Abstract
In the last decade, preclinical investigations of electroacupuncture mechanisms on persistent tissue-injury (inflammatory), nerve-injury (neuropathic), cancer, and visceral pain have increased. These studies show that electroacupuncture activates the nervous system differently in health than in pain conditions, alleviates both sensory and affective inflammatory pain, and inhibits inflammatory and neuropathic pain more effectively at 2–10 Hz than at 100 Hz. Electroacupuncture blocks pain by activating a variety of bioactive chemicals through peripheral, spinal, and supraspinal mechanisms. These include opioids, which desensitize peripheral nociceptors and reduce pro-inflammatory cytokines peripherally and in the spinal cord, and serotonin and norepinephrine, which decrease spinal n-methyl-d-aspartate receptor subunit GluN1 phosphorylation. Additional studies suggest that electroacupuncture, when combined with low dosages of conventional analgesics, provides effective pain management that can forestall the side effects of often-debilitating pharmaceuticals.
Introduction
Pain, a major health problem with serious social and economic consequences, costs the economy $560–635 billion annually in physician visits, analgesics, and loss of productivity.1 Conventional medical treatments are only moderately efficacious, and they often produce problematic side effects. Acupuncture/electroacupuncture, used in China and other Asian countries for the past 3,000 yr, represents a potentially valuable adjunct to existing pain relief strategies.2 Approximately two million American adults used acupuncture in 2002;3 this increased to three million in 2007, with chronic pain being the most common reason for seeking acupuncture treatment. Concomitant with increasing use of the modality, research has been performed on acupuncture mechanisms, and data from these studies have accumulated.
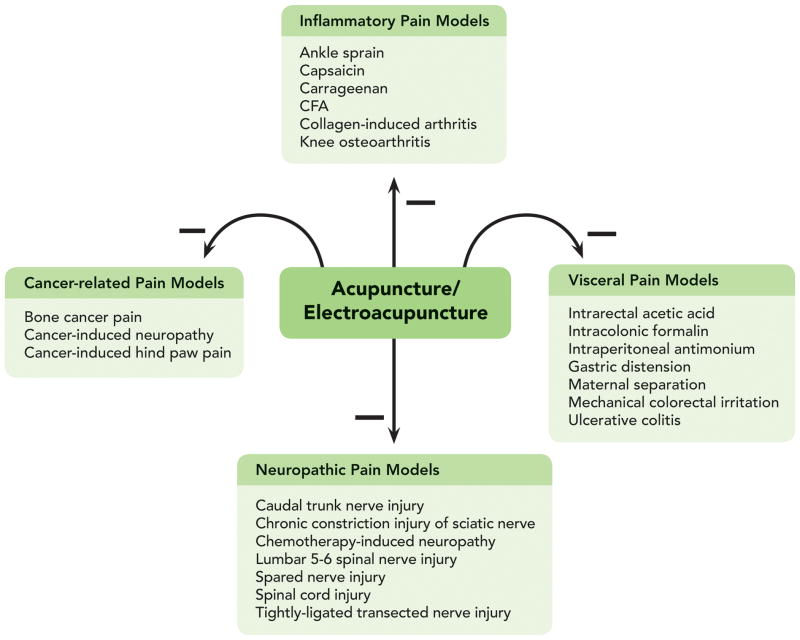
Based on etiology, pain may be classified into tissue damage-induced inflammatory/nociception and nerve damage-induced neuropathy. The former is caused by a painful stimulus on nociceptors, the latter by a primary lesion or dysfunction in the nervous system. Based on origin, pain may also be classified as somatic or visceral. Notably, some pain, for example cancer-related pain, experienced by one-third of patients receiving treatment for cancer and about two-thirds of those with advanced cancers, is not easily classifiable. A variety of animal models have been used to study the effect and mechanisms of electroacupuncture on persistent pain (fig. 1). This review synthesizes these studies to give an overall picture of how electroacupuncture alleviates pain through peripheral and central mechanisms of the body and to show that a number of bioactive chemicals are involved in electroacupuncture inhibition of pain.
Figure 1.
Electroacupuncture inhibits inflammatory, neuropathic, cancer, and visceral pain in various animal models.
1. Inflammatory pain animal models
The effect and mechanisms of acupuncture/electroacupuncture on persistent pain have been studied at peripheral, spinal, and supraspinal levels using inflammatory pain animal models, most of which were produced by complete Freund’s adjuvant (CFA: inactivated and dried Mycobacterium and adjuvant) or carrageenan. Many bioactive chemicals are involved in electroacupuncture inhibition of pain (table 1).
Table 1.
Bioactive Chemicals Involved in Electroacupuncture Attenuation of Persistent Pain in Animal Models
| Models | Peripheral | Spinal cord | Supraspinal |
|---|---|---|---|
| Inflammatory pain | Adenosine Cannabinoids CB2R, Corticosterone COX-2, CRF IAM-1 IL-1β, IL-6, PGE2 Opioids, TNF-α |
5-HT1AR, 5-HT2AR Acid-sensing ion channel 3 Akt, α2-adrenoceptors Dopamine D2 receptors Glutamate-aspartate transporter Glutamate transporter-1, GluN2A GluA1, p-GluN1, Glutamate, IL-1β, IL-6 Muscarinic cholinergic receptor Norepinephrine, Opioids, Serotonin Substance P, N/OFQ p-38 MAPK, PI3K, TNF-α |
CCK-8 GABA IL-1 receptor type I Opioids |
| Neuropathic pain | IL-1β, IL-6, TNF-α | 5-HT1AR, 5-HT3R, α2-adrenoceptors Aspartate, COX-2, extracellular signal-regulated kinases GABA, GABA receptor A, GABA receptor B GDNF, GFRα-1, Glutamate Glutamine, Glycine, IL-6, IL-1β Inducible Nitric Oxide Synthases Matrix Metallopeptidase-2/-9 Muscarinic M(1) receptors, Norepinephrine Opioids, p38 MAPK, PGE2, Serotonin Somatostatin, Superoxide anion Taurine, TNF-α |
|
| Cancer pain | β-endorphins | IL-1β, dynorphines, Substance P, TRPV1 | β-endorphins |
| Visceral pain | β-endorphins, NK1 receptors Substance P, TNF-α, VIP VIP receptors |
p38 MAPK Serotonin |
5-HT, β-endorphins CRF, GluN1 Substance P |
5-HT1AR = 5-hydroxytryptamine 1A receptors; 5-HT2AR = 5-hydroxytryptamine 2A receptors; CB2R = cannabinoid CB2 receptors; CCK-8 = Cholecystokinin octapeptide; COX-2 = cyclooxygenase-2; CRF = corticotrophin-releasing factor; GABA = γ-aminobutyric acid; GDNF = glial cell line-derived neurotrophic factor; GFRα-1 = GDNF family receptor α-1; IAM-1 = Intracellular adhesion molecule-1; IL-6 = interleukin-6; IL-1β = interleukin-1beta; NK-1 = neurokinin 1; N/OFQ = Nociceptin/orphanin FQ; p-38 MAPK = p-38 mitogen-activated protein kinase; PGE2 = prostaglandin E2; p-GluN1 = phosphorylated GluN1; TNF-α = tumor necrosis factor-α; TRPV1 = transient receptor potential cation channel subfamily V member 1; VIP = vasoactive intestinal polypeptides.
1.1. Peripheral mechanisms
Peripheral inflammatory cells-released opioids are involved in electroacupuncture inhibition of inflammatory pain. Studies in carrageenan-induced inflammatory pain rat models show that an intraplantar injection of naloxone or selective antagonists against μ (D-Phe-Cys-Tyr-D-Trp-Orn-Thr-Pen-ThrNH2), δ (naltrindole), or κ (nor-Binaltorphimine) opioid receptors 1 h before electroacupuncture treatment at Zusanli (ST36, fig. 2) dosage-dependently blocked electroacupuncture-produced inhibition of mechanical hyperalgesia assessed through paw pressure threshold.4,5 Consistent with these results, intraplantar naloxone methiodide, a peripherally acting opioid receptor antagonist and an antibody against β-endorphin, eliminated electroacupuncture-produced inhibition of CFA-induced thermal hyperalgesia assessed with paw withdrawal latency (PWL) in response to radiant thermal stimuli.6 These data indicate that electroacupuncture induces release of endogenous opioids from lymphocytes, monocytes/macrophages, and granulocytes7,8 into inflamed skin. The opioids in turn activate receptors on peripheral nerve terminals to suppress nociception.
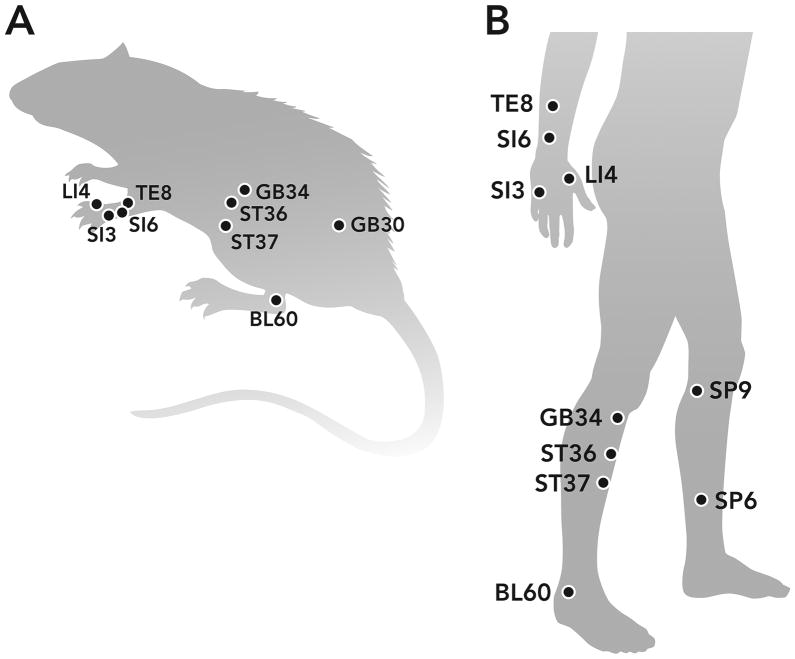
Figure 2.
Rat and human maps of acupoints used in pain studies.
Electroacupuncture activates sympathetic nerve fibers to increase endogenous opioid in inflammatory site. Sympathetic nerve fiber activation enhances the expression of intracellular adhesion molecule-1 in the blood vessels of inflamed tissue to promote migration of β-endorphin- and met-enkephalin-containing polymorphonuclear leukocytes and mononuclear cells in rats with CFA-induced hind paw inflammation.9 Further, sympathetic neuron-derived norepinephrine stimulates adrenergic receptors on inflammatory cells to release β-endorphin, leading to inhibition of pain.10 Electroacupuncture activates sympathetic nerve fibers to inhibit pain,11,12 although the exact mechanism is not clear. For instance, pretreatment with either 6-hydroxydopamine, a neurotoxin for sympathetic nerve endings, or the β-adrenoceptor antagonist propranolol, significantly prevents electroacupuncture inhibition of carrageenan-induced thermal hyperalgesia.13 This electroacupuncture action on sympathetic nerves might enhance migration of opioid-containing cells to an inflammatory site, increasing the release of endogenous opioids.
