Abstract
The processes of individual adaptation to chronic pain are complex and occur across multiple domains. The current study examined the social, cognitive, and affective context of daily pain adaptation in individuals with fibromyalgia and osteoarthritis. Using a sample of 260 women with fibromyalgia or osteoarthritis, this study examined the contributions of pain catastrophizing, negative interpersonal events, and positive interpersonal events to daily negative and positive affect across 30 days of daily diary data. Individual differences and daily fluctuations in predictor variables were estimated simultaneously by utilizing multilevel structural equation modeling techniques. The relationships between pain and negative and positive affect were mediated by stable and day-to-day levels of pain catastrophizing as well as day-to-day positive interpersonal events, but not negative interpersonal events. There are significant and independent contributions of pain catastrophizing and positive interpersonal events to adaptation to pain and pain-related affective dysregulation. These effects occur both between persons and within a person’s everyday life.
Keywords: pain catastrophizing, emotion, interpersonal relationships, chronic pain
Chronic pain adversely impacts the physical, cognitive, and emotional states of the sufferer [5]. Traditionally, psychosocial vulnerabilities have been the primary focus of studies examining failures of adaptation to chronic pain, but there are also positive psychological mechanisms that promote greater resilience to pain, which may be defined as the preservation of existing positive functioning or protection against subsequent negative emotional states [2,3,18,20,21]. Examination of both positive and negative emotional states as outcomes is therefore necessary when conceptualizing success or failure in adaptation to chronic pain, as it is likely that factors of individual resilience and vulnerability are at work at the same time [20]. In this paper, we sought to expand existing models of pain coping by examining the concurrent mediating roles of maladaptive cognitions about pain and positive and negative interpersonal events in pain-related affective disturbance in a sample of fibromyalgia patients.
Pain catastrophizing, an exaggerated cognitive and affective reaction to an expected or actual pain experience, has been identified as a powerful predictor of emotional functioning in individuals with chronic pain [23]. Pain catastrophizing is a normative, yet maladaptive, appraisal process that is motivated by a fear of experiencing pain [7]. Pain catastrophizing has been identified as an important mediator in explaining the relationship between pain experience and average and day-to-day indices of emotional dysregulation, including lower positive affect and greater depressive symptomatology and negative affect [22,23].
Pain coping is not simply an internal process, however; interpersonal relationships may dramatically impact an individual’s ability to adapt to chronic pain. Positive social interactions contribute to greater positive affect, a significant source of resilience to chronic pain [14]. Individuals with chronic pain disorders who experience many stressful interpersonal events also appear to be vulnerable to elevations in negative affect [8]. Additionally, when suffering from a pain flare, individuals may withdraw from social situations as an avoidant response or due to feelings of being misunderstood or rejected by others [11]. It might thus be expected that positive and negative interpersonal functioning also mediate the relationship between pain and emotional well-being. However, the occurrence of negative interpersonal events appears to blunt the positive effects of positive interpersonal events on a given day, and vice-versa [8], which highlights the need to model these influences concurrently in pain adaptation models.
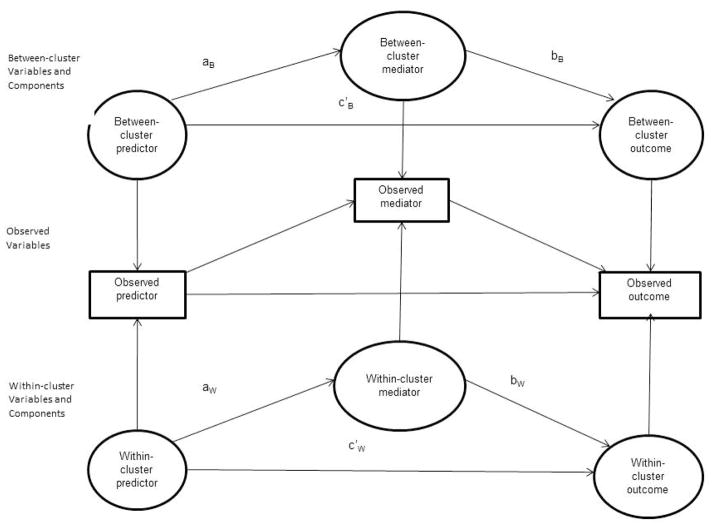
Figure 1 displays the predictions we made in this study. We hypothesized that the influence of pain on affective health would be indirect, mediated by pain catastrophizing and negative interpersonal events, both of which have been associated with poorer emotional functioning in individuals with chronic pain [8,20,22]. Furthermore, we hypothesized that the relationship between pain and affective changes would be buffered by the protective effects of positive interpersonal events, which have been implicated in enhanced positive emotions and buffered negative emotional states in individuals with chronic pain in past research [8,20].
