Abstract
Background
Evidence indicates 12-step mutual-help organizations (MHOs), such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), can play an important role in extending and potentiating the recovery benefits of professionally-delivered addiction treatment among young adults with substance use disorders (SUD). However, concerns have lingered regarding the suitability of 12-step organizations for certain clinical subgroups, such as those with dual diagnosis (DD). This study examined the influence of diagnostic status (DD vs. SUD-only) on both attendance and active involvement (e.g., having a sponsor, verbal participation during meetings) in, and derived benefits from, 12-step MHOs following residential treatment.
Methods
Young adults (N = 296; 18-24 years old; 26% female; 95% Caucasian; 47% DD [based on structured diagnostic interview]), enrolled in a prospective naturalistic study of SUD treatment effectiveness, were assessed at intake, and 3, 6, and 12 months post-treatment on 12-step attendance/active involvement and percent days abstinent (PDA). T-tests and lagged, hierarchical linear models (HLM) examined the extent to which diagnostic status influenced 12-step participation and any derived benefits, respectively.
Results
For DD and SUD-only patients, post-treatment attendance and active involvement in 12-step organizations was similarly high. Overall, DD patients had significantly lower PDA relative to SUD-only patients. All patients appeared to benefit significantly from attendance and active involvement on a combined eight-item index. Regarding the primary effects of interest, significant differences did not emerge in derived benefit between DD and SUD-only patients for either attendance (p = .436) or active involvement (p = .062). Subsidiary analyses showed, however, that DD patients experienced significantly greater abstinence-related benefit from having a 12-step sponsor.
Conclusion
Despite concerns regarding the clinical utility of 12-step MHOs for DD patients, findings indicate that DD young adults participate and benefit as much as SUD-only patients, and may benefit more from high levels of active involvement, particularly having a 12-step sponsor. Future work is needed to clarify how active 12-step involvement might offset the additional recovery burden of a comorbid mental illness on substance use outcomes.
Keywords: dual diagnosis, 12-step participation, young adults
Introduction
Young adulthood (ages 18 to 25) represents a qualitatively distinct life stage marked by unique vulnerabilities to substance use (Arnett, 2005) and mental illness (Substance Abuse and Mental Health Services Administration, 2012a). For example, rates of substance use disorder (SUD) among young adults are about three times higher (21%) than adolescents or older adults (each at 7%; Substance Abuse and Mental Health Services Administration, 2012b). Thus it follows that young adults seeking recovery from SUD face greater challenges in finding recovery-supportive friends and environments (Kelly et al., 2012).
The Role of 12-Step Mutual-Help Organizations
An increased focus on addiction among young adults has been accompanied by examinations of specific recovery pathways, including 12-step mutual-help organizations (MHOs) such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA). They are the most common of all formal and informal recovery management options among individuals with SUD (Cohen et al., 2007, Compton et al., 2007) and are supported by a substantial and increasingly sophisticated research literature highlighting their role in helping patients maintain abstinence (Kaskutas, 2009, Gossop et al., 2007, Kelly et al., 2006, Magura et al., 2013) and reducing health care costs (Humphreys and Moos, 2007, Kelly and Yeterian, 2012, Mundt et al., 2012).
Although considerably more is known about whether adults benefit from participation, data also suggest that adolescents (Chi et al., 2009, Kelly et al., 2010a, Mundt et al., 2012) and young adults (Kelly et al., 2012, Delucchi et al., 2008) can benefit as well. However, due to broad clinical heterogeneity among those with SUD (Grant et al., 2004), more research is needed to clarify whether important clinical sub-groups derive more or less benefit from 12-step participation.
Research Examining Psychiatric Comorbidity in 12-Step Organizations
Despite increasing evidence that MHOs can be valuable treatment adjuncts (Humphreys, 2004), professional concerns have lingered regarding their fit for those with dual substance use and psychiatric diagnoses (i.e., dual diagnosis [DD]; Kelly et al., 2003, Bogenschutz et al., 2006, Timko, 2008). Such concerns include potential 12-step member opposition to psychotropic medications prescribed for the comorbid disorder (Tonigan and Kelly, 2004), which has traditionally been connected to the idea that any medication use will increase someone’s risk of addiction and relapse. In order to address these concerns, preliminary research has begun to investigate questions of whether individuals with psychiatric comorbidity attend, become actively involved, and derive benefit from MHOs such as AA and NA.
Some empirical comparisons of DD and SUD-only patients show that a comorbid mental illness may hinder positive outcomes. For example, patients with psychotic disorders tend to report lower levels of 12-step participation and benefit (Bogenschutz et al., 2006) while major depressive disorder (MDD) also appears to dampen 12-step effects among adult inpatients (Kelly et al., 2003). On the other hand, Kelly et al. (2006) found that 12-step attendance bolstered abstinence rates following outpatient treatment irrespective of diagnostic status and, among outpatients with concurrent SUD and MDD, 12-step attendance may improve drinking outcomes through reductions in depressive symptomatology (Worley et al., 2012). It also appears that among patients with comorbid posttraumatic stress disorder (PTSD), 12-step participation may have greater impact on targets of SUD treatment (e.g., problem-solving coping; Ouimette et al., 1998). More recent work showed that although social anxiety symptomatology did not predict attendance or active involvement among DD outpatients followed up to 2 years, it did predict equal or better response to 12-step participation (Timko et al., 2013). Also among adolescents, Grella, Joshi, and Hser (2004) found that DD, but not SUD-only patients experienced improved 1-year abstinence rates as a function of 12-step attendance. Investigating simultaneously outcomes at 3, 5, and 7 years post-treatment, Chi et al. (2013) found that DD adolescents were more engaged in 12-step groups, while both DD and SUD-only adolescents benefitted from 12-step attendance and active involvement over time.
Importantly, questions regarding the role of psychiatric comorbidity in 12-step participation and outcomes have not been investigated in young adult samples. While recent 12-step research has begun to consider not just attendance but also active involvement (e.g., having a sponsor, working steps, verbal participation at meetings, etc.; Cloud et al., 2004), an examination of the effects of involvement seems particularly critical for DD patients given their potential difficulties relating to others within the socially-rich milieu of 12-step groups.