Electroacupuncture also increases endogenous cannabinoid CB2 receptors (CB2R) to upregulate opioids in inflamed skin tissue. At Huantiao (GB30) and Yanglingquan (GB34), the modality significantly elevated proopiomelanocortin messenger RNA (mRNA) and β-endorphin levels in inflamed skin tissue as well as the percentage of β-endorphin-immunoreactive keratinocytes, macrophages, and T-lymphocytes.14 These effects were significantly attenuated by CB2R antagonist AM630 pretreatment. Interestingly, electroacupuncture also increased the levels of endogenous anandamide in inflamed tissue15 and the expression of CB2R on keratinocytes, macrophages, and T-lymphocytes in inflammation.16
In a recent study in the CFA-induced inflammatory pain rat model, electroacupuncture significantly increased PWL and mechanical threshold assessed with von Frey filaments and significantly decreased tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), and IL-6 expression in inflamed skin.17 Moreover, electroacupuncture’s inhibition of pain was significantly attenuated by the CB2R antagonist AM630, as was cytokine expression.17 Since proinflammatory cytokines facilitate nociception18 and morphine inhibits cytokine release from peripheral blood mononuclear cell cultures,19,20 electroacupuncture mitigates pain by upregulating endogenous anandamide, which activates CB2R to promote opioid production, consequently blocking cytokine release to inhibit pain.
Electroacupuncture inhibition of cyclooxygenase-2 (COX-2) might increase levels of endogenous anandamide. The modality activated the hypothalamus-pituitary-adrenal axis to significantly increase plasma corticosterone levels in a CFA-inflammatory pain rat model21,22 and significantly downregulated carrageenan-induced expression of COX-1, COX-2 mRNA, and their proteins.23 It is known that the endocannabinoids anandamide and 2-arachidonoyl glycerol are metabolized by fatty acid amide hydrolase, monoacylglycerol lipase, and COX-2.24 Thus electroacupuncture-induced corticosterone might inhibit COX-2 to interfere with endocannabinoid metabolism, resulting in their escalation at inflammatory sites and leading to an increase in opioids.
Corticotrophin-releasing factor (CRF) and prostaglandin E2 (PGE2) are also involved in electroacupuncture analgesia. For instance, an intraplantar CRF antagonist also prevented electroacupuncture inhibition of inflammatory pain.6,25 CRF is known to block pain by stimulating the release of opioids from immune cells.26,27 Thus electroacupuncture might induce skin fibroblasts to release CRF, which in turn stimulates opioid release to inhibit pain. Electroacupuncture decreased carrageenan-induced PGE2 in inflammatory paws;23 since PGE2 receptor activation of peripheral nociceptors contributes to pain, this ability to inhibit PGE2 might also be a factor in electroacupuncture’s effect on pain.28
Manual acupuncture or a local injection of the adenosine A1 receptor agonist 2-chloro-N(6)-cyclopentyladenosine at acupoint ST36 significantly inhibits mechanical allodynia and thermal hyperalgesia in wild-type but not in adenosine A1 receptor knockout mice with inflammatory and neuropathic pain.29 Additionally, both interventions suppress high-intensity stimulation-evoked field excitatory postsynaptic potentials in the anterior cingulate cortex (ACC). Acupuncture also significantly increased extracellular adenosine near ST36. The investigators concluded that acupuncture attenuated the pain by increasing local adenosine that acts on A1 receptors in sensory afferents of ascending nerve tracks.29
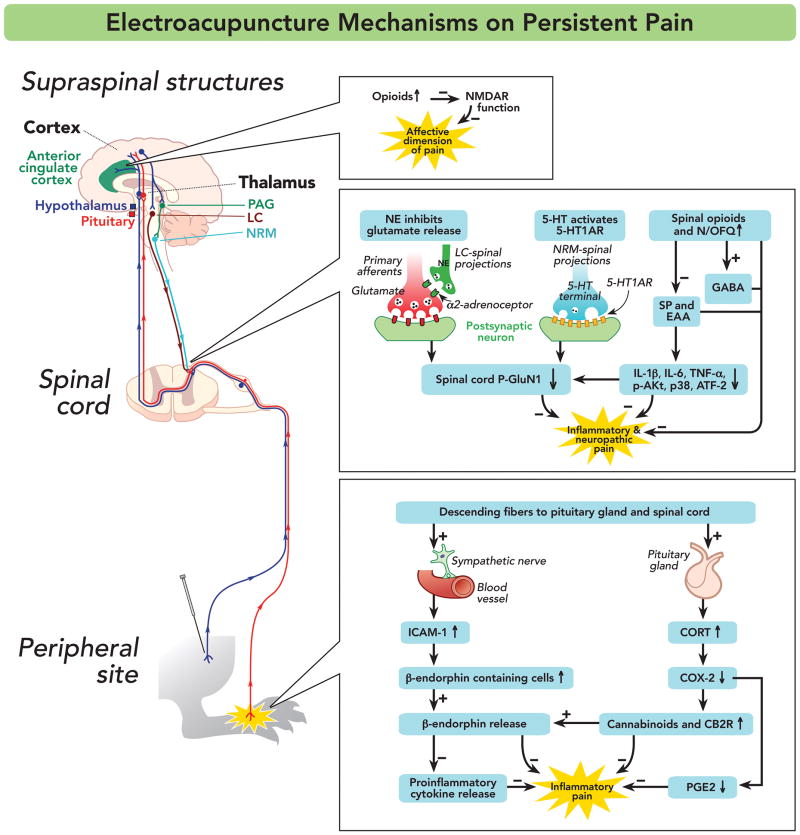
Collectively, these studies demonstrate that peripheral opioids play a central role in electroacupuncture inhibition of inflammatory pain by blocking proinflammatory cytokine release from polymorphonuclear leukocytes and mononuclear cells and by acting on peripheral opioid receptors to desensitize peripheral sensory nerves (fig. 3).
Figure 3.
Mechanisms of electroacupuncture inhibition of inflammatory and neuropathic pain. Symbols + and − respectively represent enhancement and inhibition. 5-HT1AR = 5-hydroxytryptamine 1A receptors; ACC = anterior cingulated cortex; ATF-2 = activating transcription factor-2;CB2R = Cannabinoid 2 receptor; CORT = corticosterone; COX-2 = cyclooxygenase-2; EAA = excitatory amino acid; GABA = γ-aminobutyric acid; ICAM-1 = intracellular adhesion molecule-1; IL-6 = interleukin-6; IL-1β = interleukin-1beta; LC = locus coeruleus; N/OFQ = nociceptin/orphanin FQ; NE = norepinephrine; NMDAR = n-methyl-d-aspartate receptor; NRM = nucleus raphe magnus; PAG = periaqueductal grey; p-Akt = phosphorylated Akt; PGE2 = prostaglandin E2; pGluN1 = phosphorylated GluN1; SP = substance P; TNF-α = tumor necrosis factor-α.
Electroacupuncture increases opioids at inflammatory sites via two pathways. 1) It activates sympathetic nerve fibers to enhance migration of opioid-containing cells to the site. 2) It triggers hypothalamus-pituitary-adrenal to decrease COX-2, which in turn interfere with endocannabinoid metabolism, leading to increased levels of opioids at the site. Furthermore, electroacupuncture might decrease COX-2, thus lowering PGE2 levels and alleviating pain. Electroacupuncture-upregulated endocannabinoid may directly inhibit pain because CB2 receptor activation inhibits sensory nerve activities in rat pain model.30 Although peripheral CRF and adenosine are involved in electroacupuncture action, how the modality modulates their synthesis warrants further investigation.
Overall, although the current studies show that opioid, cytokines, cannabinoids, CB2R, CRF, PGE2, and adenosine are involved in acupuncture/electroacupuncture analgesia, other peripheral bioactive chemicals and receptors such as serotonin, nerve growth factor, bradykinin, and transient receptor potential channels 31 are implicated in inflammatory pain. Their involvement in electroacupuncture analgesia is yet to be investigated.
1.2. Spinal mechanisms
Several studies demonstrate that electroacupuncture inhibits peripheral inflammation-induced Fos expression in the spinal cord.32–34 These indicate that electroacupuncture dampens the transmission of noxious inputs at the spinal level with the involvement of spinal opioids, serotonin (i.e., 5-hydroxytryptamine [5-HT]), norepinephrine, glutamate, glial cell/cytokines, and signal molecules.
1.2.1. Opioids
Electroacupuncture acts on spinal opioid receptors differently in acute pain and persistent inflammatory conditions. In studies with uninjured rats, low frequency (2 Hz) electroacupuncture at acupoint ST36 activated endorphin/endomorphin and enkephalin, while high frequency (100 Hz) electroacupuncture activated dynorphin to suppress nociception as assessed by the tail flick test.35
In a systematic evaluation of the effect of electroacupuncture frequency, intensity, treatment duration, and pulse width in a CFA-induced inflammatory pain rat model, Dr. Lao and his colleagues found that 10 and 100 Hz electroacupuncture at GB30 both significantly increased PWL. However, the effects of treatment at 10 Hz endured longer than did those of 100 Hz34 due to the greater inhibition of inflammation of the former.36 That team also showed that both 10 and 100 Hz electroacupuncture-produced inhibition of thermal hyperalgesia was blocked by intrathecal μ and δ opioid receptor antagonists but not a κ opioid receptor antagonist.37 Kim et al.,38 in a capsaicin-induced inflammatory hind paw pain model, delivered 2 Hz of four-train pulses with 100 Hz of intra-train frequency at Houxi (SI3) and Sanyangluo (TE8) on the forelimb. This stimulation significantly raised the mechanical pain threshold of the injected paw, an effect blocked by intrathecal μ or δ opioid receptor antagonists but, again, not by a κ opioid receptor antagonist.
In a rat model produced by a carrageenan injection into the knee cavity, pretreatment with 10 Hz electroacupuncture at ST36 prior to the injection significantly improved weight-bearing force (WBF), an indication of spontaneous pain, in the injected hind limb.39 This analgesic effect was blocked by an intrathecal μ-opioid receptor antagonist but not by δ or κ opioid receptor antagonists.39
In a study with a rat model of ankle sprain pain, 2 Hz of four-train pulses with 100 Hz of intra-train frequency were delivered on the forelimb at Yanglao (SI6) and Hegu (LI4).40 Electroacupuncture increased stepping force of the affected limb, and this analgesic effect was not blocked by systemic injection of the opioid antagonists naloxone or naltrexone. Using the same model, 10 Hz electroacupuncture at acupoint SI6 on the forelimb contralateral to the sprained ankle significantly improved stepping force of the sprained paw and suppressed spinal dorsal horn neural activity.41 This improvement in stepping force of the affected paw and electroacupuncture inhibition of spinal dorsal horn neural hyperactivity were not blocked by a 10 mg/kg intraperitoneal injection of the opioid receptor antagonist naltrexone, which implies that endogenous opioids are not involved in electroacupuncture-produced analgesia in walking-evoked pain in an ankle sprain pain model. However, this phenomenon needs to be confirmed with varying dosages of opioid receptor antagonist administered to the spinal cord, since different dosages of naltrexone produce distinct effects42 and systemic naltrexone-produced supraspinal and spinal effects might offset each other.
Collectively, these studies show that low and high frequency electroacupuncture respectively inhibit thermal pain through μ, δ, and κ opioid receptors during acute pain, but during persistent pain conditions both high and low frequencies inhibit thermal, mechanical, and spontaneous pain through μ and δ opioid receptors (table 2). The differential involvement of opioid receptors might be due to changes in sensitivity of the receptors during persistent pain. For example, dosage–response curves for intrathecally administered μ and/or δ opioid agonists, determined by PWL to noxious thermal stimuli, were shifted to the left for carrageenan-inflamed hind paws in comparison to contralateral uninflamed paws. A selective intrathecal κ receptor agonist showed no activity in this analgesic assay on either inflamed or noninflamed paws.43 μ and δ but not κ receptor agonists dosage-dependently reduced mechanical hyperalgesia following repeated intramuscular injections of acid.44 Since μ and δ receptors are distributed on both presynaptic primary afferent fibers and postsynaptic dorsal horn neurons,45 electroacupuncture-induced opioids might inhibit the activity of noxious neurons via pre- and post-synaptic mechanisms.
