Abstract
Introduction
Lower-risk drinking is increasingly being examined as a treatment outcome for some patients following addiction treatment. However, few studies have examined the relationship between drinking status (lower-risk drinking in particular) and health care utilization and cost which has important policy implications.
Methods
Participants were adults with alcohol dependence and/or abuse diagnoses who received outpatient alcohol and other drug treatment in a private, non-profit integrated health care delivery system and had a follow-up interview 6-months after treatment entry (N=995). Associations between past 30-day drinking status at 6 months (abstinence, lower-risk drinking defined as non-abstinence and no days of 5+ drinking, and heavy drinking defined as one or more days of 5+ drinking) and repeated measures of at least one emergency department (ED), inpatient or primary care visit and their costs over 5 years were examined using mixed effects models. We modeled an interaction between time and drinking status to examine trends in utilization and costs over time by drinking group.
Results
Heavy drinkers and lower-risk drinkers were not significantly different from the abstainers in their cost or utilization at time 0 (i.e. 6 months post intake). Heavy drinkers had increasing odds of inpatient (p<.01) and ED (p<.05) utilization over 5 years compared to abstainers. Lower-risk drinkers and abstainers did not significantly differ in their service use in any category over time. No differences were found in changes in primary care use among the three groups over time. The cost analyses paralleled the utilization results. Heavy drinkers had increasing ED (p<.05) and inpatient (p<.001) costs compared to the abstainers; primary care costs did not significantly differ. Lower-risk drinkers did not have significantly different medical costs compared to those who were abstinent over 5 years. However, post-hoc analyses found lower-risk drinkers and heavy drinkers to not significantly differ in their ED use or costs over time.
Conclusion
Performance measures for treatment settings that consider treatment outcomes may need to take into account both abstinence and reduction to non-heavy drinking. Future research should examine whether results are replicated in harm reduction treatment, or whether such outcomes are found only in abstinence-based treatment.
Keywords: lower-risk drinking, costs, health care utilization, alcohol outcomes, alcohol treatment
INTRODUCTION
An increasingly important clinical and policy question regarding alcohol and other drug (AOD) treatment is whether lower-risk drinking should be considered as a treatment outcome, in addition to abstinence. The NIAAA guidelines define “low-risk” drinking as having no more than 4 drinks on any one day and 14 drinks/week for men and no more than 3 drinks on any one day and 7 drinks/week for women. The combined cutoffs are ideal; however, research has shown that the daily limits are an adequate substitute(Dawson, 2000), and are used as proxies for the combined measures in this paper. We refer to drinking within these limits as “lower-risk” drinking.
Several factors must be considered when evaluating lower-risk drinking as a potential treatment outcome, including the long-term prognosis (i.e., drinking, psychosocial functioning, health care utilization, and costs) for individuals with an alcohol use disorder who are able to achieve lower-risk drinking following treatment – especially compared to individuals who achieved abstinence. The current study is the second of two companion studies, the first of which compared 12-month drinking and psychosocial outcomes of lower-risker and heavy drinkers versus abstainers at 6 months post-treatment (Kline-Simon et al., 2013). In this study we examine how these groups compare on health care utilization and costs over 5 years.
Historically, there has been debate about whether individuals with dependence can attain sustainable “moderate drinking” (Marlatt, 1983; Sobell and Sobell, 1995b; Sobell and Sobell, 2006). More recent findings using relatively large sample sizes have been mixed with regard to the long-term prognosis of lower-risk drinkers. Maisto and colleagues (2007) in a study of 952 Project MATCH participants, for example, found that non-problem drinkers (defined as using alcohol but having no alcohol use disorder problems) at 1 year post-treatment had less stable positive drinking outcomes over time than abstainers, whereas several studies of both general and treatment populations found that low-risk drinkers, based on NIAAA low-risk drinking limits, have social functioning outcomes similar to those of abstainers (Cunningham, 1999; Dawson and Grant, 2011; Kline-Simon et al., 2013). In a general population study of individuals in remission from alcohol use disorders Dawson et al. (2007) found that those who exceeded low-risk drinking daily limits had higher odds of recurrence of alcohol dependence, impaired driving, and liver disease a year later, with implications for increased health services utilization and cost. As mentioned above, in our prior study, using the same sample, we examined the relationship between past 30-day drinking status (i.e., abstinence, lower-risk drinking, and heavy drinking) at 6 months post-treatment, and drinking status and psychosocial outcomes 12 months post-treatment (Kline-Simon et al., 2013). Abstainers and those with no recent 5+ drinking days both had better drinking outcomes than heavy drinkers (with at least one recent 5+ drinking day), though the abstinent group had much higher odds of positive drinking outcomes (i.e., no heavy drinking) than the lower-risk drinkers. Furthermore, both the abstinent and lower-risk drinking groups had significantly lower psychiatric severity and family/social problem severity than heavy drinkers at 12 months post-treatment. These findings indicate that lower-risk drinkers had positive social outcomes similar to those in the abstinent group in this sample. However, we know little about the utilization and costs over time, which are important aspects to health systems.
