Abstract
The blood–brain barrier (BBB) is a dynamic structure that maintains the homeostasis of the brain and thus proper neurological functions. BBB compromise has been found in many pathological conditions, including neuroinflammation. Monocyte chemoattractant protein-1 (MCP1), a chemokine that is transiently and significantly up-regulated during inflammation, is able to disrupt the integrity of BBB and modulate the progression of various diseases, including excitotoxic injury and hemorrhage. In this review, we first introduce the biochemistry and biology of MCP1, and then summarize the effects of MCP1 on BBB integrity as well as individual BBB components.
Keywords: MCP1, BBB, BMECs, Pericytes, Astrocytes, BM, Microglia, Neurons
Introduction
Monocyte chemoattractant protein-1 (MCP1, also known as CCL2) is a pro-inflammatory mediator, whose up-regulation is found in many central nervous system (CNS) disorders with blood–brain barrier (BBB) breakdown. Accumulating evidence suggests that MCP1 is able to compromise the integrity of BBB and modulate the progression of various diseases. Although several studies have explored the effects of MCP1 on BBB permeability regulation, the exact mechanism, especially the effects of MCP1 on pericytes, astrocytes, neurons, and basement membrane (BM), remain elusive. Here, we review the biochemical and biological functions of MCP1 with a focus on its role in BBB regulation. Understanding the molecular mechanisms underlying MCP1-induced BBB disruption not only broadens our knowledge on chemokines and BBB but also promotes the development of novel therapeutic reagents for many CNS diseases.
Chemokines
Chemokines are a superfamily of structurally related small basic proteins with strong chemotactic activity. They function to induce cell-specific migration and activation of cells, especially immune cells, in response to insults [1–4]. Since the first chemokine was identified in 1977 [5], many chemokines and chemokine receptors have been identified [6]. Based on the number and position of conserved cysteine on their primary sequences, chemokines are divided into 4 sub-types: C, CC, CXC, and CXXXC [7–9]. The major functions of these chemokines include recruiting leukocytes during inflammatory conditions, maintaining ligand homeostasis between blood and tissue, and regulating developmental processes/disease progression, such as BBB permeability and myelination [10–12]. These biological functions are mediated through G-protein-coupled receptors [13]. Studies on chemokines and their receptors reveal promiscuity: one receptor may have more than one ligand and one ligand may have more than one receptor, which adds complexity to the studies of chemokines and chemokine receptors.
MCP1
MCP1, one of the most highly and transiently expressed chemokines during inflammation, is a member of the CC sub-type chemokines. In the brain, MCP1 is expressed by most cell types, including neurons, astrocytes, microglia, and brain microvascular endothelial cells (BMECs) [14–27]. MCP1 is synthesized with a signal peptide in its N-terminus, which is removed during secretion. The secreted MCP1 binds to soluble glycosaminoglycans (GAG) and GAG immobilized on the cell surface and the extracellular matrix [28–34]. This interaction is predicted to induce dimerization/oligomerization of MCP1, increase its local concentration, and promote formation of chemokine gradients [28, 35, 36].
Although the N-terminus of MCP1 is highly homologous among different species, the C-terminus is not. Human MCP1 has 76 amino acids, whereas mouse MCP1 has a C-terminal extension with about 50 amino acids. It has been shown that the C-terminal extension of mouse MCP1 is heavily O-glycosylated [37]. What is the function of the C-terminal extension of mouse MCP1? We have previously been able to show that plasmin cleaves mouse MCP1 and removes its C-terminal extension (see “Microglia” for details). Using recombinant wild-type and modified mouse MCP1, we further show that wild-type mouse MCP1 is able to dimerize, and that the mutant without C-terminus fails to dimerize [38]. Additionally, the C-terminus alone interacts with neither wild-type nor mutant mouse MCP1, suggesting that the highly glycosylated C-terminal extension of mouse MCP1 is necessary but not sufficient for dimerization. Surprisingly, human MCP1, which is highly homologous to the N-terminus of mouse MCP1, forms dimer in physiological concentration, and the residues crucial for the dimerization have been identified as amino acids 6–16 [39]. In agreement with this report, two mutant forms of human MCP1, P8A and Y13A, have been reported to be unable to dimerize [40].
Being able to form a dimer does not necessarily mean it functions as a dimer. The next question is whether MCP1 functions as a monomer or dimer. Zhang and Rollins showed that chemical crosslinked human MCP1 dimer was functional in attracting monocytes in vitro [39]. Furthermore, a mutant form of MCP1, 7ND, which lacks residues 2–8, has been shown to inhibit the function of wild-type MCP1 but not crosslinked MCP1 [39], suggesting that 7ND is a dominant-negative mutant and that MCP1 functions as a dimer. P8A mutant MCP1, on the other hand, has a binding affinity for CCR2 similar to wild-type MCP1 and induces calcium influx and chemotaxis at the same level as wild-type MCP1 [40], suggesting that MCP1 works as a monomer. Additionally, 7ND MCP1 has also been shown to function as a competitive inhibitor of monomeric MCP1 [40]. Consistent with the monomer theory, we have previously been able to demonstrate that, compared to full-length mouse MCP1, the mutant variant without C-terminus, which cannot form a dimer, more efficiently activates Rac1 and promotes the formation of lamellipodia [38].
MCP1 exerts its biological functions by binding to its high affinity receptor, CCR2, which is mainly expressed by microglia, astrocytes, and BMECs in the brain [41, 42]. Although MCP1 has only one high affinity receptor, CCR2 has four more ligands (CCL7, CCL8, CCL12, and CCL13) besides MCP1 [43–45]. In rodents, only one CCR2 isoform is found, whereas two alternatively spliced CCR2 isoforms with different C-terminus [46] are found in human, denoted CCR2A and CCR2B. CCR2B is mainly expressed on monocytes and activated NK cells, whereas mononuclear cells and vascular smooth muscle cells predominately express CCR2A [47].
MCP1 AND BBB
The BBB is the largest CNS barrier, and sustains brain homeostasis and thus proper neurological functions. At the BBB, specialized endothelial cells (BMECs), astrocytes, pericytes, basement membrane (BM), neurons, and microglia can be found [48]. The BMECs connect to each other via a complex network of tight junctions, which create the primary barrier and prevent paracellular transport across endothelial cells. These cells deposit a layer of BM (endothelial BM), in which pericytes are embedded. Astrocytes, which wrap BMECs and pericytes with their endfeet, deposit another layer of BM (parenchymal BM). These two layers of BM are not distinguishable except at the post-capillary venules, where a cerebrospinal fluid-drained perivascular space separates them. Neurons and microglia, which exist in the parenchyma, have direct contact with astrocytes and BMECs. The above-mentioned cells together with both endothelial and parenchymal BM are necessary for an intact barrier of the BBB [49]. Perturbation of BBB has been found in many neurological conditions, including trauma [50, 51], brain tumors [52, 53], stroke [54–56], and neurodegenerative diseases [57–61], and BBB breakdown is one of the hallmarks that accompany the progression of these diseases. Recently, BBB compromise has been found to play a causative role in the onset of Alzheimer’s disease [57] and amyotrophic lateral sclerosis [62]. A large number of molecules have been reported to affect the permeability of BBB, such as MCP1, TNF-α, IL-1β, IL-10, and IFN-γ [63–71]. Here, we focus on the effect of MCP1 on BBB integrity.
It has been shown that injection of recombinant mouse MCP1 into the brain disrupts BBB integrity [65–67, 71, 72]. We have previously been able to further demonstrate that plasmin-mediated truncation of MCP1 is indispensable for MCP1-induced BBB compromise [71]. Consistent with our report, tPA, which converts inactive plasminogen to active plasmin, has been found to promote BBB disruption and subsequent peripheral blood mononuclear cell (PBMC) infiltration [73]. Additionally, BBB compromise and PBMC infiltration have also been found in mice deficient for plasminogen activator inhibitor-1 [74], suggesting that the effect of MCP1 on BBB is dependent on plasmin activity. MCP1, however, failed to compromise BBB integrity in CCR2−/− mice [67], suggesting that the effect of MCP1 on BBB also depends on CCR2. The next question then becomes how exactly MCP1-CCR2 axis affects the integrity of BBB. The roles of MCP1-CCR2 on individual BBB components are summarized below.
BMECs
The capillary endothelium in the brain is 50–100 times tighter than that in the periphery [75]. Compared with peripheral endothelial cells, BMECs are characterized by the presence of more mitochondria, less pinocytotic activity, lack of fenestrations, and the presence of tight junctions [76–79]. BMECs connect to one another forming an impermeable monolayer. In the interendothelial space, specific structures, including adherens junctions and tight junctions, are present [68, 77, 80, 81]. Although both adherens and tight junctions act to limit paracellular permeability of endothelial cells [82], tight junctions are the primary structure that maintains the impermeability of BBB [83]. In the tight junctions, many tight junction proteins are expressed. There are two types of tight junction proteins: transmembrane ones, such as occludin and claudin-1, -5, and -11, and cytoplasmic accessory proteins, such as zonula occluden-1, -2, and -3 (ZO-1, -2, and -3) and cingulin [84, 85]. The transmembrane proteins, especially occludin, function to seal gaps between adjacent cells [86–89]. Occludin, a 60- to 65-kD transmembrane protein with its N- and C-terminus in the cytoplasm, has been shown to maintain the integrity of BBB [90–93]. There is also evidence showing that the phosphorylation state of occludin regulates BBB integrity by affecting its membrane association [94–100]. Cytoplasmic accessory proteins, on the other hand, link transmembrane proteins to cortical actin-based cytoskeleton [86–89]. ZO-1, the first identified accessory protein [101] that links occludin to actin cytoskeleton [102], plays a critical role in regulating BBB permeability. Dissociation of ZO-1 from the tight junctions has been shown to accompany the disruption of BBB [70, 71, 103–105]. In addition, ZO-1 has been detected in the nucleus and shown to co-localize with transcription factors in some conditions [106–109], suggesting its potential role as a signaling molecule.
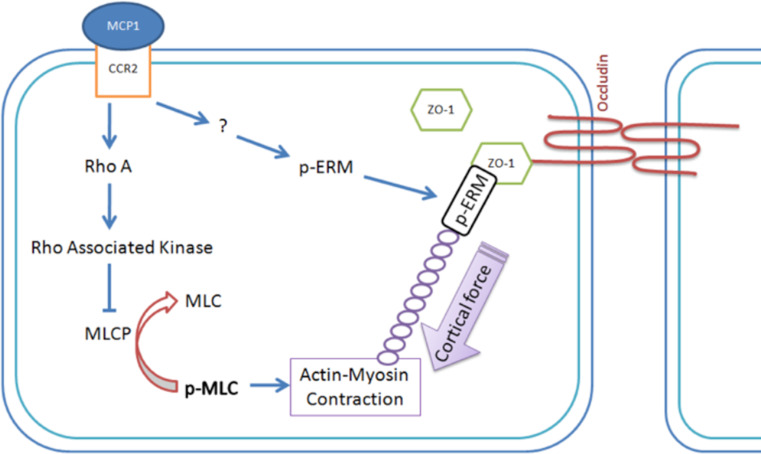
BMECs as the major barrier of BBB have been under extensive investigations. Accumulating evidence shows that MCP1 compromises BBB integrity via redistribution of tight junction proteins from cell–cell border (probable via endocytosis) and reorganization of actin cytoskeleton in BMECs [65–67, 72]. We have previously been able to verify these data and further show that these changes are dependent on plasmin activity [71]. Mechanistic studies reveal that phosphorylation of TJP regulates their functions and locations [95, 96, 110–112]. Stamatovic and colleagues further demonstrated that the binding of MCP1 to CCR2 activated PKC (specifically PKCα and PKCζ) and Rho kinase, resulting in shift of tight junction proteins from cell border to intracellular compartments [65, 66]. Additionally, this phosphorylation event also promoted the interaction between tight junction proteins and actin cytoskeleton, resulting in a shift of tight junction proteins from Triton X-100 soluble fraction to Triton X-100 insoluble fraction [65–67, 113, 114]. These changes are not limited to MCP1, because growth factors (PDGF and VEGF) also induce phosphorylation and redistribution of tight junction proteins [115, 116], suggesting that phosphorylation of tight junction proteins may be a common mechanism to transport them to different cellular compartments. In addition to tight junction protein phosphorylation, the activated kinases, especially Rho Kinase, also phosphorylate myosin light chain phosphatase (MLCP) and inhibit its activity. The inhibition of MLCP results in enhanced phosphorylation of myosin light chain (MLC), leading to increased actin–myosin interaction and thus increased cortical force in endothelial cells [66, 117–119]. In addition, we have previously been able to demonstrate that binding of MCP1 to CCR2 on BMECs also promotes phosphorylation of Ezrin/Radixin/Moesin (ERM) proteins on conserved Threonine residues (Thr567 for ezrin, Thr564 for radixin, and Thr558 for moesin) [71]. ERM proteins are a family of highly conserved proteins that act as a linker between plasma membrane and actin cytoskeleton. Unphosphorylated ERM proteins form intramolecular interactions between the N- and C-terminus. When phosphorylated on the conserved Threonine residues, they form intermolecular interactions (N-terminus binding to membrane proteins and C-terminus binding to actin cytoskeleton) [120–122]. Our data showed that MCP1 treatment led to phosphorylation of ERM proteins and promoted interaction between ZO-1 and phosphorylated ERM proteins [71], indicating an important role of ERM proteins in translocation of ZO-1 upon MCP1 treatment. Occludin, however, did not interact with ERM proteins even upon MCP1 treatment [71], indicating different ways of regulation. Taken together, we proposed a mechanism responsible for MCP1-induced BMEC and thus BBB changes as shown in Fig. 1. The binding of MCP1 to CCR2 activates unknown kinase(s), which phosphorylates ERM proteins. The phosphorylated ERM proteins then bind to ZO-1 and actin cytoskeleton. In addition, Rho-associated kinase, which is activated by MCP1, phosphorylates MLCP, resulting in decreased phosphatase activity. The imbalance of MLCP and MLC kinase activity results in over-phosphorylation of MLC, and thus increased and prolonged actin–myosin contraction. This contraction in turn pulls ZO-1 away from the tight junction complex, leading to disruption of BBB integrity. In the BMEC–astrocyte co-culture system, Stamatovic and colleagues further demonstrated that lack of expression of CCR2 in BMECs was sufficient to prevent the leakage of BBB upon MCP1 treatment [67], suggesting that MCP1-induced BBB compromise is dependent on endothelial CCR2.
