Abstract
Angiotensin II (Ang II)-induced vascular injury is exacerbated by high-salt diets. This study examined the effects of high-sodium level on Ang II-induced cell proliferation in rat vascular smooth muscle cells (VSMCs). The cells were cultured in a standard medium containing 137.5 mmol l−1 of sodium. The high-sodium medium (140 mmol l−1) contained additional sodium chloride. Extracellular signal-regulated kinase (ERK) 1/2 phosphorylation was determined by western blot analysis. Cell proliferation was evaluated by [3H]-thymidine incorporation. Ang II (100 nmol l−1) significantly increased ERK 1/2 phosphorylation and cell proliferation in the both medium containing standard sodium and high sodium. High-sodium level augmented Ang II-induced ERK 1/2 phosphorylation and cell proliferation compared with standard sodium. Pre-treatment with candesartan (1 μmol l−1, Ang II type 1 receptor blocker) or PD98095 (10 μmol l−1, ERK kinase iinhibitor) abolished the proliferative effect induced by high sodium/Ang II. Pre-treatment with 5-N,N-hexamethylene amiloride (30 μmol l−1, Na+/H+ exchanger type 1 (NHE-1) inhibitor), but not SN-6 (10 μmol l−1, Na+/Ca2+ exchanger inhibitor) or ouabain (1 mmol l−1, Na+/K+-ATPase inhibitor) attenuated ERK 1/2 phosphorylation or cell proliferation. Osmotic pressure or chloride had no effect on Ang II-induced proliferative changes. High-sodium level did not affect Ang II receptor expression. Ang II increased intracellular pH via NHE-1 activation, and high-sodium level augmented the pH increase induced by Ang II. These data suggest that high-sodium level directly augments Ang II-induced VSMC proliferation through NHE-1- and ERK 1/2-dependent pathways and may offer new insights into the mechanisms of vascular remodeling by high-sodium/Ang II.
Keywords: angiotensin II, intracellular pH, NHE-1, sodium, vascular remodeling
INTRODUCTION
Sodium homeostasis is a critical morbidity and mortality factor in patients with cardiovascular diseases. Clinical studies have shown that a high-salt diet increases the risks of cardiovascular and cerebrovas-cular diseases, independent of other risk factors including blood pressure.1,2 In addition, experimental studies have demonstrated that a high-salt treatment exaggerates the development of hypertension and cardiovascular complications in hypertensive animals.3,4 In normotensive rats, chronic treatment with high-salt diets elicited structural changes in the arterioles, reductions in the microvessel density and impaired relaxation of the skeletal muscle resistance vessels in response to a variety of vasodilator stimuli.5–7
Hansen-Smith et al.8 reported that microvascular rarefaction and profound ultrastructural alterations occur in hypertensive and normotensive animals after only 3 days on a high-salt diet. High-salt-induced vascular complication has been considered to be predominantly caused by hypertension; blood pressure-independent vascular injury has also been reported.1,2,9 Possible molecular mechanisms of high blood pressure-independent salt-induced vascular remodeling have been proposed, such as transforming growth factor-β and nitric oxide production in endothelial cells,10 hypertrophy of cardiovascular cells,11 macrophage infiltration10 and activation of the local renin–angiotensin (Ang) system.12 The mechanism of high-salt-induced vascular smooth muscle cell (VSMC) proliferation, which is involved in the progression of atherosclerosis,13 is unclear.
Ang II has crucial roles in the pathogenesis of vascular remodeling.14 A growing body of evidence indicates that salt treatment augments Ang II-induced vascular remodeling.15,16 We hypothesized that increased extracellular levels of sodium directly augment Ang II-induced pro-atherogenic changes in VSMCs. To test this hypothesis, we examined the effects of sodium on Ang II-induced proliferation in cultured VSMCs. We investigated Ang II-induced intracellular signaling in a medium with different sodium concentrations.
METHODS
Cell culture and treatment
Cells were isolated from the thoracic aorta of male Sprague–Dawley rats by enzymatic digestion as previously described.17 The experimental procedures were performed according to the guidelines for the care and use of animals established by Kagawa University. The cells were grown in 40% minimum essential medium (Na 144.4 mmol l−1: Life Technologies, Carlsbad, CA, USA) plus 60% medium 199 (Na 133.0 mmol l−1: Life Technologies) supplemented with 10% fetal bovine serum (Hyclone Laboratory, Logan, UT, USA), 100 U ml−1 of penicillin (Life Technologies) and 100 μg ml−1 of streptomycin (Life Technologies) at 37 °C under 5% CO2/95% air in a humidified incubator. This medium was used as the standard medium with a sodium concentration of 137.5±1.0 mmol l−1. Medium containing 140 mmol l−1 of sodium was made by adding sodium chloride (Wako, Osaka, Japan) to the standard medium as previously reported.11
After incubation with Ang II, protein or mRNA was extracted as described previously.18 In some experiments, the VSMCs were pre-treated with 10 μmol l−1 PD98095 (an extracellular signal-regulated kinase (ERK) kinase iinhibitor) for 30 min, 100 nmol l−1 of candesartan (Ang II type 1 (AT1) receptor blocker) for 3 h, 10 μmol l−1 of SN-6 (Na+/Ca2+ exchanger inhibitor) for 5 min, 1 mmol l−1 of ouabain (Na+/K+ ATPase inhibitor) for 5 min or 30 μmol l−1 of 5-N,N-hexamethylene amiloride (HMA, Na+/H+ exchanger type 1 (NHE-1) inhibitor) for 1 h.
