Abstract
Objectives
The purpose of this study was to compare the prevalence of metabolic syndrome diagnosed using four different definitions in the Lithuanian urban population and to determine their association with ischemic heart disease.
Methods
Data from the survey performed in the framework of the HAPIEE (Health, Alcohol, and Psychosocial factors In Eastern Europe) study were presented. A random sample of 7087 individuals aged 45-72 years was screened in 2006-2008.
Results
In Lithuanian urban population of Kaunas city aged 45-72 years, the highest prevalence of metabolic syndrome was determined according to the new Joint Interim Societies (JIS) definition (44.1% of men and 48.7% of women). After adjusting for age, education, smoking habits the metabolic syndrome (irrespective of definition) was associated with a significantly higher risk of ischemic heart disease.
Conclusion
All four metabolic syndrome definitions were associated with ischemic heart disease risk; however odds of this disease were higher in people with metabolic syndrome defined by American Heart Association National Heart Lung Blood Institute definition and National Cholesterol Education program Adult Treatment Panel III definition, than by the new JIS definition.
Keywords: metabolic syndrome, odds of ischemic heart disease
Introduction
The metabolic syndrome is a cluster of metabolic abnormalities including abdominal obesity, glucose intolerance, arterial hypertension and dyslipidemia. It has been demonstrated that individuals with metabolic syndrome are at increased risk of cardiovascular events, as well as diabetes (Wilson et al. 2005; Eddy et al. 2008). Various diagnostic criteria have been proposed by different organizations over the past decade. Most recently, these have come from the International Diabetes Federation (IDF) and the American Heart Association and National Heart Lung and Blood Institute (AHA/NHLBI). The main controversy was that the metabolic syndrome had had too many definitions and there was a lack of clarity about its role and value in clinical practice (Eckel et al. 2010). The last Joint Interim Societies (JIS) definition of the metabolic syndrome was proposed in 2009 by the several major organizations, such as, the IDF Task Force on Epidemiology and Prevention, AHA/NHLBI, American Heart Association, World Heart Federation, International Atherosclerosis Society, and International Association for the Study of Obesity. These organizations prepared joint scientific statement, which harmonized criteria of metabolic syndrome components and unified definition: a single set of cut points would be used for all components except waist circumference (national or regional cut points for waist circumference can be used) (Alberti et al. 2009). However, the expert groups decided, that further studies exploring the relation of the waist circumference thresholds to metabolic risk and cardiovascular outcomes in different populations are encouraged (Alberti et al. 2009).
In the interim, the prevalence of the metabolic syndrome within individual cohorts varies with the definition used (Daskalopoulou et al. 2006; Day 2007; Alberti et al. 2009). Previous our research data showed that there is lack of diagnostic concordance between different definitions: in Kaunas population aged 35-64 years, the prevalence of the metabolic syndrome diagnosed using IDF definition was higher in comparison with the World Health Organization (WHO) definition and third Report of the National Cholesterol Education Program-Adult Treatment Panel (NCEP-ATP III) definition (Luksiene et al. 2010). The prevalence of metabolic syndrome diagnosed by AHA/NHLBI definition and by the new JIS definition and their association with cardiovascular disease has not been studied in Kaunas city middle-aged and elderly population before. Thus, the prevalence of the metabolic syndrome varies according to the definition used (NCEP-ATP III, AHA/NHLBI, IDF and new JIS), and it is very important in identifying people at increased risk for the development of cardiovascular diseases (McNeil et al. 2005; Athyros et al. 2007; Day 2007; Li et al. 2008; Athyros et al. 2010). In Lithuania also it is very important to identify people at increased risk for the development of cardiovascular diseases, because data of Health Statistics of Lithuania informed that more than half of all deaths (55.4%) in 2009 were caused by diseases of the circulatory system and the largest percentage of deaths due those diseases was caused by ischemic heart disease (61.9%) (Health Statistics of Lithuania, 2009).
Our aim was to compare the prevalence of the metabolic syndrome diagnosed using the NCEP-ATP III, IDF, AHA/NHLBI and the new JIS definitions of the metabolic syndrome in the Lithuanian urban population and to determine their association with ischemic heart disease (IHD).
Methods
Study design
Data from the survey performed in the framework of the international Health, Alcohol and Psychosocial factors In Eastern Europe (HAPIEE) study (Peasey et al. 2006) are presented. This survey was carried out in Kaunas which is second largest city in Lithuania with population 348,624. A random sample of 10,940 Kaunas men and women aged 45-72 years, stratified by gender and age was randomly selected from Lithuanian population register; 7,087 responders (3,218 men and 3,869 women) participated in this health survey and were screened from 2006 to 2008. Thus, the response rate was 64.8%. Data from 6,752. subjects (3,051 men and 3,701 women) who were examined for all five metabolic syndrome components, were approved for statistics analysis. Data of 335 were excluded from the statistical analysis because of incomplete information about the metabolic syndrome components. The study was approved by the ethics committee at the University College London, UK and by the regional ethics committee at Kaunas University of Medicine (Lithuania).