Fig. 1.
Proposed model for MCP1-induced BBB compromise. By binding to CCR2, MCP1 induces phosphorylation of ERM proteins, which then bind to ZO-1 and actin cytoskeleton. Additionally, MCP1 also activates Rho-associated kinases, which phosphorylate and inactivate MLCP, resulting in increased phosphorylation of MLC. The over-phosphorylation of MLC induces enhanced and prolonged actin–myosin contraction, which generates forces that pull ZO-1 away from the cell–cell border, leading to BBB compromise. Adapted from [71]
Astrocytes
The unique properties of BMECs (increased mitochondria number, few pinocytotic vesicles, and the presence of tight junctions [76–79]) lead to the question: is it due to intrinsic characteristics of BMECs or the microenvironment in the brain? Stewart and Wiley elegantly demonstrated that nonvascularized brain tissue grafted into the coelomic cavity developed capillaries with BMEC properties, whereas somite tissue grafted into cerebral ventricles failed to do so [123], strongly suggesting that interaction between vascular tissue and CNS tissue contributes to the properties of BMECs. In the brain, astrocytic endfeet together with the parenchymal BM establish the glia lamitans, which defines the parenchymal border in the CNS [49]. Astrocytic endfeet cover more than 99 % of the vascular surface [124, 125], suggesting that astrocytes may confer on BMECs those unique properties and thus contribute to the impermeability of BBB. Janzer and Raff found that astrocytes induced tight junction in endothelial cells within the eyes [52], indicating that astrocytes can enhance the impermeability of endothelial cells lining the capillaries in the eyes. In consistent with these data, the BMEC–astrocyte co-culture system showed a higher transendothelial electrical resistance (TEER) and less infiltration of tracers across the in vitro BBB than BMECs alone [71, 126– 129]. Additionally, the temporary focal loss of astrocytes has been found to parallel the compromise of BBB integrity in vivo [130]. Further experiments reveal that the role of astrocytes in BBB integrity is due to the release of soluble factors, including Ang1, TGF-β, GDNF, and FGF2 [131–133], as well as the direct contact with BMECs [134]. Recently, polarized distribution of intramembranous orthogonic arrays of particles (OAPs), which contain water channel aquaporin 4 (AQP4), the potassium channel Kir4.1, and a dystroglycan–dystrophin complex, has been reported in astrocytic endfeet [135]. Given the functions of AQP4 and Kir4.1 (regulation of water and ion homeostasis at the glial–endothelial interface, respectively), OAPs have been speculated to influence BBB permeability [133, 135]. Together, these data support that astrocytes contribute to the impermeability of BBB. It should be noted that the effect of astrocytes in BBB integrity only takes place in adulthood, because astrocyte development starts after birth [136]. There is also evidence, however, suggesting astrocytes may not contribute to the BBB integrity [137]. This inconsistency may be due to different experimental conditions or methodology.
Since astrocytes are a main source of MCP1, transgenic mice over-expressing MCP1 in astrocytes have been developed and used to study the function of MCP1. In addition to enhanced nociceptive responses in these transgenic mice [138], chronic expression of MCP1 in astrocytes induces BBB compromise in vivo, indicating a crucial role of astrocytic MCP1 in BBB regulation [139]. In an in vitro system, it has been shown that MCP1 binding in human astrocytes is mediated by both CCR2 and D6 decoy chemokine receptors [140] and activation of CCR2 promotes the survival of astrocytes [141]. Additionally, caveolin-1 has been found to mediate the effects of MCP1 in astrocytes [142]. Knockout of CCR2 in astrocytes, however, failed to affect BBB integrity in the BMEC–astrocyte co-culture model [67], suggesting that CCR2 in astrocytes is dispensable for MCP1-induced BBB breakdown. This discrepancy may be due to the over-simplified in vitro BBB models used. Future studies should focus on in vivo studies or use in vitro BBB models that replicate both the anatomical and physiological characteristics of the BBB.
BM
Two layers of BM are found at the BBB: endothelial BM and parenchymal BM [49, 143]. The two layers are morphologically indistinguishable except at the post-capillary venules, where a cerebrospinal fluid-drained perivascular space separates them [49]. BM consists of a mixture of extracellular matrix (ECM) proteins, including collagens, laminins, heparin sulfate proteoglycans, fibronectin, vitronectin, nidogens, perlecan, and agrin [131, 144–147]. BM assembly mainly involves polymerization of laminins and collagens, which is cross-linked by nidogens [147, 148]. Although most ECM proteins are ubiquitously expressed at both endothelial and parenchymal BM, the former mainly expresses laminin α4 and α5 [51] and the latter predominantly expresses laminin α1 and α2 [51, 143, 149].
BM has been proposed to regulate BBB integrity directly as a physical barrier [150], given its anatomical location: i.e. between BMECs and astrocytes. Loss of BM leads to breakdown of BBB [151–156]. In addition, the BM also contributes to the integrity of BBB through individual ECM proteins, which not only anchor different cells in place at BBB but also regulate cellular processes [51, 131, 143, 144, 157]. It has been shown that laminin, collagen type IV, and fibronectin increase TEER of brain capillary endothelial cells [158]. Dystroglycan, a major receptor for ECM proteins, is selectively cleaved at the parenchymal BM at sites of leukocyte infiltration during experimental autoimmune encephalomyelitis [144]. Additionally, laminin α5, an endothelial BM-specific component, has been shown to serve as a barrier for leukocyte translocation [51]. These results suggest that ECM proteins and their receptors also contribute to the integrity of BBB.
Consistent with the detrimental role of MCP1 in BBB integrity, MCP1 has been found to promote hydrogen peroxide induced ECM protein degradation [159]. Contrary to this finding, there are reports showing that MCP1 directly contributes to the production and accumulation of ECM, especially collagen, in many disease models, including diabetic nephropathy [160], systemic sclerosis [161], and peritoneal dialysis-related epithelial–mesenchymal transition [162]. This discrepancy may be explained by different disease models and/or indirect effects of MCP1. For example, leukocytes recruited by MCP1 may secrete proteases that degrade ECM proteins [163, 164]. The exact role of MCP1 in BM needs further investigations.
Pericytes
Discovered more than 100 years ago [165], pericytes are sandwiched inbetween the abluminal side of BMECs and luminal side of astrocytic endfeet [166]. Specifically, pericytes are embedded in the endothelial BM in CNS capillaries [49, 167], and the degree of its coverage on endothelial cells varies depending on tissue type and species [166]. It has been shown that the pericyte-to-endothelial ratio is 1:1 in retina, 1:3 in brain, and 1:100 in skeletal muscles, respectively [166, 168]. The average pericyte-to-endothelial ratio is lower in rat capillaries (1:5) and relatively higher in mouse and human capillaries (1:4 and 1:3–4, respectively) [169, 170]. Although brain capillaries have high pericyte coverage, the precise percentage of capillary surface covered by pericytes varies significantly depending on different research groups, ranging from 22 to 99 % [168, 171, 172]. This difference may be due to the different pericyte markers used. There are no specific markers for pericytes so far, although several markers, including α-smooth muscle actin (SMA) [169, 173–175], PDGFRβ [25, 176], Desmin [177], CD13 [178, 179], NG2 [6, 180, 181], and RGS-5 [182, 183], have been used to identify pericytes. It should be noted that (1) these markers are also expressed by other types of cells besides pericytes, such as smooth muscle cells, myofibroblasts, and neuronal progenitors [167, 184, 185], and (2) the expression of these markers also depends on the differentiation stage of pericytes. It has been shown that TGF-β-treated (further differentiated) pericytes express significantly more SMA, VEGF, MMP-2, and MMP-9 than bFGF-treated (less differentiated) pericytes [186]. Fate-mapping experiments have shown that pericytes have several different developmental origins [167]. For example, ectoderm-derived neural crest gives rise to pericytes in the brain and thymus [187–189], whereas pericytes in the lungs [190], liver [191], and gut [192] are from mesothelium. In addition, there is also evidence suggesting that some pericytes are derived from hematopoietic stem cells [174, 193].
Pericytes have been reported to exert different functions, including BBB regulation, vascular development, homeostasis maintenance, and serving as contractile and multipotent cells [169, 173, 194]. Here, we focus only on its role in BBB regulation. It has been found that addition of pericytes to the BMEC–astrocyte co-culture system significantly enhances TEER [195, 196], suggesting that pericytes contribute to the integrity of BBB. In addition, pericytes have been shown to up-regulate P-glycoprotein functional activity in endothelial cells and control tight junction permeability [197–199], suggesting that the interaction between endothelial cells and pericytes may play an important role in BBB integrity regulation. Using mice with defects in pericyte generation, researchers have demonstrated that pericyte coverage positively correlates with tight junction tightness [134] and negatively correlates with the BBB permeability [136]. Consistently, a correlation has been reported between pericyte loss and BBB breakdown [57, 200]. Further mechanistic studies suggest that the diminished expression of BBB-specific genes in endothelial cells and lack of polarity in astrocytic endfeet are responsible for pericyte loss-induced BBB breakdown [200]. In pathological conditions, such as hypoxia or traumatic brain injury, which lead to the disruption of BBB, pericytes have been found to migrate away from the micro-vasculatures [201, 202], but the relationship between migration of pericytes and compromise of BBB has not yet been studied.
Increased MCP1 levels have been reported in many disorders, including neurodegeneration, neuroinflammation, and kidney fibrosis [203, 204]. Additionally, MCP1 concentration has also been revealed to correlate with heavily oxidized LDL-induced pericyte injury [205]. However, due to the recent discovery of the critical role of pericytes in BBB regulation, only limited data are available to answer the question that how MCP1 affects pericytes.
Microglia
Microglia, which account for 10–20 % of glial cells, are brain-resident immune cells. Their number in the brain (100–200 billion depending on the condition) is comparable to that of neurons. It had long been believed that microglia originated from myeloid progenitors in the bone marrow [206–210] and that these macrophage-like cells migrated into the brain during early development (before the formation of BBB). A recent lineage tracing study has shown that adult microglia derive from colony-stimulating factor-1 receptor (CSF1R) positive primitive myeloid progenitors that arise before embryonic day 8 [211]. Consistently, fate-mapping experiments support that microglia mostly originate from Myb-independent, FLT3-independent, but PU.1-dependent myeloid progenitors that express CSF1R at embryonic day 8.5 [212–216]. Microglia have two states: a resting state with ramified morphology and an activated state with amoeboid morphology. Compared to the amoeboid morphology, the ramified structure has a smaller cell body surrounded by many long, thin, and highly dynamic processes. In the brain parenchyma, ramified microglia extend and retract their processes continually to sense changes in the surrounding microenvironment [217]. It is estimated that microglia can survey the entire brain in a few hours [217]. When there is an injury or disturbance of homeostasis in the CNS, microglia become activated. The activation involves changes of morphology and gene expression. The activated microglia then migrate to the injury site and proliferate locally. Additionally, these cells also secrete both pro- and anti-inflammatory cytokines, phagocytose cellular debris, process antigens, and present them to T cells via MHC class I molecules [218–225]. Whether microglia play a beneficial or detrimental role in CNS injury is highly controversial. There is evidence showing that microglia play neuroprotective roles by clearing cell debris and secreting factors promoting neurite growth and neuronal survival, such as neurotrophin-3 and brain-derived neutrophic factor (BDNF) [226–228]. In contrast, microglia have also been shown to produce pro-inflammatory cytokines, including TNF-α and IL-1β, which induce direct cytotoxicity by binding to their receptors (TNFRs and IL-1RI, respectively) and activating downstream cell death pathways [229]. Given that microglia are found in the perivascular space, it is speculated that microglia may play an important role in regulating BBB integrity by interacting with other BBB components, including BMECs, astrocyte endfeet, and pericytes [230]. There is evidence showing that microglial activation restores BBB integrity after the disruption of BBB [231]. In contrast, TNF-α released from activated microglia has been shown to impair BBB integrity [232], possibly through TNF-α-induced direct cytotoxicity on BMECs. This discrepancy may be due to different injury models and different timing after injury. Therefore, further investigations are needed to clarify the role of microglia in BBB permeability.
As indicated by its name, MCP1 is a potent chemoattractant for monocytes and microglia. MCP1-induced chemotaxis of monocytes and microglia has been found in many CNS injuries, including ischemia, excitotoxicity, and hemorrhage [72, 204, 221, 233–237]. The trafficking of microglia and leukocytes, however, is impaired in mice lacking CCR2, suggesting that MCP1-induced chemotaxis is dependent on CCR2 [238, 239]. Our laboratory has previously shown that microglial activation/migration induced by excitotoxic injury is attenuated in MCP1−/− mice [204]. Similar results were found in rats or mice injected with MCP1 blocking antibody [204, 240]. Interestingly, like MCP1−/− mice, excitotoxicity-induced microglial activation/migration is decreased in mice lacking plasminogen (plg) or tissue plasminogen activator (tPA), which converts plg to active plasmin [241, 242]. These results indicate that mouse MCP1 and the plg activation system may use converging pathways. Further studies in our laboratory have revealed that plasmin, generated by the action of tPA on plg in the mouse CNS (or urokinase plasminogen activator in other systems), cleaves MCP1 at lysine (K) 104 [204]. This cleavage removes the highly glycosylated C-terminal extension and generates a N-terminal fragment that is highly homologous to human MCP1. The chemotactic potency of plasmin-cleaved MCP1 is higher than that of intact MCP1 and comparable to human MCP1 [38, 204], suggesting that plasmin is an activator of mouse MCP1. In accordance with this, infusion of plasmin-cleaved MCP1 into the CNS restored excitotoxicity-induced microglial activation/migration in plg−/− mice, whereas infusion of FL-MCP1 failed to do so. Furthermore, we have shown that mouse MCP1 C-terminus, when fused to human MCP1, is also inhibitory [70]. These data indicate that plasmin-mediated cleavage may be a mechanism used by cells to activate MCP1 and initiate downstream signaling cascades in mice. Importantly, the effects of plasmin-cleaved MCP1 are comparable to that of human MCP1 [38], suggesting that human MCP1 may be regulated similarly by an unidentified protein or differently at transcriptional/translational, transport, or signaling levels. We favor the latter, because we were not successful in pulling down proteins that specifically interact with human MCP1. In addition, the two CCR2 isoforms in human (CCR2A and CCR2B) have been shown to be able to activate different signaling pathways. Calcium influx has been found in chemotaxis of CCR2B-positive cells, but not in CCR2A-positive cells [243, 244], suggesting that the MCP1-CCR2 axis may also be regulated at the receptor or signaling levels in human.
