Abstract
Residents of Qidong, China are undergoing a rapid fluctuation in cancer incidence rates at many organ sites, reflecting a dynamic interplay of socio-behavioral, economic and environmental factors. This Perspective On Statistical Trends examines the China age-standardized incidence rates (CASR), as tracked by the Qidong Cancer Registry for the past 40 years, for the two leading cancer killers in Qidong, liver and lung. Both cancer types are strongly influenced by environmental factors. The CASR for liver cancer has dropped nearly 50% in the last 4 decades, in part from access to deep-well drinking water in the 1970s with consequent diminished exposure to tumor promoting microcystins produced by blue-green algae. There have also been substantive reductions in exposures to dietary aflatoxins, as economic reform in the mid-1980s fostered a wholesale change in dietary staple from maize to rice. In men, lung cancer CASR has trebled over this period, likely driven by a high prevalence of smokers (~65%) and an ever increasing smoking frequency in this population. Qidong women, by contrast, rarely smoke and have exhibited a flat CASR until the last decade where lung cancer rates have now doubled. This upturn may reflect an increasing burden of indoor and outdoor air pollution.
Introduction
Epidemiological hallmarks for a role of environmental factors in cancer risk include observations that risks change within a generation when people migrate from one country to another or indeed change quickly within a regional population. The residents of Qidong, China are undergoing a rapid fluctuation in cancer incidence rates at many organ sites, reflecting a dynamic interplay of socio-behavioral, economic and environmental factors. This Perspective On Statistical Trends examines the extraordinary changes in the China age-standardized incidence rates for the two leading cancer killers in the Qidong region: one going down and the other one up, liver and lung cancer, respectively. Trends in cancer are typically shaped through three inter-linked dimensions — incidence, mortality and survival, although with liver and lung cancer, incidence figures are very similar to mortality rates because survival is poor and has not improved substantially over time.1,2
Qidong is located at the mouth of the Yangtze River in eastern China, with a current population of about 1.12 million. Qidong is a region with a relatively stable population, although in the past two decades about 100,000 residents each year worked outside of Qidong (mostly in Shanghai and Nantong). Their census registration and information related to health care is still kept in Qidong. The land in this region is newly formed as deposits from the river have linked together several small islands over the past 2 centuries; county governance was not established until 1928. Linked to Southern China only by water transport, Qidong has been a largely self-suficient agricultural region. Major crops have been corn and cotton as the porous, alluvial soil was unsuitable for the cultivation of rice, the dietary staple of much of China. The agricultural and economic isolation of Qidong dissipated in the 1990s. Enormous transformations over the past decade have been capped by the completion of a tunnel and bridge system in 2011 providing direct and rapid access to Shanghai. Qidong has quickly become a manufacturing center with a highly urbanized city center, typical of modern coastal China.
Qidong has been of interest to cancer epidemiologists and biologists because, until recently, it was an endemic area for liver cancer with amongst the highest incidence rates in the world.3 Together with the founding of the Qidong Liver Cancer Institute (QDLCI) in 1972, the Qidong Cancer Registry was established. This registry is a population-based registry that collects information on all deaths and all cancer cases in the county.1,2 In addition to 40 years of continuous operation, a rarity outside of Europe and North America, this registry has, perhaps uniquely in the world, annotated changing patterns of disease in a stable population throughout a period of enormous social and cultural change, reflecting the increases in affluence, evolving lifestyles, social changes and increasing urbanization and environmental pollution. This cancer registry provides the data base for the age-standardized cancer incidence rates by China population (CASR) for lung and liver cancer presented in Figure 1. A full documentation of the data contained in this cancer registry can be found in the recent publication of the book “Cancer in Qidong, China (1972–2011).3
Figure 1.
