Abstract
Objective
Routine moderate-to-vigorous physical activity (MVPA) is associated with better health outcomes; the purpose of this work was to evaluate healthy preschooler physical activity patterns with objective measurement.
Methods and Procedures
An objective prospective study of fifty normally-developing children 3–5 years old who were ≥50th and <95th BMI percentile and enrolled in a family-based healthy lifestyle study in 2011–2012. Participants wore a tri-axial accelerometer for 7 continuous days. Outcome measures consisted of wear time examining four common MVPA patterns: isolated spurt (IS), isolated sustained activity (ISA), clustered spurt (CS), and clustered sustained activity (CSA).
Results
Participants were 4.3 years, 56% female, 52% African-American, and 26% overweight. Forty-five children met wear time criteria. On average, children spent 14.5% of wake-wear time in MVPA, requiring 11.3 hours to complete 90% of their daily MVPA. Children spent the majority of MVPA in CS (62.1%, followed by CSA (20.1%). Remaining MVPA was spent in IS (15.5%) and ISA (2.3%).
Conclusion
It takes most of the waking day for preschoolers to attain their PA. They engage in short spurts of small duration, in four common MVPA patterns. Utilizing this method could better characterize preschooler physical activity needs in practice and policy guidelines.
Keywords: Physical activity, preschool children, accelerometer, obesity, sedentary behavior
INTRODUCTION
The prevalence of pediatric obesity has almost tripled for preschool-aged children (ages 2–5) since the initial 1971–1974 National Health and Nutrition Examination Survey (NHANES) report (5.0% versus 12.1%).1,2 These percentages are even higher among Latino (16.2%) and black (18.9%) preschool-aged children.2 Childhood obesity prevention is crucial as it has been well documented that overweight and obese children are at an increased risk to be overweight adults.3 The Institute of Medicine’s (IOM’s) Committee on Accelerating Progress in Obesity Prevention recommendations include the need for state and local child care and early childhood education regulators to establish requirements to increase current physical activity guidelines.4
Young children grow in a non-linear fashion beginning with infants who initially grow linearly and then enter a period where height velocity exceeds weight velocity, resulting in a Body Mass Index (BMI) curve that decreases, reaches a nadir, and then begins to increase again. This pattern in BMI trajectory is referred to as “adiposity rebound” and generally occurs between the ages of 5 and 7 years.5 Children who rebound early seem to be at an increased risk of obesity and adverse health outcomes.6 Active children appear to experience adiposity rebound at a later age, which is associated with improved health throughout the lifespan.6 Subsequently, PA likely plays an important role in the timing of adiposity rebound and perhaps later BMI status of a child.7
Although moderate-to-vigorous physical activity (MVPA) is associated with better health outcomes,8,9 current recommendations for young children have provided only general guidance. For example, the American Academy of Pediatrics (AAP) recommends that parents encourage free play “in some form of physical activity” for at least 60 minutes every day10 while the American Heart Association (AHA) suggests that all children ages 2 and up should engage in at least 60 minutes of developmentally appropriate MVPA a day.11 However, the National Association for Sport and Physical Education’s (NASPE) guidelines provide specific recommendations for the amount of active play time for certain age groups, specifically for infants, toddlers and preschoolers. According to the NASPE, preschool-aged children should engage in at least 60 minutes of structured and 60 minutes of unstructured PA daily and should avoid sedentary behavior for more than 60 minutes at a time, excluding naps.12 The recommendations for these health-focused organizations differ based on unique objectives.
Despite AAP, AHA, and NASPE recommendations, it remains unclear how much PA preschoolers attain daily. Studies indicate daily MVPA in preschool-aged children ranges from less than 30 minutes to well over 4 hours per day13–20 and that boys generally exhibit a greater amount of MVPA per day than girls.14,15,21,22 These studies utilized different methods for capturing preschooler physical activity, likely explaining such large variances. Accelerometry remains the most popular and acceptable method of objective PA assessment.21,23 An accelerometer is a small device that is generally worn around the waist or wrist that measures acceleration of body movements to document muscle movement and derived PA intensity. Although accelerometers have the potential to be informative, different brands, epoch length, activity cut points, and wear time criteria lead to varying conclusions.
The purpose of this study was to characterize MVPA patterns in healthy American preschoolaged children using a tri-axial accelerometer and extended wear time criteria to inform methods to capture physical activity consistently in young children.
