Abstract
Objective
To explore an independent association between self-reported sleep duration and cause-specific mortality.
Methods
Data were obtained from the Multiethnic Cohort Study conducted in Los Angeles and Hawaii.
Results
Among 61,936 men and 73,749 women with no history of cancer, heart attack or stroke, 19,335 deaths occurred during an average 12.9 year follow-up. Shorter (≤5 h/day) and longer (≥9 h/day) sleepers of both sexes (vs. 7 h/day) had an increased risk of all-cause and cardiovascular disease (CVD) mortality, but not of cancer mortality. Multivariable hazard ratios for CVD mortality were 1.13 (95% CI 1.00-1.28) for ≤5 h/day and 1.22 (95% CI 1.09-1.35) for ≥9 h/day among men; and 1.20 (95% CI 1.05-1.36) for ≤5 h/day and 1.29 (95% CI 1.13-1.47) for ≥9 h/day among women. This risk pattern was not heterogeneous across specific causes of CVD death among men (Phetero 0.53) or among women (Phetero 0.72). The U-shape association for all-cause and CVD mortality was observed in all five ethnic groups included in the study and by subgroups of age, smoking status, and body mass index.
Conclusion
Insufficient or excessive amounts of sleep were associated with increased risk of mortality from CVD and other diseases in a multiethnic population.
Keywords: Sleep, mortality, cardiovascular disease, ethnic groups, prospective studies
Introduction
A number of prospective studies have shown that longer or shorter sleep times are positively associated with all-cause mortality (Chien et al., 2010; Ferrie et al., 2007; Gangwisch et al., 2008; Hammond, 1964; Heslop et al., 2002; Hublin et al., 2007; Ikehara et al., 2009; Kripke et al., 2002; Kripke et al., 1979; Mallon et al., 2002; Mesas et al., 2010; Patel et al., 2004; Shankar et al., 2008; Wingard and Berkman, 1983), or with cardiovascular mortality as a group (Burazeri et al., 2003; Ferrie et al., 2007; Ikehara et al., 2009; Lan et al., 2007; Patel et al., 2004; Shankar et al., 2008; Stone et al., 2009; Suzuki et al., 2009). However, only two previous investigations examined the relation of sleep duration to specific causes of death and these were limited to stroke and coronary heart disease (Amagai et al., 2004; Ikehara et al., 2009). Furthermore, no prospective investigation has considered consistency of findings across different ethnic groups or within strata defined by potential confounders, such as sedentary behavior.
Our objective was to improve the understanding of the association of sleep duration with cause-specific mortality while accounting for confounders and mediators of this relation.
Materials and Methods
Study Population
The Multiethnic Cohort (MEC) is a prospective study including 215,000 men and women, aged 45–75 years, who answered a mailed survey form in Hawaii and Los Angeles in the 1990s (Kolonel et al., 2000). A self-administered questionnaire was used to collect information on demographic characteristics, lifestyle factors (smoking, diet, physical activity, hours of sitting and sleeping), medical history and anthropometric measures. The study was approved by the institutional review boards of the University of Hawaii and the University of Southern California.
Several exclusions were applied to the analysis as follows: 13,989 participants who did not self-identify as African American, Japanese American, Latino, Native Hawaiian or white, and 8,263 participants with implausible dietary data based on total energy intake or its components. Subjects with missing or incomplete information on hours engaged in sleeping and physical activity (n=18,874), or on height or weight (n=2,343), and smoking history (n=5,224) were also excluded. Additionally, men and women were excluded who reported a personal history of heart attack, stroke, or cancer at baseline, or if a history of malignancy was obtained from a cancer registry (n=30,869), or who died within the first year of cohort entry (n=535). A total of 135,685 participants were included in the analysis.
The excluded subjects were similar to the analytical sample with regard to median follow-up time, BMI, energy intake, hours spent sleeping per day, and prevalence of smoking (see Table S1). The excluded subjects were somewhat older (by 4.9 years on average), consumed more fruits and vegetables, drank an average of 2.6 fewer grams of alcohol per day, were more likely to have a history of hypertension and/or diabetes, and were less likely to have a college education.. We were careful to adjust for these factors in our analyses.
Ascertainment of Mortality
Deaths were ascertained largely through linkage to state death-certificate (Curb et al., 1985). A total of 19,335 deaths were identified through December 31, 2007, with an average 12.9 years of follow-up. Causes of deaths were assigned according to the International Classification of Diseases, Ninth Revision (ICD-9) and Tenth Revision (ICD-10) (Table 1).
Table 1.
The coding assignments and number of deaths for cause-specific mortality among 135,685 men and women in the Multiethnic Cohort Study, 1993-2007
| Codes |
Deaths |
|||
|---|---|---|---|---|
| Cause of death | ICD-9 | ICD-10 | No. | % |
| All Causes | 19,335 | |||
| Malignant Neoplasms | 140-239 | C00-C97 | 6,772 | 35.0 |
| Cardiovascular disease | 6,610 | 34.2 | ||
| Coronary Heart Dis | 410-414, 429 | I20-I25 | 3,476 | 18.0 |
| Myocardial Infarction | 410 | I21, I22 | 1,188 | 6.1 |
| Ischemic Heart Disease | 411-414, 429 | I20, I23-25 | 2,288 | 11.8 |
| Stroke | 430-438 | I60-I69 | 1,259 | 6.5 |
| Cardiomyopathy | 425 | I42 | 252 | 1.3 |
| Cardiac Arrest | 427 | I46 | 250 | 1.3 |
| Hypertensive Heart Disease | 402-404 | I11-13 | 267 | 1.4 |
| Hypertension | 401-405 | I10, I12 | 235 | 1.2 |
| Congestive Heart Failure | 428 | I50 | 201 | 1.0 |
| Aortic Aneurysm | 441 | I71 | 130 | 0.7 |
| All other major cardiovascular disease | 394-398, 410-429, 440-447 | I05-I09, I26-I28, I30-I52, I70-I79 | 540 | 2.8 |
| Respiratory disease | 1,340 | 6.9 | ||
| Pneumonia | 480-488 | J10-J18 | 508 | 2.6 |
| Emphysema | 492 | J43 | 127 | 0.7 |
| Asthma | 493 | J45-J46 | 56 | 0.3 |
| All other chronic lower respiratory disease | 464-496 | J40-J47 | 649 | 3.4 |
| All Others | 4,613 | 23.9 | ||
| Infectious/Parasitic Dis | 001-139 | A,B | 354 | 1.8 |
| Disease of blood & blood-forming organs & certain disease involving immune mechanism | 279, 282-89 | D58, D61-86 | 62 | 0.3 |
| Diabetes | 250 | E10-E14 | 667 | 3.4 |
| Mental/Behavioral Disease | 298-299, 303 | F01-50 | 239 | 1.2 |
| Alzheimer's Disease | 331 | G30 | 172 | 0.9 |
| Parkinson's Disease | 332 | G20-G21 | 266 | 1.4 |
| Motor Neuron Disease | 335 | G12 | 92 | 0.5 |
| Peptic Ulcer | 531-533 | K25-K27 | 52 | 0.3 |
| Liver Disease | 571 | K70-K76 | 324 | 1.7 |
| Vascular Insufficiency of Intestine | 557 | K55 | 74 | 0.4 |
| Musculoskeletal Disease | 710-730 | M00-86 | 136 | 0.7 |
| Kidney Disease | 581-586 | N03-05, N17-19, N26 | 246 | 1.3 |
| Accidents | 800-929 | V01-X59, Y85-89 | 381 | 2.0 |
| Suicide | 950-956 | X60-X84 | 131 | 0.7 |
| In situ, benign neoplasms | 227, 230-239 | D10-D36, D37-D48 | 121 | 0.6 |
Abbreviation: ICD-9, Ninth Revision of the International Classification of Diseases; ICD-10, Tenth Revision of the International Classification of Diseases.
Data Description
Sleep duration including naps (h/day) in the year prior to cohort entry was ascertained using six categories: five hours or less, six, seven, eight, nine, and ten hours or more. For this analysis, the two longest sleeping groups were collapsed as ≥9 h/day. Participants were also asked to record hours spent in sitting activities, including transportation, work, meals, watching television; and other leisure activities, such as reading, playing cards and sewing, as well as hours spent engaging in physical activity. Physical activity was categorized in three domains, including ‘strenuous sports’, ‘vigorous work’, and ‘moderate activity’. Metabolic equivalents (METs) for physical activity were computed by assigning 4.0 METs for moderate activities and 7.2 for vigorous work and strenuous sports (Institute of Medicine, 2005). Body mass index (weight divided by height (kg/cm2)) was computed from self-reported weight and height.