Summary and Aims
Studies examining the role of DD in mutual help-related outcomes have yielded mixed results whereby some point to reduced benefit among those with DD (Kelly et al., 2003, Bogenschutz et al., 2006), some to analogous benefit (Kelly et al., 2006, Chi et al., 2013), and others to increased benefit (Grella et al., 2004, Timko et al., 2013). Despite this emerging literature on the role of DD in mutual-help participation, to our knowledge no studies have examined DD young adults – a large segment of the treated population. To these ends, the goals of the current study were to compare DD and SUD-only young adults on: 1) demographic, clinical, and substance use profiles at intake into residential treatment; 2) rates of 12-step attendance and active involvement in the year post-discharge; and 3) derived benefits from 12-step attendance and active involvement.
We expected that on average DD patients would have a more severe clinical profile at treatment intake, and would demonstrate lower levels of attendance and active involvement in 12-step organizations. Given the overall limited literature, prior mixed findings, and insufficient theoretical justifications, we made no a priori predictions about differences in their degree of derived benefit.
Methods
Participants
The current study is comprised of 296 young adults aged 18-24 (M age = 20.37) who attended a private not-for-profit residential SUD treatment program in the upper Midwestern United States. Participants were enrolled between October 2006 and April 2008. The sample was predominantly male (73.6%) and a substantial majority identified as Caucasian (94.9%). Roughly one-quarter were employed either full time (12.2%) or part-time (11.8%) and approximately one-third identified as students (32.1%). Many of the participants had completed high school or beyond, with 43.9% having earned a high school or graduate equivalency degree (GED) and 39.9% having at least completed some college. Just under half of the sample reported involvement in the criminal justice system (46.3%) and among respondents (n = 262), 69.5% reported a prior arrest.
Over one-half of the sample met criteria for each of alcohol (56.8%) and cannabis dependence (53.7%) in their lifetime, approximately 37% for cocaine dependence, and 27% for opioid dependence.
With respect to mental health comorbidity, 47.3% (n = 140) presented with dual substance use and mental health disorders (i.e., dual diagnosis [DD]). Roughly one-quarter met criteria for at least one mood disorder, including 15.5% for major depressive disorder (most with recurrent episodes; 12.2%), 8.8% for dysthymic disorder, and 2.4% for bipolar I/II disorder. Approximately one-third met criteria for at least one anxiety disorder, including 11.5% for generalized anxiety disorder, 10.5% for social phobia, 9.8% for posttraumatic stress disorder, 5.1% for specific phobia, 4.7% for obsessive-compulsive disorder, 3.4% for panic disorder, and 1.7% for agoraphobia/no panic disorder. Over 5% met criteria for an eating disorder. See Table 1 for a comparison of demographic characteristics by diagnostic status (DD vs. SUD-only).
Table 1.
Demographic, Substance Use, and Clinical Characteristics at Intake as a Function of Diagnostic Status: Dual Diagnosis (DD) vs. Substance Use Disorder-Only (SUD-Only) (N = 296)
| Diagnostic Status
|
χ2 | p | r | ||
|---|---|---|---|---|---|
| DD % | SUD-Only % | ||||
| Female | 40.00% | 14.10% | 25.50 | < .001 | .29 |
| Some college | 43.17% | 37.18% | 1.10 | .295 | .06 |
| Employeda | 33.73% | 41.51% | 1.19 | .275 | .08 |
| Arrestedb | 67.20% | 71.53% | 0.58 | .447 | .05 |
| Substance use hospitalization | 27.14% | 25.64% | 0.09 | .770 | .02 |
| Attending psychotherapyc | 47.14% | 31.41% | 7.69 | .006 | .16 |
| Taking medication | 60.00% | 34.62% | 19.11 | < .001 | .25 |
| Anti-depressant | 48.57% | 23.08% | 21.04 | < .001 | .27 |
| Anti-anxiety | 17.14% | 6.41% | 8.36 | .004 | .17 |
| Anti-psychotic | 2.14% | 0.64% | 1.25 | .264 | .07 |
| Mood stabilizer | 7.86% | 5.13% | .92 | .339 | .06 |
| Stimulant | 7.86% | 6.41% | .23 | .628 | .03 |
|
| |||||
| DD M (SD) | SUD-Only M (SD) | t | p | d | |
|
| |||||
| Age | 20.48 (1.68) | 20.27 (1.46) | 1.19 | .236 | .14 |
| Percent days abstinent | .26 (.29) | .22 (.27) | 1.04 | .297 | .12 |
| Substance use consequences | 71.40 (22.99) | 60.17 (25.10) | 4.00 | < .001 | .47 |
| Dependence severity | 19.91 (7.51) | 16.30 (8.56) | 3.84 | < .001 | .45 |
| Motivation | |||||
| Ambivalence | 10.65 (4.55) | 9.63 (4.21) | 2.01 | .045 | .23 |
| Recognition | 21.25 (9.41) | 19.02 (8.91) | 2.09 | .037 | .24 |
| Taking Steps | 25.96 (9.59) | 24.48 (8.95) | 1.37 | .173 | .16 |
| Commitment to sobrietyd | 24.10 (5.33) | 23.85 (5.22) | 0.42 | .678 | .05 |
| Self-efficacye | 38.50 (18.17) | 39.99 (16.91) | -0.72 | .470 | -.08 |
| Psychiatric symptoms | 67.42 (7.64) | 59.58 (10.51) | 7.39 | < .001 | .86 |
Note. Substantive interpretations for r, a measure of effect size reflecting magnitude of association between two variables (dichotomous in this case), include small = .1, medium = .3, and large = .5.
Note. Substantive interpretations for d, a measure of effect size for between-group comparisons, include small = .2, medium = .5, and large = .8.
n = 189.
n = 262.
n = 293.
n = 295.
n= 292.
Treatment
Treatment was philosophically consistent with the 12-step-based Minnesota model (McElrath, 1997) and supplemented with individual evidence-based approaches such as 12-step facilitation, cognitive-behavioral and motivational enhancement therapies. For more information on the residential treatment model see Kelly et al. (2012). On average, our sample remained in treatment for over 25 days and 84.5% were discharged with staff approval.
