Abstract
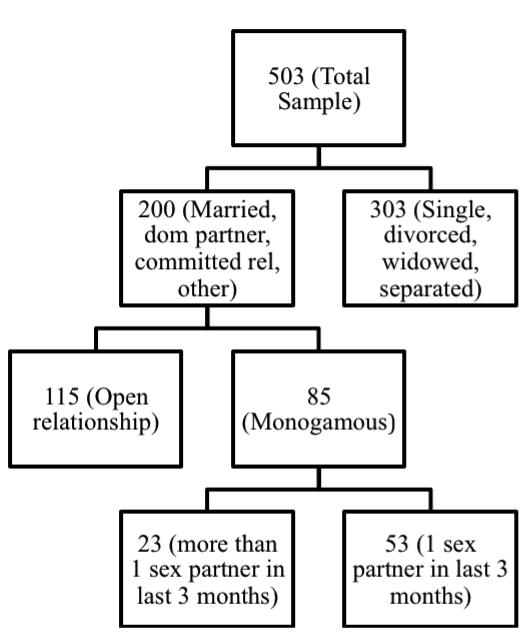
Sexual behavior of men who have sex with men (MSM), within and outside of one’s primary relationship, may contribute to increased risk of HIV transmission among those living with HIV. The current study sought to understand how HIV-infected MSM report their relationship status and the degree to which this corresponds with their sexual behavior. Further, we examined rates and psychosocial associations with sexual HIV transmission risk behavior (TRB) across relationship categories. In a sample of 503 HIV-infected MSM in HIV care, 200 (39.8%) reported having a primary partner. Of these, 115 reported that their relationship was open and 85 reported that it was monogamous. Of the 85 who reported a monogamous relationship, 23 (27%) reported more than one sexual partner in the prior three months, 53 (62%) reported only one partner, and nine did not report on the number of partners in the past 3 months. Hence, there were three categories of relationships: (1) “monogamous with one sexual partner,” (2) “monogamous with more than one sexual partner,” and (3) “open relationship.” The “monogamous with more than one sexual partner” group reported higher TRB and crystal methamphetamine use compared to the “monogamous with one sexual partner” group and different patterns of relationships with TRB emerged across the three groups. Couples-based HIV prevention interventions for MSM may be enhanced by considering that there may be different definitions of monogamy among MSM, and that the context of relationship status may require tailoring interventions to meet the needs of specific subgroups of MSM couples.
Keywords: HIV/AIDS, MSM, couples, sexual risk, monogamy, sexual orientation
INTRODUCTION
Men who have sex with men (MSM) continue to be at disproportionately high risk for HIV infection and they comprise the largest number of individuals living with HIV in the U.S. when compared with other risk groups (CDC, 2011; Prejean et al., 2011). It has been estimated that a substantive proportion (from about 33-68%) of HIV transmissions in MSM occur through unprotected anal intercourse (UAI) between primary partners (Sullivan, Salazar, Buchbinder, & Sanchez, 2009). This may be accounted for by a number of factors, including a higher number of UAI acts with primary vs. casual partners. These factors illustrate that MSM in relationships with primary partners may be at greater risk for acquiring and transmitting HIV than single men or men with casual partners only.
In addition to monogamous primary partnerships, several studies have documented the characteristics of relationships, in which one partner may be considered a “primary” partner, but additional sex partners outside of the primary couple are permitted according to rules agreed upon by both partners (Hoff & Beougher, 2010; Mitchell, Harvey, Champeau, & Seal, 2012). Findings on the differences between monogamous and non-monogamous men on a variety of health outcomes have been mixed. Some studies have shown no significant group differences on demographic, sexual risk or mental health variables (LaSala, 2004; Wagner, Remien, & Carballo-Dieguez, 2000). Others indicate that monogamy may be protective, as men in such relationships use substances less frequently (Parsons, Starks, DuBois, Grov, & Golub, 2013). Non-monogamy may also confer protective elements, as non-monogamous men may be more likely than monogamous men to discuss safe sex practices with their primary partners (Crawford et al., 2003) and are more likely than monogamous men to use condoms with their primary partners (Calsyn, Campbell, Tross, & Hatch-Maillette, 2011). However, there is literature indicating that monogamy among MSM is protective in terms of sexual risk behavior and HIV transmission, as newly infected MSM who are in multiple concurrent relationships may be at high risk of HIV transmission (Kim, Riolo, & Koopman, 2010; Morris & Little 2011).