The relationship of post-AOD treatment drinking status to health care utilization (particularly use of ED, inpatient and primary care) has significant health policy implications. High costs have been found for patients just prior to AOD treatment (mostly from avoidable hospitalizations and ED visits) (Booth et al., 1997; Holder, 1987; Holder et al., 1992), but the literature comparing post-treatment drinking status with health care utilization and cost is sparse. Zywiak et al. (1999) found that substance use patients abstinent for 24 months following AOD treatment had lower utilization than those who relapsed. A 5-year study of individuals with alcohol or drug disorders in a private treatment sample found that abstainers had higher primary care costs, and similar inpatient costs, over time compared to non-abstainers (Parthasarathy and Weisner, 2005), but lower-risk drinking was not studied. Although the health and addiction fields have begun to recognize the value of social and health outcomes of treatment that may be related to lower-risk drinking, little research has been conducted to examine health care costs associated with this outcome.
This study adds to the literature on long-term utilization and costs of treatment outcomes for patients with alcohol disorders. It compares the service use and costs of abstinence, lower-risk drinking, and heavy drinking over time. The treatment sample consists of individuals entering abstinence-based specialty treatment for alcohol use disorders in a large private, nonprofit, integrated health care system. Based on earlier findings from this sample and other literature, we expect that the utilization and costs for the lower-risk drinkers and abstainers will be comparable, and that they will both be lower than those of heavy drinkers over the 5-year period. The findings will increase our knowledge about lower-risk drinking outcomes, and will inform clinical policy regarding the outcomes for which treatment programs should be held accountable.
METHODS
Study Participants
We conducted a secondary analysis of adult chemical dependency patients (aged 18 and older) using data collected from two prior studies conducted in Kaiser Permanente Northern California (KPNC). KPNC is a non-profit, integrated health care delivery system providing health care to over 3.4 million members. The AOD treatment program provides group-based outpatient and day treatment modalities that include supportive group therapy, education, relapse prevention, family therapy and individual counseling in a model similar to other abstinence-based, group-format private and public programs.
The two studies were conducted from 1994–1996 and 1997–1998. The Day Hospital Study compared day hospital treatment to traditional outpatient treatment, and the Integrated Care Study examined integrated delivery of medical and addiction services. Reports have been published detailing the two studies (Weisner et al., 2000; Weisner et al., 2001). Treatments for both studies were the same and the average length of stay was also the same (10 weeks). For both studies, telephone interviews at intake and follow-ups collected data on demographics, alcohol and drug use, severity of related problems and out-of-health plan service use. Patients who did not agree to be randomized but agreed to other aspects of the study were consented, followed, and included in the analyses. These datasets were combined and analyzed together as has been done previously in other studies (Chi et al., 2011; Satre et al., 2007; Satre et al., 2004; Tsoh et al., 2011; Weisner et al., 2010a; Weisner et al., 2010b). Variables indicating study sample and randomization status were added to all models to control for potential study effects.
The sample for the current study consists of patients in the two studies who met criteria for alcohol abuse or dependence at intake, and were interviewed again 6 months after treatment entry (n=995). We included individuals with either abuse or dependence since evidence suggests a continuum of alcohol use disorders rather than “abuse” as distinct from “dependence” (Li et al., 2007), and this is consistent with proposed changes to the Diagnostic and Statistical Manual of Mental Disorders-V (DSM-V), which combines abuse and dependence into one “alcohol use disorder” diagnosis (American Psychiatric Association, 2010).
Measures
Demographic variables measured at intake included age, gender, marital status, income, and ethnicity. Length of stay in treatment was measured in weeks from intake.
Severity of psychiatric and medical problems were measured by the psychiatric and medical composite scores of the Addiction Severity Index (ASI) instrument (McLellan et al., 1992) at intake. These continuous measures were included in the models to control for problem severity at intake.
We used the Diagnostic Interview Schedule for Psychoactive Substance Dependence to provide a DSM-IV diagnosis for alcohol, marijuana, stimulant, painkiller, methadone, heroin, barbiturate, tranquilizer, inhalant, hallucinogen, and cocaine dependence. Our sample included only those with alcohol dependence or abuse diagnoses; thus we created a count variable of the number of alcohol dependence or abuse diagnostic criteria met at intake. A dichotomous marker indicated drug dependence (other than alcohol) at intake.
Categories of drinking status at the 6 month follow-up were: 1) abstinence from alcohol during the prior 30 days; 2) lower-risk drinking, defined as non-abstinence and no days of 5+ drinking during the prior 30 days; and 3) heavy drinking, defined as one or more days of 5+ drinking during the prior 30 days.
Utilization
Inpatient episode, emergency department (ED) and primary care visit (adult medicine, family practice or OBGYN) data were obtained from Kaiser Permanente’s automated databases (Mertens et al., 2005; Selby, 1997). Utilization measures were aggregated in 6-month intervals from 6 months post treatment intake over 5 years. Indicator variables were created for any inpatient episode, ED visit, or primary care visit. Count variables for the number of inpatient episodes, ED visits, and primary care visits in the year prior to treatment intake were included in the appropriate models as controls. To account for the varying length of enrollment in the health plan, the total number of member months was included as a covariate.
