Abstract
Importance
Relatively little is known about the prevalence of body shape concerns and disordered eating among males, and their relations to subsequent adverse outcomes.
Objective
To investigate whether males with eating and shape concern-related psychopathology are more likely to become obese, start using drugs, drinking frequently, or develop high depressive symptoms.
Design
Prospective cohort study
Setting
Growing Up Today Study data collected by questionnaire every 12–36 months.
Participants
5527 males, aged 12–18 in 1999, from across the United States.
Main outcome measures
Becoming obese, starting to use drugs, starting to binge drink at least monthly, and developing high depressive symptoms.
Results
Between 1999 and 2011, in at least one year of study, 9.2% reported high concerns with muscularity but no bulimic behaviors; 2.4% high concerns with muscularity and used supplements, growth hormone or steroids to achieve their desired physique; 2.5% high concerns with thinness but no bulimic behaviors; 6.3% high concerns with both thinness and muscularity; 0.8% had partial or full criteria bulimia nervosa (BN) or purging disorder (PD); 2.9% had partial or full criteria binge eating disorder (BED); and 31% infrequently engaged in binge eating or purging or overeating without a loss of control. BN, PD, and BED were not associated with an increased risk of any outcomes. However, independent of age and BMI, boys with high concerns with thinness, but not muscularity, were more likely to develop high depressive symptoms (Odds ratio (OR)=2.7, 95% confidence interval (CI) 1.4–5.4). Boys with high concerns with muscularity and thinness were more likely than their peers to using drugs (OR=2.1, 95% CI 1.3–3.5) and boys with high muscularity concerns who used supplements and other products to enhance physique were more likely to start binge drinking frequently (OR=2.1, 95% CI 1.6–2.7) and using drugs (OR=2.2, 95% CI 1.5–3.1).
Conclusions
High concerns with muscularity are relatively common among adolescent and young adult males.
Relevance
Males with concerns with muscularity who use potentially unhealthy products to improve their physique are at increased risk of adverse outcomes, but may not be recognized by their clinicians as having a weight-related disorder because of the gender-specific presentation.
Keywords: Eating disorders, adolescents, supplements, muscularity, epidemiology, substance use
At present, most eating disorder research has been conducted among females. Relatively little is known about eating disorders among males. Among adolescent and young adult women in the United States, approximately 0.1–1% have anorexia nervosa (AN) and 1–3% have bulimia nervosa (BN).1,2 Less is known about the prevalence of binge eating disorder (BED), which is an important type of “eating disorders not otherwise specified (EDNOS)” among adolescents and young adults. The prevalence of eating disorders among men is not well known, but is assumed to be much lower.1,3,4 Swanson et al. observed, among 10,123 adolescents, that BN and BED were three times more common among females than males, but the prevalence of partial criteria BED was similar among females and males.4 Moreover, BED is the most common eating disorder among adults1 and the lifetime prevalence of partial or full BED is similar for males (1.6%) and females (2.0%).1
However, rates of eating and weight related disorders probably are being underestimated among males. One core symptom of AN and BN is that weight and shape have an undue influence on a person’s self-evaluation. Among females, these concerns usually present as a strong desire for thinness, but males may be more focused on muscularity. At present, the diagnostic criteria assume that the same symptoms apply to both genders. The frequency of using products, such as anabolic steroids, to increase muscle size and enhance body size are at least as common among males5–7 as purging is among females8, thus suggesting that a willingness to take extreme measures to achieve an ideal physique may be similar among males as females, but that there is a gender difference in the ideal sought and the methods used. Although the Diagnostic and Statistical Manual for Mental Disorders-IV (DSM-IV) criteria are widely used to classify individuals, the eating disorder diagnoses were not empirically defined and may not be equally appropriate for males and females.