METHODS AND PROCEDURES
Study Population and Design
Participants were enrolled in a pilot study designed for parents with preschool-aged children conducted at a local community recreation center in Nashville, Tennessee. A total of 50 parent-child dyads participated in a culturally sensitive, family-based obesity prevention pilot study. Inclusion criteria included: (1) healthy, non-obese, normally developing child aged 3 to 5 years; (2) child BMI percentile ≥50th and <95th; (3) not participating in another healthy lifestyle program(s); (4) availability for contact by telephone; and (5) plans to remain in the city for the subsequent six months. Children were weighed and measured to ensure they met BMI eligibility criteria, informed consent was read aloud, and any questions were answered before obtaining written consent. Child assent was not obtained because of age; however, children were enrolled in research only when their primary caregivers provided consent and children willingly participated during data collection.24 This study was approved by the Vanderbilt University Institutional Review Board (Institutional Review Board No.100591).
Measures
Physical Activity
Physical activity was objectively measured using the ActiGraph GT3X+ accelerometer (ActiGraph, LLC, Pensacola,FL). The ActiGraph GT3X+ is a small, water resistant, lightweight monitor that is worn on an elastic belt around the waist and measures locomotion in 3 axes.25,26 In our study each accelerometer was programmed to collect raw data continuously at a sample rate of 40 Hz and was analyzed in 15-second epochs to capture the activity of young children. This monitor has been validated for use in preschool-aged and deemed an objective method of assessing PA levels.27–32 Accelerometers were distributed at baseline data collection to all study participants with instruction to wear them for 7 consecutive days including when they slept, bathed, and performed aquatic activities. Monitors were returned and data were downloaded using manufacturer provided software (ActiLife). Validated threshold values for preschool age children were used to derive time spent in rest, sedentary, light, moderate, and vigorous activity.28
Height and Weight
Body weight was measured twice, while wearing light clothing without shoes after voiding, to the nearest 0.1 kg on a research, precision-grade scale with digital read out calibrated digital scale (model 876) (Seca, Hanover, MD). Height without shoes was measured twice to the nearest 0.1 cm with a free standing stadiometer with moveable headboard (model 217) (Seca, Hanover, MD). Baseline measurements were collected at the community center by trained study staff.
Body Mass Index
BMI (weight [kg]/height [m2])33 and BMI percentiles for age and gender were calculated using the Centers for Disease Control and Prevention calculator.
Demographic Characteristics
Parent/legal guardian participants completed a demographic survey that included date of birth, gender, and race/ethnicity of primary caregiver and child, as well as highest primary caregiver education level and annual household income.
Accelerometry Statistical Analysis
Data were processed using the R statistical package.34 Each epoch was marked as wearing versus not wearing35 and waking versus sleeping (sustained periods that lack variability in counts per epoch). Time spent in sedentary and PA waking epochs were derived according to validated and commonly-cited activity counts for preschool age children by Pate et al: >37.5 to 420 for light, 420 to 842 for moderate, and >842 for vigorous PA intensity per 15 second epoch.28 We were interested in how MVPA was distributed across the day, thus only days with ≥20 hours marked as wear time were considered valid despite the fact that many studies have a minimum wear time criteria of about 6 hours per day. The proportion of waking wear time was calculated for each of the activity levels in children with at least four valid days (including at least one weekend day). For each period of MVPA, the duration was calculated as well as the intervals between episodes.
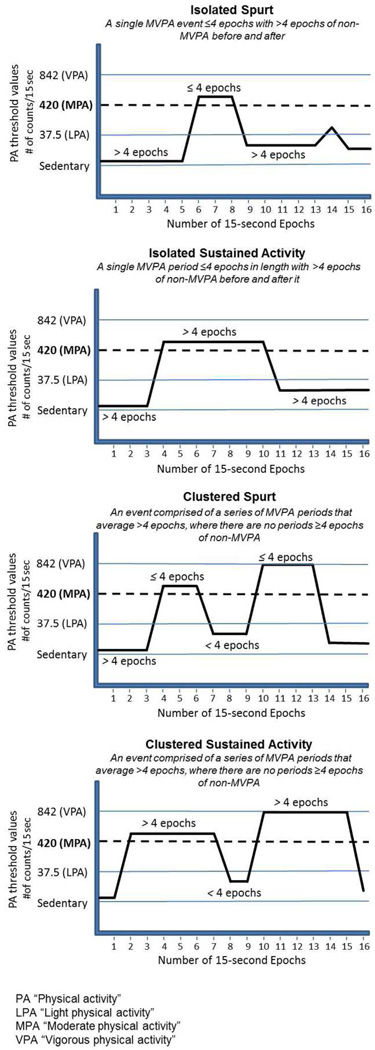
In visual examination of graphs of individuals' activity (counts) plotted against time of day, it was clear there were differences between the data of children and adults. Adults not only had lower amounts of MVPA, if present it tended to be all at the same time of day, whereas the children had MVPA was more sporadic and across the waking day. When the variances of counts were calculated the pattern was confirmed; the children had higher variances and four visually distinct patterns. This led to the classification system below (Figure 1):
Isolated Spurt: a single MVPA period ≤4 epochs in length with >4 epochs of non-MVPA before and after it.