Western blot analysis
Cells at 80–90% confluence were made quiescent by incubation in a medium containing 0.1% fetal bovine serum for 24 h. The cells were stimulated with agonists in a serum-free medium and lysed, as described previously;19 the solubilized proteins were isolated by centrifugation and quantified by Bradford assay. The proteins were separated using sodium dodecyl sulfate-polyacrylamide gel electrophoresis and transferred to nitrocellulose membranes. After blocking, the blots were incubated with primary antibodies; the blots with embedded infrared dye were visualized with the Odyssey Infrared Imaging System (LI-COR Biosciences, Lincoln, NE, USA). Antibodies to phospho-ERK 1/2 or ERK 1/2 were purchased from Cell Signaling Technology (Beverly, MA, USA), and anti-AT1 receptor antibody was purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). To confirm equal protein loading, each membrane was reprobed with anti-β-actin antibody (Sigma-Aldrich, St Louis, MO, USA). The band intensities were quantified by immunoblot densitometry using NIH ImageJ software (NIH, Bethesda, MD, USA).
Immunoprecipitation
We determined the NHE-1 phosphorylation by co-immunoprecipitation and western blotting, as reported previously.19,20 The protein samples (130 μg) from the VSMCs were immunoprecipitated by overnight incubation with anti-phospho-Ser 14-3-3 antibody (Cell Signaling Technology), followed by western blot analysis with the antibody against NHE-1 (Cell Signaling Technology).
[3H]-thymidine incorporation assay for cell proliferation
Cell proliferation was determined by [3H]-thymidine incorporation, as described previously.18 The VSMCs were counted and seeded into six-well culture plates (1 × 105 cells per well). After 24 h, the medium was changed to standard medium containing 0.1% fetal bovine serum to ensure their quiescence for 24 h. Ang II (100 nmol l−1) was added to medium containing 137.5 or 140 mmol l−1 of sodium for 24 h. The stimulated cells were labeled with 1 μCi ml−1 [3H]-thymidine during the 24 h of culture. After labeling, the cells were washed twice with phosphate-buffered saline and twice with ice-cold 5% trichloroacetic acid to remove unincorporated [3H]-thymidine, solubilized in 500 μl of 0.25 mol l−1 NaOH containing 0.1% sodium dodecyl sulfate and neutralized with HCl. Aliquots of the samples were added to 10 ml of scintillation fluid and counted in a scintillation counter.
Real-time reverse transcriptase-PCR
For the real-time reverse transcriptase-PCR analysis, the total RNAs were extracted using ISOGEN (Nippon Gene, Tokyo, Japan); the complementary DNA (from 1 μg RNA) was synthesized as described previously.21 The expression of mRNA was analyzed using a Light Cycler Fast Start DNA Master SYBR Green I kit (Life Technologies). Reverse transcriptase-PCR was performed using predesigned primers for the AT1a receptor (TaqMan Gene Expression Assays: Life Technologies) and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) primers (F: 5′-TGAACGGGAAGCTCACTGG-3′ and R: 5′-TCCACCACCCTGTTGCTGTA-3′).22 The data were normalized to the expression of GAPDH.
Intracellular pH measurement
For the intracellular pH imaging, VSMCs were grown on two-well glass chamber slides (BD Bioscience, Franklin Lakes, NJ, USA). The cells were incubated with the acetoxymethyl ester of the pH-reporter dye carboxy-SNARF-1 (Life Technologies) at 10 μmol l−1 for 30 min. Excess extracellular dye was washed away with the medium. The pHi dye was excited by a 488 nm argon laser, and fluorescence was detected by confocal microscopy (LSM 700, Carl Zeiss, Oberkochen, Germany) at 580 and 640 nm. The 580/640 nm fluorescence ratio was converted to pHi using a calibration curve. The standard curve was obtained by measuring ratio signals of carboxy-SNARF-1 AM-loading cells in high-potassium buffers (25 mmol l−1 of HEPES, 145 mmol l−1 of KCl, 0.8 mmol l−1 of CaCl2 and 5.5 mmol l−1 of glucose) at different pH levels (pH 6.7, 7.0, 7.3, 7.6 or 7.9) in the presence of 10 μg ml−1 of nigericin (electroneutral H+/K+ ionophore).
Statistical analysis
Values are presented as the mean±s.e. Multiple-group comparisons were made using one-way or two-way analyses of variance, followed by Bonferroni’s test. Student’s t-tests were performed to compare the mean values when the experimental design consisted of two individual groups. Values of P<0.05 were considered statistically significant.
RESULTS
Effect of high-sodium level on Ang II-induced ERK 1/2 phosphorylation and cell proliferation
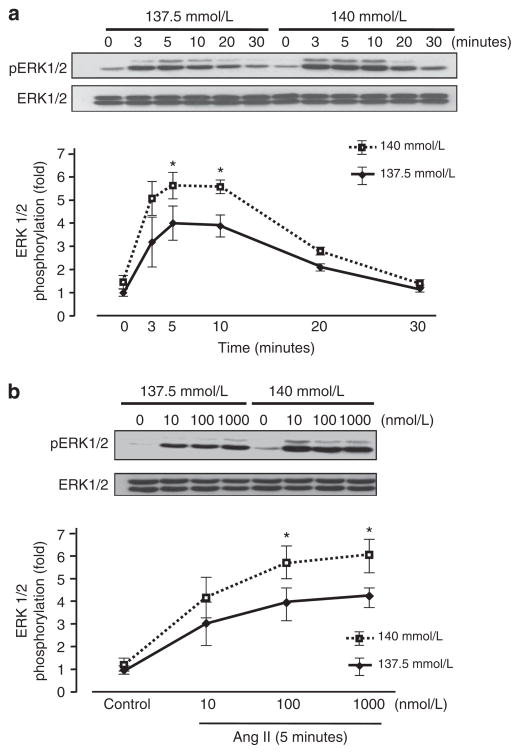
Phosphorylation of ERK 1/2 induced by Ang II was significantly higher in 140 mmol l−1 of sodium than in 137.5 mmol l−1 of sodium (Figure 1a). In addition, 100 or 1000 nmol l−1 of Ang II (5 min)-induced ERK 1/2 phosphorylation was significantly higher in 140 mmol l−1 of sodium than in 137.5 mmol l−1 of sodium (Figure 1b).