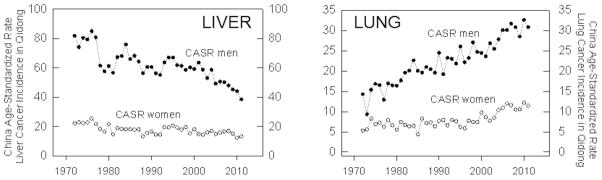
China age-standardized rate (CASR) for incidence of liver (left panel) and lung (right panel cancers in men and women residing in Qidong, China during the period of 1972 through 2011. CASR data are from Reference 2 with permission.
Liver Cancer
Qidong has been at the epicenter of research into the etiology of primary liver cancer. Even before the founding of the QDLCI, liver cancer had been recognized as the leading cause of cancer death in Qidong County (now City). At that time the CASR for liver cancer incidence stood at over 50/100,000; upwards of 1 and 10 adults in the poorest of rural areas would develop and die from this form of cancer.4 Median age of diagnosis hovered at less than 50 years of age. As shown in Figure 1, men were at a nearly 4-fold higher risk of developing liver cancer than women. The CASR has dropped in half since 1972 for both sexes, with much of the decline occurring over the past dozen years. As a result, the dichotomy between CASR in males and females now stands at 2-fold; median age of diagnosis has moved close to 60 for both sexes. Little of this decline can be accounted for by improved survival as the 1-year survival rates for liver cancer were 18.8% in the interval 1973–1977 and 17.5% in 2003–2007.2 Many questions arise from perusal of the Figure. Some are: What factors drove the high risk for liver cancer in this region 40 years ago? Why has it dropped so dramatically? Why the differential declines in men and women?
Multiple factors contribute to the etiology of liver cancer in Qidong and elsewhere. Chronic carrier status for infection with hepatitis B virus (HBV) is a prime risk factor. At least 90% of primary liver cancers in Qidong are associated with HBV infection.5 Hepatitis C virus (HCV) to date has not been observed as an important risk factor in this region,5 unlike other areas of the world. Multiple studies conducted in Shanghai, Qidong and Taiwan all support a strong co-factor role for exposure to aflatoxin together with HBV.5–7 Indeed, aflatoxins are listed as Group 1 hepatocarcinogens by IARC.8 Additive and perhaps synergistic interactions between the viral and chemical carcinogen have been observed consistently in these areas. Early surveillance studies in the Qidong countryside during the 1970s indicated a high frequency of contamination of the dietary staple, maize, with aflatoxins. In some years 99% of the sampled maize exceeded the US FDA action level of 20 ppb contamination.9 Ducks raised in the region were observed to have a high incidence of liver cancer, perhaps serving as sentinel species for the impact of moldy corn on the Qidongese themselves.9 Throughout China, procurement practices tied rural household food consumption to local production, and in the commune system of the 1960s and 1970s, yields rather than quality were emphasized. Producing quality corn was not a priority. China adopted institutional reforms after 1979 to shift from a planned economy to a market-oriented economy. Trading of foodstuffs was encouraged and beginning in 1985 rice rapidly supplanted maize as the major dietary staple in Qidong. Rice typically harbors substantially lower levels of mycotoxin contamination than maize. As we have recently documented by quantifying levels of aflatoxin albumin adducts in archived serum samples obtained from rural Qidongese during the late 1980s to present, aflatoxin exposures have dropped dramatically (>100-fold) to levels below current levels of detection using isotope dilution mass spectrometry.10
In addition to reduction of aflatoxin exposure, HBV vaccination is an exceedingly important strategy for primary prevention of liver cancer. Pilot vaccination programs were conducted in some Qidong townships from 1983 to 1990,11 although the overall coverage of Qidong newborns was perhaps 30% during this period. Vaccination programs languished in the rural townships of Qidong during the 1990s, largely due to limited access to the vaccine and its prohibitive cost relative to annual wages. Beginning in 2002 a subsidized HBV vaccination program was instituted by the Chinese government and by 2006 fees associated with the 3 injections were also provided. While HBV vaccination is now near universal in Qidong, most of the birth cohorts currently at risk for developing liver cancer were never vaccinated (current 35–65 year olds). Nonetheless, CASR has dropped indicating other factors are largely at play. While diminished exposure to aflatoxin is an attractive hypothesis, an additional theory may be relevant. Microcystins, hepatotoxic polypeptides produced by algal blooms, act as hepatic tumor promoters in animal models.12 Their levels can be quite high in ditch and pond water.13 Exposures to microcystins were greatly reduced in Qidong by the late 1970s through local government efforts to provide deep well water to all villages. Such well water is largely devoid of microcystins. This improvement in water quality preceded reductions in aflatoxin exposures by a decade and may contribute to the initial decline in CASR seen in Figure 1 for liver cancer.