Costs
Cost data were obtained from the Kaiser Permanente (KP) electronic databases (Parthasarathy and Weisner, 2005; Parthasarathy et al., 2001; Selby, 1997). Costs for services provided within KP were extracted from the Cost Management Information System, which integrates utilization data with the financial ledger. Costs for outside services paid for by KP were obtained from the billing/claims department. Costs for services not paid for by KP (including costs incurred by study participants after they left KP) were excluded. Inpatient, ED and non-emergency primary care costs were calculated in 6-month intervals from 6 months post treatment intake over 5 years. KP’s membership database provided length of enrollment in the health plan which was also summarized in 6-month intervals for this time period. To account for varying lengths of enrollment in the health plan among different risk-drinking categories, average costs per member month were calculated. Average costs per member month for the year prior to intake was included in the models as controls.
Analysis
All analyses were performed using SAS© software version 9.3; statistical significance was defined at p < 0.05. There were 10 repeated measures, measured in 6 month intervals, for each outcome measure: any ER use, any inpatient use, any primary care use, and the corresponding average costs per member month. We used frequencies and means to summarize the demographic and baseline characteristics of the sample and the drinking groups by these patient characteristics. We used chi-square tests to examine differences between the groups and the categorical variables, and t-tests to examine differences in the means of the continuous covariates. We used a repeated measures mixed-models framework to examine the effects of the explanatory variables on the participants’ longitudinal patterns of service utilization and average costs per member month over time, while allowing the initial status (i.e., intercept) to vary for every subject. The utilization measures (any inpatient episodes, ED visits or primary care visits coded 0/1) were dichotomized into indicators of any use (=1) vs. no use (=0). For these dichotomous outcomes, we used a mixed-effects logistic model with a random intercept. This model is represented as log[Pr(Yij=1)/(1- Pr(Yij=1))]= BXij + μi where Yij =1 if individual i had a visit at time point j, B represents a set of fixed-effect coefficients associated with a vector of covariates X (including time, drinking group and group by time interactions) and μi denotes the random subject effects distributed with mean 0 and variance σμ2). We first estimated a simple logistic regression model without accounting for correlation between error terms. The parameter estimates from this initial model were used as starting values for the non-linear mixed model procedure to ensure convergence of the likelihood function during estimation. The substantive findings did not differ when examining discrete and continuous measures of time; thus, we presented the results of models with time as a continuous variable. For the continuous outcomes (average inpatient, ED, and primary care costs per member month), we fitted linear mixed-effects models (Hedeker, 2005; Hedeker and Gibbons, 2006). The odds ratios and retransformed costs for each service were then calculated for all time points and graphed to illustrate the trends in service use and costs by drinker status.
All cost and utilization models controlled for individual characteristics known to have an impact on service use and cost (Parthasarathy and Weisner, 2005), including demographics, baseline medical and psychiatric severity, length of stay in treatment, drug dependence, and number of alcohol abuse/dependent symptoms. We also controlled for randomization status and study type as mentioned previously. In these models, the intercept represents the value of the outcomes (e.g. average ER cost) at initial status (6 months post-treatment) for the reference group (i.e. abstinent group). The main effect for time represents the linear time effect for the reference group (i.e. abstainers). The coefficient for drinker status (i.e., main effects for lower-risk and heavy drinkers) represents the value of the model outcome (e.g. average ER cost) for that drinker status covariate compared to the reference group (i.e., abstinence) at time 0 (6 months). The drinking status by time interaction terms indicate differences in cost and utilization trajectories by drinking status over 5 years post-intake, controlling for individual characteristics. The odds ratios for these interaction terms are calculated as follows for heavy drinkers: exp (coefficient for heavy drinker main effect + (coefficient for heavy drinker by time interaction term) x time). Due to the highly skewed nature of costs data, we examined both untransformed and log-transformed average costs and found the log-transformations to be a better fit. A US $1 value was first added to all individual costs before applying the logarithmic transformation, in order to include those who had zero costs in the analysis (Kondalsamy-Chennakesavan et al., 2011; Manning et al., 2005; Montez-Rath et al., 2006; Parthasarathy et al., 2001). A smearing estimator was then applied to the coefficients to retransform them back to the original scale as detailed in Duan et al. (1983).
RESULTS
Demographic Characteristics
Of the sample, 37% were women, 48% were married, 42% reported annual household incomes over $40,000, 30% had co-occurring drug use disorders, and the mean age was 39 (SD=11.1). The mean number of alcohol dependence or abuse symptoms was 6.8 and the average length of stay in treatment was 10 weeks (SD=14.7) (not shown). Sixty-six percent were abstinent at 6 months (n=660), 14% were lower-risk drinkers (n=137), and 20% were heavy drinkers (n=198). Heavy drinkers were younger, more likely to be men, and less likely to be married at intake compared to the other drinking groups (all p<.01). Abstainers had higher incomes and longer average treatment lengths of stay compared to the other drinking groups (all p<.01). The 6-month drinking groups did not differ on other patient characteristics (Table 1).
Table 1.