Among over 8,500 adolescent and young adult girls in the ongoing Growing Up Today Study (GUTS), we have reported empirical support for a broader range of eating disorders than are currently captured in the DSM-IV or the upcoming DSM-59. The aim of the present investigation was to assess the range of eating and shape concerns and disorders among males, and whether these groups are predictive of developing adverse outcomes thought to be associated with BN in females or becoming obese due to binge eating. We assessed these aims using eight follow-up assessments collected from more than 5500 males who were 12–18 years of age in 1999 and were followed until 2011.
METHODS
GUTS was established in 1996 by recruiting children of women participating in the Nurses’ Health Study II (NHS II). Using the NHS II data, we identified mothers who had children ages 9 to 14. Children whose mothers gave us consent to invite them to participate were mailed an invitation letter and a questionnaire. Additional details have been reported previously.10 A total of 9,039 girls and 7,843 boys returned completed questionnaires, thereby assenting to participate in the cohort. The participants were sent questionnaires in 1996, 1997, 1998, 1999, 2000, 2001, 2003, 2005, 2007, and 2010. The data collection periods in the 2001–2010 spanned approximately 2 years per cycle. The study was approved by the Human Subjects Committee at Brigham and Women’s Hospital and the analyses presented in this manuscript were approved by the Institutional Review Boards at Brigham and Women’s Hospital and Boston Children’s Hospital.
Measures
Eating Disorder Behaviors and Cognitions
Eating disorder behaviors have been assessed on all questionnaires. Weight and shape concerns were assessed with the McKnight Risk Factor Survey (MRFS),11 an instrument designed for and evaluated with preadolescent and adolescent girls. Like females, males may desire to have low body fat, but unlike females thinness may not be considered desirable. Thus to make the MRFS more appropriate for boys, we added the following question: “In the past year, how often have you thought about wanting to have bigger muscles?” (1999) or “toned or defined muscles?” (2001–2005). The muscularity subscale was the mean of questions on wanting bigger or more defined muscles and frequency of worrying about having fat on your body. The desire for thinness subscale was the mean of three questions: “how often have you worried about fat on your body?”, “how often have you thought about wanting to be thinner?”, and “how often have you felt fat?”. Boys were classified as having high concerns with muscularity if their mean response on the subscale was at least 4, which corresponded to responding “a lot” or “always” to the questions. Similarly, boys were classified as having high concerns with thinness if their mean response on the subscale was at least 4.
In 1999, questions were included on the survey that asked how often the participants used a variety of substances, including creatine, DHEA, growth hormone, and anabolic steroids, to improve physical appearance or help gain weight, strength, or muscle mass. Use of these products was assessed again in 2001, 2003, 2005, and 2010. Information from 2005 was carried forward to 2007 in the analysis.
Purging was assessed by asking how often in the past year the boy made himself throw up or used laxatives to keep from gaining weight. Binge eating was assessed with a two-part question. Participants were first asked about the frequency during the past year of eating a very large amount of food. Boys who reported overeating were directed to a question that asked whether they felt out of control during these episodes, like they could not stop eating even if they wanted. Binge eating was defined as eating a very large amount of food in a short amount of time at least monthly and feeling out of control during the eating episode. Both the binge eating and purging questions have been validated in the GUTS cohort.12
Because eating disorders are less common among males, we used the combined partial and full criteria cases into one category. Boys who reported that they engaged in binge eating at least once per month and purged less than monthly were classified as having BED. Boys who reported at least monthly use of vomiting or laxatives to control weight and binged less than monthly were classified as having PD. Boys who engaged monthly in both binge eating and purging were classified as having BN. All reported high concerns with thinness. Boys who engaged in less than monthly binge eating and/or purging and those who went on overeating episodes but did not experience a loss of control were classified as engaging in infrequent disordered eating. We augmented the eating disorder phenotypes to include several types of shape concerns, but not engaging in bulimic behaviors: high concerns with muscularity; high concerns with muscularity and using supplements, growth hormone or anabolic steroids to achieve their desired physique; high concerns with thinness; high concerns with both muscularity and thinness.