Determining the presence of concurrent sexual behavior within self-reported monogamous or non-monogamous relationships requires a nuanced means of assessment. The literature has operationalized monogamy and non-monogamy in varied ways. Most studies have assessed monogamy by simply asking participants if their relationship is monogamous (Darbes, Chakravarty, Beougher, Neilands, & Hoff, 2012; Fergus, Lewis, Darbes, & Butterfield, 2005; Fergus, Lewis, Darbes, & Kral, 2009). Some studies obtain a couple’s self-reported relationship status or a description of their sexual agreements (Hoff, Beougher, Chakravarty, Darbes, & Neilands, 2010; Wheldon & Pathak, 2010). Others have assessed each partner’s number of primary and casual sex partners to classify relationships as monogamous or non-monogamous, with the assumption that the presence of any casual sex partners within a primary relationship constitutes non-monogamy (Lightfoot, Song, Rotheram-Borus, & Newman, 2005). Moreover, other studies have utilized both of the above methods, which has often revealed a discrepancy between relationship agreements and actual behavior--that is, within some self-reported monogamous couples, one or both partners may engage in UAI with casual partners without their primary partner’s knowledge or consent (Parsons et al., 2013; Wagner et al., 2000). One study described those who engaged in these discrepant agreements as “secretive” (Wagner et al., 2000). Few studies have included secretive couples as a distinct group for analyses; one study, for example, excluded such couples from analyses because they could not be classified as monogamous or non-monogamous (Parsons et al., 2013).
Research on couples with secretive or discrepant agreements has revealed significant differences from monogamous and non-monogamous couples. For example, couples with discrepant agreements are more likely to engage in UAI with a casual partner than couples who did not have discrepant agreements, regardless of whether their agreement was monogamous or non-monogamous (Mitchell, Harvey, Champeau, Moskowitz, & Seal, 2011). This indicates that a discrepant agreement may itself serve as a marker of increased sexual risk whether or not the partners are in disagreement as to whether they are monogamous or non-monogamous. Additionally, couples where one partner has additional partners, but, in the context of a relationship that is stated to be monogamous, tend to report greater psychological distress than monogamous or non-monogamous couples (Wagner et al., 2000). These findings underlie important considerations for the sexual health of MSM couples, in that some men who self-report as monogamous may engage in UAI outside of their primary partnerships, thus putting their primary partners at risk of HIV infection. Additionally, this research also demonstrates that there can be discordance between self-reported relationship status and actual sexual behavior among MSM couples, which has implications for how interventionists or behavioral scientists assess relationship status. It is not enough to conceptualize all sexual behavior that occurs outside of a primary partnership as the same, since the context in which this behavior occurs (i.e., within an explicitly non-monogamous relationship vs. a supposedly monogamous relationship) may be a marker for other clinically relevant differences between couples, such as increased psychological distress (Wagner et al., 2000), increased risk of UAI with casual partners (Mitchell et al., 2011), and lower likelihoods of discussing safe sex practices within couples (Crawford et al., 2003).
The current study sought to better understand how HIV-infected MSM report their relationship status (i.e., monogamous or not) and the degree to which this corresponds with their sexual behavior (i.e., whether those who report monogamous relationships also report only one sexual partner). We then explored the differences between couples of the relationship statuses that emerged, on a number of psychosocial and sexual health variables. Because previous research has demonstrated that variables such as substance use (Parsons et al., 2013), psychological distress (Wagner et al., 2000), and communication about safer sex (Crawford et al., 2003) vary across different relationship statuses, similar variables were examined in this study to determine whether or not these findings would be replicated in our sample, as well as to determine whether or not these findings would be replicated when self-reported relationship status and actual sexual behavior were both taken into account for the creation of relationship status comparison groups. Rather than a broad measure of psychological distress, depressive symptoms were assessed, as moderate levels of depression have been shown to predict HIV transmission risk behavior among HIV-infected MSM (O’Cleirigh, Newcomb, Mayer, Skeer, & Safren, in press). We included measures of condom use self-efficacy, HIV transmission beliefs, and disclosure self-efficacy, as these variables are conceptually related to communication about sexual health, and have been used as covariates of sexual risk in the current sample (O'Cleirigh, Mayer, Covahey, Leidolf, & Safren, 2009). Lastly, profiles of sexual risk behavior were modeled for each relationship status group.
METHOD
Participants and Procedure
The sample was drawn from participants who were screened and/or subsequently enrolled in two secondary HIV prevention interventions for HIV-infected MSM (Safren et al., 2011; Safren, O’Cleirigh, Skeer, Elsesser, & Mayer, 2013 (see Fig. 1). Participants were recruited from the largest ambulatory HIV primary care facility in New England, based in Boston, which has traditionally served sexual minority populations generally and HIV-infected MSM specifically (Mayer et al., 2001). Eligibility for the parent studies included (1) having an HIV diagnosis for at least three months; (2) being over age 18 years; (3) self-identifying as a MSM; and (4) receiving primary HIV care at the community health center (see Table 1).
Figure 1.
Flowchart of participants
Note. Nine participants did not report on the number of partners in the past 3 months
Table 1.
