Abstract
Studies of subtypes of DSM-IV attention-deficit/hyperactivity disorder (ADHD) have provided inconsistent support for the discriminant validity of the combined type (ADHD-C) and predominantly inattentive type (ADHD-I). A large sample of children and adolescents with ADHD (N = 410) and a comparison group without ADHD (N = 311) were used to test the internal and external validity of sluggish cognitive tempo (SCT), a dimension characterized by low energy and sleepy and sluggish behavior. SCT scores were then incorporated in analyses of ADHD subtypes to test whether the discriminant validity of ADHD-C and ADHD-Icould be improved by includingSCT symptoms as part of the criteria for ADHD-I. Factor analyses of parent and teacher ratings indicated that six SCT items loaded on a factor separate from symptoms of ADHD and other psychopathology, providing important support for the internal validity of SCT. The external validity of SCT was supported by significant associationsbetween SCT and measures of functional impairment and neuropsychological functioning when symptoms of ADHD and other psychopathology were controlled. However, contrary to initial predictions, high levels of SCT did not identify a subgroup of ADHD-I that was clearly distinct from ADHD-C. Instead, the current results suggest that DSM-IV inattention and SCT are separate but correlated symptom dimensions that are each independently associated with important aspects of functional impairment and neuropsychological functioning.
Keywords: ADHD, sluggish tempo, subtypes, DSM-IV, inattention, hyperactivity-impulsivity
Despite over three decades of research since subtypes of attention-deficit/hyperactivity disorder (ADHD) were first specified in the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III; American Psychiatric Association, 1980), the optimal approach to describe heterogeneity among individuals with ADHD remains unclear. DSM-IV diagnostic criteria for ADHD defined three nominal subtypes based on differential elevations on two dimensions of nine symptoms of inattention and nine symptoms of hyperactivity-impulsivity (American Psychiatric Association, 1994). The Predominantly Inattentive Type (ADHD-I) includes individuals with six or more symptoms of inattention and fewer than six symptoms of hyperactivity-impulsivity, the Predominantly Hyperactive-Impulsive Type (ADHD-H) includes individuals with six or more symptoms of hyperactivity-impulsivity and fewer than six symptoms of inattention, and the Combined Type (ADHD-C) is defined by six or more symptoms on both dimensions.
A comprehensive literature review and meta-analysis of 546 studies was recently completed to evaluate the validity of the DSM-IV model of ADHD (Willcutt et al., 2012). Factor analyses and studies of external correlates overwhelmingly supported the internal and external validity of the inattention and hyperactivity-impulsivity symptom dimensions. In contrast, the review found weak evidence to support the distinction between ADHD-C and ADHD-I in studies of academic and cognitive functioning, longitudinal stability, etiological influences, and treatment response. These results challenged the validity of the DSM-IV subtype model and underscored the need to develop and test new theoretical models that may account for the weak discriminant validity of DSM-IV ADHD-C and ADHD-I.
In DSM-IV and previous editions of the DSM, the inattentive subtypes of ADHD (DSM-III ADD without hyperactivity, DSM-III-R undifferentiated ADD, DSM-IVADHD-I) have always been defined based on the presence of a subset of symptoms of ADHD (i.e., inattention and impulsivity in DSM-III and inattention in DSM-III-R and DSM-IV) in the absence of clinically significant elevations of hyperactivity or hyperactivity-impulsivity. Based on concerns that this approach might contribute to the weak discriminant validity of ADHD-C and ADHD-I, several authors suggested that the validity of a predominantly inattentive subgroupmight be improved by developing positive diagnostic criteria for ADHD-I (e.g., Carlson & Mann, 2002; McBurnett, Pfiffner, & Frick, 2001; Milich, Balentine, & Lynam, 2001).
Sluggish cognitive tempo and its relation to DSM-IV ADHD
One potential candidate for positive diagnostic criteria for ADHD-I is a cluster of behaviors that was first identified by exploratory factor analyses (EFA) of the Children’s Behavior Rating Scale (CBRS; Neeper & Lahey, 1984), a teacher rating scale that included a large pool of items related to developmental psychopathology (Neeper & Lahey, 1986). Many of the seven factors that were extracted were similar to dimensions of psychopathology that had been described previously in the clinical literature (Inattention-Disorganization, Hyperactivity, Conduct Disorder, Anxiety/Depression). In addition, the EFA identified a novel Sluggish Cognitive Tempo (SCT) factor that included five items related to cognitive sluggishness, drowsiness, and lethargic and apathetic behavior (Neeper & Lahey, 1986).
Measures of SCT were then included in several studies that systematically compared the DSM-III ADD subtypes on an extensive range of measures (e.g., Lahey et al., 1988; Lahey, Schaughency, Frame, & Strauss, 1985; Lahey, Schaughency, Hynd, Carlson, & Nieves, 1987; Stanford & Hynd, 1994). Results of these studies indicated that DSM-III ADD with and without hyperactivity were associated with many of the same clinical correlates, but one characteristic that consistently distinguished the subtypes were significantly higher levels of SCT symptoms in children with ADD without hyperactivity.
Based on these results, the DSM-IV field trials tested the utility of two SCT symptoms as part of the provisional diagnostic criteria for ADHD, and confirmed that SCT symptoms were associated most strongly with ADHD-I (Frick et al., 1994). However, due to relatively weak predictive power these symptoms were not included in the final DSM-IV diagnostic criteria for ADHD, and ADHD-I was once again differentiated from ADHD-C by the absence of clinically significant levels of hyperactivity-impulsivity. Nonetheless, the results of the field trials spurred additional interest in SCT, and after DSM-IV was published a number of studies continued to examine the relation between SCT and DSM-IV ADHD symptoms.
Factor analyses of SCT and DSM-IV ADHD
Seven studies have conducted exploratory or confirmatory factor analyses of parent or teacher ratings of SCT and DSM-IV ADHD symptoms (Barkley, 2013; Garner, Marceaux, Mrug, Patterson, & Hodgens, 2010; Hartman, Willcutt, Rhee, & Pennington, 2004; Lahey et al., 2004; McBurnett et al., 2001; Penny, Waschbusch, Klein, Corkum, & Eskes, 2009; Todd, Rasmussen, Wood, Levy, & Hay, 2004; see Willcutt et al., 2012 for a full review). Six of these studies found that at least a subset of putative SCT symptoms had a primary loading on a third factor that was distinct from DSM-IV inattention and hyperactivity-impulsivity symptoms.
These initial factor analytic studies provided important support for the internal validity of SCT, but also had important limitations. Several SCT items are similar to specific symptoms of major depressive disorder (e.g., psychomotor retardation and fatigue or loss of energy) and generalized anxiety disorder (e.g., mind going blank and easily fatigued), and overall SCT scores are significantly correlated with a range of measures of internalizing and externalizing symptoms (Garner et al., 2010; Hartman et al., 2004; Neeper & Lahey, 1986; Penny et al., 2009; Wahlstedt & Bohlin, 2010). Despite these correlations only two previous factor analytic studies of SCT and ADHD included items from other dimensions of psychopathology (Lahey et al., 2004; Neeper & Lahey, 1986).
As described earlier, the study that first described SCT identified an SCT factor that was distinct from six other factors that were similar to DSM-IV symptom dimensions (Neeper & Lahey, 1986). In contrast, a second study did not find an SCT factor in the six-factor solution that emerged from EFA of a parent interview that included items corresponding to ADHD, SCT, and most major domains of DSM-IV psychopathology (Lahey et al., 2004). Instead, five symptoms that were similar to the SCT items that were used in other studies (day-dreamed and lost in thoughts, dawdled and worked slowly, stared into space, took longer to answer than others, difficulty thinking or deciding) had weak loadings (.43–.49) on a factor that included items similar to DSM-IV inattention symptoms, and one potential SCT item (sleepy during the day) had a primary loading on a factor that was labeled Depression. Theseconflicting results underscore the need for additional research to clarify the relations among SCT, DSM-IV ADHD, and other dimensions of psychopathology.
External validity of SCT
For a dimension of psychopathology, significant associations with important aspects of functional impairment provide the most decisive evidence of the external validity and clinical importance of the construct. A handful of studies have reported significant univariate associations between SCT symptoms and measures of academic, social, and neuropsychological functioning (Barkley, 2013; Garner et al., 2010; Hartman et al., 2004; Neeper & Lahey, 1986; Wahlstedt & Bohlin, 2010). However, only a few measures of impairment were included in these studies, and multiple regression analyses suggest that some associations between SCT and impairment may be explained by covariance between SCT and inattention (Barkley, 2013; Wahlstedt & Bohlin, 2010). Additional systematic research is needed to clarify whetherSCT symptoms are independently associated with significant functional impairment.