Demographic Variables at Intake by Six-Month Drinking Status
| Variables | Mean or % | Mean or % | Mean or % | p-Value |
|---|---|---|---|---|
|
| ||||
| Abstinence (n=660) | Lower-Risk Drinking (n=137) | Heavy Drinking (n=198) | ||
|
|
||||
| Women (%) | 39.1 | 48.2 | 28.3 | <.001 |
| Age, mean (SD) | 40.5 (10.8) | 39.6 (11.5) | 37.3 (10.6) | <.01 |
| Income (40,000+) (%) | 45.21 | 37.96 | 34.01 | <.01 |
| Ethnicity (%) | ||||
| Caucasian | 77.74 | 77.37 | 76.02 | |
| African American | 8.69 | 10.95 | 10.2 | |
| Hispanic | 8.54 | 8.76 | 9.18 | |
| Other | 5.03 | 2.92 | 4.59 | ns |
| Married (%) | 51.29 | 51.82 | 34.01 | <.0001 |
| Weeks in treatment, mean (SD) | 14.4 (16.8) | 4.0 (6.6) | 3.7 (5.2) | <.0001 |
| Drug dependence (%) | 27.12 | 35.77 | 31.82 | ns |
| Number of alcohol abuse/dep symptoms, mean (SD) | 6.8 (2.0) | 7.0 (2.0) | 7.1 (1.9) | ns |
| ASI psychiatric severity, mean (SD) | 0.42 (0.3) | 0.42 (0.3) | 0.38 (0.3) | ns |
| ASI medical severity, mean (SD) | 0.32 (0.4) | 0.34 (0.4) | 0.31 (0.4) | ns |
| Member months, mean (SD) | 41.3 (18.0) | 37.8 (20.2) | 35.1 (20.6) | <.001 |
Analysis of Utilization
Table 2 displays the results of the repeated measures, mixed-effects multivariate logistic regression models examining the relationship between drinking status at 6 months and any ED, any inpatient and any primary care over 5 years. There was a significant negative time effect in all three utilization models indicating a declining trend over 5 years for all three utilization measures for the reference (abstinent) group (ED Adj. OR=0.88; Inpatient Adj. OR= 0.90; Primary Care Adj. OR=0.93; all p<.01). The main effects for drinker status were not significant in any of the utilization models, indicating that utilization did not differ by drinker status at time 0 (i.e. the 6 month follow-up).
Table 2.
Mixed-Effects Logistic Models of Any Emergency Department, Any Inpatient and Any Primary Care Use Over 5 Years Post Intake
| Emergency Department Use | Inpatient Episode | Primary Care Use | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Coefficient | SE | p-Value | Coefficient | SE | p-Value | Coefficient | SE | p-Value | |
| Intercept | −4.976 | 0.37 | <.001 | −6.109 | 0.44 | <.001 | −4.743 | 0.29 | <.001 |
| Time | −0.125 | 0.03 | <.001 | −0.107 | 0.04 | <.01 | −0.073 | 0.02 | <.01 |
| Lower-Risk drinking at 6M | 0.069 | 0.21 | ns | 0.180 | 0.24 | ns | 0.052 | 0.17 | ns |
| Heavy drinking at 6M | −0.029 | 0.19 | ns | −0.375 | 0.23 | ns | 0.029 | 0.15 | ns |
| Alcohol abstinence at 6M | - | - | - | - | - | - | - | - | - |
| Lower-Risk drinking x time interaction | 0.056 | 0.07 | ns | −0.087 | 0.09 | ns | 0.021 | 0.06 | ns |
| Heavy drinking x time interaction | 0.140 | 0.06 | <.05 | 0.218 | 0.08 | <.01 | −0.038 | 0.05 | ns |
+ All models control for patient demographics, drug dependence at intake, psychiatric and medical severity at intake, treatment length of stay, number of abuse/dependence alcohol symptoms, 1 year pre-treatment utilization, length of enrollment, study type and randomization status
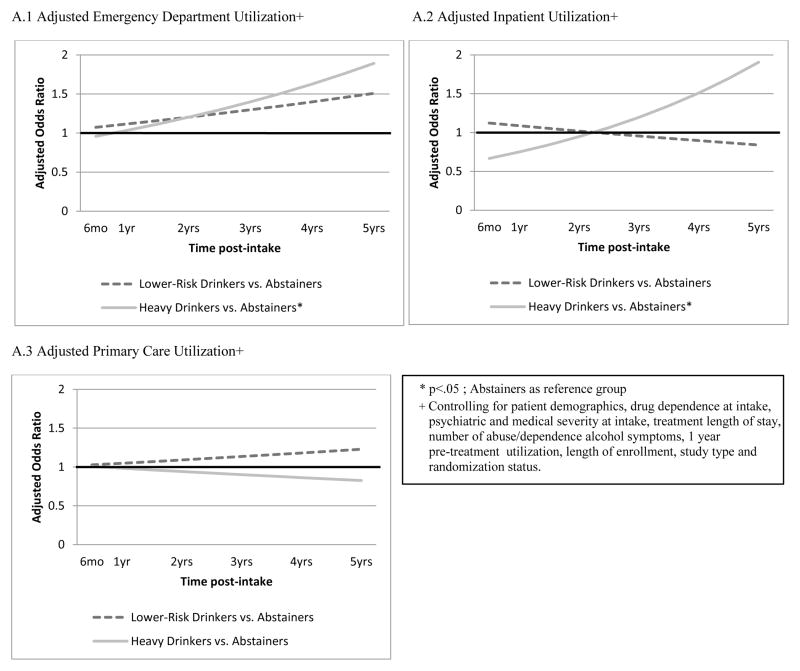
We found a positive heavy drinker group by time interaction for inpatient use, indicating that heavy drinker’s inpatient use increased over 5 years compared to abstainers (p<.01). They also had increasing ED utilization over time compared to abstainers (p<.05); heavy drinkers did not significantly differ from abstainers in terms of primary care use over time. Lower-risk drinkers and abstainers did not significantly differ in odds of service use over 5 years for any of the three services examined (p > .05). Figures A.1 through A.3 present graphs of the adjusted odds ratios for ED, inpatient and primary care utilization across the 5-year follow-up period by 6-month drinking status. Heavy drinkers (p<.05) and lower-risk drinkers (ns) had increasing odds of ED use and both had similar odds of primary care use (ns) compared to abstainers over time. Heavy drinkers had increasing odds of inpatient use (p<.01) over time while lower-risk drinkers (ns) had marginally lower odds compared to abstainers over time.
