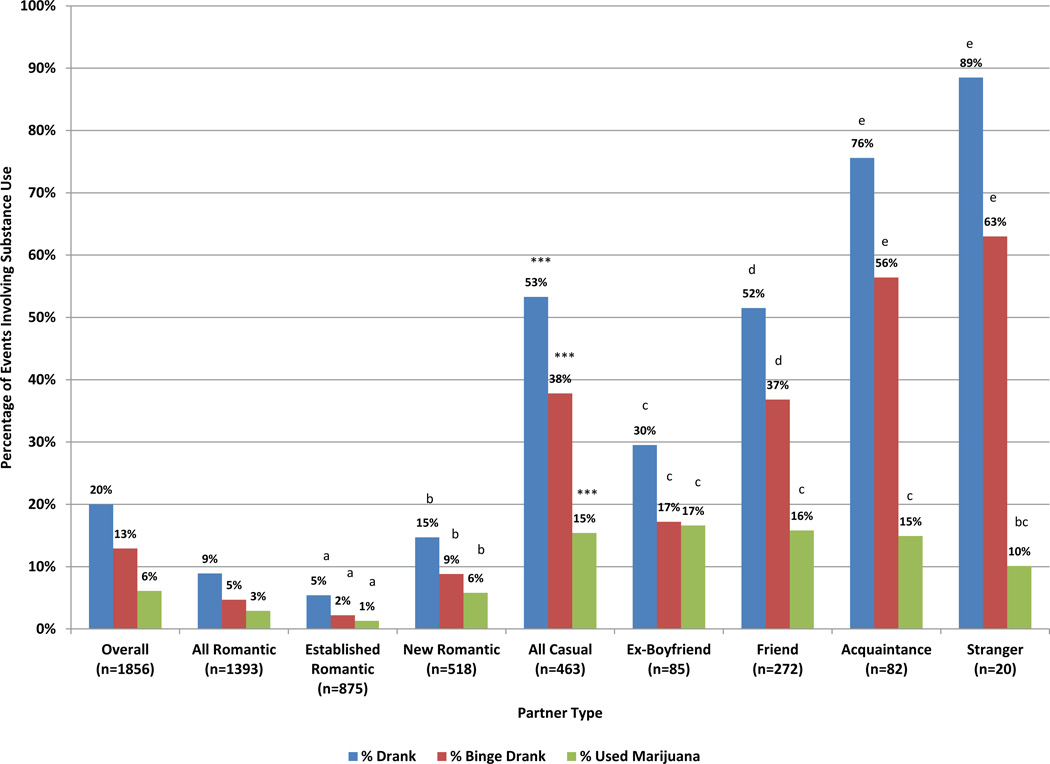
Figure 1 shows the percentage of events with different types of partners that involved any drinking, HED, or marijuana use. Overall, 20% of events (n = 371) involved any drinking, 13% (n = 240) involved HED, and 6% (n = 112) involved marijuana use. All three types of substance use were less common with romantic partners (9%, 5%, and 3% of events, respectively) than with casual partners (53%, 38%, and 15% of events, respectively). All types of substance use were more common in events with new romantic partners than in events with established romantic partners. Alcohol use was more common with relatively unknown casual partners (acquaintances and strangers) than with friends, and more common with friends than with ex-boyfriends. Marijuana use did not differ across casual partner types.
Figure 1.
Rates of substance use in sexual events involving different types of partners. Asterisks compare the likelihood of substance abuse in events involving romantic vs. casual partners (*** p < .001). Individual partner types not sharing letters significantly differ, p < .05.
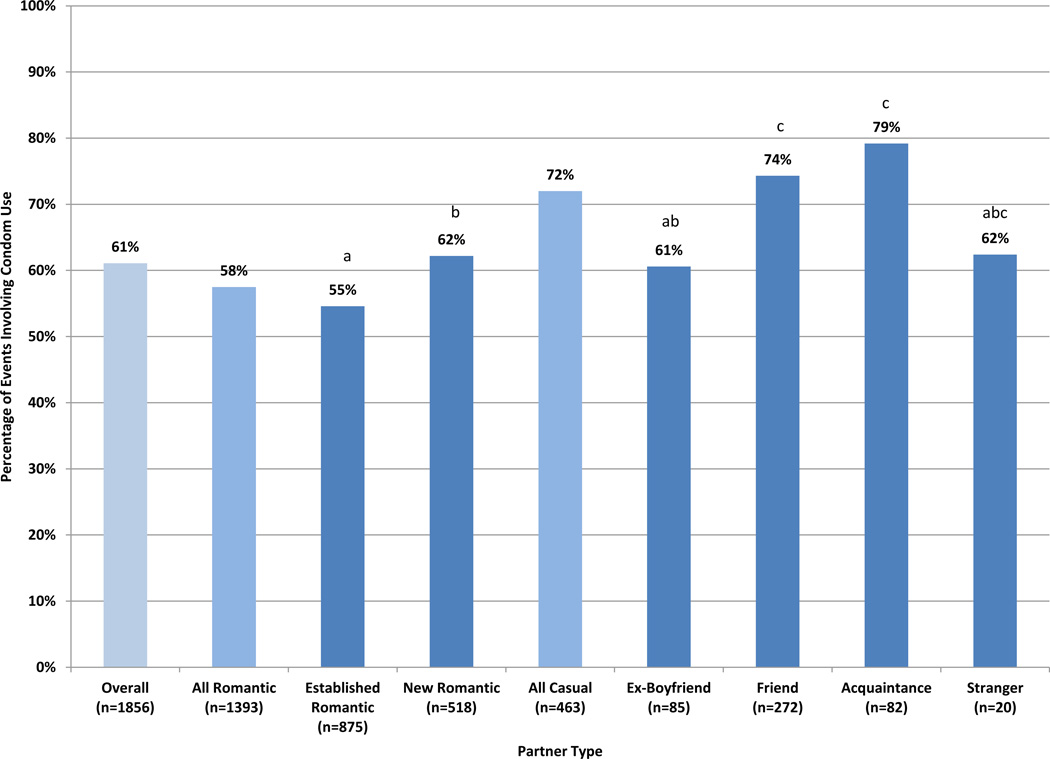
Figure 2 shows the percentage of events with different types of partners during which a condom was used. Overall, women reported using condoms during 61% of events (n = 1134). Condom use was less common in events involving romantic partners (58%) than in events involving casual partners (72%). Women were least likely to use condoms in events involving established romantic partners (55%) and most likely to use them in events involving friends (74%) and acquaintances (79%).