Demographic Characteristics of the Sample
| Mean (SD) or Percentage | |
|---|---|
| Age (in years) | 40.7 (7.8) |
| Race/Ethnicity | |
| White | 74.6% |
| Black/African American | 11.9% |
| Latino/Hispanic | 8.5% |
| Other | 5.0% |
| Education | |
| <High School | 2.0% |
| High School/GED | 10.0% |
| Some College | 33.3% |
| College Degree | 38.3% |
| Graduate Degree | 16.4% |
| Annual income | |
| Less than $20,000 | 28.9% |
| $20,001 – $40,000 | 24.9% |
| $40,001 – $60,000 | 15.9% |
| Greater than $60,000 | 30.3% |
| HIV-Disease and Medication | |
| CD4 count (cells/mm3) | 538.5 (286.6) |
| Viral load (mean plasma HIV RNA: copies/ml) | 18,332 (52,689) |
| Undetectable Viral Load | 50.0% |
| Currently taking HIV medication | 56.7% |
| Ever taken HIV medication | 66.2% |
During the screening/baseline visit, trained research assistants explained study procedures and obtained informed consent, including permission to extract information from electronic medical records. Each participant then completed an audio-computer assisted self-interviewing assessment that addressed demographic data, HIV history, psychosocial variables, and sexual risk behaviors. Participants received monetary compensation for their time and effort. The Fenway Health Institutional Review Board approved of all study procedures.
Measures
Demographics
Participants age, education, ethnicity/race, and HIV disease characteristics (years since HIV diagnosis, CD4 cell count, viral load) were measured.
HIV Sexual Transmission Risk Behaviors
Participants were asked a series of questions regarding their sexual practices, following standards from studies of HIV sexual transmission risk behaviors among MSM. Participants were asked about the number of times they had anal intercourse with their sexual partners (i.e., HIV-infected, HIV-uninfected, and unknown HIV status) and the number of times condoms were used or not used. Participants who reported engaging in serodiscordant unprotected insertive or receptive anal intercourse with partners of HIV-negative or unknown status (SDUAI) within the past three months were considered to have engaged in HIV sexual transmission risk behavior.
Monogamy
Participants initially reported their relationship status with one of the following response options: “single/never married,” “in a committed relationship (not married and not living together),” “in a domestic partnership (living with a committed partner),” “married,” “separated,” “divorced,” “widowed,” or “other.” Next, if participants reported currently being in a relationship, they indicated whether this was a monogamous or open relationship. Finally, using aspects of the sexual transmission risk behavior items referenced above, participants reported the number of sexual partners they had in the previous three months.
Condom Use Self-Efficacy
Variables related to social-cognitive theory were taken from prior work modeling HIV sexual transmission risk behaviors in HIV-infected individuals (Safren et al., 2010; Wulfert, Safren, Brown, & Wan, 1999). Accordingly, condom use self-efficacy was measured using 10 items (e.g., How sure are you that you will always use condoms for intercourse in the next 3 months? How sure are you that you will plan to always have a condom available for intercourse in the next 3 months?). Due to different response scales used among these 10 items, individual items were converted to standardized z-scores and a total condom self-efficacy variable was created, with higher scores denoting increased self-efficacy. For the current sample, internal consistency was α = .93.
Disclosure Self-Efficacy
Participants were asked a series of four questions on a 4-point scale (1 = strongly disagree to 4 = strongly agree) which was adapted from the 5-item disclosure Self-Efficacy scale created by Kalichman and Nachimson (1999) (e.g. “Telling my status before having sex,” and “I feel confident telling someone I was dating”). For the current sample, internal consistency was α = .88.
Depression
Depression was measured using responses from the 9-item Depression Severity Scale of the Patient Health Questionnaire (PHQ) (Kroenke, Spitzer, & Williams, 2001), a self-report instrument designed to detect symptoms of depression in primary care settings through diagnostic and symptom severity assessments. Participants were considered to have clinically significant symptoms of depression if they endorsed five or more items affirmatively (i.e., a score of 2, “more than half the days,” or higher on a scale ranging from 0 = “not at all” to 3 = “nearly every day”). Participants with clinically significant symptoms of depression were coded “1” while all remaining participants were coded “0.”
Substance Use
Crystal methamphetamine use over the previous three months was assessed continuously, with response options ranging from 1 = “Never” to 5 = “Every Day.” A dichotomous “any substance abuse” variable was also created, by including items that assessed crack/cocaine, heroin, crystal methamphetamine, opiate, and tranquilizer abuse. Participants who endorsed abuse of any of the above substances were coded “1” while remaining participants were coded “0.”
HIV Sexual Transmission Beliefs
Attitudes and beliefs about HIV sexual transmission risk behaviors were assessed via an HIV Sexual Transmission Beliefs scale (O'Cleirigh et al., 2009). This a 23-item questionnaire in which participants rate their agreement on a Likert scale ranging from 1 = “Agree” to 5 = “Disagree,” with statements concerning their sexual HIV transmission risk appraisals across six subscales. These subscales include Non-disclosure Beliefs (6 items; e.g., “It’s up to the other person to ask about my HIV status”), Sero-sorting Beliefs (3 items; e.g., “I am comfortable having sex with HIV-infected partners”), Viral Load Beliefs (5 items; e.g., “I make decisions about my sexual practices based on my HIV viral load”), Superinfection Beliefs (4 items; “If I have unprotected sex with another HIV-infected person, I can acquire their strain of the virus”), Strategic Positioning (3 items; e.g., “I am less likely to transmit HIV if I am a bottom”), and Condom Beliefs (2 items; e.g., “Condoms will protect me from STDs”). Subscale internal consistency ranged from .53 to .86. The original scoring was undertaken with higher total scores summing to greater disagreement with a practice or belief. To enhance the interpretability of the constructs, particularly when a negative correlation would occur, we reverse coded the items so that higher scores in the factor would denote greater agreement with the construct.