Statistical Analysis
We compared sleep duration with respect to several demographic characteristics and lifestyle factors of interest. Age-adjusted means and percentages for basic characteristics and lifestyle factors were calculated through age standardization across 5-year age groups. Cox proportional hazard models with age as the time metric was used to examine the association of sleep duration with mortality after adjustment for potential confounders. Analysis of sleep duration and mortality was stratified by sex since cause-specific mortality was distributed differently among men and women. Age at cohort entry (grouped as 45-49, 50-54, 55-60, 60-64, 65-69, ≥70 years) and ethnicity (African American, Japanese American, Latino, Native Hawaiian, white) were adjusted as strata variables. Smoking adjustment included the average number of cigarettes/day, average number of cigarettes squared, indicator variables for former and current smokers, number of years smoked (time dependent), number of years since quitting (time dependent), and interaction terms consisting of race/ethnicity with the following variables: average number of cigarettes, average number of cigarettes squared, smoking status, and number of years smoked (Haiman et al., 2006).
The following variables were considered as potential confounders: education level (less than college, college graduate or higher, missing), marital status (married, else, missing), prevalent diabetes at baseline (no, yes), prevalent hypertension at baseline (no, yes), energy intake (above and equal or below the median: 2,184 Kcal/day for men, and 1,747 Kcal/day for women), alcohol intake (above and equal or below the median: 2.8 g/day for men and 0 g/day for women), physical activity (quartiles; 0.1-15.3, 15.4-33.3, 33.4-63.9, and ≥64.0 METs/week for men, 0.1-9.9, 10.0-20.7, 20.8-45.9, ≥46.0 METs/week for women), and hours sitting watching television (<1 hour, 1-4 hours, ≥5 hours, missing).
To examine whether the association pattern between sleep duration and cause-specific mortality differed between causes, the heterogeneity of the sleep effect was tested in case-only models. The category with the largest number of deaths was used as the comparison group, with competing risk models in which each cause of death was considered as a separate event (Therneau and Grambsch, 2000). A Wald test was used to compare the parameters between causes with degrees of freedom equal to 4(g-1) where g is the number of case groups and 4 represents the number of parameters being tested.
Stratified analyses of participant characteristics were conducted for all-cause and CVD mortality. Men and women were combined in the stratified analyses to retain study power, as no statistical interaction was found between sex and sleep duration on the risk of all-cause mortality or CVD mortality (P's >0.1). The Wald statistic for cross-product terms was used to test the significance of interaction.
All tests were two-sided, and P < 0.05 was considered statistically significant. Software SAS version 9.2 software was used (SAS Institute, Inc., Cary, North Carolina).
Results
The majority of participants (83%) reported sleeping between 6 and 8 h/day (Table 2). White and Japanese men and women were more likely than other ethnic groups to sleep between 6 and 8 h/day; whereas, African-Americans and Native Hawaiians averaged fewer hours of sleep. Men and women older than 70 years of age were more likely than younger men and women to sleep ≥ 9 h/day or ≤ 5 h/day. Men and women sleeping ≤ 5 h/day or ≥ 9 h/day were more likely than average sleepers to be married, have prevalent diabetes or hypertension, be a current smoker, obese and less physically active or more sedentary, and to consume more calories. Light alcohol drinkers and nondrinkers tended to sleep fewer hours than alcohol drinkers.
Table 2.
Distribution of self-reported daily sleeping hours (row percentage) by selected characteristics among 135,685 men and women in the Multiethnic Cohort Study, 1993-1996a
| Variable | Age-adjusted row percentage |
|||||
|---|---|---|---|---|---|---|
| Daily sleeping |
||||||
| ≤5 hr | 6 hr | 7 hr | 8 hr | ≥9 hr | P-valueb | |
| Number of subjects (Row %) | 11,841 (8.7%) | 33,711 (24.8%) | 44,711 (33.0%) | 34,110 (25.1%) | 11,312 (8.3%) | |
| Ethnicity | <0.01 | |||||
| White | 4.7 | 18.9 | 35.9 | 30.9 | 9.7 | |
| African American | 14.5 | 26.7 | 26.4 | 22.7 | 9.8 | |
| Native Hawaiian | 13.4 | 27.3 | 28.2 | 22.2 | 8.9 | |
| Japanese American | 7.9 | 30.2 | 36.4 | 20.6 | 5.0 | |
| Latino | 9.4 | 22.2 | 30.3 | 27.5 | 10.7 | |
| Age at entry, years | <0.01 | |||||
| 45-64 | 8.6 | 25.7 | 33.8 | 24.3 | 7.6 | |
| 65-69 | 8.8 | 22.8 | 31.6 | 27.0 | 9.9 | |
| 70+ | 9.4 | 22.8 | 30.2 | 27.2 | 10.3 | |
| Sex | <0.01 | |||||
| Men | 7.8 | 25.0 | 33.2 | 25.4 | 8.5 | |
| Women | 9.5 | 24.8 | 32.7 | 24.9 | 8.1 | |
| Education | 0.82 | |||||
| High school or some college | 9.7 | 24.8 | 31.2 | 25.2 | 9.1 | |
| College graduate/postgraduate | 6.3 | 24.9 | 36.8 | 25.3 | 6.8 | |
| Married | <0.01 | |||||
| Yes | 11.3 | 26.2 | 30.6 | 23.5 | 8.4 | |
| No | 7.5 | 24.2 | 34.0 | 25.9 | 8.3 | |
| Diabetes | 0.12 | |||||
| Yes | 11.8 | 24.9 | 28.1 | 24.4 | 10.7 | |
| No | 8.5 | 24.9 | 33.4 | 25.2 | 8.1 | |
| Hypertension | <0.01 | |||||
| Yes | 10.2 | 26.1 | 30.8 | 24.1 | 8.8 | |
| No | 8.0 | 24.4 | 34.0 | 25.6 | 8.1 | |
| Smoking | <0.01 | |||||
| Nonsmoker | 9.0 | 25.4 | 33.7 | 24.4 | 7.5 | |
| Former smoker | 7.9 | 24.3 | 33.2 | 26.0 | 8.6 | |
| Current smoker | 9.5 | 24.3 | 30.4 | 25.5 | 10.3 | |
| Body mass index, kg/m2 | 0.22 | |||||
| Non-obese (<25.0) | 7.4 | 24.6 | 35.4 | 25.2 | 7.4 | |
| Overweight (25.0-29.9) | 9.1 | 25.2 | 31.8 | 25.3 | 8.6 | |
| Obese (≥30.0) | 11.8 | 24.4 | 28.2 | 24.7 | 10.9 | |
| Physical activity, METs/weekc | <0.01 | |||||
| <15.4 (men), <10.0 (women) | 11.1 | 24.8 | 29.4 | 24.9 | 9.8 | |
| 15.4-33.3 (men), 10.0-20.7 (women) | 9.2 | 26.2 | 32.7 | 24.2 | 7.7 | |
| 33.4-63.9 (men), 20.8-45.9 (women) | 7.7 | 25.2 | 34.7 | 24.8 | 7.7 | |
| ≥64.0 (men), ≥46.0 (women) | 7.5 | 23.4 | 34.2 | 26.6 | 8.3 | |
| Sitting watching television, h/day | <0.01 | |||||
| < 1 | 10.2 | 25.0 | 32.4 | 24.8 | 7.6 | |
| 1-4 | 8.1 | 25.0 | 33.6 | 25.3 | 8.0 | |
| ≥5 | 11.7 | 23.8 | 26.9 | 24.6 | 12.9 | |
| Calorie intake, Kcal/day | <0.01 | |||||
| <2,184 (men), <1,747 (women) | 8.4 | 25.4 | 34.2 | 24.8 | 7.2 | |
| ≥2,184 (men), ≥1,747 (women) | 9.0 | 24.3 | 31.7 | 25.5 | 9.4 | |
| Alcohol intake, g/day | <0.01 | |||||
| <2.8 (men), zero (women) | 9.7 | 26.0 | 32.0 | 24.2 | 8.1 | |
| ≥2.8 (men), >0 (women) | 7.5 | 23.5 | 34.0 | 26.2 | 8.8 | |
Abbreviation: METs, metabolic equivalent of task.
Data are presented as row percentage unless otherwise indicated. Row percentage are adjusted for age through age standardization across 5 year age groups.
P Value for the difference of mean between subgroups adjusted for age based on analysis of variance.
METs for moderate activity, vigorous work and strenuous sports.