Figure 2.
Rates of condom use in sexual events involving different types of partners. As compared to events involving romantic partners, condom use was significantly more likely to occur in events involving casual partners, OR = 1.90, CI[1.32,2.74], p < .001. Individual partner types not sharing letters significantly differ, p < .05.
Control Variables Predicting Condom Use
Prior to considering substance use, we tested associations between our control variables (partner type, alternative contraception use, demographics, average substance use, and impulsivity and sensation seeking) and condom use in order to determine which variables were important to include in substance use models. As expected, event-level partner type and alternative contraception use were predictors of condom use. Specifically, as compared to events involving established romantic partners, women were more likely to use condoms with new romantic partners, OR = 2.05, CI[1.25,3.37], p < .01, known casual partners, OR = 3.77, CI[1.82,7.81], p < .001, and unknown casual partners, OR = 4.83, CI[1.91,12.24], p < .001. Women were less likely to use condoms when they were using alterative contraception, OR = 0.24, CI[0.13,0.42], p < .001.
There were few significant predictors of condom use at the person level. Controlling for event-level factors, African American women were less likely to use condoms, B = −1.17, CI[−2.33,−0.02], p < .05. Additionally, there was a marginally significant negative association between regular HED and condom use, B = −1.00, CI[−2.16,0.17], p = .09, meaning that women who engaged in HED more regularly throughout the year were less likely to use condoms. Other demographics, average marijuana use, impulsivity, and sensation-seeking did not relate to event-level condom use. We thus controlled for partner type, alternative contraception use, African American race, and average HED in substance use models including all events.
We separately tested control variables for the number of drinks model that included only those events involving drinking (n = 371 events from n = 144 women). For this subsample of events, as compared to events with established romantic partners, condom use was more likely with known casual partners, OR = 3.19, CI[1.08,9.47], p < .05, and marginally more likely with unknown casual partners, OR = 2.99, CI[1.08,9.47], p < .10. Additionally, Asian/Asian-American women were more likely to use condoms, B = 0.26, CI[0.05,0.48], p < .05. There were no other person-level factors that related to event-level condom use. We thus controlled for partner type and Asian/Asian-American race in the number of drinks model.
We also tested control variable predictors of the drinking-condom use, HED-condom use, and number of drinks-condom use slopes (i.e., looked for variables predicting the association between alcohol use and condom use for individual women). Results showed that Asian/Asian-American race was positively associated with the drinking-condom use slope, B = 2.34, CI[0.67,4.00], p < .01, indicating that for Asian/Asian-American women, drinking was positively associated with condom use. A follow-up analysis including only Asian/Asian-American women (n = 24 women, n = 125 events) and controlling for partner type, alternative contraception use, and regular drinking showed that event-level drinking was positively associated with condom use, OR = 9.97, CI[4.60,21.65], p < .001. Asian/Asian-American women used condoms in 89% of events involving alcohol consumption and 63% of events not involving alcohol consumption. No other control variables predicted the drinking-condom use slope, and there were no control variables that predicted the HED-condom use or number of drinks-condom use slopes. Therefore, we controlled for Asian/Asian-American race when exploring the interaction between drinking and alcohol-sexual risk expectancies.
Drinking as a Predictor of Condom Use
A model containing only drinking and condom use (with no control variables) showed that events involving drinking were more likely to include condom use, OR = 1.88, CI[1.13,3.13], p < .05. Condoms were used in 70% of events involving drinking and 59% of events not involving drinking. However, this association disappeared after accounting for partner type, OR = 1.32, CI[0.81,2.17], p = .27.
A fully-controlled model including drinking, partner type, alternative contraception use, regular drinking, and African American race (see Table 1) continued to show no association between alcohol consumption and condom use, and no interactions between drinking and partner type.
Table 1.