Data Analysis
First, we sought to categorize relationships by examining the degree to which self-reported monogamy corresponded with self-reported number of sexual partners. Second, using the categories identified, we tested relationship status group differences in age, self-efficacy, depression, HIV sexual transmission risk attitudes and beliefs, substance use, and SDUAI via a series of generalized linear models, with Fisher’s LSD post-hoc tests, for continuous dependent variables (relationship status was entered as the independent variable). Generalized linear models have the advantage over traditional analysis of variance in allowing researchers to select the distribution form (e.g., linear, gamma, count, ordinal) of the dependent variables. For binary outcomes variables, logistic regression models were employed, with the relationship status variable entered as the independent variable (“monogamous with one sexual partner” relationship group set as the referent category).
To assess individual covariates of SDUAI (within each relationship status group), variables were entered into multivariate regression models determined by significant bivariate correlations (conducted within each relationship status group). Only variables which were significant at the p < .05 level in the bivariate analyses were included in the subsequent multivariate regression models.
RESULTS
Relationship Categories
Of the participants who reported being in a relationship (N = 200), three relationship groups were revealed (see Fig. 1). Open relationship (n = 115) was defined as those who stated that they were in an open relationship with their primary partner. The “monogamous with one sexual partner” group (n = 53) was defined as participants who reported being in a monogamous relationship with their primary partner and, in accordance with that relationship label, reported one or fewer sexual partners in the previous three months. The “monogamous with more than one sexual partner” participants (n = 23) reported being in a monogamous relationship with their primary partner and, contrary to their relationship label, reported more than one sexual partner in the previous three months. Nine did not report on the number of partners in the past 3 months.
Relationship Group Differences
Results from a series of generalized linear models revealed significant group differences on age, Wald χ2(2) = 12.59, p = .002, crystal methamphetamine use, Wald χ2(2) = 25.35, p < .0001, non-disclosure beliefs, Wald χ2(2) = 24.82, p < .0001, viral load beliefs, Wald χ2(2) = 15.41, p = .001, and sero-sorting beliefs, Wald χ2(2) = 13.34, p = .001 (see Table 2).
Table 2.
Relationship Group Differences on Psychosocial and Behavioral Variables
| Variable | Mean (SD) | Wald χ 2 (df) | p | ||
|---|---|---|---|---|---|
|
Monogamous with one sexual partner |
Monogamous with more than one sexual partner |
Open Relationship |
|||
|
| |||||
| Demographics | |||||
| Age | 42.91 (7.8)a | 37.39 (7.4)b | 43.28 (7.6)a | 12.59 (2) | .002 |
| Self-Efficacy | |||||
| Disclosure self-efficacy | 2.92 (.87) | 2.53 (.76) | 2.7 (.71) | 5.08 (2) | .08 |
| Condom use self-efficacya | .13 (.82) | −.26 (.88) | −.09 (.97) | 4.34 (2) | ns |
| Mental Health/Substance Use | |||||
| Crystal methamphetamine | 1.04 (.19)a | 1.30 (.75)a,b | 1.37 (.74)b | 25.35 (2) | .0001 |
| Depression | 2.13 (2.8) | 1.34 (2.1) | 1.26 (2.1) | 3.96 (2) | ns |
| Transmission Risk Beliefs | |||||
| Sero-sorting Beliefs | 2.31 (.75)a | 2.52 (.74)a,b | 2.76 (.70)b | 13.34 (2) | .001 |
| Non-disclosure Beliefs | 2.11 (.99)a | 3.01 (1.15)b | 3.02 (1.1)b | 24.82 (2) | .0001 |
| Viral load Beliefs | 1.58 (.78)a | 1.94 (.91)a,b | 2.16 (.95)b | 15.41 (2) | .001 |
| Strategic Position Beliefs | 3.20 (.90) | 3.21 (.82) | 3.08 (.90) | .88 (2) | ns |
| Condom Use Beliefs | 4.11 (.95) | 4.26 (.81) | 4.17 (.82) | .48 (2) | ns |
| Superinfection Beliefs | 1.78 (.81) | 1.96 (.85) | 2.04 (.85) | 3.47 (2) | ns |
| Sexual Transmission Risk | |||||
| SDUAI | 2.18 (9.59) | 5.17 (18.6) | 5.58 (16.6) | 2.04 (2) | ns |
Note. Common subscripts denote non-significant group differences.
Mean of 10 z-scored items (accounting for reverse score).