Although human MCP1 does not have a highly glycosylated C-terminus, it can also be truncated in the C-terminus. A fragment with 69 amino acids (1–69) has been found and this fragment has the same activity as the wild-type MCP1 [245]. Which enzyme(s) is responsible for this cleavage, however, is not clear. In the N-terminus, human MCP1 has been reported to be cleaved by matrix metalloproteinase-1, -3, -8, and -12 between aminoacid 4 and 5 [246, 247]. This cleavage generates a fragment (5-76) that functions as an antagonist for CCR2 [245–248]. Consistently, the MCP1 mutant lacking amino acids 2-8 (7ND) has been shown to inhibit MCP1-CCR2 signaling both in vitro and in vivo [39, 249, 250]. There is no report on whether these matrix metalloproteinases cleave mouse MCP1. However, it would be reasonable to assume they do, based on the similarity of human and mouse MCP1 sequence. The first eight amino acids for human and mouse MCP1 are QPDAINAP and QPDAVNAP, respectively.
Neurons
It is estimated that in human brain every neuron has its own capillary [251], which together with neurovascular coupling (local neuronal activity and metabolism regulate cerebral blood flow) [252] indicates that neurons may regulate BBB functions. Anatomical studies have shown that BMECs and astrocytic processes are directly innervated by noradrenergic, serotonergic, cholinergic, and GABAergic neurons [253–259]. The presence of neurons has been shown to increase the integrity of BBB in vitro [260]. In addition, neurons have been shown to promote the expression of specific enzymes on BMECs [187]. These data suggest that neurons contribute to the integrity of BBB.
MCP1 exerts profound functions on neurons both directly and indirectly. MCP1 has been shown to directly bind to CCR2 on rat spinal neurons and activates Akt pathway. The binding of MCP1 on these neurons potently and efficiently inhibits GABA(A)-mediated GABAergic responses [261]. The MCP1–CCR2 axis has also been shown to contribute to neuropathic pain via interaction between astrocytes and neurons [262–265]. Contrary to these reports, MCP1 has been found to protect against methylmercury neurotoxicity [266], and early expression of MCP1 in neurons is necessary for hypoxic preconditioning-induced ischemic tolerance to focal stroke [267]. MCP1-induced molecular changes in neurons may modulate the function of other BBB components, and thus affect the integrity of BBB. In accordance with this hypothesis, MCP1 level has been found to positively correlate with the permeability of BBB and progression of disease, including Gaucher’s disease, brain inflammation, stroke, and excitotoxic injury [71, 72, 204, 221, 233–237, 268, 269]. Consistently, lack of MCP1 or CCR2 prevents neuronal death, decreases BBB permeability, and improves neuronal function in many disorders, including hemorrhage and ischemia–reperfusion injury [72, 270].
Future directions
Although it is clear that plasmin removes the C-terminus of mouse MCP1 and enhances its chemotactic activity [38, 204], how human MCP1, which lacks the heavily glycosylated C-terminus, is regulated is still elusive. Future work should focus on the regulation/activation of human MCP1. In addition, how MCP1 regulates individual BBB components, especially pericytes, astrocytes, neurons, and BM, needs investigations. Such studies will shed light on our understanding of MCP1–CCR2 signaling/functioning, and may provide new molecular targets for the treatment of many CNS diseases, including brain trauma, stroke, and neurodegenerative diseases.
Acknowledgements
We thank members of the Tsirka laboratory for discussions. This work was supported by NIH R01NS42168 (SET) and Sigma Xi Grant-in-Aid of Research (YY).
References
- 1.Glabinski AR, Balasingam V, Tani M, Kunkel SL, Strieter RM, Yong VW, Ransohoff RM. Chemokine monocyte chemoattractant protein-1 is expressed by astrocytes after mechanical injury to the brain. J Immunol. 1996;156:4363–4368. [PubMed] [Google Scholar]
- 2.Hulkower K, Brosnan CF, Aquino DA, Cammer W, Kulshrestha S, Guida MP, Rapoport DA, Berman JW. Expression of CSF-1, c-fms, and MCP-1 in the central nervous system of rats with experimental allergic encephalomyelitis. J Immunol. 1993;150:2525–2533. [PubMed] [Google Scholar]
- 3.Lahrtz F, Piali L, Spanaus KS, Seebach J, Fontana A. Chemokines and chemotaxis of leukocytes in infectious meningitis. J Neuroimmunol. 1998;85:33–43. doi: 10.1016/s0165-5728(97)00267-1. [DOI] [PubMed] [Google Scholar]
- 4.Miller RJ, Meucci O. AIDS and the brain: is there a chemokine connection? Trends Neurosci. 1999;22:471–479. doi: 10.1016/s0166-2236(99)01408-3. [DOI] [PubMed] [Google Scholar]
- 5.Wu VY, Walz DA, McCoy LE. Purification and characterization of human and bovine platelet factor 4. Prep Biochem. 1977;7:479–493. doi: 10.1080/00327487708065515. [DOI] [PubMed] [Google Scholar]
- 6.Ruiter DJ, Schlingemann RO, Westphal JR, Denijn M, Rietveld FJ, De Waal RM (1993). Angiogenesis in wound healing and tumor metastasis. Behring Inst Mitt 258–272 [PubMed]
- 7.Murphy PM. The molecular biology of leukocyte chemoattractant receptors. Annu Rev Immunol. 1994;12:593–633. doi: 10.1146/annurev.iy.12.040194.003113. [DOI] [PubMed] [Google Scholar]
- 8.Rollins BJ. Chemokines. Blood. 1997;90:909–928. [PubMed] [Google Scholar]
- 9.Yoshimura T, Yuhki N, Moore SK, Appella E, Lerman MI, Leonard EJ. Human monocyte chemoattractant protein-1 (MCP-1). Full-length cDNA cloning, expression in mitogen-stimulated blood mononuclear leukocytes, and sequence similarity to mouse competence gene JE. FEBS Lett. 1989;244:487–493. doi: 10.1016/0014-5793(89)80590-3. [DOI] [PubMed] [Google Scholar]
- 10.Campbell JJ, Butcher EC. Chemokines in tissue-specific and microenvironment-specific lymphocyte homing. Curr Opin Immunol. 2000;12:336–341. doi: 10.1016/s0952-7915(00)00096-0. [DOI] [PubMed] [Google Scholar]
- 11.Cardona AE, Li M, Liu L, Savarin C, Ransohoff RM. Chemokines in and out of the central nervous system: much more than chemotaxis and inflammation. J Leukoc Biol. 2008;84:587–594. doi: 10.1189/jlb.1107763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tran PB, Miller RJ. Chemokine receptors: signposts to brain development and disease. Nat Rev Neurosci. 2003;4:444–455. doi: 10.1038/nrn1116. [DOI] [PubMed] [Google Scholar]
- 13.Ransohoff RM. The chemokine system in neuroinflammation: an update. J Infect Dis. 2002;186(Suppl 2):S152–S156. doi: 10.1086/344266. [DOI] [PubMed] [Google Scholar]
- 14.Andjelkovic AV, Kerkovich D, Shanley J, Pulliam L, Pachter JS. Expression of binding sites for beta chemokines on human astrocytes. Glia. 1999;28:225–235. [PubMed] [Google Scholar]
- 15.Andjelkovic AV, Pachter JS. Characterization of binding sites for chemokines MCP-1 and MIP-1alpha on human brain microvessels. J Neurochem. 2000;75:1898–1906. doi: 10.1046/j.1471-4159.2000.0751898.x. [DOI] [PubMed] [Google Scholar]
- 16.Andjelkovic AV, Spencer DD, Pachter JS. Visualization of chemokine binding sites on human brain microvessels. J Cell Biol. 1999;145:403–412. doi: 10.1083/jcb.145.2.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boddeke EW, Meigel I, Frentzel S, Gourmala NG, Harrison JK, Buttini M, Spleiss O, Gebicke-Harter P. Cultured rat microglia express functional beta-chemokine receptors. J Neuroimmunol. 1999;98:176–184. doi: 10.1016/s0165-5728(99)00096-x. [DOI] [PubMed] [Google Scholar]
- 18.Dicou E, Vincent JP, Mazella J. Neurotensin receptor-3/sortilin mediates neurotensin-induced cytokine/chemokine expression in a murine microglial cell line. J Neurosci Res. 2004;78:92–99. doi: 10.1002/jnr.20231. [DOI] [PubMed] [Google Scholar]
- 19.Horuk R, Martin AW, Wang Z, Schweitzer L, Gerassimides A, Guo H, Lu Z, Hesselgesser J, Perez HD, Kim J, et al. Expression of chemokine receptors by subsets of neurons in the central nervous system. J Immunol. 1997;158:2882–2890. [PubMed] [Google Scholar]
- 20.Kalehua AN, Nagel JE, Whelchel LM, Gides JJ, Pyle RS, Smith RJ, Kusiak JW, Taub DD. Monocyte chemoattractant protein-1 and macrophage inflammatory protein-2 are involved in both excitotoxin-induced neurodegeneration and regeneration. Exp Cell Res. 2004;297:197–211. doi: 10.1016/j.yexcr.2004.02.031. [DOI] [PubMed] [Google Scholar]
- 21.Mahad DJ, Ransohoff RM. The role of MCP-1 (CCL2) and CCR2 in multiple sclerosis and experimental autoimmune encephalomyelitis (EAE) Semin Immunol. 2003;15:23–32. doi: 10.1016/s1044-5323(02)00125-2. [DOI] [PubMed] [Google Scholar]
- 22.Mahajan SD, Schwartz SA, Aalinkeel R, Chawda RP, Sykes DE, Nair MP. Morphine modulates chemokine gene regulation in normal human astrocytes. Clin Immunol. 2005;115:323–332. doi: 10.1016/j.clim.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 23.Meeuwsen S, Bsibsi M, Persoon-Deen C, Ravid R, van Noort JM. Cultured human adult microglia from different donors display stable cytokine, chemokine and growth factor gene profiles but respond differently to a pro-inflammatory stimulus. NeuroImmunoModulation. 2005;12:235–245. doi: 10.1159/000085655. [DOI] [PubMed] [Google Scholar]
- 24.Mennicken F, Maki R, de Souza EB, Quirion R. Chemokines and chemokine receptors in the CNS: a possible role in neuroinflammation and patterning. Trends Pharmacol Sci. 1999;20:73–78. doi: 10.1016/s0165-6147(99)01308-5. [DOI] [PubMed] [Google Scholar]
- 25.Storer PD, Xu J, Chavis J, Drew PD. Peroxisome proliferator-activated receptor-gamma agonists inhibit the activation of microglia and astrocytes: implications for multiple sclerosis. J Neuroimmunol. 2005;161:113–122. doi: 10.1016/j.jneuroim.2004.12.015. [DOI] [PubMed] [Google Scholar]
- 26.Wittendorp MC, Boddeke HW, Biber K. Adenosine A3 receptor-induced CCL2 synthesis in cultured mouse astrocytes. Glia. 2004;46:410–418. doi: 10.1002/glia.20016. [DOI] [PubMed] [Google Scholar]
- 27.Zeng HY, Zhu XA, Zhang C, Yang LP, Wu LM, Tso MO. Identification of sequential events and factors associated with microglial activation, migration, and cytotoxicity in retinal degeneration in rd mice. Invest Ophthalmol Vis Sci. 2005;46:2992–2999. doi: 10.1167/iovs.05-0118. [DOI] [PubMed] [Google Scholar]
- 28.Hoogewerf AJ, Kuschert GS, Proudfoot AE, Borlat F, Clark-Lewis I, Power CA, Wells TN. Glycosaminoglycans mediate cell surface oligomerization of chemokines. Biochemistry. 1997;36:13570–13578. doi: 10.1021/bi971125s. [DOI] [PubMed] [Google Scholar]
- 29.Kuschert GS, Coulin F, Power CA, Proudfoot AE, Hubbard RE, Hoogewerf AJ, Wells TN. Glycosaminoglycans interact selectively with chemokines and modulate receptor binding and cellular responses. Biochemistry. 1999;38:12959–12968. doi: 10.1021/bi990711d. [DOI] [PubMed] [Google Scholar]
- 30.Middleton J, Neil S, Wintle J, Clark-Lewis I, Moore H, Lam C, Auer M, Hub E, Rot A. Transcytosis and surface presentation of IL-8 by venular endothelial cells. Cell. 1997;91:385–395. doi: 10.1016/s0092-8674(00)80422-5. [DOI] [PubMed] [Google Scholar]
- 31.Middleton J, Patterson AM, Gardner L, Schmutz C, Ashton BA. Leukocyte extravasation: chemokine transport and presentation by the endothelium. Blood. 2002;100:3853–3860. doi: 10.1182/blood.V100.12.3853. [DOI] [PubMed] [Google Scholar]
- 32.Rot A. Endothelial cell binding of NAP-1/IL-8: role in neutrophil emigration. Immunol Today. 1992;13:291–294. doi: 10.1016/0167-5699(92)90039-A. [DOI] [PubMed] [Google Scholar]
- 33.Rot A. Neutrophil attractant/activation protein-1 (interleukin-8) induces in vitro neutrophil migration by haptotactic mechanism. Eur J Immunol. 1993;23:303–306. doi: 10.1002/eji.1830230150. [DOI] [PubMed] [Google Scholar]
- 34.Wagner L, Yang OO, Garcia-Zepeda EA, Ge Y, Kalams SA, Walker BD, Pasternack MS, Luster AD. Beta-chemokines are released from HIV-1-specific cytolytic T-cell granules complexed to proteoglycans. Nature. 1998;391:908–911. doi: 10.1038/36129. [DOI] [PubMed] [Google Scholar]
- 35.Lau EK, Paavola CD, Johnson Z, Gaudry JP, Geretti E, Borlat F, Kungl AJ, Proudfoot AE, Handel TM. Identification of the glycosaminoglycan binding site of the CC chemokine, MCP-1: implications for structure and function in vivo. J Biol Chem. 2004;279:22294–22305. doi: 10.1074/jbc.M311224200. [DOI] [PubMed] [Google Scholar]