Substance Use as a Predictor of Event-Level Condom Use (Fully Controlled Models)
| Drinking Predicting Condom Use |
Heavy Episodic Drinking Predicting Condom Use |
Number of Drinks Predicting Condom Use |
Marijuana Use Predicting Condom Use |
|||||
|---|---|---|---|---|---|---|---|---|
| Event-Level Predictors | Adj. OR | 95% CI | Adj. OR | 95% CI | Adj. OR | 95% CI | Adj. OR | 95% CI |
| Substance Use | 1.21 | 0.74,1.99 | .74 | 0.35,1.56 | .46* | 0.22,0.93 | 0.16* | 0.04,0.67 |
| Alternative Contraception | .24*** | 0.09,0.61 | .24*** | 0.14,0.42 | -- | -- | 0.23*** | 0.13,0.40 |
| New Romantic Partner | 2.04** | 1.25,3.34 | 2.09** | 1.28,3.41 | 2.27 | 0.68,7.55 | 1.89* | 1.15,3.12 |
| Known Casual Partner | 3.55*** | 1.73,7.30 | 3.22** | 1.49,6.95 | 3.81* | 1.22,11.88 | 3.32** | 1.58,7.00 |
| Unknown Casual Partner | 4.27** | 1.68,10.85 | 5.92*** | 2.17,16.21 | 3.65* | 1.05,12.72 | 4.69** | 1.80,12.24 |
| Substance Use * New Romantic Partner | -- | -- | -- | -- | -- | -- | 7.26* | 1.42,37.09 |
| Substance Use * Known Casual Partner | -- | -- | 2.15 | .69,6.97 | -- | -- | 9.15** | 1.89,44.23 |
| Substance Use * Unknown Casual Partner | -- | -- | -- | -- | -- | -- | 5.03 | 0.39,65.32 |
| Person-Level Predictors | B | 95% CI | B | 95% CI | B | 95% CI | B | 95% CI |
| Black Race | −1.27* | −2.41,−0.13 | −1.27* | −2.40,−0.13 | -- | -- | −1.25* | −2.39,−0.12 |
| Asian/Asian-American Race | -- | -- | -- | -- | 1.73* | .22,3.24 | -- | -- |
| Average Binge Drinking | −1.13+ | −2.29,0.04 | −1.09+ | −2.24,0.07 | -- | -- | −1.03+ | −2.18,0.13 |
| R2 Within | .22*** | .12,.32 | .23*** | .13,.32 | .08 | −.02,.17 | .23*** | .13,.32 |
| R2 Between | .03 | −.02,.09 | .03 | −.02,.08 | .07 | −.04,.19 | .03 | −.02,.08 |
p < .10
p < .05
p < .01
p < .001
Notes. Results are reported for four separate models, one for each form of substance use. -- indicates control variables and interaction terms not included in the target model. R2 within indicates the proportion of the variance in condom use within subjects (i.e., across different sexual events) explained by event-level predictors, while R2 between indicates the proportion of the variance in condom use between subjects (i.e., across different individuals) explained by person-level predictors.
When expectancies were added to the model, we found that alcohol-sexual risk expectancies were negatively associated with condom use, B = −1.63, CI[−2.37,−0.89], p < .001, such that women who held stronger beliefs that drinking led to sexual risk-taking were less likely to use condoms. Additionally, there was a marginally significant association between alcohol-sexual risk expectancies and the drinking-condom use slope, B = −0.91, CI[−1.93,0.11], p = .08, meaning that drinking showed a trend toward being negatively associated with condom use for those women with stronger expectancies.
HED as a Predictor of Condom Use
A model containing only HED and condom use (with no control variables) showed that events involving HED were also more likely to include condom use, OR = 1.75, CI[1.01,3.04], p < .05. Condoms were used in 70% of events involving HED and 60% of events not involving HED. However, this association disappeared after accounting for partner type, OR = 1.03, CI[0.94,1.14], p = .53.
A fully-controlled model (Table 1) continued to show no association between HED and condom use. Additionally, there were no significant interactions between partner type and HED.
When expectancies were added to the model, alcohol-sexual risk expectancies were negatively associated with condom use, B = −1.66, CI[−2.36,−0.95], p < .001. Additionally, there was a marginally significant association between alcohol-sexual risk expectancies and the HED-condom use slope, B = −0.93, CI[−2.04,0.18], p < .10, meaning that HED showed a trend toward being negatively associated with condom use for those women with stronger expectancies.
Number of Drinks as a Predictor of Condom Use
We explored the association between the number of drinks consumed and condom use for events involving alcohol consumption (n = 371 events reported by n = 144 women). Controlling for partner type, events involving some drinking were more likely to be reported by women who engaged more regularly in HED, B = 2.80, CI[1.90,3.71], p < .001, and who had lower high school GPAs, B = −0.94, CI[−1.81,−0.07], p < .05.
A model containing only number of drinks and condom use (with no control variables) showed a marginal, negative association between number of drinks consumed and condom use, OR = 0.55, CI[0.27,1.11], p < .10; this association became significant when controlling for partner type, OR = 0.46, CI[0.22,0.94], p < .05.
A significant, negative association between number of drinks consumed and condom use remained in the fully-controlled model (Table 1), meaning that women who consumed more drinks had a reduced probability of condom use. There were no significant interactions between partner type and number of drinks consumed.
When expectancies were added to the model, alcohol-sexual risk expectancies were negatively associated with condom use, B = −1.43, CI[−2.19,−0.67], p < .001. There was no association between alcohol-sexual risk expectancies and the number of drinks-condom use slope, B = −0.80, CI[−1.86,0.26], p = .14; number of drinks consumed was negatively associated with condom use regardless of expectancies.
Marijuana Use as a Predictor of Condom Use
A model containing only marijuana use and condom use showed no event-level association between marijuana use and condom use, OR = 1.01, CI[0.38,2.68], p = .99. Condoms were used in 67% of events involving marijuana use and 61% of events not involving marijuana use. The relationship between marijuana use and condom use remained non-significant when accounting for partner type, OR = 0.90, CI[0.35,2.32], p = .83.
A full model (Table 1) showed significant interactions between partner type and marijuana use. Specifically, there was a negative association between event-level marijuana use and condom use for events with established romantic partners, OR = 0.16, CI[0.04,0.67], p < .05, such that women were less likely to use a condom with an established partner if they had engaged in marijuana use. Follow-up analyses showed that condoms were used in 55% of events (n = 475) with established romantic partners in which there was no marijuana use and 27% of events (n = 3) with established romantic partners in which there was marijuana use. In contrast, the interaction terms for marijuana use and new romantic partners and marijuana use and known casual partners were significant and positive, OR = 7.26, CI[1.42,37.09], p < .05 and OR = 9.15, CI[1.89,44.23], p < .01, respectively, indicating that marijuana use was associated with an increased probability of condom use for events involving new romantic and known casual partners. Follow-up analyses indicated that condoms were used in 62% of new romantic partner events not involving marijuana (n = 303) and 67% of events (n = 20) involving marijuana. Condoms were used in 70% of known casual partner events not involving marijuana (n = 211) and 75% of events (n = 43) involving marijuana.