Isolated Sustained Activity: a single MVPA period >4 epochs in length with >4 epochs of non-MVPA before and after it.
Clustered Spurt: an event comprised of a series of MVPA periods that average ≤4 epochs, where there are no periods ≥4 epochs of non-MVPA.
Clustered Sustained Activity: an event comprised of a series of MVPA periods that average >4 epochs, where there are no periods ≥4 epochs of non-MVPA.
Figure 1. Visual Description of the Four MVPA Patterns.
Visual definition of each of the four identified MVPA patterns. Dashed horizontal line denotes MVPA threshold value.
Two-tailed t-tests for the significance of the differences between the means of two independent groups with equal or unequal variances were conducted to examine differences in MVPA and MVPA categories in males and females. Sample size was not informed by a power analysis because there was no existing research investigating MVPA patterns for preschoolers. We describe common patterns that emerged from data collected.
RESULTS
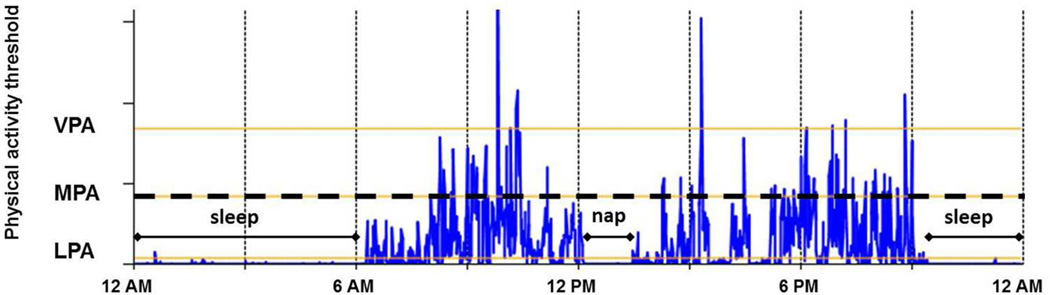
Baseline participant demographics are summarized in Table 1. Participating children had a mean age of 4.3 years. Approximately, half were female, half were African American, and a quarter were overweight. Forty-five of the 50 returned accelerometers met wear time criteria (≥20 hours/day for ≥4 days). Although we were not powered to detect small differences in demographics between those who did and those who did not meet wear time criteria, analyses and inspection suggested that the groups were similar. On average, accelerometers were worn for 23.7 (SD 0.4, min 22.6, max 24) hours/day for 6.7 (SD 0.8, min 4, max 8) days (Table 2). Children spent 52% of their wake-wear time in sedentary behavior (mean 7.4 hours, SD 0.7, min 5.9, max 9.2), about 33% in light PA (mean 4.7 hours, SD 0.5, min 3.7, max 5.7), and 15% in MVPA (mean 2.1, SD 0.5, min 0.8, max 3.1). On average, it took 11.3 (SD 1.3, min 8.9, max 14.1) hours for children to achieve 90% of their MVPA demonstrating minimal variation. There was no statistically significant difference in the average daily percent wake-wear time in MVPA between boys and girls (95% CI for mean difference [−3.74, 0.38]; p = 0.11). Refer to Figure 2 for a sample 24-hour recording from a child participant.
Table 1. Participant Demographic Characteristics.
Basic demographic information of child participants.
| Participants (N=50) | |||
|---|---|---|---|
| n (%) | Normal weight | Overweight | |
| Female | 28 (56) | 22 | 6 |
| Male | 22 (44) | 15 | 7 |
| Age | |||
| 3 years | 19 (38) | 14 | 5 |
| 4 years | 21 (42) | 16 | 5 |
| 5 years | 10 (20) | 7 | 3 |
| Weight categorya | |||
| Normal weight | 37 (74) | ||
| Overweight | 13 (26) | ||
| Mean BMI (SD) | 16.3 (0.8) | ||
| Race | |||
| Hispanic | 2 (4) | 1 | 1 |
| Ethnicity | |||
| Black | 26 (52) | 18 | 8 |
| White | 15 (30) | 14 | 1 |
| Bi-racial | 7 (14) | 4 | 3 |
| Other | 2 (4) | 1 | 1 |
| Annual household income | |||
| < $15K | 14 (28) | 9 | 5 |
| ≥ $15K, < $25K | 13 (26) | 9 | 4 |
| ≥ $25K, < $35K | 5 (10) | 2 | 3 |
| ≥ $35K, < $50K | 2 (4) | 1 | 1 |
| ≥ $50K, < $75K | 5 (10) | 5 | 0 |
| ≥ $75K | 9 (18) | 9 | 0 |
| Don't know/Prefer not to answer | 2 (4) | 2 | 0 |
| Highest education level of primary caregiver | |||
| No high school diploma | 6 (12) | 5 | 1 |
| High school diploma/GED | 8 (16) | 3 | 5 |
| Some college, no degree | 17 (34) | 11 | 6 |
| College, associate, or technical degree | 12 (24) | 11 | 1 |
| Master’s degree | 7 (14) | 7 | 0 |
Child categories were defined by using the child BMI percentile adjusted for age and gender: normal, ≥50th to <85th; overweight, 85th to <95th percentile
Table 2. Accelerometry Averages by Gender.