Procedure
A total of 607 young adults were admitted to the program during the recruitment period (six left prior to treatment onset). To ensure sufficient representation of all ages within the target range (18-24 years), a stratified sampling procedure was used such that all patients aged 21-24 years and every second patient aged 18-20 was approached for the study. Of those approached (n = 384), 64 declined to participate. Following enrollment, an additional 17 participants withdrew prior to data collection and one individual was excluded due to complications with informed consent. Assessments were conducted at treatment intake (i.e., baseline) as well as 3 months, 6 months, and 12 months after treatment discharge. This study features the sub-sample that completed a core assessment battery at treatment intake, including a structured diagnostic interview (n = 296). See Kelly et al. (2012) for further details regarding data collection methodology. Follow-up rates were 81.1% at 3 months (n = 240), 73.0% at 6 months (n = 219), and 70.3% at 12 months (n = 208). Diagnostic status was not associated with failure to complete any of the follow-up assessments (ps > .05). The study was conducted in accordance with the Institutional Review Board at Schulmann Associates IRB, an independent review board, and all participants signed informed consent documents.
Measures
Diagnostic status
Axis I mental illness was assessed with the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (SCID for DSM-IV; First et al., 2002). Individuals were included in the DD group if they met DSM-IV past-month criteria for a comorbid Axis I mood, anxiety, or eating disorder, excluding substance-induced disorders (lifetime criteria were used for more chronic conditions such as dysthymic disorder and generalized anxiety disorder). Attention-deficit/hyperactivity disorder, psychotic disorders, and personality disorders were not assessed; however, if an apparent psychotic episode occurred during the admission process, transfer to an inpatient psychiatric unit was arranged.
Psychological symptomatology
We used the short form of the Brief Symptom Inventory (BSI-18; Derogatis, 2001) to assess psychological symptomatology, yielding a global severity index (GSI). Participants rated symptomatic distress for 18 items on a 5-point scale and raw summary scores were converted to T-scores (M = 50; SD = 10). The measure has demonstrated adequate internal and test-retest reliability (coefficients = .74-.89) and construct validity in substance users (Wang et al., 2010).
Substance use
The Form-90 (Miller and Del Boca, 1994) was utilized to determine amount and frequency of use for alcohol and each of nine classes of illegal or pharmaceutical drugs. Modifications were made to subsequent assessments to capture the entire time period elapsed since the previous interview (i.e., averaging 60 days for the 3-month follow-up, 90 days for the 6-month follow-up, and 180 days for the 12-month follow-up). Thus, if a participant missed the 6-month follow-up, for example, he/she was asked to report on the time between 3 and 12-month follow-ups (a 9-month window).
Percent days abstinent (PDA) was calculated by dividing total abstinence days by the number of days in the assessment. The Form-90 has been tested with adult and adolescent samples and has demonstrated good test-retest reliability and validity (Slesnick and Tonigan, 2004, Tonigan et al., 1997).
To verify self-reported abstinence, saliva tests (Cone et al., 2002) assessing for the presence of tetrahydrocannibol (THC), cocaine metabolites, opiates, amphetamines, and phencyclidine (PCP), were administered on a sub-sample of participants that lived within 50 miles of the treatment facility and could attend follow-up interviews in-person (15%). Abstinence was confirmed in 97% of subjects who self-reported abstinence.
Severity of substance dependence
The Leeds Dependence Questionnaire (LDQ; Raistrick et al., 1994), a 10-item self-report measure, was used to determine dependence severity not specific to a particular substance. The measure has shown high internal consistency (α = .93) and construct validity in the current (Kelly et al., 2010b) and other samples (e.g., Lennings, 1999).
Substance use consequences
We used the Inventory of Drug Use Consequences – Recent Consequences (InDUC-2R; Tonigan and Miller, 2002) to assess psychosocial difficulties associated with alcohol and/or drug use (e.g., “I have felt guilty or ashamed because of my drinking or drug use”). The measure contains 50 self-report items rated in terms of 90 day-frequencies. The InDUC-2R has been shown to be sensitive to change and has good to excellent test-retest reliability (subscales ranging from r = .34 to .93; Tonigan and Miller, 2002).
Prior SUD hospitalizations, psychotherapy, and psychotropic medication
We used the Form-90 as above (Miller and Del Boca, 1994) to assess whether participants had been hospitalized at an inpatient setting for a substance use problem in the past year (n = 78; 26.4%) as well as whether the respondent was receiving psychotherapy (n = 115; 38.9%) or taking prescribed psychotropic medication (n = 138; 46.6%) in the 90 days prior to treatment entry.
Abstinence self-efficacy
The study used the Alcohol and Drug Use Self-Efficacy Scale (ADUSE), a self-report measure assessing participants’ confidence to abstain from alcohol and drugs in 20 common situations. It is based on a similar measure of only alcohol use which has good reliability and validity (DiClemente et al., 1994).
Motivation for changes in substance use
Motivation was assessed with the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES; Miller and Tonigan, 1996), a self-report measure, with two analogous 19-item scales inquiring separately about alcohol and other drugs. There are three empirically-derived subscales representing problem recognition (7 items), ambivalence (4 items), and taking steps (8 items). The minimum of each subscale for either set of alcohol or drug items was used in analyses as a conservative estimate of abstinence motivation. The subscales have demonstrated acceptable to high internal consistency and high test-retest reliability among adults (subscales ranging from r = .83 to .99; Miller and Tonigan, 1996) and concurrent and predictive validity among adolescents (Maisto et al., 2003).
Commitment to sobriety
An original scale assessed participants’ level of agreement with each of five items assessing this construct: “Staying sober is the most important thing in my life”; “I am totally committed to staying off of alcohol/drugs”; “I will do whatever it takes to recover from my addiction”; “I never want to return to alcohol/drug use again.”; “I have had enough alcohol and drugs”. The scale has demonstrated excellent internal consistency in the current sample (α = .89; Kelly et al., 2012).
12-step attendance and involvement
Patients reported 12-step participation at intake, 3, 6, and 12 months post-treatment, based on their engagement at AA, NA, Cocaine Anonymous (CA), and “Other” organizations during the time since last interview as with the Form-90. Percentage of days attending a meeting was determined by dividing the total sum of 12-step meetings attended by the total number of days in the assessment period. “Other” responses, when appropriate, were included in the sum of 12-step meetings (e.g., Marijuana Anonymous).
The Multidimensional Mutual-help Meeting Activity Scale (Kelly et al., 2011), provided in-depth information on mutual-help group participation across three dimensions: meeting participation (e.g., verbal participation); (ii) fellowship involvement (e.g., contact with sponsor outside of meetings); and step work (i.e., progress in working through the 12-step program of action). These data were used to derive a summary index of active involvement based on the sum of eight dichotomous indicators: consider yourself a member, have a sponsor, contacted your sponsor outside of meetings, contacted other members outside of meetings, read 12-step literature outside of meetings, talked or shared during meetings, helped to set up or run meetings, and completed any “action oriented” steps (either 4, 5, 8, 9, or 11). Internal consistency of the composite measure among the sample was excellent (α = 0.87 at intake, 0.88 at 3 and 6 months, and 0.95 at 12 months).