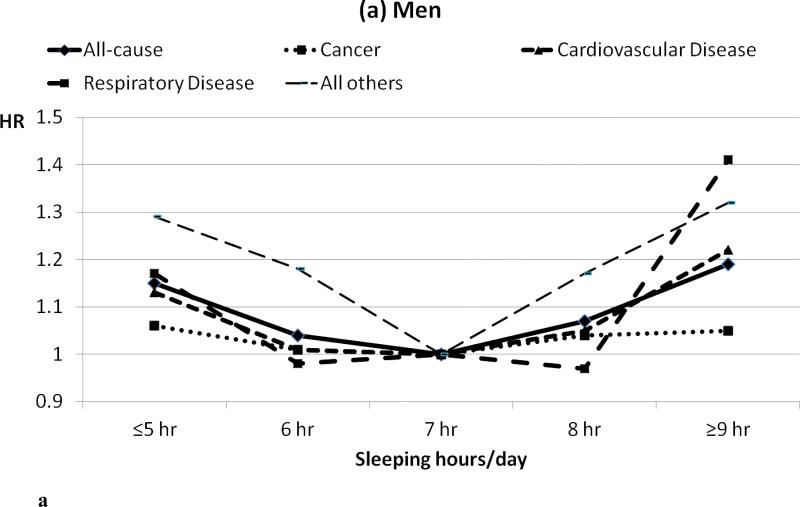
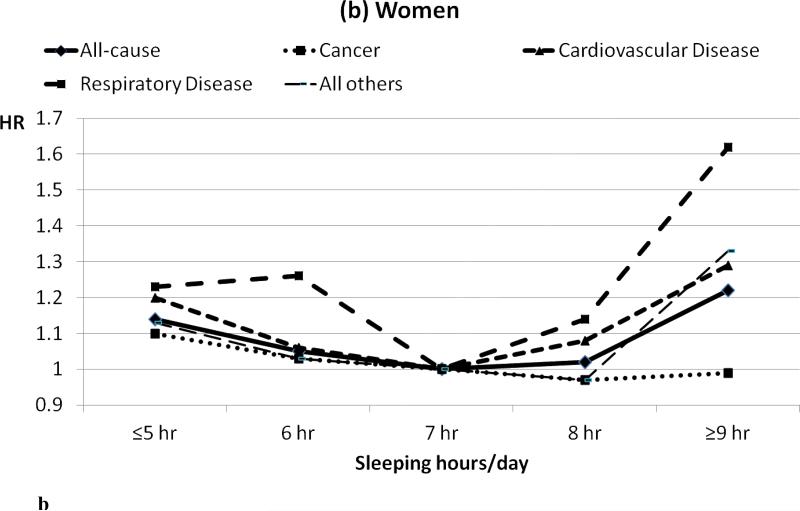
The association of sleep duration with all-cause mortality and cause-specific mortality including at least 100 deaths is presented in Tables 3 and 4. All-cause mortality showed a U-shaped association with sleep times in men (Table 3) and women (Table 4) (see also Figure 1). The four hazard ratios were simultaneously compared across the four major causes of mortality (malignant neoplasms, cardiovascular disease, respiratory disease and all others) and found to be significantly different in men (p =0.02) and women (p<0.01): sleep was not associated with mortality from malignant neoplasms, but sleep duration had a U-shaped association with mortality from CVD, respiratory disease and all other causes.
Table 3.
Hazard ratios for all-cause and cause specific mortality in relation to self-reported sleep duration among 61,936 men in the Multiethnic Cohort Study, 1993-2007a,b
| Outcomec | Deaths |
Daily sleeping |
|||||
|---|---|---|---|---|---|---|---|
| ≤5 hr |
6 hr |
7 hr |
8 hr |
≥9 hr |
|||
| No. | % | HR (95% CI) | HR (95% CI) | HR | HR (95% CI) | HR (95% CI) | |
| All Causes | 10,738 | - | 1.15 (1.06-1.23)* | 1.04 (0.99-1.10) | 1.00 | 1.07 (1.01-1.12)* | 1.19 (1.12-1.27)* |
| Malignant Neoplasms | 3,717 | 34.6 | 1.06 (0.94-1.21) | 1.01 (0.92-1.10) | 1.00 | 1.04 (0.96-1.13) | 1.05 (0.94-1.18) |
| Cardiovascular disease | 3,772 | 35.1 | 1.13 (1.00-1.28) | 1.01 (0.92-1.11) | 1.00 | 1.05 (0.96-1.14) | 1.22 (1.09-1.35)* |
| Coronary Heart Disease | 2,096 | 19.5 | 1.21 (1.04-1.42)* | 0.96 (0.85-1.08) | 1.00 | 1.00 (0.89-1.12) | 1.16 (1.00-1.34)* |
| Myocardial Infarction | 667 | 6.2 | 1.24 (0.94-1.64) | 0.92 (0.74-1.15) | 1.00 | 0.98 (0.80-1.20) | 1.16 (0.89-1.50) |
| Ischemic Heart Disease | 1,429 | 13.3 | 1.20 (0.99-1.45) | 0.98 (0.84-1.13) | 1.00 | 1.01 (0.88-1.16) | 1.16 (0.98-1.39) |
| Stroke | 627 | 5.8 | 1.02 (0.74-1.40) | 1.10 (0.88-1.37) | 1.00 | 1.13 (0.91-1.39) | 1.35 (1.03-1.75)* |
| Cardiomyopathy | 163 | 1.5 | 0.68 (0.32-1.47) | 1.46 (0.95-2.25) | 1.00 | 1.40 (0.91-2.14) | 1.62 (0.95-2.75) |
| Cardiac Arrest | 162 | 1.5 | 1.61 (0.93-2.78) | 0.98 (0.62-1.54) | 1.00 | 1.08 (0.71-1.65) | 1.48 (0.89-2.48) |
| Hypertensive Heart Disease | 137 | 1.3 | 0.75 (0.38-1.47) | 1.18 (0.76-1.84) | 1.00 | 1.01 (0.64-1.58) | 0.72 (0.37-1.41) |
| Hypertension | 129 | 1.2 | 1.14 (0.61-2.13) | 0.72 (0.42-1.23) | 1.00 | 1.16 (0.74-1.82) | 1.22 (0.68-2.18) |
| Congestive Heart Failure | 116 | 1.1 | 1.42 (0.74-2.70) | 0.80 (0.45-1.43) | 1.00 | 1.23 (0.76-2.02) | 1.43 (0.79-2.60) |
| Respiratory disease | 725 | 6.8 | 1.17 (0.89-1.55) | 0.98 (0.80-1.22) | 1.00 | 0.97 (0.79-1.18) | 1.41 (1.12-1.78)* |
| Pneumonia | 295 | 2.7 | 1.09 (0.70-1.71) | 0.98 (0.70-1.37) | 1.00 | 0.96 (0.71-1.31) | 1.36 (0.95-1.96) |
| All others | 2,524 | 23.5 | 1.29 (1.11-1.50)* | 1.18 (1.05-1.31)* | 1.00 | 1.17 (1.05-1.30)* | 1.32 (1.15-1.51)* |
| Infectious/Parasitic Disease | 210 | 2.0 | 1.26 (0.77-2.04) | 0.72 (0.47-1.09) | 1.00 | 1.29 (0.91-1.83) | 1.38 (0.87-2.19) |
| Diabetes | 355 | 3.3 | 0.89 (0.59-1.35) | 0.95 (0.71-1.28) | 1.00 | 1.03 (0.78-1.36) | 1.03 (0.72-1.48) |
| Mental/Behavioral Disease | 119 | 1.1 | 3.25 (1.65-6.38)* | 2.43 (1.37-4.29)* | 1.00 | 1.82 (1.03-3.22) | 2.91 (1.54-5.49)* |
| Alzheimer's Disease | 111 | 1.0 | 2.07 (1.00-4.29) | 1.67 (0.95-2.92) | 1.00 | 1.63 (0.96-2.78) | 1.64 (0.82-3.25) |
| Parkinson's Disease | 108 | 1.0 | 1.39 (0.60-3.18) | 2.14 (1.21-3.76)* | 1.00 | 1.87 (1.08-3.24)* | 1.82 (0.93-3.57) |
| Liver Disease | 202 | 1.9 | 1.19 (0.69-2.04) | 1.39 (0.95-2.02) | 1.00 | 1.07 (0.73-1.57) | 1.05 (0.64-1.74) |
| Kidney Disease | 140 | 1.3 | 1.81 (0.98-3.34) | 1.10 (0.64-1.90) | 1.00 | 1.81 (1.13-2.90)* | 1.99 (1.13-3.51)* |
| Accidents | 226 | 2.1 | 1.47 (0.94-2.32) | 0.97 (0.68-1.41) | 1.00 | 0.92 (0.64-1.31) | 1.18 (0.75-1.86) |
Abbreviation: CI, Confidence Intervals; HR, Hazard Ratio
HR (95% CI) which not includes 1.00.
Hazard ratios were calculated with age as the time metric, adjusted for 5-year age groups at cohort entry, sex, ethnicity, education, marital status, history of hypertension or diabetes at enrollment, alcohol consumption, energy intake, body mass index, physical activity (METs per week for moderate activity, vigorous work and strenuous sports), hours spent daily watching television, and smoking history by inclusion of the following variables: [smoking status, average number of cigarettes, average number of cigarettes squared, number of years smoked (time dependent), number of years since quitting (time dependent), and interactions between ethnicity and the smoking variables].