Outcomes
Weight Status
Body mass index (BMI) [kg/m2] was calculated using self-reported weight and height assessed on all questionnaires. Among adolescents and young adults, weight change based on serial self-reported weights has been found to underestimate weight change based on measured weights by only an average of 2.1 lbs.13 Height or BMI values detected as outliers14 were set to missing and not used in the analysis. Children and adolescents younger than 18 years were classified as obese based on the International Obesity Task Force (IOTF) cut-offs.15 Males who were 18 years or older with a BMI >30 were classified as obese.
Binge drinking
Binge drinking was assessed in 1999, 2000, 2001, 2003, 2007, and 2010 questionnaires. Children who reported that they ever consumed alcohol were asked a series of questions about their drinking behavior. One of those questions asked about the frequency in the past year of drinking five or more drinks over a few hours, which was our definition of binge drinking among males. Participants who reported at least 12 episodes of binge drinking in the past year were classified as frequent binge drinkers.
Drug use
Questions on drug use were included on the 1999, 2001, 2003, 2007, and 2010 questionnaires. Participants were asked whether they had ever used any of the following drugs in the past year: marijuana or hashish, cocaine, crack, heroin, ecstasy, PCP, GHB, LSD, mushrooms, ketamine, crystal meth, Rohypnol, and amphetamines. Because of an expected cross-sectional association between marijuana and hashish use with overeating episodes, we did not include marijuana or hashish in our drug use outcome. Participants who reported using any of the other drugs and had never reported using any of those drugs at an earlier time period were classified as incident drug users.
Depressive symptoms
In 1999, 2001, and 2003, depressive symptoms were assessed using the six-item validated scale of the McKnight Risk Factor Survey (MRFS) IV.11 All responses were scored on a 5-point Likert Scale ranging from never to always. In 2007 and 2010, the Center for Epidemiologic Studies Depression scale (CESD-10) 16,17 was used instead of the MRFS. Questions from the MRFS were identical or similar to questions included in the CESD. Participants in the top quintile of depressive symptoms were considered cases, thus incident cases of high depressive symptoms were males who were in one of the bottom four quintiles of depression symptoms on one assessment, but in the top quintile on the next assessment.
Sample
Participants were excluded from the analysis if they were female or did not return at least two contiguous assessments between 1999 and 2011 or provide information on bulimic behaviors and weight and shape concerns, thus leaving 5,595 males eligible for the analysis. In addition, males were excluded if they were prevalent cases in all outcomes in 1999 or did not provide information on any of the outcomes after 1999, thus reducing the sample to 5,527 males. In all analyses, participants who were prevalent cases at baseline were excluded and once a participant reported the outcome of interest, he was censored from analyses using subsequent time periods. After these exclusions, 4,748 males remained for the analyses predicting development of obesity, 5,250 males remained for the analyses predicting start of binge drinking at least monthly, 4,031 males remained for the analyses predicting start of using drugs, and 3,441 males remained for the analyses predicting development of high depressive symptoms.
Statistical Analysis
We estimated the probability of the four main outcomes using generalized estimating equations (GEE)18, to account for clustering within family, using PROC GENMOD (SAS version 9.2). Predictors were lagged so outcomes were modeled as a function of predictors from the previous time point. All analyses were adjusted for age. Known predictors of the outcomes were included as covariates in the final models. Participants missing information were excluded from that wave of the analyses, but retained in other years where they provided complete information. These covariates varied by outcome. BMI and dieting were included in models predicting the development of obesity; having a sibling who used drugs, ≥1 friend who use drugs, and ≥1 adult at home who drinks were adjusted for in the models predicting drug use; BMI, having a sibling who started drinking before age 18, ≥1 friend who drinks, ≥1 adult at home who drinks, and region of the country were included in models predicting binge drinking; and BMI and level of depressive symptoms at the prior assessment were adjusted for in the models of high depressive symptoms.