Differences in liver cancer incidence by gender are observed in many, but not all, regions of the world, indicating that interactions between extrinsic and intrinsic factors define risk. In animal models estrogen-mediated inhibition of IL-6 production has been associated with inhibition of diethylnitrosamine-induced hepatocarcinogenesis.14 No differences by gender are seen in the prevalence of HBV infection across all age cohorts in Qidong, so a general immunologic explanation seems unlikely. Endocrine factors may also influence the metabolism of the hepatocarcinogen aflatoxin, although the evidence is sparse. A simple explanation lies in observations that men, in time of food insufficiency, tended to consume a major portion of the meals. Perhaps aflatoxin consumption was correspondingly elevated. Understanding the factors conveying lower risk of women to liver cancer may provide important insights into prevention.
Lung Cancer
“If women smoke like men, they die like men” notes Sir Richard Peto. They don’t in Qidong, smoke that is. Approximately two-thirds of men in Qidong smoke cigarettes, while less than 5% of women do.15 There remains a social stigma associated with women smoking in the countryside. We have not noticed changes in these proportions over the past several decades as we have collected data on smoking histories associated with enrollment in liver cancer screening or chemoprevention studies.16,17 By contrast, urban women in China are beginning to acquire the habit in increasing numbers. This fact presages change in Qidong as well, as the local economy continues its rapid expansion. While there are strong differences in tobacco use by gender in much of the developing world, large recent studies in Europe and America indicate the outcomes are similar in all who smoke.18,19 The key to prevention is clear – reduce exposure. However, programs to limit access to tobacco products or prohibit smoking in public places have no traction in Qidong. Tobacco remains a near essential component of the social fabric of men at this time.
Figure 1 highlights that men are at 3-fold greater risk of developing and dying from lung cancer as women in Qidong. In men, the explanation tracks solidly with increasing tobacco use. Tobacco consumption in men more than doubled in Qidong between 1950 and 198115 and has more than doubled again by 2012 as adjudged by cigarette tax records (Qidong Tobacco Bureau). The Qidong Cancer Registry documents that the CASR for lung cancer incidence has tripled over the last 40 years, an increase in risk consonant with increased cigarette consumption in other cohorts.20 Women, by contrast, held a constant CASR from 1972 to about 2000, suggesting that long standing exposures to second hand smoke have not been a major contributor to risk. Women, have however, seen a substantive increase in lung cancer incidence over the last decade. Why?
Environmental factors beyond tobacco smoking contribute to lung cancer risk. Indoor and outdoor air pollution contains multiple lung carcinogens. Epidemiologic studies associate lung cancer in non-smoking Chinese women with Chinese-style wok cooking. Hecht and colleagues reported from the Singapore Chinese Women Health Study that women who regularly cooked at home were exposed to increased levels of volatile toxicants and carcinogens including acrolein, crotonaldehyde and benzene and have suggested that such volatile compounds generated during high temperature cooking with oils may contribute to lung cancer.21 Wok-style cooking occurs every day in China, particularly in Eastern China (including Qidong and Shanghai). A population-based case-control study among nonsmoking women living in Shanghai indicated that exposure to indoor air pollution from Chinese-style cooking, especially cooking at high temperatures in woks, may increase the risk of lung cancer22 In Qidong, as with much of China, cooking oil was severely rationed during the 1960s and 1970s. State rationing of cooking oils ended in the early-1980s as they became available in free markets. Perhaps the upsurge in lung cancer in women some 20 years on from the end of rationing reflects increasing exposures to cooking oil pyrolysis products. However, increases in the annual per capita consumption of edible oils in rural China have been linear from 1980 to 2009,23 as opposed to the delayed curvilinear response seen with lung cancer incidence in women (Figure 1).