Table 2.
Differential Involvement of Opioid Receptors in Electroacupuncture Attenuation of Pain during Health and in Pain Conditions
| Model | EA | test | opioid receptors | Refs |
|---|---|---|---|---|
| Uninjured | 2 Hz | Tail flick | μ | 35 |
| Uninjured | 15 Hz | Tail flick | μ, δ, and κ | 35 |
| Uninjured | 100 Hz | Tail flick | κ | 35 |
| Ankle sprain pain | 2Hz/100 Hz | Stepping force | None | 40 |
| Ankle sprain pain | 10 Hz | Stepping force | None | 41 |
| Intra-plantar CFA | 10 Hz and 100 Hz | Paw withdrawal latency | μ and δ | 37 |
| Intra-plantar capsaicin | 2Hz/100 Hz | Mechanical threshold | μ and δ | 38 |
| Intra-knee carrageenan | 10 Hz | Weight-bearing force | μ | 39 |
| Chemotherapy Neuropathy |
10 Hz | Mechanical threshold | μ, δ, and κ | 136 |
CFA = complete Freund’s adjuvant.
The fact that electroacupuncture induces endogenous opioids to inhibit pain has clinical significance. Electroacupuncture, added to opioid therapy, might decrease the dosages required for pain control. Indeed, in our study, electroacupuncture combined with low-dosage morphine suppressed inflammatory pain better than either one did individually.37
Nociceptin/orphanin FQ (N/OFQ) and opioid-like receptors play important roles in pain modulation.46 Fu et al.47 report that 2 and 60 Hz electroacupuncture at GB30 and GB34 significantly increased N/OFQ and opioid-like receptors in the spinal cord in a CFA-induced inflammatory pain model. Moreover, intrathecal [Nphe(1)]nociceptin(1–13)NH(2), a selective antagonist of the N/OFQ peptide receptor, significantly blocked electroacupuncture inhibition of thermal hyperalgesia, which indicates that the N/OFQ receptor mediates electroacupuncture analgesia.48 N/OFQ has been observed in fibers and neurons in superficial laminae of the dorsal horn,49 and it inhibits C-fiber-evoked responses and wind up.50 This leads to the conclusion that electroacupuncture attenuates pain by inducing release of spinal N/OFQ through both pre- and post-synaptic mechanisms.
Cholecystokinin octapeptide (CCK-8), a physiological antagonist of endogenous opioids in the central nervous system, attenuates electroacupuncture analgesia. Studies in uninjured animals show that electroacupuncture produces greater analgesia in CCK-8- and CCKa receptor-deficient rats than in control animals.51,52 Intracerebroventricular antisense CCK expression vector pSV2-CCKAS converts rats with low response to electroacupuncture and morphine into high responders,53 while subcutaneous CCK(B) receptor antagonist L365,260 produces dosage-dependent (0.125–2.0 mg/kg) potentiation of analgesia induced by 100 Hz electroacupuncture.54
Other studies show that CCKa receptors in the hypothalamus and nucleus parafascicularis and CCKb receptors in the periaqueductal grey (PAG) are associated with electroacupuncture analgesia.55–57 Interestingly, CCKa receptor-deficient rats with neuropathic pain showed more robust response to electroacupuncture treatment than did normal rats.58 The data lead us to hypothesize that dampened CCK function promotes acupuncture/electroacupuncture and morphine analgesia and that patients given a CCK receptor antagonist will be more sensitive to acupuncture treatment than those not given the antagonist. This warrants clinical investigation.
1.2.2. Norepinephrine and serotonin
Li et al.59 report that electroacupuncture activated serotonin-containing nucleus raphe magnus (NRM) neurons and norepinephrine-containing locus coeruleus neurons that project to the spinal cord. That study and studies in uninjured rats60–63 indicate that spinal serotonin and norepinephrine are involved in electroacupuncture analgesia.
Numerous studies show serotonin and norepinephrine involvement in electroacupuncture’s inhibition of pain. Silva et al.64 used the tail flick test in uninjured rats to show that the nonselective serotonin receptor antagonist methysergide blocked both 2 and 100 Hz electroacupuncture-produced analgesia, while α1- and α2-adrenoceptors antagonists only prevented 2 Hz-induced analgesia. In an intra-knee carageenan-produced rat model, systemic administration of the nonselective adrenergic receptor antagonist yohimbine and the 5-HT3 receptor (5-HT3R) antagonist ondansetron blocked 2-Hz electroacupuncture-produced increase of weight bearing in an injured hind limb.65 In a collagen-induced arthritis model, systemic administration of spiroxatrine, a 5-HT1A receptor (5-HT1AR) antagonist and a 5-HT3R antagonist blocked 2 Hz electroacupuncture analgesia evaluated with the tail flick test; ketanserin, a 5-HT2 receptor (5-HT2R) antagonist, did not.66 In a behavioral and electrophysiological study in an ankle sprain rat model, 10 Hz electroacupuncture applied contralaterally to SI6 significantly improved WBF of the sprained side and suppressed spinal dorsal horn neuron activities.41 This intervention had no effect in normal rats, and the electroacupuncture effect was blocked by the alpha-adrenoceptor antagonist phentolamine. These studies clearly demonstrated that serotonin and norepinephrine are involved in electroacupuncture-produced pain inhibition but did not differentiate between spinal and supraspinal levels of antagonist action.
Administration of intrathecal antagonist demonstrated that spinal norepinephrine and serotonin are involved in electroacupuncture inhibition of pain. Intrathecal yohimbine, an α2 adrenergic antagonist, reduced 2-Hz electroacupuncture-induced analgesia in a rat model of ankle sprain, but terazosin, an α1-adrenergic antagonist, had no effect.67 Consistent with these results, studies show that an intrathecal α2a-adrenoceptor antagonist blocked 10-Hz electroacupuncture anti-hyperalgesia in a CFA-induced inflammatory pain model, while an α2b-adrenoceptor antagonist did not.68 These studies indicate that spinal α2a-adrenoceptors are involved in 2–10 Hz electroacupuncture analgesia in inflammatory pain. In prior studies, α2a-adrenoceptor activation diminished glutamate release from the spinal cord,69 and group I metabotropic glutamate receptors enhanced phosphorylation of n-methyl-d-aspartate receptor (NMDAR) subunit GluN1 (NR1),70 which modulates NMDAR activity and promotes transmission of nociceptive inputs in inflammatory pain models.71 Moreover, intrathecal clonidine, an α2-adrenoceptor agonist, significantly suppressed GluN1 phosphorylation in a pain model.72 Immunohistochemistry shows that α2a-adrenoceptors are located in primary afferents in the spinal cord.68,73 Collectively, these studies show that electroacupuncture increases spinal norepinephrine to pre-synaptically decrease glutamate release, thus inhibiting GluN1 phosphorylation and pain (fig. 3).
Studies also demonstrate that 10 Hz electroacupuncture inhibits thermal hyperalgesia through spinal 5-HT1AR but not 5-HT2BR, 5-HT2CR, or 5-HT3R in a CFA inflammatory pain model,68,74 and improves WBF through 5-HT2AR in a knee osteoarthritis pain model.75 Investigation shows that 5-HT1AR activation prevents NMDAR GluN1 subunit phosphorylation76 and that serotonin depletion increases nociception-evoked trigeminal NMDAR phosphorylation.77 Immunohistochemistry shows that 5-HT1ARs are localized in GluN1-containing neurons in the spinal cord.74 In our studies, 10 Hz electroacupuncture at GB30 inhibited CFA-upregulated p-GluN1.78 Thus electroacupuncture inhibits pain by promoting spinal 5-HT1AR activation to post-synaptically suppress GluN1 phosphorylation (fig. 3).
It is known that pretreatment of μ receptor antagonist blocks intrathecal serotonin or clonidine-produced inhibition of inflammation-caused hyperalgesia.68 Naloxone inhibits intrathecal 5-HT anti-nociception,79 and selective norepinephrine reuptake inhibitors significantly increase intensity and duration of morphine anti-nociceptive activity via both α2 adrenergic and opioid receptors.80 Isobolographic analysis revealed a synergistic interaction between an α2-adrenoceptor agonist and morphine.81 Taken together, these data show that spinal 5-HT, norepinephrine, and opioids work in concert in electroacupuncture action. However, the mechanisms of their interaction are not clear.
Clinically, serotonin and norepinephrine reuptake inhibitors and selective serotonin reuptake inhibitors are used to manage chronic pain conditions. Since electroacupuncture induces the release of spinal 5-HT and norepinephrine, electroacupuncture treatment might enhance the inhibitory effect of serotonin and norepinephrine reuptake inhibitors/selective serotonin reuptake inhibitors on pain, thus allowing pain control medication to be decreased. This is supported by a study showing that when patients were given acupuncture/electroacupuncture as an adjunct to paroxetine, an selective serotonin reuptake inhibitor, only 5.7–8.9% required a dosage increase, significantly fewer than did those given paroxetine alone (22.9%).82
1.2.3. Glutamate and its receptors
Glutamate and its receptors, categorized as NMDA, α-amino-3-hydroxy-5-methylisoxazole-4-propionic acid, kainate, and metabotropic groups, are abundant in the spinal dorsal horn and play important roles in transmission of noxious messages.83,84 In a CFA-induced pain model, studies show that electroacupuncture at 2, 15, or 120 HZ not only significantly alleviates CFA-induced mechanical hyperalgesia but also significantly decreases CFA-upregulated GluN1, GluN2A, and GluA1 in the spinal dorsal horn.85 In dorsal root ganglia (DRG), alternation of 4 and 16 Hz electroacupuncture at GB30 and GB34 significantly inhibited CFA-induced GluN1 upregulation.86 In our studies, 10 Hz electroacupuncture at GB30 significantly decreased CFA-enhanced GluN1 phosphorylation.78 Collectively, these studies demonstrate that electroacupuncture inhibits transmission of noxious messages at the spinal level by dampening glutamate receptor activities.
Electroacupuncture might work through spinal norepinephrine, 5-HT, and opioids to decrease NMDAR activation and thus to inhibit pain. As mentioned in section 1.2.2, electroacupuncture might inhibit GluN1 phosphorylation by inducing spinal release of 5-HT and norepinephrine. It has been reported that microiontophoretic application of a selective μ opioid receptor agonist, [D-Ala2, N-Me-Phe4, Gly-ol5]enkephalin, reduced the NMDA-evoked responses of 100% of nociceptive specific, 93% of wide dynamic range, and 86% of low threshold neurons in the superficial and deeper dorsal horn of the medulla.87 These studies show that electroacupuncture-induced endogenous opioids inhibit NMDA-mediated excitation in the spinal cord, thus alleviating pain. Hence electroacupuncture inhibits NMDAR by activating at least three pathways, norepinephrine, 5-HT, and opioid, thus resulting in the alleviation of pain (fig. 3).
