Abstract
Given the importance of couples to the transmission of HIV, interventions focusing on both members of a partnership can play an important role in its prevention. We adapted and pilot tested Project Connect, an evidence-based HIV prevention intervention for couples, to determine its acceptability and feasibility among a sample of young urban South African couples. We recruited couples from a clinic in inner-city Johannesburg to take part in the study. Interviewer-administered questionnaires were conducted at baseline and post-intervention; an in-depth interview was also conducted post-intervention. Of 75 couples screened, 15 were eligible and enrolled. An important reason for ineligibility was a recent history of intimate partner violence (IPV). Couples attended, on average, five of the seven sessions. Overall, the intervention was acceptable and showed signs of potential efficacy. Couples reported enjoying Connect and feeling comfortable with its content. Participants also reported learning important communication and problem-solving skills, which resulted in more effective engagement in HIV prevention behaviors. However, the number of sessions and strict eligibility criteria proved challenging to the feasibility of the study. We recommend future couples’ interventions have fewer sessions and enroll couples with a history of IPV.
Introduction
The sexual transmission of HIV requires unprotected sexual intercourse between discordant individuals, making couples essential to the spread of the virus. Although there is debate about the importance of stable, discordant couples to the spread of the epidemic in sub-Saharan Africa (Coburn, Gerberry, & Blower, 2011; Dunkle et al., 2008; Gray et al., 2011), an estimated 1.8 million new HIV infections are attributable to discordant partners annually. Interventions focusing on couples can potentially play an important role in the prevention of HIV by disrupting this source of transmission (Curran et al., 2012; UNAIDS, 2010).
Couples-based HIV interventions offer promise in reducing risk behaviors because they engage both members of the dyad in learning and problem-solving in a safe environment. In such an environment, sensitive topics can be discussed and relationship dynamics, gender roles, power imbalances, and communication styles addressed to allow individuals to take mutual responsibility for the prevention of HIV (Burton, Darbes, & Operario, 2010; El-Bassel et al., 2010). There have been a few notable successes among couples-based interventions for HIV prevention. In particular, Couples HIV Counseling and Testing (HCT), has been found to be more effective in changing risky behavior than HCT provided to individuals tested alone (Denison, O'Reilly, Schmid, Kennedy, & Sweat, 2008). Moreover, a review of couples’ HIV prevention interventions found that, overall, these programs have successfully reduced the frequency of unprotected sex acts (Burton et al., 2010). Despite the potential efficacy of couples-based interventions for HIV prevention, to date there have been very few rigorously evaluated interventions for heterosexual couples. Aside from couples HCT, no evaluations of couples-based interventions among heterosexual couples in sub-Saharan Africa have been published. Clearly, further research in this area is warranted.
Project Connect is an evidence-based, HIV prevention intervention developed in the United States (US) for African-American and Latino couples at elevated risk for HIV/STD transmission (El-Bassel et al., 2003, 2005). The intervention content combines information on safer sex practices and prevention of HIV/STIs, couples counseling for HIV and a focus on communication and negotiation skills. The objective of the pilot study described in this paper was to assess the acceptability of feasibility of adapting Project Connect for use among young couples in Johannesburg, South Africa.
Methods
Study Site
This study took place at a public health clinic located in inner-city Johannesburg characterized by high unemployment, poverty and HIV prevalence (Stevens et al., July 2005). The clinic provides routine primary health care for Sexually Transmitted Infections (STIs), tuberculosis, family planning, HIV Counseling and Testing (HCT), and HIV treatment.
Screening, Eligibility, and Recruitment
Couples were recruited from clinic waiting rooms between August 2009 and February 2010. Couples were eligible for the study if one member of the couple had unprotected sex in the last 30 days and both members of the couple were: 1) between the ages of 18-40 (male) or the ages of 18-(female); 2) willing to attend all intervention and data sessions ; 3) living in the study area and not planning to move in the next 6 months; and 4) reported no serious physical or sexual abuse from their partner within the last six months. We did not test for HIV during screening and enrollment.