Sluggish cognitive tempo and the DSM-IV ADHD subtypes
In an attempt to improve the weak discriminant validity of DSM-IV ADHD-I and ADHD-C, several studies have tested whether the presence of high levels of SCT symptoms identify a subgroup of ADHD-I that is more clearly distinct from ADHD-C (e.g., Carlson & Mann, 2002; McBurnett et al., 2001). Consistent with this hypothesis, some initial studies found that the subgroup of ADHD-I with high SCT was significantly different from ADHD-C on some measures of functional impairment (Carlson & Mann, 2002) and selective attention (Huang-Pollock, Nigg, & Carr, 2005), whereas the group with ADHD-I without SCT was not. However, other subsequent studies reported little evidence that levels of SCT moderated the associations between ADHD-I and measures of functional impairment, neuropsychological functioning, or treatment response (e.g., Bauermeister et al., 2005; Harrington & Waldman, 2010; Hinshaw, Carte, Fan, Jassy, & Owens, 2007; Hinshaw, Carte, Sami, Treuting, & Zupan, 2002; Ludwig, Matte, Katz, & Rohde, 2009).
The current study
As part of the ongoing Colorado Learning Disabilities Research Center (CLDRC) twin study, participants who met symptom criteria for DSM-IV ADHD (N = 410) and a comparison group without ADHD (N = 311) completed an extensive battery that included measures of ADHD and SCT, internalizing and externalizing psychopathology, functional impairment, and neuropsychological functioning. These data were used for a series of analyses designed to test the internal and external validity of SCT and its relation with DSM-IV ADHD. The three primary objectives of the study were as follows:
The internal validity of SCT was tested by conducting exploratory factor analyses of nine potential SCT symptoms along with all DSM-IV symptoms of ADHD, oppositional defiant disorder (ODD), conduct disorder (CD), major depressive disorder (MDD), and generalized anxiety disorder (GAD). We hypothesized that at least a subset of putative SCT symptoms would have primary loadings on a factor that was distinct from factors that included symptoms of DSM-IV inattention and hyperactivity-impulsivity or the other dimensions of internalizing and externalizing psychopathology.
After identifying the cluster of SCT items with optimal internal validity, the external validity of SCT was examined by testing if SCT symptoms were associated with significant functional impairment or neuropsychological difficulties. The discriminant validity of SCT and DSM-IV ADHD was then tested by including symptoms of SCT, ADHD, and other psychopathology as simultaneous predictors in multiple regression models predicting each external measure. We tentatively predicted that after controlling for the other variables, SCT symptoms would be independently associated with social isolation, academic difficulties, and slow cognitive processing speed, whereas DSM-IV inattention symptoms would be more strongly associated with externalizing symptoms and weaknesses on executive function measures.
The final set of analyses tested whether the relatively weak discriminant validity of DSM-IV ADHD-C and ADHD-I was improved by subdividing the group with ADHD-I based on SCT symptoms. We hypothesized that in comparison to the group with ADHD-C, the group with ADHD-I with high levels of SCT would exhibit significantly higher levels of social withdrawal and greater impairment on measures of sustained attention and processing speed. In contrast, we anticipated that the group with ADHD-I with high SCT would exhibit lower levels of externalizing behaviors and overt social rejection in comparison to the group with ADHD-C and the group with ADHD-I without elevated SCT.
Method
Participants
The full recruitment procedures for the CLDRC study are described in detail in previous papers (e.g., Shanahan et al., 2006; Willcutt, Pennington, et al., 2010; Willcutt, Pennington, Olson, Chhabildas, & Hulslander, 2005). Briefly, families of all twins between the ages of 8 and 16 in 22 local school districts were invited to participate in the initial screening procedures for the study. If either of the twins met symptom criteria for DSM-IV ADHD based on the screening procedures described in the subsequent section, the twin pair was invited to participate in the full study (90% of selected families agreed to participate). A comparison sample was also recruited from pairs in which neither twin met screening criteria for ADHD. Twins with significant reading difficulties were recruited independently as part of the overall CLDRC study, but twins with reading difficulties alone were not included in the current analyses (reading achievement was free to vary in the ADHD and control groups).
Exclusion criteria
As part of the larger study, potential participants with a documented brain injury, significant hearing or visual impairment, or a rare genetic or environmental etiology (e.g., Fragile X syndrome, phenylketonuria, Down syndrome or other chromosomal anomalies) were excluded from the sample. In addition, any twins with a previous diagnosis of a pervasive developmental disorder, psychosis, tic disorder, or bipolar disorder were excluded from the study, and participants with a Full Scale IQ score below 75 on the Wechsler Intelligence Scale for Children, Revised (Wechsler, 1974) were excluded from the current analyses (this criterion excluded two potential participants who met research criteria for ADHD-C, three who met criteria for ADHD-I, one participant with ADHD-H, and one participant from the comparison group).
The final sample
Because twins in a pair are not independent observations, one twin was selected at random from each pair in which both twins met inclusion criteria for the control or ADHD groups. If one twin met criteria for ADHD and one did not, the twin who met criteria for ADHD was included in the study to maximize power for ADHD subtype comparisons. The final sample included 410 individuals with DSM-IV ADHD and a comparison group of 311 individuals (52% female). Consistent with results obtained in other community samples (e.g., Willcutt, 2012), more participants metresearch criteria for ADHD-I (n = 235; 36% female) than ADHD-C (n = 135; 25% female) or ADHD-H (n = 40; 30% female). The overall sample was 80% Caucasian, 12% Hispanic, 3% African American, 3% Asian American, and 2% American Indian/Native American, with no significant differences between groups with and without ADHD.
Procedure
All study procedures were fully approved by the Institutional Review Boards of the University of Colorado, Boulder, and University of Denver, and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. Parents gave their informed consent and children and adolescents assented to participate prior to their enrollment in the study.
Measures were administered in four testing sessions at the University of Colorado, Boulder, andUniversity of Denver. All examiners were unaware of the diagnostic status of the child and the results of the testing conducted at the other sites. Parents of participants that were taking psychostimulant medication were asked to withhold medication for 24 hours prior to each session of the study to minimize the influence of medication on the results.
Measures
The analyses described in this report include data from over 60 individual measures, including 45 measures of functional impairment and neuropsychological functioning. These measures have been described in detail in previous papers (e.g., Keenan, Betjemann, & Olson, 2008; McGrath et al., 2011; Willcutt, Pennington, et al., 2010; Willcutt et al., 2005), and space constraints preclude a full description of all individual measures in the body of the current paper. Therefore, this section includes abbreviated descriptions of the measures of internalizing and externalizing psychopathology, functional impairment, and neuropsychological functioning. Section 1 of the supplemental materials provides a full description and citation for each individual measure, a summary of the procedures used to create each composite score that was included in the current analyses, and information regarding the psychometric characteristics of all individual tasks and composite scores.
DSM-IV ADHD symptoms
The Disruptive Behavior Rating Scale (DBRS; Barkley & Murphy, 1998) was used to obtain parent and teacher ratings of the 18 symptoms of DSM-IV ADHD. Each symptom on the DBRS is rated on a four point scale (never or rarely, sometimes, often, and very often). For analyses of symptom counts items rated as often or very often were scored as positive symptoms and items rated as never or rarely or sometimes were scored as negative symptoms, consistent with the procedure used in previous studies (e.g., Lahey et al., 1998). Parent and teacher ratings of ADHD symptoms were combined using an adaptation of the or rule algorithm used in the DSM-IV field trials (Lahey et al., 1994). For each symptom the higher of the parent or teacher ratings was used as the score for that item. The mean of the nine items on each DSM-IV symptom dimension was then age-regressed and standardized based on the overall sample to create composite measures of inattention and hyperactivity-impulsivity. Both composite scores had high internal consistency (α=.96 for inattention and .93 for hyperactivity-impulsivity) and 12-month test-retest reliability (r = .84 for inattention and .75 for hyperactivity-impulsivity).
ADHD subtypes
DSM-IVdiagnostic criteria for ADHD require an individual to exhibit significant impairment across settings. However, functional impairment was a key dependent variable for many of the analyses described in this paper. Therefore, ADHD subtype classifications were defined for research purposes based on symptom criteria only. Participants with six or more symptoms of inattention and fewer than six symptoms of hyperactivity-impulsivity were included in the group with ADHD-I, participants with six or more symptoms of hyperactivity-impulsivity and fewer than six symptoms of inattention were coded as ADHD-H, and individuals with six or more symptoms on both symptom dimensions were categorized as ADHD-C.
Sluggish cognitive tempo items
Nine potential SCT items were developed based on theoretical models of SCT and items used in previous studies of ADHD and SCT (e.g., Carlson & Mann, 2002; McBurnett et al., 2001; Penny et al., 2009). Each itemwas added to the DBRS and administered in the same format.
Comorbid psychopathology
One parent completed modules of the DSM-IV Diagnostic Interview for Children and Adolescents (Reich, Welner, & Herjanic, 1997) for oppositional defiant disorder (ODD), conduct disorder (CD), major depressive disorder (MDD), and generalized anxiety disorder (GAD). In addition, parents and teachers completed the Achenbach Scale for Empirically Based Assessment (ASEBA; Achenbach & Rescorla, 2001), a psychopathology screening measure that includes measures of externalizing symptoms (Aggressive Behavior, Delinquent Behavior) and internalizing symptoms (Anxious/Depressed, Withdrawn, and Somatic Complaints).