As in the electroacupuncture plus morphine study,37 electroacupuncture with low-dosage dizocilpine maleate (MK-801; a noncompetitive NMDAR antagonist) suppressed inflammatory pain better than did either modality alone.88,89 The data from these studies once again provide a rationale for pain management and control that combine Western medicine and acupuncture, and they corroborate previously reported data: for example, etoricoxib plus acupuncture has been shown to be more effective than etoricoxib with sham acupuncture or etoricoxib alone for the treatment of knee osteoarthritis pain.90
1.2.4. Glial cells/cytokines
Electroacupuncture inhibits spinal glial cell activation and decreases cytokines to alleviate pain. Alternating 2 and 100 Hz at GB30 and GB34 raised PWL and markedly inhibited intra-articular CFA-induced astrocyte and microglia activation and IL-1β, IL-6, and TNF-α upregulation in the spinal cord.91–93 It is well known that spinal pro-inflammatory cytokines facilitate pain. For example, IL-1β enhances GluN1 phosphorylation to facilitate pain94–96 and TNF-α increases NMDA currents in spinal lamina II neurons.97 Thus electroacupuncture might inhibit glial cell activation to decrease production of pro-inflammatory cytokines, leading to the inhibition of pain. Moreover, two Hz electroacupuncture at ST36 and Sanyinjiao (SP6) once a day for three days significantly increased PWL and inhibited CFA-induced upregulation of glial fibrillary acidic protein, an astrocyte marker.98 It also reversed CFA-caused downregulation of glutamate-aspartate transporter and glutamate transporter-1 in astrocytes. Concomitantly, proteasome inhibitor MG132 treatment significantly increased PWL and reversed CFA-induced downregulation of glutamate-aspartate transporter and glutamate transporter-1. Since electroacupuncture decreased CFA-enhanced spinal proteasome activity, it is concluded that electroacupuncture inhibition of proteasome restores glutamate transporters, leading to pain inhibition.98
Opioid and N/OFQ peptide receptor activation might mediate electroacupuncture inhibition of cytokine synthesis in the spinal cord (fig. 3). Substance P (SP), a neuropeptide key to the transmission of noxious inputs, activates glial cells during pain.99 Its release is blocked by μ and δ opioid receptors,100 which electroacupuncture significantly activates.37 Electroacupuncture also inhibits tooth pulp stimulation-evoked increase in the release of immunoreactive SP.101 These data indicate that electroacupuncture-induced endogenous spinal opioids decrease the release of neurotransmitters such as SP and inhibit cytokine synthesis in glial cells.
It has been reported that intrathecal administration of N/OFQ significantly downregulates CFA-exaggerated IL-1β, IL-6, and TNF-α mRNA in the spinal cord in the inflammatory pain rat model, actions which were abolished when combined with the opiate receptor-like-1 receptor-specific antagonist [Nphe(1)]N/OFQ(1–13)NH2.102 ORL1 receptors are expressed on astrocytes in the rat spinal cord. In vitro studies with astrocyte cultures also show that N/OFQ inhibits cytokine gene expression through the ORL1 receptor.102 Since electroacupuncture induces release of spinal N/OFQ,47,48 it is plausible that electroacupuncture-induced spinal N/OFQ suppresses spinal cytokine synthesis (fig. 3).
1.2.5. Signal molecules
The influence of acupuncture on signal molecules and signal pathways has been investigated. In a carrageenan-induced inflammatory pain model, 2 Hz electroacupuncture at ST36 and SP6 significantly decreased mechanical and thermal hypersensitivity and simultaneously inhibited carrageenan-induced phosphorylation of phosphatidylinositol-3-kinase and Akt.103 It has been reported that SP enhances Akt phosphorylation in neurokinin 1 receptor-positive neurons in laminae I–III and that phosphorylated Akt initiates and maintains inflammatory hyperalgesia.104 It is well known that activation of spinal μ and δ opioid receptors potently inhibits the SP release induced by peripheral noxious stimuli.100 These studies show that electroacupuncture-induced endogenous opioids inhibit SP release and Akt phosphorylation to alleviate pain (fig. 3). Moreover, in a study by Liu et al.,105 10-Hz electroacupuncture-produced inhibition of inflammatory thermal hyperalgesia was prevented when spinal Gi/o-protein function was destroyed by intrathecal pretreatment with pertussis toxin. This indicates that electroacupuncture-produced anti-hyperalgesia is mediated by pertussis toxin-sensitive Gi/o proteins and the relevant signaling pathways.
Alternating 2 Hz and 100 Hz electroacupuncture bilaterally at ST36 and Kunlun (BL60) inhibited and decreased CFA-induced pain, p38 mitogen-activated protein kinase (MAPK), and activating transcription factor-2 (ATF-2) positive cells in the dorsal spinal cord.106,107 Activated p38 MAPK is known to play an important role during nociception and is translocated to the nucleus to phosphorylate transcriptional factors such as ATF-2.108 Neurokinin-1 receptors and proinflammatory cytokines such as IL-1β and TNF-α contribute to p38 MAPK activation in the spinal cord.109,108 Conclusively, electroacupuncture-induced inhibition of proinflammatory cytokines as detailed in section 1.2.4 and electroacupuncture inhibition of neurokinin-1 receptors110 inhibit p38 MAPK/ATF-2 to suppress pain (fig. 3).
Two Hz electroacupuncture at ST36 inhibited intraplantar carrageenan- and CFA-induced upregulation of acid-sensing ion channel 3 in DRG.111 At present, it is not known how electroacupuncture modulates this channel and the relevant signal cascades.
1.2.6. Other substances
Although studies in uninjured animals have demonstrated the involvement of muscarinic, γ-aminobutyric acid (GABA), and dopamine receptors in electroacupuncture analgesia,60,64,112 few studies have used persistent pain animal models. In an intra-knee carrageenan rat model, systemic administration of the dopamine D2 receptor antagonist metoclopropamide blocked electroacupuncture analgesia.65 This is consistent with dopamine D2 agonist inhibition of pain.113 Further, dopamine D2 agonists enhance the anti-nociception of 5-HT and norepinephrine reuptake inhibitors.113 Electroacupuncture-induced dopamine, 5-HT, and norepinephrine might alleviate pain synergistically. In collagen-induced arthritis, systemic administration of atropine, a muscarinic cholinergic receptor antagonist, also blocked electroacupuncture analgesia.66 Since spinal muscarinic receptors are involved in morphine- and clonidine-produced antinociceptive effects,114,115 electroacupuncture-induced acetylcholine, opioids, and norepinephrine also might alleviate pain synergistically.
Spinal mechanisms of electroacupuncture on inflammatory pain have been extensively investigated with behavioral, molecular, and pharmacological approaches. Electroacupuncture might induce several neurotransmitters, including opioids, 5-HT, norepinephrine, dopamine, and acetylcholine, which work interactively to inhibit pain. It is unclear how electroacupuncture induces these neurotransmitters.
1.3. Supraspinal mechanisms
1.3.1. Electroacupuncture inhibition of the sensory dimension of pain
Zhao’s 2008 review60 summarizes a number of studies in uninjured animals. Collectively, these show that many nuclei, including the NRM, PAG, locus coeruleus, arcuate, preoptic area, nucleus submedius, habenular, accumbens, caudate, septal area, and amygdala, are involved in acupuncture analgesia and that opioid peptides and their receptors in the arcuate-PAG-NRM-spinal dorsal horn pathway are pivotal in this effect.60,116 Recently, brain mechanisms of electroacupuncture analgesia have been investigated in an inflammatory pain model. Selective μ but not κ receptor antagonists infused into the rostral ventromedial medulla (RVM) blocked 10 and 100 Hz electroacupuncture-produced antihyperalgesia assessed with PWL.117 Double immunofluorescence staining demonstrated that μ receptor-containing neurons are GABAnergic and that GABAa receptor-containing neurons are serotonergic in the RVM.117 Hence, electroacupuncture induces release of endogenous endomorphins. These activate μ opioid receptors in GABAnergic neurons that suppress GABA release. Without GABA inhibition, RVM-spinal cord projecting serotonergic neurons can be activated to inhibit inflammatory pain.59
In a carrageenan model of inflammatory pain, 4 and 60 Hz electroacupuncture alternated at ST36 and BL60 significantly inhibited thermal hyperalgesia and carrageenan-enhanced IL-1 receptor type I mRNA expression in the PAG compared to sham control.118 As μ opioids and chemokine receptors interact,119 electroacupuncture-induced opioids might act on the latter to inhibit IL-1 receptors. Additionally, it has been reported that melanocortin 4 receptor blockage in the PAG significantly attenuated mechanical allodynia and thermal hyperalgesia and inhibited glial activation and IL-1β synthesis.120 It is possible that electroacupuncture inhibits melanocortin 4 receptors to attenuate IL-1β and IL-1 receptor activity in the PAG, thus alleviating pain.
Compared to the spinal level, brain involvement in electroacupuncture analgesia during persistent pain has been less investigated. As pain sensation is dependent on brain function and subject to brain modulation, electroacupuncture modulation of brain might play an important role in pain inhibition. For example, deep brain stimulation of the ACC in humans significantly inhibited pain.121 Brain mechanisms of electroacupuncture analgesia warrant further investigation.
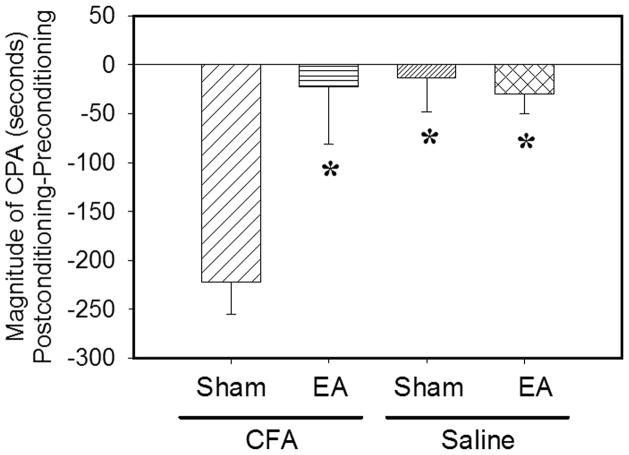
1.3.2. Electroacupuncture inhibition of the affective dimension of pain
Pain has two dimensions, the sensory/discriminative and the affective. Studies in animal pain models show that electroacupuncture inhibits the sensory dimension of pain by producing an antinociceptive effect; electroacupuncture action on the affective component has only recently been studied. A CFA inflammatory pain rat model was combined with a conditioned place avoidance test to determine whether electroacupuncture inhibits pain-induced affective response.122 During preconditioning, rats spent similar amounts of time in two compartments, indicating no aversion to either. After conditioning, rats that received sham electroacupuncture spent less time in a pain-paired compartment, demonstrating place aversion to that compartment. By contrast, electroacupuncture-treated rats showed no aversion to the pain-paired compartment, demonstrating that electroacupuncture inhibited the CFA-produced affective response.122 Saline-injected rats showed neither preference nor aversion to electroacupuncture- or sham electroacupuncture-paired chambers; this shows that the electroacupuncture treatment did not produce reward or aversion (fig. 4). Intrarostral ACC (rACC) pretreatment with a μ but not a κ opioid receptor antagonist blocked electroacupuncture inhibition of pain-related affective response.122 A microinjection of morphine into the ACC inhibited affective response but did not change the sensory pain threshold,123 and an intrathecal μ opioid receptor antagonist blocked electroacupuncture-produced increase of PWL but not electroacupuncture inhibition of affective response.122 Together, these studies show that electroacupuncture induces a release of endorphins to block affective response and that this effect is not a consequence of sensory pain inhibition. Interestingly, animal studies demonstrate that several drugs, including morphine, oxycodone, tramadol, Ibuprofen, and pregabalin, show a clear dissociation between anti-aversive and anti-nociceptive potency.124 Clinical studies found that morphine more potently attenuates the affective component than the sensory component of pain.125 Thus electroacupuncture also might differ in its actions on the sensory and affective dimensions of pain.
