Abstract
Fecal microbiota transplantation (FMT) has emerged as an effective treatment for C. difficile infection (CDI) refractory to antibiotic therapy alone. Given the important roles of microbiota in the function of the gastrointestinal tract and other aspects of human physiology, there is also growing interest in studying FMT for other clinical indications. The U.S. Food and Drug Administration has determined that FMT constitutes a drug and is an investigational agent; as such an investigational new drug application (IND) is encouraged in treatment of recurrent CDI and required to administer FMT for any other indications. Most physicians and investigators do not have the regulatory experience necessary to navigate the IND process easily. Our aim is to provide guidance to others who are interested in obtaining an IND to perform or study FMT.
Keywords: FDA, guidance, CBER
Introduction
The incidence, morbidity, and mortality of Clostridium difficile infection (CDI) have steadily increased since mid 1990s following emergence of more virulent strains of this pathogen.1–3 One particularly difficult clinical form of the infection is recurrent CDI (R-CDI) that is refractory to eradication despite multiple treatments with existing antibiotics.4 Fecal microbiota transplantation (FMT) has emerged recently as a potential answer for recurrent Clostridium difficile infection (R-CDI). Although the mechanisms by which FMT eliminates CDI remain unclear, the procedure results in restoration of normal microbial gut ecology.5,6 Therefore, it is possible that FMT may become applicable to other conditions associated with intestinal dysbiosis, including inflammatory bowel disease (IBD),7 irritable bowel syndrome, antibiotic associated diarrhea and components of the metabolic syndrome, such as obesity and diabetes.8
The U.S. Food and Drug Administration (FDA) has oversight over any substance intended to prevent, treat, or cure a disease or condition. The FDA has determined that fecal microbiota falls within the definition of a biologic product and a drug, as defined in section 351(i) of the Public Health Service Act [42 U.S.C. 262(i)] and section 201(g) of the Federal Food, Drug, and Cosmetic Act (FDCA) [21 U.S.C. 321(g)]. Since FMT has not yet been approved by the FDA for any specific clinical indication, it constitutes an investigational agent and requires an Investigational New Drug application (IND) from Center for Biologics Evaluation (CBER) and Research, a branch within the FDA that regulates biological products for human use. This decision was articulated by the FDA and NIH at the recently held public workshop to address scientific and regulatory issues surrounding FMT.9 Given the complexity of IND applications and its burden on a physician, the FDA announced its intention to exercise enforcement discretion regarding IND applications for use of FMT to treat R-CDI. In these cases, an IND is encouraged, but not required10. This decision, for now, decreases the need for IND to treat individual patients with R-CDI. However, an IND for use of FMT is still required for indications other than C. difficile infection or for research purposes.
As investigators holding INDs to use FMT in patients with CDI and IBD, we aim to provide guidance to other investigators and clinicians on the IND application process. For the purpose of this paper we will limit our discussion to research IND for R-CDI; the required elements of the application are the same for other indications.
Investigational New Drug (IND)
An IND is an FDA application to test a new drug (or biologic) in human. In the US, an IND is required whenever clinical studies are initiated on a new drug or biologic or for a new indication or different route of administration of an already approved drug.
Sponsor
An investigator/clinician who applies for the IND is the sponsor. The IND can have only one sponsor.
Types of IND
There are 3 types of INDs applicable to FMT. An Investigator (or research) IND is submitted by a physician who both initiates and conducts an investigation, and under whose immediate direction FMT is administered or dispensed. An emergency IND can be obtained if the situation does not allow time for an IND submission, for individual patients who do not meet the criteria of an existing study protocol, or if an approved study protocol does not exist. An expanded access (treatment) IND is submitted for experimental therapies showing promise in clinical testing for serious or immediately life-threatening condition. For the purpose of FMT, all the types of INDs can be applied depending on the need of a clinician; however, at this point, only research INDs are permitted when using FMT in IBD and other diseases. Individual patients (adult or pediatric) may be treated outside of an IND for R-CDI provided that the treating physician obtains informed consent which should state that use of FMT is investigational and include discussion of its potential risks10.
Responsibilities of IND sponsor
Subpart D of 21CFR 312.50–312.70 details the responsibilities of a sponsor holding an IND. Only critical aspects are discussed here and details can be found at the following link http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=312&showF R=1&subpartNode=21:5.0.1.1.3.4.
Sponsors are responsible for selecting qualified investigators, providing them with the information they need to conduct an investigation properly, ensuring proper monitoring of the investigation(s), ensuring that the investigation(s) is conducted in accordance with the investigational plan and protocols contained in the IND, maintaining an effective IND with respect to the investigations, and ensuring that FDA and all participating investigators are promptly informed of significant new adverse effects or risks with respect to the drug. The sponsor has to monitor the progress of all investigations being conducted under IND including review and evaluation of the evidence relating to the safety and effectiveness of the drug and important discussions with IRB, which should be promptly communicated with FDA.
Elements of an IND Application
1) Product name/chemical structure (example)
Fecal Microbiota Transplantation (FMT) - biologically active human fecal material
2) Proposed indications
The sponsor must provide a list of indications (e.g. R-CDI, IBD) for which FMT will be used.
3) Dosage and Route of Administration (example)
The application must include specific information about the dosage form, route of administration and dosing. For example:
Dosage form: Solution of filtered human donor stool (approximately 50 grams) homogenized in sterile normal saline (300 mL)
Dose administered: 250 mL
- Route:
-
i)Infused through the working channel of the instrument during colonoscopy or sigmoidoscopy
-
ii)Retention enema
-
iii)Naso-duodenal tube
-
i)
4) Background
It is expected that the sponsor provide some background information about the therapy. This section need not be extensive, but should provide a rationale behind the proposed treatment and reference any relevant existing literature.
5) Chemistry, Manufacturing and Controls Information
The contents of this section vary depending on the source/form of donor material. Stool is a heterogeneous substance, composed primarily of bacteria and water, but also containing viral and fungal organisms, metabolic products of these organisms, undigested foods, bile, bilirubin, cholesterol, inorganic salts, dead cells, and mucus from the lining of the intestinal wall. The process of donor eligibility determination, testing and stool processing and infusion defines the Fecal Microbiota “product.” Frozen fecal microbiota has been shown to be equally effective in treating CDI.11 If the sponsor decides to seek an IND for frozen material, they will need to provide detail about how donor stool will be processed and stored. There is now ongoing effort pursued by several groups in manufacturing of standardized fecal microbiota material. If the sponsor chooses to collaborate with one of these groups, letters authorizing cross reference to the respective files (the sponsor of this IND and the IND sponsored by the group manufacturing the fecal microbiota) should be provided to the FDA. Sponsors seeking IND for FMT-based microbial therapeutics (such as frozen preparations or purified cultures of donor microbiota) are required to provide detail about how the microbiota originating from donor stool will be processed, evaluated, packaged, labeled, stored and delivered and include a plan for assessment of quality control. Further discussion of this is beyond the scope of this paper.