Discussion
This study contributes to the literature by using reports collected over a year from a large sample of college women to clarify associations between both alcohol and marijuana use and condom use. With detailed measures of partner type and controls for alternative contraception use as well as person-level characteristics, we found no event-level association between the occurrence of drinking or HED and condom use, although there was a trend toward women with higher alcohol-sexual risk expectancies showing reduced levels of condom use when drinking. However, in events involving drinking, the number of drinks consumed was negatively associated with condom use. In contrast with past studies, we found no main effect of marijuana use on condom use. However, our data suggest that marijuana use with established romantic partners may increase risk of unprotected sex.
Associations Between Alcohol Use and Condom Use
In line with reviews of the literature (Cooper, 2002; Weinhardt & Carey, 2000), our study showed few main effects of alcohol use on condom use. Indeed, among college women, alcohol use and condom use tend to co-occur, because both are more likely in events involving casual partners. After controlling for partner type, we found no associations between either drinking and condom use, contrary to what might be predicted by alcohol myopia theory (Steele & Josephs, 1990). Even in situations involving heavy drinking (4+ drinks), during which we might expect disinhibition to lead to decreases in safe sex behavior, we found no evidence of decreased condom use across this sample of women. However, in events during which some drinking occurred (20% of all events), we found a negative association between number of drinks consumed and condom use; that is, as number of drinks increased, condom use decreased, which may suggest that only extremely high levels of drinking reduce the probability of condom use. Alternatively, there may be other factors differentiating the 20% of sexual events involving alcohol consumption from events with no alcohol consumption. Indeed, although our models explained nearly a quarter of the variance in condom use when considering all events, they explained only 7% of the variance in condom use in the model including the subset of events involving alcohol consumption, despite the fact that alcohol consumption was a significant predictor in this model (see Table 1). The differences in results across our alcohol models points to the importance of carefully specifying how substance use is operationalized.
Importantly, our research found no interactions of alcohol use with partner type. Previous studies have reported such interactions, with some studies suggesting alcohol use increases the risk of unprotected sex with romantic/steady partners (Scott-Sheldon et al., 2010), some suggesting it increases risk with casual partners (Brown & Vanable, 2007; Kiene et al., 2009; LaBrie et al., 2005), and some suggesting it decreases risk with casual partners (Leigh & Stall, 1993; Leigh et al., 2008). Our study may help to explain previous findings that suggest a positive association between alcohol use and condom use for casual partners (Leigh & Stall, 1993; Leigh et al., 2008). The interactions identified in these studies may have resulted from all casual partners being grouped together. In contrast, our study showed that both drinking and condom use were more common with less familiar casual partners (i.e., acquaintances and strangers), which could account for this interaction.
We found some evidence supporting expectancy theory (e.g., Lang, 1985). Alcohol consumption and expectancies interacted such that associations between drinking and HED and condom use were marginally more negative for those women holding strong expectancies that alcohol use would lead to sexual risk taking. Expectancy models theorize that individuals’ behavior after drinking is driven by preexisting beliefs about alcohol’s effects on behavior; in this case, women may have been less likely to use condoms after drinking when they believed that drinking would lead them to be more reckless. Alternatively, women who used condoms less frequently when drinking may have developed expectancies in line with their behavior. Notably, even in our college sample, strong alcohol-sexual risk expectancy beliefs were relatively uncommon; the mean on the 6-point scale was 2.19 (SD = 1.14), and only 13% of women (n = 39) scored above the scale midpoint (indicating they agreed that they were less likely to practice safer sex after drinking).
One unexpected finding that emerged from our study was a positive association between drinking and condom use for Asian and Asian-American women in our sample. Although our sample contained relatively few Asian/Asian-American women (n = 24), these women reported 125 sexual events. Across these events, there was a higher probability of condom use in events involving drinking (89%) than in those not involving drinking (63%), even controlling for partner type and alternative contraception use. Previous research has suggested that Asian and Asian-Americans tend to have more conservative sexual attitudes (Baldwin, Whiteley, & Baldwin, 1992) and more rigid gender-role expectations for women (Chia, Chong, Cheng, & Castellow, 1986). Research has also shown that female condom proposers may be judged more harshly by members of some Asian cultures than by European-Americans (Conley, Collins, & Garcia, 2000). Although further research is necessary, it seems possible that alcohol use may increase the probability of condom use for Asian/Asian-American women by decreasing anxiety about proposing condoms.
Associations Between Marijuana Use and Condom Use
Compared to alcohol, relatively few studies have considered marijuana use as a predictor of condom use, although the active ingredients in marijuana may impact decision making (Lane et al., 2005). Previous studies have tended to find reductions in the probability of condom use during events involving marijuana use (Bryan et al., 2012; Hendershot et al., 2010; Kingree & Betz, 2003; Kingree et al., 2000), but these studies have all focused on high-risk adolescent (i.e., younger) samples. We found no main effect of marijuana use on condom use among college women. However, the interaction we found between partner type and marijuana use suggests that marijuana use with established romantic partners decreases the probability of condom use, while marijuana use with new romantic and known casual partners increases the probability of condom use. Only one previous study of marijuana use has found an interaction between marijuana use and partner type; this study (Bryan et al., 2012), which focused on adolescents on probation, found that marijuana use was associated with a reduced probability of condom use primarily with partners participants had just met. However, there was also evidence that condom use was lower with serious relationship partners when marijuana was used (53% vs. 63%), in line with our finding. The small number of events with established romantic partners that involved marijuana use in our study limits the evidential basis of our findings. Future research should collect detailed partner and condom use data from more frequent marijuana users to confirm these results.