Functional impairment
Global functioning
Parents completed the Child Global Assessment Scale (CGAS; Setterberg, Bird, & Gould, 1992), a measure of global impairment that requiresthe rater to indicate the single number between 1 and 100 that best represents the individual’s functioning. In addition, items on the parent and teacher DBRS were used to assess the extent to which the twin has difficulty managing daily responsibilities.
Academic functioning
The CLDRC study includes an extensive battery of standardized tests of academic achievement (described in detail in Section 1 of the supplemental materials). Scores on these achievement tests were used to create reliable composite measures of word reading, reading comprehension, math, and written language. In addition to thesepsychometric measures of academic achievement, parents and teachers rated the twin’s understanding of classroom assignments and current academic performance in reading, math, and language arts.
Social functioning
Multiple measures were also administered to facilitate the assessment of different dimensions of social functioning. Scores on the ASEBA Social Problems scale and items from the DBRS were combined to create a composite measure of overall social impairment. Parent ratings on the Colorado Learning Difficulties Questionnaire (CLDQ; Willcutt et al., 2011)were used to assess social isolation (e.g., isolates self in social situations, feels anxious or out of place in new social settings) and social cognition (e.g., has trouble understanding how others are feeling). Finally, teachers estimated the proportion of children who like, dislike, or ignore the participant using the procedure described by Dishion (1990).
Neuropsychological Measures
The six composite measures of neuropsychological functioning include measures of constructs that were most strongly associated with ADHD or SCT in previous studies. As described in detail in Section 1 the supplemental materials, the individual test scores were combined to create standardized composite scores based on previous exploratory and confirmatory factor analyses (e.g., McGrath et al., 2011; Willcutt, Betjemann, et al., 2010).
Response Inhibition
The response inhibition measures assess the ability to inhibit a prepotent response. TheStop-signal Task is a computerized task that provides an estimate of stop-signal reaction time, a measure of the latency of the inhibitory process(e.g., Logan, Schachar, & Tannock, 1997). The Gordon Diagnostic System (Gordon, 1983) is a visual continuous performance test (CPT) that requires the participant to respond when a 9 appears immediately after a 1. The primary measure of inhibition is the number of commission errors in response to a sequence of numbers other than the target.
Working memory
The three verbal working memory tasks require the participant to retain and manipulate verbal information in memory. On the Sentence Span Task (Siegel & Ryan, 1989) the participant provides the last word for a set of simple sentences read by the examiner (e.g., “I throw the ball up and then it comes…”), then must reproduce the words that they provided after all sentences in that set are completed. Similarly, the Counting Span Task(Case, Kurland, & Goldberg, 1982) requires the participant to count aloud the number of dots on a series of cards, then recall the number of dots on each card in the set. Finally, the Digits Backward component of WISC-R Digit Span (Wechsler, 1974) requires the participant to repeat in reverse order a series of numbers presented aloud by the examiner.
Processing Speed
A composite processing speed score was created by averaging the standardized scores on four measures that loaded on a latent processing speed factor in our previous analyses (McGrath et al., 2011). The WISC-III Symbol Search(Wechsler, 1991) and WISC-R Coding subtests are widely-used psychometric measures of processing speed. On the Colorado Perceptual Speed Test(DeFries, Singer, Foch, & Lewitter, 1978) the participant circles one of four possible letter strings to match a target letter string as rapidly as possible. Similarly, the IdenticalPicturesTest(French, Ekstrom, & Price, 1963) requires the participant to identify as quickly as possible the one picture out of five options that matches a target picture.
Naming Speed
The Rapid Automatized NamingTest is an adaptation of the measure developed by Denckla and Rudel (Denckla & Rudel, 1976). On each of the four test trials the participant names as many objects, numbers, letters, or colors as possible in 15 seconds.
Sustained attention
As described earlier, we tentatively hypothesized that SCT would be associated with difficulty remaining consistently attentive during lengthy tasks. The primary measure of sustained attention in the current battery was the number of omission errors (failure to respond to the target sequence) during the CPT described previously (Gordon, 1983).
Response variability
Finally, the primary measures of response variability was the intraindividual standard deviation of reaction times on the primary task trials of the stop-signal task.
Data analyses
Data cleaning and adjustments
The distribution of each variable was first assessed for outliers, defined as scores that fell more than three standard deviations (SD) from the mean of the overall sample and more than 0.5 SD beyond the next most extreme score. Most measures had no scores that met these criteria, but a small number of outliers were identified on the CPT (two individuals in the ADHD group and one in the comparison group) and the stop-signal task (three individuals in the ADHD group and one in the control group). After confirming that the outlying score was entered correctly in the data file, each outlier was adjusted to a score 0.5 SD units beyond the next highest score, with multiple outliers rescored to 0.1 SD apart.
The distribution of each variable was then assessed for significant deviation from normality, and a logarithmic transformation was implemented to approximate a normal distribution if skewness or kurtosiswas greater than one (parent and teacher ratings on the ASEBA, CPT commission errors). As expected, correlational analyses suggested that several measures of impairment and neuropsychological functioning were significantly correlated with age. Therefore, an age-adjusted score was created for each measure by regressing the variable onto age and saving the standardized residual score.
Analyses to test the internal validity of SCT and ADHD
Factor analyses of ADHD and SCT
Initial EFA included the 18 DSM-IV ADHD symptoms and nine potential SCT symptoms. Because theoretical models of ADHD and SCT suggested that the extracted factors would be correlated, principal axis factor analyses were conducted with an oblique promax rotation, and all factors with Eigenvalues greater than 1.0 were extracted. Results were similar when analyses were repeated using principal components analysis with an orthogonal rotation, suggesting that the factor structure is robust across methods. Primary loadings were defined as loadings of .60 or higher, and items were considered cross-loaded if a secondary loading was greater than .30 and within .20 of the item’s primary factor loading. To examine whether the factor structure was robust across raters, initial EFA were conducted separately for parent ratings, teacher ratings, and parent and teacher ratings combined using the or rule procedure.
Expanded factor analytic models
As noted earlier, SCT symptoms bear some resemblance to features of internalizing disorders, and previous studies suggest that the factor structure of ADHD may vary depending on the specific symptoms of disorders other than ADHD that are included in the analysis (e.g., McBurnett et al., 2001; Pillow, Pelham, Hoza, Molina, & Stultz, 1998). Therefore, to provide a more definitive test of the internal validity of SCT and ADHD, a second EFA included symptoms of DSM-IV ADHD, ODD, GAD, and MDD along with the six items that loaded on the SCT factor in the first EFA. Symptoms of CD were also initially included in the second analysis, but were dropped due to extremely low rates of endorsement in the current sample (none of the CD items cross-loaded on the SCT or ADHD factors when they were initially included).
Analyses to test the external and discriminant validity of SCT and ADHD
Primary analyses of SCT and ADHD
The external validity of SCT was first examined by computing zero-order correlations between SCT and the composite measures of functional impairment and neuropsychological functioning. To test whether any significant effects were independently associated with SCT or explained by covariance with ADHD symptoms, SCT, inattention, and hyperactivity-impulsivity composite scores were entered simultaneously as independent variables in multiple regression models predicting each measure of impairment.
Other potential covariates
Zygosity and socioeconomic status were included in initial multiple regression models, but were dropped from final models because neither variable had a significant impact on any result. Potential differences in the pattern of results as a function of age or sex were examined by testing for differences in males and females and in subsets of the sample age 12 or younger versus age 13 or older. Because the pattern of results was similar, results are reported for the full sample.
Some researchers have argued that general intelligence and symptoms of concurrent mental disorders should also be statistically controlled to ensure that any associations between SCT, inattention, or hyperactivity-impulsivity and measures of functional impairment cannot be explained more parsimoniously by these correlated variables (e.g., Lahey et al., 1998). In contrast, others have pointed out that the decision to statistically control these variables may potentially remove meaningful variance if ADHD or SCT symptoms directly cause poor performance on standardized tests of intelligence (e.g., Barkley, 1997), or if shared etiological influences lead to covariance between symptoms of different disorders (e.g., Willcutt, Betjemann, et al., 2010). Because these issues have not been resolved conclusively, results are presented both ways. The first step of each regression model included symptoms of SCT, inattention, and hyperactivity-impulsivity, and Full Scale IQ and symptoms of ODD, CD, GAD, and MDD were then added simultaneously in a second step to test whether any effects that were significant in the first step of the model were explained by these covariates. Collinearity diagnostics were within the acceptable range for all multiple regression models (Tolerance = .31–.80; VIF = 1.25 – 2.80).
Analyses to test the relation between DSM-IV ADHD symptoms and SCT
A final set of analyses was conducted to test whether the presence of elevated SCT symptoms identified a subgroup of ADHD-I that was more clearly distinct from ADHD-C. The group with ADHD-I was divided into subgroups with high and low SCT based on a cutoff score one SD above the estimated population mean on the SCT composite. Analyses of variance with planned comparisons were then conducted to compare the two ADHD-Igroups to the groups with ADHD-C and ADHD-H and the comparison group without ADHD on the measures of internalizing and externalizing symptoms, functional impairment, and neuropsychological functioning.