Measurements
Blood pressure was measured three times with an osicillometric device (Omron M5-I), and the average values were used for the analysis.
Waist circumference was measured (without upper clothes) by a standard meter with an accuracy of 0.5 cm. The tape was applied at the marked level halfway between the costal margin and iliac crest. The tape was pulled taut. The participant was asked to breath out gently, to let his/her arms hang loosely by his/her sides and to look straight ahead (to ensure he/she does not contract his/her muscles or hold his/her breath). A measurement is taken to the nearest 0.1 cm and recorded. The measurement had taken in mid-expiration, when the abdominal muscles are maximally relaxed.
Biochemical analyses for glucose and lipids were done for responders (fasting for at least for 12 hours) on an empty stomach. Concentration of glucose in capillary blood was determined by an individual glucometer “Glucotrend” (Norkus et al. 2000). Blood serum samples were analysed centrally in one batch in the WHO Regional Lipid Reference Centre, Institute of Clinical and Experimental Medicine, Prague (Czech Republic). Lipid concentrations in serum were measured on a Roche COBAS MIRA autoanalyser, using a conventional enzymatic method with reagents from Boehringer Mannheim Diagnostics and Hoffman-La Roche. WHO Regional Lipid Reference Centre was responsible for quality control of biochemistry measures.
The diagnostic criteria for the metabolic syndrome by four definitions (NCEP-ATP III, AHA/NHLBI, IDF, and JIS) are show in Table 1.
Table 1. Diagnostics criteria for the metabolic syndrome by four definitions.
| Components | NCEP-ATP III (Third Report of the NCEP, 2002) |
AHA/NHLBI (Grundy et al. 2005) |
IDF (Zimmet et al. 2005) |
JIS (Alberti et al. 2009) |
|---|---|---|---|---|
| Fasting plasma glucose | ≥6.1 mmol/L | ≥5.6 mmol/L or T2DM |
≥5.6 mmol/L or T2DM |
≥5.6 mmol/L or T2DM |
|
| ||||
| Waist circumference | ≥102 cm (men) | ≥102 cm (men) | ≥94 cm (men) | ≥94 cm (men) |
| ≥88 cm (women) | ≥88cm (women) | ≥80 cm (women) | ≥80 cm (women) | |
|
| ||||
| Blood pressure | ≥130/85 mm Hg | ≥130/85 mm Hg or receiving treatment |
≥130/85 mm Hg or receiving treatment |
≥130/85 mm Hg or receiving treatment |
|
| ||||
| Triglycerides | ≥1.7 mmol/L | ≥1.7 mmol/L or receiving treatment |
≥1.7 mmol/L or receiving treatment |
≥1.7 mmol/L or receiving treatment |
|
| ||||
| High-density lipoprotein cholesterol | <1.0 mmol/L (men) <1.3 mmol/L (women) |
<1.0 mmol/L (men) <1.3 mmol/L (women) or receiving treatment |
<1.0 mmol/L (men) <1.3 mmol/L (women) or receiving treatment |
<1.0 mmol/L (men) <1.3 mmol/L (women) or receiving treatment |
|
| ||||
| Definition of metabolic syndrome and number of components for diagnosis | ≥3 of the components above | ≥3 of the components above | Central obesity (increased waist circumference) plus ≥2 others components | ≥3 of the components above |
AHA/NHLBI American Heart Association and National Heart Lung and Blood Institute,
IDF International Diabetes Federation,
JIS Joint Interim Societies,
NCEP-ATPIII National Cholesterol Education Program Adult Treatment Panel III,
T2DM type 2 diabetes mellitus
IHD was determined according to the data of medical history, Rose GA questionnaire (Rose et al. 1982) and electrocardiogram (ECG) data coded by the Minnesota codes (Prineas et al. 1982). The following these criteria IHD was determined: 1) documented history of myocardial infarction (MI) and (or) ischemic changes on electrocardiogram (ECG) coded by the Minnesota codes (MC) 1-1 or 1-2; 2) angina pectoris was defined by G. Rose questionnaire (without MI and (or) MC 1-1 or 1-2; 3) ECG findings by MC 1-3, 4-1, 4-2, 4-3, 5-1, 5-2, 5-3, 6-1, 6-2, 7-1, 8-3 (without MI and (or) MC 1-1, 1-2 and without angina pectoris).