- 36.Wang L, Fuster M, Sriramarao P, Esko JD. Endothelial heparan sulfate deficiency impairs L-selectin- and chemokine-mediated neutrophil trafficking during inflammatory responses. Nat Immunol. 2005;6:902–910. doi: 10.1038/ni1233. [DOI] [PubMed] [Google Scholar]
- 37.Ernst CA, Zhang YJ, Hancock PR, Rutledge BJ, Corless CL, Rollins BJ. Biochemical and biologic characterization of murine monocyte chemoattractant protein-1. Identification of two functional domains. J Immunol. 1994;152:3541–3549. [PubMed] [Google Scholar]
- 38.Yao Y, Tsirka SE. The C terminus of mouse monocyte chemoattractant protein 1 (MCP1) mediates MCP1 dimerization while blocking its chemotactic potency. J Biol Chem. 2010;285:31509–31516. doi: 10.1074/jbc.M110.124891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang Y, Rollins BJ. A dominant negative inhibitor indicates that monocyte chemoattractant protein 1 functions as a dimer. Mol Cell Biol. 1995;15:4851–4855. doi: 10.1128/mcb.15.9.4851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Paavola CD, Hemmerich S, Grunberger D, Polsky I, Bloom A, Freedman R, Mulkins M, Bhakta S, McCarley D, Wiesent L, et al. Monomeric monocyte chemoattractant protein-1 (MCP-1) binds and activates the MCP-1 receptor CCR2B. J Biol Chem. 1998;273:33157–33165. doi: 10.1074/jbc.273.50.33157. [DOI] [PubMed] [Google Scholar]
- 41.Banisadr G, Queraud-Lesaux F, Boutterin MC, Pelaprat D, Zalc B, Rostene W, Haour F, Parsadaniantz SM. Distribution, cellular localization and functional role of CCR2 chemokine receptors in adult rat brain. J Neurochem. 2002;81:257–269. doi: 10.1046/j.1471-4159.2002.00809.x. [DOI] [PubMed] [Google Scholar]
- 42.Ge S, Song L, Serwanski DR, Kuziel WA, Pachter JS. Transcellular transport of CCL2 across brain microvascular endothelial cells. J Neurochem. 2008;104:1219–1232. doi: 10.1111/j.1471-4159.2007.05056.x. [DOI] [PubMed] [Google Scholar]
- 43.Gong JH, Ratkay LG, Waterfield JD, Clark-Lewis I. An antagonist of monocyte chemoattractant protein 1 (MCP-1) inhibits arthritis in the MRL-lpr mouse model. J Exp Med. 1997;186:131–137. doi: 10.1084/jem.186.1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gouwy M, Struyf S, Catusse J, Proost P, Van Damme J. Synergy between proinflammatory ligands of G protein-coupled receptors in neutrophil activation and migration. J Leukoc Biol. 2004;76:185–194. doi: 10.1189/jlb.1003479. [DOI] [PubMed] [Google Scholar]
- 45.Wain JH, Kirby JA, Ali S. Leucocyte chemotaxis: examination of mitogen-activated protein kinase and phosphoinositide 3-kinase activation by Monocyte Chemoattractant Proteins-1, -2, -3 and -4. Clin Exp Immunol. 2002;127:436–444. doi: 10.1046/j.1365-2249.2002.01764.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Charo IF, Myers SJ, Herman A, Franci C, Connolly AJ, Coughlin SR. Molecular cloning and functional expression of two monocyte chemoattractant protein 1 receptors reveals alternative splicing of the carboxyl-terminal tails. Proc Natl Acad Sci USA. 1994;91:2752–2756. doi: 10.1073/pnas.91.7.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bartoli C, Civatte M, Pellissier JF, Figarella-Branger D. CCR2A and CCR2B, the two isoforms of the monocyte chemoattractant protein-1 receptor are up-regulated and expressed by different cell subsets in idiopathic inflammatory myopathies. Acta Neuropathol. 2001;102:385–392. doi: 10.1007/s004010100394. [DOI] [PubMed] [Google Scholar]
- 48.Guillemin GJ, Brew BJ. Microglia, macrophages, perivascular macrophages, and pericytes: a review of function and identification. J Leukoc Biol. 2004;75:388–397. doi: 10.1189/jlb.0303114. [DOI] [PubMed] [Google Scholar]
- 49.Engelhardt B, Ransohoff RM. Capture, crawl, cross: the T cell code to breach the blood-brain barriers. Trends Immunol. 2012;33:579–589. doi: 10.1016/j.it.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 50.Barzo P, Marmarou A, Fatouros P, Hayasaki K, Corwin F. Contribution of vasogenic and cellular edema to traumatic brain swelling measured by diffusion-weighted imaging. J Neurosurg. 1997;87:900–907. doi: 10.3171/jns.1997.87.6.0900. [DOI] [PubMed] [Google Scholar]
- 51.Sixt M, Engelhardt B, Pausch F, Hallmann R, Wendler O, Sorokin LM. Endothelial cell laminin isoforms, laminins 8 and 10, play decisive roles in T cell recruitment across the blood-brain barrier in experimental autoimmune encephalomyelitis. J Cell Biol. 2001;153:933–946. doi: 10.1083/jcb.153.5.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Janzer RC, Raff MC. Astrocytes induce blood-brain barrier properties in endothelial cells. Nature. 1987;325:253–257. doi: 10.1038/325253a0. [DOI] [PubMed] [Google Scholar]
- 53.Papadopoulos MC, Saadoun S, Woodrow CJ, Davies DC, Costa-Martins P, Moss RF, Krishna S, Bell BA. Occludin expression in microvessels of neoplastic and non-neoplastic human brain. Neuropathol Appl Neurobiol. 2001;27:384–395. doi: 10.1046/j.0305-1846.2001.00341.x. [DOI] [PubMed] [Google Scholar]
- 54.Belayev L, Busto R, Zhao W, Ginsberg MD. Quantitative evaluation of blood-brain barrier permeability following middle cerebral artery occlusion in rats. Brain Res. 1996;739:88–96. doi: 10.1016/s0006-8993(96)00815-3. [DOI] [PubMed] [Google Scholar]
- 55.Benchenane K, Lopez-Atalaya JP, Fernandez-Monreal M, Touzani O, Vivien D. Equivocal roles of tissue-type plasminogen activator in stroke-induced injury. Trends Neurosci. 2004;27:155–160. doi: 10.1016/j.tins.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 56.Moskowitz MA, Lo EH, Iadecola C. The science of stroke: mechanisms in search of treatments. Neuron. 2010;67:181–198. doi: 10.1016/j.neuron.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bell RD, Winkler EA, Sagare AP, Singh I, LaRue B, Deane R, Zlokovic BV. Pericytes control key neurovascular functions and neuronal phenotype in the adult brain and during brain aging. Neuron. 2010;68:409–427. doi: 10.1016/j.neuron.2010.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Iadecola C. The overlap between neurodegenerative and vascular factors in the pathogenesis of dementia. Acta Neuropathol. 2010;120:287–296. doi: 10.1007/s00401-010-0718-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kortekaas R, Leenders KL, van Oostrom JC, Vaalburg W, Bart J, Willemsen AT, Hendrikse NH. Blood-brain barrier dysfunction in parkinsonian midbrain in vivo. Ann Neurol. 2005;57:176–179. doi: 10.1002/ana.20369. [DOI] [PubMed] [Google Scholar]
- 60.Selkoe DJ. Alzheimer disease: mechanistic understanding predicts novel therapies. Ann Intern Med. 2004;140:627–638. doi: 10.7326/0003-4819-140-8-200404200-00047. [DOI] [PubMed] [Google Scholar]
- 61.Zlokovic BV. Neurovascular mechanisms of Alzheimer’s neurodegeneration. Trends Neurosci. 2005;28:202–208. doi: 10.1016/j.tins.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 62.Garbuzova-Davis S, Rodrigues MC, Hernandez-Ontiveros DG, Louis MK, Willing AE, Borlongan CV, Sanberg PR. Amyotrophic lateral sclerosis: a neurovascular disease. Brain Res. 2011;1398:113–125. doi: 10.1016/j.brainres.2011.04.049. [DOI] [PubMed] [Google Scholar]
- 63.Blamire AM, Anthony DC, Rajagopalan B, Sibson NR, Perry VH, Styles P. Interleukin-1beta -induced changes in blood-brain barrier permeability, apparent diffusion coefficient, and cerebral blood volume in the rat brain: a magnetic resonance study. J Neurosci. 2000;20:8153–8159. doi: 10.1523/JNEUROSCI.20-21-08153.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Oshima T, Laroux FS, Coe LL, Morise Z, Kawachi S, Bauer P, Grisham MB, Specian RD, Carter P, Jennings S, et al. Interferon-gamma and interleukin-10 reciprocally regulate endothelial junction integrity and barrier function. Microvasc Res. 2001;61:130–143. doi: 10.1006/mvre.2000.2288. [DOI] [PubMed] [Google Scholar]
- 65.Stamatovic SM, Dimitrijevic OB, Keep RF, Andjelkovic AV. Protein kinase Calpha-RhoA cross-talk in CCL2-induced alterations in brain endothelial permeability. J Biol Chem. 2006;281:8379–8388. doi: 10.1074/jbc.M513122200. [DOI] [PubMed] [Google Scholar]
- 66.Stamatovic SM, Keep RF, Kunkel SL, Andjelkovic AV. Potential role of MCP-1 in endothelial cell tight junction ‘opening’: signaling via Rho and Rho kinase. J Cell Sci. 2003;116:4615–4628. doi: 10.1242/jcs.00755. [DOI] [PubMed] [Google Scholar]
- 67.Stamatovic SM, Shakui P, Keep RF, Moore BB, Kunkel SL, Van Rooijen N, Andjelkovic AV. Monocyte chemoattractant protein-1 regulation of blood-brain barrier permeability. J Cereb Blood Flow Metab. 2005;25:593–606. doi: 10.1038/sj.jcbfm.9600055. [DOI] [PubMed] [Google Scholar]
- 68.Wolburg H, Lippoldt A. Tight junctions of the blood-brain barrier: development, composition and regulation. Vascul Pharmacol. 2002;38:323–337. doi: 10.1016/s1537-1891(02)00200-8. [DOI] [PubMed] [Google Scholar]
- 69.Yang GY, Gong C, Qin Z, Liu XH, Lorris Betz A. Tumor necrosis factor alpha expression produces increased blood-brain barrier permeability following temporary focal cerebral ischemia in mice. Brain Res Mol Brain Res. 1999;69:135–143. doi: 10.1016/s0169-328x(99)00007-8. [DOI] [PubMed] [Google Scholar]
- 70.Yao Y, Tsirka SE. Mouse MCP1 C-terminus inhibits human MCP1-induced chemotaxis and BBB compromise. J Neurochem. 2011;118:215–223. doi: 10.1111/j.1471-4159.2011.07319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yao Y, Tsirka SE. Truncation of monocyte chemoattractant protein 1 by plasmin promotes blood-brain barrier disruption. J Cell Sci. 2011;124:1486–1495. doi: 10.1242/jcs.082834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dimitrijevic OB, Stamatovic SM, Keep RF, Andjelkovic AV. Effects of the chemokine CCL2 on blood-brain barrier permeability during ischemia-reperfusion injury. J Cereb Blood Flow Metab. 2006;26:797–810. doi: 10.1038/sj.jcbfm.9600229. [DOI] [PubMed] [Google Scholar]
- 73.Reijerkerk A, Kooij G, van der Pol SM, Leyen T, van Het Hof B, Couraud PO, Vivien D, Dijkstra CD, de Vries HE. Tissue-type plasminogen activator is a regulator of monocyte diapedesis through the brain endothelial barrier. J Immunol. 2008;181:3567–3574. doi: 10.4049/jimmunol.181.5.3567. [DOI] [PubMed] [Google Scholar]
- 74.Kataoka K, Asai T, Taneda M, Ueshima S, Matsuo O, Kuroda R, Kawabata A, Carmeliet P. Roles of urokinase type plasminogen activator in a brain stab wound. Brain Res. 2000;887:187–190. doi: 10.1016/s0006-8993(00)03042-0. [DOI] [PubMed] [Google Scholar]
- 75.Abbott NJ. Astrocyte-endothelial interactions and blood-brain barrier permeability. J Anat. 2002;200:629–638. doi: 10.1046/j.1469-7580.2002.00064.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fenstermacher J, Gross P, Sposito N, Acuff V, Pettersen S, Gruber K. Structural and functional variations in capillary systems within the brain. Ann NY Acad Sci. 1988;529:21–30. doi: 10.1111/j.1749-6632.1988.tb51416.x. [DOI] [PubMed] [Google Scholar]
- 77.Kniesel U, Wolburg H. Tight junctions of the blood-brain barrier. Cell Mol Neurobiol. 2000;20:57–76. doi: 10.1023/A:1006995910836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Oldendorf WH, Cornford ME, Brown WJ. The large apparent work capability of the blood-brain barrier: a study of the mitochondrial content of capillary endothelial cells in brain and other tissues of the rat. Ann Neurol. 1977;1:409–417. doi: 10.1002/ana.410010502. [DOI] [PubMed] [Google Scholar]
- 79.Sedlakova R, Shivers RR, Del Maestro RF. Ultrastructure of the blood-brain barrier in the rabbit. J Submicrosc Cytol Pathol. 1999;31:149–161. [PubMed] [Google Scholar]
- 80.Schulze C, Firth JA. Immunohistochemical localization of adherens junction components in blood-brain barrier microvessels of the rat. J Cell Sci. 1993;104(Pt 3):773–782. doi: 10.1242/jcs.104.3.773. [DOI] [PubMed] [Google Scholar]
- 81.Vorbrodt AW, Dobrogowska DH. Molecular anatomy of intercellular junctions in brain endothelial and epithelial barriers: electron microscopist’s view. Brain Res Brain Res Rev. 2003;42:221–242. doi: 10.1016/s0165-0173(03)00177-2. [DOI] [PubMed] [Google Scholar]
- 82.Bazzoni G, Dejana E. Endothelial cell-to-cell junctions: molecular organization and role in vascular homeostasis. Physiol Rev. 2004;84:869–901. doi: 10.1152/physrev.00035.2003. [DOI] [PubMed] [Google Scholar]