Informed consent was obtained separately from each member of the couple to ensure that individuals chose to participate voluntarily without pressure from their partner. The consent form was available in English, IsiZulu, and SeSotho, while all other written study materials were in English.
A standardized screening questionnaire, used in the original Connect, was used to screen for Intimate partner violence (IPV) (Appendix 1). Participants identified as experiencing severe violence were ineligible to participate and referred to local organizations for assistance.
Study Procedures
At the first study visit, after completing consent and confirming eligibility, each member of the couple completed an interviewer administered questionnaire on demographics, sexual history, condom use skills and self-efficacy, motivation to avoid unsafe sex, HIV knowledge, and couple communication.
In total the study consisted of eight visits. The intervention comprised an orientation session plus five sessions which couples attended together and one gender-specific group session which individuals attended alone, for a total of seven sessions plus one final assessment visit. The intervention addressed couples’ HIV/STI risk behaviors, knowledge, relationship communication skills, gender and power dynamics, and safer sex negotiation skills. It emphasized the importance of communication, negotiation, and problem-solving skills, and how relationship dynamics may be affected by gender roles and expectations. Each session included didactic and experiential materials and several exercises. Participants developed and revised behavior change goals at each session. We added the gender specific group session to the intervention based on findings from formative research indicating participants would like an opportunity to discuss gender-specific relationship issues. The main objectives and key concepts of the sessions are described in more detail in Table 1. All sessions were administered in IsiZulu or SeSotho, the predominate languages in the area, and facilitated by a post-graduate psychologist with counseling experience.
Table 1.
Objectives and Key Concepts of Project Connect Sessions
| Session | Objective | Key Concepts |
|---|---|---|
| 1 | Orientation: Increase motivation to attend sessions, discuss pros/cons of participation, raise awareness of risk, reduce anxiety, and clarify misperceptions. | |
| 2 | Introductions/Dialogue/Personal Vulnerability: Increase perceptions of vulnerability to HIV, increase motivation to change, set ground rules and confidentiality procedures, and introduce communication skills and goal setting. STI video and Speaker-Listener modeling video are shown. | • HIV myths and facts • Speaker-Listener Technique (modeling, review and practice of communication) • Goal setting |
| 3 | Positive Change/Our Sexuality/Safer Sex and Loving Relationships: Identify how HIV and other STIs can affect couples in long-term relationships, identify positive changes couples have made, introduce issues of human sexuality and gender conflict in relationships, discuss importance of safer sex practices in the context of a loving relationship, identify range of low, moderate and high risk sexual behaviors on the safer sex scale, and identify where the couple fall on the scale and where they would like to be. | • Safer sex scale (couples rank sexual behaviors from high to low risk) • Speaker-Listener Technique |
| 4 | Risk Reduction Skills: Introduce concept of unwritten rules, explore how unwritten rules influence safer sex behavior, discuss male and female anatomy, discuss condom and lubricant types, learn and practice correct use of male and female condoms, and increase comfort discussing safer sex activities. | • Unwritten rules (gender expectations of how others should act in different situations and how we will act, particularly with regard to sex) • Connection Cafe (menu of safer sex activities to help couples discuss what pleases them sexually and explore new ways to provide pleasure to each other in their relationship) |
| 5 | Partner Negotiation for Safer Sex: Identify personal triggers for unsafe behavior, apply problem-solving techniques to reduce/avoid triggers, make a specific plan to reduce or avoid risk, learn about HIV testing as a risk reduction strategy and review details of testing and how to get pregnant safely, and recommit to safer sex and prevention promotion. Triggers and problem solving videos are shown. | • Triggers for unsafe sex • Problem solving techniques |