6) Clinical Data Summary
The sponsor should provide a background of the disease being treated and rationale for use of an unapproved product. This section may contain incidence and prevalence of CDI, failure of antimicrobial agents, recurrence rates, morbidly, mortality and burden on the healthcare system. A brief summary of human experience as well as the investigators' own experience or preliminary data, if any, should be presented in this section.
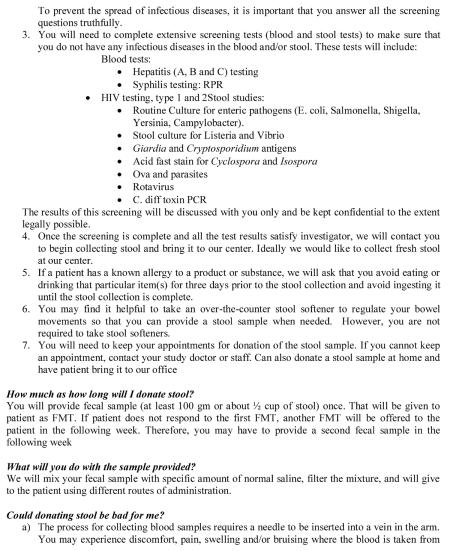
7) FMT Treatment protocol
The protocol to administer FMT should include specific indications and, in the case of clinical trials, inclusion and exclusion criteria for donors and subjects. Detailed patient and donor evaluation and testing protocols should also be provided. The FDA is currently working with professional societies to develop guidance for donor screening. The sponsor should provide rationale for deviating from recommended donor testing standards. Suggested donor screening tests are listed in table 1, but additional testing may be considered depending on the indication and/or health status of the recipient (e.g. immunocompromised). One should indicate the approximate number of patients per month (or year) that will be treated under an expanded access IND. The protocol should detail collection and handling of the fecal material as well as location and methods for preparation and processing. It must include details regarding the plans for clinical follow up of treated patients. A sample protocol treatment of CDI is included in appendix 1. This protocol should not be interpreted as a standard for all FMT; rather as a reference for other investigators to modify for their own FMT trials.
Table 1.
Donor laboratory screening
| Blood | Stool |
|---|---|
| HIV EIA, type 1 and 2 | Clostridium difficile toxin B (preferably by PCR) |
| HAV-IgM | Routine bacterial culture for enteric pathogens (E. coli, Salmonella, Shigella, Yersinia, Campylobacter) |
| HBsAg | Ova and parasites (if travel history suggests) |
| anti-HCV-Ab | |
| RPR |
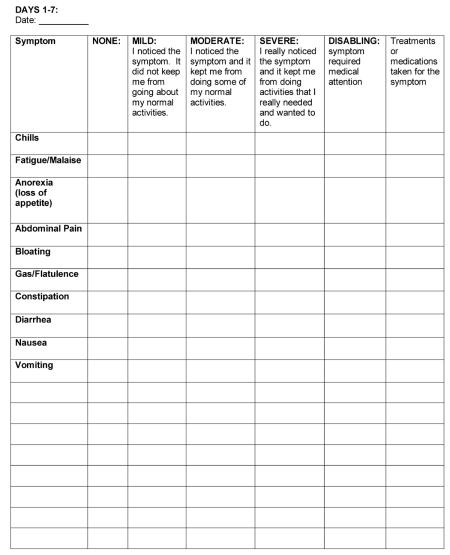
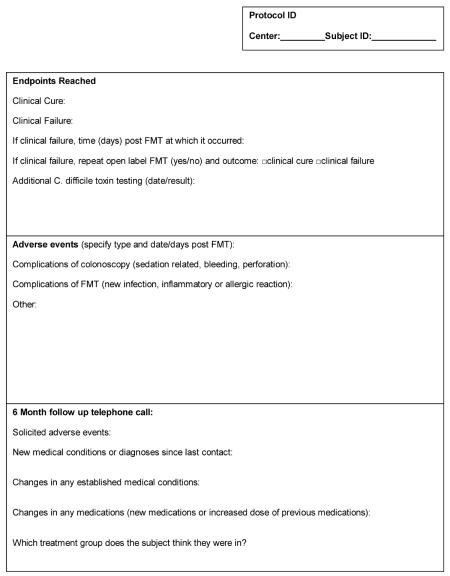
8) Adverse Event Reporting
Each protocol should develop a relevant toxicity table for capturing and recording adverse events which may be related to FMT. Examples are available on the NIH website.12 The IND application must detail which Adverse Events (AEs) the investigator will specifically document and report to the FDA (AE/SAE definitions provided in appendix 2.) These should include actual and theoretical complications related to FMT (infection, inflammatory or allergic reaction). Solicited AEs are specific symptoms inquired about at follow up telephone contacts and clinic visits, e.g. fever or chills, abdominal pain, nausea, vomiting, diarrhea or constipation. Unsolicited AEs (symptoms described by the patient or subject) may also be assessed. AEs should be assessed for causality (related or unrelated to FMT) with consideration of the temporal association between FMT exposure and onset of the AE and possible alternative causes of the AE (including the disease under treatment). Development of new symptoms/diagnoses (IBS, IBD, autoimmune disorder) which may be related or unrelated to FMT should be elicited at defined follow up time points, documented, and reported to the FDA. The FDA has published guidance for safety reporting requirements for INDs.13 The sponsor should notify the FDA of any unexpected fatal or life-threatening suspected adverse reaction as soon as possible but in no case later than 7 calendar days after the sponsor's initial receipt of the information. The FDA should also be notified within 7 days if an infectious disease is possibly, probably or definitely transmitted to a patient via FMT. All Serious Adverse Events (SAEs) must be reported within 15 days to the FDA and all other AEs are reported in annual reports to the FDA.
Sponsors must monitor for AEs and are responsible for reporting AEs that occur in patients treated by participating providers. Participating providers include all persons treating patients under the sponsor's IND. Sponsors must maintain records documenting AEs and must periodically review and analyze the entire safety database for IND safety reporting purposes. A safety report should be submitted when any of the following criteria are met:
Serious and unexpected suspected adverse reaction
Findings from other sources: This includes findings from clinical, epidemiological, or pooled analysis of multiple studies or any findings that suggest a significant risk in humans exposed to FMT.