Outdoor air pollution has been classified as a Group 1 carcinogen by IARC24 and levels of outdoor air pollution in China are among the highest in the world.25 A recent study highlighted the health effects of air pollution from the widespread use of coal for heating in Northern China.26 Southern Chinese have lived, on average, five years longer than their northern counterparts in part due to lower exposures to total suspended particles (the metric of air quality available) resulting from central planning policies fostering coal combustion in the north for heating homes. The Yangtze River Delta region of Southern China, which includes Qidong, is the fastest growing economic development area in China. Air pollution from expanding industrialization in the region nonetheless masks the horizon on many days, especially during the winter months. Increases in fossil fuel use in China’s industry, transport and residential sectors have resulted in a steep rise in emissions. The region, which constitutes only 2% of the area of China, contributes upwards of 15% of countrywide emissions of greenhouse gases.27 We have previously reported 5-fold higher levels of the PAH biomarker phenanthrene tetraol in the urines of non-smoking Qidongese compared to non-smoking residents of the Twin Cities region of Minnesota.17 Levels of mercapturic acids of benzene, crotonaldehyde and acrolein are also substantially higher in these Qidongese compared to non-smoker residents of Singapore.21 However, rigorous time-series data on the levels of these internal dose biomarkers in any population are lacking, such that it is challenging to link exposures to volatile organic chemical to changing trends in lung cancer or other adverse health outcomes such as increased rates of hospital admissions and exacerbation of chronic respiratory conditions along with decreased lung function. Measurements of these biomarkers in the non smoking women of Qidong in particular may provide insights to what extent, if any, these exposures to indoor and outdoor pollutants play in pulmonary diseases including cancer in this population.
Conclusions
While crude rates of cancer incidence increase in Qidong as the population ages, the CASR incidence trends for all cancer indicate a small overall decline over the past 40 years. Underneath this general trend, stomach, esophageal and cervical cancers have declined by 50% or more, but colorectal, pancreatic, brain and bladder cancers along with leukemias have increased markedly.2 Each cancer type has its own story to tell about changing host-environment interactions that define the emerging CASR trajectories. The changes in CASR for liver and lung cancer are not the largest, but affect the most people. The shifting landscape of known exposures to environmental carcinogens such as aflatoxins and tobacco-derived carcinogens play heavily on these altered trajectories of liver and lung cancers and can be directly documented. However, the onrushing urbanization and homogenization of the region will serve to layer more confounders over the principle etiologic determinants. The extensive longitudinal collections of archival serum and urine samples of the QDLCI together with the Qidong Cancer Registry will allow investigators to peek backwards as new ideas and companion biomarkers emerge for examination.
Acknowledgments
Funding
This work was supported by the National Institute of Environmental Health Science P01 grant ES006052 and the National Science and Technology Mega-Projects of China 2008ZX10002-015 and 2012ZX10002-008.