| 6 | Relapse Prevention/Maintenance/Resource Enhancement and Social Support Building: Elicit what the couple have learned, reinforce the couple's intention to continue the work they have begun toward taking care of each other's health, reinforce the couple's intention to be prevention promoters in their community, renew their commitment to safer sex behavior, and identify skills learned and resources for the couple after they complete Connect. | • Social support networks • Problem solving skills, Speaker-Listener Technique, and self-talk (positive thoughts to encourage change and cope with slips) to prevent relapse |
| 7 | New Group Session: Introduce the single sex group as a safe place to discuss issues particular to women/men, provide a network of peers who can provide support for issues that are difficult to discuss in a couple. | • Concurrency • Sexual rights and responsibilities • Healthy and unhealthy relationships |
The feasibility and acceptability of the intervention was evaluated using data from session feedback forms, which participants completed after each session. Specifically, participants were asked whether key concepts in the session were covered, if the session was helpful, what they liked most and least, what they learned, whether participants felt comfortable and satisfied with the sessions, and whether any social harms had occurred as a result of the intervention. At the final visit, couples separately completed an interviewer administered questionnaire to assess changes in condom use skills and self-efficacy, motivation to avoid unsafe sex, HIV knowledge, and couple communication. Couples also participated in a joint in-depth interview that addressed their experiences participating in Connect: including what they learned, what was most helpful, how their relationship has changed as a result of participation, and potential improvements to Connect for this population. Interviews were recorded, translated and transcribed into English. A code book was developed deductively based on the interview topic guide and inductively from initial reading of transcripts. Coding was completed in Atlas.ti by two of the authors after initial double coding had ensured intercoder reliability. Each member of the couple was reimbursed R150 (about 17 USD) per study visit.
Results
Feasibility
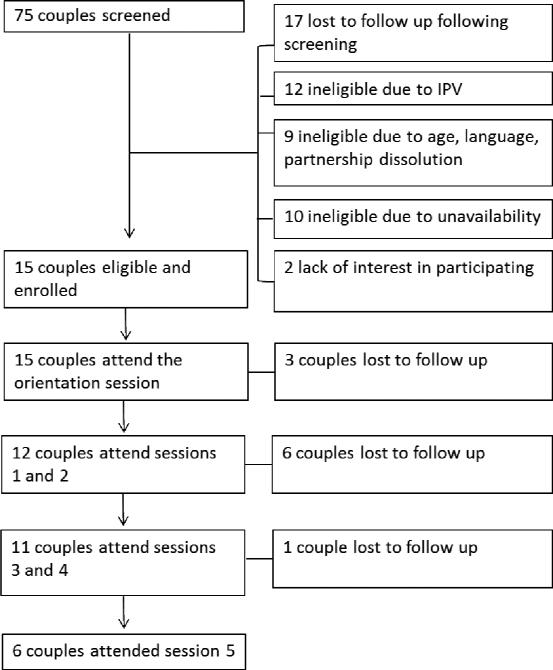
Overall, we screened 75 couples for eligibility and enrolled 15 couples (Figure 1). The primary reasons for study ineligibility were IPV (20.0%, n=12) and loss to follow up after screening (28.3%, n=17). Other main reasons screened couples did not enroll included: age (8.3%, n=5), unavailability to attend sessions (16.7%, n=10), partner died or the relationship ended (15.0%, n=9) and lack of interest (3.3%,n=2).
Figure 1.
Flow chart of study screening, enrollment, and participation
Enrolled men were on average 27 years of age while women were 24. Approximately half of participants had completed at least secondary school (53.3% among men and 46.7% among women). Self-reported HIV prevalence was 28% in men and 13% in women. Approximately two-thirds of the couples were seroconcordent at baseline (53.3% were both HIV negative, 13.3% were both HIV positive), while a smaller proportion were sero-discordent (13.3%) or had unknown HIV status (20.0%). Men reported an average of 5.8 sexual partners in the past year while women reported 6.1 partners; among participants who reported more than one sexual partner 9.1% of men (n=1/11) and 14.3% of women (n=1/6) reported concurrent sexual partnerships in the past year.
Of the 15 couples enrolled, each couple attended, on average, five of the seven intervention sessions. All 15 couples attended the first session (orientation); of these, twelve couples attended the second and third sessions; of these, 11 attended the fourth and fifth sessions; and of these, six couples attended the sixth session. At least one member from 10 of the couples attended the additional gender-specific session (seventh session); five couples completed both single gender sessions. In-depth interviews (IDIs) were conducted with 10 of the 15 original couples at the conclusion of the intervention. Couples who withdrew from the study after enrolment reported scheduling conflicts (n=3), relationship dissolution (n=3), and moving outside the study area (n=2).