Increased occurrence of serious suspected adverse reactions: The sponsor will report any clinically important increase in the rate of a serious suspected adverse reaction over that listed in the protocol
The sponsor must also submit annual safety reports under 21 CFR 312.33(b) to include:
AE (within pre-specified time periods)
SAE (within pre-specified time periods)
percentage of patients who did/did not experience cure post FMT
percentage of patients who received a second FMT
other pertinent statistics to help evaluate the safety and effectiveness of FMT
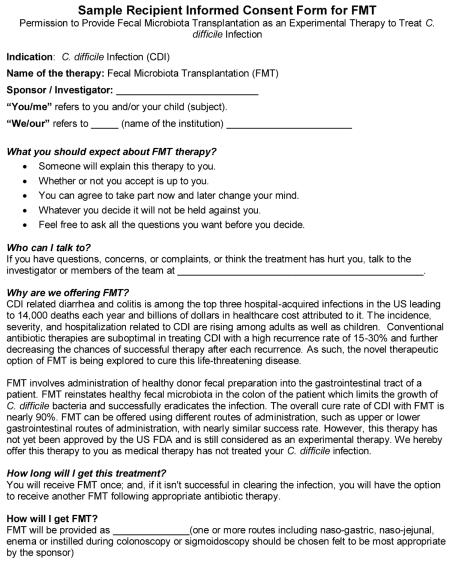
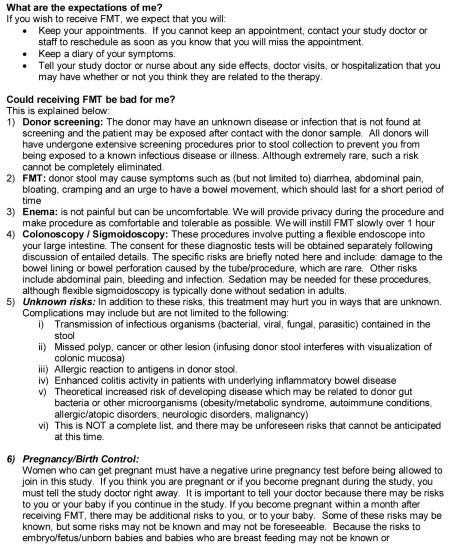
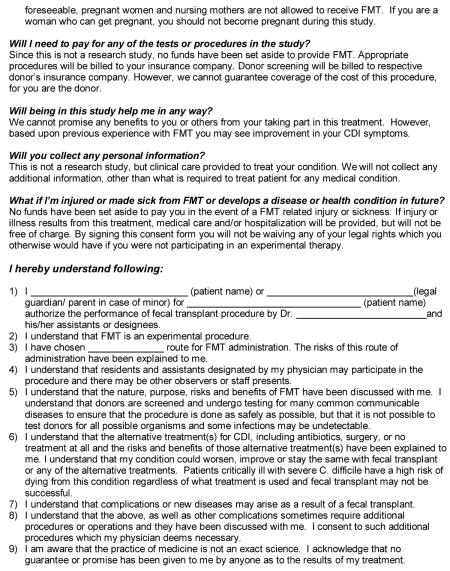
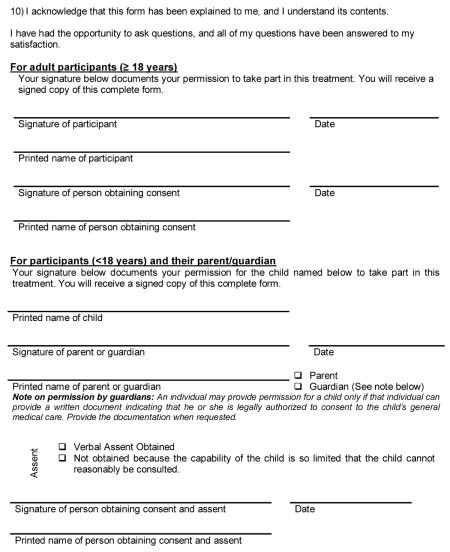
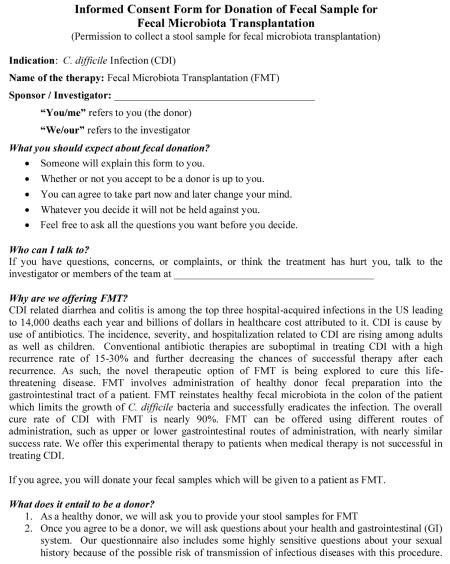
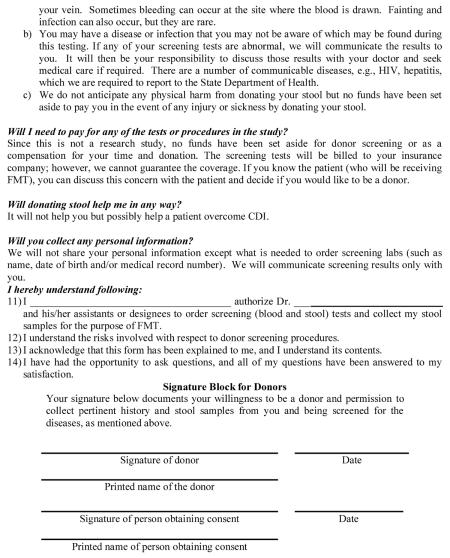
9) Risks Associated with FMT
The protocol should detail the risks involved and describe how these risks to patients will be mitigated. Patients should be given informed consent (IC) detailing all potential risks related to FMT, such as transmission of infectious agents, allergens, metabolic disorders including unforeseeable risks. The IC form should be provided with the IND application. Complications related to the method of administration (colonoscopy or sigmoidoscopy) should be discussed separately and it is expected that patients will be given standard informed consent prior to these procedures. In children, consents from parents or a legal guardian must be obtained. Children who are capable of understanding the procedure or voice their opinion (ages 7–17 years) should be able to provide assent.
Donors are at a risk of becoming aware of a new diagnosis (e.g., HIV) and consequences associated with it. This should be addressed in donor consent as well as how testing results will be communicated with donors without compromising their confidentiality.
Sample subject and donor IC and assents for children are in appendix 3.
