Abstract
Background
Older adults without dementia living in residential care facilities with toileting disability have increased care costs and dependency. Understanding associated factors could guide prevention and management strategies.
Objective
To identify the prevalence of and factors associated with toileting disability in this population.
Methods
This was a cross-sectional analysis of the 2010 National Survey of Residential Care Facilities. A subsample (N = 2,395) of adults aged 65 years or older, without dementia, and with the potential to implement behavioral interventions was examined. Associated factors were classified according to the disablement process as pathologies, impairments, functional limitations, coexisting disabilities, intra- and extra-individual factors. Logistic regression models accounting for the stratified two-stage probability sampling design were used to identify factors associated with toileting disability.
Results
Residents were mostly White women, aged 85 years and older. Prevalence of toileting disability was 15%. Associated factors included: reporting fair or poor health, living in a facility with four or less residents, living in a for-profit facility; having bowel incontinence, urinary incontinence, an increased number of physical impairments, visual and hearing impairments; and needing assistance with bathing, dressing, and transferring.
Discussion
Multicomponent and multidisciplinary prevention and management efforts should be designed for residents without dementia. Future studies testing the efficacy of prevention efforts are needed and should include treatments for incontinence, physical activity programs targeting impairments with walking, standing, sitting, stooping, reaching, and grasping, and therapy to improve dressing, bathing, and transferring skills.
Keywords: aged, assisted living facilities, toileting disability
Toileting disability is an understudied and poorly described disability in the older population. It is commonly defined as having difficulty with or requiring human or mechanical assistance with toileting. Its presence prompts increasing levels of care, which raises financial costs, as well as, personal costs through the loss of independence. Frail older adults without dementia are increasingly living in residential care facilities (i.e., assisted living) with the goal of maintaining current levels of independence. Preventing the development of toileting disability in this group of residents may help them maintain their current living arrangements and levels of independence.
Little is known about the epidemiology of toileting disability in this population. Most studies investigate disabilities with activities of daily living as a summation of difficulties with dressing, bathing, transferring, toileting, and eating, so information specific to toileting disability is scarce. A recent review indicated that very few nationally representative studies identify the prevalence of toileting disability in older adults across different residential settings (Kane, Talley, Shamliyan, & Pacala, 2011). The scant literature indicates that in the general population of community dwelling adults age 65 years and older, the prevalence of toileting disability is 6% (Lee, Lindquist, Segal, & Covinsky, 2006). This prevalence increases to 45% among frail community-dwelling older adults (Carey et al., 2008). More than 60% of older nursing home residents (Jones, Sonnenfeld, & Harris-Kojetin, 2009) and 35% of residential care facility residents have toileting disability (Caffrey, Sengupta, & Park-Lee, 2012). For frail community-dwelling older adults eligible for nursing home placement having toileting disability was associated with mortality (Carey et al., 2008).
Information on factors associated with toileting disability is even scarcer. Older adults are more likely to have disabilities with activities of daily living when they have urinary incontinence, advanced age, multiple comorbid conditions, poor self-rated health status, depression, physical impairments, and functional limitations (Holroyd-Leduc, Mehta, & Covinsky, 2004; Johnson, Bernard, Kincade, & Defriese, 2000; Nuotio, Tammela, Luukkaala, & Jylha, 2002). Pathologies, such as bowel incontinence, depression, stroke, and heart failure, may also contribute to toileting disability (DuBeau et al., 2010, Hunskaar et al., 2000), as well as environmental factors, such as type of residence and bathroom accessibility (Wyman, Elswick, Ory, Wilson, & Fantl, 1993).
Understandingfactors associated with toileting disability is necessary to develop and test prevention and management programs that accommodate resident characteristics and abilities. Currently, 58% of older adults living in residential care facilities do not have a diagnosis of Alzheimer's disease or dementia (Caffrey et al., 2012). This subgroup of residents without dementia may benefit from programs that have a different structure than programs designed for residents with dementia; thus, it is important to understand their unique risk profile. The International Continence Society's guidelines for treating urinary incontinence in frail older adults emphasize the importance of maximizing toileting ability, by combining conservative (nondrug, nonsurgical) treatments for bladder leakage with activities that improve physical function (Abrams et al., 2010). Therefore, potential components of prevention and management programs could include physical activity to maintain or improve toileting skills and conservative treatments (i.e., pelvic floor muscle exercises, bladder training, and urge suppression techniques) for bladder leakage. A necessary first step toward developing and testing these types of programs is to understand the prevalence of and factors associated with toileting disability among this subgroup of residents. Therefore, the purpose of this descriptive study was to identify the prevalence of toileting disability and associated factors in older adults without dementia living in residential care facilities who have the potential to implement conservative treatments for bladder leakage and to improve their physical function.
