Abstract
Importance
Functional recovery is an important outcome following injury. Functional impairment is persistent in the year following injury for older trauma patients.
Objective
To measure the impact of routine geriatric consultation on functional outcomes in older trauma patients.
Design
Pretest-posttest study. The pretest control group (n=37) was retrospectively-identified (December 2006-November 2007). The posttest geriatric consultation (GC) group (n=85) was prospectively enrolled (December 2007-June 2010). We then followed both groups for 1 year after enrollment.
Setting
Academic Level-1 trauma center
Participants
Adults ≥ 65 years of age admitted as an activated code trauma
Intervention
Routine geriatric consultation
Main Outcome Measure
The Short Functional Status (SFS) survey of five Activities of Daily Living (ADLs) on admission and 3, 6, and 12 months post-injury.
Results
The unadjusted SFS (GC group only) declined from 4.6 pre-injury to 3.7 at 12 months post-injury, a decline of nearly one full ADL (p<.05). The ability to shop for personal items was the specific ADL more commonly retained by the GC compared to the control group. The GC group had a better recovery of function in the year following injury than the GC group controlling for age, gender, ethnicity, length of stay, co-morbidity, injury severity, post-discharge rehabilitation, complication, and whether surgery was performed (p<.01), a difference of 0.67 ADL abilities retained by the GC compared to the control group (95% CI 0.06–1.4).
Conclusions and Relevance
Functional recovery for older adults following injury may be improved by geriatric consultation. Early introduction of multidisciplinary care in geriatric trauma patients warrants further investigation.
Introduction
Due to a rapidly growing and active older population, adults aged 65 years or older will comprise 40% of all trauma patients by 2050.1,2 Traumatic injury is a sentinel life event that can precipitate a trajectory of functional decline in older patients.3,4 In comparison to younger patients, older trauma patients suffer greater morbidity and mortality5–11, and their prolonged and complicated hospital course results in poorer recovery of functional abilities.12–15
Functional recovery after traumatic injury is a meaningful outcome, particularly in the elderly population. While a few studies of long-term recovery after traumatic injury16–22 have defined as a general return to independent living, specific measures of Activities of Daily Living (ADLs) such as toileting and bathing23 are understudied. Moreover, understanding an older trauma survivor’s ADL difficulties can directly inform caregiving needs, treatment decisions such as life support and cardiopulmonary resuscitation, and health care costs both during and after hospitalization.24–26 In a retrospective study of older trauma patients, we previously used the Short Functional Status (SFS) survey,27 a five-point ADL scale, to document a persistent 1-ADL decline at 12 months post-injury.28
Little is known about preventability of post-traumatic functional decline in older trauma patients. Geriatric consultation, which addresses inpatient issues such as delirium and immobility, has improved outcomes of hip fracture patients29,30 but has not been studied in older patients with other types of injuries. We implemented a routine geriatric consultation for all elderly trauma patients and prospectively compared pre-injury with 1-year post injury functional status to measure functional recovery.
Methods
Setting and subjects
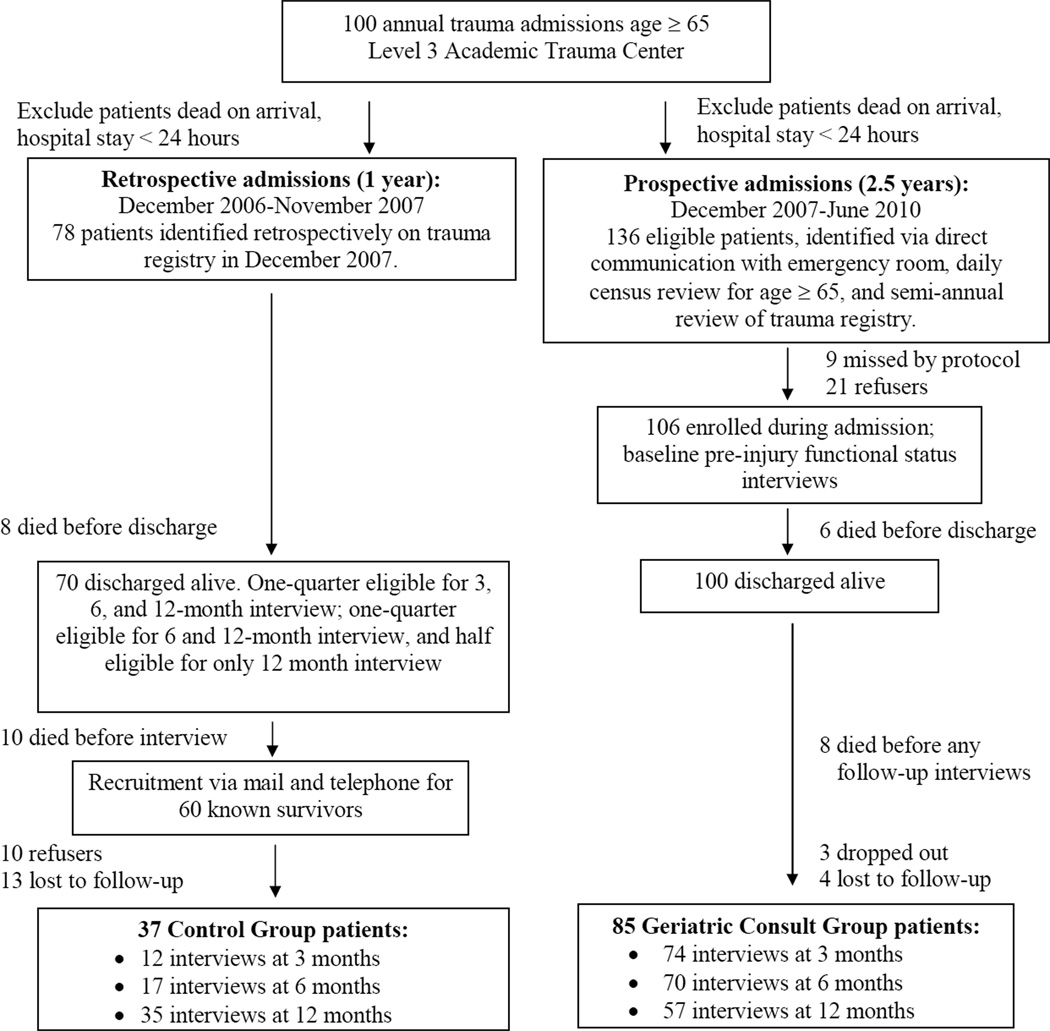
This study was approved by the UCLA Office of Protection of Human Subjects. The Geriatric Consult (GC) group consisted of all adults aged≥ 65 years that triggered trauma activation and were admitted to our academic tertiary care Level 1 trauma center between December 2007 and June 2010 (Figure 1). Patients who died, were discharged, or were transferred within 24 hours were excluded. As a comparison group, we used previously-published data from 37 trauma patients of similar age and length of stay admitted in 2006.33 We completed follow-up data collection in June, 2011 (Fig 1).
Figure 1.
Data Flow, Retrospective Control Group versus Prospective Geriatric Consult Group
