Abstract
Objective
To gather input regarding the presentation, content, and understanding of survival and support information for Prognostigram, a computer-based program that uses standard cancer registry data elements to present individualized survival estimates.
Study Design
Cross-sectional survey research
Methods
Two groups of patients (total n=40) and one group of physicians (n=5) were interviewed. The patient groups were interviewed to assess baseline patient numeracy and health literacy and patient desire for prognostic information. The first group (n=20) was introduced to generalized survival curves in a paper booklet. The second group (n=20) was introduced to individualized survival curves from Prognostigram on the computer. Both patient groups were queried about the survival curves. The physicians were asked their opinions on sharing prognostic information with patients.
Results
Numeracy assessments indicated that the patients are able to understand concepts and statistics presented by Prognostigram. According to the patient interviews, the Internet is the most frequent source for survival statistics. Of the 40 patient participants, 39 reported survival statistics as being “Somewhat” or “Very” useful to cancer patients. All five physicians believed survival statistics were useful to patients and physicians and noted accurate and understandable survival statistics are fundamental to facilitate discussions with patients regarding prognosis and expectations.
Conclusion
Formative research indicates that cancer patients and their families actively seek survival statistics on their own. All patients indicated strong interest in Prognostigram, which is a software tool designed to produce individualized survival statistics to oncologists and cancer patients in a user-friendly manner.
Keywords: Cancer survivorship, prognosis, numeracy, health literacy, decision-making
Introduction
One of the most challenging interactions between a cancer physician and a newly-diagnosed cancer patient is a discussion about prognosis.1,2,3 Patients want doctors to be realistic when providing generalized survival information, to recognize the patient as an individual, and to provide patient-specific survival information.2 More than ever, patients today are seeking data independently and unsupervised, and often gather information from a variety of other sources before coming to the office. Details may be obtained from the Internet, books, family, friends, and neighbors. Not infrequently, this information is inaccurate and, according to Fagerlin4, “…may, in fact, be detrimental to patients. Patients may hold preconceived beliefs gained from anecdotal reasoning that blind them to statistical information and reasoning." This may lead to disparate views between physicians and patients regarding the information shared during these discussions.5
A substantial barrier to presenting survival statistics is limited health literacy and mathematical numeracy of the general patient population. Multiple federal agencies6,7 as well as individual investigators8,9 report that up to half of the adult United States population is unable to function adequately within the healthcare system due to limited literacy. Limited health literacy may impact a patient’s understanding of screening tests, diagnoses, and treatment, thus impacting his or her decision-making and compliance. Furthermore, patients with low health literacy skills are frequently difficult for healthcare teams to identify; up to two-thirds of patients have not even confided this information to their spouse.10
Another important barrier to providing prognostic information to cancer patients is the fundamental lack of comprehensive and accurate survival statistics. While certain common cancers have websites devoted to detailing prognosis according to morphologic cancer stage, they are not individualized to include patient age, sex, race, and comorbid health problems. Survival statistics may be more difficult to find for rare cancers. Bernat11 noted that cancer patients suffering from coexistent medical conditions cannot obtain meaningful outcomes data ”…because many published outcome studies of primary illness [cancer] fail to control for the effect of serious comorbidities.” Multiple investigators12,13,14,15 have demonstrated that the presence of comorbidities is an important prognostic factor of survival in cancer patients.
During interviews with the first group of patients (Group A, n=20) and their families, participants were queried if they and/or a family member utilized the World Wide Web in their search for information about their disease. This formative research conducted by our team indicated that most patients and their families routinely used an internet-based resource to procure cancer information. Interviews with the second group of patients (Group B, n=20) confirmed these findings. The Prognostigram, a Web-based tool designed to provide individualized cancer survival statistics, was created to bridge the gap between clinicians and cancer patient, and facilitate the understanding of statistical information and prognostic data. The goal of this current study was to assess patient and physician views on providing patient-specific survival information in this format.
Materials and Methods
The first portion of the study included one-on-one, audio-recorded interviews between the senior author (JFP) and five oncologists. Physicians were medical, radiation, or surgical oncologists with active clinical practices within Siteman Cancer Center/Washington University Physician Faculty Practices. A scripted list of questions were asked to physicians regarding their views on the importance of survival statistics, sharing prognosis with patients, as well as their thoughts on using a web-based program that created individualized survival curves. The recorded conversations were transcribed and then analyzed as detailed below. There were no exclusion criteria for physician interviewees and all invited oncologists consented to be part of the study.