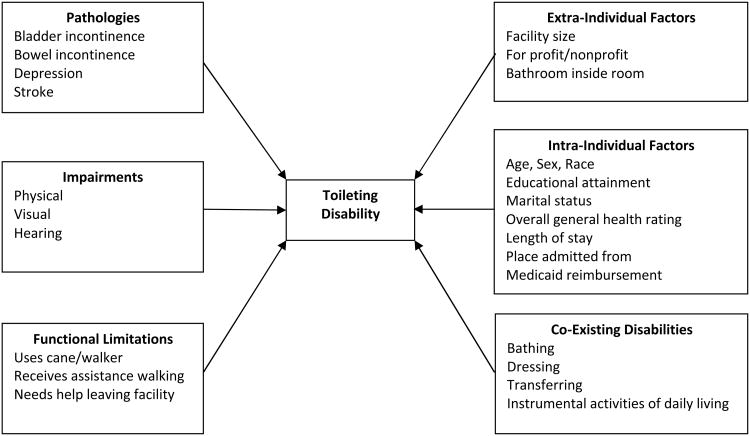
The disablement process model provides a framework for identifying factors associated with disability (Verbrugge & Jette, 1994). This model identifies a nonlinear pathway to disability involving pathologies, impairments, and functional limitations. The disability pathway is also influenced by intra-individual and extra-individual factors. Coexisting disabilities can also occur. In this model, disability is conceptually defined as difficulty doing activities of daily living. Pathologies are defined as diagnoses of disease, injury, and congenital/developmental conditions. Impairments are dysfunctions and structural abnormalities in specific body systems(e.g., musculoskeletal, cardiovascular). Functional limitations are restrictions in basic physical and mental actions, such as ambulation. Intra-individual factors include predisposing characteristics, such as demographic, social, lifestyle, behavioral and psychological traits that may exacerbate or deter disability. Extra-individual factors are protective or exacerbating conditions occurring in the individual's physical or social environment (Verbrugge & Jette, 1994).
The primary hypothesis for this study was that toileting disability is present when urinary and fecal incontinence (pathologies) occur with physical impairments, ambulation (functional limitations), transferring, bathing, and dressing (coexisting disabilities) difficulties. Extra-individual environmental factors, such as the type and size of the residential care facility and bathroom accessibility, may also contribute to toileting disability. Intra-individual factors associated with disability, such as age, perceived health status, admission status and certain pathologies (e.g., depression, stroke), were controlled for as confounders. The conceptual model is displayed in Figure 1.
Figure 1. Conceptual model of the disablement process for toileting disability.
Ultimately, this knowledge can be used to design and test prevention and management programs targeting an expanding and understudied subpopulation of older adults living in residential care facilities. The number of people living in residential care facilities is approaching the number of people who live in nursing homes. In 2010, 733,330 people lived in residential care facilities (Park-Lee, Caffrey, & Sengupta, 2011) and about 1,500,000 lived in nursing homes (Jones, Dwyer, Bercovitz, & Strahan, 2009). The average cost of living in a residential care facility is $3,165 per month (Caffrey et al., 2012), whereas the average monthly cost of living in a nursing home is $7,513 (Prudential Research Report, 2010). Preventing or delaying the onset of toileting disability may help prevent costly nursing home relocations.
Methods
Design
A secondary analysis of the 2010 National Survey of Residential Care Facility Survey (NSRCFS) public use files was conducted. The NSRCFS is a cross-sectional survey that includes 8,094 residents living in 2,302 residential care facilities that were licensed, registered, listed, certified, or otherwise regulated by the state; had four or more licensed, certified, or registered beds; had at least one resident currently living in the facility; and provided room and board with at least two meals a day; around-the-clock onsite supervision; and help with personal care, such as bathing and dressing, or health-related services such as medication management. Facilities serving mentally ill or developmentally disabled populations exclusively were excluded, as were nursing homes, unless there was a unit meeting the above definition and residents could be counted separately. The University of Minnesota Institutional Review Board deemed this research using public access datasets to be exempt from oversight.
The 2010 NSRCFS used a stratified two-stage probability sample design to create a nationally representative survey. First, residential care facilities in the United States were randomly selected with probability proportional to facility size and geographic region. Then three to six current residents per facility were randomly selected. Data were collected during in person interviews at the facility. Facility staff members answered questions about residents based on existing facility health records and personal knowledge of the resident. No residents were interviewed (Moss et al., 2011).
Sample
For this analysis a subsample of older adults without dementia and with the potential to improve incontinence using conservative treatments, and to improve their physical function, was selected. The primary reasons for exclusion were having significant cognitive impairment, having a central nervous system disorder that impairs urinary function, and not being able to walk. Residents were excluded if they lived in a dementia ward (14%); had a diagnosis of dementia or Alzheimer's disease (42%); were less than age 65 years (11%); had an intellectual or developmental disability (3%); muscular dystrophy (<1%); a central nervous system disorder (8%); partial or total paralysis (2%); schizophrenia (8%); a spinal cord injury (1%); a traumatic brain injury (2%); or a stroke within the past year (2%); was blind (3%); bedbound (2%); or chair bound (11%) or had an ostomy (2%).