Figure A.
Adjusted Odds Ratios of Utilization by 6-Month Drinking Group Over Time
Direct comparisons between heavy drinkers and lower-risk drinkers showed that lower-risk drinkers had decreased inpatient service use over time (p < .05), relative to heavy drinkers but had similar ED use and primary care use (p >.05) (not shown).
Analysis of Costs
Table 3 presents the multivariate analyses for ED, inpatient, and primary care costs. As in the utilization models, all three cost models had a significant negative time effect, indicating that the costs for the reference group (abstainers) decreased over the 5 year period (ED, p<.001; inpatient and primary care, p<.05). The main effects for the drinker status variables (lower-risk and heavy drinker) were again not significant indicating that lower-risk and heavy drinkers did not have significantly different average ED, inpatient or primary care costs per member month at time 0 (6 months post intake) compared to abstainers.
Table 3.
Linear Mixed-Effects Models of Log-Transformed Emergency Department, Inpatient and Primary Care Costs Over 5 Years Post Intake
| Emergency Department Cost | Inpatient Cost | Primary Care Cost | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Coefficient | SE | p-Value | Coefficient | SE | p-Value | Coefficient | SE | p-Value | |
| Intercept | 0.330 | 0.17 | ns | 0.027 | 0.17 | ns | 1.637 | 0.21 | <.0001 |
| Time | −0.040 | 0.01 | <.001 | −0.036 | 0.02 | <.05 | −0.033 | 0.02 | <.05 |
| Lower-Risk drinking at 6M | −0.002 | 0.10 | ns | 0.104 | 0.12 | ns | −0.069 | 0.13 | ns |
| Heavy drinking at 6M | −0.016 | 0.09 | ns | −0.181 | 0.11 | ns | −0.076 | 0.12 | ns |
| Alcohol abstinence at 6M | - | - | - | - | - | - | - | - | - |
| Lower-Risk drinking x time interaction | 0.037 | 0.03 | ns | −0.043 | 0.04 | ns | 0.032 | 0.04 | ns |
| Heavy drinking x time interaction | 0.062 | 0.03 | <.05 | 0.101 | 0.04 | <.001 | −0.049 | 0.04 | ns |
+ All models control for patient demographics, drug dependence at intake, psychiatric and medical severity at intake, treatment length of stay, number of abuse/dependence alcohol symptoms, 1 year pre-treatment costs, study type and randomization status
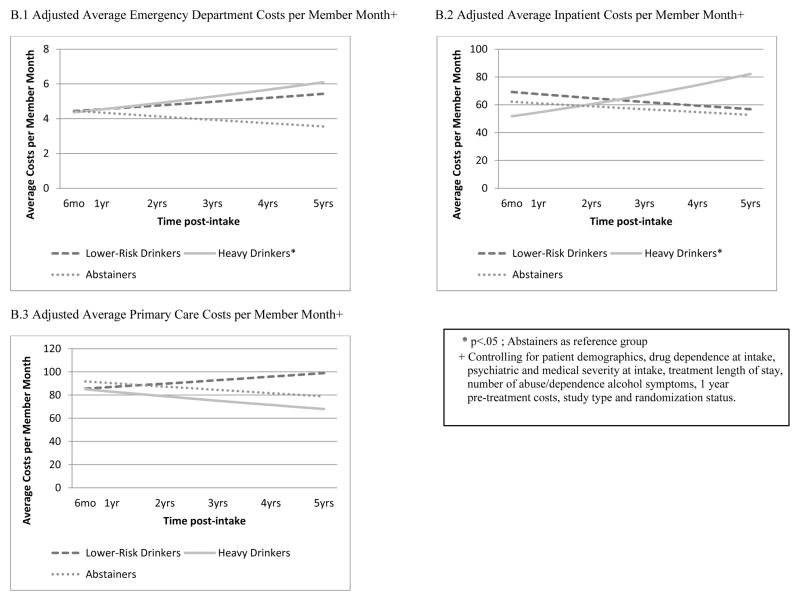
Similar to the utilization results, in the cost models there was a significant heavy drinker and time interaction in the inpatient (p<.001) and ED (p<.05) cost models indicating that the costs increased for heavy drinkers compared to abstainers over 5 years; primary care costs did not differ. Lower-risk drinkers did not differ from abstainers in costs over time for any of the three services examined. Figures B.1 through B.3 present graphs of the adjusted costs for ED, inpatient and primary care costs across the 5-year follow-up period by 6-month drinking status. Heavy drinkers had increasing ED (p<.05) and inpatient (p<.001) costs and lower average primary care costs (ns) per member month over 5 years compared to abstainers. Lower-risk drinkers had higher ED (ns), primary care (ns) and inpatient (ns) average costs per member month compared to abstainers though they had similar trends over time.