Figure 1.
Model depicting the direct effects of pain intensity and indirect effects of pain intensity through pain catastrophizing and negative and positive interpersonal events on daily positive and negative affect.
Method
Participants
The study sample was comprised of individuals with fibromyalgia (FM), a rheumatic disorder characterized by widespread bodily pain, fatigue, and high susceptibility to depression [27], and osteoarthritis (OA), a rheumatic disorder defined primarily by joint pain and stiffness [1]. Participants were 260 women between the ages of 38 and 72 (mean age 57.42 years) with a physician-confirmed diagnosis of OA (N=106), FM (N=53), or a dual diagnosis of OA/FM (N=101). Median income in the sample was 30,000 – 39,000 dollars per year. 91.7% of participants reported their ethnicity to be Caucasian, approximately 5% reported their ethnicity as Hispanic, and 4% reported their ethnicity as African American (these ethnic categories were not exclusive, as participants could report more than one ethnicity). 30% of participants reported being employed full time, 23.6% of participants reported being employed part time, and 43.1% of all participants reported being unemployed. 54.5% of participants were married at the time of data collection.
Participants were recruited in the Phoenix, AZ metropolitan area from physician’s offices, advertisements, senior citizen groups, and mailings to members of the Southwest chapter of the Arthritis Foundation. Of the 260 participants, 137 (52.3%) responded to radio, television, newspaper advertisements, 34 (13.1%) responded to flyers from arthritis fairs, 25 (9.6%) responded to postings in physician’s offices, 19 (7.3%) responded to postings at a nearby university, 12 (4.6%) reported that they had heard of the study primarily by “word of mouth”, 6 (2.3%) were participants of prior studies conducted by the research lab that performed the current study and asked to be re-contacted for future studies, 3 (1.2%) responded to mailings via the Arthritis Foundation, and 24 (9.2%) did not report their method of recruitment. This sampling method was felt to improve the generalizability of the findings, as it yielded a sample that was comprised of a variety of individuals that were receiving diverse medical treatments (e.g., massage, acupuncture, general medical interventions), as well as others that were actively involved in advocacy and other socially-connected activities (e.g., arthritis fairs, senior citizen groups).
Potential participants first underwent a preliminary screening assessment of FM and OA symptoms by telephone [26]. Upon completion of the telephone assessment, participants signed a Health Insurance Portability and Accountability Act (HIPAA) release form. The research staff then contacted each participant’s physician, who sent a written confirmation of the participant’s stated diagnosis and disconfirmed diagnosis of other autoimmune disorders, which served as the basis of their inclusion in the study. All participants, regardless of physician diagnosis, underwent an initial in-home assessment, which included a standardized tender point assessment [16] using a standardized dolorimeter and gave their history to nursing staff who were trained and supervised by board-certified rheumatologists. The presence of FM was determined according to the 1990 American College of Rheumatology criteria: history of widespread pain for 3 months or more, and pain in 11 of 18 tender points upon digital palpation [28]. However, the results of the tender point examination were used as a separate measure of pain that was not examined in the current study, and the findings were not used as inclusionary criteria. Included in the study were participants who had no diagnosed autoimmune disorders, a pain rating above 20 on a 0–100 scale, and no involvement in litigation regarding their condition. A cutoff of greater than 20/100 for pain, rather than a 30/100 cutoff utilized by other studies [4], allowed for the inclusion of participants who were coping well with their chronic pain diagnoses, as well as those participants who were reporting comparatively greater levels of pain. 41 participants (15.8% of the sample) reported pain levels between 20/100 and 30/100.
Procedure
After enrolling in the study, participants were visited by a clinician to reconfirm FM diagnosis. Next, participants were trained by a research assistant to use a laptop computer to complete daily diaries each night for 30 days. Participants were encouraged to notify laboratory staff immediately if a problem occurred with the laptop. A built-in date-checking software program prevented data entry on days other than the correct day. In the event of laptop malfunction, a research assistant traveled to the participant’s home to replace the malfunctioning laptop with a working one. After completing 30 days of diaries, participants were visited by a clinician, debriefed and compensated for their efforts. The overall rate of completion was 92.5%. Participants were compensated up to $3 for each day of diaries (up to 30 total) that were completed.
Measures
Average Pain
Daily average pain was measured in the diary with a numerical rating scale (NRS) [32]. Daily average pain was measured using the question, “Please choose a number between 0 and 100 that best describes the average level of pain you have experienced today due to your Fibromyalgia or Osteoarthritis.” A zero (0) would mean ‘no pain’ and a one hundred (100) would mean ‘pain as bad as it can be.’ Test-retest reliability for average pain was r = .624.