- 83.Romero IA, Radewicz K, Jubin E, Michel CC, Greenwood J, Couraud PO, Adamson P. Changes in cytoskeletal and tight junctional proteins correlate with decreased permeability induced by dexamethasone in cultured rat brain endothelial cells. Neurosci Lett. 2003;344:112–116. doi: 10.1016/s0304-3940(03)00348-3. [DOI] [PubMed] [Google Scholar]
- 84.Citi S, Cordenonsi M. Tight junction proteins. Biochim Biophys Acta. 1998;1448:1–11. doi: 10.1016/s0167-4889(98)00125-6. [DOI] [PubMed] [Google Scholar]
- 85.Huber JD, Egleton RD, Davis TP. Molecular physiology and pathophysiology of tight junctions in the blood-brain barrier. Trends Neurosci. 2001;24:719–725. doi: 10.1016/s0166-2236(00)02004-x. [DOI] [PubMed] [Google Scholar]
- 86.Forster C. Tight junctions and the modulation of barrier function in disease. Histochem Cell Biol. 2008;130:55–70. doi: 10.1007/s00418-008-0424-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Michel CC, Curry FE. Microvascular permeability. Physiol Rev. 1999;79:703–761. doi: 10.1152/physrev.1999.79.3.703. [DOI] [PubMed] [Google Scholar]
- 88.Mitic LL, Anderson JM. Molecular architecture of tight junctions. Annu Rev Physiol. 1998;60:121–142. doi: 10.1146/annurev.physiol.60.1.121. [DOI] [PubMed] [Google Scholar]
- 89.Ogunrinade O, Kameya GT, Truskey GA. Effect of fluid shear stress on the permeability of the arterial endothelium. Ann Biomed Eng. 2002;30:430–446. doi: 10.1114/1.1467924. [DOI] [PubMed] [Google Scholar]
- 90.Bolton SJ, Anthony DC, Perry VH. Loss of the tight junction proteins occludin and zonula occludens-1 from cerebral vascular endothelium during neutrophil-induced blood-brain barrier breakdown in vivo. Neuroscience. 1998;86:1245–1257. doi: 10.1016/s0306-4522(98)00058-x. [DOI] [PubMed] [Google Scholar]
- 91.Brown RC, Davis TP. Hypoxia/aglycemia alters expression of occludin and actin in brain endothelial cells. Biochem Biophys Res Commun. 2005;327:1114–1123. doi: 10.1016/j.bbrc.2004.12.123. [DOI] [PubMed] [Google Scholar]
- 92.Huber JD, Hau VS, Borg L, Campos CR, Egleton RD, Davis TP. Blood-brain barrier tight junctions are altered during a 72-h exposure to lambda-carrageenan-induced inflammatory pain. Am J Physiol Heart Circ Physiol. 2002;283:H1531–H1537. doi: 10.1152/ajpheart.00027.2002. [DOI] [PubMed] [Google Scholar]
- 93.McCarthy KM, Skare IB, Stankewich MC, Furuse M, Tsukita S, Rogers RA, Lynch RD, Schneeberger EE. Occludin is a functional component of the tight junction. J Cell Sci. 1996;109(Pt 9):2287–2298. doi: 10.1242/jcs.109.9.2287. [DOI] [PubMed] [Google Scholar]
- 94.Andreeva AY, Krause E, Muller EC, Blasig IE, Utepbergenov DI. Protein kinase C regulates the phosphorylation and cellular localization of occludin. J Biol Chem. 2001;276:38480–38486. doi: 10.1074/jbc.M104923200. [DOI] [PubMed] [Google Scholar]
- 95.Clarke H, Soler AP, Mullin JM. Protein kinase C activation leads to dephosphorylation of occludin and tight junction permeability increase in LLC-PK1 epithelial cell sheets. J Cell Sci. 2000;113(Pt 18):3187–3196. doi: 10.1242/jcs.113.18.3187. [DOI] [PubMed] [Google Scholar]
- 96.Hirase T, Kawashima S, Wong EY, Ueyama T, Rikitake Y, Tsukita S, Yokoyama M, Staddon JM. Regulation of tight junction permeability and occludin phosphorylation by Rhoa-p160ROCK-dependent and -independent mechanisms. J Biol Chem. 2001;276:10423–10431. doi: 10.1074/jbc.M007136200. [DOI] [PubMed] [Google Scholar]
- 97.Kale G, Naren AP, Sheth P, Rao RK. Tyrosine phosphorylation of occludin attenuates its interactions with ZO-1, ZO-2, and ZO-3. Biochem Biophys Res Commun. 2003;302:324–329. doi: 10.1016/s0006-291x(03)00167-0. [DOI] [PubMed] [Google Scholar]
- 98.Rao RK, Basuroy S, Rao VU, Karnaky KJ, Jr, Gupta A. Tyrosine phosphorylation and dissociation of occludin-ZO-1 and E-cadherin-beta-catenin complexes from the cytoskeleton by oxidative stress. Biochem J. 2002;368:471–481. doi: 10.1042/BJ20011804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sakakibara A, Furuse M, Saitou M, Ando-Akatsuka Y, Tsukita S. Possible involvement of phosphorylation of occludin in tight junction formation. J Cell Biol. 1997;137:1393–1401. doi: 10.1083/jcb.137.6.1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wachtel M, Frei K, Ehler E, Fontana A, Winterhalter K, Gloor SM. Occludin proteolysis and increased permeability in endothelial cells through tyrosine phosphatase inhibition. J Cell Sci. 1999;112(Pt 23):4347–4356. doi: 10.1242/jcs.112.23.4347. [DOI] [PubMed] [Google Scholar]
- 101.Stevenson BR, Siliciano JD, Mooseker MS, Goodenough DA. Identification of ZO-1: a high molecular weight polypeptide associated with the tight junction (zonula occludens) in a variety of epithelia. J Cell Biol. 1986;103:755–766. doi: 10.1083/jcb.103.3.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fanning AS, Jameson BJ, Jesaitis LA, Anderson JM. The tight junction protein ZO-1 establishes a link between the transmembrane protein occludin and the actin cytoskeleton. J Biol Chem. 1998;273:29745–29753. doi: 10.1074/jbc.273.45.29745. [DOI] [PubMed] [Google Scholar]
- 103.Abbruscato TJ, Lopez SP, Mark KS, Hawkins BT, Davis TP. Nicotine and cotinine modulate cerebral microvascular permeability and protein expression of ZO-1 through nicotinic acetylcholine receptors expressed on brain endothelial cells. J Pharm Sci. 2002;91:2525–2538. doi: 10.1002/jps.10256. [DOI] [PubMed] [Google Scholar]
- 104.Fischer S, Wobben M, Marti HH, Renz D, Schaper W. Hypoxia-induced hyperpermeability in brain microvessel endothelial cells involves VEGF-mediated changes in the expression of zonula occludens-1. Microvasc Res. 2002;63:70–80. doi: 10.1006/mvre.2001.2367. [DOI] [PubMed] [Google Scholar]
- 105.Mark KS, Davis TP. Cerebral microvascular changes in permeability and tight junctions induced by hypoxia-reoxygenation. Am J Physiol Heart Circ Physiol. 2002;282:H1485–H1494. doi: 10.1152/ajpheart.00645.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Balda MS, Matter K. The tight junction protein ZO-1 and an interacting transcription factor regulate ErbB-2 expression. EMBO J. 2000;19:2024–2033. doi: 10.1093/emboj/19.9.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gottardi CJ, Arpin M, Fanning AS, Louvard D. The junction-associated protein, zonula occludens-1, localizes to the nucleus before the maturation and during the remodeling of cell–cell contacts. Proc Natl Acad Sci USA. 1996;93:10779–10784. doi: 10.1073/pnas.93.20.10779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hawkins BT, Abbruscato TJ, Egleton RD, Brown RC, Huber JD, Campos CR, Davis TP. Nicotine increases in vivo blood-brain barrier permeability and alters cerebral microvascular tight junction protein distribution. Brain Res. 2004;1027:48–58. doi: 10.1016/j.brainres.2004.08.043. [DOI] [PubMed] [Google Scholar]
- 109.Riesen FK, Rothen-Rutishauser B, Wunderli-Allenspach H. A ZO1-GFP fusion protein to study the dynamics of tight junctions in living cells. Histochem Cell Biol. 2002;117:307–315. doi: 10.1007/s00418-002-0398-y. [DOI] [PubMed] [Google Scholar]
- 110.Clarke H, Marano CW, Peralta Soler A, Mullin JM. Modification of tight junction function by protein kinase C isoforms. Adv Drug Deliv Rev. 2000;41:283–301. doi: 10.1016/s0169-409x(00)00047-8. [DOI] [PubMed] [Google Scholar]
- 111.Farshori P, Kachar B. Redistribution and phosphorylation of occludin during opening and resealing of tight junctions in cultured epithelial cells. J Membr Biol. 1999;170:147–156. doi: 10.1007/s002329900544. [DOI] [PubMed] [Google Scholar]
- 112.Ward PD, Klein RR, Troutman MD, Desai S, Thakker DR. Phospholipase C-gamma modulates epithelial tight junction permeability through hyperphosphorylation of tight junction proteins. J Biol Chem. 2002;277:35760–35765. doi: 10.1074/jbc.M203134200. [DOI] [PubMed] [Google Scholar]
- 113.Tsukamoto T, Nigam SK. Tight junction proteins form large complexes and associate with the cytoskeleton in an ATP depletion model for reversible junction assembly. J Biol Chem. 1997;272:16133–16139. doi: 10.1074/jbc.272.26.16133. [DOI] [PubMed] [Google Scholar]
- 114.Tsukamoto T, Nigam SK. Role of tyrosine phosphorylation in the reassembly of occludin and other tight junction proteins. Am J Physiol. 1999;276:F737–F750. doi: 10.1152/ajprenal.1999.276.5.F737. [DOI] [PubMed] [Google Scholar]
- 115.Harhaj NS, Barber AJ, Antonetti DA. Platelet-derived growth factor mediates tight junction redistribution and increases permeability in MDCK cells. J Cell Physiol. 2002;193:349–364. doi: 10.1002/jcp.10183. [DOI] [PubMed] [Google Scholar]
- 116.Pedram A, Razandi M, Levin ER. Deciphering vascular endothelial cell growth factor/vascular permeability factor signaling to vascular permeability. Inhibition by atrial natriuretic peptide. J Biol Chem. 2002;277:44385–44398. doi: 10.1074/jbc.M202391200. [DOI] [PubMed] [Google Scholar]
- 117.Hicks K, O’Neil RG, Dubinsky WS, Brown RC. TRPC-mediated actin-myosin contraction is critical for BBB disruption following hypoxic stress. Am J Physiol Cell Physiol. 2010;298:C1583–C1593. doi: 10.1152/ajpcell.00458.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Stephan CC, Brock TA. Vascular endothelial growth factor, a multifunctional polypeptide. PR Health Sci J. 1996;15:169–178. [PubMed] [Google Scholar]
- 119.van Nieuw Amerongen GP, van Delft S, Vermeer MA, Collard JG, van Hinsbergh VW. Activation of RhoA by thrombin in endothelial hyperpermeability: role of Rho kinase and protein tyrosine kinases. Circ Res. 2000;87:335–340. doi: 10.1161/01.res.87.4.335. [DOI] [PubMed] [Google Scholar]
- 120.Bretscher A, Gary R, Berryman M. Soluble ezrin purified from placenta exists as stable monomers and elongated dimers with masked C-terminal ezrin-radixin-moesin association domains. Biochemistry. 1995;34:16830–16837. doi: 10.1021/bi00051a034. [DOI] [PubMed] [Google Scholar]
- 121.Louvet-Vallee S. ERM proteins: from cellular architecture to cell signaling. Biol Cell. 2000;92:305–316. doi: 10.1016/s0248-4900(00)01078-9. [DOI] [PubMed] [Google Scholar]
- 122.Pearson MA, Reczek D, Bretscher A, Karplus PA. Structure of the ERM protein moesin reveals the FERM domain fold masked by an extended actin binding tail domain. Cell. 2000;101:259–270. doi: 10.1016/s0092-8674(00)80836-3. [DOI] [PubMed] [Google Scholar]
- 123.Stewart PA, Wiley MJ. Developing nervous tissue induces formation of blood-brain barrier characteristics in invading endothelial cells: a study using quail–chick transplantation chimeras. Dev Biol. 1981;84:183–192. doi: 10.1016/0012-1606(81)90382-1. [DOI] [PubMed] [Google Scholar]
- 124.Kacem K, Lacombe P, Seylaz J, Bonvento G. Structural organization of the perivascular astrocyte endfeet and their relationship with the endothelial glucose transporter: a confocal microscopy study. Glia. 1998;23:1–10. [PubMed] [Google Scholar]
- 125.Simard M, Arcuino G, Takano T, Liu QS, Nedergaard M. Signaling at the gliovascular interface. J Neurosci. 2003;23:9254–9262. doi: 10.1523/JNEUROSCI.23-27-09254.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cohen-Kashi Malina K, Cooper I, Teichberg VI. Closing the gap between the in vivo and in vitro blood-brain barrier tightness. Brain Res. 2009;1284:12–21. doi: 10.1016/j.brainres.2009.05.072. [DOI] [PubMed] [Google Scholar]
- 127.Jain RK, di Tomaso E, Duda DG, Loeffler JS, Sorensen AG, Batchelor TT. Angiogenesis in brain tumours. Nat Rev Neurosci. 2007;8:610–622. doi: 10.1038/nrn2175. [DOI] [PubMed] [Google Scholar]
- 128.Siddharthan V, Kim YV, Liu S, Kim KS. Human astrocytes/astrocyte-conditioned medium and shear stress enhance the barrier properties of human brain microvascular endothelial cells. Brain Res. 2007;1147:39–50. doi: 10.1016/j.brainres.2007.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Tao-Cheng JH, Nagy Z, Brightman MW. Tight junctions of brain endothelium in vitro are enhanced by astroglia. J Neurosci. 1987;7:3293–3299. doi: 10.1523/JNEUROSCI.07-10-03293.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Willis CL, Nolan CC, Reith SN, Lister T, Prior MJ, Guerin CJ, Mavroudis G, Ray DE. Focal astrocyte loss is followed by microvascular damage, with subsequent repair of the blood-brain barrier in the apparent absence of direct astrocytic contact. Glia. 2004;45:325–337. doi: 10.1002/glia.10333. [DOI] [PubMed] [Google Scholar]