Specifically, the “monogamous with one sexual partner” and open relationship groups were older than the “monogamous with more than one sexual partner” group and the “monogamous with one sexual partner” group reported less frequent crystal methamphetamine use than the open relationship group (neither group differed from the “monogamous with more than one sexual partner” group). Further, the “monogamous with one sexual partner” group reported less agreement with non-contextual beliefs about disclosure compared to the “monogamous with more than one sexual partner” and open relationship groups. They also reported less agreement with non-contextual beliefs about viral load and sero-sorting considerations compared to those in an open relationship (although neither group differed from the “monogamous with more than one sexual partner” group).
The proportion of SDUAI within each relationship group was 21%, 42%, and 52% for the “monogamous with one sexual partner,” “open relationship,” and “monogamous with more than one sexual partner” groups, respectively. Regarding group differences in SDUAI, “monogamous with more than one sexual partner” individuals were nearly three times more likely to engage in this HIV sexual transmission risk behavior compared to the monogamous with one sexual partner group, Odds Ratio = 2.9, p = .05, controlling for the number of sexual partners over the previous three months. Individuals in an open relationship did not significantly differ from the “monogamous with one sexual partner” group, Odds Ratio = 1.2, p = .70 (see Table 3).
Table 3.
Logistic Regressions on Substance Abuse, Depression Diagnosis, and SDUAI by Relationship Group
| Variable | B | Odds Ratio | Wald (df) | SE | p |
|---|---|---|---|---|---|
| Substance abuse | |||||
| Open relationship | .09 | 1.1 | .06 (1) | .36 | ns |
| Monogamous with more than one sexual partner |
1.0 | 3.0 | 3.6 (1) | .58 | .06 |
|
| |||||
| Depression diagnosis | |||||
| Open relationship | −.31 | .73 | .35 (1) | .53 | ns |
| Monogamous with more than one sexual partner |
−.65 | .52 | .60 (1) | .83 | ns |
|
| |||||
| SDUAIa | |||||
| Open relationship | .14 | 1.2 | .15 (1) | .36 | ns |
| Monogamous with more than one sexual partner |
1.1 | 2.9 | 3.6 (1) | .56 | .05 |
Note. The monogamous with one sexual partner group served as the referent category in the above logistic regression analyses.
Controlling for total number of sexual partners over the previous 3 months.
Associations with SDUAI by Group Status
Monogamous with One Sexual Partner
For the models assessing SDUAI in men who reported being monogamous with one sexual partner, five variables were significant at the bivariate level. Positive associations were found between SDUAI and crystal methamphetamine and any substance abuse, indicating that those who had higher levels of SDUAI also had higher levels of crystal methamphetamine and any substance abuse. Positive associations were also found between SDUAI and super-infection, sero-sorting, and strategic positioning beliefs, indicating that greater agreement with these beliefs was associated with higher levels of SDUAI. When running a multivariate model with all significant bivariate predictors, the overall model was significant, F(6, 41) = 5.19, p = .001, R2 = .36, accounting for 36% of the variance in SDUAI. However, only two variables emerged as uniquely significant: crystal methamphetamine use, B = 24.6, SE = 6.7, t(41)= 3.6, p = .001, and serosorting beliefs, B = 4.4, SE = 1.6, t(41)= 2.6, p = .01. These results indicate that a one point increase in crystal methamphetamine use and agreement with serosorting beliefs was associated with an increase of 24.6 and 4.4 in the number of SDUAI acts, respectively (see Table 4).
Table 4.
Multivariate Linear Regressions on SDUAI by Relationship Group
| Variable | B | SE | β | t(df) | p |
|---|---|---|---|---|---|
| Monogamous with one sexual partner | |||||
| Superinfection | 1.59 | 1.48 | .135 | 1.07 (41) | ns |
| Sero-sorting | 4.44 | 1.65 | .345 | 2.69 (41) | .01 |
| Strategic positioning | .05 | 1.29 | .005 | .038 (41) | ns |
| Crystal methamphetmaine |
24.66 | 6.72 | .494 | 3.67 (41) | .001 |
| Substance use dx | −5.41 | 3.82 | −.204 | −1.41 (41) | ns |
|
| |||||
| Open Relationship | |||||
| Superinfection | −.083 | 2.01 | −.004 | −.041 (94) | ns |
| Sero-sorting | 3.43 | 2.52 | .142 | 1.359 (94) | ns |
| Strategic positioning | 2.61 | 1.80 | .139 | 1.448 (94) | ns |
| Crystal methamphetamine |
4.47 | 5.61 | .114 | .797 (94) | ns |
| Substance use dx | 6.84 | 5.25 | .177 | 1.30 (94) | ns |
|
| |||||
| Monogamous with more than one sexual partner | |||||
| Non-disclosure beliefs | 4.96 | 2.23 | .308 | 2.23 (20) | .038 |
| Viral load beliefs | 14.84 | 2.83 | .725 | 5.23 (20) | .0001 |
Monogamous with More than One Sexual Partner
Two variables (non-disclosure beliefs and viral load beliefs) emerged with significant positive bivariate associations with SDUAI among the “monogamous with more than one sexual partner” group. Greater agreement with these beliefs was associated with greater SDUAI. The overall multivariate model was significant, F(2, 20)= 16.1, p < .0001, R2 = .62, accounting for 62% of the variance in SDUAI. In the multivariable model, both variables remained significant as follows: non-disclosure beliefs, B = 4.9, SE = 2.2, t(20)= 2.2, p = .04, and viral load beliefs, B = 14.8, SE = 2.8, t(20)= 5.2, p < .0001. These results indicate that a one point increase in agreement with non-disclosure beliefs and in viral load beliefs was associated with an increase of 4.9 and 14.8 acts of SDUAI, respectively (see Table 4) in this subsample.