Analysis Plan
First, we conducted a series of independent t- and χ2 tests to compare DD and SUD-only participants at treatment intake on demographic characteristics as well as clinical (e.g., whether in psychotherapy), substance use (PDA), and related psychological phenomena (e.g., motivation to change substance use). Then, we conducted t-tests to examine whether rates of 12-step attendance or active involvement over time (intake and 3-month, 6-month, and 12-month follow-ups) were different for DD and SUD-only participants.
Next we conducted two lagged-panel hierarchical linear models (HLM), one each for attendance and involvement, to examine the following predictors of PDA: a) the main effect of diagnostic status, b) the main effects of attendance/active involvement, and c) whether diagnostic status moderated the effect of attendance/active involvement, captured quantitatively by the interaction (e.g., diagnostic status by 12-step attendance/active involvement). To ensure temporal precedence of the independent variables of interest and thus bolster causal inference (Kazdin and Nock, 2003), analyses were lagged such that attendance/active involvement at 3-month and 6-month follow-ups simultaneously predicted PDA at 6-month and 12-month follow-ups, respectively.
In order to identify and control for potential alternative explanations of the primary effects, we first used univariate regression to examine relationships among demographic characteristics, intake levels of relevant psychological constructs (e.g., motivation), and prior mutual-help/treatment (e.g., 12-step engagement, professional SUD treatment, psychotherapy, and psychopharmacology) with a) PDA and b) failure to complete at least one follow-up assessment. Variables associated with 6-month or 12-month PDA at α = .10 included age, having attended some college, prior SUD hospitalization, motivation (SOCRATES Recognition and Taking Steps), commitment to sobriety, self-efficacy, identifying as a 12-step member, and sponsor contact. Variables associated with failure to complete the 3-month, 6-month, or 12-month follow-up at α = .10 included being female, having never attended college, length of treatment stay, engagement in psychotherapy, and not identifying as a 12-step member. Each of the variables associated with PDA or failure to complete an assessment were included in a stepwise regression model. Variables associated with PDA that remained significant at α = .05 were included as covariates in the HLMs, while those associated with failure to complete an assessment were included as covariates irrespective of their observed significance level in the stepwise regression model. Baseline PDA was also retained as a covariate in both models.
We then tested two HLMs – one for 12-step attendance and one for active involvement – using Proc MIXED. Appropriate covariance structures were determined using likelihood ratio test comparisons. Given that PDA was considerably skewed, a negative log transformation was used to successfully reduce skewness.
Results
Group Differences on Substance Use and Clinical Characteristics at Treatment Intake
Baseline comparisons of DD and SUD-only groups indicated that DD patients had more severe substance use histories (Table 1). The groups had similar baseline PDA (26% vs. 22%, respectively), however, substance use consequences (InDUC-2R; d = .47) and substance dependence severity (LDQ; d = .45) were significantly higher among DD patients. Also, while the groups’ commitment to sobriety and abstinence self-efficacy were similar, DD young adults reported greater motivation to change their substance use; this included significantly higher mean levels of Recognition (d = .24) and Ambivalence (d = .23).
As anticipated, with respect to psychiatric profiles at treatment intake, DD patients had substantially greater psychiatric symptoms (GSI; d = .86) and were significantly more likely to be in therapy (47% vs. 31%) and taking psychotropic medication (60% vs. 35%).
12-Step Participation and Associations with Diagnostic Status
Attendance
Overall, there was an initial increase from baseline to 3 months in percent days attending a 12-step meeting, which attenuated somewhat at each of the 6-month and 12-month follow-ups (Figure 1). However, these attendance rates did not differ significantly as a function of diagnostic status (DD vs. SUD-only) at either intake (i.e., 0 months; 8% vs. 8%), 3-month (50% vs. 50%), 6-month (38% vs. 41%), or 12-month follow-ups (29% vs. 29%) (all ps > .05).
Figure 1.
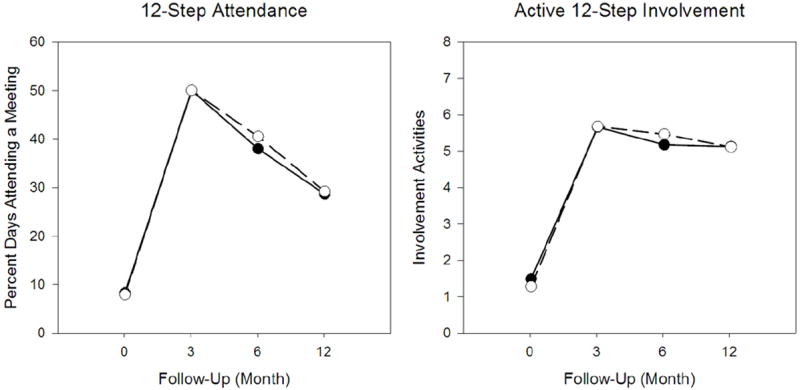
The associations between 12-step attendance (percent days attending a meeting; left panel) and active 12-step involvement (number of activities; right panel) at treatment intake (i.e., 0 months) and 3-month, 6-month, and 12-month follow-up assessments as a function of diagnostic status. No significant differences emerged between dual diagnosis (DD) and substance use disorder-only (SUD-Only) patients for either form of participation at any time point.
Involvement
A similar pattern emerged for active 12-step involvement (Figure 1). Again, these rates of involvement did not differ significantly as a function of diagnostic status at intake or any of the follow-ups (ps> .05).
Does Diagnostic Status Moderate the Effects of 12-Step Participation on PDA?
Results of the HLMs (Table 2) showed that there was a significant negative effect of diagnostic status on PDA for both the attendance and active involvement models, indicating that DD patients experienced lower overall abstinence during the follow-up periods. In addition, as previously shown (Kelly et al, 2012), there were significant positive main effects of 12-step attendance and active involvement on PDA indicating that increased levels of attendance and involvement were associated with higher abstinence rates after controlling for confounds.
Table 2.