Measures
Toileting disability
A resident was considered to have toileting disability if the question, “Does the resident currently receive any assistance using the bathroom?” was answered “yes.” Intra-individual factors included demographic variables of age, sex, race, education, marital status, and English speaking ability. Other intra-individual factors included a rating of the resident's overall general health status, length of stay in the facility at the time of data collection, place admitted from, and part of services paid by Medicaid.
Extra-individual factors
Extra-individual factors included the facility size as measured by the number of beds, whether the facility was a for-profit facility, and if the resident has a bathroom inside his/her room or apartment.
Pathologies
Pathologies were measured with the question, “As far as you know, has a doctor or other health professional ever diagnosed [the resident] with the following condition?” Pathologies examined were arthritis, cancer, depression, diabetes, eye disease, hypertension, heart disease (indicated as one or more of the following: congestive heart failure, heart attack, coronary heart disease, other heart disease), kidney disease, lung disease (indicated as COPD, emphysema, asthma, chronic bronchitis), and stroke. Bowel and bladder incontinence were measured separately with the question, “Has [the resident] had any episode of [bowel/urinary incontinence] during the last seven days?”
Impairments
A measure of physical impairments was created by combining the responses to six questions that asked “Without assistance and without equipment, how difficult is it for [the resident] to (a) walk a quarter mile, about three city blocks; (b) stand or be on feet for about two hours; (c) stoop, bend, or kneel; (d) reach up over head; (e) use fingers to grasp or handle small objects; and (f) sit for about two hours?”The original response options ranged from 0 (not at all difficult) to 6 (does not do). A physical impairment score ranging from 0-6 was calculated based on the number of items where the resident had any level of difficulty with the activity. Higher scores indicate more impairments. Impairments with vision and hearing were also measured dichotomously.
Functional limitations
Functional limitations with ambulation were measured with three items: using a cane or walker when ambulating; needing assistance in walking; and needing help leaving the facility. Each item was answered with a yes or no response.
Coexisting disability
Three coexisting disabilities in basic activities of daily living were measured separately with the questions “Does [the resident] currently receive assistance in…(a) bathing or showering; (b) dressing; and (c) transferring in and out of bed or a chair?” Responses were answered “yes” or “no.” A single measure of disabilities in instrumental activities of daily living (IADL) was created by summarizing responses to the questions “Does [the resident] currently need help from another person with…(a) going shopping for personal items; (b) managing money; (c) using the telephone; (d) doing light housework; (e) taking medication; (f) transportation to stores and elsewhere; and (g) personal laundry. A total IADL score ranging from 0-7 was calculated based on the number of items the resident needed help with; higher scores reflecting greater disability.
Analysis
Descriptive statistics
Consistent with guidelines for the analysis of complex sample designs, unweighted frequencies and weighted percentages and weighted means with standard deviations were calculated to describe the sample characteristics and to identify the prevalence of toileting disability.
Logistic regression
A multivariable logistic regression model was used to identify factors associated with toileting disability. The selection of variables for the multivariable logistic regression model followed Hosmer and Lemeshow's guidelines (2000). The primary consideration for including variables was clinical relevance. All variables representing the primary hypothesis that incontinence, ambulation, transferring, bathing, and dressing difficulties occur with toileting disability were included. To avoid overfitting the model, intra- and extra-individual factors were screened with univariable logistic regression models. Variables with a p- value of < .05 in univariable models were included in the multivariable model. The rationale for screening these variables in this manner include a lack of literature identifying related environmental factors and the unknown influence disability correlates have with toileting disability. This screening method identified which intra- and extra-individual factors were associated with toileting disability and reduced the number of variables in the model. Given the occurrence of 398 events (individuals with toileting disability), the outer limit for the number of variables would be 40 and the final multivariable model met this limit. To identify issues of colinearity, correlations between the variables in the multivariable model were calculated.
Statistical software
Analyses were performed in Stata using the svy, subpop estimation functions (StataCorp. 2007. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP). The svy function includes design weights that account for the stratified, two-stage, random, sampling design which results in an unequal probability of being selected into the sample, and for the inherently correlated data that occurs when respondents live in the same facility (Levy & Lemeshow, 2008). The subpop function estimates the standard errors for the subsample using the entire sample, providing the most conservative estimates increasing the generalizability of the results (Levy & Lemeshow, 2008).