Open Relationship
Five variables were significant at the bivariate level, with positive associations revealed between SDUAI and crystal methamphetamine and any substance abuse as well as super-infection, sero-sorting, and strategic positioning beliefs. These variables were then entered into the multivariate regression model to predict SDUAI among MSM in an open relationship, which emerged significantly, F(6, 94) = 3.4, p = .007, R2 = .14, accounting for 14% of the variance in SDUAI. However, none of the variables emerged as uniquely significant when accounting for each other in the multivariate analysis.
DISCUSSION
Three relationship status groups were revealed in a sample of HIV-infected MSM who reported a primary sexual partner: “monogamous with one sexual partner,” “monogamous with more than one sexual partner,” and “open relationships.” The readiness of MSM to describe their primary relationship as monogamous even in the presence of other sexual relationships suggests that they may view the term “monogamous” in a way that is different than it is traditionally used and speaks to the importance of developing and using more accurate and culturally sensitive/specific ways of assessing monogamy for MSM. It may not be sufficient, for example, for research investigations, or in the setting of clinical care, to simply ask, in the context of conducting a sexual risk assessment, if an individual’s relationship is “monogamous” and then infer that this means that they have only one sexual partner (see Parsons et al., 2013).
Gay and bisexual men, who use the term “monogamy” differently than is traditionally defined, may be displaying a vulnerability to a number of possible reporting biases. For example, it is possible that participants viewed monogamy different from the manner in which society typically defines this concept or perhaps social desirability influenced participants responding. Potentially, the effects of variables such as internalized homophobia (e.g., the belief that “gay men are promiscuous”) or HIV stigma (e.g., “people with HIV are a source of infection and should not be having sex with multiple partners”) may also have impacted self-report of monogamy. Our previous work has linked HIV stigma to increased rates of sexual transmission risk behavior among HIV-infected MSM (Hatzenbuehler, O’Cleirigh, Mayer, Mimiaga, & Safren, 2011). The discrepant reports may represent an attempt by participants to protect themselves from internalized negative beliefs about themselves. Finally, it is possible that participants simply did not understand the question regarding their relationship status. For instance, they may have been responding to this item in the context of how their relationship is presented in social circles or the ideal in which they wish to aspire to.
Not only were there nuances in how HIV-infected MSM selected monogamy as a description of their relationship status, but there were also several differences between these groups in psychosocial variables as well as relationships with self-reported HIV sexual transmission risk behaviors. Of note, MSM who were in the category of “monogamous with one sexual partner” reported nearly three times fewer SDUAI acts compared to the “monogamous with more than one sexual partner” group. These men also reported significantly less crystal methamphetamine use compared to those in open relationships. Thus, it appears that MSM who are monogamous and have only one sexual partner are significantly less at risk for SDUAI and psychological risk factors for SDUAI compared to MSM in monogamous relationships where there is more than one sexual partner and open relationships. In fact, these latter two groups did not significantly differ from each other on any of the variables tested in the current study. It seems that operationalizing monogamy based on both relationship identity and number of sexual partners may yield a more accurate understanding of health behaviors among this population. Future research may benefit from routinely considering both these aspects in the context of studying romantic relationships among MSM.
When covariates of HIV sexual transmission risk behavior (i.e., SDUAI) were modeled, different patterns were revealed across groups. For MSM who were in the “monogamous with one sexual partner” category, crystal methamphetamine use and serosorting beliefs were significantly positively associated with transmission risk behavior. The association between agreement with serosorting beliefs and transmission risk behavior in men with only one sexual partner is surprising. If these men are engaging in HIV transmission risk behavior, this means that their one partner is HIV negative or unknown status. There are various potential explanations for this finding, such as mutual decisions about intimacy, potentially sereopositioning (i.e., being the receptive partner), condom use fatigue, or other variables that would need further study in the context of gay male couples.
Conversely, crystal methamphetamine use was not associated with sexual transmission risk behavior for MSM in the “monogamous with more than one sexual partner” or the “open relationship” groups. The only variables that were associated with sexual transmission risk behavior in the “monogamous with more than one sexual partner” group were non-disclosure beliefs and viral load beliefs, in that greater agreement with these beliefs was associated with increased sexual transmission risk behavior. However, it is also important to note that this group was small in number and power to detect significant effects was limited; thus, again, future research is needed.