Acceptability and Perceived Efficacy
Overall, all the couples reported that they enjoyed participating in Connect, felt comfortable with the program content and facilitator, felt that the sessions met their expectations, and learned a number of new skills. No participants reported disliking any of the sessions. With respect to key skills acquired, participants reported learning how to better communicate with their partner and problem solve, how to more effectively address and prevent HIV/STI risk, and how to develop and identify community and peer support for these behaviors. These changes were reflected in the post-intervention questionnaires; we defined improvement as having at least one partner report safer sexual behavior from baseline to follow-up. Of the 10 couples who completed the pre/post questionnaire and participated in at least the first three sessions, 7 reported greater condom use skills, 10 reported fewer condom use barriers, 9 reported greater condom use self-efficacy or maintained high efficacy, and 9 reported greater average condom use or maintained consistently high condom use after completing the intervention. Additionally, 4 couples reported greater motivation to avoid unsafe sex, 9 reported improved HIV knowledge or maintained a high level of knowledge, and 7 reported improvements in couple communication.
Improved Communication and Conflict Resolution Skills
The majority of couples reported that one of the major benefits of Connect was learning to better communicate and resolve conflict with their partner. Specifically, couples reported enjoying the Speaker-Listener Technique, which provided couples with opportunities to demonstrate both listening and clarify understanding. Prior to Connect, couples reported poor communication, conflict, and problems resolving relationship issues. For example, one woman noted that “before [Connect], we never communicated [...], we just fought and decided to keep quiet and we never talked to each other until it resolved itself without solving anything. But now we talk about it [and have learned] that in a relationship, communication is the best”. Although some couples reported difficulty using the technique at home or when one partner was angry, couples maintained that they planned to continue practicing the Speaker-Listener Technique once Connect had ended.
Couples also reported learning strategies for resolving conflict. For example, through the Problem Solving exercise, couples learned “how to solve our problems without violence”. Similarly, couples reported that the Self-Talk exercises were useful in helping them talk through their problems internally and address challenges calmly. For example, one participant reported learning that “in order to solve a problem, one needs to sit and reflect first and not jump to conclusions and fight”.
Improved STI/HIV Prevention
Participants reported acquiring basic knowledge about STI and HIV transmission and developing prevention skills, such as how to use condoms correctly, negotiate condom use and reduce partner numbers, as a result of participating in Connect. The STI video was very popular among participants, despite the fact that it was developed for audiences in the US. One woman noted that “what made us do things incorrectly was the lack of knowledge. When you don't have the right information at times you tend to do things incorrectly but at least when you get knowledge then you will know what to do”. In addition, couples reported feeling empowered to make safer sexual decisions. For example, one female participant in a discordant relationship reported that “I saw that we are a discordant couple [and] sometimes I was a little afraid I might also have HIV. But now I know how to protect myself”.
With respect to learning STI and HIV prevention skills, participants reported most enjoying activities that provided more nuanced and detailed information and skills about STI and HIV prevention, that provided choices to individuals so that risk reduction plans could be tailored to their respective relationship needs, and that addressed pleasure and sexual satisfaction. Couples reported that demonstrations that taught proper condom use skills and learning male and female anatomy were most helpful. One woman reported that her favorite activity was the condom demonstration because “we learnt like parts of our body and we learnt how to use a condom, about the expiry date, and we didn't know about that but now we know. We also learnt how to insert a condom and that before you insert a condom you must make sure that the air is out of the condom. And how to take off the condom.” Sessions that introduced different strategies for identifying high risk sexual situations and taught participants problem solving were also popular. For example, one participant reported that they now store condoms in a “reachable place” after identifying lack of access to condoms as a trigger for unprotected sex. Couples also reported enjoying the Connection Café Menu which provided information for improving partner satisfaction and taught participants new ways to make safe sex exciting within their current relationship. For example, one participant mentioned that “the connection menu [...] gave us alternatives to the way we normally have sex, it was nice to see other options that we can use“.