The test of heterogeneity across causes of death was performed using competing risk techniques, where each cause was a different event. A Wald test was used to compare the parameters between causes. P for heterogeneity (degrees of freedom = 12) across malignant neoplasms, cardiovascular disease, respiratory disease, and all others was 0.02. P for heterogeneity (degrees of freedom = 32) across specific cardiovascular disease was 0.53. P for heterogeneity (degrees of freedom = 60) across cause-specific disease within ‘All others’ was 0.42.
Hazard ratios are given only for conditions with 100 cases or more.
Table 4.
Hazard ratios for all-cause and cause specific mortality in relation to self-reported sleep duration among 73,749 women in the Multiethnic Cohort Study, 1993-2007a,b
| Outcomec | Deaths |
Daily sleeping |
|||||
|---|---|---|---|---|---|---|---|
| ≤5 hr |
6 hr |
7 hr |
8 hr |
≥9 hr |
|||
| No. | % | HR (95% CI) | HR (95% CI) | HR | HR (95% CI) | HR (95% CI) | |
| All Causes | 8,597 | - | 1.14 (1.06-1.23)* | 1.05 (0.99-1.12) | 1.00 | 1.02 (0.96-1.08) | 1.22 (1.13-1.31)* |
| Malignant Neoplasms | 3,055 | 35.5 | 1.10 (0.97-1.25) | 1.03 (0.94-1.14) | 1.00 | 0.97 (0.88-1.07) | 0.99 (0.87-1.14) |
| Cardiovascular disease | 2,838 | 33.0 | 1.20 (1.05-1.36)* | 1.06 (0.96-1.18) | 1.00 | 1.08 (0.98-1.20) | 1.29 (1.13-1.47)* |
| Coronary Heart Disease | 1,380 | 16.1 | 1.18 (0.98-1.42) | 1.13 (0.97-1.31) | 1.00 | 1.12 (0.96-1.29) | 1.23 (1.02-1.49)* |
| Myocardial Infarction | 521 | 6.1 | 1.18 (0.87-1.59) | 1.23 (0.96-1.56) | 1.00 | 1.10 (0.86-1.40) | 1.29 (0.94-1.75) |
| Ischemic Heart Disease | 859 | 10.0 | 1.18 (0.94-1.49) | 1.06 (0.88-1.29) | 1.00 | 1.13 (0.94-1.36) | 1.20 (0.95-1.53) |
| Stroke | 632 | 7.4 | 1.16 (0.88-1.52) | 0.99 (0.79-1.23) | 1.00 | 1.07 (0.87-1.33) | 1.39 (1.06-1.83)* |
| Cardiomyopathy | 89 | 1.0 | --- | --- | --- | --- | --- |
| Cardiac Arrest | 88 | 1.0 | --- | --- | --- | --- | --- |
| Hypertensive Heart Disease | 130 | 1.5 | 1.45 (0.81-2.58) | 1.34 (0.81-2.20) | 1.00 | 1.13 (0.67-1.89) | 1.72 (0.95-3.09) |
| Hypertension | 106 | 1.2 | 2.21 (1.09-4.46)* | 2.03 (1.11-3.72)* | 1.00 | 2.05 (1.13-3.71)* | 2.46 (1.22-4.97)* |
| Respiratory disease | 615 | 7.2 | 1.23 (0.92-1.65) | 1.26 (1.00-1.58) | 1.00 | 1.14 (0.91-1.43) | 1.62 (1.25-2.11)* |
| Pneumonia | 213 | 2.5 | 0.87 (0.49-1.52) | 1.45 (0.98-2.15) | 1.00 | 1.45 (0.98-2.13) | 2.08 (1.32-3.26)* |
| All others | 2,089 | 24.3 | 1.13 (0.97-1.31) | 1.03 (0.91-1.16) | 1.00 | 0.97 (0.86-1.10) | 1.33 (1.15-1.55)* |
| Infectious/Parasitic Disease | 144 | 1.7 | 1.59 (0.94-2.71) | 0.93 (0.58-1.51) | 1.00 | 1.04 (0.66-1.66) | 1.90 (1.11-3.26)* |
| Diabetes | 312 | 3.6 | 1.24 (0.84-1.84) | 1.22 (0.87-1.69) | 1.00 | 1.15 (0.83-1.59) | 1.57 (1.09-2.28)* |
| Mental/Behavioral Disease | 120 | 1.4 | 0.92 (0.46-1.83) | 1.33 (0.83-2.11) | 1.00 | 0.93 (0.56-1.54) | 0.90 (0.44-1.86) |
| Alzheimer's Disease | 155 | 1.8 | 0.93 (0.34-2.53) | 0.98 (0.48-2.02) | 1.00 | 1.36 (0.72-2.59) | 1.70 (0.73-3.97) |
| Parkinson's Disease | 64 | 0.7 | --- | --- | --- | --- | --- |
| Liver Disease | 122 | 1.4 | 1.55 (0.83-2.88) | 1.20 (0.71-2.04) | 1.00 | 1.29 (0.77-2.14) | 1.97 (1.09-3.54)* |
| Kidney Disease | 106 | 1.2 | 0.71 (0.34-1.45) | 0.73 (0.42-1.27) | 1.00 | 0.92 (0.55-1.53) | 1.36 (0.74-2.49) |
| Accidents | 155 | 1.8 | 0.74 (0.39-1.40) | 1.10 (0.73-1.66) | 1.00 | 0.86 (0.55-1.35) | 1.41 (0.82-2.44) |
Abbreviation: CI, Confidence Intervals; HR, Hazard Ratio.
HR (95% CI) which not includes 1.00
Hazard ratios were calculated with age as the time metric, adjusted for 5-year age groups at cohort entry, sex, ethnicity, education, marital status, history of hypertension or diabetes at enrollment, alcohol consumption, energy intake, body mass index, physical activity (METs per week for moderate activity, vigorous work and strenuous sports), hours spent daily watching television, and smoking history by inclusion of the following variables: [smoking status, average number of cigarettes, average number of cigarettes squared, number of years smoked (time dependent), number of years since quitting (time dependent), and interactions between ethnicity and the smoking variables].
The test of heterogeneity across causes of death was performed using competing risk techniques, where each cause was a different event. A Wald test was used to compare the parameters between causes. P for heterogeneity (degrees of freedom = 12) across malignant neoplasms, cardiovascular disease, respiratory disease, and all others was <0.01. P for heterogeneity (degrees of freedom = 32) across specific cardiovascular disease was 0.72. P for heterogeneity (degrees of freedom = 60) across cause-specific disease within ‘All others’ was 0.54.
Hazard ratios are given only for conditions with 100 cases or more.
Figure 1.
Hazard ratios of all-cause and cause specific mortality as a group among men (a) and women (b) in the Multiethnic Cohort Study, 1993-2007.
Multivariable HRs for CVD mortality were 1.13 for men and 1.20 for women sleeping ≤5 h/day; and 1.22 for men and 1.29 for women sleeping ≥ 9 h/day. This risk pattern for mortality was not heterogeneous across specific causes of death among men or among women within either the CVD category or the ‘all others’ category.
Stratification by various characteristics known to influence the risk of death had little influence on the U-shaped association between sleep duration and all-cause mortality (Table 5). A significant interaction was found between body mass index and sleep duration on all-cause mortality (Pint 0.03).
Table 5.