Figure 4.
Electroacupuncture inhibited the affective component of pain. Conditioned place avoidance scores, used to indicate affective response, were determined by subtracting time spent in the pain-paired compartment during preconditioning from time spent in that compartment during the post-conditioning test: the less post-conditioning time spent in the compartment, the greater the affective response. * P < 0.05 compared to sham control in CFA-injected rats. Reprinted with permission from Elsevier, Eur J Pain 16(2), 2012. EA = electroacupuncture, CFA = complete Fruend’s adjuvant.
In another study, electroacupuncture attenuated formalin-induced conditioned place avoidance.126 Further, selectively blocking of the GluN2A or GluN2B subunit of the rACC abolished intra-plantar formalin injection-induced affective pain but not the nociceptive behaviors.127 It is known that the μ opioid receptor agonist [D-Ala2, N-Me-Phe4, Gly-ol5]enkephalin significantly decreases both NMDA and non-NMDA excitatory postsynaptic potential amplitudes in nucleus accumbens neurons; this action is reversed by a μ opioid receptor antagonist.128 Immunohistochemical data showed that NMDAR and μ receptors are colocated in rACC neurons (fig. 5). The hypothesis is that electroacupuncture-produced μ opioid receptor activation modulates NMDAR activities to attenuate pain-associated affective response (fig. 3).
Figure 5.
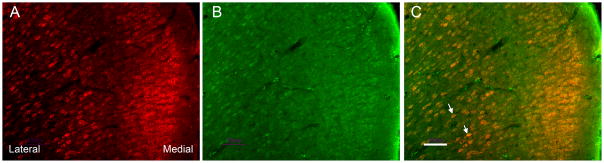
Microphotographs showing distribution and co-localization of GluN1 and μ opioid receptors in rACC neurons. A, B: Sections were double-labeled with guinea pig polyclonal antibody against μ opioid receptors (A, red) and goat polyclonal antibody against GluN1 (B, green). C: Merged A and B photographs showing co-localization of μ opioid receptors and GluN1 in the rACC. Arrows point to double-labeled neurons (yellow). Scale bars=50 μm. rACC = rostral anterior cingulate cortex.
In summary, electroacupuncture inhibits both sensory and affective dimensions of pain. Electroacupuncture-induced endogenous opioids in the rACC may suppress NMDAR functions, which play an important role in electroacupuncture inhibition of the affective dimension of pain. It is unclear whether other neurotransmitters, such as norepinephrine which is located in the ACC, are involved in electroacupuncture inhibition of the affective component of pain.
2. Neuropathic pain models
Although mechanisms of acupuncture analgesia have been investigated at each level of the pain pathway in inflammatory pain models, acupuncture analgesia has been studied mainly at the spinal level in neuropathic pain models129 and shows involvement of opioids, serotonin, norepinephrine, amino acids, and glia cell/cytokines.
2.1. Opioids
Spinal opioids are involved in electroacupuncture inhibition of neuropathic pain. Systemic administration of naloxone blocked 2 Hz electroacupuncture inhibition of L5 and L6 spinal nerve ligation (SNL)- and caudal trunk nerve injury-induced neuropathic pain.130,131 Manual acupuncture, applied at ST36 and SP6 in an SNL-induced neuropathic pain rat model, significantly reduced SNL-induced hypersensitivity; this effect was blocked by systemic nolaxone.132 Furthermore, administration of cumulative doses (5, 10, 20 nmol) of the μ or δ opioid receptor antagonists β-funaltrexamine hydrochloride and naltrindole blocked 2-Hz-produced electroacupuncture anti-mechanical allodynia, corroborating μ and δ opioid receptor involvement in electroacupuncture action. Cumulative doses of the κ opioid receptor antagonist nor-binaltorphimine at 3, 6, and 12 nmol did not significantly influenced electroacupuncture inhibition of pain,133 possibly due to the low dosages administered. Moreover, chemotherapy-induced peripheral neuropathy is the most common and serious adverse effect of chemotherapeutic agents.134 A paclitaxel-evoked peripheral neuropathy model has been developed using intraperitoneal 2 mg/kg/ml of paclitaxel on four alternate days (0, 2, 4, and 6).135 Beginning on day 13, the response frequency to von Frey filaments (bending force: 4–15 g) was significantly increased in paclitaxel-injected rats compared to that in those injected with vehicle. Ten Hz electroacupuncture at GB30 significantly decreased response frequency at 4–15 g compared to sham electroacupuncture;136 10 Hz electroacupuncture plus a μ, δ, or κ opioid receptor antagonist did not significantly decrease mechanical hypersensitivity compared to sham electroacupuncture plus vehicle; this shows that all three antagonists blocked electroacupuncture action in this model. Clearly, μ, δ, and κ receptors are involved in 10 Hz electroacupuncture inhibition of chemotherapy-induced neuropathic pain; this is different from the opioid involvement in electroacupuncture inhibition of peripheral tissue injury-caused inflammatory pain, in which only μ and δ receptors participate. (See table 2). It has been reported that an interaction exists between μ and κ receptors: spinal μ receptor activation might promote κ receptor activation-produced antinociception.137 Thus it is hypothesized μ and κ receptor interaction is modulated differently in neuropathic and inflammatory pain conditions. This would account for the differential involvement of opioid receptors in electroacupuncture action.
Low frequency electroacupuncture inhibits neuropathic pain more effectively than does high frequency electroacupuncture. Ten Hz electroacupuncture at GB30 significantly decreased mechanical response frequency at 4–15 g compared to sham electroacupuncture;136 100 Hz electroacupuncture only decreased response frequency at 15 g in a paclitaxel-evoked peripheral neuropathy model. This indicates that 10 Hz electroacupuncture inhibits mechanical allodynia/hyperalgesia more potently than 100 Hz does.136 Similarly, 2 Hz electroacupuncture, in a caudal trunk nerve injury-induced neuropathic pain model, induced a robust and longer lasting inhibitory effect on mechanical allodynia assessed with a von Frey filament (bending force: 2 g) than did 100 Hz.133 Consistent with these results, 2 Hz decreased mechanical and thermal hypersensitivity more powerfully in an L5/L6 nerve ligation-induced neuropathic pain model than did 100 Hz.138 A single treatment at 2 Hz electroacupuncture inhibited thermal hypersensitivity for 48 h; a single treatment at 100 Hz electroacupuncture was only effective for 8 h.138 In an electrophysiological study,139 2 Hz electroacupuncture induced long-term depression of C-fiber-evoked potentials in rats with SNL, while 100 Hz electroacupuncture induced long-term potential in SNL rats. Synaptic long-term depression in the spinal dorsal horn in SNL rats might be involved in the long-lasting analgesia produced by 2 HZ electroacupuncture.
2.2. Serotonin and norepinephrine
Spinal serotonin and norepinephrine participate in electroacupuncture inhibition of neuropathic pain. For example, 2 Hz electroacupuncture inhibited cold allodynia in rats with right caudal trunk resection between the S1 and S2 spinal nerves innervating the tail.140 Intrathecal injection of the 5-HT1AR antagonist NAN-190 and the 5-HT3R antagonist MDL-72222 significantly blocked this effect; the 5-HT2AR antagonist ketanserin did not. Intrathecal injection of the α2-adrenoceptor antagonist yohimbine also significantly blocked electroacupuncture action, but the α1-adrenoceptor antagonist prazosin did not. These data show that spinal α2-adrenoceptors, 5-HT1ARs, and 5-HT3Rs are involved in electroacupuncture inhibition of cold allodynia in neuropathic pain. Although α2-adrenoceptors and 5-HT1ARs are involved in electroacupuncture inhibition of both inflammatory and neuropathic pain, 5-HT3Rs play a role in electroacupuncture inhibition of neuropathic but not inflammatory pain. Consistent with that activity, 5-HT3Rs are involved in spinal cord stimulation-induced analgesia during neuropathic pain.141 It is possible that nerve injury changes spinal 5-HT3R activities leading to the receptors’ participation in neuropathic pain modulation.
It has been reported that 2 Hz electroacupuncture inhibits nerve injury-induced GluN1 expression in the spinal cord131 and that 5-HT1ARs are located on GluN1-containing spinal cord neurons.68 These data lead us to hypothesize that electroacupuncture activates 5-HT1ARs to inhibit NMDAR activities, thus attenuating neuropathic pain.
Although inflammatory and neuropathic pain differ, certain central spinal and brain mechanisms such as activation of NMDA receptors are common to both.142 Interestingly, electroacupuncture attenuates both inflammatory and neuropathic pain by activating spinal α2-adrenoceptors and 5-HT1ARs and inhibiting GluN1 (fig. 3).
2.3. Amino acids
Both excitatory amino acids and inhibitory amino acids play roles in electroacupuncture attenuation of neuropathic pain. In a study with a chronic constriction injury model, 2 Hz electroacupuncture significantly elevated thermal and mechanical threshold, decreased concentration of spinal glutamate, aspartate, and glutamine, and increased the contents of glycine, GABA, and taurine in the spinal cord.143 Since this study did not employ a sham electroacupuncture control, those data need to be confirmed. Further, microdialysis was used to collect the dialysate from the spinal cord in a spared nerve injury rat model. Electroacupuncture significantly decreased dialysate glutamate compared to sham electroacupuncture.144 Moreover, intrathecal administration of the GABA(A) or GABA(B) receptor antagonists gabazine and saclofen blocked electroacupuncture inhibition of cold allodynia in the rats with resected caudal trunk nerves.145 Collectively, these studies demonstrate that electroacupuncture reduces the release of excitatory amino acids and promotes the release of inhibitory amino acid neurotransmitters to stop pain. In regard to excitatory amino acids, morphine decreased the formalin-enhanced release of glutamate in the spinal dorsal horn,146 presynaptic 5-HT1BRs decreased glutamate release from primary afferent terminals onto medullary dorsal horn neurons,147 and α2a-adrenoceptor activation diminished glutamate release from the spinal cord in previous studies.69 Based on those studies, it is proposed that endogenous electroacupuncture-induced opioids, 5-HT, and norepinephrine suppress excitatory amino acid release (fig. 3). Regarding the inhibitory amino acid GABA, a study showed that 5-HT1ARs are expressed on GABAergic neurons.148 It seems that electroacupuncture-induced 5-HT promotes the inhibitory effect of GABA to inhibit pain. Moreover, activation of δ opioid receptors reduces GABA uptake;149 thus electroacupuncture-induced endogenous opioids might increase GABA in extracellular space, enhancing GABA function and leading to pain inhibition (fig. 3). Additionally, intrathecal administration of the GABA receptor A or B agonists muscimol and baclofen potentiated the antinociceptive effects of morphine.150 Thus it is plausible that endogenous opioids and GABA interact during electroacupuncture treatment to alleviate pain.