For the second part of the study, forty patients were identified through the practices of participating oncologists at Siteman Cancer Center at Washington University/Barnes-Jewish Hospital as well as its affiliated practices at the Barnes West County Hospital and we recruited patients from both sites. Patients had a diagnosis of a primary cancer from a solid organ tumor less than one year from recruitment. Patients were undergoing or had completed their initial round of therapy at the Siteman Cancer Center. All patients were over 18 years of age, were under the care of one of the collaborating oncologists, spoke English, and were fully able to understand all questions. Patients were excluded if they self-reported that they did not understand the questions being asked or if they had not previously discussed both their current diagnosis and prognosis with their oncologist. The patient interviews were conducted by a medical student or resident physician completing an NIH-sponsored research training program.
Clinical nursing staff of participating oncologists helped identify patients who filled eligibility criteria to the research assistant. All patients discussed their diagnoses and prognoses with their oncologist prior to being recruited into the study, thus reducing potential stress on patients. Family members or friends present during the interviews were not allowed to speak for the patient or provide answers to questions involving assessment of literacy or mathematical numeracy.
The Institutional Review Board at Barnes-Jewish Hospital reviewed and approved the conduct of the study.
Measures
Demographics and Cancer Staging
Participants identified their age, gender, race, highest educational level achieved, familiarity with computer use, and location of index cancer. Each patient had a Tumor Information Sheet that identified a patient’s index cancer site, stage, and grade. (See Supplemental Information online)
Newest Vital Sign
Participants were asked to complete the Newest Vital Sign16 to assess baseline literacy. This survey has been shown to quickly and accurately assess literacy in a variety of patient populations, and correlates well with previously used assessments such as the Test of Functional Health Literacy in Adults (TOFHLA).
Numeracy Assessments
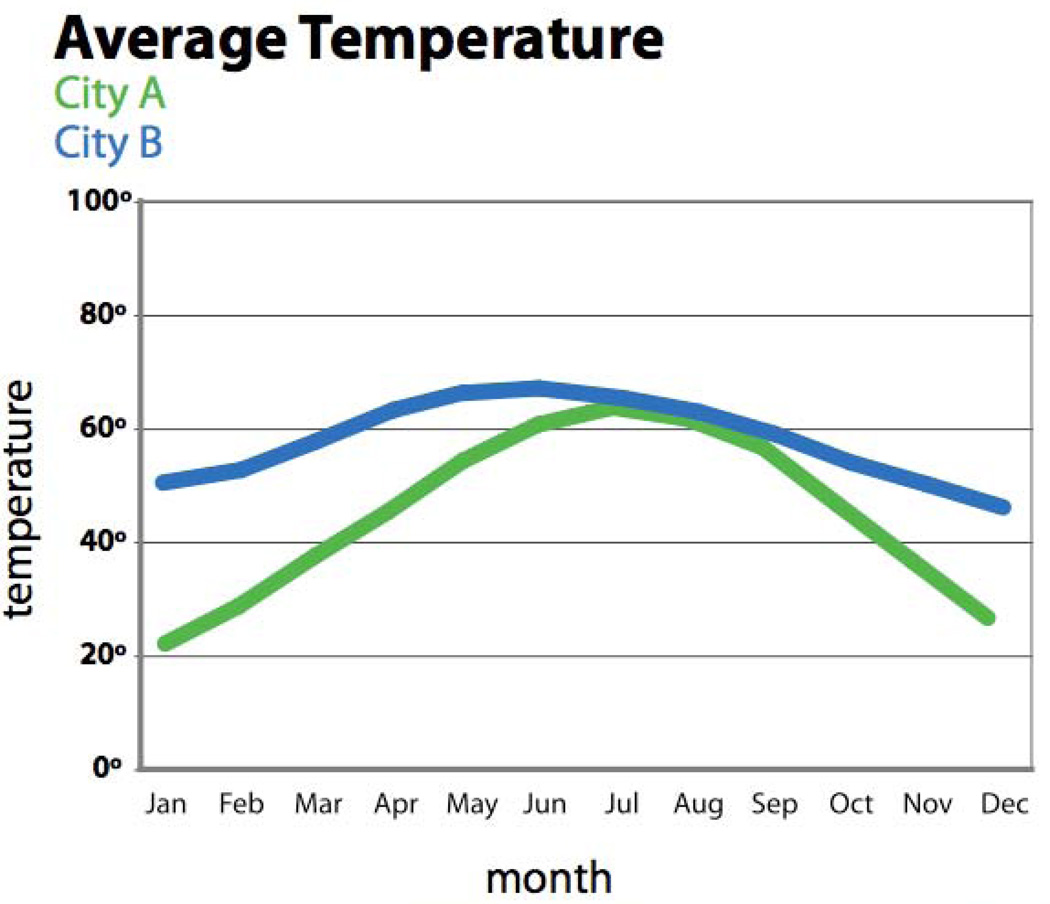
Patients were given a booklet with a series of graphs, beginning with graphical representation of temperatures between two cities (City A and City B) (Figure 1).