Average accelerometry wear time and percent wake-wear time by MVPA patterns
| Overall | Girls | Boys | P-valuee | 95% CI for difference between girls and boys |
||
|---|---|---|---|---|---|---|
| Total valid days (SD) | 6.7 (0.8) | 6.5 (0.9) | 7.0 (0.6) | 0.06 | −0.92 | 0.01 |
| Daily wear time in hours (SD) | 23.7 (0.4) | 23.6 (0.4) | 23.8 (0.3) | 0.11 | −0.4 | 0.04 |
| Daily wake–wear time in hours (SD) | 14.1 (0.9) | 14.1 (0.8) | 14.2 (1.0) | 0.68 | −0.63 | 0.42 |
| Percent wake–wear time Sedentary (SD) | 52.5 (4.7) | 53.3 (5.2) | 51.5 (3.9) | 0.20 | −0.98 | 4.6 |
| Percent wake–wear time in LPAa (SD) | 33.0 (2.5) | 33.0 (2.7) | 33.1 (2.3) | 0.87 | −1.67 | 1.42 |
| Percent wake–wear time in MPAb (SD) | 10.0 (2.2) | 9.6 (2.5) | 10.5 (1.7) | 0.18 | −2.15 | 0.42 |
| Percent wake–wear time in VPAc (SD) | 4.5 (1.6) | 4.1 (1.7) | 4.9 (1.3) | 0.08 | −1.75 | 0.11 |
| Percent wake–wear time in MVPAd (SD) | 14.5 (3.5) | 13.7 (4.0) | 15.4 (2.6) | 0.11 | −3.74 | 0.38 |
LPA, Light Physical Activity
MPA, Moderate Physical Activity
VPA, Vigorous Physical Activity
MVPA, Moderate-to-Vigorous Physical Activity
Two-tailed t-test
Figure 2. Sample 24-Hour Activity Recording.
Sample 24-hour activity recording from a child participant. Spikes above the dashed horizontal line denote MVPA.
While in MVPA, children spent 62.1% (SD 6.7%) of their time in clustered spurts, followed by 20.1% (8.7%) in clustered sustained activities, 15.5% (SD 4.3%) in isolated spurts, and 2.3% (SD 1.1%) in isolated sustained activities (Table 3). Overall, the data showed differences in boys and girls, in MVPA pattern distribution. Girls spent a significantly greater percentage of their MVPA in isolated spurts (16.9% vs. 13.8%; 95% CI for mean difference [0.7, 5.42]; p = 0.01), and they also spent a significantly smaller percentage of their MVPA in clustered sustained activity than boys (23.6% vs. 17.1%; 95% CI for mean difference [−11.43, −1.54]; p = 0.01) (Table 3).
Table 3. MVPA Category Distribution as a Percentage of Total MVPA.
MVPA category distribution as a percentage of total daily MVPA by gender.
| Overall | Girls | Boys | P-valuea | 95% CI for difference between girls and boys |
||
|---|---|---|---|---|---|---|
| Isolated Spurt % (SD) | 15.5 (4.3) | 16.9 (4.8) | 13.8 (2.9) | 0.01 | 0.7 | 5.42 |
| Isolated Sustained Activity % (SD) | 2.3 (1.1) | 2.6 (1.3) | 2.0 (0.7) | 0.08 | −0.08 | 1.14 |
| Clustered Spurt % (SD) | 62.1 (6.7) | 63.5 (5.5) | 60.6 (7.7) | 0.15 | −1.09 | 6.87 |
| Clustered Sustained Activity % (SD) | 20.1 (8.7) | 17.1 (7.8) | 23.6 (8.7) | 0.01 | −11.43 | −1.54 |
two-tailed t-test
MVPA, Moderate-to-Vigorous Physical Activity
According to a descriptive examination of the PA patterns throughout the day, both isolated and clustered spurts maintained a relatively equal percentage across the day (morning (6am–11am); midday (11am–4pm); and evening (4pm–9pm)). However, results indicate that the percentage for both isolated and clustered sustained patterns increased throughout the day. The activity levels of the non-MVPA breaks within the clusters was largely (85%) light PA. The remainder (15%) being sedentary. Results found no statistically significant difference in MVPA patterns between weekdays and weekends.