Pain Catastrophizing
Daily pain catastrophizing was assessed in the daily diaries with two questions from the Coping Strategies Questionnaire (CSQ) [19], in which participants rated their level of agreement with each statement for that day: “I worried about whether my pain would ever end” and “I felt my pain was so bad I couldn’t stand it any more”. Ratings were made on a scale of 1 to 5 with 1 meaning “Strongly Disagree” and 5 meaning “Strongly Agree.” Daily catastrophizing scores were computed by averaging the two items. The internal consistency of the 2-item pain catastrophizing scale was good (α = .898).
Positive and Negative Affect
Positive affect (PA) and negative affect (NA) were measured through the use of the Positive and Negative Affect Schedule-Expanded Form (PANAS-X) [25]. Participants were given a list of 10 positive mood adjectives and 10 negative mood adjectives and asked to rate the extent to which they had experienced each mood on a 5-point scale from 1 “Very slightly or not at all“ to 5 “Extremely“. The internal consistency of the negative affect scale was good (α= .864), and the internal consistency for the positive affect scale was also good (α = .945).
Interpersonal Events
Measures of daily interpersonal events in daily life were assessed using the Inventory of Small Life Events (ISLE) [29]. Daily positive and negative interpersonal events were computed as sums of daily occurrences of stressful and positive events in the workplace and with one’s spouse or significant other, friends, and family. As the ISLE was designed to assess non-overlapping domains of interpersonal functioning [31], Cronbach’s alpha reliabilities for positive and negative interpersonal events were not computed. For total positive events, the test-retest reliability was r = .571, and for negative events the test-retest reliability was r =.432.
Data Analytic Strategy
The analyses in this study were conducted as a secondary data analysis from a dataset previously published by Finan, Zautra, & Davis [9]. The aims of this study did not overlap with those of any previous study relying on this data set. Multilevel structural equation models were estimated using the Mplus software [15] to test the direct effects of pain intensity on positive and negative affect and the indirect effects of pain intensity through three variables measured in the daily diaries: pain catastrophizing, positive interpersonal events, and negative interpersonal events (see Figure 1). The use of daily diaries allowed for the partitioning of stable and day-today variance, which could be modeled separately using multilevel structural equation modeling techniques. Multilevel structural equation modeling is preferable to regression modeling in conducting mediation analyses with hierarchical data sets for several reasons. First, statistical and theoretical mediating relationships often vary significantly across different levels of analysis, such that the temporal (day-to-day) relationship between variables may differ from the contextual (stable) relationship between those same variables. Multilevel structural equation modeling, unlike multilevel regression, can effectively estimate mediation models with more than one mediator at multiple levels of analysis [17]. Multilevel structural equation modeling is also valuable because this approach yields indices of model fit, which provide a valuable measure of the usefulness and appropriateness of an estimated model for a given dataset. Mediation analyses were conducted using the TYPE=TWOLEVEL RANDOM command, which allows for varying relationships among the variables at the person (Level-2) and daily observation (Level-1) levels. All of the variables in the structural equation models had a significant intraclass correlation, which indicated that there was significant stable variance in each of the examined diary variables (see Table 1).
Table 1.
Descriptive Statistics
| Item Composite | Mean | Standard Deviation | Intraclass Correlation |
|---|---|---|---|
| Negative Affect | 1.36 | .53 | .511 |
| Positive Affect | 2.47 | .97 | .671 |
| Pain Intensity | 54.20 | 23.58 | .571 |
| Pain Catastrophizing | 2.18 | 1.05 | .619 |
| Negative Interpersonal Events | .75 | 1.31 | .387 |
| Positive Interpersonal Events | 5.86 | 3.59 | .527 |
Observations were made based on 30 daily diary assessments from 260 women with a fibromyalgia and/or osteoarthritis diagnosis.