Results
Internal validity
EFA of symptoms of ADHD and SCT
Exploratory factor analyses of parent ratings, teacher ratings, and combined parent and teacher ratings of ADHD and SCT symptoms each yielded three factors with Eigenvalues greater than one. Consistent with expectations based on the DSM-IV model of ADHD, all DSM-IV inattention symptoms had a primary loading on the first factor that was extracted, and all DSM-IV hyperactivity-impulsivity symptoms had a primary loading on the second extracted factor. Six of the potential SCT items had a primary loading on a third factor, whereas the other three putative SCT items cross-loaded on the Inattention factor in at least one of the analyses (due to space constraints only the factor loadings for the six final SCT items are provided in Table 1; Supplement Table 1 includes factor loadings for all 27 items). After the three items that cross-loaded on the SCT and Inattention factors were dropped, all ADHD and SCT items had a primary loading on the predicted factor, and none cross-loaded on either of the other factors. The same pattern of results emerged when analyses were restricted to the comparison sample without ADHD.
Table 1.
Exploratory factor analyses of DSM-IV ADHD symptoms and potential SCT items
| Itema | Parent Ratings
|
Teacher Ratings
|
Combined Parent and Teacher
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Factor 1 Inattention | Factor 2 Hyp-Imp | Factor 3 SCT | Factor 1 Inattention | Factor 2 Hyp-Imp | Factor 3 SCT | Factor 1 Inattention | Factor 2 Hyp-Imp | Factor 3 SCT | |
| Sluggish/slow to respond | .25 | .06 | .80 | .29 | .04 | .86 | .29 | .04 | .83 |
| Seems to be “in a fog” | .28 | .16 | .73 | .33 | .02 | .75 | .29 | .12 | .76 |
| drowsy, sleepy | .15 | .06 | .85 | .19 | .02 | .84 | .17 | .06 | .86 |
| stares blankly | .21 | .25 | .68 | .26 | .05 | .79 | .24 | .14 | .76 |
| underactive, slow moving | .13 | −.14 | .73 | .23 | −.02 | .86 | .18 | −.04 | .84 |
| daydreams, lost in thought | .38 | .17 | .67 | .47 | .06 | .71 | .43 | .19 | .66 |
| Eigenvalue | 10.91 | 3.07 | 1.49 | 11.10 | 4.78 | 1.38 | 11.50 | 3.83 | 1.33 |
Note:SCT = sluggish cognitive tempo. Hyp-imp = hyperactivity-impulsivity. Loadings in bold type indicate primary factor loadings.
Three potential SCT items (seems not to hear, easily confused, and absentminded) cross-loaded on the Inattention factor, and were dropped from the final model. Supplement Table 1 provides loadings of all ADHD and SCT items on each factor, and Supplement Table 2 summarizes EFA that included symptoms of ODD, GAD, and MDD along with SCT and ADHD items.
EFA of symptoms of SCT, ADHD and other psychopathology
When symptoms of GAD, MDD, and ODD were also included in a second EFA, all six SCT items continued to have a primary loading on a single factor with no cross-loadings on the other five factors that were extracted (Supplement Table 2). Similarly, all DSM-IV inattention and hyperactivity-impulsivity items had a primary loading on their expected factor, although two hyperactivity-impulsivity items also cross-loaded on the inattention factor (fidgets and leaves seat in the classroom). Nearly all symptoms of ODD, GAD, and MDD had a primary loading on their expected factor. Most importantly, none of the inattention, hyperactivity-impulsivity, or SCT symptoms loaded on factors with symptoms of ODD, GAD, or MDD, and only one MDD symptom (psychomotor retardation) loaded on the factor with the SCT items.
External validity
A standardizedSCT composite score was created based on the mean of the six items that loaded on the SCT factor (α=.93 and 12-month test-retest reliability r = .73). Analyses of external validityyielded similar results for parent ratings, teacher ratings, and combined parent and teacher ratings of ADHD and SCT symptoms. To simplify presentationresults are reported for the combined parent and teacher ratings, and a detailed summary of the analyses of parent and teacher ratings alone is available from the first author upon request.
Concurrent mental disorders
Zero-order correlations indicated that SCT symptoms were significantly associated with both ADHD symptom dimensions and all measures of internalizing and externalizing symptoms (Table 2), and multiple regression analyses indicated that SCT symptoms were independently associated with all measures of internalizing symptoms when inattention and hyperactivity-impulsivity were controlled. In contrast, SCT was not associated with externalizing symptoms when inattention and hyperactivity-impulsivity were also included in the multiple regression models.
Table 2.
Multiple regression analyses of the relations between symptoms of ADHD and sluggish cognitive tempo and symptoms of other psychopathology
| Correlation with SCT | Multiple regression modelsa
|
|||||
|---|---|---|---|---|---|---|
| Inattention
|
Hyp-Imp
|
SCT
|
R2 | F | ||
| B [95% CI] | B [95% CI] | B [95% CI] | ||||
| ADHD symptoms | ||||||
| Inattention | .63*** | -- | -- | -- | -- | -- |
| Hyperactivity-Impuls | .25*** | -- | -- | -- | -- | -- |
| Internalizing symptoms | ||||||
| Withdrawnb | .56*** | .12 [.00, .24] | −.05[−.15, .05] | .50 [.42, .58]*** | .311 | 106.4*** |
| Somatic Complaints | .46*** | .08 [−.03, .19] | .17 [.07, .27]** | .49 [.39, .59]*** | .225 | 68.4*** |
| Anxious/Depressed | .42*** | .04 [−.08, .16] | .21 [.11, .31]** | .31 [.21, .41]*** | .237 | 69.2*** |
| DSM-IV GAD | .24*** | .06 [−.08, .20] | .19 [.09, .29]** | .26 [.16, .36]*** | .068 | 15.1*** |
| DSM-IV MDD | .38*** | .24 [.12, .36]*** | .05 [−.05, .15] | .17 [.07, .27]** | .167 | 44.1*** |
| Externalizing symptoms | ||||||
| Delinquent Behavior | .31*** | .25 [.12, .36]*** | .39 [.31, .47]*** | .08 [−.01, .17] | .385 | 148.3*** |
| Aggressive Behavior | .27*** | .23 [.14, .31]*** | .54 [.48, .60]*** | .01 [−.02, .07] | .560 | 288.3*** |
| DSM-IV ODD | .24*** | .26 [.15, .37]*** | .36 [.28, .44]*** | −.02[−.10, .06] | .315 | 109.1*** |
| DSM-IV CD | .22*** | .26 [.14, .38]*** | .29 [.19, .39]*** | −.01[−.09, .09] | .206 | 54.2*** |
Note: N = 711. GAD = generalized anxiety disorder, MDD = major depressive disorder, ODD = oppositional defiant disorder, CD = conduct disorder.
the inattention, hyperactivity-impulsivity, and SCT composites were entered simultaneously in step 1 of each multiple regression model. Full Scale IQ was then entered as a covariate in a second step in each model, but the inclusion of IQ as a covariate did not change the significance of any result.
Two items (stares) were omitted from the withdrawn score for these analyses due to their similarity to items included on the SCT scale.
= p < .05,
= p < .01,
= p < .001.
Functional impairment
With the exception of the tendency to be disliked by peers, SCT symptoms were independently associated with all aspects of global, academic, and social impairment when symptoms of inattention and hyperactivity-impulsivity were controlled (Table 3). DSM-IV inattention symptoms were also independently associated with many of these impairment measures, but only SCT symptoms were independently associated with social isolation and low achievement in written language. Importantly, nearly all of these results remained significant when full scale IQ and symptoms of ODD, CD, GAD, and MDD were added to the model (Supplement Table 3).
Table 3.
Multiple regression analyses of the relations between symptoms of ADHD and sluggish cognitive tempo and measures of functional impairment
| Correlation with SCT | Multiple regression modelsa
|
|||||
|---|---|---|---|---|---|---|
| Inattention
|
Hyp-Imp
|
SCT
|
R2 | F | ||
| B [95% CI] | B [95% CI] | B [95% CI] | ||||
| Global functioning | ||||||
| CGASc | .49*** | .37 [.25, .49]*** | .24 [.14, .34]*** | .19 [.09, .29]*** | .434 | 121.8*** |
| Daily responsibilitiesd | .53*** | .69 [.61, .77]*** | .10 [.02, .18]*b | .08 [.01, .15]*b | .632 | 354.8*** |
| Social functioning | ||||||
| Total Problemsd | .49*** | .28 [.18, .38]*** | .26 [.18, .34]*** | .28 [.20, .36]*** | .463 | 203.6*** |
| Liked by peerse | .40*** | .20 [.07, .33]** | .14 [.03, .25]*b | .24 [.13, .35]*** | .231 | 56.9*** |
| Ignored by peerse | .38*** | .27 [.12, .42]*** | .03 [−.09, .22] | .23 [.10, .36]*** | .185 | 30.9*** |
| Disliked by peerse | .18*** | .20 [.05, .35]**b | .21 [.07, .35]**b | .06 [−.08, .20] | .130 | 20.4*** |
| Social Cognitiond | .31*** | .13 [.01, .25]*b | .41 [.31, .51]*** | .15 [.05, .25]*** | .298 | 90.3*** |
| Social Isolationd | .39*** | .08 [−.06, .22] | .11 [−.01, .22] | .29 [.19, .39]*** | .174 | 44.9*** |
| Overall academic functioning | ||||||
| Understand assignd | .55*** | .45 [.32, .58]*** | .07 [−.03, .17] | .22 [.12, .32]*** | .440 | 114.0*** |
| Gradese | .42*** | .48 [.36, .60]*** | .02 [−.09, .13] | .16 [.04, .30]** | .303 | 67.1*** |
| Academic achievement | ||||||
| Mathd | .38*** | .33 [.21, .45]*** | .01 [−.09, .11] | .19 [.09, .29]*** | .212 | 56.2*** |
| Word readingd | .37*** | .33 [.21, .45]*** | −.03[−.12, .06] | .16 [.07, .25]*** | .205 | 60.4*** |
| Reading Comp.f | .33*** | .26 [.12, .40]*** | .08 [−.04, .20] | .16 [.04, .28]**b | .182 | 39.4*** |
| Written Languageg | .48*** | .21 [−.02, .44] | .20 [−.02, .42] | .28 [.09, .47]** | .286 | 22.6*** |
Note: All measures are scaled so that a positive B indicates greater impairment.