Figure 1.
Time course of angiotensin II (Ang II)-induced vascular smooth muscle cell (VSMC) extracellular signal-regulated kinase (ERK) 1/2 phosphorylation in media containing 137.5 and 140 mmol l−1 of sodium (a). VSMCs were incubated with 100 nmol l−1 of Ang II for the indicated times. Dose-dependent change of Ang II-induced ERK 1/2 phosphorylation (b). VSMCs were incubated with the indicated concentrations of Ang II for 5 min. Western blotting was performed with anti-phospho-ERK 1/2 or anti-ERK 1/2 antibody. Data represent the mean±s.e. (n = 4), expressed as fold change compared with the unstimulated cells. Two-way analysis of variance (ANOVA) showed that the time- or dose-dependent increase of ERK 1/2 phosphorylation induced by Ang II was significantly higher in 140 mmol l−1 of sodium than in 137.5 mmol l−1 of sodium. *P<0.05 vs. control VSMCs.
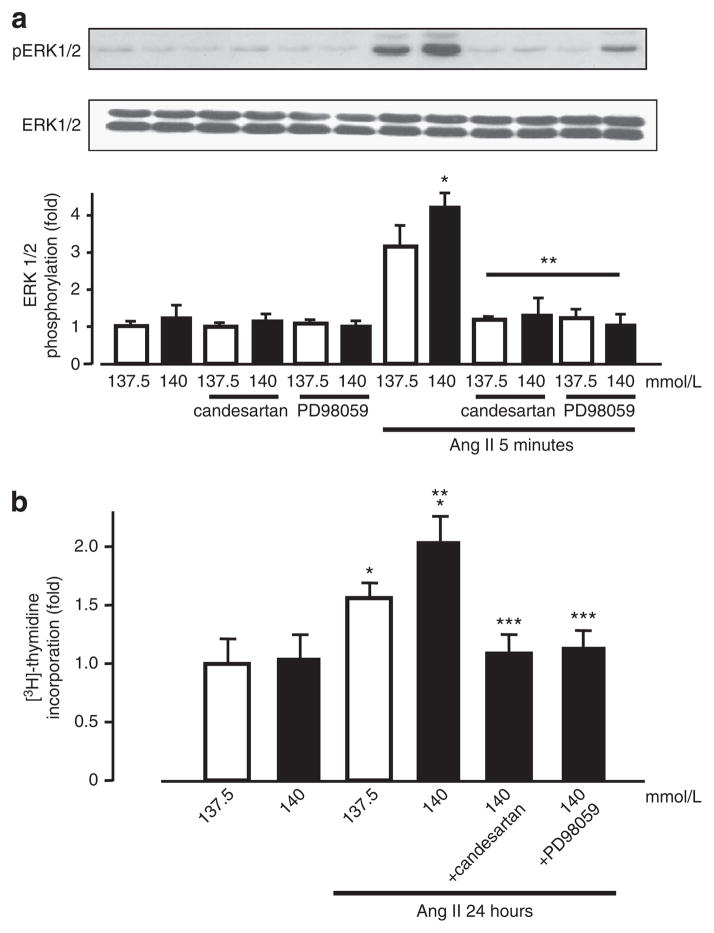
We investigated the potential roles of AT1 receptor and ERK 1/2 activation in high-sodium/Ang II-induced cell proliferation by using candesartan (AT1 receptor blocker) and PD98095 (ERK 1/2 kinase inhibitor). Candesartan and PD98095 inhibited ERK 1/2 phosphor-ylation in 137.5 or 140 mmol l−1 of sodium medium to basal levels (Figure 2a). The Ang II-stimulated cell proliferation was assessed by [3H]-thymidine incorporation. After treatment with Ang II (100 nmol l−1) for 24 h, the [3H]-thymidine incorporation in the 140 mmol l−1 sodium medium was significantly higher than in the 137.5 mmol l−1 sodium medium (Figure 2b). These data suggest that increased extracellular sodium concentration augments Ang II-induced cell proliferation through the AT1 receptor- and ERK 1/2 activation-dependent pathway in the VSMCs.
Figure 2.
Effects of Ang II type 1 (AT1) receptor blocker and extracellular signal-regulated kinase (ERK) 1/2 kinase inhibitor on angiotensin II (Ang II)-induced vascular smooth muscle cell (VSMC) ERK 1/2 phosphorylation (a) and cell proliferation (b) in media containing 137.5 and 140 mmol l−1 of sodium. (a) Western blotting was performed with anti-phospho-ERK 1/2 or anti-ERK 1/2 antibody. (b) Cell proliferation was evaluated by [3H]-thymidine incorporation. Data represent the mean±s.e. (n = 4), expressed as fold change compared with unstimulated cells. *P<0.05 vs. control VSMCs. **P<0.05 vs. Ang II-treated VSMCs in normal sodium medium. ***P<0.05 vs. Ang II-treated VSMCs in high-sodium medium.