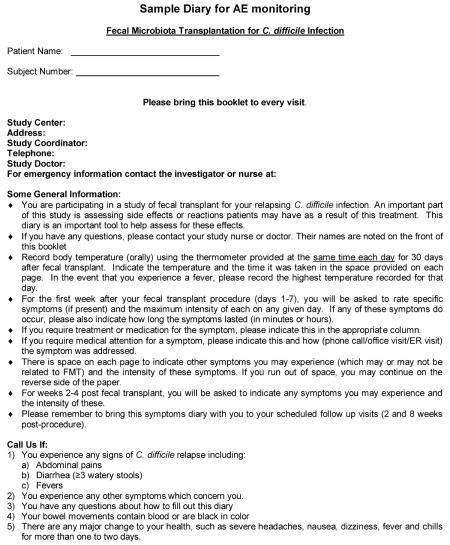
10) Safety Monitoring Protocol
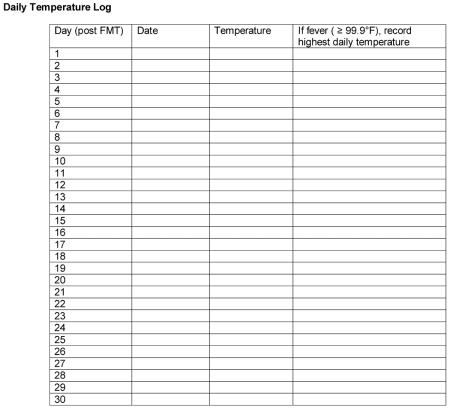
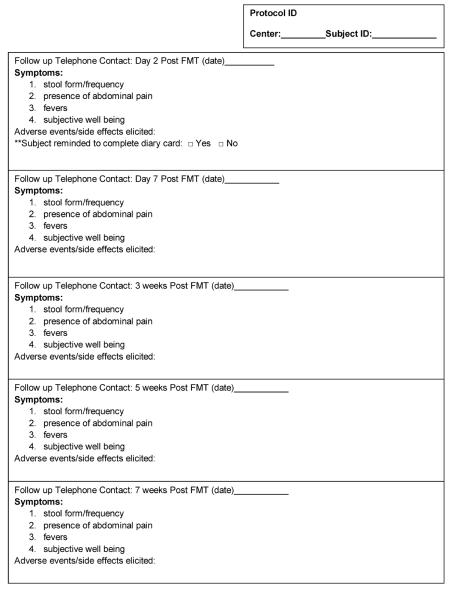
This section must detail how the sponsor will monitor for and report AEs related or unrelated to FMT. The sponsor may itemize specific AEs which will be elicited (such as fever, abdominal pain or diarrhea). It is expected that AEs will be recorded and reported to the FDA. Both anticipated and unanticipated AEs and problems must be formally monitored and recorded. The sponsor must determine the relationship of these AEs to FMT (unrelated, possible, probably and definite). The guidance for AE monitoring, grading severity and assessing relationship to the intervention can be inferred from `common terminology criteria for adverse events (CTCAE v4.0). Methods may consist of symptom diaries maintained by patients/subjects, follow-up telephone contacts and clinic visits. A sample diary card is provided in appendix 4. The Sponsor is responsible for monitoring the safety and efficacy of this treatment and complying with the reporting requirements.
The sponsor must convene a data safety monitoring board (DSMB) independent of the protocol to periodically review the outcomes of patients treated under the protocol (clinical or research). This board should have the power to halt the treatment of patients under the protocol if it is determined that safety concerns exist. The FDA should be notified within 48 hours if the IND is halted for review.
In randomized controlled trials and other experiments on human subjects, stopping (or halting) rules are laid down in advance. These specify conditions under which the study will be terminated. For example, a study may be stopped if there is demonstration that one regimen is clearly harmful or superior to the other. Since FMT is considered experimental therapy by the FDA, stopping rules are also required for expanded access (treatment) INDs. Examples are provided in appendix 2.
What else is needed?
IND application FDA Form 1571
The initial and each subsequent IND submission should be accompanied by Form FDA 1571 and must be submitted in triplicate (the original and two photocopies). Mailing addresses for initial IND Submissions are: Food and Drug Administration, Center for Drug Evaluation and Research, Therapeutic Biological Products Document Room, 5901-B Ammendale Road, Beltsville, MD 20705-1266. Upon receipt of the IND by FDA, an IND number will be assigned. Study intervention or enrollment of subjects should not be initiated until 30 days after the date of receipt of the IND by FDA unless you receive earlier notification by FDA that studies may begin. It is recommended that the sponsor communicate with FDA before proceeding with study. Revised applications require tracked changes. The first application is numbered “0000” with addendums or revisions numbered subsequently “0001, 0002 etc.” Form 1571 can be obtained at: http://www.fda.gov/downloads/AboutFDA/ReportsManualsForms/Forms/UCM083533.pdf
FDA Form 1572
This form should be sent to FDA to satisfy requirement of Form 1571, box 12, item 6, b-d. Information can be supplied in the form of attachments (such as curriculum vitae) rather than entering that information directly onto the form, but this should be so noted under the relevant section numbers. Form 1572 can be obtained at: http://www.fda.gov/downloads/AboutFDA/ReportsManualsForms/Forms/UCM074728.pdf
Local IRB approval
In addition to the IND, local IRB approval is mandatory to conduct the research protocol. Many documents reviewed by the FDA will also be needed by the IRB. It is critical to facilitate communication between local IRB and FDA, so that protocols, consents and other documents submitted to both agencies match.
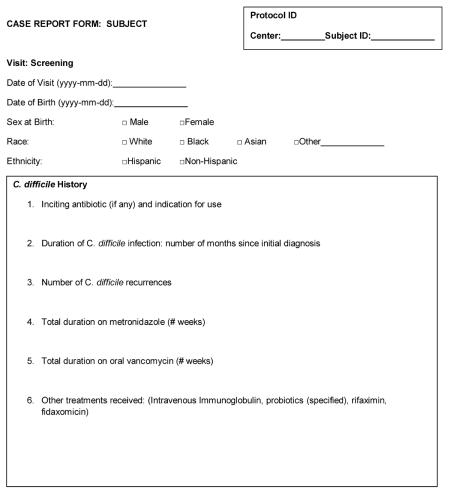
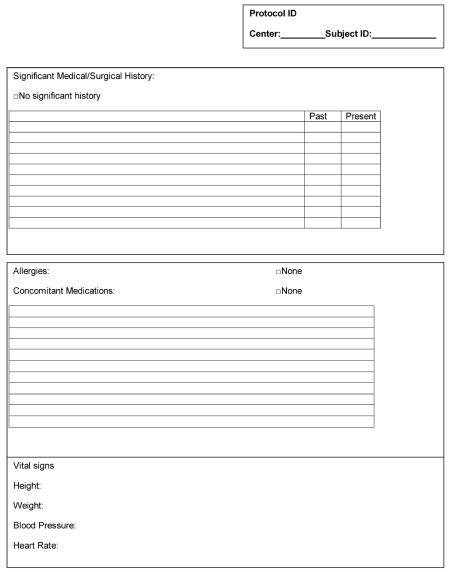
Case report form
Case report forms (CRF) are tools used by the sponsor of a clinical trial to collect data. The sponsor is responsible for designing a CRF that collects specific data necessary to answer study questions. All data on participating subjects and donors (including adverse events) should be documented in the CRF. A copy of the CRF should be included with the IND application. The CRF should be organized to promote complete and accurate data entry. An example of a CRF for an R-CDI trial is included in appendix 5.
Investigators brochure (for studies being performed at multiple sites)
The sponsor must submit an investigator's brochure (IB) when investigators, other than the sponsor will be administering FMT under the IND. Its purpose is to provide the investigators and others involved in the trial with the information to needed to understand the protocol. The information should be presented in a concise, simple form that enables a clinician, or potential investigator, to make his/her own unbiased risk-benefit assessment of the appropriateness of the proposed trial.14 The sponsor is responsible for ensuring that an up-to-date IB is made available to other investigator(s) and the investigators are responsible for providing the up-to-date IB to the responsible IRBs. The IB should contain a brief summary, introductory statement, description of the product, proposed indications, dosage form, route of administration, and dosing regimen. It should include a clinical data summary with the background of the disease, summary of previous human experience (known safety and efficacy data) and may also contain the complete study protocol. The IB should be reviewed annually and revised when necessary to include any new relevant information.