- 131.Cardoso FL, Brites D, Brito MA. Looking at the blood-brain barrier: molecular anatomy and possible investigation approaches. Brain Res Rev. 2010;64:328–363. doi: 10.1016/j.brainresrev.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 132.Persidsky Y, Ramirez SH, Haorah J, Kanmogne GD. Blood-brain barrier: structural components and function under physiologic and pathologic conditions. J Neuroimmune Pharmacol. 2006;1:223–236. doi: 10.1007/s11481-006-9025-3. [DOI] [PubMed] [Google Scholar]
- 133.Quaegebeur A, Lange C, Carmeliet P. The neurovascular link in health and disease: molecular mechanisms and therapeutic implications. Neuron. 2011;71:406–424. doi: 10.1016/j.neuron.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 134.Lai CH, Kuo KH. The critical component to establish in vitro BBB model: pericyte. Brain Res Brain Res Rev. 2005;50:258–265. doi: 10.1016/j.brainresrev.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 135.Wolburg H, Wolburg-Buchholz K, Fallier-Becker P, Noell S, Mack AF. Structure and functions of aquaporin-4-based orthogonal arrays of particles. Int Rev Cell Mol Biol. 2011;287:1–41. doi: 10.1016/B978-0-12-386043-9.00001-3. [DOI] [PubMed] [Google Scholar]
- 136.Daneman R, Zhou L, Kebede AA, Barres BA. Pericytes are required for blood-brain barrier integrity during embryogenesis. Nature. 2010;468:562–566. doi: 10.1038/nature09513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Krum JM, Kenyon KL, Rosenstein JM. Expression of blood-brain barrier characteristics following neuronal loss and astroglial damage after administration of anti-Thy-1 immunotoxin. Exp Neurol. 1997;146:33–45. doi: 10.1006/exnr.1997.6528. [DOI] [PubMed] [Google Scholar]
- 138.Menetski J, Mistry S, Lu M, Mudgett JS, Ransohoff RM, Demartino JA, Macintyre DE, Abbadie C. Mice overexpressing chemokine ligand 2 (CCL2) in astrocytes display enhanced nociceptive responses. Neuroscience. 2007;149:706–714. doi: 10.1016/j.neuroscience.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 139.Huang D, Wujek J, Kidd G, He TT, Cardona A, Sasse ME, Stein EJ, Kish J, Tani M, Charo IF, et al. Chronic expression of monocyte chemoattractant protein-1 in the central nervous system causes delayed encephalopathy and impaired microglial function in mice. FASEB J. 2005;19:761–772. doi: 10.1096/fj.04-3104com. [DOI] [PubMed] [Google Scholar]
- 140.Fouillet A, Mawson J, Suliman O, Sharrack B, Romero IA, Woodroofe MN. CCL2 binding is CCR2 independent in primary adult human astrocytes. Brain Res. 2012;1437:115–126. doi: 10.1016/j.brainres.2011.11.049. [DOI] [PubMed] [Google Scholar]
- 141.Quinones MP, Kalkonde Y, Estrada CA, Jimenez F, Ramirez R, Mahimainathan L, Mummidi S, Choudhury GG, Martinez H, Adams L, et al. Role of astrocytes and chemokine systems in acute TNFalpha induced demyelinating syndrome: CCR2-dependent signals promote astrocyte activation and survival via NF-kappaB and Akt. Mol Cell Neurosci. 2008;37:96–109. doi: 10.1016/j.mcn.2007.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ge S, Pachter JS. Caveolin-1 knockdown by small interfering RNA suppresses responses to the chemokine monocyte chemoattractant protein-1 by human astrocytes. J Biol Chem. 2004;279:6688–6695. doi: 10.1074/jbc.M311769200. [DOI] [PubMed] [Google Scholar]
- 143.Owens T, Bechmann I, Engelhardt B. Perivascular spaces and the two steps to neuroinflammation. J Neuropathol Exp Neurol. 2008;67:1113–1121. doi: 10.1097/NEN.0b013e31818f9ca8. [DOI] [PubMed] [Google Scholar]
- 144.Agrawal S, Anderson P, Durbeej M, van Rooijen N, Ivars F, Opdenakker G, Sorokin LM. Dystroglycan is selectively cleaved at the parenchymal basement membrane at sites of leukocyte extravasation in experimental autoimmune encephalomyelitis. J Exp Med. 2006;203:1007–1019. doi: 10.1084/jem.20051342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Baumann E, Preston E, Slinn J, Stanimirovic D. Post-ischemic hypothermia attenuates loss of the vascular basement membrane proteins, agrin and SPARC, and the blood-brain barrier disruption after global cerebral ischemia. Brain Res. 2009;1269:185–197. doi: 10.1016/j.brainres.2009.02.062. [DOI] [PubMed] [Google Scholar]
- 146.Fukuda S, Fini CA, Mabuchi T, Koziol JA, Eggleston LL, Jr, del Zoppo GJ. Focal cerebral ischemia induces active proteases that degrade microvascular matrix. Stroke. 2004;35:998–1004. doi: 10.1161/01.STR.0000119383.76447.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Yurchenco PD, Amenta PS, Patton BL. Basement membrane assembly, stability and activities observed through a developmental lens. Matrix Biol. 2004;22:521–538. doi: 10.1016/j.matbio.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 148.Yurchenco PD, Patton BL. Developmental and pathogenic mechanisms of basement membrane assembly. Curr Pharm Des. 2009;15:1277–1294. doi: 10.2174/138161209787846766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.van Horssen J, Bo L, Vos CM, Virtanen I, de Vries HE. Basement membrane proteins in multiple sclerosis-associated inflammatory cuffs: potential role in influx and transport of leukocytes. J Neuropathol Exp Neurol. 2005;64:722–729. doi: 10.1097/01.jnen.0000173894.09553.13. [DOI] [PubMed] [Google Scholar]
- 150.Barber AJ, Lieth E. Agrin accumulates in the brain microvascular basal lamina during development of the blood-brain barrier. Dev Dyn. 1997;208:62–74. doi: 10.1002/(SICI)1097-0177(199701)208:1<62::AID-AJA6>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 151.del Zoppo GJ. Relationship of neurovascular elements to neuron injury during ischemia. Cerebrovasc Dis. 2009;27(Suppl 1):65–76. doi: 10.1159/000200442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Del Zoppo GJ, Milner R, Mabuchi T, Hung S, Wang X, Koziol JA. Vascular matrix adhesion and the blood-brain barrier. Biochem Soc Trans. 2006;34:1261–1266. doi: 10.1042/BST0341261. [DOI] [PubMed] [Google Scholar]
- 153.Kwon I, Kim EH, del Zoppo GJ, Heo JH. Ultrastructural and temporal changes of the microvascular basement membrane and astrocyte interface following focal cerebral ischemia. J Neurosci Res. 2009;87:668–676. doi: 10.1002/jnr.21877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Lo EH, Rosenberg GA. The neurovascular unit in health and disease: introduction. Stroke. 2009;40:S2–S3. doi: 10.1161/STROKEAHA.108.534404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Wang CX, Shuaib A. Critical role of microvasculature basal lamina in ischemic brain injury. Prog Neurobiol. 2007;83:140–148. doi: 10.1016/j.pneurobio.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 156.Zhang X, Winkles JA, Gongora MC, Polavarapu R, Michaelson JS, Hahm K, Burkly L, Friedman M, Li XJ, Yepes M. TWEAK-Fn14 pathway inhibition protects the integrity of the neurovascular unit during cerebral ischemia. J Cereb Blood Flow Metab. 2007;27:534–544. doi: 10.1038/sj.jcbfm.9600368. [DOI] [PubMed] [Google Scholar]
- 157.Tilling T, Engelbertz C, Decker S, Korte D, Huwel S, Galla HJ. Expression and adhesive properties of basement membrane proteins in cerebral capillary endothelial cell cultures. Cell Tissue Res. 2002;310:19–29. doi: 10.1007/s00441-002-0604-1. [DOI] [PubMed] [Google Scholar]
- 158.Tilling T, Korte D, Hoheisel D, Galla HJ. Basement membrane proteins influence brain capillary endothelial barrier function in vitro. J Neurochem. 1998;71:1151–1157. doi: 10.1046/j.1471-4159.1998.71031151.x. [DOI] [PubMed] [Google Scholar]
- 159.Kim DS, Kang SI, Lee SY, Noh KT, Kim EC (2013). Involvement of SDF-1 and monocyte chemoattractant protein-1 in hydrogen peroxide-induced extracellular matrix degradation in human dental pulp cells. Int Endod J (in press) [DOI] [PubMed]
- 160.Park J, Ryu DR, Li JJ, Jung DS, Kwak SJ, Lee SH, Yoo TH, Han SH, Lee JE, Kim DK, et al. MCP-1/CCR2 system is involved in high glucose-induced fibronectin and type IV collagen expression in cultured mesangial cells. Am J Physiol Renal Physiol. 2008;295:F749–F757. doi: 10.1152/ajprenal.00547.2007. [DOI] [PubMed] [Google Scholar]
- 161.Arai M, Ikawa Y, Chujo S, Hamaguchi Y, Ishida W, Shirasaki F, Hasegawa M, Mukaida N, Fujimoto M, Takehara K. Chemokine receptors CCR2 and CX3CR1 regulate skin fibrosis in the mouse model of cytokine-induced systemic sclerosis. J Dermatol Sci. 2013;69:250–258. doi: 10.1016/j.jdermsci.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 162.Lee SH, Kang HY, Kim KS, Nam BY, Paeng J, Kim S, Li JJ, Park JT, Kim DK, Han SH, et al. The monocyte chemoattractant protein-1 (MCP-1)/CCR2 system is involved in peritoneal dialysis-related epithelial-mesenchymal transition of peritoneal mesothelial cells. Lab Invest. 2012;92:1698–1711. doi: 10.1038/labinvest.2012.132. [DOI] [PubMed] [Google Scholar]
- 163.Greenlee KJ, Werb Z, Kheradmand F. Matrix metalloproteinases in lung: multiple, multifarious, and multifaceted. Physiol Rev. 2007;87:69–98. doi: 10.1152/physrev.00022.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Stamenkovic I. Extracellular matrix remodelling: the role of matrix metalloproteinases. J Pathol. 2003;200:448–464. doi: 10.1002/path.1400. [DOI] [PubMed] [Google Scholar]
- 165.Rouget C. Mémoire sur le développement, la structure et les propriétés physiologiques des capillaires sanguins et lymphatiques. Archs Physiol Norm Pathol. 1873;5:603–663. [Google Scholar]
- 166.Sa-Pereira I, Brites D, Brito MA. Neurovascular unit: a focus on pericytes. Mol Neurobiol. 2012;45:327–347. doi: 10.1007/s12035-012-8244-2. [DOI] [PubMed] [Google Scholar]
- 167.Armulik A, Genove G, Betsholtz C. Pericytes: developmental, physiological, and pathological perspectives, problems, and promises. Dev Cell. 2011;21:193–215. doi: 10.1016/j.devcel.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 168.Dalkara T, Gursoy-Ozdemir Y, Yemisci M. Brain microvascular pericytes in health and disease. Acta Neuropathol. 2011;122:1–9. doi: 10.1007/s00401-011-0847-6. [DOI] [PubMed] [Google Scholar]
- 169.Dore-Duffy P. Pericytes: pluripotent cells of the blood brain barrier. Curr Pharm Des. 2008;14:1581–1593. doi: 10.2174/138161208784705469. [DOI] [PubMed] [Google Scholar]
- 170.Dore-Duffy P, Cleary K. Morphology and properties of pericytes. Methods Mol Biol. 2011;686:49–68. doi: 10.1007/978-1-60761-938-3_2. [DOI] [PubMed] [Google Scholar]
- 171.Engelhardt B, Sorokin L. The blood-brain and the blood-cerebrospinal fluid barriers: function and dysfunction. Semin Immunopathol. 2009;31:497–511. doi: 10.1007/s00281-009-0177-0. [DOI] [PubMed] [Google Scholar]
- 172.Frank RN, Dutta S, Mancini MA. Pericyte coverage is greater in the retinal than in the cerebral capillaries of the rat. Invest Ophthalmol Vis Sci. 1987;28:1086–1091. [PubMed] [Google Scholar]
- 173.Fisher M. Pericyte signaling in the neurovascular unit. Stroke. 2009;40:S13–S15. doi: 10.1161/STROKEAHA.108.533117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Krueger M, Bechmann I. CNS pericytes: concepts, misconceptions, and a way out. Glia. 2010;58:1–10. doi: 10.1002/glia.20898. [DOI] [PubMed] [Google Scholar]
- 175.Nehls V, Drenckhahn D. The versatility of microvascular pericytes: from mesenchyme to smooth muscle? Histochemistry. 1993;99:1–12. doi: 10.1007/BF00268014. [DOI] [PubMed] [Google Scholar]
- 176.Lindahl P, Johansson BR, Leveen P, Betsholtz C. Pericyte loss and microaneurysm formation in PDGF-B-deficient mice. Science. 1997;277:242–245. doi: 10.1126/science.277.5323.242. [DOI] [PubMed] [Google Scholar]
- 177.Nehls V, Denzer K, Drenckhahn D. Pericyte involvement in capillary sprouting during angiogenesis in situ. Cell Tissue Res. 1992;270:469–474. doi: 10.1007/BF00645048. [DOI] [PubMed] [Google Scholar]
- 178.Dermietzel R, Krause D. Molecular anatomy of the blood-brain barrier as defined by immunocytochemistry. Int Rev Cytol. 1991;127:57–109. doi: 10.1016/s0074-7696(08)60692-0. [DOI] [PubMed] [Google Scholar]