In a clinical partnership between trauma surgery and geriatric medicine, we aimed to request a formal geriatric consultation for all trauma patients age 65 and older in the GC group. The hospital geriatric consultation service consists of geriatric faculty and a rotating geriatric medicine fellow, with a typical practice of daily visits until resolution of geriatric medical and disposition issues. The goal of our usual consultation is to identify risks early in the hospital course, including: pre-existing cognitive and functional impairment, early detection of delirium, medication review for harm, review of advanced directives and care preferences, and psychosocial history to identify issues that might complicate safe and timely discharge. We provided guidance to reduce risks identified, as well as care for general medical issues if requested by the primary team. The control group received our medical center’s usual care, which included the option of requesting a general medical or geriatric consultation. We analyzed our results according to intention-to-treat, even if patients crossed over their original group assignments, a method that allows for generalizable results than per-protocol designs.
Measures of functional outcome
We measured functional status using the SFS, a community-based screen for sentinel functional impairment.27 The SFS measures ability to perform five ADLs independently, without help from another person: shopping (e.g., obtaining personal items from a store), bathing, walking across the room, light housework and managing finances. Higher SFS indicates greater independence. The SFS can be completed in less than 4 minutes via personal or telephone interview by non-clinical administrative personnel31 and was validated as a measure of functional change in uninjured community-dwelling elders,32 where the mean decline in SFS was zero over 9–14 months. A decline of 1 point is considered to be clinically significant.32
For the GC group, we first administered the SFS in-person upon admission (reflecting pre-injury function), and at 3, 6, and 12 months after the injury by telephone interview. We defined change in function as follow-up minus pre-injury SFS, with higher (less negative) value indicating better recovery of baseline function.
In addition, we asked both control and GC patients to compare their current to pre-injury function using a 5-point ordinal rating of their self-rated degree of global recovery: 0% or none, 25% or somewhat, 50% or partial, 75% or almost full, and 100% or full. We used the global recovery question, as well as age, gender, ethnicity, co-morbidity, marital status, and pre-injury living situation to model the GC group’s pre-injury score, then applied the model to the control group to predict each control patients’ most likely baseline SFS score.
We obtained co-variables (age, gender, ethnicity, co-morbidity, Injury Severity Score [ISS]33, discharge to nursing or other facility for physical rehabilitation, any surgical procedure, and hospital complication) from the institutional trauma registry. Hospital complications were pre-specified according to the Trauma Quality Improvement Program.34
Statistical Analysis
To quantify functional recovery for the GC group only, we compared SFS scores at 3, 6, and 12 months to pre-injury scores using unadjusted paired two-tailed t-tests. We used correlation (r) in the GC group only to internally-validate the new self-reported global assessment of recovery item against the change in SFS. We compared the other clinical characteristics using chi-squared and one-way analysis of variance.
Our primary outcome measure of functional recovery was change in SFS score (follow-up minus baseline, with a higher [less negative] value indicating better recovery of pre-injury function) at 3, 6, and 12-month time point as three separate models. We controlled for gender, ethnicity, living situation, age, ISS, co-morbidity, length of stay, nursing home or rehabilitation center discharge, any surgical procedure, any complication, and the baseline ADL score. Last, we performed a longitudinal analysis using multilevel random effects regression, which allows for testing for differences in recovery at all three follow-up time points as well as whether functional recovery differs in their slopes across time.