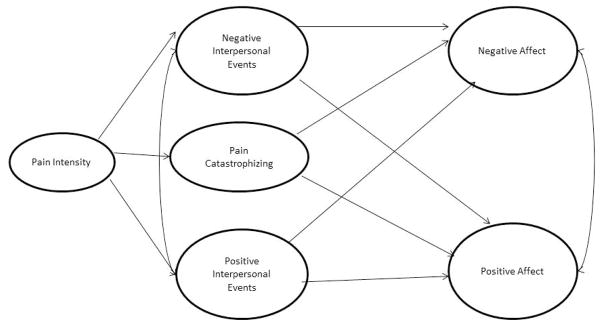
As Mplus two-level models create latent variable scores for both level-1 and level-2 variance [15], the model results reflect relationships between latent variables at each level, rather than between the observed variables themselves (see Figure 2). Predictors in the level-1 models were centered using individual cluster means, and predictors in level-2 models were centered using the grand mean. Mediating (indirect) effects were calculated using the product of the coefficients of the predictor-mediator path (the a path) and the mediator-outcome path (the b path). As multilevel mediation models are susceptible to correlations between the a and b paths, which can result in artificial inflation or deflation of path coefficients due to the covariance between two effects [14], asymmetric confidence limits for the mediating effect of each mediator were computed using Rmediation, which can account for correlations between the a and b paths [24]. Adequacy of model fit was determined by estimation of several fit indices, including the comparative fit index (CFI), the root mean square error of approximation (RMSEA), and the within- and between-cluster standardized root-mean-square residuals (SRMRs). As chi square tests are susceptible to overestimation of model misfit as the sample size increases [12], chi square estimates were computed and reported, but were interpreted with caution. Following the recommendations of Hu and Bentler [12], good model fit was indicated by scores of .90 or higher on the CFI and scores under .05 for RMSEA and SRMR parameters. Freeing positive and negative interpersonal events to co-vary in both the within-person and between-person models substantially improved model fit for all variables and was deemed appropriate in order to account for any non-specific effect of general interpersonal activity. As a result, these covariances were freed in both between-person and within-person models.
Figure 2.
Conceptual model depicting between-person and within-person relationships using two-level multilevel structural equation modeling techniques.
Note: Paths marked with an a denote paths from predictor to mediator, and paths marked with a b denote paths from mediator to outcome.
Note: Paths marked with a W subscript denote within-cluster paths, and with a B subscript denote between-cluster paths.
Results
Demographics
Individuals who were employed reported a significantly greater average number of both daily negative events (t(250) = −4.015, p < .001) and daily positive events t(250) = −1.987, p = .048 than those who were unemployed. Married participants reported a significantly greater number of both positive daily events (t(250) = 4.153, p < .001) and negative daily events (t(250) = 2.997, p = .003) than unmarried participants. As marital status and employment status predicted differences in the number of positive and negative interpersonal events reported by participants, separate models were estimated for married, unmarried, employed, and unemployed participants.
Within-person mediation path models
Within-person (state) mediation models were estimated using multilevel path models that estimated mediated effects at the day-to-day level (see Table 2). Pain intensity was positively related to daily pain catastrophizing levels (aW1C= .016, p < .01) and positive interpersonal events (aW2C = −.009, p < .01), but was unrelated to daily negative interpersonal events (aW3C = .001, p > .10). Daily pain catastrophizing levels significantly predicted greater daily negative affect (bW1C = .144, p < .01) and daily lower positive affect (bW2C = −.145, p < .01). A greater number of daily positive interpersonal events were significantly related to less daily negative affect (bW3C = −.007, p < .01) and greater daily positive affect (bW4C = .060, p < .01) on the same day. More daily negative interpersonal events predicted greater same-day negative affect (bW5C = .086, p < .01) but were unrelated to same-day positive affect (bW6C = −.010, p > .10). Pain catastrophizing levels were found to significantly mediate the relationship between pain levels and daily average negative affect (abW1C = −.002, p < .01) and positive affect (abW2C = .002, p < .01). Daily frequency of positive interpersonal events significantly mediated the relationships between daily pain intensity and both daily negative affect (abW3C = .0001, p < .05) and positive affect (abW4C = −.0005, p < .01). The frequency of daily negative interpersonal events did not mediate any relationships between daily pain intensity and daily levels of negative affect or positive affect (ps > .10). Asymmetric confidence limits calculated from Rmediation indicated that these mediated effects did not change when the correlation between a and b path coefficients were taken into account.
Table 2.
Within-participant mediation models
| Outcome | Mediator | a Path B (SE B) | b Path B (SE B) | ab Mediating Effect | Correlation of a and b | Asymmetric Confidence Limits |
|---|---|---|---|---|---|---|
| Negative Affect | Positive Events | −.009 (.002)** | −.007 (.002)** | .00006* | .089 | [.00002, .0001] |
| Negative Events | .001 (.001) | .086 (.008)** | .00009 | .114 | [−.0001, .0003] | |
| Pain Catastrophizing | .016 (.001)** | .144 (.012)** | .002** | −.057 | [.002, .003] | |
|
| ||||||
| Positive Affect | Positive Events | −.009 (.002)** | .060 (.003)** | −.0005** | −.137 | [−.008 −.003] |
| Negative Events | .001 (.001) | −.010 (.007) | −.0001 | .069 | [−.0004, .0001] | |
| Pain Catastrophizing | .016 (.001)** | −.145 (.017)** | −.002** | .134 | [−.0003, −.0002] | |
p < .10.
p < .05.
p < .01.