Diabetes mellitus was determined according to the answers of responders to the question “Has a doctor ever told that you have diabetes?”.
Lifestyle habits were evaluated using frequency questionnaire. The standard questionnaire included questions regarding the respondent’s age, health, social status (education, marital status), smoking status, and etc. Education was measured by six education levels: primary, incomplete secondary, secondary, vocational, college and university. The responders with primary, incomplete secondary, secondary, and vocational education were considered as having secondary and lower education. Smoking habits were assessed according to a current smoking status. A subject who smoked at least one cigarette per day was classified as current smoker.
Statistical analysis
All data were analyzed in male and female groups separately. Association between categorical variables was estimated by Chi squared (χ2) test. The difference was considered to be statistically significant when p < 0.05.
The direct method was used for age standardization of prevalence of the IHD, metabolic syndrome (irrespective of definition) and their components, education level and smoking status among men and women using European population as a standard (Ahmad et al. 2001). Multivariable logistic regression analysis was performed to determine the independent associations between the metabolic syndrome (by four definitions) and IHD, in consideration of age, education level and smoking status, expressed as odds ratio (OR) with 95% confidence intervals (CI). Independent variables in the logistic regression models were categorical variables: metabolic syndrome status, education, smoking and continuous variable age. Statistical packages EPIINFO6, SPSS version 13.0 were used.
Results
Table 2 presents characteristics of the study population. The prevalence of the metabolic syndrome (irrespective of definition) was higher in women than in men (p<0.001). The highest prevalence of the metabolic syndrome was determined according to the new JIS definition. The prevalence of components of metabolic syndrome such as elevated blood pressure and elevated triglycerides level were higher in men than in women (p<0.001). However, elevated fasting glucose (≥5.6 mmol/L), elevated waist circumference levels (irrespective of definition) and reduced HDL cholesterol level were lower in men than in women (p<0.05). Smoking rate was significantly (p<0.001) higher in men than in women groups.
Table 2. Characteristics of the HAPIEE study on the middle and older age Lithuanian population of Kaunas city screened in 2006-2008.
| Characteristics | Men N = 3051 (%) |
Women N=3701 (%) |
Chi square (χ2) value (p value) |
|---|---|---|---|
| Age groups, | χ2=4.14 (p>0.05) | ||
| 45-54 years | 23.6 | 25.6 | |
| 55-64 years | 40.1 | 39.8 | |
| ≥65 years | 36.3 | 34.6 | |
|
| |||
| Ischemic heart disease, | |||
| 45-54 years | 7.8 | 11.6 | χ2=6.71 (p=0.01) |
| 55-64 years | 17.9 | 19.4 | χ2=0.99 (p>0.05) |
| >64 years | 25.8 | 27.0 | χ2=0.45 (p>0.05) |
| All | 15.1 | 17.3 | χ2=5.84 (p=0.016) |
|
| |||
| Metabolic syndrome defined by: | |||
| NCEP-ATPIII | 27.2 | 33.9 | χ2=35.2 (p<0.001) |
| AHA/NHLBI | 33.4 | 41.5 | χ2=46.7 (p<0.001) |
| IDF | 39.4 | 47.2 | χ2=41.4 (p<0.001) |
| JIS | 44.1 | 48.7 | χ2=14.3 (p<0.001) |
|
| |||
| Elevated fasting glucose or T2DM levels, | |||
| ≥ 5.6 mmol/L | 53.8 | 56.2 | χ2=3.94 (p=0.047) |
| ≥ 6.1 mmol/L | 31.9 | 31.0 | χ2=0.63 (p>0.05) |
|
| |||
| Elevated waist circumference levels, | |||
| ≥ 94 cm (men) or ≥ 80 cm (women) | 53.9 | 71.0 | χ2=211.0 (p<0.001) |
| ≥ 102 cm (men) or ≥ 88 cm (women) | 27.7 | 49.2 | χ2=323.7 (p<0.001) |
|
| |||
| Elevated blood pressure (systolic ≥130 and/or diastolic ≥85 mm Hg) or receiving treatment, | 83.3 | 69.9 | χ2=164.0 (p<0.001) |
|
| |||
| Elevated triglycerides level (≥1.7 mmol/L) or receiving treatment, | 29.0 | 25.1 | χ2=12.98 (p<0.001) |
|
| |||
| Reduced HDL cholesterol level (<1.0 mmol/L (men) or <1.30 mmol/L (women)) or receiving treatment, | 12.1 | 23.4 | χ2=143.0 (p<0.001) |
|
| |||
| Level of education, | χ2=87.9 (p<0.001) | ||
| Secondary and lowerb | 46.6 | 37.2 | |
| College | 19.3 | 28.8 | |
| University | 34.1 | 34.0 | |
|
| |||
| Smoking, | 34.9 | 13.1 | χ2=449.5v (p<0.001) |
AHA/NHLBI American Heart Association and National Heart Lung and Blood Institute,
HAPIEE Health, Alcohol and Psychosocial factors In Eastern Europe,
HDL high-density lipoprotein,
IDF International Diabetes Federation, JIS Joint Interim Societies,
NCEP-ATPIII National Cholesterol Education Program Adult Treatment Panel III,
T2DM type 2 diabetes mellitus.