To analyze secondary functional outcomes, we used logistic regression to predict each of the 5 ADL impairments and ordinal logistic regression to predict better self-rated global recovery. All secondary outcome models used the same co-variables as the main analysis. We performed all analyses using STATA 12.0 (College Station, TX). A p-value <0.05 was considered significant.
Results
Of 136 patients eligible for the GC group (Figure 1), we enrolled 106 (78%) patients to participate in this functional outcomes study. Of these, 85 (80%) survived and participated in at least one follow-up telephone interview (n=74, 70, 57 at 3, 6, and 12 months). Patients who refused enrollment were more likely to be of non-white ethnicity than those who enrolled (33% versus 14%, p<0.04) but were otherwise similar with respect to age, gender, co-morbidity, and ISS (p>0.7). Patients lost to follow-up had a higher mean ISS (18 vs 13, p<.03), but were otherwise similar in age, ethnicity, co-morbidity and gender (p>.2). We provided geriatric consultation for 59 of the enrolled GC group patients (69%), compared to 6 (17%) in the control group. GC group patients without a geriatric consultation were short-stay patients with less-severe injury than GC patients with consult (mean length of stay 6 versus 12, p<.05; mean ISS 9 vs 15, p<.01) , most with a planned uncomplicated discharge before a consult could be requested. Combining the GC with the control group interviews, we collected 488 total observations for 122 patients for statistical analysis. We compared GC to control group characteristics (Table 1). The GC group was more likely to be male, but the groups were otherwise similar.
Table 1.
Comparison of Group Characteristics
| Geriatric Consult Group (n=85) |
Control Group (n=37) |
P value* | |
|---|---|---|---|
| Age | 78 (±8.0) | 77 (±7.8) | .56 |
| Gender (male) | 65% | 46% | .053 |
| Co-morbidity (Charlson Comorbidity Index Score52) |
4.6 (±2.3) | 4.1 (±1.4) | .18 |
| Injury Severity Score | 13 (±9.3) | 12 (±7.6) | .42 |
| White race | 86% | 86% | .93 |
| Living alone | 18% | 16% | .73 |
| Living with spouse | 26% | 32% | .46 |
| Any complication | 26% | 22% | .38 |
| Any surgery | 41% | 30% | .23 |
| Length of stay | 10.5 | 7.1 | .17 |
| Discharge to rehabilitation at a nursing home or other facility |
37% | 30% | .48 |
Unadjusted t-tests for continuous variables (age, co-morbidity, Injury Severity Score) and Chi-squared tests for dichotomous variables (gender, race, living alone, living with spouse, any complication, any surgery). Table 2 Mean Short Functional Status (SFS) Survey Scores Pre- and Post-Injury
Comparing Functional Status Outcomes between GC and Control Groups
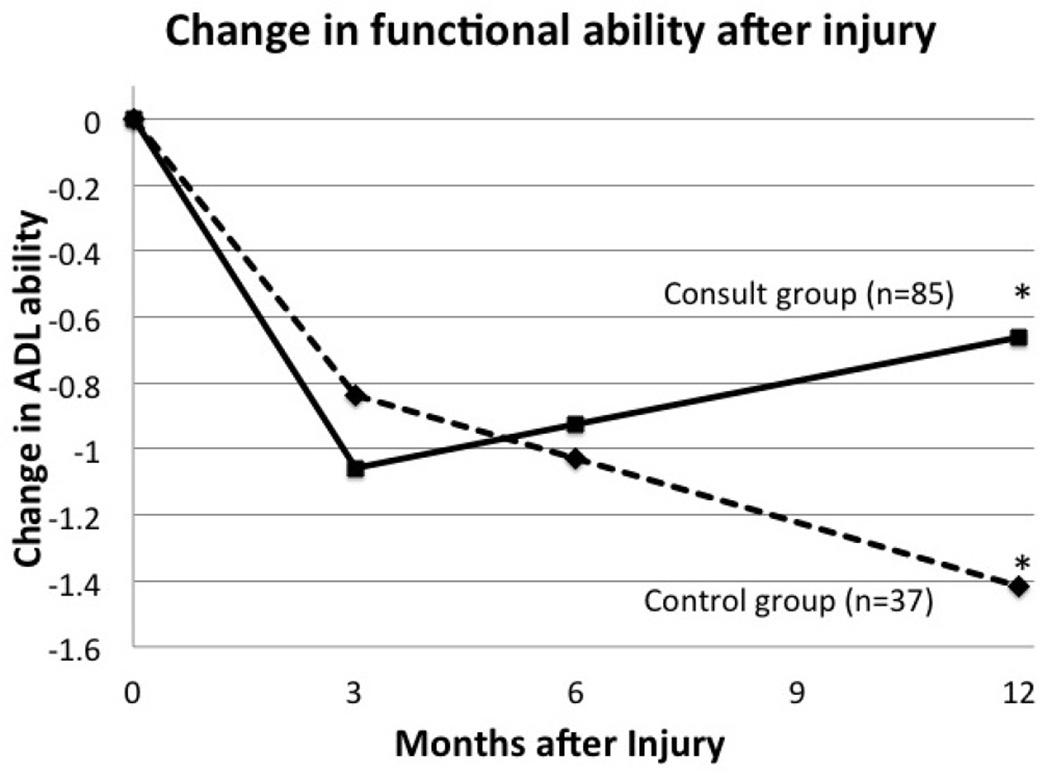
The GC group reported having 0.79 ADL fewer abilities by 1 year compared to preinjury baseline (SD 1.48, range of 5 fewer to 2 greater ADLs) on the SFS score, compared to 1.36 ADLs fewer (SD 1.34, range of 5 fewer to 1 greater ADL) for the control group, a difference that was not statistically significant on unadjusted analysis (p<0.08, Table 2). In the multivariable model predicting ADL decline, (Table 3) there were no differences between the groups at 3 and 6 months, but by 12 months, the GC group had more recovery of 0.67 ADLs more compared to the control (p<0.03). In the hierarchical linear model using all 488 observations for 122 patients and independent trajectories between the GC and control group over time, both groups had downsloping trajectories over time, but the GC had less decline (difference in slope of 0.11 fewer ADLs below baseline per month, p<0.01) than the control group (Figure 2). In this final model, we found that the GC group had recovered more of their function ([0.76 ADLs [95% CI 1.0,.4] below baseline) than the control group (1.4 ADLs [95% CI 1.8, 1.1) below baseline) by the 12-month follow-up.