Influence of Diagnostic Status on Lagged Associations between 12-Step Attendance/Active Involvement and Percent Days Abstinent
| Attendance
|
Active Involvement
|
|||||||
|---|---|---|---|---|---|---|---|---|
| b | SE | F | p | b | SE | F | p | |
| Demographics | ||||||||
| Gender | -0.413 | 0.22 | 3.68 | 0.057 | -0.474 | 0.21 | 5.17 | 0.024 |
| Education | 0.409 | 0.19 | 4.84 | 0.029 | 0.451 | 0.18 | 6.28 | 0.013 |
| Baseline Covariates | ||||||||
| Percent days abstinent | -0.002 | 0.13 | 0.00 | 0.986 | -0.006 | 0.12 | 0.00 | 0.964 |
| Substance use hospitalization | -0.704 | 0.20 | 12.15 | 0.001 | -0.628 | 0.20 | 10.12 | 0.001 |
| Identifies as 12-step member | 0.161 | 0.21 | 0.58 | 0.448 | 0.148 | 0.21 | 0.52 | 0.474 |
| Commitment to sobriety | 0.087 | 0.02 | 21.55 | < 0.001 | 0.066 | 0.19 | 12.36 | 0.001 |
| Length of treatment stay | 0.008 | 0.02 | 0.14 | 0.712 | 0.011 | 0.02 | 0.28 | 0.595 |
| Attending psychotherapy | 0.118 | 0.19 | 0.40 | 0.527 | -0.009 | 0.19 | 0.00 | 0.959 |
| Main Model | ||||||||
| Time | -0.359 | 0.11 | 10.67 | 0.001 | -0.396 | 0.11 | 13.69 | < 0.001 |
| Attendance/Involvement (A/I) | 0.992 | 0.32 | 12.24 | 0.001 | 0.202 | 0.04 | 22.65 | < 0.001 |
| Diagnostic Status | -0.564 | 0.28 | 4.19 | 0.042 | -0.973 | 0.37 | 6.79 | 0.010 |
| Diagnostic Status * A/I | 0.345 | 0.44 | 0.61 | 0.436 | 0.109 | 0.06 | 3.52 | 0.062 |
Note. Dichotomous effects were coded as follows: gender (male = 1); education (some college = 1); substance use hospitalization (yes = 1); identifies as 12-step member (yes = 1); attending psychotherapy (yes = 1); diagnostic status (dual diagnosis = 1).
Note. Attendance/Involvement (A/I) variables were lagged relative to percent days abstinent (PDA) such that these effects examined simultaneously the associations between 3-month and 6-month attendance/active involvement and 6-month and 12-month PDA, respectively.
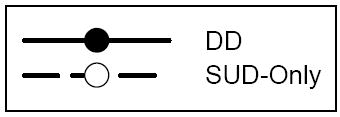
Assessing for the presence of moderation, the interaction term revealed that attendance-related benefits did not differ as a function of diagnostic status (p = 0.436). Although a somewhat larger difference between DD and SUD-only patients emerged in the active involvement model, the moderating influence of diagnostic status did not reach statistical significance (p = .062). In order to elucidate this effect, we split attendance and active involvement into “high” and “low” categories based on median values across 3-month and 6-month follow-ups and examined raw PDA means as a function of diagnostic status (Figure 2). Descriptively, at lower levels of active involvement (6 or fewer activities) DD patients had lower PDA than SUD-only patients at the 12-month follow-up (67.2% vs. 82.3%, respectively). However, there was no such disadvantage at higher levels of active involvement (89.3% vs. 90.4%, respectively). Thus, relative to SUD-only patients, DD patients appeared to show similar benefit from 12-step participation and, despite an overall disadvantage, may have similar abstinence outcomes if actively involved at higher levels.
Figure 2.
Percent days abstinent (PDA) for dual diagnosis (DD) relative to substance use disorder-only (SUD-Only) participants as a function of median split attendance (i.e., “high” attendance reflected at least 43% days attending a meeting; left panel) and median split involvement (i.e., “high” involvement reflected 7 or 8 activities; right panel) during the prior follow-up period (e.g., 3-month and 6-month participation). For attendance, 56.1% and 42.3% of DD patients and 59.7% and 41.3% of SUD-only patients were in the high group at 3-month and 6-month follow-ups, respectively. For active involvement, 53.5% and 49.0% of DD patients and 51.6% and 51.8% of SUD-only patients were in the high group at 3-month and 6- month follow-ups, respectively. Lower PDA for DD individuals in both graphs reflects a main effect of diagnostic status. Greater PDA for all patients high in participation reflects a main effect of 12-step attendance (left panel) and active involvement (right panel). Overall, DD and SUD-only patients show similar associations between attendance and abstinence. Although the graph suggests relative to their SUD-only counterparts, DD patients with low active involvement had worse PDA and DD patients with high active involvement had similar PDA, the moderating effect of diagnostic status did not reach statistical significance (p = .062).
In addition, having attended some college, no prior SUD hospitalization, greater commitment to sobriety, and greater self-efficacy were all independently associated with higher PDA in both attendance and active involvement models, and being female in the latter model only.
Subsidiary Analyses
In order to explore if specific aspects of involvement were significantly associated with PDA, we ran eight identical HLMs, one for each of the eight involvement activities as primary predictors in lieu of the overall index, addressing the problem of multiple significance testing by controlling for the expected false discovery rate as described by Benjamini and Hochberg (1995). Moderation tests suggested that the effects of having a sponsor and sponsor contact on PDA were significantly greater for DD patients (ps = .033 and .048, respectively). None of the other moderation analyses were significant (ps > .05).
Discussion
The current paper investigated the impact of psychiatric comorbidity on the relationship between 12-step participation and substance use abstinence in a naturalistic, prospective study of young adult inpatients. Results suggested that both attendance and active involvement predicted higher subsequent rates of abstinence. Regarding the influence of diagnostic status, despite worse abstinence rates over time, DD patients were found to benefit similarly from 12-step attendance compared to SUD-only patients. They appeared to benefit somewhat (but non-significantly) more from high levels of involvement, whereby their outcomes were comparable to those of SUD-only patients.