When the within-person path models were estimated separately for married and unmarried participants, a few notable differences emerged. The path from positive interpersonal events to negative affect was significant and negative in unmarried participants (bW3C = −.008, p < .01), but was non-significant in married participants (bW3C = −.004, p > .10). Similarly, the mediated effect of pain intensity on negative affect through positive interpersonal events was significant for unmarried participants and non-significant for married participants when asymmetric confidence limits were constructed. When the within-person path models were estimated separately for employed and unemployed participants, the path from positive interpersonal events to negative affect was found to be significant and negative in unemployed participants (bW3C = −.008, p < .05), but non-significant in employed participants (bW3C = −.005, p > .10). However, the mediated effect of pain intensity on negative affect through positive interpersonal events remained non-significant in both employed and unemployed participants.
Between-person mediation path models
Between-person (stable variance) mediation models were also estimated using multilevel path models (see Table 3). Average pain intensity levels were positively related to average pain catastrophizing levels (aB1= .026, p < .01), but did not predict average positive interpersonal events (aB2 = −.015, p > .10) or negative interpersonal events (aB3 = .002, p > .10). Average pain catastrophizing levels were significantly related to greater average negative affect (bB1 = .185, p < .01) and were significantly related to lower average positive affect (bB2 = −.381, p < .01). Average number of positive interpersonal events were significantly related to greater average levels of positive affect (bB4 = .081, p < .01), but unrelated to average levels of negative affect (bB3 = −.013, p > .10). Average number of negative interpersonal events was related to average levels of negative affect (bB5 = .140, p < .01) but unrelated to average positive affect levels (bB6 = −.024, p > .10). Average pain catastrophizing levels were found to significantly mediate the relationship between average pain levels and both average negative affect (abB1 = .005, p < .01) and average negative affect (abB2 = −.010, p < .01). Average levels of positive interpersonal events and negative interpersonal events were not found to mediate any paths between average pain intensity and either average negative affect or average positive affect levels (ps > .10). Asymmetric confidence limits calculated from Rmediation indicated that these mediated effects did not change when the correlation between the a and b path coefficients were taken into account. The fit indices for the multilevel SEM indicated good model fit, specifically the RMSEA (RMSEA = .020), CFI (CFI = .995), TLI (TLI = .966) and within-level and between-level SRMR indices (SRMRW = .008, SRMRB = .038). The chi square for the estimated model indicated model misfit (χ2(4) = 13.192, p < .05), but, as mentioned previously, this indicator of misfit may have been due to the large sample size.
Table 3.
Between-participant mediation models
| Outcome | Mediator | a Path B (SE B) | b Path B (SE B) | ab Mediating Effect | Correlation of a and b | Asymmetric Confidence Limits |
|---|---|---|---|---|---|---|
| Negative Affect | Positive Events | −.015 (.010) | −.013 (.008) | .0002 | −.010 | [−.0009, .007] |
| Negative Events | .002 (.003) | .140 (.031)** | .0003 | .344 | [−.001, .001] | |
| Pain Catastrophizing | .026 (.003)** | .185 (.031)** | .005** | −.030 | [.003, .007] | |
|
| ||||||
| Positive Affect | Positive Events | −.015 (.010) | .081 (.017)** | −.001 | .060 | [−.003, .004] |
| Negative Events | .002 (.003) | −.024 (.051) | −.00005 | .177 | [−.0003, .0006] | |
| Pain Catastrophizing | .026 (.003)** | −.381 (.066)** | −.010** | −.026 | [−.015, −.006] | |
p < .10.
p < .05.
p < .01.
When the between-person path models were estimated separately for married and unmarried participants, the ab product representing the mediated effect of average pain intensity on average positive affect through the average number of positive interpersonal events was found to be significant in married participants but non-significant in unmarried participants. However, when the correlation between the a and b path coefficients was taken into account using Rmediation, this difference disappeared and the mediated effect was non-significant for both married and unmarried participants. When between-person path models were estimated separately for employed and unemployed participants, one path was found to differ between the groups: the path from average positive interpersonal events to average positive affect was significant for unemployed participants (bB4 = .108, p < .01) and only marginally significant in employed participants (bB4 = .048, p < .10). However, the mediated effect of average pain on average positive affect through average positive interpersonal events remained non-significant for both employed and unemployed participants.
Discussion
In the current study, we sought to expand current models of pain coping by examining the independent contributions of social and cognitive contributors to pain adaptation using both day-to-day and stable variance yielded from 30 days of daily diaries. Our results replicate previous research on the role of pain catastrophizing in daily pain adaptation [22], and indicate that day-to-day changes (i.e., level-1) in pain catastrophizing play a key role in decreases in positive affect and increases in negative affect that accompany increases in pain. Likewise, more frequent engagement in pain catastrophizing on average partially explains why individuals with higher stable levels of pain report lower average levels of positive affect and higher average levels of negative affect. Our findings also indicate that the effects of pain on emotional well-being are mediated by not only cognitive reactions, but by the independent contributions of both positive and negative social relations.