Table 2.
Mean Short Functional Status (SFS) Survey Scores Pre- and Post-Injury
| Geriatric Consult (GC) group (n=85) |
Control Group (n=37) | Unadjusted Difference in Decline §§ |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Post- injury time-point |
Sample (N) |
Pre- injury |
Post- injury |
Sample (N) |
Pre- injury§ |
Post- injury |
Estimate | 95% CI | |
| 3 months | 74 | 4.7 | 3.5 | 12 | 4.8 | 3.7 | .12 | −.92 | 1.2 |
| 6 months | 70 | 4.7 | 4.0 | 17 | 4.7 | 3.8 | −.26 | −.98 | .46 |
| 12 months | 57 | 4.6 | 3.9 | 35 | 4.7 | 3.3 | −.57 | −1.2 | 0.5 |
Baseline ADL count for control group was predicted using age, gender, ethnicity, co-morbidity, marital status, pre-injury living situation, and self-reported degree of recovery (using poisson regression of ADL count).
Interpretation of the difference between GC decline (follow-up minus pre-injury SFS) and control group decline (follow up minus pre-injury SFS): a negative result indicates that the GC group outcome had less decline, expressed in units of count of ADL abilities.
Table 3.
Change in function at 12 months compared to pre-injury baseline
| Beta Coefficient* |
Lower 95% CI |
Upper 95% CI |
|
|---|---|---|---|
|
CG versus control group |
0.67 | 0.10 | 1.22 |
| Age (in years) | −0.02 | −0.06 | 0.03 |
| Male versus female | 0.53 | −0.03 | 1.09 |
| Co-morbidity (Charlson Comorbidity Index Score52, points ranging from 2 to 12) |
−0.03 | −0.19 | 0.13 |
| ISS (range 1–41 points) | 0.02 | −0.03 | 0.06 |
| Length of Stay (in days, ranging from 1 to 61) |
−0.08 | −0.12 | −0.04 |
| Any surgery versus no surgery |
0.49 | −0.22 | 1.20 |
| Any complication versus no complication |
0.51 | −0.31 | 1.32 |
| White versus non-white | 0.88 | 0.07 | 1.70 |
| Pre-injury ADL count (Range 0 to 5 ADL abilities, where higher= better baseline function) |
−0.47 | −0.89 | −0.05 |
| Discharge to post-acute rehabilitation |
.05 | −.69 | .80 |
GC=geriatric consult; ISS=injury severity score; ADL=activity of daily living
The effect of each variable is expressed as a change in count of ADL abilities at 1 year compared to baseline. A positive effect (whose 95% confidence intervals do not cross zero) indicates that each increase in the variable is associated with functional recovery; a negative effect indicates association with decline.
Figure 2.
* Bootstrapped 95% confidence intervals around the 12-month mean ADL-count change from baseline for consult group (−.35, −1) versus control group (−1.05, −1.8) were non-overlapping.
There were 122 unique patients in the model, who were observed at 3 months (n=86), 6 months (n=87), and 12 months (n=92).
Among the clinical co-variables tested, the sole predictors of functional outcome in the final hierarchical model were longer hospitalization (β=.08 fewer ADLs recovered per additional hospital day, p<.001) and white ethnicity (β=0.9 more ADLs compared to non-white, p<0.03) (Table 3).
Secondary outcomes (specific ADLs and 5-item global recovery)
Of the 5 specific ADLs recovery, the most common new impairment after injury was shopping disability for both groups at all time points. GC patients were also more likely than the control group to regain shopping ability at 3 and 12 months (Table 4). The 5-item global recovery item was well-correlated with change in SFS score (r=0.39, 0.32, and 0.43 at 3, 6, and 12 months, p<.05 for all time points). The most common self-perceived global recovery rating for both groups at month 3 and 6 was “recovery of 75%” and “fully recovered” at 12 months, with no difference between the GC and control group at any time point for unadjusted and multivariable analyses.