Summary
The practice of FMT is evolving rapidly. For example, minimal requirements for donor testing are likely to change over time. Some testing that is currently merely recommended15 may become absolute requirements or may be found unnecessary. In fact, the specifics of the local donor testing protocols vary among the individual existing programs represented by authors in this manuscript. Each IND sponsor must consider the unique aspects of their target patient population and clinical capability in developing their own protocol. This manuscript is only a guide to all the elements necessary to put together a protocol and an FDA application, and a starting point for the new IND sponsor.
Acknowledgments
Grant Support:
1NIH 1R21DK093839-01A1
3NIH R21 AI091907
Appendix 1
I. Indications
This protocol will be used to treat adults (ages 18 to ___ years) and/or children (ages ___ to 17 years) with fecal microbiota transplantation for C. difficile infection (CDI). FMT will be used to treat CDI in either of the following circumstances:
- Recurrent or relapsing CDI.
- At least three episodes of mild-to-moderate CDI and failure of a 6–8 week taper with vancomycin with or without an alternative antibiotic (e.g.,rifaximin, nitazoxanide, fidaxomicin).
- Recurrent CDI with at least one episode of severe CDI resulting in hospitalization and associated with significant morbidity.
Moderate CDI not responding to standard therapy (metronidazole, vancomycin or fidaxomicin) for at least a week.
Definitions16
Recurrent or relapsing CDI: Recurrent CDI within 8 weeks of completion of therapy.
Mild to moderate CDI: Diarrhea plus any additional signs or symptoms not meeting severe or complicated criteria.
Severe CDI: WBC ≥ 15,000 cells/mm3, albumin < 3g/dl and/or abdominal tenderness
Complicated CDI defined by at least one of the following: admission to the ICU, hypotension with or without the use of vasopressors, fever ≥ 38.5°C, ileus or significant abdominal distention, mental status changes, WBC ≥ 35,000 cells/mm3, or < 2 cells/mm3, serum lactate >2.2 mmol/L or any evidence of end-organ failure
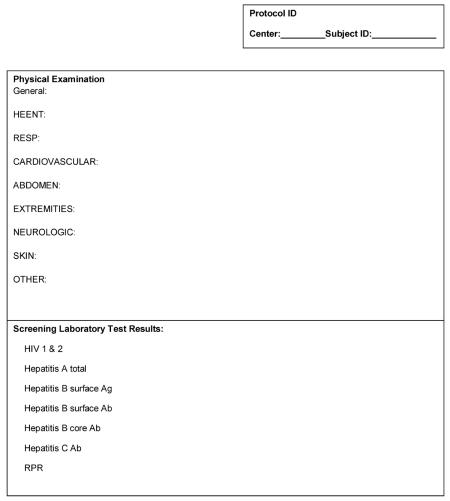
II. Patient Eligibility Determination
History and physician exam: potential FMT patients will undergo a medical interview to determine eligibility for the treatment and a physical exam will be performed.
Serologic testing: All patients will undergo blood testing to document baseline status prior to FMT including: HIV 1 & 2, Hepatitis A total, Hepatitis B surface Ag, surface Ab and core Ab, Hepatitis C Ab, and RPR.
Female subjects and pregnancy: Females of childbearing potential will have a urine pregnancy test on the day of the FMT procedure (to ensure eligibility). Patients who are pregnant will not be permitted to receive FMT.
III. Donor Eligibility Determination
Donor selection and screening: Patients may identify a donor (related or unrelated). For cases in which the patient does not have an available, qualified or willing donor, potential healthy volunteer donors will be recruited. Donors under the age of ______years (generally less than 18 years) will be excluded. Prospective donors will undergo a medical interview and physical exam as well as screening questionnaire and laboratory testing.
-
Donor interview and screening Questionnaire: Potential donors will have a brief interview to determine the presence of medical or infectious conditions using Donor History Questionnaire (DHQ) materials prepared by the AABB Donor History Task Force for use in screening blood donors. DHQ v1.3 can be found at: http://www.fda.gov/downloads/BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/LicensedProductsBLAs/BloodDonorScreening/UCM213552.pdf. Additional questions (such as listed below) which are felt relevant to FMT and physiologic roles of gut microbiota, can be added to this questionnaire:
- Known communicable disease
- Systemic autoimmunity or atopic diseases
- Chronic pain syndromes (for example: fibromyalgia, chronic fatigue)
- Neurologic, neuro-developmental or neurodegenerative disorders
- Malignancy
- Diarrheal disorder (IBS, IBD, celiac disease)
- Constipation
- Use of antibiotics for any indication within the past 3 months
DHQ will be used to exclude donors with these and other risk factors:- High risk sexual behaviors (examples: sexual contact with anyone with HIV/AIDS or hepatitis, men who have sex with men, sex for drugs or money)
- Known exposure to HIV or viral hepatitis within the previous 12 months.
- Being held in a correctional facility for more than 72 hours in the last 12 months
- Use of intravenous drugs or intranasal cocaine
- Recent tattoo or body piercing
- Use of antibiotics within the past 3 months
- Recent transfusion, transplant or skin graft
- Risk factors for variant Creutzfeldt-Jakob disease
- Use of antibiotics a period of 3 months.
DHQ will be completed within 30 days before FMT.
IV. Donor Laboratory Testing
Required stool and serologic testing is detailed in table below. HIV 1 & 2 testing will be performed within 2 weeks before fecal donation for FMT. The other serologic and stool screening will be performed within one month before fecal donation for FMT.
|
| |
| Blood | Stool |
|
| |
| HIV ELISA, type 1 and 2 | Clostridium difficile toxin by PCR |
|
| |
| HAV IgM | Routine bacterial culture for enteric pathogens (E. coli, Salmonella, Shigella, Yersinia, Campylobacter) |
|
| |
| HBsAg, anti-HBc (both IgG and IgM), and anti-HBs |
Culture for Listeria monocytogenes and Vibrio (parahaemolyticus and cholerae) |
|
| |
| HCV Ab | Cryptosporidium antigen |
|
| |
| RPR | Acid-fast stain for Cyclospora and Isospora |
|
| |
| Giardia antigen | |
|
| |
| Ova and parasites | |
|
| |
| Rotavirus via EIA | |
|
| |
V. Collection and Preparation of Stool for FMT Infusion
- On the day of fecal donation, donor should be questioned regarding the following:
- Fever, vomiting, diarrhea or other symptoms of infection within the last 30 days.
- Ingestion of potential allergen where the recipient has a known allergy to the agent.
- Stool collection
- Donors will be supplied a toilet hat and clean, sealable containers for collection and transport of stool. Containers will be labeled with the name, date of birth and date/time of stool collection.
- Collected stool will be immediately refrigerated, transferred to the laboratory facility for processing on ice within a biohazard bag (but not frozen) and used within 6 hours collection.