Hazard ratios for all-cause mortality in relation to self-reported sleep duration by several characteristics among 135,685 men and women in the Multiethnic Cohort Study, 1993-2007a
| Variable | No. Deaths | Daily sleeping |
P intb | ||||
|---|---|---|---|---|---|---|---|
| ≤5 hr |
6 hr |
7 hr |
8 hr |
≥9 hr |
|||
| HR (95% CI) | HR (95% CI) | HR | HR (95% CI) | HR (95% CI) | |||
| Ethnicity | 0.34 | ||||||
| White | 4,417 | 1.30 (1.14-1.48) | 1.07 (0.98-1.17) | 1.00 | 1.07 (0.99-1.16) | 1.26 (1.14-1.38) | |
| African American | 4,391 | 1.06 (0.96-1.17) | 1.01 (0.93-1.10) | 1.00 | 0.99 (0.91-1.08) | 1.17 (1.06-1.30) | |
| Native Hawaiian | 1,515 | 1.22 (1.04-1.44) | 0.96 (0.83-1.11) | 1.00 | 1.10 (0.95-1.28) | 1.26 (1.05-1.51) | |
| Japanese American | 5,110 | 1.11 (1.00-1.23) | 1.09 (1.01-1.17) | 1.00 | 1.09 (1.01-1.18) | 1.23 (1.10-1.37) | |
| Latino | 3,902 | 1.10 (0.98-1.24) | 1.01 (0.93-1.11) | 1.00 | 1.01 (0.92-1.09) | 1.12 (1.01-1.25) | |
| Age at enrollment | 0.89 | ||||||
| 45-64 | 8,145 | 1.17 (1.08-1.26) | 1.05 (0.99-1.12) | 1.00 | 1.02 (0.96-1.09) | 1.23 (1.14-1.33) | |
| 65-69 | 4,746 | 1.13 (1.02-1.26) | 1.07 (0.98-1.16) | 1.00 | 1.05 (0.97-1.13) | 1.25 (1.14-1.38) | |
| 70+ | 6,444 | 1.09 (0.99-1.19) | 1.02 (0.95-1.09) | 1.00 | 1.07 (1.00-1.14) | 1.14 (1.05-1.24) | |
| Education | 0.14 | ||||||
| High school or some college | 15,447 | 1.12 (1.06-1.19) | 1.05 (1.00-1.10) | 1.00 | 1.03 (0.99-1.08) | 1.19 (1.13-1.26) | |
| College graduate/postgraduate | 3,836 | 1.21 (1.06-1.37) | 1.03 (0.95-1.13) | 1.00 | 1.10 (1.01-1.20) | 1.23 (1.10-1.38) | |
| Diabetes | 0.31 | ||||||
| Yes | 3,858 | 1.09 (0.97-1.22) | 1.00 (0.91-1.10) | 1.00 | 1.06 (0.97-1.15) | 1.30 (1.17-1.44) | |
| No | 15,477 | 1.15 (1.09-1.22) | 1.06 (1.01-1.10) | 1.00 | 1.04 (1.00-1.09) | 1.17 (1.11-1.24) | |
| Hypertension | 0.99 | ||||||
| Yes | 9,483 | 1.17 (1.09-1.25) | 1.04 (0.99-1.11) | 1.00 | 1.05 (0.99-1.11) | 1.22 (1.14-1.31) | |
| No | 9,852 | 1.11 (1.03-1.20) | 1.05 (0.99-1.11) | 1.00 | 1.04 (0.99-1.1) | 1.19 (1.11-1.28) | |
| Smoking status | 0.48 | ||||||
| Nonsmokers | 6,556 | 1.14 (1.04-1.24) | 1.01 (0.95-1.08) | 1.00 | 1.03 (0.96-1.10) | 1.19 (1.09-1.30) | |
| Former smokers | 7,900 | 1.19 (1.10-1.30) | 1.09 (1.03-1.16) | 1.00 | 1.10 (1.03-1.17) | 1.23 (1.14-1.33) | |
| Current smokers | 4,879 | 1.07 (0.96-1.19) | 1.02 (0.95-1.11) | 1.00 | 0.99 (0.92-1.07) | 1.19 (1.08-1.31) | |
| Body mass index, kg/m2 | 0.03 | ||||||
| Non-obese (<25.0) | 9,057 | 1.13 (1.04-1.22) | 1.02 (0.96-1.08) | 1.00 | 1.05 (0.99-1.11) | 1.24 (1.15-1.33) | |
| Overweight (25.0-29.9) | 6,753 | 1.13 (1.03-1.23) | 1.05 (0.98-1.12) | 1.00 | 1.07 (1.00-1.14) | 1.25 (1.15-1.35) | |
| Obese (≥30.0) | 3,525 | 1.19 (1.06-1.33) | 1.12 (1.02-1.23) | 1.00 | 1.00 (0.91-1.10) | 1.08 (0.96-1.21) | |
| Physical activity, METs/weekb | 0.09 | ||||||
| <15.4 (men), <10.0 (women) | 6,162 | 1.17 (1.07-1.28) | 1.12 (1.04-1.21) | 1.00 | 1.13 (1.06-1.21) | 1.28 (1.18-1.40) | |
| 15.4-33.3 (men), 10.0-20.7 (women) | 4,199 | 1.15 (1.03-1.28) | 1.05 (0.96-1.14) | 1.00 | 0.98 (0.91-1.07) | 1.13 (1.01-1.26) | |
| 33.4-63.9 (men), 20.8-45.9 (women) | 5,259 | 1.06 (0.96-1.18) | 1.00 (0.93-1.08) | 1.00 | 1.01 (0.93-1.08) | 1.19 (1.08-1.31) | |
| ≥64.0 (men), ≥46.0 (women) | 3,715 | 1.22 (1.08-1.38) | 1.00 (0.91-1.09) | 1.00 | 1.05 (0.96-1.14) | 1.20 (1.07-1.34) | |
| Sitting watching television, h/day | 0.10 | ||||||
| < 1 | 2,073 | 1.17 (1.01-1.36) | 1.11 (0.98-1.26) | 1.00 | 1.13 (1.00-1.28) | 1.38 (1.18-1.62) | |
| 1-4 | 14,120 | 1.13 (1.06-1.20) | 1.06 (1.01-1.11) | 1.00 | 1.02 (0.98-1.07) | 1.19 (1.12-1.26) | |
| ≥5 | 2,766 | 1.20 (1.06-1.37) | 0.95 (0.85-1.07) | 1.00 | 1.09 (0.99-1.22) | 1.17 (1.04-1.32) | |
| Healthy populationc | 2,437 | 1.08 (0.93-1.25) | 1.09 (0.98-1.21) | 1.00 | 1.05 (0.94-1.17) | 1.32 (1.14-1.53) | - |
Abbreviation: CI, Confidence Intervals; HR, Hazard Ratio; METs, metabolic equivalent of task; Pint, P-value for interaction
Hazard ratios were calculated with age as the time metric, adjusted for variables not relevant to the stratified variables: 5-year age groups at cohort entry, sex, ethnicity, education, marital status, history of hypertension or diabetes at enrollment, alcohol consumption, energy intake, body mass index, physical activity (METs per week for moderate activity, vigorous work and strenuous sports), hours spent daily watching television, and smoking history by inclusion of the following variables: [smoking status, average number of cigarettes, average number of cigarettes squared, number of years smoked (time dependent), number of years since quitting (time dependent), and interactions between ethnicity and the smoking variables].
Calculated using the Wald statistic for cross-product terms.
Restricted to men and women who are nonsmokers, non-obese, and who don't have hypertension nor diabetes at baseline (n=68,243).
Stratification analyses had little effect on the association between sleep duration and CVD mortality (P's for interaction >0.05), with the exception of a significant interaction with education (Pint 0.02) (Table 6). Longer sleepers (8 or ≥9 hr/day) among more highly educated subjects had a greater risk of CVD mortality compared to the reference group (7 h/day). The U-shaped associations of CVD mortality with sleep duration were robust to exclusion of participants who were current smokers, obese, or had a history of hypertension or diabetes.
Table 6.
Hazard ratios for cardiovascular mortality in relation to self-reported sleep duration by several characteristics among 135,685 men and women in the Multiethnic Cohort Study, 1993-2007a
| Variable | No. Deaths | Daily sleeping |
P intb | ||||
|---|---|---|---|---|---|---|---|
| 7 hr |
6 hr |
7 hr |
8 hr |
≥9 hr |
|||
| HR (95% CI) | HR (95% CI) | HR | HR (95% CI) | HR (95% CI) | |||
| Ethnicity | 0.19 | ||||||
| White | 1,367 | 1.56 (1.25-1.95) | 1.10 (0.94-1.29) | 1.00 | 1.13 (0.99-1.30) | 1.28 (1.08-1.53) | |
| African American | 1,721 | 1.06 (0.91-1.25) | 1.02 (0.89-1.17) | 1.00 | 1.04 (0.91-1.19) | 1.30 (1.11-1.53) | |
| Native Hawaiian | 564 | 1.02 (0.78-1.34) | 0.87 (0.69-1.11) | 1.00 | 0.98 (0.77-1.24) | 1.17 (0.88-1.56) | |
| Japanese American | 1,608 | 1.10 (0.91-1.33) | 1.06 (0.93-1.21) | 1.00 | 1.16 (1.02-1.33) | 1.41 (1.17-1.70) | |
| Latino | 1,350 | 1.13 (0.94-1.37) | 0.99 (0.85-1.16) | 1.00 | 0.96 (0.84-1.11) | 1.01 (0.84-1.21) | |
| Age at enrollment | 0.64 | ||||||
| 45-64 | 2,507 | 1.12 (0.97-1.28) | 1.00 (0.90-1.11) | 1.00 | 0.99 (0.89-1.10) | 1.18 (1.03-1.36) | |
| 65-69 | 1,600 | 1.27 (1.06-1.52) | 1.15 (1.00-1.33) | 1.00 | 1.07 (0.93-1.22) | 1.43 (1.22-1.68) | |
| 70+ | 2,503 | 1.09 (0.94-1.26) | 0.98 (0.88-1.10) | 1.00 | 1.14 (1.03-1.27) | 1.20 (1.05-1.37) | |
| Education | 0.02 | ||||||
| High school or some college | 5,364 | 1.16 (1.05-1.27) | 1.03 (0.95-1.11) | 1.00 | 1.04 (0.96-1.12) | 1.22 (1.11-1.33) | |
| College graduate/postgraduate | 1,230 | 1.11 (0.88-1.39) | 1.04 (0.88-1.21) | 1.00 | 1.20 (1.04-1.39) | 1.34 (1.10-1.63) | |
| Diabetes | 0.25 | ||||||
| Yes | 1,618 | 0.98 (0.82-1.17) | 0.95 (0.82-1.09) | 1.00 | 0.97 (0.85-1.11) | 1.21 (1.03-1.42) | |
| No | 4,992 | 1.21 (1.10-1.34) | 1.06 (0.98-1.14) | 1.00 | 1.10 (1.02-1.19) | 1.24 (1.13-1.37) | |
| Hypertension | 0.73 | ||||||
| Yes | 3,826 | 1.11 (0.99-1.25) | 1.00 (0.92-1.10) | 1.00 | 1.07 (0.98-1.16) | 1.24 (1.12-1.39) | |