Table 4.
Specific functional impairments at baseline and 12 months
| Prevalence at baseline |
Prevalence at 12 months | Adjusted Relative Risk Ratio (aRRR) of Impairment at 12 months associated with CG versus Control * |
||||
|---|---|---|---|---|---|---|
| Geriatric Consult (GC) |
Geriatric Consult (GC) |
Control | aRRR | 95%CI | ||
| Finances | 11% | 19% | 26% | .67 | .6 | 1.0 |
| Shopping | 9% | 39% | 89% | .40 | .36 | .45 |
| Housework | 6% | 29% | 23% | .67 | .58 | .99 |
| Walking | 5% | 14% | 11% | 1.16 | 1.05 | 1.18 |
| Bathing | 3% | 19% | 14% | 1.55 | 1.00 | 1.68 |
Adjusted for age, gender, co-morbidity, race, complication, surgery, discharge to post-acute rehabilitation. An aRRR < 1 indicates that the GC group had less impairment, whereas an aRRR > 1 indicates that the GC group had more impairment.
Discussion
Compared to their younger counterparts, older adults require substantial healthcare resources after traumatic injury.5–8 Long-term data measuring meaninful recovery in geriatric populations following an acute hospitalization after traumatic injury is lacking. In this study, we demonstrated that a routine geriatric medicine consultation can feasibly be added to the hospital care of older patients admitted for acute injury without affecting hospital course. Consistent with our prior retrospectively-identified cohort,28 we also found a substantial decline in functional status among our new cohort of GC group patients enrolled after implementation of a routine geriatric consultation However, these patients exibited a lesser degree of ADL decline when compared to patients in the pre-implementation control group. Furthermore, after discharge, injured elders in the GC group exhibited fewer total ADL dependencies, mostly in the area of shopping for personal items.
Measurement of functional trajectory for older adults is increasingly recognized as an important benchmark in geriatric surgical care.35 In the present study, the GC group had few functional impairments prior to injury (mean SFS score of 4.7), consistent with prior studies of SFS in the general geriatric population.27,32 These results suggest that the injured elders examined in this study were in good health prior to injury. The mean 0.6 ADL decrement that our GC group sustained after the injury and up to 1-year after the injury is substantial. Longitudinal community-dwelling elders report no decline in ADLs over time.32 Any measureable ADL impairment predicts substantial increased risk (∼30% absolute risk increase) of further functional decline and death in an injured community-dwelling individual.36,37 These findings imply that injured elders are at a particularly increased risk of detrimental post-injury decline.
When analyzing specific functional activities, the ability to shop independently was the most notable post-injury functional decrement in our study. Shopping for personal items requires physical and cognitive reserve to obtain goods outside of the home, differing from the other ADLs in the SFS that are performed in the home. Of the five SFS items, shopping is also considered to be the most difficult functional status activity when arranged on a hierarchical scale.38 With respect to shopping disability, our cohort of geriatric trauma patients was healthier prior to injury than the average Medicare patient (15.6% need help with shopping39), but much worse after injury. These results underscore the loss of independence and functional decline continuing in the year following injury for the injured elderly patient.
Our study of a health care intervention targeted to older trauma patients joins a handful of similar studies. Demetriades et al. demonstrated better survival in 76 older patients admitted after implementation of a system-wide policy of early trauma activation for patients age > 70, compared to 260 older patients admitted prior to the new policy.40 Fallon and colleagues used multidisciplinary geriatric team consultation to study hospital care in an uncontrolled study of older trauma patients. The team was more likely to provide consultation to patients who survived the hospitalization and provided geriatric care such as pain management and delirium evaluation.41 Further studies of targeted geriatric services with concurrent controls aimed at improving immediate and long-term outcomes are needed. Functional status outcomes has also been proposed as a target for future comparison of hospital quality of care that identifies different high and low-performing medical centers rather than survival outcomes.42
To date, studies of routine inpatient geriatric consultation alone for older patients undergoing non-trauma surgery show minimal or no improvement of long-term functional status.43,44 However, geriatrics involvement in combination with post-acute care such as geriatric rehabilitation, does improve long term functional outcomes, particularly in patients with hip fracture repair.29,45 One multi-component inpatient consultation intervention prevented delirium30 in hip fracture patients. Because delirium itself is cause of prolonged functional impairment in older surgery patients,46,47 future geriatric consultation studies that include early delirium detection for trauma and non-trauma surgery patients are much needed.
Although our new GC cohort had better functional recovery than our retrospective cohort, it is likely too early to directly attribute the improvement to our routine geriatric consultation intervention. Our geriatric consultation was a complex intervention including comprehensive evaluation and recommended care tailored to the needs of the individual patient. A more detailed secondary data analysis of specific care provided by the geriatricians in collaboration with the primary surgery team is under way. However, this study was not powered to study whether specific consultative services were linked to improved long-term function. Similarly, although only the shopping ability ADL reached statistical significance, this study was not powered to isolate ADLs responsive to geriatric consultation. Future research to improve post-injury geriatric health will likely require a stronger intervention on the most effective types of care. A larger study will be needed to answer questions about specific care processes and differences in ADL recovery.