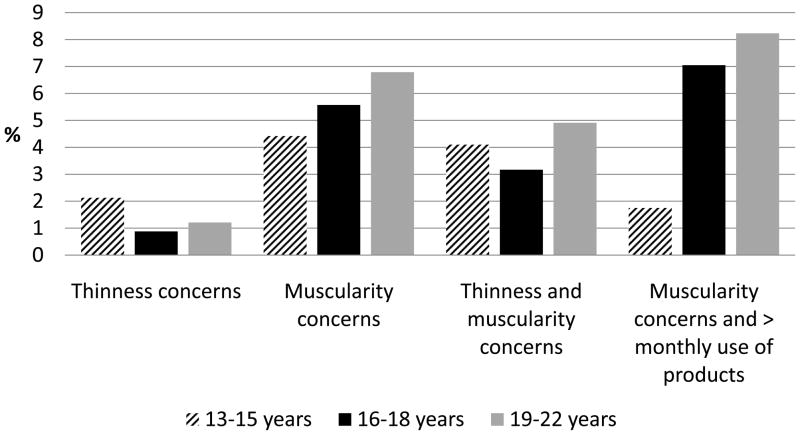
RESULTS
In 1999, the boys were 11 to 18 years of age (Table 1). Less than 1% had partial or full BN, PD, or BED; however, approximately 8.5% were either extremely concerned with their muscularity, concerned with their muscularity and using supplements and other products to improve their physique, or very concerned with both thinness and muscularity. Muscularity concerns with or without using products increased with age, but thinness concerns did not (Figure 1). Between 1999 and 2011, 9.2% reported high concerns with muscularity; 2.4% high concerns with muscularity and used supplements, growth hormone or steroids to achieve their desired physique; 2.5% high concerns with thinness; 6.3% high concerns with both thinness and muscularity; 0.8% had partial or full criteria BN or PD; 2.9% had partial or full criteria BED; and 31% infrequently engaged in binge eating or purging or overeating without a loss of control.
Table 1.
Baseline demographics (mean (S.D) and %) of 5527 adolescent boys in the Growing Up Today Study
| Age (years) | 14.9 (1.6) |
|
| |
| BMI (kg/m2) | 21.4 (3.8) |
|
| |
| Overweight or obese (%) | 26.2% |
|
| |
| Frequently dieting (%) | 4.5% |
|
| |
| Region of residence | |
| Northeast | 34.8% |
| South | 14.3% |
| West | 15.5% |
| Midwest | 35.3% |
|
| |
| High concerns with thinness, but not muscle size or tone* | 1.6% |
|
| |
| High concerns with muscle size or tone, but not thinness* | 2.8% |
|
| |
| High concerns with thinness and muscle size or tone* | 2.7% |
|
| |
| High concerns with muscle size or tone and using creatine, steroids or other products to improve physique* | 3.0% |
|
| |
| Partial or full criteria purging disorder or bulimia nervosa | 0.2% |
|
| |
| Partial or full criteria binge eating disorder | 0.4% |
|
| |
| Infrequent binge eating or purging or overeating, but not experiencing a loss of control | 7.5% |
not engaging in binge eating or purging at least monthly
Figure 1.
Age-group specific prevalence of concerns with weight and shape and use of products to enhance appearance among adolescent and young adult males in Growing Up Today Study
In age-adjusted analyses, all four categories of weight and shape concerns were predictive of an increased risk of becoming obese. However, after adjusting for BMI and dieting frequency, only males with high concerns with thinness, but not muscularity concerns were more likely to become obese (odds ratio (OR)=3.21, 95% confidence interval (CI) 1.44–7.13).
In analyses predicting start of frequent binge drinking, males who were highly concerned with muscularity and used potentially unhealthy products to achieve their desired physique were more likely than their peers to start binge drinking frequently (OR=2.06, 95%CI 1.58–2.69) (Table 2). In addition, males with high concerns with muscularity and thinness (OR=2.13, 95% CI 1.31–3.46) and those with muscularity concern and using products to improve muscle size or strength (OR=2.16, 95% CI 1.49–3.11) were much more likely than their peers to start using drugs. There was little evidence that males with just high concerns with thinness or those with partial or full BN, PD, or BED were at increased risk of starting to binge drink frequently or use drugs, however, there was a suggestion that males with high concerns with muscularity but not using products or supplements might be at increased risk.