| No | 2,784 | 1.22 (1.07-1.40) | 1.08 (0.97-1.19) | 1.00 | 1.08 (0.97-1.19) | 1.26 (1.11-1.43) | |
| Smoking status | 0.65 | ||||||
| Nonsmokers | 2,359 | 1.17 (1.02-1.35) | 1.00 (0.89-1.12) | 1.00 | 1.07 (0.95-1.19) | 1.21 (1.04-1.40) | |
| Former smokers | 2,673 | 1.19 (1.03-1.37) | 1.06 (0.95-1.18) | 1.00 | 1.11 (1.00-1.23) | 1.29 (1.13-1.47) | |
| Current smokers | 1,578 | 1.08 (0.90-1.30) | 1.05 (0.91-1.20) | 1.00 | 1.00 (0.87-1.15) | 1.22 (1.04-1.44) | |
| Body mass index, kg/m2 | 0.10 | ||||||
| Non-obese (<25.0) | 2,861 | 1.12 (0.98-1.29) | 1.03 (0.93-1.14) | 1.00 | 1.03 (0.93-1.14) | 1.30 (1.15-1.48) | |
| Overweight (25.0-29.9) | 2,392 | 1.11 (0.95-1.29) | 1.00 (0.89-1.12) | 1.00 | 1.16 (1.04-1.29) | 1.28 (1.12-1.47) | |
| Obese (≥30.0) | 1,357 | 1.26 (1.05-1.50) | 1.08 (0.93-1.26) | 1.00 | 0.98 (0.84-1.14) | 1.11 (0.93-1.34) | |
| Physical activity, METs/weekb | 0.96 | ||||||
| <15.4 (men), <10.0 (women) | 2,227 | 1.13 (0.98-1.31) | 1.11 (0.99-1.26) | 1.00 | 1.13 (1.01-1.27) | 1.33 (1.15-1.53) | |
| 15.4-33.3 (men), 10.0-20.7 (women) | 1,494 | 1.24 (1.04-1.48) | 1.00 (0.87-1.15) | 1.00 | 0.96 (0.84-1.11) | 1.15 (0.96-1.37) | |
| 33.4-63.9 (men), 20.8-45.9 (women) | 1,738 | 1.09 (0.91-1.30) | 1.01 (0.88-1.15) | 1.00 | 1.01 (0.89-1.15) | 1.23 (1.05-1.45) | |
| ≥64.0 (men), ≥46.0 (women) | 1,151 | 1.21 (0.97-1.51) | 0.96 (0.81-1.14) | 1.00 | 1.18 (1.02-1.38) | 1.25 (1.02-1.53) | |
| Sitting watching television, h/day | 0.08 | ||||||
| < 1 | 701 | 1.08 (0.83-1.40) | 1.20 (0.97-1.48) | 1.00 | 1.10 (0.89-1.36) | 1.44 (1.10-1.87) | |
| 1-4 | 4,800 | 1.20 (1.08-1.33) | 1.04 (0.96-1.13) | 1.00 | 1.07 (0.99-1.15) | 1.26 (1.14-1.39) | |
| ≥5 | 977 | 1.08 (0.87-1.35) | 0.86 (0.72-1.04) | 1.00 | 1.02 (0.86-1.22) | 1.11 (0.91-1.36) | |
| Healthy populationc | 673 | 1.30 (0.99-1.70) | 1.13 (0.92-1.39) | 1.00 | 1.05 (0.85-1.29) | 1.35 (1.02-1.79) | - |
Abbreviation: CI, Confidence Intervals; HR, Hazard Ratio; METs, metabolic equivalent of task; Pint, P-value for interaction
Hazard ratios were calculated with age as the time metric, adjusted for variables not relevant to the stratified variables: 5-year age groups at cohort entry, sex, ethnicity, education, marital status, history of hypertension or diabetes at enrollment, alcohol consumption, energy intake, body mass index, physical activity (METs per week for moderate activity, vigorous work and strenuous sports), hours spent daily watching television, and smoking history by inclusion of the following variables: [smoking status, average number of cigarettes, average number of cigarettes squared, number of years smoked (time dependent), number of years since quitting (time dependent), and interactions between ethnicity and the smoking variables].
Calculated using the Wald statistic for cross-product terms.
Restricted to men and women who are nonsmokers, non-obese, and who don't have hypertension nor diabetes at baseline (n=68,243).
Restricting the sample to participants with at least 10 yrs of follow-up attenuated the HRs for mortality in the shortest sleeping group, but in general the patterns of risk were consistent with results that included participants with less follow-up time (Table 7).
Table 7.
Hazard ratios for all-cause and cause specific mortality as a group in relation to self-reported sleep duration among 123,628 men and women who were followed ≥10 years in the Multiethnic Cohort Study, 1993-2007a,b
| Outcome | Deaths |
Daily sleeping |
|||||
|---|---|---|---|---|---|---|---|
| ≤5 hr |
6 hr |
7 hr |
8 hr |
≥9 hr |
|||
| No. | % | HR (95% CI) | HR (95% CI) | HR | HR (95% CI) | HR (95% CI) | |
| All Causes | 7.517 | - | 1.08 (0.99-1.18) | 1.07 (1.01-1.14) | 1.00 | 1.00 (0.94-1.06) | 1.18 (1.09-1.28) |
| Malignant Neoplasms | 2.380 | 31.7 | 1.07 (0.92-1.24) | 1.09 (0.98-1.21) | 1.00 | 0.95 (0.85-1.05) | 1.08 (0.93-1.25) |
| Cardiovascular disease | 2,604 | 34.6 | 1.09 (0.95-1.26) | 1.05 (0.94-1.17) | 1.00 | 1.04 (0.93-1.15) | 1.23 (1.07-1.40) |
| Respiratory disease | 552 | 7.3 | 1.03 (0.75-1.42) | 1.07 (0.85-1.35) | 1.00 | 0.94 (0.75-1.18) | 1.11 (0.83-1.48) |
| All others | 1,981 | 26.4 | 1.09 (0.93-1.28) | 1.11 (0.98-1.25) | 1.00 | 1.04 (0.93-1.17) | 1.26 (1.09-1.47) |
Abbreviation: CI, Confidence Intervals; HR, Hazard Ratio.
Hazard ratios were calculated with age as the time metric, adjusted for 5-year age groups at cohort entry, sex, ethnicity, education, marital status, history of hypertension or diabetes at enrollment, alcohol consumption, energy intake, body mass index, physical activity (METs per week for moderate activity, vigorous work and strenuous sports), hours spent daily watching television, and smoking history by inclusion of the following variables: [smoking status, average number of cigarettes, average number of cigarettes squared, number of years smoked (time dependent), number of years since quitting (time dependent), and interactions between ethnicity and the smoking variables].
The test of heterogeneity across causes of death was performed using competing risk techniques, where each cause was a different event. A Wald test was used to compare the parameters between causes. P for heterogeneity (degrees of freedom = 12) across malignant neoplasms, cardiovascular disease, respiratory disease, and all others was 0.72.
Discussion
In this study, men and women in the extremes of sleep duration faced higher risk of death, particularly from CVD. Moreover, the consistency of the U-shaped association of all cause and CVD mortality with sleep duration in analyses by subgroups of demographic and lifestyle factors, adds to the public health significance of our observations. A unique aspect of the current analysis was the consistency of the major findings among diverse ethnic groups.
Recent meta-analyses of results from prospective studies found that the risk of all-cause mortality was increased by 10-12% in short sleepers and 23-30% in long sleepers (Cappuccio et al., 2010; Gallicchio and Kalesan, 2009). Our result for all-cause mortality is consistent with the results from large cohort studies (Kripke et al., 2002; Patel et al., 2004; Tamakoshi and Ohno, 2004), namely a U-shaped relation of all-cause mortality with sleep duration.
We observed a U-shaped association of CVD mortality with sleep duration, in contrast to inconsistent results from previous studies (Burazeri et al., 2003; Heslop et al., 2002; Ikehara et al., 2009; Lan et al., 2007; Mallon et al., 2002; Patel et al., 2004; Shankar et al., 2008; Stone et al., 2009; Suzuki et al., 2009). While some investigators report null associations (Heslop et al., 2002; Mallon et al., 2002), others report significant positive associations of CVD mortality specific to longer sleepers (Burazeri et al., 2003; Ikehara et al., 2009; Lan et al., 2007; Patel et al., 2004; Stone et al., 2009; Suzuki et al., 2009). Meta-analyses found that the risk of all CVD mortality was increased by 23-41% in longer sleepers, but no association was observed in shorter sleepers (Cappuccio et al., 2011; Gallicchio and Kalesan, 2009). However, consistent with our result, men and women who decreased their sleep hours had a 2-fold higher risk of CVD mortality compared to men and women who had no change in their sleeping time in the Whitehall II Cohort (Ferrie et al., 2007).