Overall, the main patterns of results suggest that there are different HIV sexual transmission risk factors for MSM in divergent relationships. Accordingly, secondary HIV prevention interventions with HIV-infected MSM with primary partners may benefit from tailoring content to the accurate type of relationship the individuals are in. For example, based on the results of the current study, MSM who are in a “monogamous with more than one sexual partner” relationship may benefit more from cognitive interventions around HIV sexual transmission risk attitudes and beliefs, given their association with sexual transmission risk behavior in this group.
Despite the additions to the literature, the current study was not without limitations. Data were cross-sectional, thus precluding inferences regarding temporal prediction. Future studies employing prospective designs are needed to properly address the associations of psychosocial and HIV sexual transmission risk behaviors among MSM in various relationships. The sample size of the monogamous groups was also somewhat small and results should be interpreted as preliminary. For instance, the monogamous with more than one sexual partner group consisted of only 23 participants, thus limiting statistical power to detect effects and questionable reliability of the estimates that did emerge significantly. Future research with larger samples will be needed to replicate the findings obtained in the current study.
In sum, the results from the current study revealed three distinct relationship status groups: “monogamous with one sexual partner,” “monogamous with more than one sexual partner,” and “open relationships.” MSM in “monogamous with one sexual partner” relationships report less sexual transmission risk, methamphetamine use, and less agreement with HIV sexual transmission risk attitudes and beliefs compared to MSM in “monogamous with more than one sexual partner” and open relationships. There were also divergent patterns found in covariates of sexual transmission risk between relationship groups, suggesting that couples-based HIV prevention interventions may benefit from a tailored approach depending on the context of individual primary relationships.
Acknowledgments
Data collection for this study was supported by NIMH grant 5R01MH068746-05 and HRSA grant H97HA01293 awarded to Kenneth H. Mayer and Steven A. Safren. Author time was also supported by grant K23MH096647 (Blashill), K24MH094214 (Safren), and the Harvard University Center for AIDS Research, 5P30AI060354 (O’Cleirigh, Blashill, Mayer).
REFERENCES
- Calsyn DA, Campbell AN, Tross S, Hatch-Maillette MA. Is monogamy or committed relationship status a marker for low sexual risk among men in substance abuse treatment? Clinical and methodological considerations. American Journal of Drug and Alcohol Abuse. 2011;37:294–300. doi: 10.3109/00952990.2011.596874. doi:10.3109/00952990.2011.596874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention HIV surveillance--United States, 1981-2008. Morbidity and Mortality Weekly Report. 2011;60:689–693. [PubMed] [Google Scholar]
- Crawford I, Hammack PL, McKirnan DJ, Ostrow DD, Zamboni BD, Robinson BB, Hope BB. Sexual sensation seeking, reduced concern about HIV and sexual risk behaviour among gay men in primary relationships. AIDS Care. 2003;15:513–524. doi: 10.1080/0954012031000134755. doi:10.1080/0954012031000134755. [DOI] [PubMed] [Google Scholar]
- Darbes LA, Chakravarty D, Beougher SC, Neilands TB, Hoff CC. Partner-provided social support influences choice of risk reduction strategies in gay male couples. AIDS and Behavior. 2012;16:159–167. doi: 10.1007/s10461-010-9868-8. doi:10.1007/s10461-010-9868-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergus S, Lewis MA, Darbes LA, Butterfield RM. HIV risk and protection among gay male couples: The role of gay community integration. Health Education & Behavior. 2005;32:151–171. doi: 10.1177/1090198104271964. doi:10.1177/1090198104271964. [DOI] [PubMed] [Google Scholar]
- Fergus S, Lewis MA, Darbes LA, Kral AH. Social support moderates the relationship between gay community integration and sexual risk behavior among gay male couples. Health Education & Behavior. 2009;36:846–859. doi: 10.1177/1090198108319891. doi:10.1177/1090198108319891. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, O'Cleirigh C, Mayer KH, Mimiaga MJ, Safren SA. Prospective associations between HIV-related stigma, transmission risk behaviors, and adverse mental health outcomes in men who have sex with men. Annals of Behavioral Medicine. 2011;42:227–234. doi: 10.1007/s12160-011-9275-z. doi:10.1007/s12160-011-9275-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoff CC, Beougher SC. Sexual agreements among gay male couples. Archives of Sexual Behavior. 2010;39:774–787. doi: 10.1007/s10508-008-9393-2. doi:10.1007/s10508-008-9393-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoff CC, Beougher SC, Chakravarty D, Darbes LA, Neilands TB. Relationship characteristics and motivations behind agreements among gay male couples: Differences by agreement type and couple serostatus. AIDS Care. 2010;22:827–835. doi: 10.1080/09540120903443384. doi:10.1080/09540120903443384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Nachimson D. Self-efficacy and disclosure of HIV-positive serostatus to sex partners. Health Psychology. 1999;18:281–287. doi: 10.1037//0278-6133.18.3.281. doi:10.1037/0278-6133.18.3.281. [DOI] [PubMed] [Google Scholar]