Table 2.
Prospective association between eating disorder subtypes and risk of developing adverse outcomes between 1999 and 2011 among 5527 males in the Growing Up Today Study
| Development of Obesity | Starting to binge drink frequently (≥ 12 X/year) | Starting to use drugs | Developing high depressive symptoms | |||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | ||||||||
| Age-adjusted | Multivariablea | Age-adjusted | Multivariableb | Age-adjusted | Multivariablec | Age-adjusted | Multivariabled | |
| Only high concern with thinness | 8.13 (3.71–17.81) | 3.21 (1.44–7.13) | 0.55 (0.29–1.04) | 0.69 (0.35–1.33) | 1.32 (0.56–3.09) | 0.86 (0.28–2.68) | 2.67 (1.39–5.16) | 2.72 (1.36–5.44) |
| Only high concern with muscularity | 1.69 (1.02–2.80) | 1.16 (0.64–2.10) | 1.40 (1.06–1.84) | 1.34 (0.99–1.82) | 1.57 (1.12–2.18) | 1.43 (0.98–2.09) | 1.32 (0.90–1.94) | 1.32 (0.89–1.95) |
| High concern with both thinness and muscularity | 2.62 (1.49–4.58) | 0.90 (0.47–1.73) | 1.40 (1.04–1.88) | 1.26 (0.89–1.80) | 1.71 (1.10–2.65) | 2.13 (1.31–3.46) | 1.53 (0.91–2.57) | 1.56 (0.90–2.71) |
| High concerns w/muscles and use of products | 1.99 (1.31–3.00) | 1.30 (0.79–2.13) | 2.04 (1.59–2.61) | 2.06 (1.58–2.69) | 1.98 (1.42–2.77) | 2.16 (1.49–3.11) | 1.13 (0.77–1.66) | 1.19 (0.81–1.75) |
| Partial or full PD or BN | 2.27 (0.27–18.75) | 1.37 (0.20–9.43) | 0.96 (0.32–2.91) | 0.96 (0.30–3.10) | 1.54 (0.39–6.12) | 2.05 (0.49–8.63) | 2.85 (0.66–12.33) | 2.80 (0.84–9.34) |
| Partial or full BED | 1.09 (0.29–4.09) | 0.57 (0.17–1.99) | 1.04 (0.55–1.98) | 0.67 (0.30–1.49) | 1.62 (0.72–3.63) | 1.76 (0.73–4.24) | 0.93 (0.27–3.13) | 0.93 (0.27–3.15) |
| Infrequent D.E. | 1.38 (1.00–1.91) | 1.18 (0.78–1.77) | 1.15 (0.96–1.37) | 1.09 (0.89–1.33) | 1.07 (0.82–1.39) | 0.97 (0.72–1.31) | 1.30 (1.00–1.68) | 1.28 (0.99–1.67) |
Abbreviations: PD=purging disorder; BN=bulimia nervosa; BED=binge eating disorder; DE=disordered eating
Lagged analysis, using generalized estimating equations, adjusted for age, BMI, and dieting
Lagged analysis, using generalized estimating equations, adjusted for age, BMI, having a sibling who started drinking before age 21, ≥ 1 friend who drinks, ≥ 1 adult at home who drinks, and region of the country
Lagged analysis, using generalized estimating equations, adjusted for age, having a sibling who used drugs, ≥ 1 friend who use drugs, ≥ 1 adult at home who drinks, and region of the country
Lagged analysis, using generalized estimating equations, adjusted for age, BMI, and level of depressive symptoms at the prior assessment
The pattern of association between eating disorder type and risk of developing high depressive symptoms was similar to the pattern observed for the development of obesity. Only males with high concerns with thinness, but not muscularity concerns were more likely than their peers to develop high depressive symptoms (OR=2.72, 95% CI 1.36–5.44). However, there was a suggestion that males who engaged infrequently in bulimic behaviors or who engaged in overeating without a loss of control were also at increased risk (OR=1.28, 95% CI 0.99–1.67).