Substance Use, Condom Use, and Partner Type
In contrast to past studies that have often characterized partners as only romantic/steady or casual, we collected data on a wider range of sexual partners. We found that both substance use and condom use varied dramatically based on specific partner type. Not only were alcohol use and condom use both less likely with romantic than with casual partners (see Figures 1 and 2), but specific subtypes of romantic partners (new vs. established) and casual partners (ex-boyfriends, friends, acquaintances, and strangers) differed from one another. Both drinking and HED decreased in a linear fashion as partners became more familiar, with drinking occurring in 87% of events involving strangers but just 5% of events involving established romantic partners. Partner types also proved to be important event-level predictors of condom use (Table 1), and, as discussed, our results suggested differences in associations between marijuana and condom use for different subtypes of romantic partners. These differences suggest the value of detailed assessments of partner types; future research should consider categorizing sexual partners in a similar manner.
Impulsivity, Sensation-Seeking, and Other Control Variables
Our study makes clear the importance of event-level factors such as partner type and alternative contraception use in explaining condom use. In contrast, few person-level factors were important predictors of event-level condom use. Indeed, although personality factors such as impulsivity and sensation-seeking are seen as important predictors of both alcohol use and sexual risk-taking (Justus et al., 2000; Kalichman et al., 1996), both were unrelated to event-level condom use when we accounted for partner type and contraception use. Even regular levels of alcohol use were only marginally associated with event-level condom use, and regular marijuana use did not predict condom use. Alcohol-sexual risk expectancies were one person-level factor that did play an important role; these expectancies were a significant, positive predictor of condom use in our sample. Overall, event-level factors explained much more of the variance in condom use than did person-level factors, and future research might choose to focus on identifying additional predictors at the event level.
Limitations and Future Directions
Several limitations of the current study suggest directions for future research. First, our data came exclusively from female students at one university, among whom rates of condom use were relatively high and rates of marijuana use were relatively low. Future studies should assess male students as well, and might target students who are heavier substance users (regular drinkers or marijuana users). Second, although we assessed both levels of alcohol use and marijuana use, we did not assess partner substance use, which may also be an important predictor of condom use (e.g., Scott-Sheldon et al., 2009). There also may be other event-level and person-level predictors that are important in explaining condom use; our models explained only a quarter of the variance in condom use. Future research might particularly want to consider contextual factors, such as setting and condom availability, and marijuana expectancies in addition to alcohol expectancies. Additionally, future research should consider issues of consent given both the high rates of sexual victimization among college women (Humphrey & White, 2000) and men’s greater control over condom use (Amaro, 1995). Finally, although we assessed substance use and condom use at the event-level, we are unable to determine if associations between substance use and condom use are causal.
Conclusions and Implications
Despite strong theory connecting alcohol use to risky sexual behavior, our study adds to others that fail to show any strong association between alcohol use and condom use (Cooper, 2002; Weinhardt & Carey, 2000). We chose to test associations between substance use and condom use among college women based on the mixed results in the literature related to partner type and the relative scarcity of studies examining marijuana. Our methods (e.g., large sample, multiple events, detailed assessments) improve upon most previous research, allowing stronger inferences regarding the alcohol (marijuana)-condom use association. Our study identified a negative association between number of drinks consumed and condom use when considering events involving drinking and suggests that alcohol use may be a predictor of condom use for women with strong alcohol-sexual risk expectancies. Additionally, in line with recent studies (e.g., Bryan et al., 2012; Hendershot et al., 2010), our research suggests marijuana use may put women at risk for unprotected sex in some contexts, such as with established romantic partners. Future studies of college students might benefit most from focusing on high-risk subsamples or on particular types of relationships. Possible areas for intervention with young adults are reducing alcohol-sexual risk expectancies and/or counteracting the influence of expectancies by educating women that they can exert control over their actions despite being intoxicated (e.g., employing a positive deviance approach, Marsh, Schroeder, Dearden, Sternin, & Sternin, 2004). Our findings also suggest that efforts to reduce alcohol-involved sexual risk behavior might emphasize the dose-response relationship of drinks to condom use once one decides to drink.
Acknowledgements
This research was supported by grant R21-AA018257 awarded to Michael P. Carey from the National Institutes on Alcohol Abuse and Alcoholism.
Footnotes
Conflict of Interest Statement: The authors have no conflict of interest to disclose.