Our results are also limited by the temporal nature of our study. First, as in any pre-post study, secular time trends could may some of the differences observed. During GC group enrollment, economic downturn occurred, which is associated with less traumatic injury.21 It is possible that fewer or less-severe trauma injury was the underlying reason we found less functional decline, however, the similar ISS for both groups would suggest otherwise. Second, because our control group was retrospectively-identified, we expect greater survivor-bias and poorer retention than the prospective group. However, we would expect that this bias would result in a healthier control group with less functional decline, which we expect would have lessened the effect of our quality improvement intervention.
As one-third of older persons experience functional decline following acute hospitalization,48 identification of elders most at risk will be paramount for targeting future interventions35,49,50. We identified prolonged hospital stay, a marker of more severe injury and complicated hospital course, as a potential future target for increased efforts to improve long-term function. Other studies among older hospital patients have identified other patient-level variables that might also predict functional outcomes: pre-injury cognitive and mobility impairment, malnutrition, and nursing home status.50,51 Future refinement of geriatric consultation for acute injury should consider targeting for the most high-risk patients.
In summary, we present evidence suggesting that geriatric-specific interventions in the acute setting may contribute to improved functional recovery after traumatic injury in the elderly. In order to achieve substantial and lasting functionality in this vulnerable population, it will be critical to identify effective hospital services targeted to the clinical and rehabilitative needs of older injured patients during complex and prolonged hospitalizations.
Acknowledgements
Lillian Min and Areti Tillou had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. There are no relevant conflicts of interest. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. We would like to acknowledge the technical assistance of Asmik Tantoushan and Chiao-Li Chan.
Dr. Tillou was supported by an American Geriatrics Society Jahnigen Award (2009–11). Drs. Tillou and Min were supported by the (NIA) K12 UCLA Mentored Clinical Scientist Development Program in Geriatrics. Dr. Min is supported by a Research Career Development Core grant from the University of Michigan Pepper Center (NIA).
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Interim results of this research were presented at the Annual Scientific Meeting, Association for the Surgery of Trauma, Boston, MA, September 2010 and full results will be presented at the American Geriatrics Society Annual Scientific Meeting on May 3, 2013.
There are no relevant conflicts of interest.
References
- 1.Rzepka SG, Malangoni MA, Rimm AA. Geriatric trauma hospitalization in the United States: a population-based study. J Clin Epidemiol. 2001;54(6):627–633. doi: 10.1016/s0895-4356(00)00337-1. [DOI] [PubMed] [Google Scholar]
- 2.Campbell PR. Population projections for states by age, sex, race, and Hispanic origin: 1995 to 2025. Population Projections Branch, Population Division, US Bureau of the Census; 1996. [Google Scholar]
- 3.Givens JL, Sanft TB, Marcantonio ER. Functional recovery after hip fracture: the combined effects of depressive symptoms, cognitive impairment, and delirium. J Am Geriatr Soc. 2008;56(6):1075–1079. doi: 10.1111/j.1532-5415.2008.01711.x. [DOI] [PubMed] [Google Scholar]
- 4.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet. 1999;353(9147):93–97. doi: 10.1016/S0140-6736(98)06119-4. [DOI] [PubMed] [Google Scholar]
- 5.Taylor MD, Tracy JK, Meyer W, Pasquale M, Napolitano LM. Trauma in the elderly: intensive care unit resource use and outcome. J Trauma. 2002;53(3):407–414. doi: 10.1097/00005373-200209000-00001. [DOI] [PubMed] [Google Scholar]
- 6.McKevitt EC, Calvert E, Ng A, et al. Geriatric trauma: resource use and patient outcomes. Can J Surg. 2003;46(3):211–215. [PMC free article] [PubMed] [Google Scholar]
- 7.Shabot MM, Johnson CL. Outcome from critical care in the "oldest old" trauma patients. J Trauma. 1995;39(2):254–259. doi: 10.1097/00005373-199508000-00011. discussion 259–260. [DOI] [PubMed] [Google Scholar]
- 8.vanderSluis CK, Klasen HJ, Eisma WH, tenDuis HJ. Major trauma in young and old: What is the difference? Journal of Trauma-Injury Infection and Critical Care. 1996;40(1):78–82. doi: 10.1097/00005373-199601000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Perdue PW, Watts DD, Kaufmann CR, Trask AL. Differences in mortality between elderly and younger adult trauma patients: geriatric status increases risk of delayed death. J Trauma. 1998;45(4):805–810. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- 10.Knudson MM, Lieberman J, Morris JA, Jr., Cushing BM, Stubbs HA. Mortality factors in geriatric blunt trauma patients. Arch Surg. 1994;129(4):448–453. doi: 10.1001/archsurg.1994.01420280126017. [DOI] [PubMed] [Google Scholar]