Figure B.
Adjusted Average Costs per Member Month by 6-Month Drinking Group Over Time
As before, using heavy drinkers as the reference group, we found that lower-risk drinkers had higher inpatient costs compared to heavy drinkers at time 0 (i.e. 6 months) (p<.05), however they had a decreasing cost trajectory (p<.05) over 5 years indicating that this effect diminished over time as heavy drinkers’ costs significantly increased. There were no significant differences in ED or primary care costs over time between lower-risk and heavy drinkers (p>.05) (not shown).
DISCUSSION
Our purpose was to inform clinical and treatment policy by comparing utilization and cost over 5 years for patients who were abstinent, lower-risk or heavy drinkers 6 months after beginning alcohol and other drug (AOD) treatment. We were particularly interested in inpatient and ED services, as they are costly and proxies of poor treatment outcomes and ill health. We found that those who were lower-risk drinkers at 6 months did not significantly differ from abstainers in any service use examined (ED, inpatient or primary care) across the 5-year follow-up, while heavy drinkers had increasing odds of inpatient and ED use and costs over time compared to abstainers.
In post-hoc comparison models using heavy drinkers as the reference group, we found that both the lower-risk drinkers and abstainers had higher inpatient use at 6 months than heavy drinkers. However, the drinker status (both for abstainers and lower-risk drinkers) and time interactions were negative and significant suggesting that although abstainers and lower-risk drinkers had higher odds of inpatient use at 6 months, the effect diminished over 5 years when controlling for important covariates such as age and gender. ED use and costs between heavy drinkers and abstainers were not significantly different at 6 months, but the abstainer group and time interaction was negative and significant indicating a decrease in ED use for abstainers over time compared to heavy drinkers. Surprisingly, we did not find significant differences in ED use or costs between the lower-risk drinking group and heavy drinkers. As mentioned previously, at 6 months after AOD treatment, lower-risk drinkers and heavy drinkers did not differ significantly from abstinent individuals in primary care use or costs after adjusting for patient characteristics. This is not surprising because a health policy issue for AOD treatment is to help patients change their medical utilization behavior, and to use more preventive primary and well-care rather than urgent or emergency care (Mertens et al., 2008; Weisner et al., 2001).
Our prior work found that abstainers and lower-risk drinkers at 6 months had similar 12-month psychosocial outcomes, including psychiatric, family/social and employment problem outcomes; lower-risk drinkers also had better 12-month medical severity outcomes (p<.05) compared to abstainers (Kline-Simon et al., 2013). Moreover, both the lower-risk and abstinent groups did better than the heavy drinking groups on these outcomes. These findings, combined with findings in the present study indicating the lack of significant differences in cost and utilization outcomes between lower-risk drinkers and abstainers, adds additional support for considering lower-risk drinking as a potential treatment outcome. At the same time, we note that our prior study (Kline-Simon et al., 2013) found that lower-risk drinkers had better psychosocial outcomes than heavy drinkers, but abstainers did have higher odds of positive drinking outcomes (i.e., no heavy drinking) than the heavy and lower-risk drinking groups.
The study has several limitations. Telephone interview data were used across all time points, which could have led to self-report bias. Some women may have been misclassified as lower-risk drinkers (defined by NIAAA as 4+ drinks for women) because of the current study’s definition of heavy drinking as 5+ drinks for men and women (4+ was not available in the dataset, and the only measure of actual number of drinks consumed each day was regarding the number of days drinking 5+). Future research would benefit from measuring a combined variable of days drinking and typical number of drinks consumed. We note that the assignment to the three drinking categories was based on clinically meaningful benchmarks as well as prior work; this resulted in unbalanced group sizes. We acknowledge that cost and utilization data are likely less sensitive to actual differences in outcomes than are alcohol use measures, which we examined in our prior analysis (Kline-Simon et al., 2013). In addition, we also note that significant differences in outcomes between treatment groups (Kline-Simon et al., 2013) are often not replicated in cost analyses due to the high variance in cost distributions. Although many longitudinal outcome and cost studies use 30-day time frames to enhance recall (McDermott et al., 1996; Murphy et al., 2010; Sobell and Sobell, 1995a), we acknowledge that assessing initial drinking patterns over a longer period at the 6-month follow-up might have produced different relationships with subsequent drinking statuses, utilization, and cost.
The study sample was drawn from a private integrated health care delivery system which may not be representative of public or other private health care populations. However, it is a system where all services can be examined, and its epidemiologic and program characteristics are similar to other AOD treatment programs. A large number of health plans are organized similarly, including the 19 health plans of the HMO Research Network (HMO Research Network, 2005). Further, generalizability of the health plan will increase substantially as health reform (the Affordable Care Act) is implemented (Blumenthal and Tavenner, 2010; Mental Health America), which targets integration in private and public health care. In particular, it provides resources to public Federally Qualified Health Centers to integrate health care and behavioral health care (Blumenthal and Tavenner, 2010; McDermott et al., 1996; Mental Health America, 2011; Murphy et al., 2010; Sobell and Sobell, 1995a).