Participants reported reducing their STI/HIV risk by communicating about prevention more openly with their partner, and learning to be more equitable when making decisions about using and being responsible for carrying condoms. After participating in Connect, couples reported using condoms more consistently, stating that using condoms “shows that your partner cares about you”, “[we] enjoy sex more when [we] use a condom”, and that “it should not only be one person making the decisions about wearing condoms”.
Gender Specific Session
One key difference between the original Connect program and the program implemented in the pilot study was the inclusion of a gender-specific group session. Although both men and women found the gender-specific sessions acceptable and reported enjoying them, women were more likely than men to attend the sessions. Women, in particular, reported feeling empowered by the experience, noting for example, that they “liked the fact that we were all women advising each other”. One woman reported that she “learned that it is important to share problems with peers because they may be going through similar challenges too.”
Discussion
In this pilot of Project Connect conducted among young couples in inner-city Johannesburg, we found that the couples-based intervention was acceptable and showed signs of limited efficacy. Overall, couples reported enjoying the intervention and reported benefits in improved communication in their relationships and in reducing HIV risk behaviors. However, there were some elements of the intervention, as implemented, that would need to be modified to make wider implementation feasible in resource-constrained settings.
Beyond general acceptability of the intervention, participants reported some perceived efficacy of the intervention. Improved communication and problem-solving were reported as the most important skills acquired by participants, and they associated these skills with reducing risk in their relationships. This finding is consistent with prior research with young South Africans, demonstrating that communication with partners about condom use is one the strongest predictors of using condoms (Hendriksen, Pettifor, Lee, Coates, & Rees, 2007). Some participants also attributed a reduction in relationship violence to the effective communication skills they learned through Connect. Although these findings are promising, it is important to note that the extremely small sample size of the pilot limits the generalizability of the results.
There were a number of issues that influenced the feasibility implementing Project Connect. Overall, there were too many sessions; even with reimbursement for each visit, some participants were unable to attend multiple sessions. We recommend that future interventions offer fewer sessions. Based on feedback from participants, it seems that the sessions which focused on communication skills, problem-solving and HIV prevention skills were most helpful.
From a context perspective, many participants engaged in shift work, which made formal scheduling challenging. We also found many couples were unavailable during weekdays. Offering couples counseling in the evenings and weekends, and perhaps in non-clinical settings such as churches or NGOs, could improve accessibility. Further, new technology may allow interventions such as this to be delivered electronically, allowing greater flexibility and thus compliance with the intervention (Ybarra & Bull, 2007). While integrating couples interventions into couples HCT may make such interventions more feasible, the low rates of male participation in traditional health services might limit the potential to scale up such interventions. Research is needed to identify the best venues through which couples interventions can be delivered to reach large numbers of men and women.
We found that a large proportion of screened couples reported a history of IPV with their current partner at baseline. While there was a priori concern about enrolling couples with a history of IPV, there was no evidence that the intervention precipitated violence. In fact, couples mentioned that the intervention taught them to communicate more effectively, allowing them to discuss issues rather than resorting to violence. Given the prevalence of IPV in South Africa and elsewhere, future couples-based interventions should explore the potential benefits of screening for and specifically addressing IPV. This is particularly important given the evidence supporting IPV as a risk factor for HIV (Jewkes, Dunkle, Nduna, & Shai, 2010; Joyner & Mash, 2011; Seedat, Van Niekerk, Jewkes, Suffla, & Ratele, 2009).
Importantly, we found that many of the techniques used in Project Connect sessions were acceptable and appeared to be feasible. We were concerned that some of concepts such as the Speaker-Listener-Technique, which is based in marital therapy, might be perceived as too “Western” and inappropriate for this setting. We found the opposite; participants reported liking this technique and other problem-solving techniques such as “self-talk” and learning about “triggers.” We believe such skills are a necessary precursor to enabling couples to disclose HIV status – a particularly challenging element of safer sex. For the same reason, we were concerned that participants may not relate to the video demonstrations of techniques. However, this did not appear to reduce enthusiasm or understanding of these tools. Importantly, couples identified the helpfulness of learning basic anatomy, condom use demonstrations, and HIV risk behaviors, underscoring the importance of quality HIV education that is skills based.