Data were standardized using European standard population (Ahmad et al. 2001)
Secondary and lower - secondary, vocational, primary, incomplete secondary levels of education
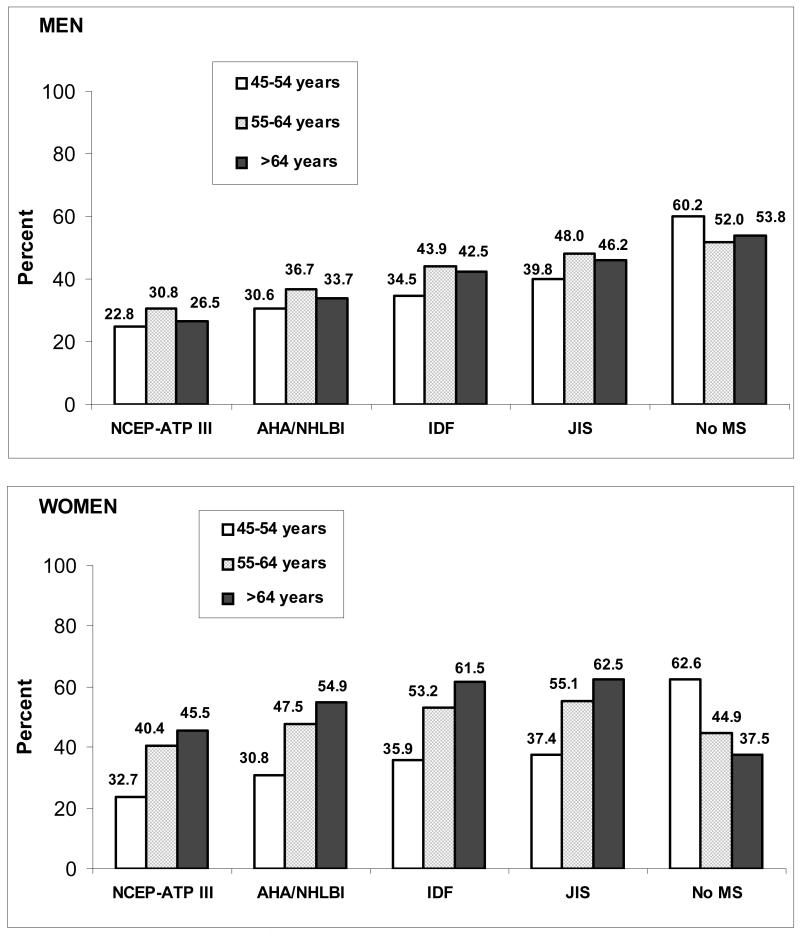
The distribution of Kaunas city inhabitants with and without any metabolic syndrome diagnosed using four definitions (NCEP-ATP III, AHA/NHLBI, IDF, and JIS) by 10-year age group is depicted in Fig. 1. In male and female groups, the prevalence of the metabolic syndrome significantly increased with age (p<0.05). On the contrary, the proportions of individuals without any metabolic syndrome (no MS) significantly decreased with age (p<0.001). The highest prevalence of the metabolic syndrome (irrespective of definition) was recorded in men aged 55-64 years and in women aged 65 years and older.
Fig. 1. Distribution of responders with the metabolic syndrome diagnosed using four definitions and without any metabolic syndrome by 10-year age groups (the Health, Alcohol and Psychosocial factors In Eastern Europe study screened in Lithuanian population of Kaunas city, 2006-2008).
AHA/NHLBI American Heart Association and National Heart Lung and Blood Institute, IDF International Diabetes Federation, JIS Joint Interim Societies, MS metabolic syndrome, NCEP-ATP III National Cholesterol Education Program Adult Treatment Panel III, No MS without any metabolic syndrome.
Chi-Square (χ2) test showed a significant association of metabolic syndrome (irrespective of definition) with age among men and women (χ2 8.59-18.2; p<0.05 among men and χ2 117.8-143.2; p<0.001 among women).
Chi-Square (χ2) test showed a significant association of metabolic syndrome (irrespective of definition) with gender only in age groups of 54-64 years and >64 years (respectively χ2 8.19-21.3; p≤0.04 and χ2 50.2-89.9; p<0.001).