Results
This subsample (2395/8094) of older adults without dementia and with the potential to benefit from conservative treatments for incontinence and physical activity represents 35% of the NSRCFS sample after accounting for the sample weights. Fifteen percent of residents had toileting disability. Table 1 summarizes the characteristics for the total sample and compares the characteristics for those with and without toileting disability. The p value from the univariable logistic regression for each factor is also provided. The sample consisted mainly of English speaking, widowed, White women age 85 years or older with an educational attainment level of high school or less. Most residents lived in for-profit facilities with at least 26 beds for one to five years. Seventy-one percent of residents were not admitted to the residential care facility after a hospital, rehabilitation, or nursing home stay, and less than 12% had part of their services paid by Medicaid. The most common pathologies were hypertension, heart disease, arthritis, and depression. Over 18% had bladder incontinence and 6% had bowel incontinence. Residents had an average of four physical impairments. Visual and hearing impairments were present in 14% to16% of the sample. Functional limitations were common with 71% using a walker or cane, and 48% needing assistance in walking and leaving the facility. Common concurrent disabilities were bathing (57%) and dressing (32%).
Table 1. Comparisons between Residents with and Without Toileting Disability.
| Total Sample | Toileting Disability | No Toileting Disability | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| Variable | n | % | M (SD) | n | % | M (SD) | n | % | M (SD) | pa |
| Intra-Individual Factors | ||||||||||
| Age: 65-74 years | 206 | 7 | 23 | 7 | 183 | 8 | .85 | |||
| 75-84 years | 635 | 27 | 95 | 27 | 540 | 28 | ||||
| ≥ 85 | 1554 | 65 | 280 | 67 | 1274 | 65 | ||||
| Sex (Female) | 1766 | 73 | 308 | 75 | 1458 | 73 | .68 | |||
| Race (White) | 2249 | 94 | 371 | 94 | 1878 | 95 | .62 | |||
| Education: High school or less | 1244 | 46 | 208 | 48 | 1036 | 45 | .71 | |||
| Some college or more | 782 | 37 | 132 | 36 | 650 | 38 | ||||
| Don't know | 363 | 17 | 57 | 16 | 306 | 17 | ||||
| Marital status: Married | 263 | 12 | 35 | 11 | 228 | 12 | .04 | |||
| Divorced/legally separated | 174 | 7 | 22 | 5 | 152 | 7 | ||||
| Widowed | 1710 | 73 | 312 | 79 | 1398 | 72 | ||||
| Never married | 219 | 8 | 24 | 4.9 | 195 | 9 | ||||
| Language (English speaking) | 2342 | 99 | 386 | 98 | 1956 | 99 | .16 | |||
| Overall health rating: Excellent | 150 | 6 | 6 | 1 | 144 | 7 | < .0001 | |||
| Very good | 468 | 20 | 37 | 8 | 431 | 22 | ||||
| Good | 925 | 39 | 111 | 28 | 814 | 41 | ||||
| Fair | 687 | 29 | 179 | 48 | 508 | 25 | ||||
| Poor | 162 | 6 | 64 | 16 | 98 | 5 | ||||
| Length of stay: ≤ 1 year | 788 | 32 | 135 | 33 | 653 | 32 | .43 | |||
| 1-5 years | 1255 | 52 | 209 | 54 | 1046 | 52 | ||||
| > 5 years | 351 | 15 | 53 | 13 | 298 | 16 | ||||
| Place admitted from: Hospital | 240 | 9 | 42 | 11 | 198 | 9 | < .001 | |||
| Rehabilitation facility | 219 | 10 | 56 | 15 | 163 | 9 | ||||
| Nursing home | 271 | 10 | 60 | 14 | 211 | 9 | ||||
| None of the above | 1614 | 71 | 235 | 60 | 1379 | 73 | ||||
| Part of services paid by Medicaid | 351 | 12 | 54 | 12 | 297 | 12 | .96 | |||
| Extra-Individual Factors | ||||||||||
| Facility size: Small 4-10 beds | 286 | 5 | 100 | 13 | 186 | 3 | < .0001 | |||
| Medium 11-25 beds | 473 | 7 | 65 | 6 | 408 | 7 | ||||
| Large 26-100 beds | 1082 | 52 | 169 | 51 | 913 | 52 | ||||
| Extra large over 100 beds | 554 | 37 | 64 | 29 | 490 | 39 | ||||
| Facility profit status (for profit) | 1605 | 68 | 310 | 80 | 1295 | 66 | < .001 | |||
| Has bathroom inside room/apartment | 2107 | 95 | 324 | 90 | 1783 | 96 | < .0001 | |||
| Pathologies | ||||||||||
| Arthritis | 806 | 32 | 147 | 36 | 659 | 31 | .14 | |||
| Cancer/malignant neoplasm | 310 | 13 | 51 | 14 | 259 | 13 | .63 | |||
| Depression | 550 | 21 | 109 | 29 | 441 | 20 | < .001 | |||
| Diabetes | 443 | 18 | 76 | 19 | 367 | 17 | .46 | |||
| Eye disease | 298 | 12 | 40 | 9 | 258 | 12 | .08 | |||
| Hypertension | 1470 | 61 | 258 | 66 | 1221 | 61 | .14 | |||
| Heart disease | 990 | 41 | 182 | 44 | 808 | 40 | .25 | |||
| Lung disease | 431 | 17 | 85 | 20 | 346 | 17 | .13 | |||
| Stroke | 252 | 10 | 69 | 16 | 183 | 9 | < .001 | |||
| Bowel incontinence | 171 | 6 | 99 | 23 | 72 | 3 | < .0001 | |||
| Bladder incontinence | 528 | 18 | 219 | 53 | 309 | 12 | < .0001 | |||
| Impairments | ||||||||||
| Visual (even when wearing glasses) | 328 | 14 | 90 | 22 | 238 | 13 | < .001 | |||