Conclusions
We found that an intervention designed for couples to reduce HIV risk was acceptable among this population of young, urban South Africans. Couples reported that the intervention strengthened communication and helped them to identify and reduce HIV risk. Feasibility of the intervention was problematic due to the number and timing of sessions. Future interventions for couples in settings such as this should consider reducing session numbers; emphasizing communication, problem solving, risk identification and reduction. In addition, including couples who report IPV and addressing the interface between IPV and HIV risk could be important in settings with high IPV prevalence.
Table 2.
Baseline demographics of South African couples participating in Project Connect
| Men (n=15) | Women (n=15) | |
|---|---|---|
| Mean age (SD) | 27.07 (3.71) | 24.00 (3.25) |
| Education, n (%) | ||
| Some primary school | 1 (6.66%) | 0 (0%) |
| Some secondary school | 6 (40%) | 8 (53.33%) |
| Completed secondary school | 6 (40%) | 5 (33.33%) |
| Higher education | 2 (13.33%) | 2 (13.33%) |
| HIV positive, n (%) | ||
| No | 9 (60%) | 12 (80%) |
| Yes | 4 (27.67%) | 2 (13.33%) |
| Status unknown | 2 (13.33%) | 1 (6.66%) |
| Couple HIV status, n (%)1 | ||
| Sero-concordent, HIV positive | 2 (13.33%) | |
| Sero-concordent, HIV negative | 8 (53.33%) | |
| Sero-discordent | 2 (13.33%) | |
| Status unknown | 3 (20%) | |
| Mean number of sexual partners in the past year | 5.75 | 6.12 |
| Concurrent partner in the past year1 | 1 (9.09%) | 1 (14.29%) |
Only individuals who reported more than one sexual partner in the past year were asked about concurrency
Acknowledgements
We would like to thank Dr. Nora Rosenberg for her help in setting up this project, Zanele Dubazana who counseled all of the couples as part of the study, and Dr. Nabila El-Bassel and colleagues at Columbia University who provided training to our team and helpful advice when planning this study.
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number 5R21HD058288-02. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health
Appendix
Appendix 1.
Screening tool used to assess intimate partner violence for Project Connect.
| Answer | |
|---|---|
| 0 = This has never happened. | |
| 1 = This has not happened in the past six months, but it has happened. | |
| 2 = This has happened at least one time in the past six months. | |
| 1. My partner twisted my arm or hair, or threw something at me that could hurt me | |
| 2. I did this to my partner | |
| 3. My partner pushed, grabbed, or slapped me | |
| 4. I did this to my partner | |
| 5. My partner used threats to make me have oral or anal sex | |
| 6. I did this to my partner | |
| 7. My partner kicked me, slammed me against a wall, punched me or hit me with something that could hurt | |
| 8. I did this to my partner | |
| 9. My partner beat me up, burned or scalded me on purpose | |
| 10. I did this to my partner | |
| 11. My partner choked me, or used a knife or gun on me | |
| 12. I did this to my partner | |
| 13. My partner used force, like hitting, holding me down, or using a weapon, to make me have sex | |
| 14. I did this to my partner |
*Participants who answered yes to questions 7-14 of the screening questionnaire were excluded from the study and referred for care.