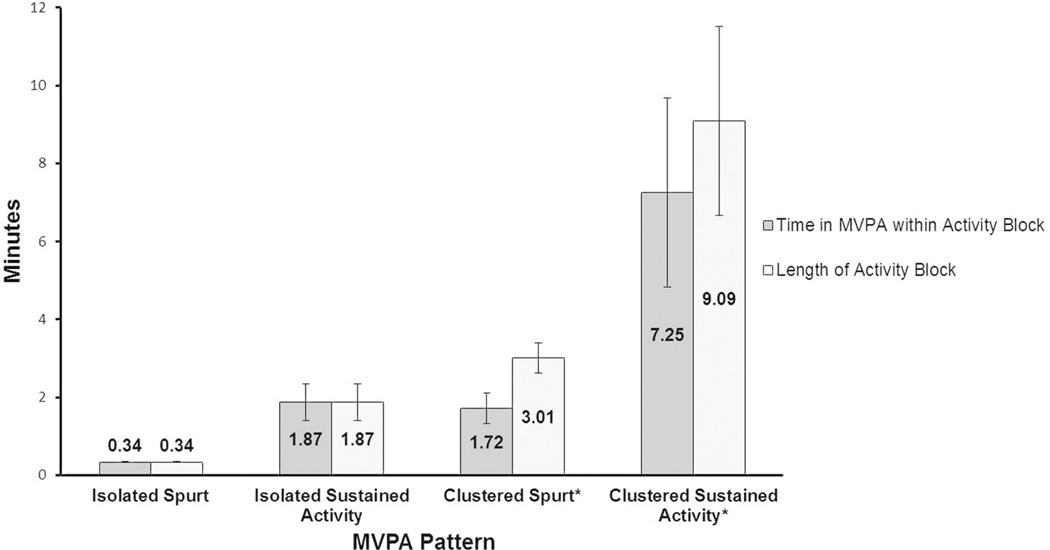
Figure 3 illustrates the duration of each MVPA category type among participants, demonstrating the average length of each activity block and time in MVPA during this block. An isolated spurt on average lasted 0.3 (SD 0.01) minutes and occurred 53.1 (SD 7.3) times per day. Isolated sustained activity, on the other hand, lasted 1.9 (SD 0.5) minutes and occurred 1.5 (SD 0.6) times per day. The most common MVPA category, clustered spurt, averaged 3.0 (SD 0.4) minutes in length, 1.7 (SD 0.3) minutes of which were MVPA, and occurred on average 44.6 (SD 8.5) times per day. Clustered sustained activities averaged 9.1 (SD 2.4) minutes in length, 7.3 (SD 2.0) minutes of which were MVPA, and occurred 3.5 (SD 1.6) times per day.
Figure 3. MVPA Pattern Duration Among Participants.
Isolated pattern events are comprised solely of MVPA. Clustered pattern events are comprised of MVPA and non-MVPA periods. Length of activity block is the summation of both MVPA and non-MVPA periods, while MVPA within an activity block is the summation of only MVPA periods.
DISCUSSION
There is no doubt that PA plays a pivotal role in the prevention of pediatric obesity. However, little is known about what PA patterns exist in preschool-aged children. Understanding these PA patterns may help preschools, policy makers, day care centers, and parents create developmentally appropriate PA programs. In this study, we identified four preschooler MVPA patterns (isolated spurt, isolated sustained activity, clustered spurt, and clustered sustained activity). Our findings provide further evidence that children incorporate MVPA throughout most of their waking hours unlike adults that exhibit discrete and lesser amounts of MVPA, if at all, in a particular time of the day. Using the accelerometry method we describe and the MVPA pattern definitions with preschool-aged children could inform future research to combat high levels of sedentary behavior, increase developmentally appropriate physical activity, and promote healthy habits at critical windows of child development.
Regarding research methods, our accelerometry wear time criteria of at least 20 hours per day for a minimum of 4 days is unique; most studies with preschool-aged children have a wear time criteria that ranges from 4 to 12 hours per day.13–16,20 Some investigators have suggested that as little as 3 hours a day may provide a reliable measure of activity in 5 year old children;36 however, our study found that preschool-aged children take roughly 11 hours with minimal variation, to complete 90% of their daily MVPA. To our knowledge this has not been shown previously. As future research including preschool age range evolves, taking these findings into consideration could assist in establishing prolonged minimum wear-time when objectively assessing physical activity in this age group.