The lack of diagnostic concordance between different definitions of the metabolic syndrome is by now (Day 2007; Eckel et al. 2010), thus we calculated the agreement and disparity in the diagnoses of the metabolic syndrome using the NCEP-ATP III definition, AHA/NHLBI definition, the IDF definition and the JIS definition. Among HAPIEE study responders who qualified for the diagnosis of the metabolic syndrome by at least one of these definitions (1386 men and 1967 women), more than half appeared to be diagnosable by all four definitions: 54.8% of men and 69.2% of women. It is important, that the new JIS definition was defined for all responders who qualified for the diagnosis of the metabolic syndrome by at least one of these four definitions. 17.4% of men and 16.1% of women appeared to be diagnosable by three definitions (mostly by JIS, IDF and AHA/NHLBI). 27.8% of men and 14.7% of women were identified as having the metabolic syndrome using two definitions (only by JIS and IDF definitions were present 24.8% of men and 13.9% of women; by JIS and AHA/NHLBI definitions were present 3.0% of men and 0.8% of women).
Metabolic syndrome and odds of ischemic heart disease
The age-standardized IHD was identified for 15.1% of men and for 17.3% of women (p=0.016).
Among men and women without any metabolic syndrome the age-standardized rate of IHD was significantly lower than among persons who qualified for the diagnosis of the metabolic syndrome by at least one of these four definitions: in men group 11.6% vs. 19.5% respectively (p<0.001); in women group 14.7% vs. 20.8% respectively (p<0.001). The gender differences were defined only in persons without any metabolic syndrome group: in men the age-standardized rate of IHD was significantly lower than in women (p=0.007).
After adjusting for age, education level and smoking habits, men and women diagnosed with the metabolic syndrome (irrespective of definition) had significantly higher odds of having IHD as compared to those without metabolic syndrome by the same definition (Table 3). Nonetheless, AHA/NHLBI and NCEP-ATPIII definitions were more predictive of IHD, than the IDF and the new JIS definition.
Table 3. Prevalence of ischemic heart disease and odds of ischemic heart disease among 45-72 years persons in relation to the presence of the metabolic syndrome according to four definitions (the Health, Alcohol and Psychosocial factors In Eastern Europe study, screened in Lithuanian population of Kaunas city, 2006-2008).
| Metabolic syndrome definitions | Men | Women | ||
|---|---|---|---|---|
|
| ||||
| Percent# | OR (95% CI) | Percent# | OR (95% CI) | |
| NCEP-ATP III | ||||
| No | 12.3 | 1 | 15.5 | 1 |
| Yes | 22.3 | 2.04 (1.67-2.49) | 21.8 | 1.44 (1.21-1.70) |
|
| ||||
| AHA/NHLBI | ||||
| No | 11.8 | 1 | 14.8 | 1 |
| Yes | 21.8 | 2.06 (1.70-2.50) | 21.6 | 1.50 (1.27-1.77) |
|
| ||||
| IDF | ||||
| No | 12.1 | 1 | 14.9 | 1 |
| Yes | 19.7 | 1.78 (1.47-2.16) | 20.6 | 1.42 (1.20-1.68) |
|
| ||||
| JIS | ||||
| No | 11.6 | 1 | 14.7 | 1 |
| Yes | 19.5 | 1.88 (1.55-2.28) | 20.8 | 1.43 (1.21-1.70) |
AHA/NHLBI American Heart Association and National Heart Lung and Blood Institute,
CI confidence interval,
IDF International Diabetes Federation,
JIS Joint Interim Societies
NCEP-ATPIII National Cholesterol Education Program Adult Treatment Panel III,OR odds ratio,
# Data were standardized using European standard population (Ahmad et al. 2001) Odds ratios adjusted by age, education and smoking habits
Discussion
The NCEP-ATP III, AHA/NHLBI, IDF and new JIS definitions of the metabolic syndrome agree on essential components – glucose intolerance, obesity, hypertension, and dyslipidemia – but they differ in the cut-off points for the criteria of each component of the cluster and the method of combining them to define the metabolic syndrome. The major criteria of metabolic syndrome came from the NCEP-ATP III in 2001 (Third Report of the National Cholesterol Education Program 2002). NCEP-ATP III made the presence of 3 of the following 5 factors the basis for establishing the diagnosis: abdominal obesity, elevated triglyceride, reduced high density lipoprotein (HDL) cholesterol, elevated blood pressure and elevated fasting glucose. The AHA/NHLBI slightly modified NCEP-ATP III criteria, but did not mandate abdominal obesity as required risk factor as it dropped IDF. The main difference between the NCEP-ATP III, AHA/NHLBI and IDF definitions was that the IDF definition had a threshold value for waist circumference as obligatory. The IDF guidelines stressed the need to adopt different values for waist circumference measurement in different ethnic groups. Recently, IDF and AHA/NHLBI representatives held discussions to attempt to resolve the remaining differences between definitions of metabolic syndrome (Alberti et al. 2009). Both sides agreed that abdominal obesity should not be a prerequisite for diagnosis but that it is 1 of 5 criteria, so that the presence of any 3 of 5 risk factors constitutes a diagnosis of metabolic syndrome. Thus, created the new metabolic syndrome definition defined by JIS criteria are closest to IDF in that they include the same variables, but they differ in that central obesity is not an essential component.