- 179.Kunz J, Krause D, Kremer M, Dermietzel R. The 140-kDa protein of blood-brain barrier-associated pericytes is identical to aminopeptidase N. J Neurochem. 1994;62:2375–2386. doi: 10.1046/j.1471-4159.1994.62062375.x. [DOI] [PubMed] [Google Scholar]
- 180.Huang FJ, You WK, Bonaldo P, Seyfried TN, Pasquale EB, Stallcup WB. Pericyte deficiencies lead to aberrant tumor vascularizaton in the brain of the NG2 null mouse. Dev Biol. 2010;344:1035–1046. doi: 10.1016/j.ydbio.2010.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Ozerdem U, Grako KA, Dahlin-Huppe K, Monosov E, Stallcup WB. NG2 proteoglycan is expressed exclusively by mural cells during vascular morphogenesis. Dev Dyn. 2001;222:218–227. doi: 10.1002/dvdy.1200. [DOI] [PubMed] [Google Scholar]
- 182.Bondjers C, Kalen M, Hellstrom M, Scheidl SJ, Abramsson A, Renner O, Lindahl P, Cho H, Kehrl J, Betsholtz C. Transcription profiling of platelet-derived growth factor-B-deficient mouse embryos identifies RGS5 as a novel marker for pericytes and vascular smooth muscle cells. Am J Pathol. 2003;162:721–729. doi: 10.1016/S0002-9440(10)63868-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Cho H, Kozasa T, Bondjers C, Betsholtz C, Kehrl JH. Pericyte-specific expression of Rgs5: implications for PDGF and EDG receptor signaling during vascular maturation. FASEB J. 2003;17:440–442. doi: 10.1096/fj.02-0340fje. [DOI] [PubMed] [Google Scholar]
- 184.Bandopadhyay R, Orte C, Lawrenson JG, Reid AR, De Silva S, Allt G. Contractile proteins in pericytes at the blood-brain and blood-retinal barriers. J Neurocytol. 2001;30:35–44. doi: 10.1023/a:1011965307612. [DOI] [PubMed] [Google Scholar]
- 185.Nehls V, Drenckhahn D. Heterogeneity of microvascular pericytes for smooth muscle type alpha-actin. J Cell Biol. 1991;113:147–154. doi: 10.1083/jcb.113.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Thanabalasundaram G, Schneidewind J, Pieper C, Galla HJ. The impact of pericytes on the blood-brain barrier integrity depends critically on the pericyte differentiation stage. Int J Biochem Cell Biol. 2011;43:1284–1293. doi: 10.1016/j.biocel.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 187.Etchevers HC, Vincent C, Le Douarin NM, Couly GF. The cephalic neural crest provides pericytes and smooth muscle cells to all blood vessels of the face and forebrain. Development. 2001;128:1059–1068. doi: 10.1242/dev.128.7.1059. [DOI] [PubMed] [Google Scholar]
- 188.Heglind M, Cederberg A, Aquino J, Lucas G, Ernfors P, Enerback S. Lack of the central nervous system- and neural crest-expressed forkhead gene Foxs1 affects motor function and body weight. Mol Cell Biol. 2005;25:5616–5625. doi: 10.1128/MCB.25.13.5616-5625.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Korn J, Christ B, Kurz H. Neuroectodermal origin of brain pericytes and vascular smooth muscle cells. J Comp Neurol. 2002;442:78–88. doi: 10.1002/cne.1423. [DOI] [PubMed] [Google Scholar]
- 190.Que J, Wilm B, Hasegawa H, Wang F, Bader D, Hogan BL. Mesothelium contributes to vascular smooth muscle and mesenchyme during lung development. Proc Natl Acad Sci USA. 2008;105:16626–16630. doi: 10.1073/pnas.0808649105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Asahina K, Zhou B, Pu WT, Tsukamoto H. Septum transversum-derived mesothelium gives rise to hepatic stellate cells and perivascular mesenchymal cells in developing mouse liver. Hepatology. 2011;53:983–995. doi: 10.1002/hep.24119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Wilm B, Ipenberg A, Hastie ND, Burch JB, Bader DM. The serosal mesothelium is a major source of smooth muscle cells of the gut vasculature. Development. 2005;132:5317–5328. doi: 10.1242/dev.02141. [DOI] [PubMed] [Google Scholar]
- 193.Hess DC, Abe T, Hill WD, Studdard AM, Carothers J, Masuya M, Fleming PA, Drake CJ, Ogawa M. Hematopoietic origin of microglial and perivascular cells in brain. Exp Neurol. 2004;186:134–144. doi: 10.1016/j.expneurol.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 194.Dore-Duffy P, Katychev A, Wang X, Van Buren E. CNS microvascular pericytes exhibit multipotential stem cell activity. J Cereb Blood Flow Metab. 2006;26:613–624. doi: 10.1038/sj.jcbfm.9600272. [DOI] [PubMed] [Google Scholar]
- 195.Dente CJ, Steffes CP, Speyer C, Tyburski JG. Pericytes augment the capillary barrier in in vitro cocultures. J Surg Res. 2001;97:85–91. doi: 10.1006/jsre.2001.6117. [DOI] [PubMed] [Google Scholar]
- 196.Nakagawa S, Deli MA, Kawaguchi H, Shimizudani T, Shimono T, Kittel A, Tanaka K, Niwa M. A new blood-brain barrier model using primary rat brain endothelial cells, pericytes and astrocytes. Neurochem Int. 2009;54:253–263. doi: 10.1016/j.neuint.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 197.Dohgu S, Takata F, Yamauchi A, Nakagawa S, Egawa T, Naito M, Tsuruo T, Sawada Y, Niwa M, Kataoka Y. Brain pericytes contribute to the induction and up-regulation of blood-brain barrier functions through transforming growth factor-beta production. Brain Res. 2005;1038:208–215. doi: 10.1016/j.brainres.2005.01.027. [DOI] [PubMed] [Google Scholar]
- 198.Edelman DA, Jiang Y, Tyburski J, Wilson RF, Steffes C. Pericytes and their role in microvasculature homeostasis. J Surg Res. 2006;135:305–311. doi: 10.1016/j.jss.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 199.Peppiatt CM, Howarth C, Mobbs P, Attwell D. Bidirectional control of CNS capillary diameter by pericytes. Nature. 2006;443:700–704. doi: 10.1038/nature05193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Armulik A, Genove G, Mae M, Nisancioglu MH, Wallgard E, Niaudet C, He L, Norlin J, Lindblom P, Strittmatter K, et al. Pericytes regulate the blood-brain barrier. Nature. 2010;468:557–561. doi: 10.1038/nature09522. [DOI] [PubMed] [Google Scholar]
- 201.Dore-Duffy P, Owen C, Balabanov R, Murphy S, Beaumont T, Rafols JA. Pericyte migration from the vascular wall in response to traumatic brain injury. Microvasc Res. 2000;60:55–69. doi: 10.1006/mvre.2000.2244. [DOI] [PubMed] [Google Scholar]
- 202.Gonul E, Duz B, Kahraman S, Kayali H, Kubar A, Timurkaynak E. Early pericyte response to brain hypoxia in cats: an ultrastructural study. Microvasc Res. 2002;64:116–119. doi: 10.1006/mvre.2002.2413. [DOI] [PubMed] [Google Scholar]
- 203.Chen YT, Chang FC, Wu CF, Chou YH, Hsu HL, Chiang WC, Shen J, Chen YM, Wu KD, Tsai TJ, et al. Platelet-derived growth factor receptor signaling activates pericyte-myofibroblast transition in obstructive and post-ischemic kidney fibrosis. Kidney Int. 2011;80:1170–1181. doi: 10.1038/ki.2011.208. [DOI] [PubMed] [Google Scholar]
- 204.Sheehan JJ, Zhou C, Gravanis I, Rogove AD, Wu YP, Bogenhagen DF, Tsirka SE. Proteolytic activation of monocyte chemoattractant protein-1 by plasmin underlies excitotoxic neurodegeneration in mice. J Neurosci. 2007;27:1738–1745. doi: 10.1523/JNEUROSCI.4987-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Zhang SX, Wang JJ, Dashti A, Wilson K, Zou MH, Szweda L, Ma JX, Lyons TJ. Pigment epithelium-derived factor mitigates inflammation and oxidative stress in retinal pericytes exposed to oxidized low-density lipoprotein. J Mol Endocrinol. 2008;41:135–143. doi: 10.1677/JME-08-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Chan WY, Kohsaka S, Rezaie P. The origin and cell lineage of microglia: new concepts. Brain Res Rev. 2007;53:344–354. doi: 10.1016/j.brainresrev.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 207.Hailer NP, Heppner FL, Haas D, Nitsch R. Fluorescent dye prelabelled microglial cells migrate into organotypic hippocampal slice cultures and ramify. Eur J Neurosci. 1997;9:863–866. doi: 10.1111/j.1460-9568.1997.tb01436.x. [DOI] [PubMed] [Google Scholar]
- 208.Ling EA. Transformation of monocytes into amoeboid microglia in the corpus callosum of postnatal rats, as shown by labelling monocytes by carbon particles. J Anat. 1979;128:847–858. [PMC free article] [PubMed] [Google Scholar]
- 209.Ono K, Takii T, Onozaki K, Ikawa M, Okabe M, Sawada M. Migration of exogenous immature hematopoietic cells into adult mouse brain parenchyma under GFP-expressing bone marrow chimera. Biochem Biophys Res Commun. 1999;262:610–614. doi: 10.1006/bbrc.1999.1223. [DOI] [PubMed] [Google Scholar]
- 210.Wu YP, McMahon E, Kraine MR, Tisch R, Meyers A, Frelinger J, Matsushima GK, Suzuki K. Distribution and characterization of GFP(+) donor hematogenous cells in Twitcher mice after bone marrow transplantation. Am J Pathol. 2000;156:1849–1854. doi: 10.1016/S0002-9440(10)65058-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Ginhoux F, Greter M, Leboeuf M, Nandi S, See P, Gokhan S, Mehler MF, Conway SJ, Ng LG, Stanley ER, et al. Fate mapping analysis reveals that adult microglia derive from primitive macrophages. Science. 2010;330:841–845. doi: 10.1126/science.1194637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Buza-Vidas N, Woll P, Hultquist A, Duarte S, Lutteropp M, Bouriez-Jones T, Ferry H, Luc S, Jacobsen SE. FLT3 expression initiates in fully multipotent mouse hematopoietic progenitor cells. Blood. 2011;118:1544–1548. doi: 10.1182/blood-2010-10-316232. [DOI] [PubMed] [Google Scholar]
- 213.Erblich B, Zhu L, Etgen AM, Dobrenis K, Pollard JW. Absence of colony stimulation factor-1 receptor results in loss of microglia, disrupted brain development and olfactory deficits. PLoS ONE. 2011;6:e26317. doi: 10.1371/journal.pone.0026317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Gomez Perdiguero E, Schulz C, Geissmann F. Development and homeostasis of “resident” myeloid cells: the case of the microglia. Glia. 2013;61:112–120. doi: 10.1002/glia.22393. [DOI] [PubMed] [Google Scholar]
- 215.Qian BZ, Li J, Zhang H, Kitamura T, Zhang J, Campion LR, Kaiser EA, Snyder LA, Pollard JW. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature. 2011;475:222–225. doi: 10.1038/nature10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Schulz C, Gomez Perdiguero E, Chorro L, Szabo-Rogers H, Cagnard N, Kierdorf K, Prinz M, Wu B, Jacobsen SE, Pollard JW, et al. A lineage of myeloid cells independent of Myb and hematopoietic stem cells. Science. 2012;336:86–90. doi: 10.1126/science.1219179. [DOI] [PubMed] [Google Scholar]
- 217.Nimmerjahn A, Kirchhoff F, Helmchen F. Resting microglial cells are highly dynamic surveillants of brain parenchyma in vivo. Science. 2005;308:1314–1318. doi: 10.1126/science.1110647. [DOI] [PubMed] [Google Scholar]
- 218.Abromson-Leeman S, Hayashi M, Martin C, Sobel R, al-Sabbagh A, Weiner H, Dorf ME. T cell responses to myelin basic protein in experimental autoimmune encephalomyelitis-resistant BALB/c mice. J Neuroimmunol. 1993;45:89–101. doi: 10.1016/0165-5728(93)90168-x. [DOI] [PubMed] [Google Scholar]
- 219.Aloisi F. Immune function of microglia. Glia. 2001;36:165–179. doi: 10.1002/glia.1106. [DOI] [PubMed] [Google Scholar]
- 220.Giulian D, Baker TJ. Characterization of ameboid microglia isolated from developing mammalian brain. J Neurosci. 1986;6:2163–2178. doi: 10.1523/JNEUROSCI.06-08-02163.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Hanisch UK, Kettenmann H. Microglia: active sensor and versatile effector cells in the normal and pathologic brain. Nat Neurosci. 2007;10:1387–1394. doi: 10.1038/nn1997. [DOI] [PubMed] [Google Scholar]
- 222.Kim SU, de Vellis J. Microglia in health and disease. J Neurosci Res. 2005;81:302–313. doi: 10.1002/jnr.20562. [DOI] [PubMed] [Google Scholar]
- 223.Nakajima K, Kohsaka S. Microglia: neuroprotective and neurotrophic cells in the central nervous system. Curr Drug Targets Cardiovasc Haematol Disord. 2004;4:65–84. doi: 10.2174/1568006043481284. [DOI] [PubMed] [Google Scholar]
- 224.Suzumura A, Mezitis SG, Gonatas NK, Silberberg DH. MHC antigen expression on bulk isolated macrophage-microglia from newborn mouse brain: induction of Ia antigen expression by gamma-interferon. J Neuroimmunol. 1987;15:263–278. doi: 10.1016/0165-5728(87)90121-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Ulvestad E, Williams K, Bjerkvig R, Tiekotter K, Antel J, Matre R. Human microglial cells have phenotypic and functional characteristics in common with both macrophages and dendritic antigen-presenting cells. J Leukoc Biol. 1994;56:732–740. doi: 10.1002/jlb.56.6.732. [DOI] [PubMed] [Google Scholar]