- 11.McGwin G, Jr., MacLennan PA, Fife JB, Davis GG, Rue LW., 3rd. Preexisting conditions and mortality in older trauma patients. J Trauma. 2004;56(6):1291–1296. doi: 10.1097/01.ta.0000089354.02065.d0. [DOI] [PubMed] [Google Scholar]
- 12.DeMaria EJ, Merriam MA, Casanova LA, Gann DS, Kenney PR. Do DRG payments adequately reimburse the costs of trauma care in geriatric patients? J Trauma. 1988;28(8):1244–1249. doi: 10.1097/00005373-198808000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Schwab CW, Kauder DR. Trauma in the geriatric patient. Arch Surg. 1992;127(6):701–706. doi: 10.1001/archsurg.1992.01420060077011. [DOI] [PubMed] [Google Scholar]
- 14.Ross N, Timberlake GA, Rubino LJ, Kerstein MD. High cost of trauma care in the elderly. South Med J. 1989;82(7):857–859. doi: 10.1097/00007611-198907000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Covington DL, Maxwell JG, Clancy TV. Hospital resources used to treat the injured elderly at North Carolina trauma centers. J Am Geriatr Soc. 1993;41(8):847–852. doi: 10.1111/j.1532-5415.1993.tb06182.x. [DOI] [PubMed] [Google Scholar]
- 16.van Aalst JA, Morris JA, Jr., Yates HK, Miller RS, Bass SM. Severely injured geriatric patients return to independent living: a study of factors influencing function and independence. J Trauma. 1991;31(8):1096–1101. discussion 1101–1092. [PubMed] [Google Scholar]
- 17.Glance LG, Osler TM, Dick A, Mukamel D. The relation between trauma center outcome and volume in the National Trauma Databank. J Trauma. 2004;56(3):682–690. doi: 10.1097/01.ta.0000053469.92142.40. [DOI] [PubMed] [Google Scholar]
- 18.Oreskovich MR, Howard JD, Copass MK, Carrico CJ. Geriatric trauma: injury patterns and outcome. J Trauma. 1984;24(7):565–572. [PubMed] [Google Scholar]
- 19.Livingston DH, Lavery RF, Mosenthal AC, et al. Recovery at one year following isolated traumatic brain injury: a Western Trauma Association prospective multicenter trial. J Trauma. 2005;59(6):1298–1304. doi: 10.1097/01.ta.0000196002.03681.18. discussion 1304. [DOI] [PubMed] [Google Scholar]
- 20.Mosenthal AC, Livingston DH, Lavery RF, et al. The effect of age on functional outcome in mild traumatic brain injury: 6-month report of a prospective multicenter trial. J Trauma. 2004;56(5):1042–1048. doi: 10.1097/01.ta.0000127767.83267.33. [DOI] [PubMed] [Google Scholar]
- 21.Ruhm CJ. Commentary: mortality increases during economic upturns. International journal of epidemiology. 2005;34(6):1206–1211. doi: 10.1093/ije/dyi143. [DOI] [PubMed] [Google Scholar]
- 22.Jacobs DG, Plaisier BR, Barie PS, et al. Practice management guidelines for geriatric trauma: the EAST Practice Management Guidelines Work Group. J Trauma. 2003;54(2):391–416. doi: 10.1097/01.TA.0000042015.54022.BE. [DOI] [PubMed] [Google Scholar]
- 23.McGwin G, Jr., Melton SM, May AK, Rue LW. Long-term survival in the elderly after trauma. J Trauma. 2000;49(3):470–476. doi: 10.1097/00005373-200009000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Gillick MR. Rethinking the role of tube feeding in patients with advanced dementia. N Engl J Med. 2000;342(3):206–210. doi: 10.1056/NEJM200001203420312. [DOI] [PubMed] [Google Scholar]
- 25.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346(14):1061–1066. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 26.Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE. Functional status of elderly adults before and after initiation of dialysis. New England Journal of Medicine. 2009;361(16):1539–1547. doi: 10.1056/NEJMoa0904655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saliba D, Orlando M, Wenger NS, Hays RD, Rubenstein LZ. Identifying a short functional disability screen for older persons. J Gerontol A Biol Sci Med Sci. 2000;55(12):M750–756. doi: 10.1093/gerona/55.12.m750. [DOI] [PubMed] [Google Scholar]
- 28.Kelley-Quon L, Min L, Morley E, Hiatt JR, Cryer H, Tillou A. Functional status after injury: a longitudinal study of geriatric trauma. Am Surg. 2010;76(10):1055–1058. [PMC free article] [PubMed] [Google Scholar]
- 29.Kennie DC, Reid J, Richardson IR, Kiamari AA, Kelt C. Effectiveness of geriatric rehabilitative care after fractures of the proximal femur in elderly women: a randomised clinical trial. Bmj. 1988;297(6656):1083–1086. doi: 10.1136/bmj.297.6656.1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516–522. doi: 10.1046/j.1532-5415.2001.49108.x. [DOI] [PubMed] [Google Scholar]
- 31.Saliba D, Elliott M, Rubenstein LZ, et al. The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community. J Am Geriatr Soc. 2001;49(12):1691–1699. doi: 10.1046/j.1532-5415.2001.49281.x. [DOI] [PubMed] [Google Scholar]