References
- Burton J, Darbes LA, Operario D. Couples-focused behavioral interventions for prevention of HIV: systematic review of the state of evidence. AIDS Behav. 2010;14(1):1–10. doi: 10.1007/s10461-008-9471-4. doi: 10.1007/s10461-008-9471-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coburn BJ, Gerberry DJ, Blower S. Quantification of the role of discordant couples in driving incidence of HIV in sub-Saharan Africa. Lancet Infect Dis. 2011;11(4):263–264. doi: 10.1016/S1473-3099(11)70080-9. doi: 10.1016/s1473-3099(11)70080-9. [DOI] [PubMed] [Google Scholar]
- Curran K, Baeten JM, Coates TJ, Kurth A, Mugo NR, Celum C. HIV-1 prevention for HIV-1 serodiscordant couples. Curr HIV/AIDS Rep. 2012;9(2):160–170. doi: 10.1007/s11904-012-0114-z. doi: 10.1007/s11904-012-0114-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denison JA, O'Reilly KR, Schmid GP, Kennedy CE, Sweat MD. HIV voluntary counseling and testing and behavioral risk reduction in developing countries: a meta-analysis, 1990--2005. AIDS Behav. 2008;12(3):363–373. doi: 10.1007/s10461-007-9349-x. doi: 10.1007/s10461-007-9349-x. [DOI] [PubMed] [Google Scholar]
- Dunkle KL, Stephenson R, Karita E, Chomba E, Kayitenkore K, Vwalika C, Allen S. New heterosexually transmitted HIV infections in married or cohabiting couples in urban Zambia and Rwanda: an analysis of survey and clinical data. Lancet. 2008;371(9631):2183–2191. doi: 10.1016/S0140-6736(08)60953-8. [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Witte S, Wu E, Hunt T, Remien RH. Couple-based HIV prevention in the United States: advantages, gaps, and future directions. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):S98–101. doi: 10.1097/QAI.0b013e3181fbf407. doi: 10.1097/QAI.0b013e3181fbf407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Witte SS, Gilbert L, Wu E, Chang M, Hill J, Steinglass P. The efficacy of a relationship-based HIV/STD prevention program for heterosexual couples. Am J Public Health. 2003;93(6):963–969. doi: 10.2105/ajph.93.6.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Witte SS, Gilbert L, Wu E, Chang M, Hill J, Steinglass P. Long-term effects of an HIV/STI sexual risk reduction intervention for heterosexual couples. AIDS Behav. 2005;9(1):1–13. doi: 10.1007/s10461-005-1677-0. [DOI] [PubMed] [Google Scholar]
- Gray R, Ssempiija V, Shelton J, Serwadda D, Nalugoda F, Kagaayi J, Wawer MJ. The contribution of HIV-discordant relationships to new HIV infections in Rakai, Uganda. AIDS. 2011;25(6):863–865. doi: 10.1097/QAD.0b013e3283448790. doi: 10.1097/QAD.0b013e3283448790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriksen ES, Pettifor A, Lee SJ, Coates TJ, Rees HV. Predictors of condom use among young adults in South Africa: the Reproductive Health and HIV Research Unit National Youth Survey. Am J Public Health. 2007;97(7):1241–1248. doi: 10.2105/AJPH.2006.086009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376(9734):41–48. doi: 10.1016/S0140-6736(10)60548-X. doi: S0140-6736(10)60548-X [pii]10.1016/S0140-6736(10)60548-X. [DOI] [PubMed] [Google Scholar]
- Joyner K, Mash RJ. The value of intervening for intimate partner violence in South African primary care: project evaluation. BMJ Open. 2011;1(2):e000254. doi: 10.1136/bmjopen-2011-000254. doi: 10.1136/bmjopen-2011-000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seedat M, Van Niekerk A, Jewkes R, Suffla S, Ratele K. Violence and injuries in South Africa: prioritising an agenda for prevention. Lancet. 2009;374(9694):1011–1022. doi: 10.1016/S0140-6736(09)60948-X. doi: 10.1016/s0140-6736(09)60948-x. [DOI] [PubMed] [Google Scholar]
- Stevens W, Akkers E, Scott L, Myers M, Motloung T, Pilcher C, Venter F. High Prevalence of Acute, undetected HIV infection in a Primary Care Clinic in South Africa.. Paper presented at the International AIDS Society Conference on Pathogenesis and Treatment; Rio De Janeiro, Brazil. Jul, 2005. [Google Scholar]
- UNAIDS Report on the global AIDS epidemic. 2010 [Google Scholar]
- Ybarra ML, Bull SS. Current trends in Internet- and cell phone-based HIV prevention and intervention programs. Curr HIV/AIDS Rep. 2007;4(4):201–207. doi: 10.1007/s11904-007-0029-2. [DOI] [PubMed] [Google Scholar]