2.4. Glial cells/cytokines
Glial cell and cytokines participate in electroacupuncture inhibition of neuropathic pain. For instance, two Hz electroacupuncture at ST36 significantly increased mechanical and thermal thresholds in rats with superior caudal trunk transection; it significantly inhibited nerve-damage-induced upregulation of glial fibrillary acidic protein and OX-42, matrix metallopeptidase-9 and matrix metallopeptidase-2, TNF-α, IL-6, and IL-1β in the spinal cord.151 In a spinal cord injury rat model, manual acupuncture at GB34 and Shuigou (DU26) significantly relieved mechanical allodynia and thermal hyperalgesia.152 Acupuncture also inhibited microglia activation, p38 MAPK and extracellular signal-regulated kinase phosphorylation, and superoxide anion production in microglia; it decreased IL-1β, IL-6, TNF-α, inducible nitric oxide synthases, COX-2, and PGE2 levels in the lumbar4–5 spinal cord.152 In rats with tightly ligated and transected tibial and sural nerves, 1 Hz electroacupuncture at ST36 and Yinlingquan (SP9) significantly decreased nerve injury-enhanced, immune response expression of IL-1β, IL-6, and TNF-α in peripheral nerves.153 Electroacupuncture also inhibited spinal Cox-2 in the SNL model.154 These chemicals positively promote transmission of noxious inputs at the spinal level; their inhibition might contribute to electroacupuncture analgesia. As stated in 1.2.4, opioid and N/OFQ peptide receptor activation might mediate electroacupuncture inhibition of cytokine synthesis in the spinal cord. In addition, p38 MAPK and extracellular signal-regulated kinase phosphorylation mediate the development of tolerance to morphine-induced analgesia,155 making electroacupuncture inhibition of this phosphorylation clinically relevant for the purpose of mitigating or delaying the development of morphine tolerance.
2.5. Other bioactive molecules
Muscarinic receptors and glial cell line-derived neurotrophic factor (GDNF) are involved in electroacupuncture action. One study demonstrates that spinal muscarinic M(1) subtype receptors mediate electroacupuncture-induced antiallodynia in neuropathic rats.156 This is consistent with a report that M1 receptor activation induced analgesia in a neuropathic pain model.157 Electroacupuncture significantly enhanced expression of somatostatin, GDNF, and the GDNF family receptor GFRα-1 (the high-affinity receptor of GDNF) in DRG and the spinal dorsal horn in rats with neuropathic pain.158,159 That pretreatment with antisense oligodeoxynucleotide specifically against GFRα-1 attenuates electroacupuncture analgesia indicates that electroacupuncture enhancement of GFRα-1 contributes to analgesia.160 This is supported by the fact that overexpression of GDNF in the uninjured DRG exerts analgesic effects on neuropathic pain.161 Interestingly, other studies showed that 5-HT induces GDNF mRNA expression in rat C6 glioma cells162 and that GDNF receptor activation significantly suppresses transient receptor potential cation channel subfamily A, number 1 channel activities that facilitate the sensation of pain.163 We conclude that electroacupuncture-induced enhancement of serotonin activities increases GDNF synthesis, then decreases transient receptor potential cation channel subfamily A, number 1 channel activities in the spinal cord to suppress pain.
Moreover, electroacupuncture has been shown to inhibit P2×3 to attenuate neuropathic pain.164 Electroacupuncture at ST36 induces nitric oxide in the gracile nucleus to attenuate pain in Zucker diabetic fatty rats.165 In contrast, another study showed that electroacupuncture at ST36 and SP9 inhibits nitric oxide synthase expression in the spinal cord of neuropathic rats.166 Involvement of nitric oxide in electroacupuncture analgesia needs to be confirmed.
Overall, electroacupuncture induces numerous bioactive chemicals that have inhibited neuropathic pain in several rat models (fig. 1). Whether and how it modulates supraspinal and peripheral nerve activities, which might be responsible for electroacupuncture inhibition of neuropathic pain, have not been investigated as yet.
3. Cancer pain models
Electroacupuncture has alleviated bone cancer pain in animal models. Studies in a prostate cancer pain rat model clearly show that 10 Hz electroacupuncture for 30 min a day at the equivalent of human acupoint GB 30 between days 14 and 18 after a cancer-cell injection significantly attenuated both thermal and mechanical hyperalgesia.167,168 Moreover, electroacupuncture treatment inhibited upregulation of preprodynorphin mRNA, dynorphin, and IL-1β and its mRNA compared to sham control. Intrathecal antiserum against dynorphin A (1–17) and an IL-1 receptor antagonist significantly suppressed cancer-induced hyperalgesia. These studies show that electroacupuncture inhibition of dynorphin and IL-1β contribute to electroacupuncture analgesia in cancer pain models.167,168
In another model, S-180 sarcoma cells were injected around the left sciatic nerve of BALB/c mice to cause mechanical allodynia.169 Nine days of 2 Hz electroacupuncture at ST36 once a day for 30 min significantly inhibited thermal hyperalgesia and spontaneous pain. Electroacupuncture also inhibited SP expression in the spinal dorsal horn and increased the concentration of β-endorphin in the blood and brains of mice.169 Those data warrant further confirmation since the study did not include a sham control.
In a third model, Walker 256 carcinoma cells were subcutaneously injected into the plantar region of the hind paw to cause pain,170 and 2 Hz electroacupuncture, administered bilaterally at ST36, significantly decreased the induced mechanical and thermal hypersensitivity and spontaneous pain. It also markedly suppressed cancer-driven upregulation of transient receptor potential cation channel subfamily V member 1 expression in corresponding L3–5 DRG. Since transient receptor potential cation channel subfamily V member 1 facilitates cancer pain, electroacupuncture inhibition of this protein might diminish pain.171 Taken together, these findings indicate that electroacupuncture treatment significantly inhibits cancer pain. Since cancer-related pain is debilitating and has not been well controlled, electroacupuncture might be a useful adjuvant therapy in patients with such pain.
4. Visceral pain models
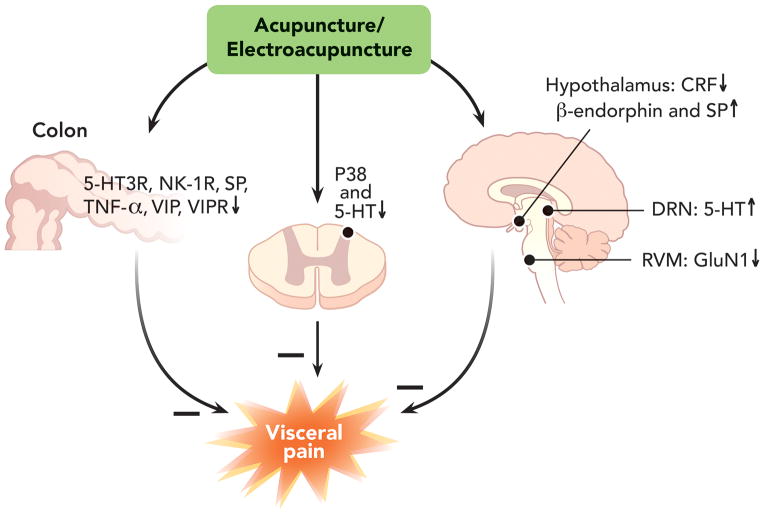
Increasing evidence shows that acupuncture effectively alleviates visceral pain in animal models through peripheral, spinal, and supraspinal mechanisms (fig. 6).
Figure 6.
Mechanisms of electroacupuncture inhibition of visceral pain. Symbols + and − respectively represent enhancement and inhibition. CRF = corticotrophin-releasing factor; DRN = dorsal raphe nucleus; NK-1 = neurokinin 1; RVM = rostral ventromedial medulla; SP = substance P; TNF-α = tumor necrosis factor-α; VIP = vasoactive intestinal polypeptides; VIPR = VIP receptor; 5-HT = 5-hydroxytryptamine
4.1. Peripheral mechanisms
Numerous peripheral chemicals including neurotransmitters, neuropeptides, and cytokines are involved in electroacupuncture inhibition of visceral pain. Alternation of 5 and100 Hz electroacupuncture bilaterally at ST36 significantly decreased visceral pain and colon 5-HT3R levels in an irritable bowel syndrome (IBS) model induced by intrarectal administration of acetic acid.172 Alternating 2 and 50 Hz electroacupuncture at ST25 and ST37 (Shangjuxu) significantly decreased colorectal distension (CRD)-induced abdominal withdrawal reflex (AWR), the number of mucosal mast cells, SP, neurokinin 1 receptors, vasoactive intestinal polypeptides (VIP), and VIP receptor expression in the colon in an IBS rat model induced by mechanical colorectal irritation.173,174 Electroacupuncture at ST36 significantly decreased colon damage and serum and colon TNF-α mRNA expression in rats with ulcerative colitis induced by intracolon ethanol and 2,4,6-trinitrobenzenesulfonic acid.175 These studies demonstrate that electroacupuncture relieves visceral pain by modulating mast cells, SP, VIP, 5-HT3Rs, and TNF-α function. In keeping with the electroacupuncture studies, a study demonstrated that blockage of 5-HT3Rs significantly increases colonic distension perception threshold in IBS patients with diarrhea.176 Studies also show that SP, serotonin, and histamine, which can be released by mast cells, sensitize visceral afferents.177 Patients with recurrent abdominal pain showed significantly greater expression of VIP, neurokinin 1 receptors, and TNF-α mRNA compared to control.178,179 Thus it seems that electroacupuncture decreases numerous chemicals at peripheral sites to desensitize visceral afferents and alleviate visceral pain.
4.2. Spinal mechanisms
Opioids are involved in electroacupuncture inhibition of visceral pain. A study demonstrated that alternating 4 and 100 Hz electroacupuncture bilaterally at ST36 and ST37 significantly decreases CRD-induced AWR and the magnitude of electromyograms.180 In another study, alternating 2 and 100 Hz electroacupuncture bilaterally at ST36 significantly attenuated visceral motor response to CRD and the hyperexcitability of colon DRG neurons in rats instilled with intracolonic acetic acid;181 this attenuation was prevented by intraperitoneal naloxone pretreatment, displaying the involvement of opioids without differentiation between peripheral, spinal, and supraspinal levels of opioid action. Pretreatment with 20 Hz electroacupuncture at Jiaji (EX-B2) significantly inhibited intracolonic formalin-caused visceral pain behavior, including abdominal licking, backward extension, contraction of the flanks, and whole body contraction.182 It suppressed p38 phosphorylation and Fos expression in the spinal cord and colon, indicating that electroacupuncture modulates spinal neuronal activities. It also increased serum β-endorphin, which might act on peripheral and central site to suppress pain. Those changes were not found in healthy electroacupuncture-treated rats,182 demonstrating that electroacupuncture modulates the nervous system differently in healthy animals and those with pain conditions. Indeed, it has been shown that patients with Bell’s palsy have distinct brain responses to acupuncture treatment compared to healthy volunteers.183 Further, patients at different stages of Bell’s palsy varied in brain responses to acupuncture. Taken together, electroacupuncture alleviates visceral pain by modulating spinal and DRG activities through endogenous opioids. Phosphorylated p38 in microglia is known to be involved in inflammatory, neuropathic, and visceral pain.108,184 As discussed in 1.2.4, endogenous electroacupuncture-induced opioids reduce the release of neurotransmitters such as SP and subsequently inhibit glial cell activation, which might decrease p38 phosphorylation and inhibit visceral pain.