There were marked clinical differences between DD and SUD-only young adults at treatment intake. Despite similar intake levels of abstinence, DD patients had experienced higher levels of psychosocial consequences and dependence symptomatology. Consistent with expectations, they also reported more severe psychiatric problems and were more likely to have been in psychotherapy and taking psychotropic medication. This pattern is similar to the adult sample in Timko et al. (2010), where psychiatric problems—but not substance use—differed as a function of diagnostic status, the Ouimette et al. (1998) sample where DD patients endorsed more psychological distress at intake, and the Grella et al. (2004) adolescent sample where DD patients required more extensive mental health services during treatment. Additionally, in keeping with higher prevalence rates of mood and anxiety disorders among women (see Kessler et al., 2005), the DD group contained a significantly higher percentage of females, while lower abstinence rates among women are consistent with findings reported by Witbrodt and Delucchi (2011).
While it follows that DD patients were better able to recognize having a problem, they did not evidence more frequent patterns of 12-step attendance or active involvement. This stands in contrast to a younger adolescent sample, where DD patients attended 12-step groups at higher rates (Grella et al., 2004), but was consistent with Timko et al. (2010) where DD and SUD-only adults reported similar rates of meeting attendance, identification as a 12-step member, having a sponsor, and working steps. Clinicians working at the 12-step-oriented residential treatment program attended by this sample may have been especially skilled at facilitating 12-step involvement irrespective of patients’ baseline motivation. Nevertheless, findings here indicate that young adult DD patients with mostly concurrent depressive and anxiety disorders can participate at rates similar to SUD-only individuals.
Relative to SUD-only patients, DD patients showed analogous improvement as a function of attendance and active involvement. Despite evidencing worse overall abstinence rates across the follow-up periods, at high levels of involvement (i.e., engagement in seven or eight 12-step activities), outcomes rivaled those of their SUD-only counterparts. The contrast between an apparent interaction graphically and a statistically nonsignificant finding may be explained by lack of statistical power. For example, in their analysis of approximately 1400 patients, Ouimette et al. (1998) found that the group of patients with comorbid PTSD/SUD showed greater clinical benefit from 12-step involvement than the SUD-only group. Thus, while 12-step involvement appears to buttress recovery (see also Kelly et al., 2012, Delucchi et al., 2008) for DD and SUD-only young adults alike, future work may clarify whether it helps offset worse SUD outcomes related to the increased disease burden of comorbid psychiatric illness.
As a clinical corollary, prior research points to “Making AA Easier” as a particularly effective 12-step-facilitation intervention for patients higher in psychiatric severity (Kaskutas and Oberste, 2002, Kaskutas et al., 2009). The protocol also dedicates an entire session to sponsorship, which the current study suggests may be a key factor in improving outcomes for DD patients. The precise reason for a more pronounced abstinence-related benefit from sponsorship is unclear, though we speculate that greater emotional distress conferred by the psychiatric illness may be associated with greater problem recognition, and, in turn, more motivation to follow their sponsor’s advice (e.g., avoiding high-risk situations), an attitude not directly measured. Given a prior contradictory finding among DD adults (Timko et al., 2010), however, future work is needed to clarify the relationship between sponsorship and psychiatric comorbidity.
In combination with extant literature, our study suggests psychiatric severity and patient age should be considered in contextualizing research on DD and 12-step participation for clinical purposes. For example, patients with primarily less severe depressive or anxiety disorders may benefit from 12-step participation (e.g., Ouimette et al., 2000) while those with more severe variants of psychopathology may affiliate less readily and/or derive less benefit (e.g., psychotic disorders; Bogenschutz et al., 2006). In addition, while older DD patients likely struggle with a more substantial accumulation of psychosocial impairment secondary to chronic mental illness (e.g., Kelly et al., 2003) younger DD patients (e.g., Grella et al., 2004, Chi et al., 2013) may still possess the ability to tap into AA and NA’s socially-grounded mechanisms of action (Kelly et al., 2011). In fact, psychiatric distress appears to be motivating and may be a potential catalyst for both formal and informal help-seeking behaviors (Finney and Moos, 1995). Of note in the current study, post-hoc exploratory analyses (not shown) revealed that when significant associations between baseline psychiatric severity and 12-step participation were present, they consistently favored patients with greater psychiatric impairment.
Limitations
First, results from our study of primarily Caucasian participants may not generalize to other racial or ethnic groups. Second, despite the use of structured diagnostic interviews (i.e., SCID), the complex interplay between substance use and psychiatric disturbance (e.g., substance-induced symptoms) raises some concerns about the validity of diagnoses so early in the treatment process. Moreover, diagnostic interviews did not assess for psychotic or personality disorders. Therefore, we cannot compare young adults to previous work with adults that showed reduced participation and benefit among patients with psychotic disorders (Bogenschutz et al., 2006), nor can we speak to the potential influence of character pathology in these domains (Cacciola et al., 2001). Third, our study was silent regarding perceived saliency of the comorbid psychiatric illness (primary or secondary to SUD). Although one could speculate that dually-focused 12-step groups (e.g., Laudet et al., 2004) may be a better fit than SUD-only focused groups like AA and NA for individuals with an identified primary psychiatric illness, matching hypotheses have yet to be tested. Fourth, the influence of professional continuing care options (e.g., outpatient SUD treatment, psychotherapy, psychopharmacological interventions, etc.) on abstinence rates among DD patients was not examined here, and warrant more thorough investigation. Fifth, the equivocal validity of self-reported substance use/abstinence (verified by drug test in only 15% of the overall sample) and 12-step participation are also worth mentioning. While it is possible that missed follow-up assessments may reflect current, unmeasured substance use, this limitation was partially addressed by statistical control for those demographic and intake characteristics associated with failure to complete a follow-up assessment (e.g., gender). Finally, while care was taken to conduct a controlled, lagged, prospective design in order to assess the independent effect of 12-step participation on later outcome, our non-experimental design cannot completely eradicate alternative explanations for benefits attributed to 12-step attendance and involvement.
Conclusions
Young adulthood is the period of highest risk for the development of SUD and the presence of a current comorbid psychiatric problem increases the psychological burden for about half of all patients in SUD treatment (Grella et al., 2004, Chi et al., 2013, Timko et al., 2010). Such individuals are likely to pose additional clinical challenges to treatment staff, both in terms of symptomatology and more pronounced life difficulties. Thus, crafting individualized recovery management plans for these patients is vital. This study provides preliminary evidence that facilitating active involvement in widely accessible 12-step MHOs is clinically appropriate for young adult DD patients in early recovery. Clinicians, therefore, may wish to facilitate DD patients’ engagement in 12-step MHOs, as active involvement in particular may help offset potentially worse substance use outcomes related to the added burden of a comorbid psychiatric illness.