The prevalence of the metabolic syndrome within individual cohorts varies with the definition used. In the United States, 39% of adults were classified as having the metabolic syndrome using the IDF definition, a figure that is higher than that estimated by the NCEP-ATP III definition (34.5%) (Ford 2005). Similarly, in a study done in South Australia, the prevalence of the metabolic syndrome was higher using the IDF definition (22.8%) as compared to the NCEP-ATP III definition (15%) (Adams et al. 2005). In the Greek (Mediterranean) population, the prevalence of metabolic syndrome was higher using the new JIS and IDF definitions (45.7% and 43.4% respectively) as compared to the NCEP-ATP III and AHA/NHLBI definitions (24.5% and 26.3% respectively) (Athyros et al. 2010). Results of this HAPIEE study have demonstrated that the prevalence of metabolic syndrome using new JIS and IDF definitions was higher in men and women than using the NCEP-ATP III and AHA/NHLBI definitions. One of the reasons of these differences could be that JIS and IDF definitions waist circumference criteria are higher compared with NCEP-ATP III and AHA/NHLBI waist circumference criteria.
As expected, the prevalence of the metabolic syndrome varied by age group. We found that the prevalence of the metabolic syndrome increased with age irrespective of the definitions used. The highest prevalence of the metabolic syndrome (irrespective of definition) was recorded in men aged 55-64 years and in women aged 65 years and older. These findings are similar to those of previous reports in the literature that prevalence of the metabolic syndrome increased with age (Adams et al. 2005; Athyros et al. 2010; Luksiene et al. 2010).
Recent analyses have estimated that people who have the metabolic syndrome are at increased risk of developing cardiovascular disease (McNeil et al. 2005; Cerniauskiene et al. 2005; Lorenzo et al. 2007; Nilsson et al. 2007; Luksiene et al. 2010; Athyros et al. 2010). Data show that the metabolic syndrome associated increase in the risk of cardiovascular disease may depend on the definition used (Athyros et al. 2007; Lorenzo et al. 2007; Li et al. 2008; Luksiene et al. 2010; Athyros et al. 2010). Our study has demonstrated that all four metabolic syndrome definitions provide opportunity to identify subjects with IHD however AHA/NHLBI and NCEP-ATP III definitions were more predictive of IHD, than the new JIS definition. The results from Greek (Mediterranean) population study also show that the NCEP-ATP III and AHA/NHLBI definitions were more predictive of cardiovascular disease risk than the new JIS definition (Athyros et al. 2010). One of the reasons for such differences is the lack of diagnostic concordance between different definitions for the metabolic syndrome. Recent analyses have estimated that about 30% of people appear to be diagnosed by most definitions, and about 35-40% of people diagnosed with the metabolic syndrome is only classified as such using one definition (Day 2007). Our study has demonstrated that among HAPIEE study responders aged 45-72 years who qualified for the diagnosis of the metabolic syndrome by at least one of these definitions, more than half appeared to be diagnosable by all four definitions (54.8% of men and 69.2% of women). It’s important, that the new JIS definition was defined for all responders who qualified for the diagnosis of the metabolic syndrome by at least one of these four definitions. Thus, the prospective long-term studies are needed to validate the prognostic power of these definitions of the metabolic syndrome.
In recent research literature, there are currently debates regarding the validity of the term metabolic syndrome, but most authors made a conclusion that the presence of one cardiovascular risk factor should raise suspicion that additional risk factors may also be present and encourage investigation (Day 2007; Daskalopoulou et al. 2006; Eddy et al. 2008; Alberti et al. 2009; Eckel et al. 2010). On the other hand, as the metabolic syndrome defined by the IDF definition and the new JIS definition is more prevalent in comparison with the NCEP-ATP III and AHA/NHLBI definitions, its recommends “aggressive and uncompromising” management of those classified to reduce the risk of cardiovascular disease (Adams et al. 2005; Day 2007; Alberti et al. 2009). If new JIS definition will be widespread acceptance, then there is probability that more people will receive management, including drug therapy. Our study shows that when diagnosed according to the new JIS definition, the prevalence of metabolic syndrome in Lithuanian urban population of Kaunas city aged 45-72 years, was determined in about half of the adult population. Therefore, a diagnosis of the metabolic syndrome should be used in order to find high-risk individuals to motivate for lifestyle changes, not to label low risk individuals. In particular, the metabolic syndrome is not an absolute risk indicator, because it does not contain many of the factors that determine absolute risk, for example, age, sex, cigarette smoking, and low-density lipoprotein cholesterol levels. Yet more, previous our data have showed that combination of the metabolic syndrome defined by the NCEP-ATP III definition and oxidative stress and smoking were associated with IHD among persons aged 45-64 years (Cerniauskiene et al. 2008; Luksiene et al. 2008).