Our results indicated that increases in daily pain predicted a decreased number of daily positive interpersonal events, which, in turn predicted lower levels of positive affect and increased levels of negative affect on the same day. However, pain intensity levels were unrelated to day-to-day changes in the number of reported negative interpersonal events. Pain intensity thus influences daily negative affect and daily positive affect through decreases in daily positive interpersonal events, independent of the effects of daily negative interpersonal events. Interestingly, stable levels of pain were found to be unrelated to average reported numbers of both positive and negative interpersonal events, which indicates that the interpersonal consequences of pain (specifically, decreased positive social engagement) are best characterized as normative and dynamic, rather than stable individual differences. Individuals whose typical pain levels are higher do not seem to demonstrate an increased tendency to withdraw from positive social engagement; rather, this process of social withdrawal appears to occur on days of greater pain intensity than is typical for an individual, regardless of the intensity of his or her average pain level.
It is also noteworthy that negative interpersonal events, though unrelated to pain levels, predicted negative affect in both within-person and between-person models. That negative interpersonal events are related to negative emotional outcomes is not a novel finding [29], but the findings indicate a potential two-factor model of affective vulnerability in individuals with chronic pain. First, individuals with chronic pain may suffer from day-to-day reductions in their positive emotions that are due to the immediate intensity of their current pain catastrophizing and withdrawal from their positive relationships. Furthermore, those individuals with greater stable levels of pain will be more likely to report lower average levels of positive affect due to greater average levels of pain catastrophizing. Second, their negative emotional states are exacerbated by unpleasant or conflictual social interactions, independent of stable or diurnal pain levels. Thus, when individuals are suffering from greater immediate levels of pain, they do not withdraw from their environment completely (as this hypothesis might predict individuals in pain would engage in fewer events overall, regardless of their valence), but ultimately engage in fewer positive interpersonal events. These findings may explain why the strategy of pain avoidance may have such profoundly negative consequences for individuals suffering from chronic pain. Consistent with previous findings [30], individuals who withdraw from their surroundings due to pain do not successfully withdraw from stressful interactions; instead, they exacerbate their emotional distress by removing one powerful source of emotional resilience, positive social interactions, while negative interpersonal events continue to occur.
The current study has some important limitations that should be acknowledged. It should be noted that the variables in the current study are likely to be mutually influential and, given the concurrent measurement of items in the daily diaries, the true temporal order of these relationships cannot be stated with certainty. For example, the relationship between negative interpersonal events and negative affect is likely to be bi-directional, such that the intensity of negative affective states would significantly predict the frequency of negative interpersonal events, as negative emotional states, specifically high-activation emotional states like anger, have been found to presage social conflict in individuals with chronic pain [7]. Similarly, as catastrophizing is commonly defined as containing both cognitive and affective aspects [23], there is necessarily an overlap between pain catastrophizing and affective states; we propose, however, that pain catastrophizing may be appropriately defined as a maladaptive appraisal process that connects pain and mood, as others have done [23]. Although pain catastrophizing, interpersonal functioning, and mood states are certainly mutually influential, the model proposed in the current paper attempts to deconstruct the processes underlying pain-related affective dysregulation by imposing a theoretical explanation that may clarify the directionality of these effects. More specifically, the current results indicate that individuals in pain have concurrent processes of both resilience (positive interpersonal events that dampen negative emotional reactions and buffer positive emotional functioning in response to pain) and vulnerability (pain catastrophizing and negative interpersonal events that exacerbate negative emotional states and dampen positive emotional states), all of which must be considered to yield an accurate understanding of emotional adaptation to pain.
Also missing from the current paper is any measure of individual volition, which might better reflect the construct of social or behavioral avoidance than does a count of daily interpersonal events. Inclusion of motivational factors is an increasingly important consideration for models of pain coping, and may provide an incremental improvement in modeling of fluctuations in pain adaptation [5]. It is worthwhile to consider whether individuals who are suffering from greater immediate pain make a conscious decision to withdraw from their social environment (e.g., due to a feeling that they cannot handle any interpersonal challenges) or whether this social withdrawal is largely secondary to a broader sense of behavioral avoidance (e.g., missing work, avoiding exercise or other pleasurable activities). Further clarification of the motivational aspects of pain-related social avoidance may provide valuable information about the nature of pain avoidance and potentially valuable information about intervention to maintain positive social engagement in individuals coping with recurrent pain.