Roles of sodium channels in Ang II-induced ERK 1/2 phosphorylation and cell proliferation
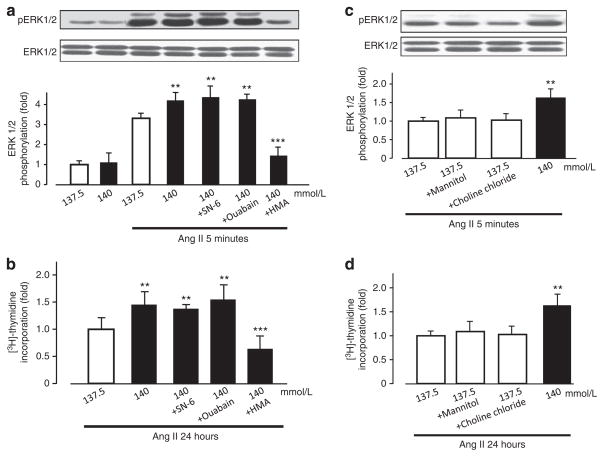
To investigate the roles of different sodium transporters in high-sodium/Ang II-induced ERK 1/2 phosphorylation, we examined the effects of SN-6 (Na+/Ca2+ exchanger inhibitor), ouabain (Na+/K+ ATPase inhibitor) and HMA (NHE-1 inhibitor) on ERK 1/2 phosphorylation and cell proliferation. Whereas HMA completely attenuated high-sodium/Ang II-induced ERK 1/2 phosphorylation (Figure 3a) and cell proliferation (Figure 3b), SN-6 and ouabain showed no effect. A number of studies report that inhibition of ouabain23 or NHE-1,24 is involved in VSMC proliferation. As shown in Supplementary Figure 1, these inhibitors alone have no effect on cell proliferation. Ang II increased NHE-1 phosphorylation, although the sodium concentration did not affect Ang II-induced NHE-1 phosphorylation (Supplementary Figure 2). These data suggest that NHE-1 has a role in the augmentation of Ang II-induced ERK 1/2 phosphorylation with high-sodium level.
Figure 3.
Effects of inhibitors, osmolarity and chloride concentration on angiotensin II (Ang II)-induced vascular smooth muscle cell (VSMC) extracellular signal-regulated kinase (ERK) 1/2 phosphorylation (a, c) and cell proliferation (b, d) in media containing 137.5 and 140 mmol l−1 of sodium. (a, c) Western blotting was performed with anti-phospho-ERK 1/2 or anti-ERK 1/2 antibody. (b, d) Cell proliferation was evaluated by [3H]-thymidine incorporation. Data represent the mean±s.e. (n = 4), expressed as fold change compared with unstimulated cells. *P<0.05 vs. control VSMCs. **P<0.05 vs. Ang II-treated VSMCs in normal sodium medium. ***P<0.05 vs. Ang II-treated VSMCs in high-sodium medium.
Effects of osmolarity and chloride on Ang II-induced ERK 1/2 phosphorylation and cell proliferation
To evaluate the effects of osmolarity on Ang II-induced ERK 1/2 phosphorylation, we used mannitol to obtain the identical osmolarity in the media. The changes in osmolarity by the addition of mannitol showed no effect on Ang II-induced ERK 1/2 phosphorylation and cell proliferation in a normal sodium medium (Figures 3c and d), suggesting that high-sodium level augments Ang II-induced cell proliferation in an osmotic pressure-independent manner.
We measured the effect of chloride concentration on Ang II-induced VSMC proliferation. Choline chloride did not affect ERK 1/2 phosphorylation (Figure 3c) or [3H]-thymidine incorporation (Figure 3d), suggesting that sodium, but not chloride, induces cell proliferation by Ang II.
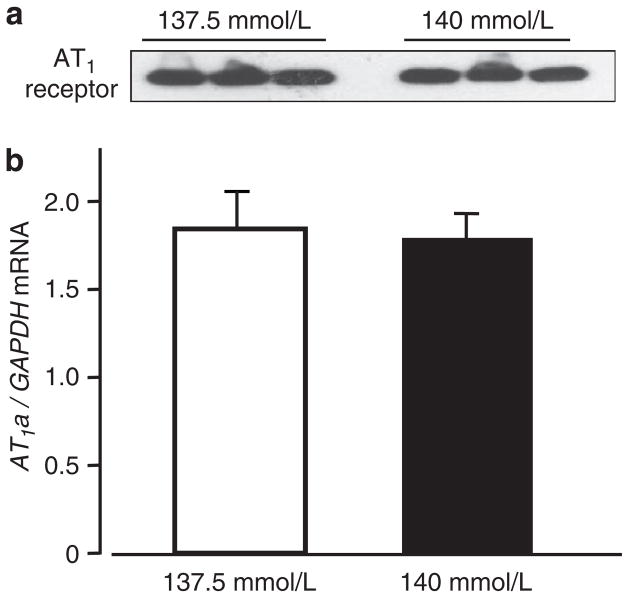
Effect of high-sodium level on expression of the AT1 receptor
After Ang II stimulation for 24 h, protein expression of the AT1 receptor in the normal and high-sodium media did not significantly differ (Figure 4a). The mRNA expression of the AT1a receptor was not affected by sodium (Figure 4b). These data suggested that high-sodium level augments Ang II-induced cell proliferation through the AT1 receptor, but does not change the receptor expression.
Figure 4.
Vascular smooth muscle cell (VSMC) protein expression of angiotensin II type 1 (AT1) receptor in media containing 137.5 or 140 mmol l−1 of sodium (a). Western blotting performed with anti-AT1 receptor antibody. Representative data from three samples are shown. Effect of high sodium on VSMC mRNA expression of AT1a receptor (b). AT1a receptor mRNA was measured by reverse transcriptase-PCR (RT-PCR). The data represent the mean±s.e. (n = 4), normalized to glyceraldehyde-3-phosphate dehydrogenase (GAPDH) mRNA levels.