As the AOD treatment program is abstinence-based, our findings reflect outcomes for individuals who did not receive interventions aimed at lower-risk drinking. Studying a program where interventions are focused on lower-risk drinking as an outcome might have different findings. Also, this was an observational study and clearly it is not possible to randomize participants to drinker status. However, we adjusted for differences in the groups by controlling for patient characteristics. Finally, as with any longitudinal study, some sample attrition occurred, although at a lesser rate than many other studies. At the 5-year follow-up, membership rates were lower for heavy drinkers (57%) compared to the abstinent (70%) and lower-risk drinking (65%) groups. We addressed this by using length of enrollment in the health plan in the utilization model, and by using average cost per member month in multivariate cost analyses. However, we note that there are unobservable variables (i.e. poor functioning) that may account for differences in both attrition and service use.
Conclusion
This study adds to the small number of studies on lower-risk drinking and health services utilization and cost in an AOD treatment setting; further research is warranted, particularly from different health systems and populations. The findings that lower-risk drinkers did not differ from those of abstinent individuals, in inpatient use in particular, even when controlling for patient characteristics, suggests that a health policy perspective may consider benefits of lower-risk drinking. Future research should examine whether results are replicated in samples of older patients who are more sensitive to alcohol’s effects at lower drinking levels. Research is also needed on whether the findings are replicated in patients from harm reduction treatment, or whether such outcomes are found only in abstinence-based treatment.
Acknowledgments
This study was supported by grants from the National Institute on Alcoholism and Alcohol Abuse Grant (R37 AA10359) and the National Institute on Drug Abuse (R37 DA10572). We thank Agatha Hinman, BA for editorial assistance.
References
- American Psychiatric Association. R 00 Alcohol Use Disorder. [Accessed Oct 30, 2012.];DSM-5 Development. 2010 Available at http://www.dsm5.org/ProposedRevision/Pages/proposedrevision.aspx?rid=452.
- Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363:501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- Booth BM, Blow FC, Cook CA, Bunn JY, Fortney JC. Relationship between inpatient alcoholism treatment and longitudinal changes in health care utilization. J Stud Alcohol. 1997;58:625–637. doi: 10.15288/jsa.1997.58.625. [DOI] [PubMed] [Google Scholar]
- Chi FW, Parthasarathy S, Mertens JR, Weisner CM. Continuing care and long-term substance use outcomes in managed care: early evidence for a primary care based model. Psychiatr Serv. 2011;62:1194–2000. doi: 10.1176/appi.ps.62.10.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham JA. Resolving alcohol-related problems with and without treatment: the effects of different problem criteria. J Stud Alcohol. 1999;60:463–466. doi: 10.15288/jsa.1999.60.463. [DOI] [PubMed] [Google Scholar]
- Dawson DA. US low-risk drinking guidelines: an examination of four alternatives. Alcohol Clin Exp Res. 2000;24:1820–1829. [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Grant BF. Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: a 3-year follow-up. Alcohol Clin Exp Res. 2007;31:2036–2045. doi: 10.1111/j.1530-0277.2007.00536.x. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF. The “gray area” of consumption between moderate and risk drinking. J Stud Alcohol Drugs. 2011;72:453–458. doi: 10.15288/jsad.2011.72.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan N. Smearing estimate: a nonparametric retransformation method. J Am Stat Assoc. 1983;78:605–610. [Google Scholar]
- Hedeker D. Generalized linear mixed models. In: Everitt B, Howell D, editors. Encyclopedia of Statistics in Behavioral Science. Wiley; New York: 2005. [Google Scholar]
- Hedeker D, Gibbons RD. Longitudinal Data Analysis. John Wiley & Sons; Hoboken, NJ: 2006. [Google Scholar]
- HMO Research Network. HMO Research Network; 2005. [Accessed Dec 20, 2012.]. HMO Research Network Members. Available at http://hmoresearchnetwork.org/members.htm. [Google Scholar]
- Holder HD. Alcoholism treatment and potential health care cost saving. Med Care. 1987;25:52–71. doi: 10.1097/00005650-198701000-00007. [DOI] [PubMed] [Google Scholar]
- Holder HD, Lennox RD, Blose JO. The economic benefits of alcoholism treatment: A summary of twenty years of research. J Employ Assist Res. 1992;1:63–82. [Google Scholar]
- Kline-Simon AH, Falk DE, Litten RZ, Mertens JR, Fertig J, Ryan M, Weisner CM. Posttreatment low-risk drinking as a predictor of future drinking and problem outcomes among individuals with alcohol use disorders. Alcohol Clin Exp Res. 2013;37:E373–380. doi: 10.1111/j.1530-0277.2012.01908.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondalsamy-Chennakesavan S, Gordon LG, Sanday K, Bouman C, De Jong S, Nicklin J, Land R, Obermair A. Hospital costs associated with adverse events in gynecological oncology. Gynecol Oncol. 2011;121:70–75. doi: 10.1016/j.ygyno.2010.11.030. [DOI] [PubMed] [Google Scholar]