| Hearing (severe)b | 419 | 16 | 70 | 16 | 349 | 16 | .04 | |||
| A little trouble hearing | 726 | 30 | 146 | 37 | 580 | 29 | ||||
| Hearing is good | 1247 | 54 | 182 | 47 | 1065 | 55 | ||||
| Physical impairment scale (range 0-6) | 4.1 (1.4) | 4.7 (1.1) | 3.9 (1.4) | < .0001 | ||||||
| Functional Limitations | ||||||||||
| Use a cane or walker | 1724 | 71 | 327 | 82 | 1397 | 70 | < .0001 | |||
| Assistance in walking | 1156 | 48 | 306 | 77 | 850 | 42 | < .0001 | |||
| Needs help leaving facility | 1153 | 46 | 300 | 76 | 853 | 41 | < .0001 | |||
| BADL Disabilities | ||||||||||
| Bathing | 1506 | 57 | 385 | 97 | 1121 | 50 | < .0001 | |||
| Dressing | 809 | 32 | 350 | 89 | 459 | 21 | < .0001 | |||
| Transferring | 263 | 10 | 201 | 50 | 62 | 3 | < .0001 | |||
| Toileting | 398 | 15 | N/Ac | N/Ac | N/Ac | |||||
| IADL Disabilities (range 0-7) | 3.1 (1.5) | 3.7 (1.4) | 2.9 (1.4) | < .0001 | ||||||
Note. N = 2395. Frequencies reported are raw numbers, but proportions are weighted.
p value is from univariable logistic regression. BADL = basic activities of daily living. IADL = instrumental activities of daily living. Toileting disability is the primary outcome in this analysis.
Severe hearing impairment reflects lot of trouble hearing or deaf without hearing aid.
Toileting disability is the outcome in this analysis.
Table 2 lists the factors associated with toileting disability in the multivariable logistic regression model. Only one intra-individual factor (having a fair or poor health status rating) was associated with toileting disability. Two extra-individual factors were associated with toileting disability, including living in a facility with four to 10 residents and living in a for-profit facility. Bladder and bowel incontinence were the only pathologies associated with toileting disability. Visual and hearing impairments were associated with having toileting disability. Having more physical impairments (i.e., walking, standing, sitting, stooping, reaching, and grasping) increased the odds of having toileting disability. For each one unit increase in the physical impairment score, the odds of having toileting disability increased by 27 percent. The functional limitation variables were not associated with toileting disability. Residents requiring dressing assistance were seven times more likely to have toileting disability, while those requiring transferring assistance were nine times more likely and those requiring bathing assistance were twice as likely.
Table 2. Multivariate Logistic Regression: Factors Associated with Toileting Disability.
| Characteristics | OR [(95% CI] | p |
|---|---|---|
| Intra-Individual Factors | ||
| Marital status (reference: married) | ||
| Divorced/legally separated | 0.96 [0.33, 2.82] | .94 |
| Widowed | 1.39 [0.77, 2.52] | .28 |
| Never married | 1.07 [0.47, 2.47] | .86 |
| Overall health rating (reference: excellent) | ||
| Very good | 2.06 [0.55, 7.66] | .28 |
| Good | 2.51 [0.65, 9.66] | .18 |
| Fair | 4.61 [1.20, 17.68] | .03 |
| Poor | 4.38 [1.05, 18.31] | .04 |
| Place admitted from (reference: hospital) | ||
| Rehabilitation facility | 1.08 [0.49, 2.36] | .85 |
| Nursing home | 1.54 [0.69, 3.45] | .30 |
| None of the above | 1.51 [0.79, 2.87] | .21 |
| Extra-individual Factors | ||
| Facility size (reference: extra large > 100 beds) | ||
| Small 4-10 beds | 2.59 [1.25, 5.38] | .01 |
| Medium 11-25 beds | 0.78 [0.41, 1.49] | .45 |
| Large 26-100 beds | 1.01 [0.62, 1.67] | .96 |
| For-profit facility | 1.82 [1.16, 2.84] | .009 |
| Has bathroom inside room/apartment | 1.12 [0.56, 2.27] | .74 |
| Pathologies | ||
| Depression | 1.04 [0.66, 1.62] | .88 |
| Stroke | 1.16 [0.64, 2.10] | .63 |
| Bowel incontinence | 2.19 [1.15, 4.17] | .02 |
| Bladder incontinence | 3.07 [2.01, 4.67] | < .0001 |
| Impairments | ||
| Physical impairments | 1.27 [1.06, 1.54] | .01 |
| Visual impairment (even when wearing glasses) | 0.59 [0.35, 0.99] | .05 |
| Hearing impairment (reference: no trouble hearing) | ||
| Severea | 0.48 [.27, .85] | .01 |
| A little trouble hearing | 0.81 [54, 1.22] | .32 |
| Functional Limitations | ||
| Uses a cane or walker | 1.11 [0.66, 1.89] | .68 |
| Receives any assistance walking | 1.45 [0.93, 2.28] | .10 |
| Needs assistance going outside | 1.49 [0.98, 2.26] | .06 |
| BADL Disabilities | ||
| Bathing | 2.57 [1.22, 5.42] | .01 |
| Dressing | 7.06 [4.43, 11.24] | < .0001 |
| Transferring | 9.45 [6.04, 14.80] | < .0001 |
| IADL Disabilities | 1.03 [0.89, 1.20] | .66 |
Note. N = 2,316. OR = odds ratio. CI = confidence interval. BADL = basic activities of daily living. IADL = instrumental activities of daily living.