As the result, the metabolic syndrome is now both a public health and a clinical problem (Alberti et al. 2009). In the public health arena, more attention must be given to modification of lifestyles, to reduce obesity and to increase physical activity. Therefore, increasing recognition of risk levels in the population with a simple focus on waist size and hypertension, along with corrected lifestyle habits (smoking, physical activity, healthy nutrition habits), are important steps in the addressing metabolic problems. At a clinical level, individual patients with the metabolic syndrome need to be identified so that their multiple risk factors, including lifestyle risk factors, can be reduced. Thus, the results of this study confirm that metabolic syndrome (irrespective of definitions) were associated with increased risk of IHD; however odds of IHD were higher in subjects with metabolic syndrome defined by AHA/NHLBI and NCEP-ATP III definitions, than by the new JIS definition. These findings may have implications regarding the choice of the definition to diagnose metabolic syndrome.
There are some limitations to our study
The authors of some studies (Buckland et al. 2008; Santos et al. 2008) suggested that life-course socioeconomic position appeared to be an important confounder in the association of the metabolic syndrome with probability of IHD. In this article, the impact of the socioeconomic status, except for education, on the IHD was not analyzed, so this is a limitation. The main limitation of this study is the cross-sectional data: cardiovascular risk profile and coronary heart disease were estimated at the same point in time and we can not certainly assert what happened first. Definitely in our further studies the follow-up data will be presented to estimate the relative risk of the new CHD cases according to cardiovascular risk profile investigated at the baseline. Also, we cannot assert that the study population of Kaunas city is perfectly representative of the general population of Lithuania.
Footnotes
Conflict of interest. The authors declare that they have no competing interests.
References
- Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- Adams RJ, Appleton S, Wilson DH, Taylor AW, Dal Grande E, Chittleborough C, et al. Population comparison of two clinical approaches to the metabolic syndrome: implications of the new International Diabetes Federation consensus definition. Diabetes Care. 2005;28:2777–2779. doi: 10.2337/diacare.28.11.2777. [DOI] [PubMed] [Google Scholar]
- Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M. Age standardization of rates: a new WHO standard. WHO; Geneva (Switzerland): 2001. (GPE Discussion Paper No. 31). [Google Scholar]
- Athyros VG, Ganotakis ES, Elisaf MS, Liberopoulos EN, Goudevenos IA, Karagiannis A. Prevalence of vascular disease in metabolic syndrome using three proposed definitions. Int J Cardiol. 2007;117:204–210. doi: 10.1016/j.ijcard.2006.04.078. [DOI] [PubMed] [Google Scholar]
- Athyros VG, Ganotakis ES, Tziomalos K, Papageorgiou AA, Anagnostis P, Griva T, et al. Comparison of four definitions of the metabolic syndrome in a Greek (Mediterranean) population. Curr Med Res Opin. 2010;26:713–719. doi: 10.1185/03007991003590597. [DOI] [PubMed] [Google Scholar]
- Buckland G, Salas-Salvadó J, Roure E, Bulló M, Serra-Majem L. Sociodemographic risk factors associated with metabolic syndrome in a Mediterranean population. Public Health Nutr. 2008;11:1372–1378. doi: 10.1017/S1368980008003492. [DOI] [PubMed] [Google Scholar]
- Cerniauskiene LR, Luksiene DI, Tamosiunas A, Reklaitiene R, Margeviciene L. Association of metabolic syndrome and oxidative stress with ischemic heart disease in middle-aged persons. Medicina (Kaunas) 2008;44:392–399. [PubMed] [Google Scholar]
- Cerniauskiene LR, Reklaitiene R, Luksiene DI, Domarkiene S, Tamosiunas A, Margevicienė L. Association of metabolic syndrome with ischemic heart disease among middle-aged Kaunas population. Medicina (Kaunas) 2005;41:435–441. [PubMed] [Google Scholar]
- Day C. Metabolic syndrome, or what you will: definitions and epidemiology. Diab Vasc Dis Res. 2007;4:32–38. doi: 10.3132/dvdr.2007.003. [DOI] [PubMed] [Google Scholar]