point estimates from amodel in which inattention, hyperactivity-impulsivity, and SCT were entered simultaneously as independent variables. Full scale IQ and symptoms of MDD, GAD, ODD, and CD were then entered simultaneously as covariates in a second step (Supplement Table 3).
the effect was not significant after FSIQ and symptoms of MDD, GAD, ODD, and CD were added (P > .05).
N = 545.
N = 716.
N = 595.
n = 510.
186
= p < .05,
= P < .01,
= P < .001
Neuropsychological functioning
Zero-order correlations were significant between SCT and all six neuropsychological composites (Table 4), and both SCT and DSM-IV inattention were significantly associated with processing and naming speed when SCT, inattention, and hyperactivity-impulsivity were included in multiple regression models. In contrast, the multiple regression models indicated that only inattention was independently associated with response inhibition, working memory, and increased response variability, and only SCT was independently associated with a weakness in sustained attention after full scale IQ was controlled (Supplement Table 4).
Table 4.
Multiple regression analyses of the relations between symptoms of ADHD and sluggish cognitive tempo and measures of neuropsychological functioning
| Neuropsychological Composite | Correlation with SCT | Multiple regression modelsa
|
||||
|---|---|---|---|---|---|---|
| Inattention
|
Hyp-Imp
|
SCT
|
R2 | F | ||
| B [95% CI] | B [95% CI] | B [95% CI] | ||||
| Full Scale IQ | .37*** | .34 [.23, .45]*** | −.02 [−.11, .07] | .14 [.05, .23]** | .195 | 57.2*** |
| Processing Speed | .39*** | .38 [.27, .49]*** | .04 [−.04, .12] | .15 [.07, .23]** | .259 | 82.3*** |
| Naming Speed | .34*** | .29 [.17, .41]*** | −.03 [−.12, .06] | .16 [.08, .24]*** | .171 | 47.9*** |
| Sustained Attention | .33*** | .16 [.04, .28]*b | .02 [−.08, .11] | .20 [.10, .30]*** | .112 | 26.4*** |
| Inhibition | .29*** | .27 [.14, .41]*** | .13 [.03, .23]* | .10 [−.01, .21] | .163 | 42.1*** |
| Working Memory | .26*** | .22 [.12, .36]*** | .03 [−.06, .12] | .09 [−.01, .19] | .126 | 29.6*** |
| Response Variability | .29*** | .29 [.15, .43]*** | .05 [−.05, .15] | .10 [.00, .20] | .141 | 32.9*** |
Note: N = 716. All measures are scaled so that a positive B indicates an association between higher levels of SCT and ADHD and greater neuropsychological weakness.
point estimates from amodel in which inattention, hyperactivity-impulsivity, and SCT were entered simultaneously as independent variables. Full scale IQ and symptoms of MDD, GAD, ODD, and CD were then entered simultaneously as covariates in a second step (Supplement Table 4).
the effect was not significant after FSIQ and symptoms of MDD, GAD, ODD, and CD were added (P > .05).
= p < .05,
= P < .01,
= P < .001
To supplement the primary neuropsychological analyses, additional multiple regression analyses were conducted to test whether SCT, inattention, or hyperactivity-impulsivity were each associated with multiple independent neuropsychological weaknesses. In the first step of each model, scores on one of the symptom dimensions were regressed simultaneously onto the six neuropsychological composites. Scores on the other two symptom dimensions were then added as independent variables in a second step to test whether any significant neuropsychological weaknesses in the first step were uniquely associated with the symptom dimension when scores on the other two dimensions were controlled.
Inattention symptoms were associated with independent weaknesses in response inhibition (B = .22, 95% CI [.12, .32], p< .0001), response variability (B = .10, 95% CI [.02, .18], p< .01), naming speed (B = .14, 95% CI [.06, .22], p< .01), and processing speed (B = .33, 95% CI [.23, .43], p< .0001), and all of these effects remained significant when hyperactivity-impulsivity and SCT were controlled in the second step of the regression model (all p< .01). SCT scores were also independently associated with weaknesses in naming speed (B = .17, 95% CI [.07, .27], p< .0001), and processing speed (B = .20, 95% CI [.09, .31], p< .0001), along with a significant weakness in sustained attention (B = .10, 95% CI [.02, .18], p< .01). However, only the weakness in sustained attention was significantly associated with SCT when symptoms of inattention and hyperactivity-impulsivity were added in the second step of the model. Finally, hyperactivity-impulsivity symptoms were predicted independently by weaknesses in response inhibition (B = .26, 95% CI [.16, .36], p< .0001) and processing speed (B = .25, 95% CI [.14, .36], p< .0001), but only the association with inhibition remained significant after controlling for symptoms of inattention and SCT.
Analyses of the relation between SCT and DSM-IV ADHD subtypes
The final series of analyses examined the relation between SCT scores and groups that met research criteria for the DSM-IV ADHD subtypes (descriptive characteristics of the subtype groups are summarized in Table 5). Mean SCT scores were significantly higher in groups with ADHD-I and ADHD-C than the group with ADHD-H and the comparison group without ADHD. The group with ADHD-I also exhibited significantly more symptoms of SCT than the group with ADHD-C based on teacher ratings and combined parent and teacher ratings. However, the effect sizes for these comparisons were small (Hedges’ g = 0.2 – 0.3), and groups with ADHD-C and ADHD-I did not differ on parent ratings of SCT.
Table 5.
Characteristics of groups with and without DSM-IV ADHD subtypes based on research criteria
| Comparison (N = 311) M (SD) |
ADHD-C (N=135) M (SD) |
ADHD-I (N = 235) M (SD) |
ADHD-H (N = 40) M (SD) |
F | |
|---|---|---|---|---|---|
| Descriptive characteristics | |||||
| Age | 11.2 (2.9) | 10.9 (2.5) | 11.3 (2.7) | 10.6 (2.4) | 2.8 |
| Parental education (years) | 15.3 (2.1)a | 14.4 (2.3)b | 14.6 (2.3)b | 14.5 (2.2)b | 8.3** |
| Socioeconomic status | 3.6 (1.1)a | 3.1 (1.2)b | 3.1 (1.2)b | 3.0 (1.3)b | 9.2** |
| Full Scale IQ | 112.9 (12.0)a | 101.8 (13.2)b | 100.3 (12.4)b | 108.1 (12.0)c | 54.0*** |
| DSM-IV ADHD symptoms | |||||
| Inattention | 0.6 (1.2)a | 8.0 (1.4)b | 7.7 (1.1)b | 2.4 (1.7)c | 884.2** |
| Hyperactivity-impulsivity | 0.5 (1.0)a | 7.5 (1.4)b | 2.1 (1.7)c | 7.0 (1.0)b | 575.0** |
| Sluggish Tempo ratings | |||||
| Parent | 0.12 (0.36)a | 0.61 (0.63)b | 0.59 (0.60)b | 0.17 (0.31)a | 73.6** |
| Teacher | 0.14 (0.36)a | 0.68 (0.66)b | 0.89 (0.77)c | 0.15 (0.34)a | 54.1** |
| Or rule | 0.16 (0.39)a | 0.86 (0.67)b | 1.05 (0.75)c | 0.18 (0.47)a | 121.2** |
| Concurrent mental disorders | N (%) | N (%) | N (%) | N (%) | Χ2 |
|
|
|||||
| Internalizing Disorders | |||||
| DICA-IV GAD | 23 (7%)a | 35 (26%)b | 36 (15%)b | 8 (20%)b | 28.5** |
| DICA-IV MDD | 6 (2%)a | 24 (18%)b | 35 (15%)b | 2 (5%)a | 42.0** |
| Externalizing Disorders | |||||
| DICA-IV ODD | 22 (7%)a | 77 (57%)b | 65 (27%)c | 17 (43%)d | 136.1** |
| DICA-IV CD | 9 (3%)a | 44 (31%)b | 50 (22%)c | 8 (20%)c | 74.9** |
| Learning Disorders | |||||
| Reading Disorder | 5 (2%)a | 35 (26%)b | 67 (29%)b | 3 (8%)a | 91.9** |
| Math Disorder | 15 (5%)a | 38 (28%)b | 83 (35%)b | 4 (10%)a | 90.7** |
Note: Means and percentages with no shared subscripts are significantly different (P < .01). DICA-IV = DSM-IV Diagnostic Interview for children and Adolescents. GAD = generalized anxiety disorder, MDD = major depressive disorder, ODD = oppositional defiant disorder, CD = conduct disorder.