- Kim JH, Riolo RL, Koopman JS. HIV transmission by stage of infection and pattern of sexual partnerships. Epidemiology. 2010;21:676–684. doi: 10.1097/EDE.0b013e3181e6639f. doi:10.1097/EDE.0b013e3181e6639f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. doi:10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaSala MC. Extradyadic sex and gay male couples: Comparing monogamous and non- monogamous relationships. Families in Society. 2004;85:405–412. [Google Scholar]
- Lightfoot M, Song J, Rotheram-Borus M, Newman P. The influence of partner type and risk status on the sexual behavior of young men who have sex with men living with HIV/AIDS. Journal of Acquired Immune Deficiency Syndromes. 2005;38:61–68. doi: 10.1097/00126334-200501010-00012. doi:10.1097/00126334-200501010-00012. [DOI] [PubMed] [Google Scholar]
- Mayer K, Appelbaum J, Rogers T, Lo W, Bradford J, Boswell S. The evolution of the Fenway Community Health Model. American Journal of Public Health. 2001;91:892–894. doi: 10.2105/ajph.91.6.892. doi:10.2105/AJPH.91.6.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell J, Harvey S, Champeau D, Moskowitz D, Seal D. Relationship factors associated with gay male couples’ concordance on aspects of their sexual agreements: Establishment, type, and adherence. AIDS and Behavior. 2011;16:1560–1569. doi: 10.1007/s10461-011-0064-2. doi:10.1007/s10461-011-0064-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JW, Harvey S, Champeau D, Seal DW. Relationship factors associated with HIV risk among a sample of gay male couples. AIDS and Behavior. 2012;16:404–411. doi: 10.1007/s10461-011-9976-0. doi:10.1007/s10461-011-9976-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris SR, Little SJ. MSM: resurgent epidemics. Current Opinion on HIV and AIDS. 2011;6:326–332. doi: 10.1097/COH.0b013e3283476c29. doi:10.1097/COH.0b013e3283476c29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Cleirigh C, Newcomb M, Mayer K, Skeer M, Safren S. Moderate levels of depression predict sexual risk in HIV-infected MSM: A longitudinal analysis of data from six sites involved in a “Prevention for Positives” study. AIDS and Behavior. doi: 10.1007/s10461-013-0462-8. (in press) doi: 10.1007/s10461-013-0462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Cleirigh C, Mayer K, Covahey C, Leidolf E, Safren S. Safer sex attitudes as functional targets for HIV prevention interventions?; Oral presentation at the National HIV Prevention Conference; Atlanta, GA. Aug, 2009. [Google Scholar]
- Parsons JT, Starks TJ, DuBois S, Grov C, Golub SA. Alternatives to monogamy among gay male couples in a community survey: Implications for mental health and sexual risk. Archives of Sexual Behavior. 2013;42:303–312. doi: 10.1007/s10508-011-9885-3. doi:10.1007/s10508-011-9885-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, Hall HI. Estimated HIV incidence in the United States, 2006–2009. PLoS ONE. 2011;6:e17502. doi: 10.1371/journal.pone.0017502. doi:10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, O’Cleirigh C, Skeer MR, Driskell J, Goshe BM, Covahey C, Mayer KH. Demonstration and evaluation of a peer-delivered, individually-tailored, HIV prevention intervention for HIV-infected MSM in their primary care setting. AIDS and Behavior. 2011;15:949–958. doi: 10.1007/s10461-010-9807-8. doi:10.1007/s10461-010-9807-8. [DOI] [PubMed] [Google Scholar]
- Safren SA, O'Cleirigh CM, Skeer M, Elsesser SA, Mayer KH. Project enhance: A randomized controlled trial of an individualized HIV prevention intervention for HIV-infected men who have sex with men conducted in a primary care setting. Health Psychology. 2013;32:171–179. doi: 10.1037/a0028581. doi:10.1037/a0028581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, Traeger L, Skeer M, O’Cleirigh C, Meade CS, Covahey C, Mayer KH. Testing a social-cognitive model of HIV transmission risk behaviors in HIV-infected MSM with and without depression. Health Psychology. 2010;29:215–221. doi: 10.1037/a0017859. doi:10.1037/a0017859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23:1153–1162. doi: 10.1097/QAD.0b013e32832baa34. doi:10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- Wagner GJ, Remien RH, Carballo-Diéguez A. Prevalence of extradyadic sex in male couples of mixed HIV status and its relationship to psychological distress and relationship quality. Journal of Homosexuality. 2000;39:31–46. doi: 10.1300/J082v39n02_02. doi:10.1300/J082v39n02_02. [DOI] [PubMed] [Google Scholar]
- Wheldon CW, Pathak EB. Masculinity and relationship agreements among male same-sex couples. Journal of Sex Research. 2010;47:460–470. doi: 10.1080/00224490903100587. doi:10.1080/00224490903100587. [DOI] [PubMed] [Google Scholar]
- Wulfert E, Safren SA, Brown I, Wan CK. Cognitive, behavioral, and personality correlates of HIV-positive persons’; unsafe sexual behavior. Journal of Applied Social Psychology. 1999;29:223–244. [Google Scholar]