- Daskalopoulou SS, Athyros VG, Kolovou GD, Anagnostopoulou KK, Mikhailidis DP. Definitions of metabolic syndrome: where are we now? Curr Vasc Pharmacol. 2006;4:185–197. doi: 10.2174/157016106777698450. [DOI] [PubMed] [Google Scholar]
- Eckel RH, Alberti KG, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2010;375:181–183. doi: 10.1016/S0140-6736(09)61794-3. [DOI] [PubMed] [Google Scholar]
- Eddy DM, Schlessinger L, Heikes K. The metabolic syndrome and cardiovascular risk: implications for clinical practice. Int J Obes. 2008;32:S5–S10. doi: 10.1038/ijo.2008.28. [DOI] [PubMed] [Google Scholar]
- Ford ES. Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the U.S. Diabetes Care. 2005;28:2745–2749. doi: 10.2337/diacare.28.11.2745. [DOI] [PubMed] [Google Scholar]
- Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- Health Statistics of Lithuania 2009 . Lithuanian Ministry of Health Information. Centre of Institute of Hygiene; Vilnius: 2010. [Google Scholar]
- Li WJ, Xue H, Sun K, Song XD, Wang YB, Zhen YS, Han YF, Hui RT. Cardiovascular risk and prevalence of metabolic syndrome by differing criteria. Chinese Medical Journal. 2008;121:1532–1536. [PubMed] [Google Scholar]
- Lorenzo C, Williams K, Hunt KJ, Haffner SM. The National Cholesterol Education Program-Adult Treatment Panel III, International Diabetes Federation, and World Health Organization definitions of the metabolic syndrome as predictors of incident cardiovascular disease and diabetes. Diabetes Care. 2007;30:8–13. doi: 10.2337/dc06-1414. [DOI] [PubMed] [Google Scholar]
- Luksiene DI, Baceviciene M, Tamosiunas A, Cerniauskiene LR, Margeviciene L, Reklaitiene R. Prevalence of the metabolic syndrome diagnosed using three different definitions and risk of ischemic heart disease among Kaunas adult population. Medicina (Kaunas) 2010;46:61–69. [PubMed] [Google Scholar]
- Luksiene DI, Cerniauskiene LR, Margeviciene L, Tamosiunas A. Changes in the prevalence of metabolic syndrome and smoking habits during a 10-year period and relation between these risk factors and ischemic heart disease among men aged 45-64 years. Medicina (Kaunas) 2008;44:400–406. [PubMed] [Google Scholar]
- McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, et al. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care. 2005;28:385–390. doi: 10.2337/diacare.28.2.385. [DOI] [PubMed] [Google Scholar]
- Nilsson PM, Engström G, Hedblad B. The metabolic syndrome and incidence of cardiovascular disease in non-diabetic subjects-a population-based study comparing three different definitions. Diabet Med. 2007;24:464–472. doi: 10.1111/j.1464-5491.2007.02142.x. [DOI] [PubMed] [Google Scholar]
- Norkus A, Ostrauskas R, Sulcaitė R, Baranauskiene E, Baliutaviciene D. Classification and diagnostics of diabetes mellitus. Kaunas (Lithuania): 2000. [Google Scholar]
- Peasey A, Bobak M, Kubinova R, Malyutina S, Pajak A, Tamosiunas A, Pikhart H, Nicholson A, Marmot M. Determinants of cardiovascular diseases and other non-communicable diseases in Central and Eastern Europe: rationale and design of the HAPIEE study. BMC Public Health. 2006 doi: 10.1186/1471-2458-6-255. doi:10.1186/1471-2458-6-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prineas RJ, Crow RS, Blackburn H. The Minnesota Code manual of electrocardiographic findings. John Wright; London: 1982. [Google Scholar]
- Rose GA, Blackburn H, Gillum RF, Prineas RJ. Cardiovascular survey methods. Cardiovascular Disease Unit, WHO; Geneva (Switzerland): 1982. [Google Scholar]
- Santos AC, Ebrahim S, Barros H. Gender, socio-economic status and metabolic syndrome in middle-aged and old adults. BMC Public Health. 2008;8:62. doi: 10.1186/1471-2458-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- Wilson PW, D’Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066–3072. doi: 10.1161/CIRCULATIONAHA.105.539528. [DOI] [PubMed] [Google Scholar]
- Zimmet P, Alberti KG, Serrano Rios M. A new International Diabetes Federation worldwide definition of the metabolic syndrome: the rationale and the results. Rev Esp Cardiol. 2005;58:1371–1376. [PubMed] [Google Scholar]