To test whether elevations of SCTsymptoms identified a subgroup of ADHD-I that was more clearly distinct from ADHD-C, the group with ADHD-I was divided into groups with low versus high levels of SCT (Figure 1; results were similar for all neuropsychological measures, so were combined in the Figure). Results indicated that the group with ADHD-C and both groups with ADHD-I differed from the comparison group and the group with ADHD-H on all measures of functional impairment and neuropsychological functioning (p < .001). In contrast, the only significant difference between the group with ADHD-C and the group with ADHD-I with high SCT was the significantly higher number of externalizing symptoms in the group with ADHD-C.
Figure 1.
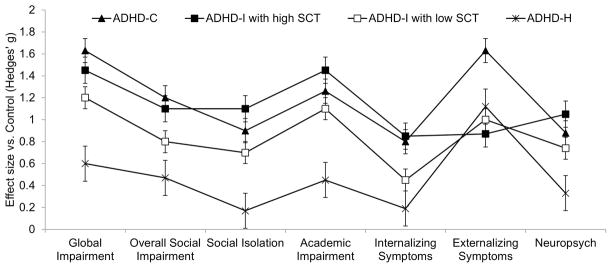
Point estimates indicate effect sizes (Hedges’ g) for comparisons of each DSM-IV ADHD subtype and the control group without ADHD. The group with ADHD-I was subdivided into groups with (N = 89) and without (N = 144) high SCT based on a cutoff score one standard deviation above the estimated population mean on the SCT composite measure. Error bars indicate the standard error of each effect size.
Discussion
This study systematically evaluated the internal and external validity of SCT and its relation with DSM-IV ADHD and other psychopathology. In this section we first discuss the implications of the current results for the internal and external validity of SCT and the DSM-IV model of ADHD. We then examine the broader clinical and theoretical implications of these findings, and conclude by highlighting several key directions for future research to better understand the nature of SCT and its relation with ADHD and other disorders.
Internal validity of SCT
Exploratory factor analyses identified six SCT items that loaded on a factorseparate from symptoms of DSM-IV inattention and hyperactivity-impulsivity, replicating most previous factor analytic studies of SCT and ADHD symptoms (Barkley, 2013; Garner et al., 2010; McBurnett et al., 2001; Penny et al., 2009; Todd et al., 2004). Furthermore, the same 6-item SCT factor emerged in a second EFA that also included symptoms of DSM-IV MDD, GAD, ODD, and CD. These results are consistent with one previous study that identified a SCT factor among seven factors that emerged in EFA of teacher ratings on a psychopathology screening measure (Neeper & Lahey, 1986). However, a second EFA of a larger pool of items derived from symptoms of DSM-IV disorders did not identify a separate SCT factor, and instead found that several potential SCT symptoms loaded on a factor with items similar to DSM-IV inattention symptoms (Lahey et al., 2004).
One possible explanation for the apparent discrepancy between the current results and the study by Lahey and colleagues (2004) is the specific SCT items that were included in each study. The SCT items with the highest factor loadings in the current study emphasize low physical energy, sleepiness, and sluggishness (e.g., underactive, slow moving, sluggish, drowsy/sleepy), whereas the items in the earlier study primarily assess slow responses to questions and difficulty completing tasks efficiently (dawdled and worked slowly, difficulty thinking or deciding, took longer to answer than others). Two other independent EFA of large pools of potential SCT items also found that items that assessed slow initiation and completion of tasks loaded with DSM-IV inattention symptoms, whereas items similar to the SCT items included in the current study loaded on a Sleepy/Daydreamer factor that was distinct from DSM-IV inattention (Barkley, 2013; Penny et al., 2009).
Overall, results of the current EFA provide strong support for the internal validity of SCT. Although SCT symptoms are significantly correlated with most other dimensions of psychopathology, these results provide initial support for the hypothesis that SCT is a distinct symptom dimension, especially when measured by items that assess low energy and sluggish orsleepy behavior.
External validity of SCT and discriminant validity of SCT and DSM-IV inattention
Zero-order correlations indicated that SCT symptoms are associated with nearly all measures of functional impairment, replicating and extending previous studies (e.g., Garner et al., 2010; Neeper & Lahey, 1986). Further, most of these associations remained significant when symptoms of inattention and hyperactivity-impulsivity, internalizing and externalizing psychopathology, and Full Scale IQ were controlled. Symptoms of SCT and DSM-IV inattention were both independently associated with overall social difficulties, higher rates of being ignored by peers, and lower achievement in reading and math. In contrast, only SCT was significantly associated with social isolation and weaknesses in written production, and only DSM-IV inattention and hyperactivity-impulsivity were independently associated with greater likelihood of being disliked by peers.
Analyses of neuropsychological measures yielded a similar pattern of shared and distinct weaknesses associated with SCT and inattention. SCT and inattention were both significantly correlated with all six neuropsychological composites, and multiple regression analyses indicated that SCT and inattention were independently associated with slow naming and processing speed. In contrast, only SCT symptoms were also associated with deficits in sustained attention, and this weakness remained significant when the other five neuropsychological composites were included in a single multiple regression model. On the other hand, only DSM-IV inattention symptoms were associated with independent weaknesses on measures of response inhibition and response variability. The patterns of results for SCT and DSM-IV inattention are both consistent with the findings reported by the only other dimensional study of the neuropsychological correlates of SCT and inattention (Wahlstedt & Bohlin, 2010) and a recent study of the relations among parent ratings of SCT, ADHD, and executive functions (Barkley, 2013).
In summary, the external validity ofSCT was strongly supported by significant associations between SCT and multiple dimensions of functional impairment and neuropsychological functioning, and most of these effects remained significant when general cognitive ability and symptoms of ADHD and other psychopathology were controlled. Although many external correlates were associated with both SCT and ADHD, the discriminant validity of SCT and DSM-IV inattention was supported by differential associations with social isolation, academic achievement, and several dimensions of neuropsychological functioning. These results suggest that SCT may be best conceptualized as a clinically valid construct that is at least partially distinct from ADHD and other DSM-IV disorders.
Impact of SCT on ADHD subtype classification
The group with ADHD-I had significantly higher SCT scores than any other group, but the effect size of the difference between groups with ADHD-C and ADHD-I was small in magnitude (g = 0.2 – 0.3). In contrast, both ADHD-I and ADHD-C exhibited significantly more SCT symptoms than the comparison group without ADHD, and effect sizes were large for both groups (ADHD-I vs. controlg = 1.3 – 1.5; ADHD-C vs. control g = 1.1 – 1.3).
To test directly whether elevations of SCT symptoms identified a subgroup of ADHD-I that was more clearly distinct from ADHD-C, the group with ADHD-I was subdivided into groups with low versus high levels of SCT. The only significant difference between the group with ADHD-C and the subgroup with ADHD-I with high SCT was the significantly higher number of externalizing symptoms in the group with ADHD-C. Contrary to our initial hypothesis, elevations of SCT symptomsdo not appear to be a marker for a subset of cases with ADHD-I that are distinct from ADHD-C. Instead, the current findings and the results of a recent meta-analysis (Willcutt et al., 2012) suggest that SCT symptoms are strongly associated with both ADHD-C and ADHD-I.
Clinical implications of SCT
From a clinical perspective, arguably the most important resultfrom the current study is the finding that ADHD and SCT symptoms are independently associated with multiple aspects of functional impairment even after symptoms of ODD, CD, GAD, and MDD are controlled. These findings indicate that ADHD and SCT symptoms provide unique information that has important clinical implications, andsuggest that symptoms of SCT should be assessed routinely as part of a comprehensive clinical evaluation.
Multiple regression models of ADHD and SCT composite scores indicated that only SCT symptoms were independently associated with increased social isolation and withdrawal and specific difficulties in written language, but the causes of these associations are unknown. Although admittedly speculative, one possible explanation is that individuals with SCT may become overwhelmed by the rapid flow of complex information that must be processed continuously to successfully navigate social interactions, which may then lead to avoidance of social situations and subsequent isolation. Similarly, difficulty sustaining attention and working quickly could have an especially pronounced impact on writing tasks that require sustained effort over an extended period of time. Alternatively, poor performance on tests of achievement in written language could also reflect weaknesses in more basic processes such as the fine-motor movements that were not assessed in the current study. Future research is needed to test these tentative hypotheses and other competing explanations for the relations between SCT and specific aspects of functional impairment.