- 32.Min LC, Wenger NS, Reuben DB, Saliba D. A short functional survey is responsive to changes in functional status in vulnerable older people. J Am Geriatr Soc. 2008;56(10):1932–1936. doi: 10.1111/j.1532-5415.2008.01921.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baker SP, O'Neill B, Haddon W, Jr., Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–196. [PubMed] [Google Scholar]
- 34.American College of Surgeons. National Trauma Data Bank Research Data Set v. 7.0 User Manual. 2007 [Google Scholar]
- 35.Malani PN. Functional status assessment in the preoperative evaluation of older adults. JAMA. 2009;302(14):1582–1583. doi: 10.1001/jama.2009.1453. [DOI] [PubMed] [Google Scholar]
- 36.Min LC, Elliott MN, Wenger NS, Saliba D. Higher vulnerable elders survey scores predict death and functional decline in vulnerable older people. J Am Geriatr Soc. 2006;54(3):507–511. doi: 10.1111/j.1532-5415.2005.00615.x. [DOI] [PubMed] [Google Scholar]
- 37.Min L, Yoon W, Mariano J, et al. The vulnerable elders-13 survey predicts 5-year functional decline and mortality outcomes in older ambulatory care patients. J Am Geriatr Soc. 2009;57(11):2070–2076. doi: 10.1111/j.1532-5415.2009.02497.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kempen GI, Suurmeijer TP. The development of a hierarchical polychotomous ADL-IADL scale for noninstitutionalized elders. Gerontologist. 1990;30(4):497–502. doi: 10.1093/geront/30.4.497. [DOI] [PubMed] [Google Scholar]
- 39.Dudgeon BJ, Hoffman JM, Ciol MA, Shumway-Cook A, Yorkston KM, Chan L. Managing activity difficulties at home: a survey of Medicare beneficiaries. Arch Phys Med Rehabil. 2008;89(7):1256–1261. doi: 10.1016/j.apmr.2007.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Demetriades D, Karaiskakis M, Velmahos G, et al. Effect on outcome of early intensive management of geriatric trauma patients. Br J Surg. 2002;89(10):1319–1322. doi: 10.1046/j.1365-2168.2002.02210.x. [DOI] [PubMed] [Google Scholar]
- 41.Fallon WF, Jr., Rader E, Zyzanski S, et al. Geriatric outcomes are improved by a geriatric trauma consultation service. J Trauma. 2006;61(5):1040–1046. doi: 10.1097/01.ta.0000238652.48008.59. [DOI] [PubMed] [Google Scholar]
- 42.Glance LG, Dick A, Osler TM, Mukamel D. Judging trauma center quality: does it depend on the choice of outcomes? J Trauma. 2004;56(1):165–172. doi: 10.1097/01.TA.0000047808.77902.83. [DOI] [PubMed] [Google Scholar]
- 43.Agostini JV, Baker DI, Inouye SK, Bogardus ST. Multidisciplinary Geriatric Consultation Services. Chapter 29 in: Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment, No. 43. [accessed on 4/3/13. 2001.];AHRQ Publication No. 01-E058. http://archive.ahrq.gov/clinic/tp/ptsaftp.htm.
- 44.Deschodt M, Flamaing J, Haentjens P, Boonen S, Milisen K. Impact of geriatric consultation teams on clinical outcome in acute hospitals: a systematic review and meta-analysis. BMC medicine. 2013;11:48. doi: 10.1186/1741-7015-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bachmann S, Finger C, Huss A, Egger M, Stuck AE, Clough-Gorr KM. Inpatient rehabilitation specifically designed for geriatric patients: systematic review and meta-analysis of randomised controlled trials. BMJ. 2010;340:c1718. doi: 10.1136/bmj.c1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marcantonio ER, Flacker JM, Michaels M, Resnick NM. Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc. 2000;48(6):618–624. doi: 10.1111/j.1532-5415.2000.tb04718.x. [DOI] [PubMed] [Google Scholar]
- 47.Rudolph JL, Schreiber KA, Culley DJ, et al. Measurement of post-operative cognitive dysfunction after cardiac surgery: a systematic review. Acta Anaesthesiol Scand. 2010;54(6):663–677. doi: 10.1111/j.1399-6576.2010.02236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sager MA, Franke T, Inouye SK, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med. 1996;156(6):645–652. [PubMed] [Google Scholar]
- 49.McCusker J, Kakuma R, Abrahamowicz M. Predictors of functional decline in hospitalized elderly patients: a systematic review. J Gerontol A Biol Sci Med Sci. 2002;57(9):M569–577. doi: 10.1093/gerona/57.9.m569. [DOI] [PubMed] [Google Scholar]
- 50.Sager MA, Rudberg MA, Jalaluddin M, et al. Hospital admission risk profile (HARP): identifying older patients at risk for functional decline following acute medical illness and hospitalization. J Am Geriatr Soc. 1996;44(3):251–257. doi: 10.1111/j.1532-5415.1996.tb00910.x. [DOI] [PubMed] [Google Scholar]
- 51.Wu HY, Sahadevan S, Ding YY. Factors associated with functional decline of hospitalised older persons following discharge from an acute geriatric unit. Ann Acad Med Singapore. 2006;35(1):17–23. [PubMed] [Google Scholar]
- 52.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]