COMMENT
In this large prospective study of adolescent males, we observed that by young adulthood approximately 2.9% had developed partial or full BED for at least one year, but many more (17%) became extremely concerned with their weight and shape. As expected, more males wanted bigger or more toned and defined muscles rather than thinness, the shape concern that is relatively common among females. Particularly troubling is that, among 16–22 year old males, 7.6% were not only very concerned with muscularity, but also using potentially unhealthy means to achieve their desired physique. These individuals may represent the male equivalent of purging disorder: instead of using extreme weight control behaviors (i.e., vomiting and laxatives) to achieve a desired thin physique, these males may use different extreme and possibly unhealthy behaviors (i.e., creatine, growth hormone, and anabolic steroids) to achieve a desired muscular or toned physique.
Muscularity concerns increased with age. Boys who had high concerns with muscularity and used products to improve their physique were more likely than their peers to start using drugs and binge drinking frequently. In addition, there was a suggestion that boys with these concerns, but not using potentially unhealthy means to achieve their desired physique, were at a slightly lower increased risk of these adverse outcomes. Our results suggest that the failure of most eating disorder assessments to measure concerns with muscularity may result in overlooking a substantial number of males with a potential eating disorder. Currently and in the upcoming DSM-5, eating disorders are grouped as disorders characterized by aberrant eating behaviors (not eating with anorexia nervosa and overeating with BN and BED) in the context of weight and shape-related cognitions (e.g., fat phobia or overvaluation). However, our results suggest that instead the focus should be the cognitive symptoms – undue influence of weight and shape on self-evaluation, which may be the driver of the aberrant eating or use of unhealthy behaviors. Recognizing the clinical relevance of cognitive symptoms (even in the absence of aberrant eating or behaviors to enhance physique) would promote detection of an eating disorder presentation characterized by preoccupation with having larger, toned, or more defined muscles and using potentially unhealthy strategies to achieve the desired physique. Gender differences are well-described in the presentation of other psychiatric disorders, such as attention deficit hyperactivity disorder, and we believe that future revisions to the diagnostic criteria should allow for a gender difference in presentation of eating disorders.
Since our cohort is > 90% white and we have relatively few from low socioeconomic status (SES), it is not clear if the results are generalizable to males of color or from a lower SES. Also, we used validated self-report questionnaires, to assess eating disorder behaviors and cognitions, thus we may have slightly overestimated the number of eating disorder cases and slightly underestimated the associations with adverse outcomes. In addition, although we have collected information on a variety of types of physical activity, we have not measured whether they play on sports teams. However, the study strengths easily outweigh these limitations. This is the largest longitudinal sample of males with repeated assessments of eating disorder and weight and shape concerns. Moreover, it is the first study to prospectively examine the association between eating disorder subtypes, including high concerns with muscularity, and risk of developing a range of adverse outcomes.
In summary, we observed that by late adolescence and young adulthood 7.6% of males were extremely focused on wanting more toned or defined muscles and using potentially unhealthy products at least monthly to improve their physique. This large group has been understudied in research and may be entirely missed by clinicians since they are not captured by the current (DSM-IV) or the upcoming (DSM-5) diagnostic criteria for eating disorders. The DSM-5 criteria are a large improvement, but future revisions will need to expand the diagnoses to better capture presentations more common among males. Until then, clinicians need to be made aware of this large group of males. We encourage researchers to conduct research on this issue so that it’s better understood before the next DSM taskforce begins revisions on the diagnostic criteria.
Acknowledgments
Data collection was supported by research grants from the National Institutes of Health (MH087786, DK59570, DK46200, HL68041, and HD049889), the analysis was supported by MH087786. The authors would like to thank the thousands of participants in the Growing Up Today Study and their mothers.