Figure 1.
Patient participants were asked to identify: what the X and Y axes represented; what month the temperature was either 40 degrees or 65 degrees; in what month(s) were the temperatures the same; and in what month(s) were the temperatures most different, etc.
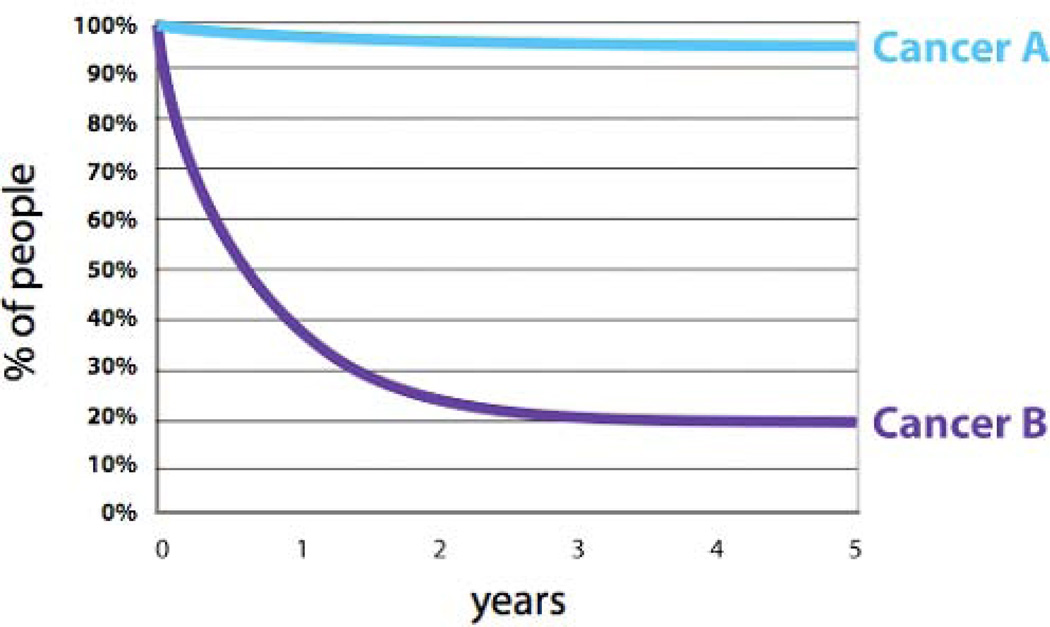
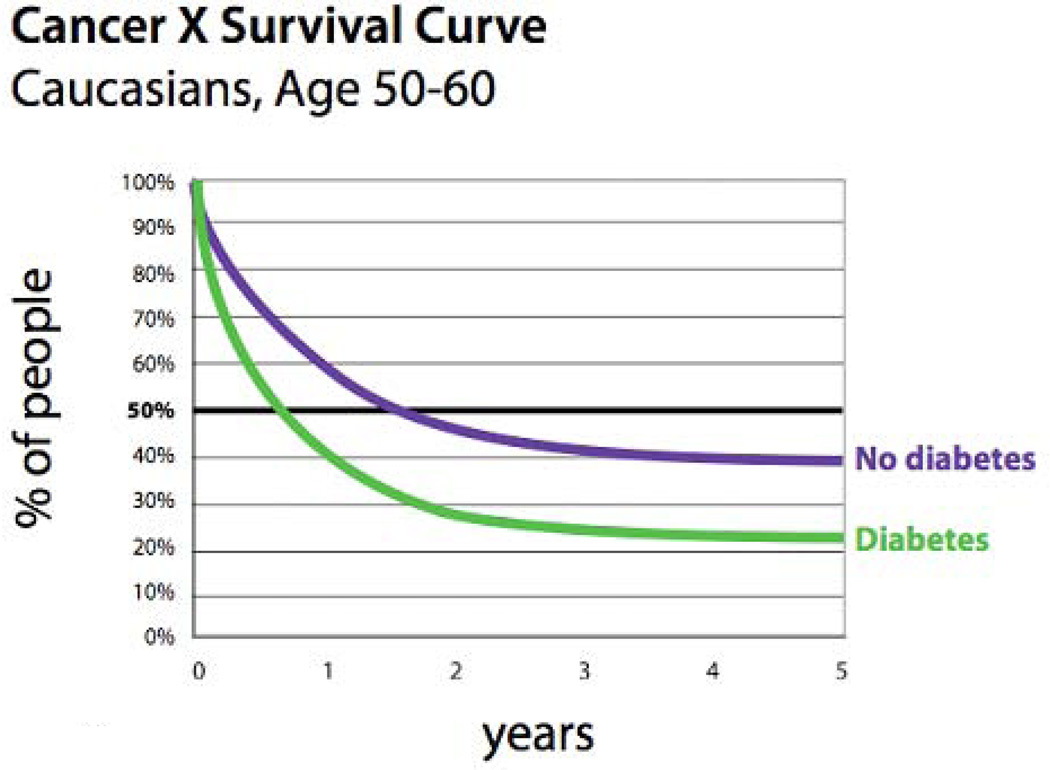
Patients were additionally questioned regarding a series of generic survival graphs included in their patient booklets. Patients were shown graphical representations of five-year survival of two fictitious cancers – “Cancer A” and “Cancer B”. (Figure 2) Participants were also shown and queried about graphs depicting the decrease in survival that occurs when a patient has other comorbid medical conditions in addition to their index cancer. (Figure 3) Patients were asked basic questions about the graphs.
Figure 2.
Patients were shown graphical representations of five-year survival of two fictitious cancers – “Cancer A” and “Cancer B”. Patients were then asked what percentage of people survived 3 years; at what point did half the people survive; and for which cancer were more patients alive at five years.
Figure 3.
Patients were shown and queried about graphs depicting the decrease in survival that occurs when a patient has other comorbid medical conditions in addition to their index cancer.
Prognostigram Development
The Prognostigram web-based program v2.0 began as a software program that compiled data from about 30,000 cancer patients seen at the Siteman Cancer Center since 1995. Tumor registrars at Siteman Cancer Center captured data elements on newly-diagnosed cancer patients according to the American College of Surgeons Commission on Cancer Registry Data Standards.17 Prognostic data, including age, sex, race, overall severity of comorbidities, tumor site and stage were used to generate graphic representations of survival curves for six cancer sites. National normative data obtained from the Office of Vital Statistics was used to generate age, gender, and race-matched survival curves for comparison. Prognostigram was initially designed for use by health care professionals. Improved technologies allowed the further development of Prognostigram