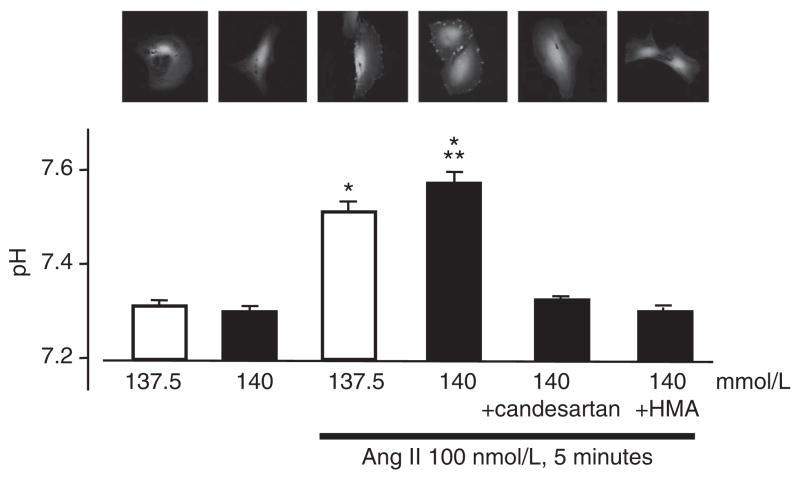
Effect of sodium on intracellular pH in Ang II-treated VSMCs
NHE-1 participates in the regulation of intracellular pH by exchange of Na+ for H+ across the plasma membrane.25 We examined the effect of sodium concentration on intracellular pH in Ang II-treated VSMCs. Ang II (100 nmol l−1, 5 min) significantly increased intracellular pH, and high-sodium level augmented the pH increase induced by Ang II, whereas HMA or candesartan completely inhibited Ang II-induced intracellular pH changes (Figure 5). To confirm the effect of sodium on Ang II-induced VSMC proliferation through NHE-1, we measured the effect of HMA on Ang II-induced changes under normal sodium concentrations. Pre-treatment with HMA inhibited Ang II-induced ERK phosphorylation (Supplementary Figure 3A), thymidine incorporation (Supplementary Figure 3B) and pHi (Supplementary Figure 3C) under normal sodium concentrations; the inhibition is similar to that seen with high-sodium concentrations.
Figure 5.
Effect of sodium on intracellular pH in angiotensin II (Ang II)-treated vascular smooth muscle cells (VSMCs). Cells were incubated with the pH-reporter dye carboxy-SNARF-1. The pHi dye was excited with a 488 nm argon laser, and fluorescence was detected by confocal microscopy at 580 and 640 nm. Intracellular pH was evaluated by the fluorescence ratio using a standard curve. Data represent the mean±s.e. (n = 4). *P<0.05 vs. control VSMCs. **P<0.05 vs. Ang II-treated VSMCs in normal sodium medium. A full color version of this figure is available at the Hypertension Research journal online.
DISCUSSION
The relationship between dietary salt intake and Ang II-induced cardiovascular remodeling has been previously demonstrated in animal and clinical experiments.15,16,26 In Dahl salt-sensitive rats that were fed high levels of salt, treatment with Ang-converting enzyme inhibitors or AT1 receptor blockers did not alter blood pressure, but it did reduce cardiac and/or renal dysfunction.27–29 The precise molecular mechanism by which salt augments Ang II-induced vascular injury has been fully elucidated. In this study, we hypothesized that high-sodium level directly augments Ang II-induced pro-atherogenic changes. Our in vitro study provides evidence that an increased sodium concentration in medium augments Ang II-induced VSMC proliferation through the ERK 1/2-dependent pathway via the AT1 receptor and NHE-1. These findings have implications regarding the molecular mechanisms of Ang II-dependent development and the progression of vascular remodeling in a high-salt diet.
Sodium homeostasis is strictly regulated, particularly the blood sodium concentration. In this study, we assumed high-sodium concentration to be 140 mmol l−1, which is frequently seen in physiological conditions. A recent clinical report clearly revealed that the plasma sodium concentration significantly increased after salt intake,30 suggesting that a high-sodium condition (140 mmol l−1) may be observed in vivo as similar as in this in vitro study. A previous in vivo experiment demonstrated that interstitial sodium concentration differs from the blood sodium concentration and is altered by a high-salt diet.31 The vascular interstitial concentration of sodium might be increased by a high-salt diet.
Ang II increases intracellular calcium ions in the VSMCs.32 The ERK 1/2 activation induced by Ang II has been previously shown to be mediated by at least two pathways; one pathway is Ca2+ dependent, and the other is Ca2+ independent.33–35 To determine whether the augmented effect of high-sodium level on Ang II-induced ERK 1/2 phosphorylation depends on increased intracellular Ca2+ though the sodium–calcium exchange, we used SN-6, a recently developed sodium–calcium exchange inhibitor, to decrease intracel-lular Ca2+.36 The results showed no effect by SN-6 on proliferation or ERK 1/2 phosphorylation, indicating that the augmented effect of high-sodium level on Ang II-induced VSMC proliferation might be Ca2+ independent.
NHE-1 is a member of a multigene family whose activities are increased in the tissues of hypertensive patients37 and animal models.38 As NHE-1 is activated by hyperplastic agonists, it has been proposed that abnormal NHE-1 function is involved in the pathophysiology of hypertension and its complications. Bobik et al.24 and Mitsuke et al.39 have shown that the growth of cultured VSMCs is attenuated by NHE-1 inhibition with pharmacological agents. Despite the increasing interest in the potential role of ERK 1/2 in the activation of NHE-1, several reports suggest that NHE-1 has a role in regulating ERK 1/2 activation. Some evidence supports NHE-1 inhibition suppressing ERK 1/2 phosphorylation in human gut cells40 and cardiomyocytes.41 In this study, Ang II increased NHE-1 phosphorylation and inhibition of NHE-1, and HMA completely attenuated ERK 1/2 phosphorylation and cell proliferation induced by high-sodium/Ang II, suggesting that these changes are regulated by NHE-1. These data are in agreement with previous studies that indicate intracellular pH change via NHE-1 to be a crucial factor in high-salt-induced vascular remodeling.41,42 Although the affinity of NHE-1 for sodium (Km 17.5±3.4 mmol l−1)43 is lower than the sodium concentration in this study (137.5–140 mmol l−1), our results indicate a novel mechanism for NHE-1 activation under high-sodium conditions.