Footnotes
Financial Disclosures
The authors have indicated they have no financial relationships relevant to this article to disclose.
References
- 1.Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological psychiatry. 2007 Feb 1;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Practice guideline for the treatment of patients with eating disorders (revision) American Psychiatric Association Work Group on Eating Disorders. The American journal of psychiatry. 2000 Jan;157(1 Suppl):1–39. [PubMed] [Google Scholar]
- 3.Patton GC, Selzer R, Coffey C, Carlin JB, Wolfe R. Onset of adolescent eating disorders: population based cohort study over 3 years. Bmj. 1999 Mar 20;318(7186):765–768. doi: 10.1136/bmj.318.7186.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and Correlates of Eating Disorders in Adolescents: Results From the National Comorbidity Survey Replication Adolescent Supplement. Archives of general psychiatry. 2011 Mar 7; doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.vandenBerg P, Neumark-Sztainer D, Cafri G, Wall M. Steroid use among adolescents: longitudinal findings from Project EAT. Pediatrics. 2007 Mar;119(3):476–486. doi: 10.1542/peds.2006-2529. [DOI] [PubMed] [Google Scholar]
- 6.National Institute on Drug A. Anabolic Steroid Abuse. Bethesda, MD: United States Department of Health and Human Services, National Institutes of Health; 2006. [Google Scholar]
- 7.Eisenberg MA, Wall M, Neumark-Sztainer D. Muscle-enhancing behaviors among adolescent girls and boys. Pediatrics. 2012 doi: 10.1542/peds.2012-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Field AE, Javaras KM, Aneja P, et al. Family, peer, and media predictors of becoming eating disordered. Archives of pediatrics & adolescent medicine. 2008 Jun;162(6):574–579. doi: 10.1001/archpedi.162.6.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Field AE, Sonneville KR, Micali N, et al. Prospective association of common eating disorders and adverse outcomes. Pediatrics. 2012 Aug;130(2):e289–295. doi: 10.1542/peds.2011-3663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Field AE, Camargo CA, Jr, Taylor CB, Berkey CS, Roberts SB, Colditz GA. Peer, parent, and media influences on the development of weight concerns and frequent dieting among preadolescent and adolescent girls and boys. Pediatrics. 2001 Jan;107(1):54–60. doi: 10.1542/peds.107.1.54. [DOI] [PubMed] [Google Scholar]
- 11.Shisslak CM, Renger R, Sharpe T, et al. Development and evaluation of the McKnight Risk Factor Survey for assessing potential risk and protective factors for disordered eating in preadolescent and adolescent girls. The International journal of eating disorders. 1999 Mar;25(2):195–214. doi: 10.1002/(sici)1098-108x(199903)25:2<195::aid-eat9>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 12.Field AE, Taylor CB, Celio A, Colditz GA. Comparison of self-report to interview assessment of bulimic behaviors among preadolescent and adolescent girls and boys. The International journal of eating disorders. 2004 Jan;35(1):86–92. doi: 10.1002/eat.10220. [DOI] [PubMed] [Google Scholar]
- 13.Field AE, Aneja P, Rosner B. The validity of self-reported weight change among adolescents and young adults. Obesity (Silver Spring, Md. 2007 Sep;15(9):2357–2364. doi: 10.1038/oby.2007.279. [DOI] [PubMed] [Google Scholar]
- 14.Rosner B. Percentage Points for a Generalized ESD Many-Outlier Procedure. Technometrics. 1983;25(2):165–172. [Google Scholar]
- 15.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000 May 6;320(7244):1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American journal of preventive medicine. 1994 Mar-Apr;10(2):77–84. [PubMed] [Google Scholar]
- 17.Radloff L. The Use of the Center for Epidemiological Studies of Depression Scale in Adolescents and Young Adults. J Youth Adoles. 1991;20:149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- 18.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986 Mar;42(1):121–130. [PubMed] [Google Scholar]