Although the prevalence of osteoarthritis over the age of 45 and the overall prevalence of fibromyalgia are significantly higher in women than in men [10], it should be noted that the entirely female sample used in the current paper may affect interpretability of the current findings. Rates of catastrophizing and certain behaviors of pain expression may vary between men and women with chronic pain [13]. As a result, the current results should be interpreted with an understanding that the cognitive and social consequences of pain noted in the current study may have been different if the study had included male participants.
The use of multilevel structural equation modeling techniques was a novel feature of the current study, as these techniques allowed for estimation of relationships at both the day-to-day (within-person) and stable (between-person) levels of analysis. These techniques allowed us to ask who are the individuals who demonstrate a comparatively better or worse ability to cope with changes in their everyday pain, and when are the moments that this process of adaptation is more difficult or altogether unsuccessful? Our findings demonstrated that some relationships (e.g., between pain intensity, pain catastrophizing, and emotional states) are significant in both stable-variance and day-to-day variance models. For example, those individuals who report greater stable levels of pain catastrophizing tend to report greater stable levels of negative affect and lower stable levels of positive affect, but greater catastrophizing on a given day also predicts greater negative affect and lower positive affect on the same day for all individuals. Other relationships, however, are best understood as dynamic processes that occur independent of an individual’s average level of pain intensity; our findings indicated that individuals reported fewer positive interpersonal events on days of greater pain, but an individual’s average level of pain across 30 diaries was unrelated to their average number of positive events reported per day. The current findings provided greater clarity into the dynamics of affective adaptation to pain, as maladaptive appraisal patterns and intrapersonal dynamics were found to play a key role in the emotional dysregulation in individuals with osteoarthritis and fibromyalgia. Given the multidimensional nature of pain experience, the current study highlights the value of concurrently examining multiple mechanisms that may be involved in adaptation to chronic pain.
Supplementary Material
Acknowledgments
The current study was supported by Grant R01 AR046034 from the National Institute of Musculoskeletal, Immune, and Skin Disease. The authors have no conflict of interest to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Arden N, Nevitt MC. Osteoarthritis: Epidemiology. Best Pract Res Clin Rheumatol. 2006;20:3–25. doi: 10.1016/j.berh.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 2.Baliki MN, Geha PH, Jabakhanji R, Harden N, Schnitzer TJ, Apkarian AV. A preliminary fMRI study of analgesic treatment in chronic back pain and knee osteoarthritis. Molecular Pain. 2008:4. doi: 10.1186/1744-8069-4-47. http://www.molecularpain.com/content/4/1/47. [DOI] [PMC free article] [PubMed]
- 3.Bonanno G. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- 4.Bonanno GA, Diminich ED. Annual research review: Positive adjustment to adversity- Trajectories of minimal-impact resilience and emergent resilience. J Child Psychol Psychiatry. 2013;54:378–401. doi: 10.1111/jcpp.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crombez G, Eccleston C, Van Damme S, Vlaeyen JWS, Karoly P. Fear-avoidance model of chronic pain: The next generation. Clin J Pain. 2012;28:475–483. doi: 10.1097/AJP.0b013e3182385392. [DOI] [PubMed] [Google Scholar]
- 6.Crombez G, Viane I, Eccleston C, Devulder J, Goubert L. Attention to pain and fear of pain in patients with chronic pain [published online ahead of print May 22 2012] J Behav Med. 2012 doi: 10.1007/s10865-012-9433-1. http://link.springer.com/article/10.1007%2Fs10865-012-9433-1. [DOI] [PubMed]
- 7.Feldman SI, Downey G, Shaffer-Neitz R. Pain, negative mood, and perceived support in chronic pain patients: A daily diary study of people with reflex sympathy dystrophy syndrome. J Consult Clin Psychol. 1999;67:776–785. doi: 10.1037//0022-006x.67.5.776. [DOI] [PubMed] [Google Scholar]
- 8.Finan PH, Okun MA, Kruszewski D, Davis MC, Zautra AJ, Tennen H. The interplay of concurrent positive and negative interpersonal events in the prediction of daily negative affect and fatigue for rheumatoid arthritis patients. Health Psychol. 2010;29:429–437. doi: 10.1037/a0020230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Finan PH, Zautra AJ, Davis MC. Daily affect relations in fibromyalgia patients reveal positive affect disturbance. Psychosom Med. 2009;71:474–482. doi: 10.1097/PSY.0b013e31819e0a8b. [DOI] [PubMed] [Google Scholar]