- Location & preparation of processing area
- Stool will be processed in a designated area within the endoscopy unit.
- Universal precautions will be used during processing (gown, gloves, eye protection).
- Clean counter surface will be covered with a Chux® pad.
- After the FMT, all surfaces will be wiped with hospital-approved disinfectant solution.
- Preparation materials
- Non-bacteriostatic normal saline
- Sterile container with lid (optional – a blender) to homogenize donor stool with saline
- Clean gauze pieces (optional - disposable sieve) for filtration
- Clean plastic spoon
- 60 cc disposable slip (catheter)-tip syringes
- Disposable enema syringe (if enema is the chosen route of administration)
- Preparation method
- Available quantity of stool (typically 50 grams) will be added to sterile normal saline (250–500 ml) in sterile container
- The mixture can be homogenized by shaking or using a blender.
- This solution will then be filtered if necessary to remove larger articulate matter.
- The fecal suspension will be drawn into aliquots of 60 cc slip (catheter) tip syringes or enema bottles for infusion.
- Syringes will be delivered to procedure area for administration during colonoscopy, sigmoidoscopy or via retention enema.
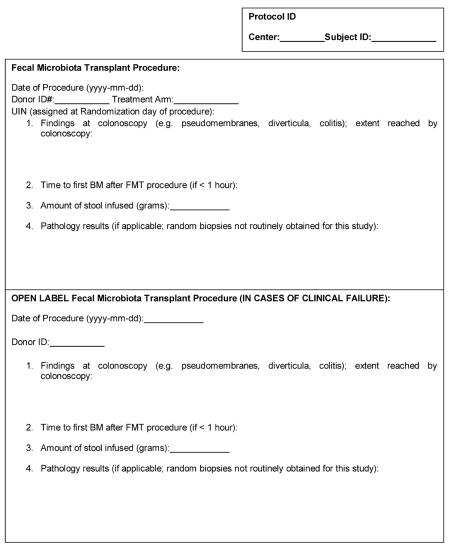
VI. FMT Procedure
- Patient preparation
- Patients will have completed at least a 10 day course of vancomycin (or other anti-CDI therapy such as fidaxomicin or metronidazole) for the most recently diagnosed acute CDI prior to undergoing FMT.
- To prevent disease relapse while awaiting FMT, anti-CDI therapy will be continued by patients up until 2–3 days prior to scheduled procedure.
- For endoscopic administration of FMT, the subject will be prepped with standard bowel purge administered the day before the procedure,
- 1–2 hours before colonoscopy, the patient may take 2 loperamide tablets to aid in retention of administered donor stool (many practitioners do not do this without any apparent loss of efficacy).
- Methods of FMT infusion.
- Procedure will be performed within GI/endoscopy units of the centers.
- The method used to deliver the FMT will depend on individual characteristics of the patient and is at the discretion of the treating physician. FMT may be administered by the following methods.
- colonoscopy- This method allows full endoscopic examination of the colon and exclusion of co-morbid conditions (such as IBD, microscopic colitis, malignancy, diverticulosis) which may have an impact on patient's treatment or response to therapy.
- sigmoidoscopy- This method still allows infusion of the stool into a more proximal segment of the colon than an enema, and provides some diagnostic information. It does not require sedation for adults, although children may need sedation. This method may be beneficial in patients who are elderly or multiparous and who may have difficulty retaining the material when given as enema. Sigmoidoscopic administration eliminates the additional risks associated with colonoscopy in patients who may not have a clear indication for colonoscopy.
- retention enema- This method may be preferable in younger patients who have already had recent endoscopic evaluation, in patients who prefer not to undergo endoscopy or in patients with significant co-morbidities and may not tolerate endoscopy. During retention enema, tolerance to the administration should be monitored to avoid leaking and failure of the procedure. We recommend administration of 60 cc enema every 15 minutes in left lateral decubitus position with elevated hips.
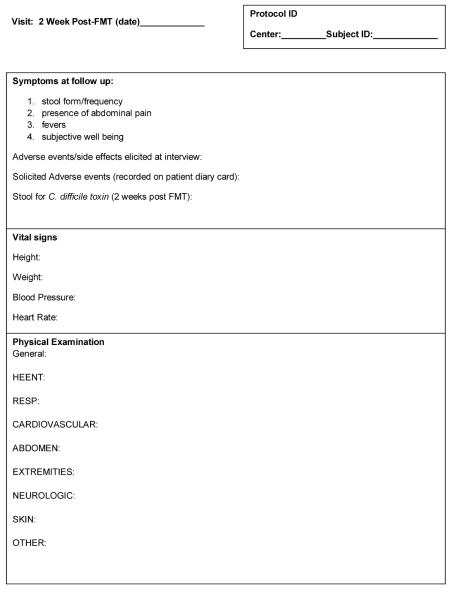
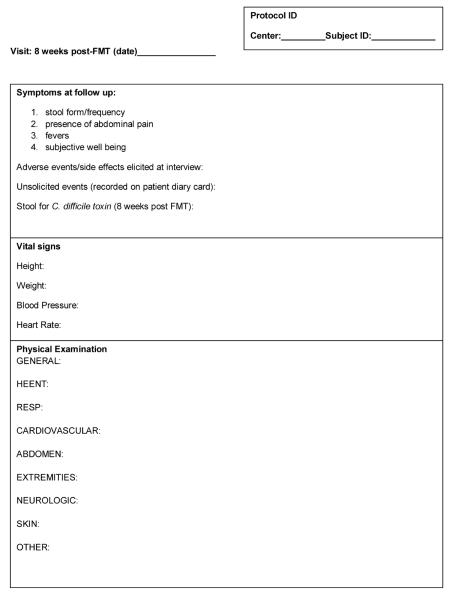
VII. Follow up
Patients will be encouraged to contact the clinical team immediately if they experience recurrence of diarrhea so that stool can be tested for C. difficile toxins A & B and treatment with anti-CDI therapy can be initiated if necessary.
Per SHEA-IDSA guidelines, patients will only submit stool specimens for C. difficile toxin testing if they experience symptoms suggestive of CDI relapse. Testing to confirm cure in asymptomatic patients is not indicated.
Patients will be contacted via telephone by a member of the clinical team 24 hours and 14 days post FMT and again 6 months post FMT to assess symptoms and adverse events.
Subjects may be scheduled in the office for follow up visit at 4–8 weeks post FMT.
Patients will be instructed to inform the treating physician of any infectious symptoms or new medical conditions which develop after FMT. Adverse events will be elicited at follow up telephone contacts and follow up visits and all patients will be contacted via telephone by the treating physician 6 months after the last treatment to record any SAEs, new medical conditions/diagnoses or changes in medical conditions/medications since last clinical contact.
VIII. Patients Who Relapse After FMT
In the event of treatment failure (defined as CDI recurrence requiring additional anti-infective therapy), the treating physician will have the following options.
