Adaptive Optics Scanning Light Ophthalmoscopy (AOSLO) allows non-invasive visualization of the photoreceptor mosaic.1 Structures in the inner retina, such as blood vessels, cystoid macular edema (CME), or microcysts may interfere with the ability to study the underlying photoreceptor mosaic.2,3 Here we demonstrate a case where the presence of a microcyst alters the magnification of the photoreceptor mosaic.
A 20-year-old male involved in a motor vehicle accident resulting in commotio retinae presented with visual complaints of a central scotoma and generalized blurred vision. Spectral domain OCT (Bioptigen, Morrisville, NC) on the left eye revealed a microcyst in the inner nuclear layer (Figure 1A). AOSLO imaging 1,4 revealed microcysts not seen on OCT (Figure 1B). The cones underlying the microcyst appeared more tightly packed in the AOSLO images (average nearest neighbor spacing of 4.40 μm) than those immediately adjacent to the microcyst (average nearest neighbor spacing of 5.82 μm, p<0.0001). We observed uniform scaling within the cyst area, consistent with predictions from paraxial optical ray tracing modeling the microcyst as a spherical lens (Figure 2). Based on these same concepts, the image magnification should be directly proportional to both the distance between the cyst and the photoreceptor layer and the radius of the cyst. The potential consequences a cyst may have on AO Ophthalmoscopy include shifting the image, monochromatic aberrations or blur, and a dimming of the confocal image.
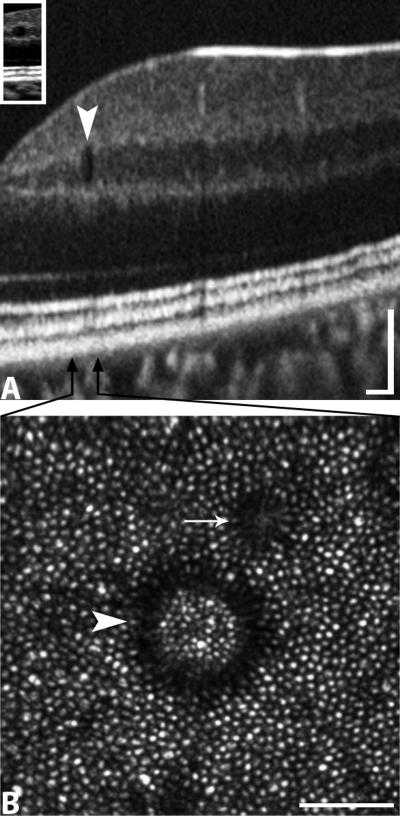
Figure 1.
A, OCT image of the left eye showing a microcyst in the inner nuclear layer. Arrows indicate the width of the AOSLO image scaled to the OCT. B AOSLO image showing the photoreceptor mosaic within and adjacent to the border of the cyst (arrow head). The photoreceptors appear more closely packed within the cyst than outside the border. This demonstrates the lensing effect of the cyst. Also shown is a shadow from a smaller microcyst not observed on OCT (arrow).
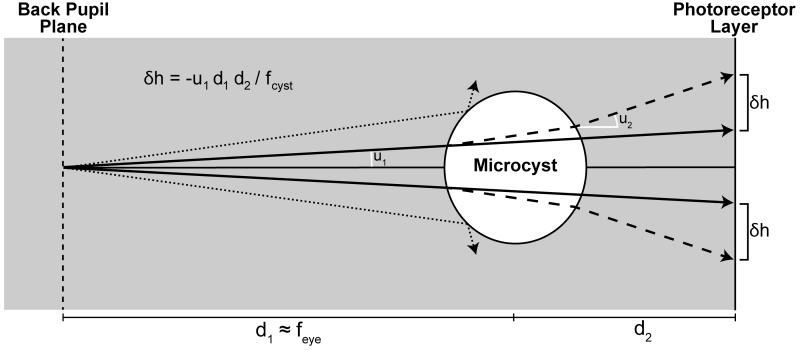
Figure 2.
This ray tracing shows the effect of a spherical cyst in near the retina. The principal rays shown here with arrows indicate light propagation without the cyst present (solid line) and the bending of the path due to the cyst (dashed line). The space between these two rays is seen in the image as a dark ring around the scaled portion of the image; this space is described by the equation shown in the figure. The effect is stronger with a longer axial length (d1 + d2), the cyst being further from the photoreceptor layer (d2), or a larger radius of curvature of the cyst. d1 = distance from the lens to the cyst; d2 = distance from cyst to photoreceptor layer; u1 = angle of principal ray from edge of cyst to lens; u2 = angle between the chief ray and the bent ray through the cyst; δh = the space between the chief ray with and without the cyst present.
This finding demonstrates the need for caution when analyzing AOSLO images in patients with cystic conditions like CME to avoid misinterpretation of photoreceptor structure, as certain metrics for assessing mosaic geometry may be affected by the optical properties of these cysts.
Acknowledgments
Funding: This study was supported by NIH Grants P30EY001931 and R01EY017607, Thomas M. Aaberg, Sr., Retina Research Fund, Foundation Fighting Blindness, and an unrestricted departmental grant from Research to Prevent Blindness. This investigation was conducted in a facility constructed with support from Research Facilities Improvement Program Grant Number C06 RR016511 from the National Center for Research Resources, National Institutes of Health. Alfredo Dubra, PhD. holds a Career Award at the Scientific Interface from the Burroughs Wellcome Fund and is the recipient of a Career Development Award from Research to Prevent Blindness.
Footnotes
The authors have no financial interest in the work presented here.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dubra A, Sulai Y, Norris JL, et al. Non-invasive imaging of the human rod photoreceptor mosaic using a confocal adaptive optics scanning ophthalmoscope. Biomed. Opt. Express. 2011;2(7):1864–1876. doi: 10.1364/BOE.2.001864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duncan JL, Ratnam K, Birch DG, et al. Abnormal cone structure in foveal schisis cavities in X-linked retinoschisis from mutations in exon 6 of the RS1 gene. Invest. Ophth. Vis. Sci. 2011;52(13):9614–9623. doi: 10.1167/iovs.11-8600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duncan JL, Zhang Y, Gandhi J, et al. High-resolution imaging with adaptive optics in patients with inherited retinal degeneration. Invest. Ophth. Vis. Sci. 2007;48(7):3283–3291. doi: 10.1167/iovs.06-1422. [DOI] [PubMed] [Google Scholar]
- 4.Dubra A, Sulai Y. Reflective afocal broadband adaptive optics scanning ophthalmoscope. Biomed. Opt. Express. 2011;2(6):1757–1768. doi: 10.1364/BOE.2.001757. [DOI] [PMC free article] [PubMed] [Google Scholar]