Acknowledgments
This work was funded by 1R21AA018185-01A2 and by an anonymous donation for youth research to the Hazelden Foundation.
Dr. Hoeppner’s participation is supported by NIDA grant K01DA027097
Dr. Kelly’s participation is supported by NIAAA grant 1R21AA018185-01A2
Contributor Information
Brandon G. Bergman, Center for Addiction Medicine, Massachusetts General Hospital and Harvard Medical School, Boston MA
M. Claire Greene, Center for Addiction Medicine, Massachusetts General Hospital, Boston, MA
Bettina B. Hoeppner, Center for Addiction Medicine, Massachusetts General Hospital and Harvard Medical School, Boston, MA
Valerie Slaymaker, Hazelden Foundation, Center City, MN
John F. Kelly, Center for Addiction Medicine, Massachusetts General Hospital and Harvard Medical School, Boston, MA
References
- Arnett JJ. The developmental context of substance use in emerging adulthood. Journal of Drug Issues. 2005;35:235–254. [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. Series B (Methodological) 1995;57:289–300. [Google Scholar]
- Bogenschutz MP, Geppert CMA, George J. The role of 12-step approaches in dual-diagnosis treatment and recovery. The American Journal on Addictions. 2006;15:50–60. doi: 10.1080/10550490500419060. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, McKay JR, Rutherford MJ. Psychiatric comorbidity in patients with substance use disorders: Do not forget axis II disorders. Psychiatric Annals. 2001;31:321–331. [Google Scholar]
- Chi FW, Kaskutas LA, Sterling S, Campbell CI, Weisner C. Post-treatment 12-step involvement and 3-year outcomes among adolescents with substance use problems: Social support and religiosity as mediators. Addiction. 2009;104:927–939. doi: 10.1111/j.1360-0443.2009.02524.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi FW, Sterling S, Campbell CI, Weisner C. Twelve-step participation and outcomes over seven years among adolescent substance use patients with and without psychiatric comorbidity. Substance Abuse. 2013;34:33–42. doi: 10.1080/08897077.2012.691780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloud RN, Ziegler CH, Blondell RD. What is Alcoholics Anonymous Affiliation? Substance Use & Misuse. 2004;39:1117–1136. doi: 10.1081/ja-120038032. [DOI] [PubMed] [Google Scholar]
- Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2007;86:214–221. doi: 10.1016/j.drugalcdep.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Cone EJ, Presley L, Lehrer M, Seiter W, Smith M, Kardos KW, Fritch D, Salamone S, Niedbala RS. Oral fluid testing for drugs of abuse: positive prevalence rates by Intercept immunoassay screening and GC-MS-MS confirmation and suggested cutoff concentrations. Journal of analytical toxicology. 2002;26:541–546. doi: 10.1093/jat/26.8.541. [DOI] [PubMed] [Google Scholar]
- Delucchi KL, Matzger H, Weisner C. Alcohol in emerging adulthood: 7-year study of problem and dependent drinkers. Addictive Behaviors. 2008;33:134–142. doi: 10.1016/j.addbeh.2007.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR. Administration, scoring, and procedures manual. NCS Pearson; Minneapolis, MN: 2001. BSI-I8: Brief Symptom Inventory 18. [Google Scholar]
- DiClemente CC, Carbonari JP, Montgomery RPG, Hughes SO. The Alcohol Abstinence Self-Efficacy scale. Journal of Studies on Alcohol. 1994;55:141–148. doi: 10.15288/jsa.1994.55.141. [DOI] [PubMed] [Google Scholar]
- Finney JW, Moos RH. Entering treatment for alcohol abuse: A stress and coping model. Addiction. 1995;90:1223–1240. doi: 10.1046/j.1360-0443.1995.90912237.x. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P), Biometrics Research. New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- Gossop M, Stewart D, Marsden J. Attendance at Narcotics Anonymous and Alcoholics Anonymous meetings, frequency of attendance and substance use outcomes after residential treatment for drug dependence: A 5-year follow-up study. Addiction. 2007;103:119–125. doi: 10.1111/j.1360-0443.2007.02050.x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grella CE, Joshi V, Hser Y. Effects of comorbidity on treatment processes and outcomes among adolescents in drug treatment programs. Journal of Child & Adolescent Substance Abuse. 2004;13:13–32. [Google Scholar]
- Humphreys K. Circles of recovery: Self-help organizations for addictions. Cambridge University Press; Cambridge, UK: 2004. [Google Scholar]
- Humphreys K, Moos R. Can encouraging substance abuse patients to participate in self-help groups reduce demand for continuing care services: 2-year clinical and utilization outcomes. Alcoholism: Clinical and Exerimental Research. 2007;31:64–68. doi: 10.1111/j.1530-0277.2006.00273.x. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA. Alcoholics Anonymous effectiveness: Faith meets science. Journal of Addictive Diseases. 2009;28:145–157. doi: 10.1080/10550880902772464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Oberste E. Making Alcoholics Anonymous Easier. [June 1, 2012]; Available at: http://www.ebcrp.org/sites/default/files/MAAEZ_Manual.pdf.