Our study shows that high-sodium concentration augments Ang II-induced VSMC proliferation. A possible molecular mechanism of the upregulated proliferative effect of high-sodium concentration is ERK 1/2 activation via the AT1 receptor and NHE-1. These findings may offer new insights into the molecular mechanisms of atherosclerosis induced by high-sodium/Ang II. Inhibition of NHE-1 might be a novel therapeutic target for vascular remodeling in patients with salt-sensitive hypertension.
Supplementary Material
Acknowledgments
This work was supported by a grant-in-aid for scientific research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (20590253 and 22790792). We are grateful to Takeda for supplying the candesartan. We thank Yoshiko Fujita and Ya Liu for their excellent technical assistance.
Footnotes
Supplementary Information accompanies the paper on Hypertension Research website (http://www.nature.com/hr)
References
- 1.Tuomilehto J, Jousilahti P, Rastenyte D, Moltchanov V, Tanskanen A, Pietinen P, Nissinen A. Urinary sodium excretion and cardiovascular mortality in Finland: a prospective study. Lancet. 2001;357:848–851. doi: 10.1016/S0140-6736(00)04199-4. [DOI] [PubMed] [Google Scholar]
- 2.Ikeda M, Kasahara M, Koizumi A, Watanabe T. Correlation of cerebrovascular disease standardized mortality ratios with dietary sodium and the sodium/potassium ratio among the Japanese population. Prev Med. 1986;15:46–59. doi: 10.1016/0091-7435(86)90035-6. [DOI] [PubMed] [Google Scholar]
- 3.Manning RD, Jr, Hu L, Tan DY, Meng S. Role of abnormal nitric oxide systems in salt-sensitive hypertension. Am J Hypertens. 2001;14:68S–73S. doi: 10.1016/s0895-7061(01)02072-6. [DOI] [PubMed] [Google Scholar]
- 4.Dahl LK, Heine M, Tassinari L. Role of genetic factors in susceptibility to experimental hypertension due to chronic excess salt ingestion. Nature. 1962;194:480–482. doi: 10.1038/194480b0. [DOI] [PubMed] [Google Scholar]
- 5.Liu Y, Rusch NJ, Lombard JH. Loss of endothelium and receptor-mediated dilation in pial arterioles of rats fed a short-term high salt diet. Hypertension. 1999;33:686–688. doi: 10.1161/01.hyp.33.2.686. [DOI] [PubMed] [Google Scholar]
- 6.Frisbee JC, Sylvester FA, Lombard JH. High-salt diet impairs hypoxia-induced cAMP production and hyperpolarization in rat skeletal muscle arteries. Am J Physiol Heart Circ Physiol. 2001;281:H1808–H1815. doi: 10.1152/ajpheart.2001.281.4.H1808. [DOI] [PubMed] [Google Scholar]
- 7.Liu Y, Fredricks KT, Roman RJ, Lombard JH. Response of resistance arteries to reduced PO2 and vasodilators during hypertension and elevated salt intake. Am J Physiol. 1997;273:H869–H877. doi: 10.1152/ajpheart.1997.273.2.H869. [DOI] [PubMed] [Google Scholar]
- 8.Hansen-Smith FM, Morris LW, Greene AS, Lombard JH. Rapid microvessel rarefaction with elevated salt intake and reduced renal mass hypertension in rats. Circ Res. 1996;79:324–330. doi: 10.1161/01.res.79.2.324. [DOI] [PubMed] [Google Scholar]
- 9.Ying WZ, Sanders PW. Increased dietary salt activates rat aortic endothelium. Hypertension. 2002;39:239–244. doi: 10.1161/hy0202.104142. [DOI] [PubMed] [Google Scholar]
- 10.Kanbay M, Chen Y, Solak Y, Sanders PW. Mechanisms and consequences of salt sensitivity and dietary salt intake. Curr Opin Nephrol Hypertens. 2011;20:37–43. doi: 10.1097/MNH.0b013e32834122f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gu JW, Anand V, Shek EW, Moore MC, Brady AL, Kelly WC, Adair TH. Sodium induces hypertrophy of cultured myocardial myoblasts and vascular smooth muscle cells. Hypertension. 1998;31:1083–1087. doi: 10.1161/01.hyp.31.5.1083. [DOI] [PubMed] [Google Scholar]
- 12.Bayorh MA, Ganafa AA, Emmett N, Socci RR, Eatman D, Fridie IL. Alterations in aldosterone and angiotensin II levels in salt-induced hypertension. Clin Exp Hypertens. 2005;27:355–367. [PubMed] [Google Scholar]
- 13.Min LJ, Mogi M, Li JM, Iwanami J, Iwai M, Horiuchi M. Aldosterone and angiotensin II synergistically induce mitogenic response in vascular smooth muscle cells. Circ Res. 2005;97:434–442. doi: 10.1161/01.RES.0000180753.63183.95. [DOI] [PubMed] [Google Scholar]