References
- Adefuye AS, Abiona TC, Balogun JA, Lukobo-Durrell M. HIV sexual risk behaviors and perception of risk among college students: implications for planning interventions. BMC Public Health. 2009;9(1):281. doi: 10.1186/1471-2458-9-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy, White women. Health Psychology. 2000;19(6):586. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Amaro H. Love, sex and power. American Psychologist. 1995;50(6):437–447. doi: 10.1037//0003-066x.50.6.437. [DOI] [PubMed] [Google Scholar]
- American College Health Association. The American College Health Association–National College Health Assessment II: Reference group executive summary Spring 2012. Hanover, MD: American College Health Association; 2012. [Google Scholar]
- Baer JS. Effects of college residence on perceived norms for alcohol consumption: An examination of the first year in college. Psychology of Addictive Behaviors. 1994;8(1):43. [Google Scholar]
- Bailey SL, Gao W, Clark DB. Diary study of substance use and unsafe sex among adolescents with substance use disorders. Journal of Adolescent Health. 2006;38(3) doi: 10.1016/j.jadohealth.2004.12.001. [DOI] [PubMed] [Google Scholar]
- Baldwin JD, Whiteley S, Baldwin JI. The effect of ethnic group on sexual activities related to contraception and STDs. Journal of Sex Research. 1992;29(2):189–205. [Google Scholar]
- Bellis M, Hughes K, Calafat A, Juan M, Ramon A, Rodriguez J, et al. Sexual uses of alcohol and drugs and the associated health risks: A cross sectional study of young people in nine European cities. BMC Public Health. 2008;8(1):155. doi: 10.1186/1471-2458-8-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM, Mooijaart A. Choice of structural model via parsimony: A rationale based on precision. Psychological Bulletin. 1989;106(2):315–317. doi: 10.1037/0033-2909.106.2.315. [DOI] [PubMed] [Google Scholar]
- Brown JL, Vanable PA. Alcohol use, partner type, and risky sexual behavior among college students: Findings from an event-level study. Addictive Behaviors. 2007;32(12):2940–2952. doi: 10.1016/j.addbeh.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan AD, Aiken LS, West SG. Young women's condom use: the influence of acceptance of sexuality, control over the sexual encounter, and perceived susceptibility to common STDs. Health Psychology. 1997;16(5):468. doi: 10.1037//0278-6133.16.5.468. [DOI] [PubMed] [Google Scholar]
- Bryan AD, Ray LA, Cooper ML. Alcohol use and protective sexual behaviors among high-risk adolescents. Journal of Studies on Alcohol and Drugs. 2007;68(3):327–335. doi: 10.15288/jsad.2007.68.327. [DOI] [PubMed] [Google Scholar]
- Bryan AD, Schmiege SJ, Magnan RE. Marijuana use and risky sexual behavior among high-risk adolescents: Trajectories, risk factors, and event-level relationships. Developmental Psychology. 2012;48(5):1429–1442. doi: 10.1037/a0027547. [DOI] [PubMed] [Google Scholar]
- Campbell CA. Male gender roles and sexuality: Implications for women's AIDS risk and prevention. Social Science & Medicine. 1995;41(2):197–210. doi: 10.1016/0277-9536(94)00322-k. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance, 2006. Atlanta, GA: U.S. Department of Health and Human Services; 2009. [Google Scholar]
- Centers for Disease Control and Prevention. Condoms and STDs: Fact sheet for public health personnel. Atlanta, GA: National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; 2010. [Google Scholar]
- Charnigo R, Noar SM, Garnett C, Crosby R, Palmgreen P, Zimmerman RS. Sensation seeking and impulsivity: Combined associations with risky sexual behavior in a large sample of young adults. Journal of Sex Research. 2013;50(5):480–488. doi: 10.1080/00224499.2011.652264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia RC, Chong CJ, Cheng BS, Castellow W. Attitude toward marriage roles among Chinese and American college students. The Journal of Social Psychology. 1986;126(1):31–35. [Google Scholar]
- Civic D. College students' reasons for nonuse of condoms within dating relationships. Journal of Sex & Marital Therapy. 2000;26(1):95–105. doi: 10.1080/009262300278678. [DOI] [PubMed] [Google Scholar]
- Conley TD, Collins BE, Garcia D. Perceptions of women condom proposers among Chinese Americans, Japanese Americans, and European Americans. Journal of Applied Social Psychology. 2000;30(2):389–406. [Google Scholar]
- Cooper ML. Alcohol use and risky sexual behavior among college students and youth: Evaluating the evidence. Journal of Studies on Alcohol. 2002;(SUPPL14):101–117. doi: 10.15288/jsas.2002.s14.101. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Does drinking promote risky sexual behavior? A complex answer to a simple question. Current Directions in Psychological Science. 2006;15(1):19–23. [Google Scholar]
- Corbin WR, Fromme K. Alcohol use and serial monogamy as risks for sexually transmitted diseases in young adults. Health Psychology. 2002;21(3):229–236. doi: 10.1037//0278-6133.21.3.229. [DOI] [PubMed] [Google Scholar]
- Cousins G, McGee H, Layte R. Suppression effects of partner type on the alcohol-risky sex relationship in young Irish adults. Journal of Studies on Alcohol and Drugs. 2010;71(3):357–365. doi: 10.15288/jsad.2010.71.357. [DOI] [PubMed] [Google Scholar]
- Dermen KH, Cooper ML. Sex-related alcohol expectancies among adolescents: I. Scale development. Psychology of Addictive Behaviors. 1994;8(3):152–160. [Google Scholar]
- Dermen KH, Cooper ML. Inhibition conflict and alcohol expectancy as moderators of alcohol's relationship to condom use. Experimental and Clinical Psychopharmacology. 2000;8(2):198–206. doi: 10.1037//1064-1297.8.2.198. [DOI] [PubMed] [Google Scholar]
- Dermen KH, Cooper ML, Agocha VB. Sex-related alcohol expectancies as moderators of the relationship between alcohol use and risky sex in adolescents. Journal of Studies on Alcohol. 1998;59(1):71–77. doi: 10.15288/jsa.1998.59.71. [DOI] [PubMed] [Google Scholar]