Finally, the significant impairment associated with SCT suggests that future research is needed to develop and test interventions that target SCT symptoms. To the best of our knowledge no previous or ongoing intervention studies have focused specifically on SCT, suggesting that it may be some time before these data are available. Until then, preliminary analyses of the impact of SCT on treatment response could potentially be conducted as an extension of ongoing treatment studies of ADHD or other disorders that included measures of SCT.
Implications and future directions for theoretical models of SCT
Despite a growing literature that suggests that SCT is a reliable and valid construct that is clinically important, theoretical models of SCT remain largely descriptive (e.g., Penny et al., 2009). To facilitate the development of a more comprehensive model of SCT, this section highlights several findings from the current study that may provide useful guidance or important constraints for future theoretical models.
Refinement of the construct of SCT
Although EFA are descriptive and largely atheoretical, these results provide useful data to refine theoretical models of SCT. Along with other factor analyses (e.g., Barkley, 2013; Penny et al., 2009), the current results suggest that SCT items that are characterized by low energy and sluggish and sleepy behavior are more clearly separable from symptoms of ADHD than items that assess confusion, slow responding, and difficulty completing tasks efficiently. These converging results suggest that future theoretical models of SCT may be improved by focusing on this sluggish/sleepy dimension of behavior.
Neuropsychologicalmodels of ADHD and SCT
The current study is one of the first studies to examine the neuropsychological correlates of SCT, extending our previous work on the neuropsychology of ADHD (e.g., McGrath et al., 2011; Willcutt, Pennington, et al., 2010). Similar to other complex disorders (e.g., Pennington, 2006), SCT and ADHD appear to arise from the combinedeffects of multiple neuropsychological weaknesses rather than a single primary deficit. As described earlier, slow naming and processing speed may represent a shared weakness that accounts for covariance between SCT and inattention, whereas SCT and inattention are distinguished by differential associations with measures of sustained attention, response inhibition, and response variability.
Several future lines of research may facilitate the continued development and refinement of a comprehensive cognitive model of SCT. Future research should include measures of a broader range of cognitive constructs that may be relevant to SCT. These may potentially include measures of the speed, consistency, and variability of simple reaction time and more complex speeded responses, along with tasks designed to assess sustained attention and other aspects of attentional processing. In addition, future studies of behavioral measures of vigilance, processing speed, and response variability may be further strengthened by incorporating electrophysiological or neuroimaging techniques to more directly measurethe neurophysiological correlates of SCT. As a straightforward first step to facilitate this line of research, it may be useful for ongoing or newly initiated neuroimaging studies of related constructs such as ADHD and internalizing disorders to include a brief measure of SCT.
Developmental and etiological models
Despite the fact that over 25 years of research has been completed since SCT was first described (Neeper & Lahey, 1986), virtually nothing is known about the etiology or developmental course of SCT. Etiologically-informative designs such as family and twin studies and longitudinal studies that track the development of SCT and other symptom dimensions from an early age would provide important new information for theoretical models of SCT.
Other limitations and future directions
Sample
An important limitation of the current study is the fact that the sample was initially selected for ADHD. Resultsof the factor analyses and the analyses of external validity were similar when analyses were restricted to the comparison group without ADHD, and several key findings are consistent with results reported in an unselected sample of children (Wahlstedt & Bohlin, 2010) and in groups of children that were selected independently for elevations of ADHD or SCT (Barkley, 2013). Nonetheless, future studies of unselected samples or groups selected directly for SCT would provide a useful extension of the current research.
SCT item pool
The initial pool of nine potential SCT items is among the largest that has been analyzed to date, and represents a significant improvement over previous studies for which only two or three SCT symptoms were available (e.g., Carlson & Mann, 2002; Frick et al., 1994; McBurnett et al., 2001; see Willcutt et al., 2012 for a detailed review). On the other hand, the six items that loaded on the final SCT scale for the current analyses did not include several additional items that loaded on SCT factors in the most extensive factor analytic studies of SCT symptoms (tired, lethargic, yawning/stretching/sleepy-eyed appearance, low energy, in a world of his/her own; Barkley, 2013; Penny et al., 2009). Future studies should also incorporate these symptoms and continue to develop and test new SCT itemstocontinue to improve the measurement model of SCT.
Conclusion
The current results provide strong support for the internal and external validity of SCT. SCT symptoms are elevated in both ADHD-C and ADHD-I, and high levels of SCT do not appear to be a marker for a subgroup of ADHD-I that is distinct from the remainder of cases with DSM-IV ADHD. Instead, the current results suggest that DSM-IV inattention and SCT are correlated but distinct symptom dimension that are each independently associated with important aspects of functional impairment and neuropsychological functioning.
Supplementary Material
Acknowledgments
Funding information and disclosures. Primary funding for the study was provided by agrant from the National Institute of Child Health and Human Development (P50 HD27802). The authors were also supported by NIH grants R01 HD 47264, R01 DC 05190, R01 HD38526, R01 MH 62120, R01 MH 63941, and R01 MH 70037 during the preparation of this report. Portions of these data were included in masters and doctoral theses at the University of Denver (N. A. Chhabildas). Earlier subsets of these results were presented at the annual meetings of the International Society for Research on Child and Adolescent Psychopathology and the International Neuropsychological Society.
Contributor Information
Erik G. Willcutt, University of Colorado at Boulder
Nomita Chhabildas, University of Colorado at Boulder.
Mikaela Kinnear, University of Colorado at Boulder.
John C. DeFries, University of Colorado at Boulder
Richard K. Olson, University of Colorado at Boulder
Daniel R. Leopold, University of Colorado at Boulder
Janice M. Keenan, University of Denver
Bruce F. Pennington, University of Denver
References
- Achenbach TM, Rescorla LA. Manual for ASEBA School-age Forms and Profiles. Burlington, VT: University of Vermont Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychological Bulletin. 1997;121:65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: Executive functioning, impairment, and comorbidity. Journal of Clinical Child and Adolescent Psychology. 2013;42:161–173. doi: 10.1080/15374416.2012.734259. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Murphy K. Attention-deficit hyperactivity disorder: A clinical workbook. 2. New York, NY: Guilford Press; 1998. [Google Scholar]
- Bauermeister JJ, Barkley RA, Martinez JV, Cumba E, Ramirez RR, Reina G, Salas CC. Time estimation and performance on reproduction tasks in subtypes of children with attention deficit hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2005;34:151–162. doi: 10.1207/s15374424jccp3401_14. [DOI] [PubMed] [Google Scholar]
- Carlson CL, Mann M. Sluggish cognitive tempo predicts a different pattern of impairment in the attention deficit hyperactivity disorder, predominantly inattentive type. Journal of Clinical Child and Adolescent Psychology. 2002;31:123–129. doi: 10.1207/S15374424JCCP3101_14. [DOI] [PubMed] [Google Scholar]
- Case R, Kurland M, Goldberg J. Operational efficiency and the growth of short-term memory span. Journal of Experimental Child Psychology. 1982;33:386–404. [Google Scholar]
- DeFries JC, Singer SM, Foch TT, Lewitter FI. Familial nature of reading disability. British Journal of Psychiatry. 1978;132:361–367. doi: 10.1192/bjp.132.4.361. [DOI] [PubMed] [Google Scholar]
- Denckla MB, Rudel RG. Rapid “automatized” naming (R.A.N): dyslexia differentiated from other learning disabilities. Neuropsychologia. 1976;14:471–479. doi: 10.1016/0028-3932(76)90075-0. [DOI] [PubMed] [Google Scholar]
- Dishion T. The peer context of troublesome child and adolescent behavior. In: Leone PE, editor. Understanding troubled and troubling youth. Newbury Park, CA: Sage; 1990. pp. 128–153. [Google Scholar]
- French JW, Ekstrom RG, Price LA. Manual for a kit of reference tests for cognitive factors. Princeton, NJ: Educational Testing Service; 1963. [Google Scholar]
- Frick PJ, Lahey BB, Applegate B, Kerdyck L, Ollendick T, Hynd GW, Barkley RA. DSM-IV field trials for the disruptive behavior disorders: symptom utility estimates. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:529–539. doi: 10.1097/00004583-199405000-00011. [DOI] [PubMed] [Google Scholar]