Patient may undergo a second FMT using the same or an alternate donor. This second FMT will be given after the subject has completed at least a 10 day course of oral vancomycin (or other anti-infective therapy for CDI).
Patient may choose not to receive further FMT, but may continue to be treated in accordance with the current standard of care. The will continue to be followed for closely for AEs with telephone calls and clinic visits as per this protocol.
Alternatively, patients who chose not to receive further FMT may decide to be treated at another facility of their choosing. They will still be followed as per protocol through the 4 week post FMT period and asked to receive a 6 month follow-up telephone call to assess for late SAEs or changes in medical conditions/diagnoses or medications.
Patients who chose to undergo a second FMT will have the identical procedure, including donor eligibility determination, follow up, and safety monitoring.
Appendix 2
I. Definitions
A. Adverse Event (AE)
An AE is any untoward medical occurrence in a patient after administration of study drug (FMT) that does not necessarily have to have a causal relationship with this treatment. An AE can therefore be any unfavorable and unintended sign (including an abnormal laboratory finding), symptom, or disease temporally associated with the use of a FMT, whether or not related to the FMT.
AEs may be new events or may be pre-existing conditions that have become aggravated or have worsened in severity or frequency.
AEs may be clinically significant changes from baseline in physical examination, laboratory tests, or other diagnostic investigation (e.g., laboratory results, x-ray findings).
Pregnancy is not an AE; however, if a female subject becomes pregnant during 4 week period post-FMT, the treating physician will notify the FDA.
B. Serious Adverse Event (SAE)
A serious adverse event is any adverse experience occurring during or after FMT that results in any of the following outcomes:
Death
-
Life-threatening experience;
Note: An adverse event or suspected adverse reaction is considered “life-threatening” if, in the view of either the investigator or sponsor, its occurrence places the patient or subject at immediate risk of death. It does not include an adverse event or suspected adverse reaction that, had it occurred in a more severe form, might have caused death.
-
Requires inpatient hospitalization or prolongation of existing hospitalization
Note: Adverse events requiring hospital admissions that are less than 24 hours in duration do not meet this criterion. A scheduled hospitalization for a pre-existing condition that has not worsened during participation in the study does not meet this criterion. Pre-planned hospitalizations for an elective medical/surgical procedure or routine check-ups do not meet this criterion;
Results in persistent or significant disability or incapacity
Is a congenital anomaly or birth defect
-
Is considered to be an important medical event.
Note: Important medical events are those that may not be immediately life threatening or result in death or hospitalization but may jeopardize the patient or may require intervention to prevent one of the outcomes listed in the definition above.
C. Planned Hospitalization
A hospitalization planned prior to FMT is to be considered a therapeutic intervention and not the result of a new SAE. If the planned hospitalization or procedure is executed as planned, it will be recorded in the subject's medical history or procedures. However, if the event/condition worsens during the trial, it must be reported as an AE.
D. Adverse reaction
An adverse reaction means any adverse event caused by FMT. Adverse reactions are a subset of all suspected adverse reactions for which there is reason to conclude that FMT caused the event.
E. Suspected Adverse Reaction
Suspected adverse reaction means any adverse event for which there is a reasonable possibility that FMT caused the adverse event. For the purposes of IND safety reporting, `reasonable possibility' means there is evidence to suggest a causal relationship between FMT and the adverse event. A suspected adverse reaction implies a lesser degree of certainty about causality than adverse reaction, which means any adverse event caused by a drug.
F. Unexpected
An adverse event or suspected adverse reaction is considered “unexpected” if it is not listed in the investigator brochure or is not listed at the specificity or severity that has been observed; or is not consistent with the risk information described in the general investigational plan or elsewhere in the current application.
II. Monitoring of AE
Each patient will be monitored for the occurrence of AEs, including SAEs, beginning immediately after FMT. Patients will be questioned at each follow up time-point regarding stool form/frequency, presence of abdominal pain, fevers and subjective well being and/or examined (at 4 week follow up visits) by the treating physician for evidence of AEs. The questioning of subjects with regard to the possible occurrence of adverse events will be generalized such as, “How have you been feeling since your last visit?”
Patients having AEs will be monitored with relevant clinical assessments and laboratory tests, as determined by the treating physician.
AEs, actions taken as a result of AEs, and follow-up results must be recorded in the patient's medical record.
Patients will receive a follow up phone call 6 months post transplant to record any SAEs, new medical conditions/diagnoses or changes in conditions or diagnoses since last study contact.
For all SAEs and AEs, relevant clinical assessments and laboratory tests will be repeated as clinically appropriate, until final resolution or stabilization of the event(s).
III. Assessment of AE
A. Assessment of Severity
The severity of each AE can be assessed using `common terminology criteria for adverse events' (CTCAE v3.0, 2006). It can be found at http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf. In general, the severity of AEs can be assessed using following guidelines:
|
| |
| Severity | Description |
|
| |
| Mild (1) | Transient or mild discomfort; no limitation in baseline activity; no medical intervention or therapy required. The subject may be aware of the sign or symptom, but tolerates it reasonably well. |
|
| |
| Moderate (2) | Mild to moderate limitation from baseline activity, no or minimal medical intervention/therapy required. |
|
| |
| Severe (3) | Marked limitation from baseline activity, medical intervention/therapy required, hospitalizations possible |
|
| |
| Life- threatening/ disabling (4) |
The subject is at risk of death due to the adverse event as it occurred. This does not refer to an event that hypothetically might have caused death if it were more severe. |
|
| |
B. Assessment of Causality
The physician must assess the relationship of any AE (including SAEs) to FMT, as related or not related, based on clinical judgment and using all available information. This may include consideration of temporal association between FMT exposure and onset of the AE and whether the manifestations of the AE are consistent with known actions or theoretical toxicity of FMT. AE assessment of causality can be adopted from FDA's toxicity grading scales guidance from vaccine trials (Sept 2007) as follows:
|
| |
| Relationship to FMT |
Description |
|
| |
| Definitely | Previously known toxicity of product; or an event that follows a reasonable temporal sequence from administration of the study product; that follows a known or expected response pattern to the suspected study product; that is confirmed by stopping or reducing the volume of the study product; and that is not explained by any other reasonable hypothesis. |
|
| |
| Probably | An event that follows a reasonable temporal sequence from administration of study product; that follows a known or expected response pattern to the suspected study product; that is confirmed by stopping or reducing the dosage of the study product; and that is unlikely to be explained by the known characteristics of the subject's clinical state or by other interventions. |
|
| |
| Possibly | An event that follows a reasonable temporal sequence from administration of study product; that follows a known or expected response pattern to the suspected study product; but that could readily have been produced by a number of other factors. |
|
| |
| Unrelated | An event that can be determined with certainty to have no relationship to the study drug. |
|
| |
VI. Reporting Safety Observations by the Investigator to the Sponsor
-
Reporting of Non-serious AEs
All AEs, regardless of seriousness, severity, or causal relationship to FMT, will be recorded in the patient's medical record.