Severe hearing impairment reflects lot of trouble hearing or deaf without hearing aid.
Colinearity among the variables in the multivariable model was minimal (see Table, Supplemental Digital Content 1, which illustrates correlations among the variables in the multivariable model). The only correlations exceeding .50 in absolute value were those between bathing and dressing disability (r = .58) and those between needing assistance walking and use of a cane or walker (r = .50). Since these variables represent key clinical variables they were retained in the final model.
Discussion
This study is the first to report the prevalence of and factors associated with toileting disability in older adults without dementia living in residential care facilities who may have the potential to implement conservative treatments for urinary incontinence and improve their physical function potentially reducing their risk for toileting disability. This subgroup represents 34% of all residents and indicates that about one third of residents may benefit from prevention efforts that accommodate their unique profile.
Approximately 15% had toileting disability. This prevalence is double that for community-dwelling older adults (Lee et al., 2006), but less than the 35% reported among all residential care facility residents (Caffrey et al., 2012).
The primary hypothesis that toileting disability is present when urinary and fecal incontinence occurs with physical impairments, transferring, bathing, and dressing difficulties was supported. These results describe generic skills needed for independent toileting such as the ability to walk, stand, sit, stoop, reach, grasp, transfer positions, bath, disrobe, and maintain continence. The results also indicate that as the number of impairments with walking, standing, sitting, stooping, reaching and grasping increases, so too does the likelihood of having a toileting disability. Thus, interventions attempting to prevent or manage toileting disability should focus on improving these skills.
Few environmental factors were associated with toileting disability. The only environmental factors associated with toileting disability were living in a for-profit facility or living in a small facility (4-10 beds).The presence of a bathroom inside the resident's room or apartment was not associated with toileting disability. However, the NSRCF did not ask about environmental factors, such as spaciousness of the bathroom, presence of grab bars, and height of the toilet seat, which may contribute to toileting disability. Visual impairments were also associated with toileting disability. It may be that the physical environment does not accommodate the needs of residents with visual impairment, such as having a clear accessible path to the bathroom. Hearing impairments were also associated with toileting disability. This association may represent difficulty with communicating the need for toileting between residents and paid caregivers.
The results of this study can be used to guide future research. Researchers interested in developing and testing prevention programs should take a multicomponent and multidisciplinary approach. For this group of older adults without dementia and central nervous system disorders contributing to urinary incontinence, the composition of prevention programs could include behavioral interventions for urinary incontinence and physical activity. Programs combining conservative treatments for urinary incontinence and physical activity have improved toileting skills in nursing home residents (Ouslander et al., 2005; Schnelle et al., 2002). Effective nursing home interventions have used caregiver dependent interventions such as prompted voiding (Fink, Taylor, Tacklind, Rutks, & Wilt, 2008). Programs can be modified for residents of residential care facilities who do not have dementia. Promising conservative behavioral treatments for incontinence include pelvic floor muscle exercises, bladder training, and lifestyle changes related to food and fluid consumption (Talley, Wyman, & Shamliyan, 2011). Physical activity programs adhering to national exercise recommendations (Nelson et al., 2007) should target walking, standing, sitting, stooping, reaching and grasping skills needed for independent toileting. Occupational and physical therapy could be used to improve dressing, bathing, and transferring skills.
These findings also suggest that the setting in which care is provided may influence toileting disability. Future research is needed to determine how the environment and resident-caregiver interactions influence toileting disability. There are limitations to this study, its cross-sectional design does not allow for temporal inferences. It is unknown what develops first—incontinence and impairments or toileting disability. However, the intent of the current study was to identify factors that could be investigated in future trials. Residents were not interviewed, rather facility staff familiar with their care answered questions using existing health records. Residents may have answered questions differently than facility staff. Still, there is face validity in using these sources as respondents, as these same health records are used to determine the level of care provided to residents and for reimbursement.