The relatively large size of the Multiethnic Cohort allowed us to examine the relation of sleep duration to specific CVD outcomes. In accord with our findings, Japanese investigators reported significantly increased mortality from stroke among longer sleeping (≥10 h/day vs. 7 h/day) men (66% increased risk) and women (69% increased risk) (Ikehara et al., 2009). While risk of CHD death among shorter sleeping (≤4 h/day) women was increased 2.32-fold compared to average sleepers, CHD death was not associated with sleeping duration among men (Ikehara et al., 2009). However, the number of deaths from CHD in the extreme sleeping group was small (Ikehara et al., 2009). Another study of specific CVD outcomes showed non-significant relations to sleep, but this investigation had a small number of deaths (63 deaths from stroke, and 54 deaths from heart diseases) (Amagai et al., 2004). Finally, increased risks of CHD mortality in shorter and longer sleepers (≤5 h/day and ≥10 h/day vs. 7 h/day) were observed in a cohort of Singapore Chinese (Shankar et al., 2008).
We observed an increased risk of death from hypertension in extreme sleepers among women, but not men, although heterogeneity in risk across cardiovascular outcomes was not statistically significant in either sex. This result is consistent with findings from a large cross-sectional study showing increased hypertension among shorter sleeping (<6 h/day) women only (Stranges et al., 2008); as well as the Whitehall II study which reported that shorter sleeping women (≤5 h/day vs. 7 h/day), but not men, had a 19% increased risk of incident hypertension (Cappuccio et al., 2007). Mechanisms are not fully understood, but sex-specific differences in the activity of the angiotensin and renin-angiotensin systems might contribute to poorer control of hypertension in women than in men (Guarner-Lans et al., 2011; Ramírez-Expósito and Martínez-Martos, 2008; Yanes and Reckelhoff, 2011).
This is the first prospective study, to our knowledge, which examined the association of sleep duration with various specific non-CVD causes of death. Although false-positive results are a concern, longer sleeping women, but not men, had an increased risk of death from diabetes; whereas, shorter and longer sleeping men, but not women, had an increased risk of death from mental/behavioral disease and kidney disease. Differences between sexes in insulin resistance (Yanes et al., 2005) or the hypothalamic-pituitary-adrenocortical axis (Pesonen et al., 2012) may provide a partial explanation for our sex-specific findings for death from diabetes and from kidney disease. It is likely that unadjusted confounders such as sleep disturbances, insomnia or mood disorders, might have inflated the association for deaths due to mental/behavioral disease among men (Dew et al., 2003; Pollak et al., 1990; Rod et al., 2011).
In accordance with other studies (Basner et al., 2007; Chaput et al., 2008; Krueger and Friedman, 2009; López-García et al., 2008; Lauderdale et al., 2006; Magee et al., 2009; Nishiura and Hashimoto, 2010; Stamatakis et al., 2007; Stranges et al., 2008), we observed multiple demographic, lifestyle and co-morbid conditions that were associated with sleep duration. Older people, who are at greater risk of death, tend to sleep longer than younger people (Ferrie et al., 2007; Gangwisch et al., 2008), although it is unclear if this association is causal (Patel et al., 2012). Consistent with our results, African Americans had greater variability in sleep duration than other ethnic groups, and Hispanics had a greater tendency to sleep ≥9 hr/day (Hale and Do, 2007). Shorter (Hasler et al., 2004; Kohatsu et al., 2006; Nishiura and Hashimoto, 2010) and longer duration of sleep (Chaput et al., 2008; Hairston et al., 2010; López-García et al., 2008) have been associated with greater body mass, as well as with greater accumulation of abdominal fat (Hairston et al., 2010). A more pronounced impact of short sleep on all-cause mortality in obese compared to non-obese participants is worrisome, but may have resulted from residual confounding resulting from the strong correlation of energy intake, sitting hours, and physical activity with both sleep time and obesity (Horne, 2008; Marshall et al., 2008). Shorter sleepers and longer sleepers engage in less physical activity (Tu et al., 2012) and watch more television than average sleepers (Basner et al., 2007). It is reassuring that the increased risk of all-cause and CVD mortality among shorter and longer sleepers was generally consistent across various subgroups in our study.
Strengths of the study include the large number of subjects from a multiethnic population with long-term follow-up and multiple cause-specific outcomes. Accordingly, we were able to restrict the analyses of sleep duration and mortality to a healthy population and to a long-term followed population. One potential limitation of our study design was the absence of information concerning sleep quality, such as insomnia and sleep disturbance, or medical conditions/diseases that could affect sleep duration which might also influence risk of death. Because sleep was measured by self-administered questionnaire and not by objective tools, we cannot rule out the possibility that sleep duration may have been misclassified. Sleep duration was over-reported in a study comparing self-reported sleep to actinographic measurement (Lauderdale et al., 2008), implying that the association of higher mortality in the shortest sleeping group may be an underestimate of the true risk of death.
Conclusion
Men and women who have insufficient or excessive amounts of sleep are at increased risk of premature mortality from cardiovascular and other chronic diseases in a representative multiethnic populations.
Highlights.
Shorter and longer sleep increased the risk of all-cause and CVD mortality.
Risk pattern for CVD mortality was not heterogeneous across specific causes.
The association for all-cause and CVD mortality was consistent across subgroups.
Sleep duration was not associated with cancer mortality.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
References
- Amagai Y, Ishikawa S, Gotoh T, Doi Y, Kayaba K, Nakamura Y, Kajii E. Sleep duration and mortality in Japan: the Jichi Medical School Cohort Study. J Epidemiol. 2004;14:124–8. doi: 10.2188/jea.14.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basner M, Fomberstein KM, Razavi FM, Banks S, William JH, Rosa RR, Dinges DF. American time use survey: sleep time and its relationship to waking activities. Sleep. 2007;30:1085–95. doi: 10.1093/sleep/30.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burazeri G, Gofin J, Kark JD. Over 8 hours of sleep--marker of increased mortality in Mediterranean population: follow-up population study. Croat Med J. 2003;44:193–8. [PubMed] [Google Scholar]
- Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32:1484–92. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappuccio FP, Stranges S, Kandala NB, Miller MA, Taggart FM, Kumari M, Ferrie JE, Shipley MJ, Brunner EJ, et al. Gender-specific associations of short sleep duration with prevalent and incident hypertension: the Whitehall II Study. Hypertension. 2007;50:693–700. doi: 10.1161/HYPERTENSIONAHA.107.095471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput JP, Despres JP, Bouchard C, Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008;31:517–23. doi: 10.1093/sleep/31.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien KL, Chen PC, Hsu HC, Su TC, Sung FC, Chen MF, Lee YT. Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: report from a community-based cohort. Sleep. 2010;33:177–84. doi: 10.1093/sleep/33.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curb JD, Ford CE, Pressel S, Palmier M, Babcock C, Hawkins M. Ascertainment of vital status through the national death index and the social security administration. Am J Epidemiol. 1985;121:754–66. doi: 10.1093/aje/121.5.754. [DOI] [PubMed] [Google Scholar]
- Dew MA, Hoch CC, Buysse DJ, Monk TH, Begley AE, Houck PR, Hall M, Kupfer DJ, Reynolds CF. Healthy Older Adults’ Sleep Predicts All-Cause Mortality at 4 to 19 Years of Follow-Up. Psychosomatic Medicine. 2003;65:63–73. doi: 10.1097/01.psy.0000039756.23250.7c. [DOI] [PubMed] [Google Scholar]
- Ferrie JE, Shipley MJ, Cappuccio FP, Brunner E, Miller MA, Kumari M, Marmot MG. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30:1659–66. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta- analysis. J Sleep Res. 2009;18:148–58. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Opler MG, Pickering TG, Rundle AG, Zammit GK, et al. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep. 2008;31:1087–96. [PMC free article] [PubMed] [Google Scholar]