v3.0 to include more cancer sites and to allow the creation of a more user-friendly interface accessible to both physicians and patients. Interviews from the first group of patients in our study were used to guide the development of updated versions of Prognostigram. Wording on the site was developed internally and reviewed by staff associated with the Health Communication Research Laboratory at Washington University [http://hcrl.wustl.edu/]. [http://www.prognostigram.com/ajaxTest.html]
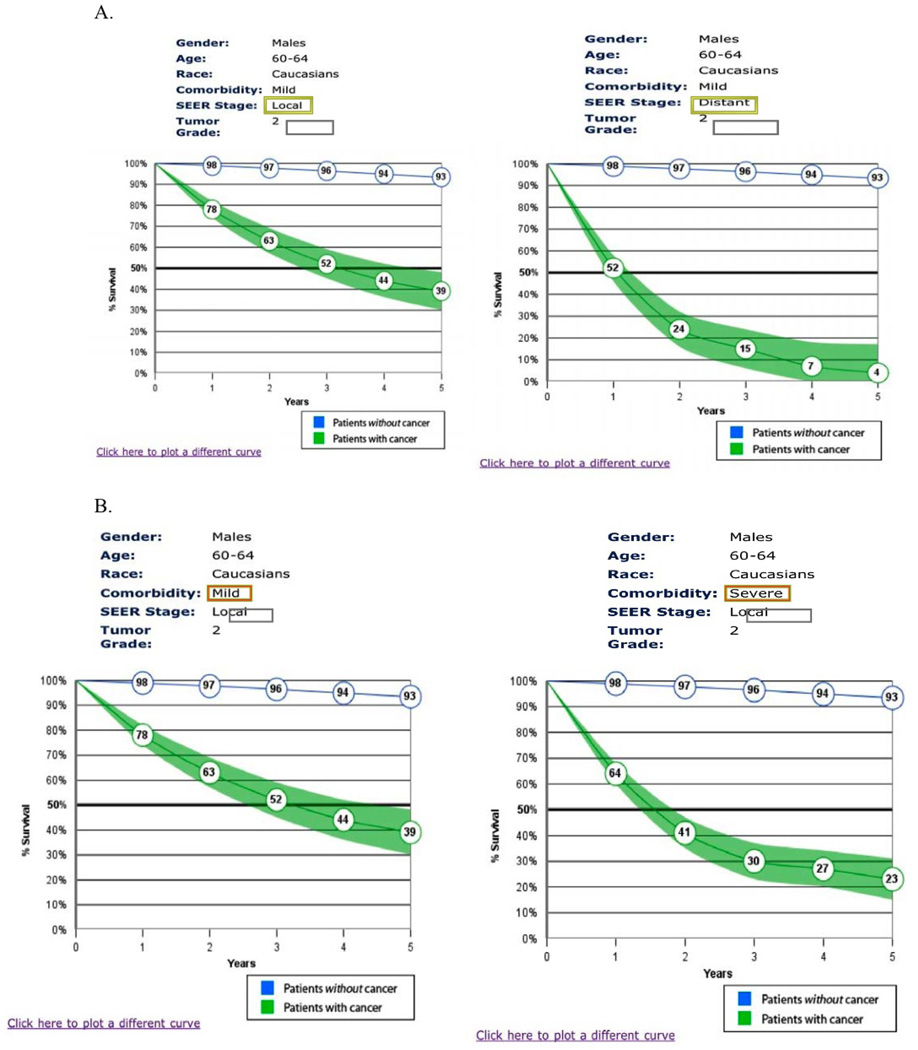
The first group of patients (Group A, n=20) was asked their preferences regarding the presentation of generic survival curves, including wording of titles, graphics arrangements, and legend formulation. These preferences were included in the development of the Prognostigram v3.0, which generated the individualized survival curves used during the interviews with the second group of patients (Group B, n=20) (Figure 4).
Figure 4.
Screen shots of Prognostigram. A. This example shows Esophageal cancer patients living since diagnosis – the change in survival due to changes in SEER stage (local v. distant spread of cancer). B. This example shows Esophageal cancer patients living since diagnosis – the change in survival due to changes in coexisting comorbid health problems.
Usefulness and Timing of Survival Statistics
At the conclusion of their interviews, both patients and doctors were asked to rate the usefulness of survival statistics for cancer patients. Participant choices were Very Useful, Somewhat Useful, Not Very Useful, Not Useful At All, or Don’t Know.
Analysis
Open-ended questions and participant preferences regarding the manner of sharing prognostic information were analyzed using descriptive statistics. A Grounded Theory Approach was utilized to evaluate the data. Line-by-line review of the interview transcripts allowed for concepts to be tagged as they became apparent. A “constant comparison” method was utilized to ensure that additional text assigned to the same tag accurately reflects the same concept as other bodies of text assigned the same code. Coding was performed until the point of “theoretical saturation”, or the point at which no new concepts emerged from analysis. This process allowed for the development of common themes.