- 10.Greenspan JD, Craft RM, LeResche L, Arendt-Nielsen L, Berkley KJ, Fillingim RB, Traub RJ. Studying sex and gender differences in pain and analgesia: A consensus report. Pain. 2007;132:S26–S45. doi: 10.1016/j.pain.2007.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hadjistavropoulos T, Craig KD, Duck S, Cano A, Goubert L, Jackson PL, Mogil JS, Rainville P, Sullivan MJ, de C Williams AC, Vervoort T, Fitzgerald TD. A biopsychosocial formulation of pain communication. Psychol Bull. 2011;137:910–939. doi: 10.1037/a0023876. [DOI] [PubMed] [Google Scholar]
- 12.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 13.Keefe FJ, Lefebvre JC, Egert JR, Affleck G, Sullivan MJ, Caldwell DS. The relationship of gender to pain, pain behavior, and disability in osteoarthritis patients: The role of catastrophizing. Pain. 2000;87:325–334. doi: 10.1016/S0304-3959(00)00296-7. [DOI] [PubMed] [Google Scholar]
- 14.Kenny DA, Bolger N, Korchmaros JD. Lower-level mediation in multilevel models. Psychol Methods. 2003;8:115–128. doi: 10.1037/1082-989x.8.2.115. [DOI] [PubMed] [Google Scholar]
- 15.Muthen LK, Muthen BO. Mplus Users’s Guide. 4. Los Angeles: Muthen & Muthen; 2007. [Google Scholar]
- 16.Okifuji A, Turk DC, Marcus DA. A standardized manual tender point survey. I. Development and determination of a threshold point for the identification of positive tender points FM syndrome. J Rheumatol. 1997:377–383. [PubMed] [Google Scholar]
- 17.Preacher KJ, Zyphur MJ, Zhang Z. A general multilevel SEM framework for assessing multilevel mediation. Psychol Methods. 2010;15:209–233. doi: 10.1037/a0020141. [DOI] [PubMed] [Google Scholar]
- 18.Reich JW, Zautra AJ, Hall JS, editors. Handbook of Adult Resilience. New York: Guilford Press; 2010. [Google Scholar]
- 19.Rosentiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: the relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 20.Smith BW, Zautra AJ. Vulnerability and resilience in women with arthritis: Test of a two-factor model. J Consult Clin Psychol. 2008;76:799–810. doi: 10.1037/0022-006X.76.5.799. [DOI] [PubMed] [Google Scholar]
- 21.Sturgeon JA, Zautra AJ. Resilience: A new paradigm for adaptation to chronic pain. Curr Pain Headache Rep. 2010;14:105–112. doi: 10.1007/s11916-010-0095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sturgeon JA, Zautra AJ. State and trait pain catastrophizing and emotional health in rheumatoid arthritis. Ann Behav Med. 2013;45:69–77. doi: 10.1007/s12160-012-9408-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sullivan MJL, Thorn B, Haythornthwaite JA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Tofighi D, MacKinnon DP. RMediation: An R package for mediation analysis confidence intervals. Behav Res Methods. 2011;43:692–700. doi: 10.3758/s13428-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Watson D, Clark LA. Manual for the Positive and Negative Affect Schedule-Expanded Form. Iowa City, IA: The University of Iowa; 1994. The PANAS-X. [Google Scholar]
- 26.White KP, Speechley M, Harth M, Ostbye T. The London Fibromyalgia Epidemiology Study: the prevalence of fibromyalgia syndrome in London, Ontario. J Rheumatol. 1999;26:1570–1576. [PubMed] [Google Scholar]
- 27.Wolfe F. Determinants of WOMAC function, pain and stiffness scores: Evidence for the role of low back pain, symptom counts, fatigue and depression in osteoarthritis, rheumatoid arthritis, and fibromyalgia. Rheumatol. 1999;38:355–361. doi: 10.1093/rheumatology/38.4.355. [DOI] [PubMed] [Google Scholar]
- 28.Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg Sheon RP. The American College of Rheumatology 1990 Criteria for the classification of fibromyalgia. Arthritis Rheum. 1990;33:160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 29.Zautra AJ, Guarnaccia CA, Dohrenwend BP. Measuring small life events. Am J Community Psychol. 1986;14:629–655. doi: 10.1007/BF00931340. [DOI] [PubMed] [Google Scholar]
- 30.Zautra AJ, Hamilton NA, Burke HM. Comparison of stress responses in women with two types of chronic pain: Fibromyalgia and osteoarthritis. Cognit Ther Res. 1999;23:209–230. [Google Scholar]
- 31.Zautra AJ, Johnson LM, Davis MC. Positive affect as a source of resilience for women in chronic pain. J Consult Clin Psychol. 2005;73:212–220. doi: 10.1037/0022-006X.73.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zautra AJ, Smith B, Affleck G, Tennen H. Examinations of chronic pain and affect relationships: Applications of a dynamic model of affect. J Consult Clin Psychol. 2001;69:786–795. doi: 10.1037//0022-006x.69.5.786. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.