-
Reporting of FMT Exposure during Pregnancy
If a female patient or the female partner of a male patient becomes pregnant during 4 week period post-FMT, the physician is required to follow up on the pregnancy until it has completed. The outcome of the pregnancy and the status of the newborn (if applicable) will be reported within 24 hours of becoming aware. If the female partner of a male subject becomes pregnant, the physician must obtain consent to collect pregnancy information (including the status of the newborn, if applicable).
-
Reporting of Safety Observations by the Physician
Any occurrence of the following events or outcomes a patient treated under this IND must be reported expeditiously by the treating physician to the FDA.
SAE
Death of subject
The investigator is to report any safety observations from the list above to the FDA within 7 days of becoming aware of the event. Any observation that is also an AE will be recorded in the medical record along with any actions taken. If not all information is available at the time of initial report, follow up SAE reports will be completed and submitted. The investigator is required to follow SAEs until resolution. Resolution is defined as:- Resolved with or without residual effects
- Return to baseline for a pre-existing condition
- Fatal outcome; if autopsy is performed, the autopsy report must be provided to the sponsor.
-
Protocol-Specific Exceptions to (Serious) Adverse Event Reporting
A suspected clinical endpoint event, regardless of when the event occurs, is not to be reported as an AE or SAE or reported in an expedited manner as an SAE. The suspected clinical endpoint event includes:
Recurrent CDAD: The patient meets all of the following:- Initial response to therapy with cure of CDI at end of treatment (vancomycin) before FMT
- A minimum of three unformed bowel movements over a 24 hour period
- A positive result for C. difficile toxin by EIA or PCR.
VII. Halting Rules
Specific safety findings will result in temporarily suspending enrollment until a safety review is convened, the objective of which is a decision as to whether the study should continue per protocol, proceed with caution, be further investigated, be discontinued, or be modified and then proceed. Suspension of enrollment (for a particular group or for the entire study) is another potential outcome of a safety review.
Subsequent review of serious, unexpected, and related AEs by the DSMB, IRB, the sponsor, or the FDA or relevant local regulatory authorities may also result in suspension of further trial interventions/administration of FMT at a site. The FDA and study sponsor(s) retain the authority to suspend additional enrollment and study interventions/administration of FMT for the entire study, as applicable.
Findings that will trigger a safety review are
Death
Transmission of an infection from donor to subject via FMT
If more than 10% of subjects experience the same Grade 3 Adverse Event
If one or more subjects experiences a serious, unexpected adverse event
Increased frequency of events (specifically, new diagnoses of inflammatory bowel disease in > 2 FMT treated subjects).
For individual subjects enrolled in the study: any subject who has an SAE related to FMT will be ineligible for a second FMT during the course of the study.
FDA/CBER will be notified by phone or fax within 48 hours if the study is halted for review.
Appendix 3
Appendix 4
Appendix 5
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: CK1 and SK2 have none. AK3 has received funding from CIPAC LLC to carry out research on FMT using frozen fecal microbiota. AK also provided consulting services for CIPAC; conflicts of interest are being managed by the University of Minnesota Conflicts of Interest Program.
Writing Assistance: NA
Author Contributions:
Colleen R. Kelly: manuscript concept, drafting manuscript, revisions of manuscript, preparation of manuscript for submission
Sachin S. Kunde: drafting manuscript, revisions of manuscript
Alexander Khoruts: drafting manuscript, revisions of manuscript
References
- 1.Kelly CP, LaMont JT. Clostridium difficile--more difficult than ever. N Engl J Med. 2008;359:1932–40. doi: 10.1056/NEJMra0707500. [DOI] [PubMed] [Google Scholar]
- 2.Ananthakrishnan AN. Clostridium difficile infection: epidemiology, risk factors and management. Nature reviews Gastroenterology & hepatology. 2011;8:17–26. doi: 10.1038/nrgastro.2010.190. [DOI] [PubMed] [Google Scholar]
- 3.He M, Miyajima F, Roberts P, et al. Emergence and global spread of epidemic healthcare-associated Clostridium difficile. Nature genetics. 2013;45:109–13. doi: 10.1038/ng.2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Surawicz CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108:478–98. doi: 10.1038/ajg.2013.4. quiz 99. [DOI] [PubMed] [Google Scholar]
- 5.van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal Infusion of Donor Feces for Recurrent Clostridium difficile. N Engl J Med. 2013;368:407–15. doi: 10.1056/NEJMoa1205037. [DOI] [PubMed] [Google Scholar]
- 6.Hamilton MJ, Weingarden AR, Unno T, Khoruts A, Sadowsky MJ. High-throughput DNA sequence analysis reveals stable engraftment of gut microbiota following transplantation of previously frozen fecal bacteria. Gut Microbes. 2013;4:125–35. doi: 10.4161/gmic.23571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kunde S, Pham A, Bonczyk S, et al. Safety, Tolerability, and Clinical Response after Fecal Transplantation in Children and Young Adults with Ulcerative Colitis. Journal of pediatric gastroenterology and nutrition. 2013;56:597–601. doi: 10.1097/MPG.0b013e318292fa0d. [DOI] [PubMed] [Google Scholar]
- 8.Aroniadis OC, Brandt LJ. Fecal microbiota transplantation: past, present and future. Current opinion in gastroenterology. 2013;29:79–84. doi: 10.1097/MOG.0b013e32835a4b3e. [DOI] [PubMed] [Google Scholar]
- 9.FDA/NIH . Fecal Microbiota for Transplantation: Scientific and Regulatory Issues. 2013. [Google Scholar]
- 10.Guidance for Industry: Enforcement Policy Regarding Investigational New Drug Requirements for Use of Fecal Microbiota for Transplantation to Treat Clostridium difficile Infection Not Responsive to Standard Therapies. 2013 Accessed at http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guidances/Vaccines/ucm361379.htm.
- 11.Hamilton MJ, Weingarden AR, Sadowsky MJ, Khoruts A. Standardized Frozen Preparation for Transplantation of Fecal Microbiota for Recurrent Clostridium difficile Infection. Am J Gastroenterol. 2012;107:761–7. doi: 10.1038/ajg.2011.482. [DOI] [PubMed] [Google Scholar]
- 12.Microbiology and Infectious Diseases Clinical Research Policies, Guidance, and Tools. DMID Toxicity Tables. 2007 Accessed at http://www.niaid.nih.gov/LabsAndResources/resources/DMIDClinRsrch/pages/toxtables.aspx.
- 13.Guidance for Industry and Investigators: Safety Reporting Requirements for INDs and BA/BE Studies. 2010 Accessed at http://www.fda.gov/downloads/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guidances/UCM333226.pdf.
- 14.The U.S. D.H.H.S and F.D.A. - CBER C . Guidance for Industry - E6 Good Clinical Practice: Consolidated Guidance. 1996. [Google Scholar]
- 15.Bakken JS, Borody T, Brandt LJ, et al. Treating Clostridium difficile infection with fecal microbiota transplantation. Clin Gastroenterol Hepatol. 2011;9:1044–9. doi: 10.1016/j.cgh.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]