- Guarner-Lans V, Rubio-Ruiz ME, Pérez-Torres I, Baños de MacCarthy G. Relation of aging and sex hormones to metabolic syndrome and cardiovascular disease. Experimental Gerontology. 2011;46:517–23. doi: 10.1016/j.exger.2011.02.007. [DOI] [PubMed] [Google Scholar]
- Haiman CA, Stram DO, Wilkens LR, Pike MC, Kolonel LN, Henderson BE, Le Marchand L. Ethnic and Racial Differences in the Smoking-Related Risk of Lung Cancer. N Engl J Med. 2006;354:333–42. doi: 10.1056/NEJMoa033250. [DOI] [PubMed] [Google Scholar]
- Hairston KG, Bryer-Ash M, Norris JM, Haffner S, Bowden DW, Wagenknecht LE. Sleep duration and five-year abdominal fat accumulation in a minority cohort: the IRAS family study. Sleep. 2010;33:289–95. doi: 10.1093/sleep/33.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond EC. Some preliminary findings on physical complaints from a prospective study of 1,064,004 men and women. Am J Public Health Nations Health. 1964;54:11–23. doi: 10.2105/ajph.54.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler G, Buysse DJ, Klaghofer R, Gamma A, Ajdacic V, Eich D, Rossler W, Angst J. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27:661–6. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C. Sleep duration and mortality: the effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Medicine. 2002;3:305–14. doi: 10.1016/s1389-9457(02)00016-3. [DOI] [PubMed] [Google Scholar]
- Horne J. Short sleep is a questionable risk factor for obesity and related disorders: statistical versus clinical significance. Biol Psychol. 2008;77:266–76. doi: 10.1016/j.biopsycho.2007.12.003. [DOI] [PubMed] [Google Scholar]
- Hublin C, Partinen M, Koskenvuo M, Kaprio J. Sleep and mortality: a population-based 22-year follow-up study. Sleep. 2007;30:1245–53. doi: 10.1093/sleep/30.10.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, Inaba Y, Tamakoshi A. Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep. 2009;32:295–301. doi: 10.1093/sleep/32.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, amino acids. National Academics Press; Washington D.C.: 2005. [Google Scholar]
- Kohatsu N, Tsai R, Young T, Vangilder R, Burmeister L, Stromquist A. SLeep duration and body mass index in a rural population. Arch Intern Med. 2006;166:1701–05. doi: 10.1001/archinte.166.16.1701. [DOI] [PubMed] [Google Scholar]
- Kolonel LN, Henderson BE, Hankin JH, Nomura AMY, Wilkens LR, Pike MC, Stram DO, Monroe KR, Earle ME, et al. A Multiethnic Cohort in Hawaii and Los Angeles: Baseline Characteristics. Am J Epidemiol. 2000;151:346–57. doi: 10.1093/oxfordjournals.aje.a010213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality Associated With Sleep Duration and Insomnia. Arch Gen Psychiatry. 2002;59:131–36. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- Kripke DF, Simons RN, Garfinkel L, Hammond EC. Short and Long Sleep and Sleeping Pills: Is Increased Mortality Associated? Arch Gen Psychiatry. 1979;36:103–16. doi: 10.1001/archpsyc.1979.01780010109014. [DOI] [PubMed] [Google Scholar]
- Krueger PM, Friedman EM. Sleep Duration in the United States: A Cross-sectional Population-based Study. Am J Epidemiol. 2009;169:1052–63. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-García E, Faubel R, León-Muñoz L, Zuluaga MC, Banegas JR, Rodríguez-Artalejo F. Sleep duration, general and abdominal obesity, and weight change among the older adult population of Spain. Am J Clin Nutr. 2008;87:310–16. doi: 10.1093/ajcn/87.2.310. [DOI] [PubMed] [Google Scholar]
- Lan TY, Lan TH, Wen CP, Lin YH, Chuang YL. Nighttime sleep, Chinese afternoon nap, and mortality in the elderly. Sleep. 2007;30:1105–10. doi: 10.1093/sleep/30.9.1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hulley SB, Sidney S, Liu K. Objectively Measured Sleep Characteristics among Early-Middle-Aged Adults. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- Magee CA, Iverson DC, Caputi P. Factors associated with short and long sleep. Prev Med. 2009;49:461–7. doi: 10.1016/j.ypmed.2009.10.006. [DOI] [PubMed] [Google Scholar]
- Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Int Med. 2002;251:207–16. doi: 10.1046/j.1365-2796.2002.00941.x. [DOI] [PubMed] [Google Scholar]
- Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12:289–98. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Mesas AE, Lopez-Garcia E, Leon-Munoz LM, Guallar-Castillon P, Rodriguez-Artalejo F. Sleep duration and mortality according to health status in older adults. J Am Geriatr Soc. 2010;58:1870–7. doi: 10.1111/j.1532-5415.2010.03071.x. [DOI] [PubMed] [Google Scholar]
- Nishiura C, Hashimoto H. A 4-year study of the association between short sleep duration and change in body mass index in Japanese male workers. J Epidemiol. 2010;20:385–90. doi: 10.2188/jea.JE20100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, Stampfer MJ, Hu FB. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–4. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- Patel SR, Blackwell T, Ancoli-Israel S, Stone KL. Sleep characteristics of self- reported long sleepers. Sleep. 2012;35:641–8. doi: 10.5665/sleep.1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesonen AK, Kajantie E, Heinonen K, Pyhala R, Lahti J, Jones A, Matthews KA, Eriksson JG, Strandberg T, et al. Sex-specific associations between sleep problems and hypothalamic-pituitary-adrenocortical axis activity in children. Psychoneuroendocrinology. 2012;37:238–48. doi: 10.1016/j.psyneuen.2011.06.008. [DOI] [PubMed] [Google Scholar]
- Pollak CP, Perlick D, Linsner JP, Wenston J, Hsieh F. Sleep problems in the community elderly as predictors of death and nursing home placement. J Community Health. 1990;15:123–35. doi: 10.1007/BF01321316. [DOI] [PubMed] [Google Scholar]
- Ramírez-Expósito M, Martínez-Martos J. Hypertension, RAS, and gender: what is the role of aminopeptidases? Heart Failure Reviews. 2008;13:355–65. doi: 10.1007/s10741-008-9082-1. [DOI] [PubMed] [Google Scholar]
- Rod NH, Vahtera J, Westerlund H, Kivimaki M, Zins M, Goldberg M, Lange T. Sleep disturbances and cause-specific mortality: Results from the GAZEL cohort study. Am J Epidemiol. 2011;173:300–9. doi: 10.1093/aje/kwq371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankar A, Koh WP, Yuan JM, Lee HP, Yu MC. Sleep duration and coronary heart disease mortality among Chinese adults in Singapore: a population-based cohort study. Am J Epidemiol. 2008;168:1367–73. doi: 10.1093/aje/kwn281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamatakis KA, Kaplan GA, Roberts RE. Short Sleep Duration Across Income, Education, and Race/Ethnic Groups: Population Prevalence and Growing Disparities During 34 Years of Follow-Up. Ann Epidemiol. 2007;17:948–55. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone KL, Ewing SK, Ancoli-Israel S, Ensrud KE, Redline S, Bauer DC, Cauley JA, Hillier TA, Cummings SR. Self-reported sleep and nap habits and risk of mortality in a large cohort of older women. J Am Geriatr Soc. 2009;57:604–11. doi: 10.1111/j.1532-5415.2008.02171.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stranges S, Dorn JM, Shipley MJ, Kandala N-B, Trevisan M, Miller MA, Donahue RP, Hovey KM, Ferrie JE, et al. Correlates of Short and Long Sleep Duration: A Cross-Cultural Comparison Between the United Kingdom and the United States. Am J Epidemiol. 2008;168:1353–64. doi: 10.1093/aje/kwn337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki E, Yorifuji T, Ueshima K, Takao S, Sugiyama M, Ohta T, Ishikawa-Takata K, Doi H. Sleep duration, sleep quality and cardiovascular disease mortality among the elderly: a population-based cohort study. Prev Med. 2009;49:135–41. doi: 10.1016/j.ypmed.2009.06.016. [DOI] [PubMed] [Google Scholar]
- Tamakoshi A, Ohno Y. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;27:51–4. [PubMed] [Google Scholar]
- Therneau T, Grambsch P. Modeling Survival Data: Extending the Cox Model. Springer-Verlag; New York: 2000. [Google Scholar]
- Tu X, Cai H, Gao YT, Wu X, Ji BT, Yang G, Li H, Zheng W, Shu XO. Sleep duration and its correlates in middle-aged and elderly Chinese women: the Shanghai Women's Health Study. Sleep Med. 2012;13:1138–45. doi: 10.1016/j.sleep.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingard DL, Berkman L. Mortality risk associated with sleeping patterns among adults. Sleep. 1983;6:102–7. doi: 10.1093/sleep/6.2.102. [DOI] [PubMed] [Google Scholar]
- Yanes LL, Reckelhoff JF. Postmenopausal Hypertension. Am J Hypertens. 2011;24:740–49. doi: 10.1038/ajh.2011.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanes LL, Romero DG, Cucchiarelli VE, Fortepiani LA, Gomez-Sanchez CE, Santacruz F, Reckelhoff JF. Role of endothelin in mediating postmenopausal hypertension in a rat model. Am J Physiol Regul Integr Comp Physiol. 2005;288:R229–33. doi: 10.1152/ajpregu.00697.2003. [DOI] [PubMed] [Google Scholar]