- Donohew L, Zimmerman R, Cupp PS, Novak S, Colon S, Abell R. Sensation seeking, impulsive decision-making, and risky sex: implications for risk-taking and design of interventions. Personality and Individual Differences. 2000;28(6):1079–1091. [Google Scholar]
- Eaton D, Kann L, Kinchen S, Shanklin S, Flint K, Hawkins J, et al. Youth risk behavior surveillance-United States, 2011. MMWR Surveillance Summaries. 2012;61(4):1–162. [PubMed] [Google Scholar]
- Fielder RL, Carey KB, Carey MP. Are hookups replacing romantic relationships? A longitudinal study of first-year female college students. Journal of Adolescent Health. 2013;52(5):657–659. doi: 10.1016/j.jadohealth.2012.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George WH, Stoner SA, Norris J, Lopez PA, Lehman GL. Alcohol expectancies and sexuality: A self-fulfilling prophecy analysis of dyadic perceptions and behavior. Journal of Studies on Alcohol and Drugs. 2000;61(1):168. doi: 10.15288/jsa.2000.61.168. [DOI] [PubMed] [Google Scholar]
- Graham J, Olchowski A, Gilreath T. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prevention Science. 2007;8(3):206–213. doi: 10.1007/s11121-007-0070-9. [DOI] [PubMed] [Google Scholar]
- Guo J, Stanton B, Cottrell L, Clemens RL, Li X, Harris C, et al. Substance use among rural adolescent virgins as a predictor of sexual initiation. Journal of Adolescent Health. 2005;37(3):252–255. doi: 10.1016/j.jadohealth.2004.11.124. [DOI] [PubMed] [Google Scholar]
- Hammer JC, Fisher JD, Fitzgerald P, Fisher WA. When two heads aren't better than one: AIDS risk behavior in college-age couples. Journal of Applied Social Psychology. 1996;26(5):375–397. [Google Scholar]
- Hendershot CS, Magnan RE, Bryan AD. Associations of marijuana use and sex-related marijuana expectancies with HIV/STD risk behavior in high-risk adolescents. Psychology of Addictive Behaviors. 2010;24(3):404. doi: 10.1037/a0019844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hittner JB, Swickert R. Sensation seeking and alcohol use: A meta-analytic review. Addictive Behaviors. 2006;31(8):1383–1401. doi: 10.1016/j.addbeh.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Honaker J, King G, Blackwell M. Amelia II: A program for missing data. Journal of Statistical Software. 2011;45(7):1–47. [Google Scholar]
- Hoyle RH, Fejfar MC, Miller JD. Personality and Sexual Risk Taking: A Quantitative Review. Journal of Personality. 2000;68(6):1203–1231. doi: 10.1111/1467-6494.00132. [DOI] [PubMed] [Google Scholar]
- Humphrey JA, White JW. Women's vulnerability to sexual assault from adolescence to young adulthood. Journal of Adolescent Health. 2000;27(6):419–424. doi: 10.1016/s1054-139x(00)00168-3. [DOI] [PubMed] [Google Scholar]
- Justus AN, Finn PR, Steinmetz JE. The influence of traits of disinhibition on the association between alcohol use and risky sexual behavior. Alcoholism: Clinical and Experimental Research. 2000;24(7):1028–1035. [PubMed] [Google Scholar]
- Kahn JA, Kaplowitz RA, Goodman E, Emans SJ. The association between impulsiveness and sexual risk behaviors in adolescent and young adult women. Journal of Adolescent Health. 2002;30(4):229–232. doi: 10.1016/s1054-139x(01)00391-3. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Heckman T, Kelly JA. Sensation seeking as an explanation for the association between substance use and HIV-related risky sexual behavior. Archives of Sexual Behavior. 1996;25(2):141–154. doi: 10.1007/BF02437933. [DOI] [PubMed] [Google Scholar]
- Kiene SM, Barta WD, Tennen H, Armeli S. Alcohol, helping young adults to have unprotected sex with casual partners: Findings from a daily diary study of alcohol use and sexual behavior. Journal of Adolescent Health. 2009;44(1):73–80. doi: 10.1016/j.jadohealth.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingree J, Betz H. Risky sexual behavior in relation to marijuana and alcohol use among African-American, male adolescent detainees and their female partners. Drug and Alcohol Dependence. 2003;72(2):197–203. doi: 10.1016/s0376-8716(03)00196-0. [DOI] [PubMed] [Google Scholar]
- Kingree J, Braithwaite R, Woodring T. Unprotected sex as a function of alcohol and marijuana use among adolescent detainees. Journal of Adolescent Health. 2000;27(3):179–185. doi: 10.1016/s1054-139x(00)00101-4. [DOI] [PubMed] [Google Scholar]
- LaBrie J, Earleywine M, Schiffman J, Pedersen E, Marriot C. Effects of alcohol, expectancies, and partner type on condom use in college males: event-level analyses. Journal of Sex Research. 2005;42(3):259–266. doi: 10.1080/00224490509552280. [DOI] [PubMed] [Google Scholar]
- Lane SD, Cherek DR, Tcheremissine OV, Lieving LM, Pietras CJ. Acute marijuana effects on human risk taking. Neuropsychopharmacology. 2005;30(4):800–809. doi: 10.1038/sj.npp.1300620. [DOI] [PubMed] [Google Scholar]
- Lang AR. The social psychology of drinking and human sexuality. Journal of Drug Issues. 1985;15(2):273–289. [Google Scholar]
- Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV: Issues in methodology, interpretation, and prevention. American Psychologist. 1993;48(10):1035. doi: 10.1037//0003-066x.48.10.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh BC, Vanslyke JG, Hoppe MJ, Rainey DT, Morrison DM, Gillmore MR. Drinking and condom use: Results from an event-based daily diary. AIDS and Behavior. 2008;12(1):104–112. doi: 10.1007/s10461-007-9216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magid V, MacLean MG, Colder CR. Differentiating between sensation seeking and impulsivity through their mediated relations with alcohol use and problems. Addictive Behaviors. 2007;32(10):2046–2061. doi: 10.1016/j.addbeh.2007.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Carey MP, Carey KB, Gordon CM, Schum JL. Effects of alcohol and expectancies on HIV-related risk perception and behavioral skills in heterosexual women. Experimental and Clinical Psychopharmacology. 2004;12(4):288–297. doi: 10.1037/1064-1297.12.4.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh DR, Schroeder DG, Dearden KA, Sternin J, Sternin M. The power of positive deviance. British Medical Journal. 2004;329(7475):1177–1179. doi: 10.1136/bmj.329.7475.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles, CA: Muthén & Muthén; 1998–2013. [Google Scholar]