Moreover, the majority of accelerometry-based studies present their findings as total MVPA/day to assess if children meet current MVPA recommendations or to test the effect of the intervention. It is generally accepted that preschool-aged children exhibit sporadic PA.37–39 Several studies have suggested that boys accrue more daily MVPA than girls.14,15,21,22 In this study, no difference in the total amount of MVPA between girls and boys was detected, however their MVPA patterns were statistically distinct. Boys spent a greater percentage of their MVPA in clustered sustained activity and a lesser percentage of their MVPA in isolated spurts compared to girls. Although it was not evaluated in our cohort, it would be interesting to examine if these changes in MVPA pattern distribution later lead to a difference in total MVPA. Further study will be needed to understand how this could influence daycare providers and preschool programs.
This study suggests that more frequent MVPA periods of relatively short duration throughout the entire day (morning, afternoon, and early evening) naturally occurs in preschool age children. The IOM 2012 report recommends that licensed child care providers provide physical activity opportunities such as free or outdoor play for 15 minutes every hour and as a minimum, require half-day programs provide 30 minutes total and full-day programs provide 60 minutes total of physical activity.4 Utilizing our study’s current findings strengthen these recommendations. Given that spurt-like MVPA patterns comprise over 75% of young children’s daily MVPA and last anywhere from seconds to 1.7 minutes in duration, developing daycare or preschool physical activity programs considering games such as short relay races that incorporate the notion of the game of “tag” (brief bursts of running) might be most aligned with preschool child development. Future directions could include utilizing the method presented here to develop and test physical activity programs for preschool age children, similar to the SPARK curriculum.40
LIMITATIONS
Although our racially and socioeconomically diverse study participants were extremely compliant and provided a robust accelerometry dataset, limitations existed. First, our sample size was small. This highlights the importance of the statistically significant findings in differences in boys and girls patterns of MVPA, but does not provide sufficient power to test other differences that could have existed. Although accelerometers can objectively capture movement associated with PA, different models and makes, wear time criteria, and threshold cut points have decreased cross-study generalizability. To date, there is no gold standard for accelerometry data analysis. Although we used validated threshold preschool age cut points that are common among researchers in this field, they are not used by all.28
CONCLUSION
Applying an extended wear-time methodology, preschool-aged children participate in MVPA throughout the majority of their waking hours and engage in four common patterns of MVPA, that we describe for the first time here. In general, boys seem to spend a greater percentage of their MVPA in clustered sustained activities while girls spend a greater percentage of their MVPA in isolated spurts. Applying this methodology of capturing MVPA patterns in preschool age children could inform future research designed to promote obesity prevention and enhanced physical activity practices for preschoolers.
What’s Known on This Subject
Physical activity (PA) improves health outcomes and is foundational to obesity prevention.
Preschool-age children require a minimum of 60 minutes of PA/day.
Heterogeneity of PA measurement makes it challenging to guide practice and policy to promote PA for preschoolers.
What This Study Adds
On average it takes 11 hours over the course of a day for preschoolers to attain their PA.
They engage in short spurts of small duration.
This informs a new method of understanding preschooler PA.
Acknowledgements
Rachel M. Ruiz: Ms. Ruiz was responsible for analysis and interpretation of the data, acquisition of data, drafting the manuscript and critical revision of the manuscript for important intellectual content.
Dustin Tracy: Mr. Tracy was responsible for analysis and interpretation of the data, critical revision of the manuscript for important intellectual content, and statistical analysis.
Evan C. Sommer: Mr. Sommer was responsible for analysis and interpretation of the data, critical revision of the manuscript for important intellectual content, and statistical analysis.
Shari L. Barkin: Dr. Barkin was responsible for conceptualization and design of the pilot study, analysis and interpretation of the data, critical revision of the manuscript, for intellectual content, obtaining funding, and supervision. Dr. Barkin had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
All authors read and approved the final manuscript.
Funding Source: The project described was supported by Award Number U01 HL03620-03 from the National Heart, Lung, And Blood Institute, the Eunice Kennedy Shriver National Institute of Child Health and Development and the Office of Behavioral and Social Sciences Research. Additional funding sources include: Vanderbilt Medical Scholars Program and NIH grant number UL1 RR 024975, The Vanderbilt Institute for Clinical and Translation research and NIH grant number Ul1 TR 000445, and the Vanderbilt Center for Diabetes Translation Research and NIH grant number P30 DK 092986.
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Footnotes
Conflict of Interest:
Competing interests: the authors have no competing interests.
References
- 1.Ogden CC M. [Accessed September 8, 2011];Prevalence of Obesity Among Children and Adolescents: United States, Trends 1963–1965 through 2007–2008. 2010 http://www.cdc.gov/nchs/data/hestat/obesity_child_07_08/obesity_child_07_08.htm.