4.3. Supraspinal mechanisms
Electroacupuncture might also attenuate visceral pain through supraspinal mechanisms. An early study showed that vasopressinergic neurons in the hypothalamic paraventricular nucleus participate in the electroacupuncture inhibition of visceral pain induced by an intraperitoneal injection of antimonium potassium tartrate.185 In a gastric distension-induced pain model, 10 or 100 Hz electroacupuncture at ST36 significantly mitigated visceral pain assessed with AWR and increased hypothalamus β-endorphin and SP.186 In an IBS rat model produced by mechanical colorectal irritation, alternating 2 and 50 Hz electroacupuncture at ST37 significantly inhibited visceral pain and hypothalamic CRF synthesis.187 In a neonatal maternal separation stress-induced IBS rat model, 10 Hz electroacupuncture at ST36 significantly suppressed visceral hyperalgesia and inhibited Fos expression in dorsal raphe nuclei of the brainstem, the superficial dorsal horn of the spinal cord, and colonic epithelium as well as 5-HT expression in dorsal raphe nuclei and the spinal cord.188
In an electrophysiological study in anesthetized healthy rats, response to CRD by convergent somatic and visceral neurons in the thalamic ventrobasal nucleus was inhibited by electrical stimulation at either the skin receptive field or acupoint ST36.189 It is interesting that skin receptive fields of thalamic neurons which respond to visceral nociception lie more or less along traditional Chinese medicine’s Stomach Channel and that simulating the receptive field produces more robust inhibition than does stimulating ST36, an important point on that channel. However, it has not been determined whether the same phenomenon can be found for such behavioral tests as AWR. Moreover, alternating 5 and 100 Hz electroacupuncture at ST36 and ST37 decreased AWR and IBS-exaggerated GluN1 and Fos expression in the RVM.190 Since an intra-RVM NMDAR antagonist inhibited visceral pain,191 electroacupuncture might relieve visceral pain by inhibiting NMDAR activation in the RVM.
Collectively, several chemicals, including β-endorphin and 5-HT, are involved in electroacupuncture inhibition of visceral pain (fig. 6), but the underlying mechanisms are not yet understood. Also, although brain structures such as the thalamic ventrobasal nucleus, the hypothalamus, paraventricular nucleus, dorsal raphe nuclei, and the RVM are involved in electroacupuncture action, how those structures work together to modulate visceral pain during electroacupuncture treatment warrants further investigation.
5. Clinical implications
The preclinical studies summarized in this review provide solid evidence that electroacupuncture treatment, compared to sham electroacupuncture, results in significant changes in bioactive chemicals--including opioids, N/OFQ, serotonin, norepinephrine, glutamate receptors and transporters, cytokines, and signal molecules--in peripheral injury sites, the spinal cord, and supraspinal structures. Findings from animal models demonstrate that electroacupuncture and sham control work through different mechanisms, which implies that patients with persistent pain might respond differently to electroacupuncture and sham controls. Indeed, electroacupuncture led to significantly higher activation at the right insula, pulvinar, and medial nucleus of the thalamus compared to sham control in patients with IBS.192
In animal models, electroacupuncture significantly inhibits pain in comparison to sham control. Systematic reviews have shown that in clinical studies, most of which used manual acupuncture, acupuncture performed either significantly better193 or not significantly better than sham although both improved pain score.194 Interestingly, in some clinical studies, electroacupuncture produced higher pain threshold elevation195 and significantly better subjective evaluations of treatment effects196 than did manual acupuncture. Further, early clinical trials with electrical stimulation of acupoints in patients with osteoarthritis showed significant pain inhibition compared to sham control.2,197,198 This is confirmed by a more recent study employing electrical stimulation of acupoints during treatment.90 In contrast, manual acupuncture produced no significant effects compared to sham control.199,200 Based on that evidence, we hypothesize that electroacupuncture is superior to manual acupuncture, but further investigation is warranted to confirm this premise.
The studies using electroacupuncture plus pain medication provide significant and useful information for maximizing the effect of integrative medicine in clinical settings.90 Such combination treatments might provide effective strategies for pain management, both by enhancing treatment effectiveness and by lowering pain medication dosages thus decreasing the risk of debilitating adverse effects. For example, in an animal study, electroacupuncture combined with a subeffective dose of morphine enhanced inflammatory pain inhibition compared to morphine.37 In a clinical study,201 electroacupuncture treatment prior to surgery significantly decreased the total amount of morphine required during the first 24 h postoperation and significantly reduced the incidence of nausea and dizziness during the same period compared to sham electroacupuncture. Similarly, electroacupuncture enhanced the effects of low-dosage celecoxib on monoarthritic pain202 and low-dosage indomethacin on CFA-induced inflammatory pain,203 as well as intrathecal antisense oligodeoxynucleotide to interleukin-1 receptor type I204 and GluA (α-amino-3-hydroxy-5-methylisoxazole-4-propionic acid)/GluK (Kainate) receptor antagonists33 on carrageenan-induced pain. These studies show that electroacupuncture treatment has the potential to allow the use of lower dosages of such medications in clinical settings, thus reducing side effects and improving patient quality of life.
These animal studies also show that electroacupuncture inhibition of pain is parameter dependent. Ten Hz electroacupuncture produces longer alleviation of inflammatory pain and more powerful inhibition of neuropathic pain than does 100 Hz electroacupuncture.34 Electroacupuncture at 10 Hz inhibits inflammation, while electroacupuncture at 100 Hz does not.36 This is useful information for designing appropriate clinical trials: we used low frequency electroacupuncture in our knee osteoarthritis clinical trial; the resulting effects were significantly better than those produced by sham control and lasted for 26 weeks.2 Thus, low frequency electroacupuncture could be useful in clinical settings to manage pain.
6. Summary
In summary, the studies show that electroacupuncture significantly alleviated inflammatory, neuropathic, cancer, and visceral pain in the corresponding animal models (fig. 1). Electroacupuncture intervention activates the nervous system differently in health than in pain, as shown by the fact that opioid receptors are differentially involved in electroacupuncture inhibition of pain in healthy animals and those with persistent pain (table 2), as well as by the brain responses to acupuncture displayed by patients with Bell’s palsy compared to those of healthy volunteers.183 Moreover, electroacupuncture parameters affect outcomes: 10 Hz electroacupuncture produces longer lasting alleviation of inflammatory pain than does 100 Hz, and 2–10 Hz inhibit nerve injury-caused allodynia/hyperalgesia more potently than does electroacupuncture at 100 Hz.
Electroacupuncture mechanisms on inflammatory pain have been extensively studied. The modality inhibits both the sensory and the affective components of inflammatory pain, acting through peripheral, spinal, and supraspinal mechanisms with the involvement of a battery of bioactive molecules including opioids, N/OFQ, serotonin, norepinephrine, glutamate receptors and transporters, cytokines, and signal molecules (table 1). Of these, opioids play a central role in electroacupuncture inhibition of all kinds of pain. Opioids desensitize peripheral nociceptors, decrease pro-inflammatory cytokines in peripheral sites, decrease cytokines and SP in the spinal cord, and are involved in electroacupuncture inhibition of affective pain. Opioids also activate the descending inhibitory system, the main neurotransmitters of which are serotonin and norepinephrine. Electroacupuncture induces serotonin and norepinephrine that in turn decrease GluN1 phosphorylation to inhibit pain (fig. 3).
Electroacupuncture mechanisms on neuropathic pain have been studied mainly at the spinal level, less so at the supraspinal level and peripheral sites. Most bioactive chemicals involved in electroacupuncture inhibition of inflammatory pain are also implicated in electroacupuncture inhibition of neuropathic pain (table 1, fig. 3).
Only a few studies have investigated the mechanisms of electroacupuncture on cancer-related pain at the spinal level, but electroacupuncture has been shown to inhibit spinal SP, IL-1β, dynorphin, and transient receptor potential cation channel subfamily V member 1 to stop cancer-caused pain. Numerous papers report that electroacupuncture inhibits visceral pain through peripheral, spinal, and supraspinal mechanisms with involvement of SP, SP receptors, VIP, and VIP receptors in the colon, 5-HT and p38 in the spinal cord, hypothalamic β-endorphin, SP, CRF, neuropeptide Y, and 5-HT in the brainstem, and NMDAR in the RVM. How these structures and bioactive molecules work together remains elusive.
Although the studies reviewed provide solid evidence for electroacupuncture analgesia, the current research has some shortcomings. First, brain mechanisms underpinning electroacupuncture analgesia are less studied than are peripheral and spinal mechanisms. Although many nuclei have been found to be involved in electroacupuncture analgesia, it is not clear how they work together in electroacupuncture inhibition of persistent pain. For example, the involvement of ACC afferents and efferents in electroacupuncture inhibition of pain has not been clarified. Given that neuronal electrical activities play important roles in the functional connection of neuronal circuits, how electroacupuncture modulates neuronal activities during persistent pain warrants investigation; imaging and electrophysiological studies may be used to explore how electroacupuncture modulates neuronal circuit connections. Second, as summarized in table 1, although many bioactive chemicals in the spinal cord participate in electroacupuncture inhibition of inflammatory and neuropathic pain, it is unclear whether these chemicals play similar roles in the brain; the peripheral mechanisms of electroacupuncture inhibition of neuropathic pain and the mechanisms of electroacupuncture inhibition of cancer pain are not well studied. Third, female rats have been seldom used in electroacupuncture analgesia studies. Since there is strong evidence for gender differences in pain and treatment outcomes,205,206 female rats should be included in future acupuncture studies to determine whether males and females respond differently to acupuncture/electroacupuncture treatment. Clarification of acupuncture/electroacupuncture mechanisms will open a variety of opportunities to combine acupuncture/electroacupuncture with medications to manage and control pain, which makes it all the more important to continue such research.
Acknowledgments
We would like to thank Dr. Lyn Lowry, Ph.D. for her editorial support.
Funding resources:
This work was made possible by grant numbers P01AT002605 and R21AT005474 from the National Center for Complementary and Alternative Medicine at the National Institutes of Health, Bethesda, Maryland.
Footnotes
Conflicts of interest: The authors declare no competing interests.