A limitation of using existing datasets is the reliance on the measures used in the survey. Toileting disability was measured with the question, “Does [the resident] currently receive any assistance using the bathroom?” The word “toilet” would have provided a more clear response than bathroom. This question does intend to ask about the need for toileting assistance,, however, and in the published data dictionary it is referred to as toileting help (http://www.cdc.gov/nchs/nsrcf/nsrcf_questionnaires.htm). Additionally, in the same section of the questionnaire, there are questions specifically asking about bathing/showering and dressing assistance, which further differentiates the question as addressing toileting.
There are additional limitations with using national surveys with a complex sampling design. In public use data sets, when cell sizes are less than 30, estimates using those variables are unreliable (Moss et. al., 2011). Unfortunately, this was the case with race and ethnicity variables, so the identification of racial and ethnic disparities was not possible. The degree to which subgroup analysis reflects the representativeness of the complex sample design is currently a topic of uncertainty in the field (Lee & Forthofer, 2006). In the current analysis, the proportion of facilities and residents in each of the 12 primary sampling strata differed an average of 3% (range 0%-7%) between the subgroup and entire sample. This minimal change in the composition of the primary sampling strata lend some confidence that the subgroup examined in the current study reflects of sampling design of the survey. Despite these limitations, the study's generalizability is strengthened by the use of a nationally representative sample, estimation procedures that account for the complex sampling design, and confirmation of a theory driven hypothesis.
Conclusions
This study identified the prevalence of and factors associated with toileting disability among older adults without dementia living in residential care facilities. The relatively high prevalence of toileting disability warrants prevention and management efforts. In this nationally representative sample, factors associated with toileting disability included having bowel and bladder incontinence, physical, visual and hearing impairments, and difficulties with dressing, bathing, and transferring. Multicomponent and multidisciplinary approaches may be needed to prevent or manage toileting disability. Promising prevention and management efforts may include conservative treatments for incontinence, physical activity programs targeting impairments with walking, standing, sitting, stooping, reaching and grasping, and therapy to improve dressing and transferring skills.
Supplementary Material
Supplemental Digital Content 1. Table that illustrates correlations among the variables in the multivariable model.
Acknowledgments
The authors acknowledge their research was supported by the Building Interdisciplinary Research Careers in Women's Health Grant (# K12HD055887) from the Eunice Kennedy Shriver National Institutes of Child Health and Human Development (NICHD), the Office of Research on Women's Health, and the National Institute on Aging, NIH, administered by the University of Minnesota Deborah E. Powell Center for Women's Health. The content is solely the responsibility of the authors and does not necessarily represent the office views of the NICHD or NIH. Parts of this project were presented at the 2012 Gerontological Society of America's Annual Meeting in San Diego, CA.
Footnotes
The authors have no conflicts of interest to report.
References
- Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Fourth International Consultation on Incontinence. Fourth International Consultation on Incontinence recommendations of the international scientific committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourology and Urodynamics. 2010;29:213–240. doi: 10.1002/nau.20870. [DOI] [PubMed] [Google Scholar]
- Caffrey C, Sengupta M, Park-Lee E, Moss A, Rosenoff E, Harris-Kojetin L. NCHS Data Brief No 91. Hyattsville, MD: National Center for Health Statistics; 2012. Residents living in residential care facilities: United States, 2010. Retrieved from http://www.cdc.gov/nchs/data/databriefs/db91.htm. [PubMed] [Google Scholar]
- Carey EC, Covinsky KE, Lui LY, Eng C, Sands LP, Walter LC. Prediction of mortality in community-living frail elderly people with long-term care needs. Journal of the American Geriatrics Society. 2008;56:68–75. doi: 10.1111/j.1532-5415.2007.01496.x. [DOI] [PubMed] [Google Scholar]
- DuBeau CE, Kuchel GA, Johnson T, II, Palmer MH, Wagg A Fourth International Consultation on Incontinence. Incontinence in the frail elderly: Report from the 4th International Consultation on Incontinence. Neurourology and Urodynamics. 2010;29:165–178. doi: 10.1002/nau.20842. [DOI] [PubMed] [Google Scholar]
- Fink HA, Taylor BC, Tacklind JW, Rutks IR, Wilt TJ. Treatment interventions in nursing home residents with urinary incontinence: A systematic review of randomized trials. Mayo Clinic Proceedings. 2008;83:1332–1343. doi: 10.1016/S0025-6196(11)60781-7. [DOI] [PubMed] [Google Scholar]