- Parks KA, Hsieh Y-P, Collins RL, Levonyan-Radloff K. Daily assessment of alcohol consumption and condom use with known and casual partners among young female bar drinkers. AIDS and Behavior. 2011;15(7):1332–1341. doi: 10.1007/s10461-010-9829-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson J. Personal control, self-efficacy in sexual negotiation, and contraceptive risk among adolescents: The role of gender. Sex Roles. 2006;54(9):615–625. [Google Scholar]
- Robbins JM, Krueger JI. Social projection to ingroups and outgroups: A review and meta-analysis. Personality and Social Psychology Review. 2005;9(1):32–47. doi: 10.1207/s15327957pspr0901_3. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation after 18+ years. Journal of the American Statistical Association. 1996;91(434):473–489. [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. New York: Chapman and Hall; 1997. [Google Scholar]
- Schafer JL. Multiple imputation: A primer. Statistical Methods in Medical Research. 1999;8(1):3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- Schalling D. Psychopathy-related personality variables and the psychophysiology of socialization. In: Hare RD, Schalling D, editors. Psychopathic behavior: Approaches to research. New York: Wiley; 1978. pp. 85–105. [Google Scholar]
- Schroder KE, Johnson CJ, Wiebe JS. An event-level analysis of condom use as a function of mood, alcohol use, and safer sex negotiations. Archives of Sexual Behavior. 2009;38(2):283–289. doi: 10.1007/s10508-007-9278-9. [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, Carey MP, Carey KB. Alcohol and risky sexual behavior among heavy drinking college students. AIDS and Behavior. 2010;14(4):845–853. doi: 10.1007/s10461-008-9426-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, Carey MP, Vanable PA, Senn TE, Coury-Doniger P, Urban MA. Alcohol consumption, drug use, and condom use among STD clinic patients. Journal of Studies on Alcohol and Drugs. 2009;70(5):762–770. doi: 10.15288/jsad.2009.70.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrier LA, Walls C, Lops C, Kendall AD, Blood EA. Substance use, sexual intercourse, and condom nonuse among depressed adolescents and young adults. Journal of Adolescent Health. 2012;50(3):264–270. doi: 10.1016/j.jadohealth.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skosnik PD, Spatz-Glenn L, Park S. Cannabis use is associated with schizotypy and attentional disinhibition. Schizophrenia Research. 2001;48(1):83–92. doi: 10.1016/s0920-9964(00)00132-8. [DOI] [PubMed] [Google Scholar]
- Smith A, Ferris JA, Simpson JM, Shelley J, Pitts MK, Richters J. Cannabis use and sexual health. Journal of Sexual Medicine. 2010;7(2pt1):787–793. doi: 10.1111/j.1743-6109.2009.01453.x. [DOI] [PubMed] [Google Scholar]
- Spitalnick JS, DiClemente RJ, Wingood GM, Crosby RA, Milhausen RR, Sales JM, et al. Brief report: Sexual sensation seeking and its relationship to risky sexual behaviour among African-American adolescent females. Journal of adolescence. 2007;30(1):165–173. doi: 10.1016/j.adolescence.2006.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele CM, Josephs RA. Alcohol myopia: Its prized and dangerous effects. American Psychologist. 1990;45(8):921. doi: 10.1037//0003-066x.45.8.921. [DOI] [PubMed] [Google Scholar]
- Swann WB, Silvera DH, Proske CU. On “knowing your partner”: Dangerous illusions in the age of AIDS? Personal Relationships. 1995;2(3):173–186. [Google Scholar]
- Verdejo-García A, Lawrence AJ, Clark L. Impulsivity as a vulnerability marker for substance-use disorders: review of findings from high-risk research, problem gamblers and genetic association studies. Neuroscience and biobehavioral reviews. 2008;32(4):777. doi: 10.1016/j.neubiorev.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Walsh JL, Fielder RL, Carey KB, Carey MP. Changes in women's condom use over the first year of college. Journal of Sex Research. 2012;50(2):128–138. doi: 10.1080/00224499.2011.642024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Dowdall GW, Davenport A, Rimm EB. A gender-specific measure of binge drinking among college students. American Journal of Public Health. 1995;85(7):982–985. doi: 10.2105/ajph.85.7.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annual Review of Sex Research. 2000;11:125–157. [PMC free article] [PubMed] [Google Scholar]
- Williams SS, Kimble DL, Covell NH, Weiss LH, Newton KJ, Fisher JD, et al. College students use implicit personality theory instead of safer sex. Journal of Applied Social Psychology. 1992;22(12):921–933. [Google Scholar]
- Wilson CM, Wright PF, Safrit JT, Rudy B. Epidemiology of HIV infection and risk in adolescents and youth. Journal of Acquired Immune Deficiency Syndromes. 2010;54(Suppl 1):S5. doi: 10.1097/QAI.0b013e3181e243a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Education & Behavior. 2000;27(5):539–565. doi: 10.1177/109019810002700502. [DOI] [PubMed] [Google Scholar]
- Wu LT, Ringwalt C, Patkar A, Hubbard R, Blazer D. Association of MDMA/ecstasy and other substance use with self-reported sexually transmitted diseases among college-aged adults: A national study. Public Health. 2009;123(8):557–564. doi: 10.1016/j.puhe.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan AF, Chiu YW, Stoesen CA, Wang MQ. STD-/HIV-related sexual risk behaviors and substance use among US rural adolescents. Journal of the National Medical Association. 2007;99(12):1386. [PMC free article] [PubMed] [Google Scholar]
- Zuckerman M, Buchsbaum MS, Murphy DL. Sensation seeking and its biological correlates. Psychological Bulletin. 1980;88(1):187. [Google Scholar]