Results
Demographic information from all forty patients may be found in Table 1. There was no significant difference between the educational backgrounds of patients within Groups A and B.
Table 1.
Patient demographics
| Characteristic | Categories | Sample size (N) | Percentage |
|---|---|---|---|
| Age | 18–35y/o | 2 | 5% |
| 36–55 | 15 | 37.5% | |
| 56–75 | 19 | 47.5% | |
| 76–95 | 4 | 10% | |
| >95y/o | 0 | 0% | |
| Gender | Male | 24 | 60% |
| Female | 16 | 40% | |
| Race | White | 34 | 85% |
| African-American | 6 | 15% | |
| Highest educational level achieved | Middle School | 2 | 5% |
| HS or GED | 19 | 47.5% | |
| College or University | 10 | 25% | |
| Graduate or Professional School | 8 | 20% | |
| Did not answer | 1 | 2.5% | |
| Computer Use | Never | 12 | 31% |
| Only with guidance | 1 | 3% | |
| Less than once a month | 1 | 3% | |
| More than once a month, less than once a week | 3 | 9% | |
| More than once a week, less than once a day | 6 | 14% | |
| Daily | 16 | 40% |
Overall, the combined patient groups scored very well in numeracy assessments. Patient participants were administered the “Newest Vital Sign” literary assessment at the start of the interview. [See Table 2] Eighty-five percent or greater of the total patient participants were able to answer numeracy questions correctly, with two exceptions. Group “A” patient participants had difficulty with more complex calculations: 1) only 40% of patient participants were able to identify a 20% decrease in survival between Years 1 and 3 on fictitious survival curves, and 2) only 45% of participants were able to appropriately identify that survival curves of fictitious Cancers “A” and “B” both showed the same percentage change in survival between Years 4 and 5. Those two questions were not asked of Group “B” participants. Ninety-two percent of patient participants were able to correctly distinguish which survival curve belonged to cancer patients with diabetes v. cancer patients without diabetes, and ninety-seven percent of patient participants were able to identify that diabetes negatively impacted survival in cancer patients. [Figure 3]
Table 2.