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. Jama. 2012 Feb 1;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008 Sep;9(5):474–488. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 4.The National Academies. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. 2012 [PubMed] [Google Scholar]
- 5.Rolland-Cachera MF, Deheeger M, Bellisle F, Sempe M, Guilloud-Bataille M, Patois E. Adiposity rebound in children: a simple indicator for predicting obesity. Am J Clin Nutr. 1984 Jan;39(1):129–135. doi: 10.1093/ajcn/39.1.129. [DOI] [PubMed] [Google Scholar]
- 6.Taylor RW, Grant AM, Goulding A, Williams SM. Early adiposity rebound: review of papers linking this to subsequent obesity in children and adults. Curr Opin Clin Nutr Metab Care. 2005 Nov;8(6):607–612. doi: 10.1097/01.mco.0000168391.60884.93. [DOI] [PubMed] [Google Scholar]
- 7.Janz KF, Levy SM, Burns TL, Torner JC, Willing MC, Warren JJ. Fatness, physical activity, and television viewing in children during the adiposity rebound period: the Iowa Bone Development Study. Prev Med. 2002 Dec;35(6):563–571. doi: 10.1006/pmed.2002.1113. [DOI] [PubMed] [Google Scholar]
- 8.Janz KF, Kwon S, Letuchy EM, et al. Sustained effect of early physical activity on body fat mass in older children. Am J Prev Med. 2009 Jul;37(1):35–40. doi: 10.1016/j.amepre.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. Jama. 2012 Feb 15;307(7):704–712. doi: 10.1001/jama.2012.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Academy of Pediatrics. [Accessed May 13, 2012];Physical Activity: Make the Right Choice for Your Child. 2012 http://www.healthychildren.org/English/healthy-living/fitness/Pages/Physical-Activity-Make-the-Right-Choice-for-Your-Child.aspx.
- 11.American Heart Association. [Accessed May 14, 2012];Physical Activity and Children. 2012 http://www.heart.org/HEARTORG/GettingHealthy/PhysicalActivity/Physical-Activity-and-Children_UCM_304053_Article.jsp.
- 12.National Association for Sport and Physical Education. [Accessed May 14, 2012];Active Start: A Statement of Physical Activity Guidelines for Cihldren From Birth to Age 5. 2012 2nd http://www.aahperd.org/naspe/standards/nationalGuidelines/ActiveStart.cfm.
- 13.Dwyer GM, Hardy LL, Peat JK, Baur LA. The validity and reliability of a home environment preschool-age physical activity questionnaire (Pre-PAQ) Int J Behav Nutr Phys Act. 2011;8:86. doi: 10.1186/1479-5868-8-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kwon S, Janz KF, Burns TL, Levy SM. Effects of adiposity on physical activity in childhood: Iowa Bone Development Study. Med Sci Sports Exerc. 2011 Mar;43(3):443–448. doi: 10.1249/MSS.0b013e3181ef3b0a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beets MW, Bornstein D, Dowda M, Pate RR. Compliance with national guidelines for physical activity in U.S. preschoolers: measurement and interpretation. Pediatrics. 2011 Apr;127(4):658–664. doi: 10.1542/peds.2010-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Loprinzi PD, Trost SG. Parental influences on physical activity behavior in preschool children. Prev Med. 2010 Mar;50(3):129–133. doi: 10.1016/j.ypmed.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 17.Taylor RW, Murdoch L, Carter P, Gerrard DF, Williams SM, Taylor BJ. Longitudinal study of physical activity and inactivity in preschoolers: the FLAME study. Med Sci Sports Exerc. 2009 Jan;41(1):96–102. doi: 10.1249/MSS.0b013e3181849d81. [DOI] [PubMed] [Google Scholar]
- 18.Williams HG, Pfeiffer KA, O'Neill JR, et al. Motor skill performance and physical activity in preschool children. Obesity (Silver Spring) 2008 Jun;16(6):1421–1426. doi: 10.1038/oby.2008.214. [DOI] [PubMed] [Google Scholar]
- 19.Ruiz R, Gesell SB, Buchowski MS, Lambert W, Barkin SL. The relationship between hispanic parents and their preschool-aged children's physical activity. Pediatrics. 2011 May;127(5):888–895. doi: 10.1542/peds.2010-1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burgi F, Meyer U, Granacher U, et al. Relationship of physical activity with motor skills, aerobic fitness and body fat in preschool children: a cross-sectional and longitudinal study (Ballabeina) Int J Obes (Lond) 2011 Jul;35(7):937–944. doi: 10.1038/ijo.2011.54. [DOI] [PubMed] [Google Scholar]
- 21.Oliver M, Schofield GM, Kolt GS. Physical activity in preschoolers: understanding prevalence and measurement issues. Sports medicine. 2007;37(12):1045–1070. doi: 10.2165/00007256-200737120-00004. [DOI] [PubMed] [Google Scholar]
- 22.Grontved A, Pedersen GS, Andersen LB, Kristensen PL, Moller NC, Froberg K. Personal characteristics and demographic factors associated with objectively measured physical activity in children attending preschool. Pediatric Exercise Science. 2009 May;21(2):209–219. doi: 10.1123/pes.21.2.209. [DOI] [PubMed] [Google Scholar]
- 23.Pate RR, O'Neill JR, Mitchell J. Measurement of physical activity in preschool children. Med Sci Sports Exerc. 2010 Mar;42(3):508–512. doi: 10.1249/MSS.0b013e3181cea116. [DOI] [PubMed] [Google Scholar]
- 24.Office of Human Subjects Research. [Accessed May 14, 2012];Regulations and Ethical Guidelines. 2005 http://ohsr.od.nih.gov/guidelines/45cfr46.html.