Abbreviations
- QDLCI
Qidong Liver Cancer Institute
- CASR
China age-standardized rate
- HBV
hepatitis B virus
- IARC
International Agency for Research on Cancer
References
- 1.Chen JG, Zhu J, Zhang YH, Lu JH. Cancer survival in Qidong, China, 1992–2000. IARC Sci Publ. 2011;162:43–53. [PubMed] [Google Scholar]
- 2.Chen JG, editor. Cancer in Qidong, China (1972–2011) Beijing: Military Medical Scientific Press; 2013. pp. 1–346. [Google Scholar]
- 3.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 4.Kensler TW, Qian GS, Chen JG, Groopman JD. Translational strategies for cancer prevention in liver. Nat Rev Cancer. 2003;3:321–329. doi: 10.1038/nrc1076. [DOI] [PubMed] [Google Scholar]
- 5.Ming L, Thorgeirsson SS, Gail MH, Lu P, Harris CC, Wang N, Shao Y, Wu Z, Liu G, Wang X, Sun Z. Dominant role of hepatitis B virus and cofactor role of aflatoxin in hepatocarcinogenesis in Qidong, China. Hepatology. 2002;36:1214–1220. doi: 10.1053/jhep.2002.36366. [DOI] [PubMed] [Google Scholar]
- 6.Qian GS, Ross RK, Yu MC, Yuan JM, Gao YT, Henderson BE, Wogan GN, Groopman JD. A follow-up study of urinary markers of aflatoxin exposure and liver cancer risk in Shanghai, People’s Republic of China. Cancer Epidemiol Biomarkers Prev. 1994;3:3–10. [PubMed] [Google Scholar]
- 7.Chen CJ, Wang LY, Lu SN, Wu MH, YOU SL, Zhang YJ, Wang LW, Santella RM. Elevated aflatoxin exposure and increased risk of hepatocellular carcinoma. Hepatology. 1996;24:38–42. doi: 10.1002/hep.510240108. [DOI] [PubMed] [Google Scholar]
- 8.International Agency for Research on Cancer (IARC) IARC Mongraphs on the Evaluation of Carcinogenic Risks to Humans. Vol. 100. World Health Organization; Lyon, France: 2012. [Google Scholar]
- 9.Zhu YR, Chen JG, Huang XY. Hepatocellular carcinoma in Qidong County. In: Tang ZY, Wu MC, Xia SS, editors. Primary Liver Cancer. Beijing: China Academic Publishers, Springer-Verlag; 1989. pp. 204–222. [Google Scholar]
- 10.Chen JG, Egner PA, Ng D, Jacobson LJ, Muñoz A, Zhu YR, Qian GS, Wu F, Yuan JM, Groopman JD, Kensler TW. Reduced aflatoxin exposure presages decline in liver cancer mortality in an endemic region of China. Cancer Prev Res. 2013;6:1038–1045. doi: 10.1158/1940-6207.CAPR-13-0168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun TT, Chu YR, Ni ZQ, Lu JH, Huang F, Ni ZP, Pei XF, Yu ZI, Liu GT. A pilot study on universal immunization of newborn infants in an area of hepatitis B virus and primary hepatocellular carcinoma prevalence with a low dose of hepatitis B vaccine. J Cell Physiol Suppl. 1986;4:83–90. [PubMed] [Google Scholar]
- 12.Nishiwaki-Matsushima R, Ohta T, Nishiwaki S, Suganuma M, Kohyama K, Ishikawa T, Carmichael WW, Fujiki H. Liver tumor promotion by the cyanobacterial cyclic peptide toxin microcystin-LR. J Cancer Res Clin Oncol. 1992;118:420–424. doi: 10.1007/BF01629424. [DOI] [PubMed] [Google Scholar]
- 13.Ueno Y, Nagata S, Tsutsumi T, Hasegawa A, Watanabe MF, Park HD, Chen GC, Chen G, Yu SZ. Detection of microcystins, a blue-green algal hepatotoxin, in drinking water sampled in Haimen and Fusui, endemic areas of primary liver cancer in China, by highly sensitive immunoassay. Carcinogenesis. 1996;17:1317–1321. doi: 10.1093/carcin/17.6.1317. [DOI] [PubMed] [Google Scholar]
- 14.Naugler WE, Sakurai T, Kim S, Maeda S, Kim K, Eisharkawy AM, Karin M. Gender disparity in liver cancer due to sex differences in MyD88-dependent IL-6 production. Science. 2007;317:121–124. doi: 10.1126/science.1140485. [DOI] [PubMed] [Google Scholar]
- 15.Chen JG, Peto R, Sun ZT, Zhu YR. Feasibility of a prospective study of smoking and mortality in Qidong, China. In: O’Neill IK, Chen J, Bartsch H, editors. Relevance to Human Cancer of N-Nitroso Compounds, Tobacco Smoke and Mycotoxins. IARC; Lyon: 1991. pp. 502–506. [PubMed] [Google Scholar]