Newest Vital Sign
| Newest Vital Sign | Score | N | Percentage |
|---|---|---|---|
| 0 | 2 | 5% | |
| 1 | 2 | 5% | |
| 2 | 3 | 7.5% | |
| 3 | 5 | 12.5% | |
| 4 | 11 | 27.5% | |
| 5 | 8 | 20% | |
| 6 | 9 | 22.5% |
Patient participants were administered the “Newest Vital Sign” literary assessment at the start of the interview. The median score for participants was 5, with a range from 0–6. A score of 4–6 almost always indicates adequate literacy.
The five physician participants included surgical oncologists (n=1), medical oncologists (n=2), and radiation oncologists (n=2). Demographic data (age, years of practice, etc) were not collected on physician participants.
Patient and Physician Preferences
Participants in Patient Group A (n=20) were asked their preference for using the Prognostigram – on the Internet by themselves or in the office with a physician. Seventy percent (n=12) of patients who expressed a preference (n=17) stated they would like to use a web-based statistical tool on the Internet themselves, versus accessing it in the clinic with a physician (n=5). Feeling frustration due to limited time constraints during doctor visits, one patient stated, “The doctors don’t have time to tell you all of it.“ Patients were also queried whether they would discuss survival statistics they found on the Internet with their physician. Of those patients who expressed a preference (n=13, 65%), one hundred percent of patients (n=13) indicated they would discuss the statistical information they found with their physician.
All physicians (n=5) preferred a web-based tool that would be accessed by the physician alone or the physician with a patient. None of the physicians wanted patients to use the tool on their own. Physicians expressed concerns that patients would not remember the correct information to enter into Prognostigram, or that poor prognosis might affect patient willingness to continue with treatment or cause patients to become suicidal.
Theme Dominance
Usefulness of Survival Statistics
Ninety-eight percent of patient participants (n= 39) described survival statistics as “Very Useful” or “Somewhat Useful”. One patient stated simply, “Because it is good to know how long you have.” Another reported, “…I really wanted to know because it gave me time to do things that I want to do for the children and grandchildren.” One hundred percent of physician participants described survival statistics as “Very Useful” or “Somewhat Useful” to both patients and physicians. One physician noted, “I think patients are entitled and we are obligated to tell them when we are able to cure them or not cure them so it will help a little bit with their planning.” [See Table 3]
Table 3.
Usefulness of Survival Statistics
| Patient impression of survival statistics | |||
|---|---|---|---|
| Question | Categories | N | Percentage |
| How helpful are statistics | Very Useful | 26 | 65% |
| Somewhat useful | 12 | 30% | |
| Not very useful | 1 | 2.5% | |
| Not at all useful | 1 | 2.5% | |
| Physician impression of survival statistics | |||
| Question | Categories | N | Percentage |
| How helpful are statistics | Very Useful | 3 | 60% |
| Somewhat useful | 2 | 40% | |
| Not very useful | 0 | -- | |
| Not at all useful | 0 | -- | |
Prognostic Timelines
Although it was not a question that was specifically asked of patients, more than half (58%) of patients volunteered that they were seeking specific timelines related to their survival. As one patient stated, “I was wondering how bad the cancer was and how long I had.” Interestingly, when specifically queried about whether patients are seeking general versus specific survival information, eighty percent of physicians believed that patients want general trends regarding survival estimates. Four out of five of the physicians interviewed also stated that their decision to share survival estimates was prognosis-specific. Three of the five discuss likelihood of survival in terms of upcoming holidays or family events (i.e., Christmas or weddings) to patients with severe disease. Physicians reported the contradicting emotions affecting health professionals when dealing with newly diagnosed advanced cancer. As one physician stated, “…it is really hard when you have a patient with very aggressive disease that you just diagnosed to tell them that they have almost no chance of cure.”