- 14.Hitomi H, Kaifu K, Fujita Y, Sofue T, Nakano D, Moriwaki K, Hara T, Kiyomoto H, Kohno M, Kobori H, Nishiyama A. Angiotensin II shifts insulin signaling into vascular remodeling from glucose metabolism in vascular smooth muscle cells. Am J Hypertens. 2011;24:1149–1155. doi: 10.1038/ajh.2011.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tojo A, Kimoto M, Wilcox CS. Renal expression of constitutive NOS and DDAH: separate effects of salt intake and angiotensin. Kidney Int. 2000;58:2075–2083. doi: 10.1111/j.1523-1755.2000.00380.x. [DOI] [PubMed] [Google Scholar]
- 16.Sasser JM, Pollock JS, Pollock DM. Renal endothelin in chronic angiotensin II hypertension. Am J Physiol Regul Integr Comp Physiol. 2002;283:R243–R248. doi: 10.1152/ajpregu.00086.2002. [DOI] [PubMed] [Google Scholar]
- 17.Hitomi H, Fukui T, Moriwaki K, Matsubara K, Sun GP, Rahman M, Nishiyama A, Kiyomoto H, Kimura S, Ohmori K, Abe Y, Kohno M. Synergistic effect of mechanical stretch and angiotensin II on superoxide production via NADPH oxidase in vascular smooth muscle cells. J Hypertens. 2006;24:1089–1095. doi: 10.1097/01.hjh.0000226199.51805.88. [DOI] [PubMed] [Google Scholar]
- 18.Nishiyama A, Yao L, Fan Y, Kyaw M, Kataoka N, Hashimoto K, Nagai Y, Nakamura E, Yoshizumi M, Shokoji T, Kimura S, Kiyomoto H, Tsujioka K, Kohno M, Tamaki T, Kajiya F, Abe Y. Involvement of aldosterone and mineralocorticoid receptors in rat mesangial cell proliferation and deformability. Hypertension. 2005;45:710–716. doi: 10.1161/01.HYP.0000154681.38944.9a. [DOI] [PubMed] [Google Scholar]
- 19.Taniyama Y, Hitomi H, Shah A, Alexander RW, Griendling KK. Mechanisms of reactive oxygen species-dependent downregulation of insulin receptor substrate-1 by angioten-sin II. Arterioscler Thromb Vasc Biol. 2005;25:1142–1147. doi: 10.1161/01.ATV.0000164313.17167.df. [DOI] [PubMed] [Google Scholar]
- 20.Snabaitis AK, D’Mello R, Dashnyam S, Avkiran M. A novel role for protein phosphatase 2A in receptor-mediated regulation of the cardiac sarcolemmal Na +/H +exchanger NHE1. J Biol Chem. 2006;281:20252–20262. doi: 10.1074/jbc.M600268200. [DOI] [PubMed] [Google Scholar]
- 21.Moriwaki K, Kiyomoto H, Hitomi H, Ihara G, Kaifu K, Matsubara K, Hara T, Kondo N, Ohmori K, Nishiyama A, Fukui T, Kohno M. Interferon-gamma enhances superoxide production in human mesangial cells via the JAK-STAT pathway. Kidney Int. 2006;70:788–793. doi: 10.1038/sj.ki.5001639. [DOI] [PubMed] [Google Scholar]
- 22.Zhang GX, Ohmori K, Nagai Y, Fujisawa Y, Nishiyama A, Abe Y, Kimura S. Role of AT1 receptor in isoproterenol-induced cardiac hypertrophy and oxidative stress in mice. J Mol Cell Cardiol. 2007;42:804–811. doi: 10.1016/j.yjmcc.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 23.Golomb E, Hill MR, Brown RG, Keiser HR. Ouabain enhances the mitogenic effect of serum in vascular smooth muscle cells. Am J Hypertens. 1994;7:69–74. doi: 10.1093/ajh/7.1.69. [DOI] [PubMed] [Google Scholar]
- 24.Bobik A, Grooms A, Little PJ, Cragoe EJ, Jr, Grinpukel S. Ethylisopropylamiloride-sensitive pH control mechanisms modulate vascular smooth muscle cell growth. Am J Physiol. 1991;260:C581–C588. doi: 10.1152/ajpcell.1991.260.3.C581. [DOI] [PubMed] [Google Scholar]
- 25.Schelling JR, Abu Jawdeh BG. Regulation of cell survival by Na +/H +exchanger-1. Am J Physiol Renal Physiol. 2008;295:F625–F632. doi: 10.1152/ajprenal.90212.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Drenjancevic-Peric I, Jelakovic B, Lombard JH, Kunert MP, Kibel A, Gros M. High-salt diet and hypertension: focus on the renin-angiotensin system. Kidney Blood Press Res. 2011;34:1–11. doi: 10.1159/000320387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sakata Y, Masuyama T, Yamamoto K, Doi R, Mano T, Kuzuya T, Miwa T, Takeda H, Hori M. Renin angiotensin system-dependent hypertrophy as a contributor to heart failure in hypertensive rats: different characteristics from renin angiotensin system-independent hypertrophy. J Am Coll Cardiol. 2001;37:293–299. doi: 10.1016/s0735-1097(00)01064-0. [DOI] [PubMed] [Google Scholar]
- 28.Hayashida W, Kihara Y, Yasaka A, Inagaki K, Iwanaga Y, Sasayama S. Stage-specific differential activation of mitogen-activated protein kinases in hypertrophied and failing rat hearts. J Mol Cell Cardiol. 2001;33:733–744. doi: 10.1006/jmcc.2001.1341. [DOI] [PubMed] [Google Scholar]
- 29.Otsuka F, Yamauchi T, Kataoka H, Mimura Y, Ogura T, Makino H. Effects of chronic inhibition of ACE and AT1 receptors on glomerular injury in dahl salt-sensitive rats. Am J Physiol. 1998;274:R1797–R1806. doi: 10.1152/ajpregu.1998.274.6.R1797. [DOI] [PubMed] [Google Scholar]