- Holroyd-Leduc JM, Mehta KM, Covinsky KE. Urinary incontinence and its association with death, nursing home admission, and functional decline. Journal of the American Geriatrics Society. 2004;52:712–718. doi: 10.1111/j.1532-5415.2004.52207.x. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied logistic regression. 2nd. New York, NY: Wiley; 2000. [Google Scholar]
- Hunskaar S, Arnold EP, Burgio K, Diokno AC, Herzog AR, Mallett VT. Epidemiology and natural history of urinary incontinence. International Urogynecology Journal. 2000;11:301–319. doi: 10.1016/S0090-4295(03)00755-6. [DOI] [PubMed] [Google Scholar]
- Johnson TM, II, Bernard SL, Kincade JE, Defriese GH. Urinary incontinence and risk of death among community-living elderly people: Results from the national survey on self-care and aging. Journal of Aging and Health. 2000;12:25–46. doi: 10.1177/089826430001200102. [DOI] [PubMed] [Google Scholar]
- Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. Vital and Health Statistics. Vol. 13. National Center for Health Statistics; 2009. The National Nursing Home Survey: 2004 overview; pp. 1–155. Retrieved from http://www.cdc.gov/nchs/data/series/sr_13/sr13_167.pdf. [PubMed] [Google Scholar]
- Jones AL, Sonnenfeld NL, Harris-Kojetin LD. NCHS Data Brief No 25. Hyattsville, MD: National Center for Health Statistics; 2009. Racial differences in functioning among elderly nursing home residents, 2004. Retrieved from http://www.cdc.gov/nchs/data/databriefs/db25.pdf. [PubMed] [Google Scholar]
- Kane RL, Talley KMC, Shamliyan T, Pacala JT. Evidence Report/Technology assessment No 87, AHRQ publication no 11-05157-EF-1. Rockville, MD: Agency for Healthcare Research and Quality; 2011. Common syndromes in older adults related to primary and secondary prevention. Retrieved from http://www.uspreventiveservicestaskforce.org/uspstf11/es87.pdf. [PubMed] [Google Scholar]
- Lee ES, Forthofer RN. Analyzing complex survey data. 2nd. Thousand Oaks, CA: Sage; 2006. [Google Scholar]
- Lee SJ, Lindquist K, Segal MR, Covinsky KE. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295:801–808. doi: 10.1001/jama.295.7.801. [DOI] [PubMed] [Google Scholar]
- Levy PS, Lemeshow S. Sampling of populations: Methods and applications. 4th. New York, NY: Wiley; 2008. [Google Scholar]
- Moss AJ, Harris-Kojetin LD, Sengupta M, Park-Lee E, Caffrey C National Center for Health Statistics,… RTI International. Design and operation of the 2010 National Survey of Residential Care Facilities. National Center for Health Statistics. Vital Health Statistics. 2011;1 Retrieved from http://www.cdc.gov/nchs/data/series/sr_01/sr01_054.pdf. [PubMed] [Google Scholar]
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, Castaneda-Sceppa C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Medicine & Science in Sports & Exercise. 2007;39:1435–1445. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- Nuotio M, Tammela TL, Luukkaala T, Jylhä M. Urgency and urge incontinence in an older population: Ten-year changes and their association with mortality. Aging Clinical and Experimental Research. 2002;14:412–419. doi: 10.1007/BF03324470. [DOI] [PubMed] [Google Scholar]
- Ouslander JG, Griffiths PC, McConnell E, Riolo L, Kutner M, Schnelle J. Functional incidental training: A randomized, controlled, crossover trial in veterans affairs nursing homes. Journal of the American Geriatrics Society. 2005;53:1091–1100. doi: 10.1111/j.1532-5415.2005.53359.x. [DOI] [PubMed] [Google Scholar]
- Park-Lee E, Caffrey C, Sengupta M, Moss AJ, Rosenoff E, Harris-Kojetin LD. NCHS data brief, No 78. Hyattsville, MD: National Center for Health Statistics; 2011. Residential care facilities: A key sector in the spectrum of long-term care providers in the United States. Retrieved from http://www.cdc.gov/nchs/data/databriefs/db78.htm. [PubMed] [Google Scholar]
- Prudential Research Report. Long-term care cost study. Newark, NJ: The Prudential Insurance Company of America; 2010. Retrieved from http://www.taberbrokerage.com/uploads/resource-1341248107.pdf. [Google Scholar]
- Schnelle JF, Alessi CA, Simmons SF, Al-Samarrai NR, Beck JC, Ouslander JG. Translating clinical research into practice: A randomized controlled trial of exercise and incontinence care with nursing home residents. Journal of the American Geriatrics Society. 2002;50:1476–1483. doi: 10.1046/j.1532-5415.2002.50401.x. [DOI] [PubMed] [Google Scholar]
- Talley KMC, Wyman JF, Shamliyan TA. State of the science: Conservative interventions for urinary incontinence in frail community-dwelling older adults. Nursing Outlook. 2011;59:215–220.e1. doi: 10.1016/j.outlook.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge LM, Jette AM. The disablement process. Social Science & Medicine. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Wyman JF, Elswick RK, Ory MG, Wilson MS, Fantl JA. Influence of functional, urological, and environmental characteristics on urinary incontinence in community-dwelling older women. Nursing Research. 1993;42:270–275. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. Table that illustrates correlations among the variables in the multivariable model.