- Garner AA, Marceaux JC, Mrug S, Patterson C, Hodgens B. Dimensions and correlates of attention deficit/hyperactivity disorder and sluggish cognitive tempo. Journal of Abnormal Child Psychology. 2010;38:1097–1107. doi: 10.1007/s10802-010-9436-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon M. The Gordon Diagnostic System. DeWitt, NY: Gordon Systems; 1983. [Google Scholar]
- Harrington KM, Waldman ID. Evaluating the utility of sluggish cognitive tempo in discriminating among DSM-IV ADHD Subtypes. Journal of Abnormal Child Psychology. 2010;38:173–184. doi: 10.1007/s10802-009-9355-8. [DOI] [PubMed] [Google Scholar]
- Hartman CA, Willcutt EG, Rhee SH, Pennington BF. The relation between sluggish cognitive tempo and DSM-IV ADHD. Journal of Abnormal Child Psychology. 2004;32:491–503. doi: 10.1023/b:jacp.0000037779.85211.29. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Carte ET, Fan C, Jassy JS, Owens EB. Neuropsychological functioning of girls with attention-deficit/hyperactivity disorder followed prospectively into adolescence: evidence for continuing deficits? Neuropsychology. 2007;21:263–273. doi: 10.1037/0894-4105.21.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP, Carte ET, Sami N, Treuting JJ, Zupan BA. Preadolescent girls with attention-deficit/hyperactivity disorder: II. Neuropsychological performance in relation to subtypes and individual classification. Journal of Consulting and Clinical Psychology. 2002;70:1099–1111. doi: 10.1037//0022-006x.70.5.1099. [DOI] [PubMed] [Google Scholar]
- Huang-Pollock CL, Nigg JT, Carr TH. Deficient attention is hard to find: applying the perceptual load model of selective attention to attention deficit hyperactivity disorder subtypes. Journal of Child Psychology and Psychiatry. 2005;46:1211–1218. doi: 10.1111/j.1469-7610.2005.00410.x. [DOI] [PubMed] [Google Scholar]
- Keenan JM, Betjemann RS, Olson RK. Reading comprehension tests vary in the skills they assess: Differential dependence on decoding and oral comprehension. Scientific Studies of Reading. 2008;12:281–300. [Google Scholar]
- Lahey BB, Applegate B, McBurnett K, Biederman J, Greenhill L, Hynd GW, Richters J. DSM-IV field trials for attention deficit hyperactivity disorder in children and adolescents. American Journal of Psychiatry. 1994;151:1673–1685. doi: 10.1176/ajp.151.11.1673. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: generating new hypotheses. Journal of Abnormal Psychology. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Schaughency EA, Atkins MS, Murphy HA, Hynd G, Lorys-Vernon A. Dimensions and types of attention deficit disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27:330–335. doi: 10.1097/00004583-198805000-00011. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Stein MA, Loney J, Trapani C, Nugent K, Baumann B. Validity of DSM-IV attention-deficit/hyperactivity disorder for younger children. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:695–702. doi: 10.1097/00004583-199807000-00008. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Schaughency EA, Frame CL, Strauss CC. Teacher ratings of attention problems in children experimentally classified as exhibiting attention deficit disorder with and without hyperactivity. Journal of the American Academy of Child Psychiatry. 1985;24:613–616. doi: 10.1016/s0002-7138(09)60064-9. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Schaughency EA, Hynd GW, Carlson CL, Nieves N. Attention deficit disorder with and without hyperactivity: comparison of behavioral characteristics of clinic-referred children. Journal of the American Academy of Child and Adolescent Psychiatry. 1987;26:718–723. doi: 10.1097/00004583-198709000-00017. [DOI] [PubMed] [Google Scholar]
- Logan GD, Schachar RJ, Tannock R. Impulsivity and inhibitory control. Psychological Science. 1997;8:60–64. [Google Scholar]
- Ludwig HT, Matte B, Katz B, Rohde LA. Do sluggish cognitive tempo symptoms predict response to methylphenidate in patients with attention-deficit/hyperactivity disorder-inattentive type? Journal of Child and Adolescent Psychopharmacology. 2009;19:461–465. doi: 10.1089/cap.2008.0115. [DOI] [PubMed] [Google Scholar]
- McBurnett K, Pfiffner LJ, Frick PJ. Symptom properties as a function of ADHD type: an argument for continued study of sluggish cognitive tempo. Journal of Abnormal Child Psychology. 2001;29:207–213. doi: 10.1023/a:1010377530749. [DOI] [PubMed] [Google Scholar]
- McGrath LM, Pennington BF, Shanahan MA, Santerre-Lemmon LE, Barnard HD, Willcutt EG, Olson RK. A multiple deficit model of reading disability and attention-deficit/hyperactivity disorder: Searching for shared cognitive deficits. Journal of Child Psychology and Psychiatry. 2011;52:547–557. doi: 10.1111/j.1469-7610.2010.02346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milich R, Balentine AC, Lynam DR. ADHD combined type and ADHD predominantly inattentive type are distinct and unrelated disorders. Clinical Psychology-Science and Practice. 2001;8:463–488. [Google Scholar]
- Neeper R, Lahey BB. Identification of two dimensions of cognitive deficits through the factor analysis of teacher ratings. School Psychology Review. 1984;13:485–490. [Google Scholar]
- Neeper R, Lahey BB. The Children’s Behavior Rating Scale: A factor analytic developmental study. School Psychology Review. 1986;15:277–288. [Google Scholar]
- Pennington BF. From single to multiple deficit models of developmental disorders. Cognition. 2006;101:385–413. doi: 10.1016/j.cognition.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Penny AM, Waschbusch DA, Klein RM, Corkum P, Eskes G. Developing a measure of sluggish cognitive tempo for children: content validity, factor structure, and reliability. Psychological Assessment. 2009;21:380–389. doi: 10.1037/a0016600. [DOI] [PubMed] [Google Scholar]
- Pillow DR, Pelham WE, Jr, Hoza B, Molina BS, Stultz CH. Confirmatory factor analyses examining attention deficit hyperactivity disorder symptoms and other childhood disruptive behaviors. Journal of Abnormal Child Psychology. 1998;26:293–309. doi: 10.1023/a:1022658618368. [DOI] [PubMed] [Google Scholar]
- Reich W, Welner Z, Herjanic B. Diagnostic Interview for Children and Adolescents - IV. North Towanda Falls, NY: Multi-Health System, Inc; 1997. [Google Scholar]
- Setterberg S, Bird H, Gould M. Parent and Interviewer version of the Children’s Global Assessment Scale. New York: Columbia University; 1992. [Google Scholar]
- Shanahan MA, Pennington BF, Yerys BE, Scott A, Boada R, Willcutt EG, DeFries JC. Processing speed deficits in attention deficit/hyperactivity disorder and reading disability. Journal of Abnormal Child Psychology. 2006;34:585–602. doi: 10.1007/s10802-006-9037-8. [DOI] [PubMed] [Google Scholar]
- Siegel LS, Ryan EB. The development of working memory in normally achieving and subtypes of learning disabled children. Child Development. 1989;60:973–980. doi: 10.1111/j.1467-8624.1989.tb03528.x. [DOI] [PubMed] [Google Scholar]
- Stanford LD, Hynd GW. Congruence of behavioral symptomatology in children with ADD/H, ADD/WO, and learning disabilities. Journal of Learning Disabilities. 1994;27:243–253. doi: 10.1177/002221949402700406. [DOI] [PubMed] [Google Scholar]
- Todd RD, Rasmussen ER, Wood C, Levy F, Hay DA. Should sluggish cognitive tempo symptoms be included in the diagnosis of attention-deficit/hyperactivity disorder? Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:588–597. doi: 10.1097/00004583-200405000-00012. [DOI] [PubMed] [Google Scholar]
- Wahlstedt C, Bohlin G. DSM-IV defined inattention and sluggish cognitive tempo: Independent and interactive relations to neuropsychological factors and comorbidity. Child Neuropsychology. 2010;16:350–365. doi: 10.1080/09297041003671176. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Manual for the Wechsler Intelligence Scale for Children, Revised. New York, NY: The Psychological Corporation; 1974. [Google Scholar]
- Wechsler D. Manual for the Wechsler Intelligence Scale for Children, Third Edition. San Antonio, TX: The Psychological Corporation; 1991. [Google Scholar]
- Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490–499. doi: 10.1007/s13311-012-0135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcutt EG, Betjemann RS, McGrath LM, Chhabildas NA, Olson RK, DeFries JC, Pennington BF. Etiology and neuropsychology of comorbidity between RD and ADHD: The case for multiple-deficit models. Cortex. 2010;46:1345–1361. doi: 10.1016/j.cortex.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcutt EG, Boada R, Riddle MW, Chhabildas N, DeFries JC, Pennington BF. Colorado Learning Difficulties Questionnaire: Validation of a parent-report screening measure. Psychological Assessment. 2011;23:778–791. doi: 10.1037/a0023290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcutt EG, Nigg JT, Pennington BF, Solanto MV, Rohde LA, Tannock R, Lahey BB. Validity of DSM-IV attention-deficit/hyperactivity disorder dimensions and subtypes. Journal of Abnormal Psychology. 2012;121:991–1010. doi: 10.1037/a0027347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcutt EG, Pennington BF, Duncan L, Smith SD, Keenan JM, Wadsworth SJ, DeFries JC. Understanding the complex etiology of developmental disorders: Behavioral and molecular genetic approaches. Journal of Developmental and Behavioral Pediatrics. 2010;31:533–544. doi: 10.1097/DBP.0b013e3181ef42a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcutt EG, Pennington BF, Olson RK, Chhabildas N, Hulslander J. Neuropsychological analyses of comorbidity between reading disability and attention deficit hyperactivity disorder: In search of the common deficit. Developmental Neuropsychology. 2005;27:35–78. doi: 10.1207/s15326942dn2701_3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