Discussion
Physicians and patients report that survival statistics are useful to cancer patients. Our research has confirmed the previously identified large void in cancer communication, specifically the communication of prognostic information to cancer patients. In general, patients are not necessarily seeking successful prognosis from their physicians, but rather accurate prognosis successfully communicated. One patient noted, “I mean if it is two years [to live]…then so be it. But if it is five, than that gives you something to sit and have your chemo for…”
The overwhelming majority of our patient participants reported acquiring information regarding their cancer from someone or somewhere other than their physician or physician’s office. Most of our patient participants reported using the Internet to gain information about their cancer although many were frustrated by the amount of data available – too little in certain areas and too much in other areas. One patient noted, “I was going with the information that my doctor had given me and then I just typed cancer in on search engine…then you just get kind of overwhelmed.” Although more people, in general, report using the Internet to obtain health information, more than sixty percent of the time, Internet users cannot find the information they are looking for.10
A recurrent theme identified in our research was that patients want individualized cancer information that applies to them. Patients report seeing survival data on the Internet or hearing it from friends or relatives, but note they are unsure how relevant that information is to them. A unique component of Prognostigram is the incorporation of comorbid health problems as well as other demographic information to create individualized survival curves, which incorporate patients’.
Interestingly, the physician participants unanimously expressed a preference that patients not use the Prognostigram alone. Rather, physicians preferred to utilize Prognostigram themselves, either alone or with a patient. Physician participants expressed important concerns regarding patient use of the Prognostigram, including incorrect entry of data into Prognostigram thus generating an incorrect curve, as well as patient misinterpretation of the graphs adversely leading to treatment withdrawal or even patient suicide. While these concerns are valid, it was noted that multiple patient participants already misapplied anecdotal information to their own cancer beliefs and treatment decisions. ‘Medical misinformation’ is already a part of most patients’ lives. Fagerlin, et al. cite a distinct and clear dichotomy that patients may relate to – either a person was cured or not – versus a statistical estimate which is a more abstract concept and does not require knowledge of statistics.18 A user-friendly tool, such as Prognostigram, that conveys prognostic information to patients in a simple manner by a means (the Internet) already utilized by patients and their families, may reduce the dependence on anecdotal information.
Despite the varied educational background of our patient participants, the overwhelming majority did well on numeracy assessments and appeared to easily grasp the survival information presented on Prognostigram. Participants' responses encouraged us that the program content and display were well conceived and designed. The positive responses suggest a strong likelihood that patients would regularly use this tool in the future. Although some patients reported they would be more comfortable accessing the website with assistance (from a more computer-savvy friend or relative) most patients felt they would be able to navigate the site easily themselves.
We are currently working on Prognostigram v4.0, which includes more cancer sites and subsites, and survival estimates based on treatment. Prognostigram v4.0 will also accommodate patient information from other hospitals and cancer centers as long as the data is coded appropriately (see above).17 Risk-adjusted survival curves for patients treated at different hospitals presented on the same figure would allow for comparative effectiveness research, and, for example, the identification of poor performing hospitals for whom quality assessment and improvement programs should be initiated.
There are several limitations of this study. While patients had varied educational backgrounds, they were all literate. Additionally, they were all under the care of an oncologist and already receiving treatment. All participants had already had prognostic discussions with their oncologist, thus each participant likely had a more thorough baseline understanding of survival curves. To fully explore if Prognostigram is superior to printed materials in educating patients, an assessment of understanding of survival statistics before and after exposure to Prognostigram is needed.
Conclusion
Computer technology has revolutionized the healthcare industry in many aspects. Simultaneously, improving patient education is now seen as an effective and integral part of informed decision making. Many organizations are implementing PC- and Web-based performance measurement tools that allow patients and health-care providers to make more informed treatment decisions. Our results suggest that cancer patients are able and willing to use a web-based computer program that generates patient-specific survival information. Prognostigram has the potential to fill a much-needed void in cancer communication. Future research with Prognostigram should include assessments of newly diagnosed and not yet treated cancer patients to evaluate the potential of Prognostigram to improve patient understanding of cancer survival expectations.
Supplementary Material
Acknowledgement
Support from the National Institutes of Health (NIH)-National Institute on Deafness and Other Communication Disorders (NIDCD), Ruth L. Kirschstein National Research Service Award (NRSA) Institutional Research Training Grant (T32) entitled “Development of Clinician/Researchers in Academic ENT” (5T32DC000022). We would also like to acknowledge the time and effort of the cancer patients, physicians and their staff who participated in this project.