- 30.Suckling RJ, He FJ, Markandu ND, Macgregor GA. Dietary salt influences postprandial plasma sodium concentration and systolic blood pressure. Kidney Int. 2012;81:407–411. doi: 10.1038/ki.2011.369. [DOI] [PubMed] [Google Scholar]
- 31.Machnik A, Neuhofer W, Jantsch J, Dahlmann A, Tammela T, Machura K, Park JK, Beck FX, Muller DN, Derer W, Goss J, Ziomber A, Dietsch P, Wagner H, van Rooijen N, Kurtz A, Hilgers KF, Alitalo K, Eckardt KU, Luft FC, Kerjaschki D, Titze J. Macrophages regulate salt-dependent volume and blood pressure by a vascular endothelial growth factor-C-dependent buffering mechanism. Nat Med. 2009;15:545–552. doi: 10.1038/nm.1960. [DOI] [PubMed] [Google Scholar]
- 32.Touyz RM, Schiffrin EL. Signal transduction mechanisms mediating the physiological and pathophysiological actions of angiotensin II in vascular smooth muscle cells. Pharmacol Rev. 2000;52:639–672. [PubMed] [Google Scholar]
- 33.Liao DF, Monia B, Dean N, Berk BC. Protein kinase C-zeta mediates angiotensin II activation of ERK1/2 in vascular smooth muscle cells. J Biol Chem. 1997;272:6146–6150. doi: 10.1074/jbc.272.10.6146. [DOI] [PubMed] [Google Scholar]
- 34.Sadoshima J, Qiu Z, Morgan JP, Izumo S. Angiotensin II and other hypertrophic stimuli mediated by G protein-coupled receptors activate tyrosine kinase, mitogen-activated protein kinase, and 90-kD S6 kinase in cardiac myocytes. The critical role of Ca(2 +)dependent signaling. Circ Res. 1995;76:1–15. doi: 10.1161/01.res.76.1.1. [DOI] [PubMed] [Google Scholar]
- 35.Lucchesi PA, Bell JM, Willis LS, Byron KL, Corson MA, Berk BC. Ca(2 +)-dependent mitogen-activated protein kinase activation in spontaneously hypertensive rat vascular smooth muscle defines a hypertensive signal transduction phenotype. Circ Res. 1996;78:962–970. doi: 10.1161/01.res.78.6.962. [DOI] [PubMed] [Google Scholar]
- 36.Iwamoto T, Inoue Y, Ito K, Sakaue T, Kita S, Katsuragi T. The exchanger inhibitory peptide region-dependent inhibition of Na +/Ca2 + exchange by SN-6 [2-[4-(4-nitrobenzyloxy)benzyl]thiazolidine-4-carboxylic acid ethyl ester], a novel benzyloxyphe-nyl derivative. Mol Pharmacol. 2004;66:45–55. doi: 10.1124/mol.66.1.45. [DOI] [PubMed] [Google Scholar]
- 37.Garciandia A, Lopez R, Tisaire J, Arrazola A, Fortuno A, Bueno J, Diez J. Enhanced Na(+)-H + exchanger activity and NHE-1 mRNA expression in lymphocytes from patients with essential hypertension. Hypertension. 1995;25:356–364. doi: 10.1161/01.hyp.25.3.356. [DOI] [PubMed] [Google Scholar]
- 38.Siczkowski M, Davies JE, Ng LL. Na(+)-H + exchanger isoform 1 phosphorylation in normal Wistar-Kyoto and spontaneously hypertensive rats. Circ Res. 1995;76:825–831. doi: 10.1161/01.res.76.5.825. [DOI] [PubMed] [Google Scholar]
- 39.Mitsuka M, Nagae M, Berk BC. Na(+)-H + exchange inhibitors decrease neointimal formation after rat carotid injury. Effects on smooth muscle cell migration and proliferation. Circ Res. 1993;73:269–275. doi: 10.1161/01.res.73.2.269. [DOI] [PubMed] [Google Scholar]
- 40.Nemeth ZH, Deitch EA, Szabo C, Mabley JG, Pacher P, Fekete Z, Hauser CJ, Hasko G. Na +/H + exchanger blockade inhibits enterocyte inflammatory response and protects against colitis. Am J Physiol Gastrointest Liver Physiol. 2002;283:G122–G132. doi: 10.1152/ajpgi.00015.2002. [DOI] [PubMed] [Google Scholar]
- 41.Takewaki S, Kuro-o M, Hiroi Y, Yamazaki T, Noguchi T, Miyagishi A, Nakahara K, Aikawa M, Manabe I, Yazaki Y, et al. Activation of Na(+)-H + antiporter (NHE-1) gene expression during growth, hypertrophy and proliferation of the rabbit cardiovascular system. J Mol Cell Cardiol. 1995;27:729–742. doi: 10.1016/s0022-2828(08)80063-6. [DOI] [PubMed] [Google Scholar]
- 42.Touyz RM, Schiffrin EL. Activation of the Na(+)-H + exchanger modulates angioten-sin II-stimulated Na(+)-dependent Mg2 + transport in vascular smooth muscle cells in genetic hypertension. Hypertension. 1999;34:442–449. doi: 10.1161/01.hyp.34.3.442. [DOI] [PubMed] [Google Scholar]
- 43.Noel J, Germain D, Vadnais J. Glutamate 346 of human Na +-H + exchanger NHE1 is crucial for modulating both the affinity for Na + and the interaction with amiloride derivatives. Biochemistry. 2003;42:15361–15368. doi: 10.1021/bi035296a. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.