- Li TK, Hewitt BG, Grant BF. The Alcohol Dependence Syndrome, 30 years later: a commentary. The 2006 H. David Archibald Lecture. Addiction. 2007;102:1522–1530. doi: 10.1111/j.1360-0443.2007.01911.x. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Clifford PR, Stout RL, Davis CM. Moderate drinking in the first year after treatment as a predictor of three-year outcomes. J Stud Alcohol Drugs. 2007;68:419–427. doi: 10.15288/jsad.2007.68.419. [DOI] [PubMed] [Google Scholar]
- Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24:465–488. doi: 10.1016/j.jhealeco.2004.09.011. [DOI] [PubMed] [Google Scholar]
- Marlatt GA. The controlled-drinking controversy: A commentary. Am Psychol. 1983;38:1097–1110. doi: 10.1037//0003-066x.38.10.1097. [DOI] [PubMed] [Google Scholar]
- McDermott PA, Alterman AI, Brown L, Zaballero A, Snider EC, McKay JR. Construct refinement and confirmation for the Addiction Severity Index. Psychol Assess. 1996;8:182–189. [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Mental Health America. Parity and health care reform: important changes for behavioral health. Mental Health America; 2011. [Accessed Oct 30, 2012]. Available at http://www.nmha.org/action/webinars/2010-07/Parity_and_HCR_July-8-2010.pdf. [Google Scholar]
- Mertens JR, Flisher AJ, Satre DD, Weisner CM. The role of medical conditions and primary care services in 5-year substance use outcomes among chemical dependency treatment patients. Drug Alcohol Depend. 2008;98:45–53. doi: 10.1016/j.drugalcdep.2008.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens JR, Weisner C, Ray GT. Readmission among chemical dependency patients in private, outpatient treatment: patterns, correlates and role in long-term outcome. J Stud Alcohol. 2005;66:842–847. doi: 10.15288/jsa.2005.66.842. [DOI] [PubMed] [Google Scholar]
- Montez-Rath M, Christiansen CL, Ettner SL, Loveland S, Rosen AK. Performance of statistical models to predict mental health and substance abuse cost. BMC Med Res Methodol. 2006;6:53. doi: 10.1186/1471-2288-6-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Hser YI, Huang D, Brecht ML, Herbeck DM. Self-report of longitudinal substance use: a comparison of the UCLA Natural History Interview and the Addiction Severity Index. J Drug Issues. 2010;40:495–516. doi: 10.1177/002204261004000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parthasarathy S, Weisner C. Five-year trajectories of health care utilization and cost in a drug and alcohol treatment sample. Drug Alcohol Depend. 2005;80:231–240. doi: 10.1016/j.drugalcdep.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Parthasarathy S, Weisner C, Hu TW, Moore C. Association of outpatient alcohol and drug treatment with health care utilization and cost: revisiting the offset hypothesis. J Stud Alcohol Drugs. 2001;62:89–97. doi: 10.15288/jsa.2001.62.89. [DOI] [PubMed] [Google Scholar]
- Satre DD, Blow FC, Chi FW, Weisner C. Gender differences in seven-year alcohol and drug treatment outcomes among older adults. Am J Addict. 2007;16:216–221. doi: 10.1080/10550490701375673. [DOI] [PubMed] [Google Scholar]
- Satre DD, Mertens JR, Weisner C. Gender differences in treatment outcomes for alcohol dependence among older adults. J Stud Alcohol. 2004;65:638–642. doi: 10.15288/jsa.2004.65.638. [DOI] [PubMed] [Google Scholar]
- Selby JV. Linking automated databases for research in managed care settings. Ann Intern Med. 1997;127:719–724. doi: 10.7326/0003-4819-127-8_part_2-199710151-00056. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. In: Alcohol consumption measures, in Assessing Alcohol Problems: A Guide for Clinicians and Researchers. Allen JP, Columbus M, editors. National Institute on Alcohol and Alcoholism; Bethesda, MD: 1995a. [Google Scholar]
- Sobell MB, Sobell LC. Controlled drinking after 25 years: How important was the great debate? Addiction. 1995b;90:1149–1153. discussion 1157–1177. [PubMed] [Google Scholar]
- Sobell MB, Sobell LC. Obstacles to the adoption of low risk drinking goals in the treatment of alcohol problems in the United States: A commentary. Addiction Research and Theory. 2006;14:19–24. [Google Scholar]
- Tsoh JY, Chi FW, Mertens JR, Weisner CM. Stopping smoking during first year of substance use treatment predicted 9-year alcohol and drug treatment outcomes. Drug Alcohol Depend. 2011;114:110–118. doi: 10.1016/j.drugalcdep.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Hinman A, Lu Y, Chi FW, Mertens J. Addiction treatment ultimatums and U.S. health reform: a case study. Nordisk Alkohol Nark. 2010a;27:685–698. doi: 10.1177/145507251002700612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Mertens J, Parthasarathy S, Moore C, Hunkeler EM, Hu T, Selby JV. The outcome and cost of alcohol and drug treatment in an HMO: day hospital versus traditional outpatient regimens. Health Serv Res. 2000;35:791–812. [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Mertens J, Parthasarathy S, Moore C, Lu Y. Integrating primary medical care with addiction treatment: a randomized controlled trial. JAMA. 2001;286:1715–1723. doi: 10.1001/jama.286.14.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Parthasarathy S, Moore C, Mertens JR. Individuals receiving addiction treatment: are medical costs of their family members reduced? Addiction. 2010b;105:1226–1234. doi: 10.1111/j.1360-0443.2010.02947.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zywiak WH, Hoffmann NG, Stout RL, Hagberg S, Floyd AS, DeHart SS. Substance abuse treatment cost offsets vary with gender, age, and abstinence likelihood. J Health Care Finance. 1999;26:33–39. [PubMed] [Google Scholar]