Footnotes
This work was awarded first prize in the Head & Neck category at the Triological Poster Session at 115th COSM meeting in San Diego, CA, USA, April 18–22, 2012.
Financial Disclosures: None
Conflict of Interest: None
Supplemental Information. Tumor Information Sheet. Patients filled in this sheet to identify their index cancer site, stage, and grade.
Reference List
- 1.Faulkner A, Maguire P. Talking To Cancer Patients and Their Relatives. 1st ed. New York, NY: Oxford University Press; 1995. [Google Scholar]
- 2.Hagerty RG, Butow PN, Ellis PM, et al. Communicating with realism and hope: incurable cancer patients' views on the disclosure of prognosis. J Clin Oncol. 2005;23:1278–1288. doi: 10.1200/JCO.2005.11.138. [DOI] [PubMed] [Google Scholar]
- 3.Campbell TC, Carey EC, Jackson VA, et al. Discussing prognosis: balancing hope and realism. Cancer J. 2010;16:461–466. doi: 10.1097/PPO.0b013e3181f30e07. [DOI] [PubMed] [Google Scholar]
- 4.Fagerlin A, Wang C, Ubel PA. Reducing the influence of anecdotal reasoning on people's health care decisions: is a picture worth a thousand statistics? Med Decis Making. 2005;25:398–405. doi: 10.1177/0272989X05278931. [DOI] [PubMed] [Google Scholar]
- 5.Back A. Patient-physician communication in oncology: what does the evidence show? Oncology. 2006;20:67–74. [PubMed] [Google Scholar]
- 6.Kindig D, Affonso D, Chudler E, et al. Health Literacy: A Prescription to End Confusion. Washington, D.C.: National Academies Press; 2004. Apr, [PubMed] [Google Scholar]
- 7.Lohr KN, Berkman SD, Sheridan SL, et al. Health Literacy Interventions and Outcomes: An Updated Systematic Review. Rockville, MD: Agency for Healthcare Research and Quality; 2011. Mar. Report No.: 199. [PMC free article] [PubMed] [Google Scholar]
- 8.Davis TC, Dolan NC, Ferreira MR, et al. The role of inadequate health literacy skills in colorectal cancer screening. Cancer Invest. 2001;19:193–200. doi: 10.1081/cnv-100000154. [DOI] [PubMed] [Google Scholar]
- 9.Understanding Health Literacy. Implications for Medicine and Public Health. Chicago, IL: American Medical Association; 2005. [Google Scholar]
- 10.Davis TC, Williams MV, Marin E, Parker RM, Glass J. Health literacy and cancer communication. CA A Cancer Journal for Clinicians. 2002;52:134–149. doi: 10.3322/canjclin.52.3.134. [DOI] [PubMed] [Google Scholar]
- 11.Bernat JL. Ethical issues in the perioperative management of neurologic patients. Neurol Clin. 2004;22:viii–ix. 457–471. doi: 10.1016/j.ncl.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Feinstein AR. The pre-therapeutic classification of co-morbidity in chronic disease. J Chron Dis. 1970;23:455–468. doi: 10.1016/0021-9681(70)90054-8. [DOI] [PubMed] [Google Scholar]
- 13.Satariano WA. Comorbidity and functional status in older women with breast3cancer: implications for screening, treatment, and prognosis. J Gerontol. 1992;47:24–31. [PubMed] [Google Scholar]
- 14.Piccirillo JF. Purposes, problems, and proposals for progress in cancer staging. Archives of Otolaryngology -- Head & Neck Surgery. 1995;121:145–149. doi: 10.1001/archotol.1995.01890020009003. [DOI] [PubMed] [Google Scholar]
- 15.Yancik R, Havlik RJ, Wesley MN, et al. Cancer and comorbidity in older patients: a descriptive profile. AEP. 1996;6:399–412. doi: 10.1016/s1047-2797(96)00063-4. [DOI] [PubMed] [Google Scholar]
- 16.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American College of Surgeons. Facility Oncology Registry Data Standards (FORDS) Chicago: 2002. [Google Scholar]
- 18.Fagerlin A, Zikmund-Fisher BJ, Ubel PA. Helping patients decide: ten steps to better risk communication. J Natl Cancer Inst. 2011;103:1436–1443. doi: 10.1093/jnci/djr318. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.