- 25.Vanhelst J, Mikulovic J, Bui-Xuan G, et al. Comparison of two ActiGraph accelerometer generations in the assessment of physical activity in free living conditions. BMC Res Notes. 2012;5:187. doi: 10.1186/1756-0500-5-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sasaki JE, John D, Freedson PS. Validation and comparison of ActiGraph activity monitors. Journal of science and medicine in sport / Sports Medicine Australia. 2011 Sep;14(5):411–416. doi: 10.1016/j.jsams.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 27.Puyau MR, Adolph AL, Vohra FA, Butte NF. Validation and calibration of physical activity monitors in children. Obes Res. 2002 Mar;10(3):150–157. doi: 10.1038/oby.2002.24. [DOI] [PubMed] [Google Scholar]
- 28.Pate RR, Almeida MJ, McIver KL, Pfeiffer KA, Dowda M. Validation and calibration of an accelerometer in preschool children. Obesity (Silver Spring) 2006 Nov;14(11):2000–2006. doi: 10.1038/oby.2006.234. [DOI] [PubMed] [Google Scholar]
- 29.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998 May;30(5):777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 30.Trost SG, Way R, Okely AD. Predictive validity of three ActiGraph energy expenditure equations for children. Med Sci Sports Exerc. 2006 Feb;38(2):380–387. doi: 10.1249/01.mss.0000183848.25845.e0. [DOI] [PubMed] [Google Scholar]
- 31.Welk GJ, Blair SN, Wood K, Jones S, Thompson RW. A comparative evaluation of three accelerometry-based physical activity monitors. Med Sci Sports Exerc. 2000 Sep;32(9 Suppl):S489–S497. doi: 10.1097/00005768-200009001-00008. [DOI] [PubMed] [Google Scholar]
- 32.Bassett DR, Jr, Ainsworth BE, Swartz AM, Strath SJ, O'Brien WL, King GA. Validity of four motion sensors in measuring moderate intensity physical activity. Med Sci Sports Exerc. 2000 Sep;32(9 Suppl):S471–S480. doi: 10.1097/00005768-200009001-00006. [DOI] [PubMed] [Google Scholar]
- 33.Mei Z, Grummer-Strawn LM, Pietrobelli A, Goulding A, Goran MI, Dietz WH. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. American Journal of Clinical Nutrition. 2002:7597–7985. doi: 10.1093/ajcn/75.6.978. [DOI] [PubMed] [Google Scholar]
- 34.Choi L, Liu Zhouwen, Matthews C, Buchowski M. Package 'Physical Activity'. 2013 [Google Scholar]
- 35.Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011 Feb;43(2):357–364. doi: 10.1249/MSS.0b013e3181ed61a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Penpraze VR, MacLean CM, Montgomery C, et al. Monitoring of physical activity in young children: how much is enought? Pediatric Exercise Science. 2006;18:483–491. doi: 10.1123/pes.18.4.483. [DOI] [PubMed] [Google Scholar]
- 37.Nilson A, Ekeland U, Yngve A, Sjoestroem M . Assessing physical activity among children with accelerometers using different time sampling intervals and placements. Pediatr Exerc Sci. 2002;14(1):87–96. [Google Scholar]
- 38.Pellegrini AD, Smith PK. Physical activity play: the nature and function of a neglected aspect of playing. Child Dev. 1998 Jun;69(3):577–598. [PubMed] [Google Scholar]
- 39.Bailey RC, Olson J, Pepper SL, Porszasz J, Barstow TJ, Cooper DM. The level and tempo of children's physical activities: an observational study. Med Sci Sports Exerc. 1995 Jul;27(7):1033–1041. doi: 10.1249/00005768-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 40.Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Faucette N, Hovell MF. The effects of a 2-year physical education program (SPARK) on physical activity and fitness in elementary school students. Sports, Play and Active Recreation for Kids. American journal of public health. 1997 Aug;87(8):1328–1334. doi: 10.2105/ajph.87.8.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]