- 16.Jacobson LP, Zhang BC, Zhu YR, Wang JB, Wu Y, Zhang QN, Yu LY, Qian GS, Kuang SY, Li YF, Fang X, Zarba A, Chen B, Enger C, Davidson NE, Gorman MB, Gordon GB, Prochaska HJ, Egner PA, Groopman JD, Muñoz A, Helzlsouer KJ, Kensler TW. Oltipraz chemoprevention trial in Qidong, People’s Republic of China: study design and clinical outcomes. Cancer Epidmiol Biomarkers Prev. 1997;6:257–265. [PubMed] [Google Scholar]
- 17.Kensler TW, Ng D, Carmella SG, Chen M, Jacobson LP, Muñoz A, Egner PA, Chen JG, Qian GS, Chen TY, Fahey JW, Talalay P, Groopman JD, Yuan JM, Hecht SS. Modulation of the metabolism of airborne pollutants by glucoraphanin-rich and sulforaphane-rich broccoli sprout beverages in Qidong, China. Carcinogenesis. 2012;33:101–107. doi: 10.1093/carcin/bgr229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pirie K, Peto R, Reeves GK, Green J, Beral V Million Women Study Collaborators. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet. 2013;381:133–141. doi: 10.1016/S0140-6736(12)61720-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thun MJ, Carter BD, Feskanich D, Freedman ND, Prentice R, Lopez AD, Hartge P, Gapstur SM. 50-Year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368:351–364. doi: 10.1056/NEJMsa1211127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Law MR, Morris JK, Watt HC, Wald NJ. The dose-response relationship between cigarette consumption, biochemical markers and risk of lung cancer. Br J Cancer. 1997;75:1690–1693. doi: 10.1038/bjc.1997.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hecht SS, Seow A, Wang M, Meng L, Koh WP, Carmella SG, Chen M, Han S, Yu MC, Yuan JM. Elevated levels of volatile organic carcinogen and toxicant biomarkers in Chinese women who regularly cook at home. Cancer Epidemiol Biomarkers Prev. 2010;19:1185–1192. doi: 10.1158/1055-9965.EPI-09-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhong L, Goldberg MS, Gao YT, Jin F. Lung cancer and indoor air pollution arising from Chinese-style cooking among nonsmoking women living in Shanghai, China. Epidemiol. 1999;10:488–494. [PubMed] [Google Scholar]
- 23.Huang J, Yang J, Rozelle S. Changing Food comsumption pattern and demand for agri-based industrial products in China: implications for Southeast Asia’s agricultural trade. In: Intal PS Jr, Oum S, Simorangkir MJO, editors. Agricultural Development, Trade & Regional Cooperationin Developing East Asia. ERIA; Jakarta: 2011. pp. 162–210. [Google Scholar]
- 24.Loomis D, Grosse Y, Lauby-Secretan B, El Ghissassi F, Bouvard V, Benbrahim-Tallaa L, Guha N, Baan R, Mattock H, Straif K IARC Working Group. The carcinogenicity of outdoor air pollution. Lancet Oncol. 2013 doi: 10.1016/S0140-6736(08)61345-8. http://dx.doi.org/10.1016/S1470-2045(13)70487-X. [DOI] [PubMed]
- 25.Chen B, Hong C, Kan H. Exposures and health outcomes from outdoor air pollutants in China. Toxicology. 2004;198:291–300. doi: 10.1016/j.tox.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 26.Chen Y, Ebenstein A, Greenstone M, Li H. Evidence on the impact of sustained exposure to air pollution on life expectancy from China’s Huai River policy. Proc Natl Acad Sci USA. 2013;110:12936–12941. doi: 10.1073/pnas.1300018110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou Y, Fu JS, Zhuang G, Levy JI. Risk-based prioritization among air pollution control strategies in the Yangze River delta, China. Environ Health Perspect. 2010;118:1204–1210. doi: 10.1289/ehp.1001991. [DOI] [PMC free article] [PubMed] [Google Scholar]