- 226.Elkabes S, DiCicco-Bloom EM, Black IB. Brain microglia/macrophages express neurotrophins that selectively regulate microglial proliferation and function. J Neurosci. 1996;16:2508–2521. doi: 10.1523/JNEUROSCI.16-08-02508.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Nakajima K, Tohyama Y, Kohsaka S, Kurihara T. Ceramide activates microglia to enhance the production/secretion of brain-derived neurotrophic factor (BDNF) without induction of deleterious factors in vitro. J Neurochem. 2002;80:697–705. doi: 10.1046/j.0022-3042.2001.00752.x. [DOI] [PubMed] [Google Scholar]
- 228.Rabchevsky AG, Streit WJ. Grafting of cultured microglial cells into the lesioned spinal cord of adult rats enhances neurite outgrowth. J Neurosci Res. 1997;47:34–48. [PubMed] [Google Scholar]
- 229.MacEwan DJ. TNF ligands and receptors–a matter of life and death. Br J Pharmacol. 2002;135:855–875. doi: 10.1038/sj.bjp.0704549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Choi YK, Kim KW. Blood-neural barrier: its diversity and coordinated cell-to-cell communication. BMB Rep. 2008;41:345–352. doi: 10.5483/bmbrep.2008.41.5.345. [DOI] [PubMed] [Google Scholar]
- 231.Willis CL. Glia-induced reversible disruption of blood-brain barrier integrity and neuropathological response of the neurovascular unit. Toxicol Pathol. 2011;39:172–185. doi: 10.1177/0192623310385830. [DOI] [PubMed] [Google Scholar]
- 232.Nishioku T, Matsumoto J, Dohgu S, Sumi N, Miyao K, Takata F, Shuto H, Yamauchi A, Kataoka Y. Tumor necrosis factor-alpha mediates the blood-brain barrier dysfunction induced by activated microglia in mouse brain microvascular endothelial cells. J Pharmacol Sci. 2010;112:251–254. doi: 10.1254/jphs.09292sc. [DOI] [PubMed] [Google Scholar]
- 233.Capoccia BJ, Gregory AD, Link DC. Recruitment of the inflammatory subset of monocytes to sites of ischemia induces angiogenesis in a monocyte chemoattractant protein-1-dependent fashion. J Leukoc Biol. 2008;84:760–768. doi: 10.1189/jlb.1107756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Frangogiannis NG, Dewald O, Xia Y, Ren G, Haudek S, Leucker T, Kraemer D, Taffet G, Rollins BJ, Entman ML. Critical role of monocyte chemoattractant protein-1/CC chemokine ligand 2 in the pathogenesis of ischemic cardiomyopathy. Circulation. 2007;115:584–592. doi: 10.1161/CIRCULATIONAHA.106.646091. [DOI] [PubMed] [Google Scholar]
- 235.Kim GH, Kellner CP, Hahn DK, Desantis BM, Musabbir M, Starke RM, Rynkowski M, Komotar RJ, Otten ML, Sciacca R, et al. Monocyte chemoattractant protein-1 predicts outcome and vasospasm following aneurysmal subarachnoid hemorrhage. J Neurosurg. 2008;109:38–43. doi: 10.3171/JNS/2008/109/7/0038. [DOI] [PubMed] [Google Scholar]
- 236.Morimoto H, Hirose M, Takahashi M, Kawaguchi M, Ise H, Kolattukudy PE, Yamada M, Ikeda U. MCP-1 induces cardioprotection against ischaemia/reperfusion injury: role of reactive oxygen species. Cardiovasc Res. 2008;78:554–562. doi: 10.1093/cvr/cvn035. [DOI] [PubMed] [Google Scholar]
- 237.Yan YP, Sailor KA, Lang BT, Park SW, Vemuganti R, Dempsey RJ. Monocyte chemoattractant protein-1 plays a critical role in neuroblast migration after focal cerebral ischemia. J Cereb Blood Flow Metab. 2007;27:1213–1224. doi: 10.1038/sj.jcbfm.9600432. [DOI] [PubMed] [Google Scholar]
- 238.Chen BP, Kuziel WA, Lane TE. Lack of CCR2 results in increased mortality and impaired leukocyte activation and trafficking following infection of the central nervous system with a neurotropic coronavirus. J Immunol. 2001;167:4585–4592. doi: 10.4049/jimmunol.167.8.4585. [DOI] [PubMed] [Google Scholar]
- 239.El Khoury J, Toft M, Hickman SE, Means TK, Terada K, Geula C, Luster AD. Ccr2 deficiency impairs microglial accumulation and accelerates progression of Alzheimer-like disease. Nat Med. 2007;13:432–438. doi: 10.1038/nm1555. [DOI] [PubMed] [Google Scholar]
- 240.Galasso JM, Liu Y, Szaflarski J, Warren JS, Silverstein FS. Monocyte chemoattractant protein-1 is a mediator of acute excitotoxic injury in neonatal rat brain. Neuroscience. 2000;101:737–744. doi: 10.1016/s0306-4522(00)00399-7. [DOI] [PubMed] [Google Scholar]
- 241.Tsirka SE, Gualandris A, Amaral DG, Strickland S. Excitotoxin-induced neuronal degeneration and seizure are mediated by tissue plasminogen activator. Nature. 1995;377:340–344. doi: 10.1038/377340a0. [DOI] [PubMed] [Google Scholar]
- 242.Tsirka SE, Rogove AD, Bugge TH, Degen JL, Strickland S. An extracellular proteolytic cascade promotes neuronal degeneration in the mouse hippocampus. J Neurosci. 1997;17:543–552. doi: 10.1523/JNEUROSCI.17-02-00543.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Cho ML, Yoon BY, Ju JH, Jung YO, Jhun JY, Park MK, Park SH, Cho CS, Kim HY. Expression of CCR2A, an isoform of MCP-1 receptor, is increased by MCP-1, CD40 ligand and TGF-beta in fibroblast like synoviocytes of patients with RA. Exp Mol Med. 2007;39:499–507. doi: 10.1038/emm.2007.55. [DOI] [PubMed] [Google Scholar]
- 244.Sanders SK, Crean SM, Boxer PA, Kellner D, LaRosa GJ, Hunt SW., 3rd Functional differences between monocyte chemotactic protein-1 receptor A and monocyte chemotactic protein-1 receptor B expressed in a Jurkat T cell. J Immunol. 2000;165:4877–4883. doi: 10.4049/jimmunol.165.9.4877. [DOI] [PubMed] [Google Scholar]
- 245.Proost P, Struyf S, Couvreur M, Lenaerts JP, Conings R, Menten P, Verhaert P, Wuyts A, Van Damme J. Posttranslational modifications affect the activity of the human monocyte chemotactic proteins MCP-1 and MCP-2: identification of MCP-2(6-76) as a natural chemokine inhibitor. J Immunol. 1998;160:4034–4041. [PubMed] [Google Scholar]
- 246.Dean RA, Cox JH, Bellac CL, Doucet A, Starr AE, Overall CM. Macrophage-specific metalloelastase (MMP-12) truncates and inactivates ELR+CXC chemokines and generates CCL2, -7, -8, and -13 antagonists: potential role of the macrophage in terminating polymorphonuclear leukocyte influx. Blood. 2008;112:3455–3464. doi: 10.1182/blood-2007-12-129080. [DOI] [PubMed] [Google Scholar]
- 247.McQuibban GA, Gong JH, Wong JP, Wallace JL, Clark-Lewis I, Overall CM. Matrix metalloproteinase processing of monocyte chemoattractant proteins generates CC chemokine receptor antagonists with anti-inflammatory properties in vivo. Blood. 2002;100:1160–1167. [PubMed] [Google Scholar]
- 248.Gong JH, Clark-Lewis I. Antagonists of monocyte chemoattractant protein 1 identified by modification of functionally critical NH2-terminal residues. J Exp Med. 1995;181:631–640. doi: 10.1084/jem.181.2.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Kitamoto S, Egashira K. Anti-monocyte chemoattractant protein-1 gene therapy for cardiovascular diseases. Expert Rev Cardiovasc Ther. 2003;1:393–400. doi: 10.1586/14779072.1.3.393. [DOI] [PubMed] [Google Scholar]
- 250.Ni W, Egashira K, Kitamoto S, Kataoka C, Koyanagi M, Inoue S, Imaizumi K, Akiyama C, Nishida KI, Takeshita A. New anti-monocyte chemoattractant protein-1 gene therapy attenuates atherosclerosis in apolipoprotein E-knockout mice. Circulation. 2001;103:2096–2101. doi: 10.1161/01.cir.103.16.2096. [DOI] [PubMed] [Google Scholar]
- 251.Zlokovic BV. The blood-brain barrier in health and chronic neurodegenerative disorders. Neuron. 2008;57:178–201. doi: 10.1016/j.neuron.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 252.Iadecola C. Neurovascular regulation in the normal brain and in Alzheimer’s disease. Nat Rev Neurosci. 2004;5:347–360. doi: 10.1038/nrn1387. [DOI] [PubMed] [Google Scholar]
- 253.Ben-Menachem E, Johansson BB, Svensson TH. Increased vulnerability of the blood-brain barrier to acute hypertension following depletion of brain noradrenaline. J Neural Transm. 1982;53:159–167. doi: 10.1007/BF01243407. [DOI] [PubMed] [Google Scholar]
- 254.Cohen Z, Bonvento G, Lacombe P, Hamel E. Serotonin in the regulation of brain microcirculation. Prog Neurobiol. 1996;50:335–362. doi: 10.1016/s0301-0082(96)00033-0. [DOI] [PubMed] [Google Scholar]
- 255.Cohen Z, Molinatti G, Hamel E. Astroglial and vascular interactions of noradrenaline terminals in the rat cerebral cortex. J Cereb Blood Flow Metab. 1997;17:894–904. doi: 10.1097/00004647-199708000-00008. [DOI] [PubMed] [Google Scholar]
- 256.Hawkins BT, Davis TP. The blood-brain barrier/neurovascular unit in health and disease. Pharmacol Rev. 2005;57:173–185. doi: 10.1124/pr.57.2.4. [DOI] [PubMed] [Google Scholar]
- 257.Tong XK, Hamel E. Regional cholinergic denervation of cortical microvessels and nitric oxide synthase-containing neurons in Alzheimer’s disease. Neuroscience. 1999;92:163–175. doi: 10.1016/s0306-4522(98)00750-7. [DOI] [PubMed] [Google Scholar]
- 258.Vaucher E, Hamel E. Cholinergic basal forebrain neurons project to cortical microvessels in the rat: electron microscopic study with anterogradely transported Phaseolus vulgaris leucoagglutinin and choline acetyltransferase immunocytochemistry. J Neurosci. 1995;15:7427–7441. doi: 10.1523/JNEUROSCI.15-11-07427.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Vaucher E, Tong XK, Cholet N, Lantin S, Hamel E. GABA neurons provide a rich input to microvessels but not nitric oxide neurons in the rat cerebral cortex: a means for direct regulation of local cerebral blood flow. J Comp Neurol. 2000;421:161–171. [PubMed] [Google Scholar]
- 260.Minami M. Neuro-glio-vascular interaction in ischemic brains. Yakugaku Zasshi. 2011;131:539–544. doi: 10.1248/yakushi.131.539. [DOI] [PubMed] [Google Scholar]
- 261.Gosselin RD, Varela C, Banisadr G, Mechighel P, Rostene W, Kitabgi P, Melik-Parsadaniantz S. Constitutive expression of CCR2 chemokine receptor and inhibition by MCP-1/CCL2 of GABA-induced currents in spinal cord neurones. J Neurochem. 2005;95:1023–1034. doi: 10.1111/j.1471-4159.2005.03431.x. [DOI] [PubMed] [Google Scholar]
- 262.Guo W, Wang H, Zou S, Dubner R, Ren K. Chemokine signaling involving chemokine (C–C motif) ligand 2 plays a role in descending pain facilitation. Neurosci Bull. 2012;28:193–207. doi: 10.1007/s12264-012-1218-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Old EA, Malcangio M. Chemokine mediated neuron-glia communication and aberrant signalling in neuropathic pain states. Curr Opin Pharmacol. 2012;12:67–73. doi: 10.1016/j.coph.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 264.Zhang H, Boyette-Davis JA, Kosturakis AK, Li Y, Yoon SY, Walters ET, Dougherty PM (2013). Induction of monocyte chemoattractant protein-1 (MCP-1) and its receptor CCR2 in primary sensory neurons contributes to paclitaxel-induced peripheral neuropathy. J Pain (in press) [DOI] [PMC free article] [PubMed]
- 265.Zhang ZJ, Dong YL, Lu Y, Cao S, Zhao ZQ, Gao YJ. Chemokine CCL2 and its receptor CCR2 in the medullary dorsal horn are involved in trigeminal neuropathic pain. J Neuroinflammation. 2012;9:136. doi: 10.1186/1742-2094-9-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Godefroy D, Gosselin RD, Yasutake A, Fujimura M, Combadiere C, Maury-Brachet R, Laclau M, Rakwal R, Melik-Parsadaniantz S, Bourdineaud JP, Rostene W. The chemokine CCL2 protects against methylmercury neurotoxicity. Toxicol Sci. 2012;125:209–218. doi: 10.1093/toxsci/kfr252. [DOI] [PubMed] [Google Scholar]
- 267.Stowe AM, Wacker BK, Cravens PD, Perfater JL, Li MK, Hu R, Freie AB, Stuve O, Gidday JM. CCL2 upregulation triggers hypoxic preconditioning-induced protection from stroke. J Neuroinflammation. 2012;9:33. doi: 10.1186/1742-2094-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Schellenberg AE, Buist R, Del Bigio MR, Toft-Hansen H, Khorooshi R, Owens T, Peeling J. Blood-brain barrier disruption in CCL2 transgenic mice during pertussis toxin-induced brain inflammation. Fluids Barriers CNS. 2012;9:10. doi: 10.1186/2045-8118-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Dimitrijevic OB, Stamatovic SM, Keep RF, Andjelkovic AV. Absence of the chemokine receptor CCR2 protects against cerebral ischemia/reperfusion injury in mice. Stroke. 2007;38:1345–1353. doi: 10.1161/01.STR.0000259709.16654.8f. [DOI] [PubMed] [Google Scholar]
- 270.Yao Y, Tsirka SE. The CCL2-CCR2 system affects the progression and clearance of intracerebral hemorrhage. Glia. 2012;60:908–918. doi: 10.1002/glia.22323. [DOI] [PMC free article] [PubMed] [Google Scholar]