- Kaskutas LA, Subbaraman MS, Withrodt J, Zemore SE. Effectiveness of Making Alcoholics Anonymous Easier: A group format 12-step facilitation approach. Journal of Substance Abuse Treatment. 2009;37:228–239. doi: 10.1016/j.jsat.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Dow SJ, Yeterian JD, Kahler CW. Can 12-step group participation strengthen and extend the benefits of adolescent addiction treatment? A prospective analysis. Drug and Alcohol Dependence. 2010a;110:117–125. doi: 10.1016/j.drugalcdep.2010.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Magill M, Slaymaker V, Kahler C. Psychometric validation of the Leeds Dependence Questionnaire (LDQ) in a young adult clinical sample. Addictive Behaviors. 2010b;35:331–336. doi: 10.1016/j.addbeh.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, McKellar JD, Moos R. Major depression in patients with substance use disorders: Relationship to 12-Step self-help involvement and substance use outcomes. Addiction. 2003;98:499–508. doi: 10.1046/j.1360-0443.2003.t01-1-00294.x. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Stout R, Zywiak W, Schneider R. A 3-year study of addiction mutual-help group participation following intensive outpatient treatment. Alcoholism: Clinical and Exerimental Research 30. 2006 doi: 10.1111/j.1530-0277.2006.00165.x. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Stout RL, Slaymaker V. Emerging adults’ treatment outcomes in relation to 12-step mutual-help attendance and involvement. Drug and Alcohol Dependence. 2012 doi: 10.1016/j.drugalcdep.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Urbanoski KA, Hoeppner BB, Slaymaker V. Facilitating comprehensive assessment of 12-step experiences: A Multidimensional Measure of Mutual-Help Activity. Alcoholism Treatment Quarterly. 2011;29:181–203. doi: 10.1080/07347324.2011.586280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Yeterian JD. Empirical awakening: The new science on mutual help and implications for cost containment under health care reform. Substance Abuse. 2012;33:85–91. doi: 10.1080/08897077.2011.634965. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Laudet AB, Magura S, Cleland CM, Vogel HS, Knight EL, Rosenblum A. The effect of 12-step based fellowship participation on abstinence among dually diagnosed persons: A 2-year longitudinal study. Journal of Psychoactive Drugs. 2004;36:207–216. doi: 10.1080/02791072.2004.10399731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennings CJ. An evaluation of the Leeds Dependence Questionnaire. Journal of Child & Adolescent Substance Abuse. 1999;8:73–87. [Google Scholar]
- Magura S, McKean J, Kosten S, Tonigan JS. A novel application of propensity score matching to estimate Alcoholics Anonymous’ effect on drinking outcomes. Drug and Alcohol Dependence. 2013;129:54–59. doi: 10.1016/j.drugalcdep.2012.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Chung TA, Cornelius JR, Martin CS. Factor structure of the SOCRATES in a clinical sample of adolescents. Psychology of Addictive Behaviors. 2003;17:98–107. doi: 10.1037/0893-164x.17.2.98. [DOI] [PubMed] [Google Scholar]
- McElrath D. The Minnesota Model. Journal of Psychoactive Drugs. 1997;29:141–144. doi: 10.1080/02791072.1997.10400180. [DOI] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol SUPPL. 1994;12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS. Assessing drinkers’ motivation for change: The stages of change readiness and treatment eagerness scale (SOCRATES) Psychology of Addictive Behaviors. 1996;10:81–89. [Google Scholar]
- Mundt MP, Parthasarathy S, Chi FW, Sterling S, Campbell CI. 12-step participation reduces medical use costs among adolescents with a history of alcohol and other drug treatment. Drug and Alcohol Dependence. 2012;126:124–130. doi: 10.1016/j.drugalcdep.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouimette PC, Ahrens C, Moos RH, Finney JW. During treatment changes in substance abuse patients with posttraumatic stress disorder: The influence of specific interventions and program environments. Journal of Substance Abuse Treatment. 1998;15:555–564. doi: 10.1016/s0740-5472(97)00315-2. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Moos RH, Finney JW. Two-year mental health service use and course of remission in patients with substance use and posttraumatic stress disorders. Journal of Studies on Alcohol. 2000;61:247–253. doi: 10.15288/jsa.2000.61.247. [DOI] [PubMed] [Google Scholar]
- Raistrick D, Bradshaw J, Tober G, Weiner J, Allison J, Healey C. Development of the Leeds Dependence Questionnaire (LDQ): a questionnaire to measure alcohol and opiate dependence in the context of a treatment evaluation package. Addiction. 1994;89:563–572. doi: 10.1111/j.1360-0443.1994.tb03332.x. [DOI] [PubMed] [Google Scholar]
- Slesnick N, Tonigan JS. Assessment of Alcohol and Other Drug Use by Runaway Youths: A Test-Retest Study of the Form 90. Alcoholism Treatment Quarterly. 2004;22:21–34. doi: 10.1300/J020v22n02_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Mental Health Findings, Substance Abuse and Mental Health Services Administration. Rockville, MD: 2012a. NSDUH Series H-45, HHS Publication No. (SMA) 12-4725. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings, Substance Abuse and Mental Health Services Administration. Rockville, MD: 2012b. NSDUH Series H-44, HHS Publication No. (SMA) 12-4713. [Google Scholar]
- Timko C. Outcomes of AA for special populations, in Research on Alcoholics Anonymous and spirituality in addiction recovery. In: GALANTER M, KASKUTAS LA, editors. Recent developments in alcoholism., Research on Alcoholics Anonymous and spirituality in addiction recovery Recent developments in alcoholism. Springer Science + Business Media; New York, NY: 2008. pp. 373–392. [DOI] [PubMed] [Google Scholar]
- Timko C, Cronkite RC, McKellar J, Zemore S, Moos RH. Dually diagnosed patients’ benefits of mutual-help groups and the role of social anxiety. Journal of Substance Abuse Treatment. 2013;44:216–223. doi: 10.1016/j.jsat.2012.05.007. [DOI] [PubMed] [Google Scholar]
- Timko C, Sutkowi A, Moos R. Patients with dual diagnoses or substance use disorders only: 12-step group participation and 1-year outcomes. Substance Use & Misuse. 2010;45:613–627. doi: 10.3109/10826080903452421. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Kelly JF. Beliefs about AA and the use of medications: A comparison of three groups of AA-exposed alcohol dependent persons. Alcoholism Treatment Quarterly. 2004;22:67–78. [Google Scholar]
- Tonigan JS, Miller WR. The Inventory of Drug Use Consequences (InDUC): Test-retest reliability and sensitivity to detect change. Psychology of Addictive Behaviors. 2002;16:165–168. [PubMed] [Google Scholar]
- Tonigan JS, Miller WR, Brown JM. The reliability of Form 90: An instrument for assessing alcohol treatment outcome. Journal of Studies on Alcohol. 1997;58:358–364. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- Wang J, Kelly BC, Booth BM, Falck RS, Leukefeld C, Carlson RG. Examining factorial structure and measurement invariance of the Brief Symptom Inventory (BSI)-18 among drug users. Addictive Behaviors. 2010;35:23–29. doi: 10.1016/j.addbeh.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witbrodt J, Delucchi K. Do women differ from men on Alcoholics Anonymous participation and abstinence? A multi-wave analysis of treatment seekers. Alcoholism: Clinical and Experimental Research. 2011;35:2231–2241. doi: 10.1111/j.1530-0277.2011.01573.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worley MJ, Tate SR, Brown SA. Mediational relations between 12-step attendance, depression and substance use in patients with comorbid substance dependence and major depression. Addiction. 2012;107:1974–1983. doi: 10.1111/j.1360-0443.2012.03943.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