This work is attributed to: Center for Integrative Medicine, School of Medicine, University of Maryland
References
- 1.Institute of medicine. (US) committee on advancing pain research, care, and education: Relieving pain in America: A blueprint for transforming prevention, care, education, and research. Washington DC: National Academies Press (US); 2011. [PubMed] [Google Scholar]
- 2.Berman BM, Lao L, Langenberg P, Wen Lin L, Gilpin AMK, Hochberg MC. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee. Ann Intern Med. 2004;141:901–10. doi: 10.7326/0003-4819-141-12-200412210-00006. [DOI] [PubMed] [Google Scholar]
- 3.Barnes PM, Barbara B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. National Health Statistics Reports. 2008;12:1–24. [PubMed] [Google Scholar]
- 4.Taguchi R, Taguchi T, Kitakoji H. Involvement of peripheral opioid receptors in electroacupuncture analgesia for carrageenan-induced hyperalgesia. Brain Res. 2010;1355:97–103. doi: 10.1016/j.brainres.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Sekido R, Ishimaru K, Sakita M. Differences of electroacupuncture-induced analgesic effect in normal and inflammatory conditions in rats. Am J Chin Med. 2003;31:955–65. doi: 10.1142/S0192415X03001491. [DOI] [PubMed] [Google Scholar]
- 6.Zhang GG, Yu C, Lee W, Lao L, Ren K, Berman BM. Involvement of peripheral opioid mechanisms in electroacupuncture analgesia. Explore (NY) 2005;1:365–71. doi: 10.1016/j.explore.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 7.Cabot PJ, Carter L, Gaiddon C, Zhang Q, Schafer M, Loeffler JP, Stein C. Immune cell-derived beta-endorphin. Production, release, and control of inflammatory pain in rats. J Clin Invest. 1997;100:142–8. doi: 10.1172/JCI119506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rittner HL, Brack A, Machelska H, Mousa SA, Bauer M, Schafer M, Stein C. Opioid peptide-expressing leukocytes: Identification, recruitment, and simultaneously increasing inhibition of inflammatory pain. Anesthesiology. 2001;95:500–8. doi: 10.1097/00000542-200108000-00036. [DOI] [PubMed] [Google Scholar]
- 9.Mousa SA, Shaqura M, Brendl U, Al-Khrasani M, Fürst S, Schäfer M. Involvement of the peripheral sensory and sympathetic nervous system in the vascular endothelial expression of ICAM-1 and the recruitment of opioid-containing immune cells to inhibit inflammatory pain. Brain Behav Immun. 2010;24:1310–23. doi: 10.1016/j.bbi.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 10.Binder W, Mousa SA, Sitte N, Kaiser M, Stein C, Schäfer M. Sympathetic activation triggers endogenous opioid release and analgesia within peripheral inflamed tissue. Eur J Neurosci. 2004;20:92–100. doi: 10.1111/j.1460-9568.2004.03459.x. [DOI] [PubMed] [Google Scholar]
- 11.Kimura K, Masuda K, Wakayama I. Changes in skin blood flow and skin sympathetic nerve activity in response to manual acupuncture stimulation in humans. Am J Chinese Med. 2006;34:189–96. doi: 10.1142/S0192415X06003758. [DOI] [PubMed] [Google Scholar]
- 12.Song JG, Li HH, Cao YF, Lv X, Zhang P, Li YS, Zheng YJ, Li Q, Yin PH, Song SL, Wang HY, Wang XR. Electroacupuncture improves survival in rats with lethal endotoxemia via the autonomic nervous system. Anesthesiology. 2012;116:406–14. doi: 10.1097/ALN.0b013e3182426ebd. [DOI] [PubMed] [Google Scholar]
- 13.Kim H-W, Uh D-K, Yoon S-Y, Roh D-H, Kwon Y-B, Han H-J, Lee H-J, Beitz AJ, Lee J-H. Low-frequency electroacupuncture suppresses carrageenan-induced paw inflammation in mice via sympathetic post-ganglionic neurons, while high-frequency EA suppression is mediated by the sympathoadrenal medullary axis. Brain Res Bull. 2008;75:698–705. doi: 10.1016/j.brainresbull.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 14.Su TF, Zhang LH, Peng M, Wu CH, Pan W, Tian B, Shi J, Pan HL, Li M. Cannabinoid CB2 receptors contribute to upregulation of beta-endorphin in inflamed skin tissues by electroacupuncture. Mol Pain. 2011;7:98. doi: 10.1186/1744-8069-7-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen L, Zhang J, Li F, Qiu Y, Wang L, Li Y-h, Shi J, Pan H-L, Li M. Endogenous anandamide and cannabinoid receptor-2 contribute to electroacupuncture analgesia in rats. J Pain. 2009;10:732–9. doi: 10.1016/j.jpain.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 16.Zhang J, Chen L, Su T, Cao F, Meng X, Pei L, Shi J, Pan HL, Li M. Electroacupuncture increases CB2 receptor expression on keratinocytes and infiltrating inflammatory cells in inflamed skin tissues of rats. J Pain. 2010;11:1250–8. doi: 10.1016/j.jpain.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 17.Su TF, Zhao YQ, Zhang LH, Peng M, Wu CH, Pei L, Tian B, Zhang J, Shi J, Pan HL, Li M. Electroacupuncture reduces the expression of proinflammatory cytokines in inflamed skin tissues through activation of cannabinoid CB2 receptors. Eur J Pain. 2012;16:624–35. doi: 10.1002/j.1532-2149.2011.00055.x. [DOI] [PubMed] [Google Scholar]
- 18.Ozaktay AC, Kallakuri S, Takebayashi T, Cavanaugh JM, Asik I, DeLeo JA, Weinstein JN. Effects of interleukin-1 beta, interleukin-6, and tumor necrosis factor on sensitivity of dorsal root ganglion and peripheral receptive fields in rats. Eur Spine J. 2006;15:1529–37. doi: 10.1007/s00586-005-0058-8. [DOI] [PubMed] [Google Scholar]
- 19.Chao CC, Molitor TW, Close K, Hu S, Peterson PK. Morphine inhibits the release of tumor necrosis factor in human peripheral blood mononuclear cell cultures. Int J Immunopharmacol. 1993;15:447–53. doi: 10.1016/0192-0561(93)90057-6. [DOI] [PubMed] [Google Scholar]
- 20.Bonnet MP, Beloeil H, Benhamou D, Mazoit JX, Asehnoune K. The mu opioid receptor mediates morphine-induced tumor necrosis factor and interleukin-6 inhibition in toll-like receptor 2-stimulated monocytes. Anesth Analg. 2008;106:1142–9. doi: 10.1213/ane.0b013e318165de89. [DOI] [PubMed] [Google Scholar]
- 21.Li A, Zhang RX, Wang Y, Zhang H, Ren K, Berman BM, Tan M, Lao L. Corticosterone mediates electroacupuncture-produced anti-edema in a rat model of inflammation. BMC Complement Altern Med. 2007;7:27. doi: 10.1186/1472-6882-7-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li A, Lao L, Wang Y, Xin J, Ren K, Berman BM, Tan M, Zhang R. Electroacupuncture activates corticotrophin-releasing hormone-containing neurons in the paraventricular nucleus of the hypothalammus to alleviate edema in a rat model of inflammation. BMC Complement Altern Med. 2008;8:20. doi: 10.1186/1472-6882-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee J, Jang K, Lee Y, Choi Y, Choi B. Electroacupuncture inhibits inflammatory edema and hyperalgesia through regulation of cyclooxygenase synthesis in both peripheral and central nociceptive sites. Am J Chin Med. 2006;34:981–8. doi: 10.1142/S0192415X06004454. [DOI] [PubMed] [Google Scholar]
- 24.Jhaveri MD, Richardson D, Chapman V. Endocannabinoid metabolism and uptake: Novel targets for neuropathic and inflammatory pain. Br J Pharmacol. 2007;152:624–32. doi: 10.1038/sj.bjp.0707433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sekido R, Ishimaru K, Sakita M. Corticotropin-releasing factor and interleukin-1beta are involved in the electroacupuncture-induced analgesic effect on inflammatory pain elicited by carrageenan. Am J Chin Med. 2004;32:269–79. doi: 10.1142/S0192415X04001928. [DOI] [PubMed] [Google Scholar]
- 26.Kapitzke D, Vetter I, Cabot PJ. Endogenous opioid analgesia in peripheral tissues and the clinical implications for pain control. Ther Clin Risk Manag. 2005;1:279–97. [PMC free article] [PubMed] [Google Scholar]
- 27.Mousa SA, Bopaiah CP, Richter JF, Yamdeu RS, Schafer M. Inhibition of inflammatory pain by CRF at peripheral, spinal and supraspinal sites: Involvement of areas coexpressing CRF receptors and opioid peptides. Neuropsychopharmacology. 2007;32:2530–42. doi: 10.1038/sj.npp.1301393. [DOI] [PubMed] [Google Scholar]
- 28.Kawabata A. Prostaglandin E2 and pain--an update. Biol Pharm Bull. 2011;34:1170–3. doi: 10.1248/bpb.34.1170. [DOI] [PubMed] [Google Scholar]
- 29.Goldman N, Chen M, Fujita T, Xu Q, Peng W, Liu W, Jensen TK, Pei Y, Wang F, Han X, Chen JF, Schnermann J, Takano T, Bekar L, Tieu K, Nedergaard M. Adenosine A1 receptors mediate local anti-nociceptive effects of acupuncture. Nature Neurosci. 2010;13:883–8. doi: 10.1038/nn.2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Anand P, Whiteside G, Fowler CJ, Hohmann AG. Targeting CB2 receptors and the endocannabinoid system for the treatment of pain. Brain Res Rev. 2009;60:255–66. doi: 10.1016/j.brainresrev.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.White JP, Cibelli M, Rei Fidalgo A, Paule CC, Noormohamed F, Urban L, Maze M, Nagy I. Role of transient receptor potential and acid-sensing ion channels in peripheral inflammatory pain. Anesthesiology. 2010;112:729–41. doi: 10.1097/ALN.0b013e3181ca3179. [DOI] [PubMed] [Google Scholar]
- 32.Chang KH, Won R, Shim I, Lee H, Lee BH. Effects of Electroacupuncture at BL60 on formalin-induced pain in rats. Evid Based Complement Alternat Med. 2012;2012:324039. doi: 10.1155/2012/324039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang Y-Q, Ji G-C, Wu G-C, Zhao Z-Q. Excitatory amino acid receptor antagonists and electroacupuncture synergetically inhibit carrageenan-induced behavioral hyperalgesia and spinal fos expression in rats. Pain. 2002;99:525–35. doi: 10.1016/S0304-3959(02)00268-3. [DOI] [PubMed] [Google Scholar]
- 34.Lao L, Zhang R-X, Zhang G, Wang X, Berman BM, Ren K. A parametric study of electroacupuncture on persistent hyperalgesia and Fos protein expression in rats. Brain Res. 2004;1020:18–29. doi: 10.1016/j.brainres.2004.01.092. [DOI] [PubMed] [Google Scholar]
- 35.Han J-S. Acupuncture: Neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. 2003;26:17–22. doi: 10.1016/s0166-2236(02)00006-1. [DOI] [PubMed] [Google Scholar]
- 36.Zhang RX, Lao L, Wang X, Fan A, Wang L, Ren K, Berman BM. Electroacupuncture attenuates inflammation in a rat model. J Altern Complement Med. 2005;11:135–42. doi: 10.1089/acm.2005.11.135. [DOI] [PubMed] [Google Scholar]
- 37.Zhang R-X, Lao L, Wang L, Liu B, Wang X, Ren K, Berman BM. Involvement of opioid receptors in electroacupuncture-produced anti-hyperalgesia in rats with peripheral inflammation. Brain Res. 2004;1020:12–7. doi: 10.1016/j.brainres.2004.05.067. [DOI] [PubMed] [Google Scholar]
- 38.Kim HY, Wang J, Lee I, Kim HK, Chung K, Chung JM. Electroacupuncture suppresses capsaicin-induced secondary hyperalgesia through an endogenous spinal opioid mechanism. Pain. 2009;145:332–40. doi: 10.1016/j.pain.2009.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang E, Koo S, Kim Y, Lee J, Hwang H, Lee M, Choi S-M. Contralateral electroacupuncture pretreatment suppresses carrageenan-induced inflammatory pain via the opioid-mu receptor. Rheumatol Int. 2011;31:725–30. doi: 10.1007/s00296-010-1364-y. [DOI] [PubMed] [Google Scholar]
- 40.Koo ST, Park YI, Lim KS, Chung K, Chung JM. Acupuncture analgesia in a new rat model of ankle sprain pain. Pain. 2002;99:423–31. doi: 10.1016/S0304-3959(02)00164-1. [DOI] [PubMed] [Google Scholar]
- 41.Kim JH, Kim HY, Chung K, Chung JM. Electroacupuncture reduces the evoked responses of the spinal dorsal horn neurons in ankle-sprained rats. J Neurophysiol. 2011;105:2050–7. doi: 10.1152/jn.00853.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Crain SM, Shen KF. Ultra-low concentrations of naloxone selectively antagonize excitatory effects of morphine on sensory neurons, thereby increasing its antinociceptive potency and attenuating tolerance/dependence during chronic cotreatment. Proc Natl Acad Sci U S A. 1995;92:10540–4. doi: 10.1073/pnas.92.23.10540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hylden JL, Thomas DA, Iadarola MJ, Nahin RL, Dubner R. Spinal opioid analgesic effects are enhanced in a model of unilateral inflammation/hyperalgesia: Possible involvement of noradrenergic mechanisms. Eur J Pharmacol. 1991;194:135–43. doi: 10.1016/0014-2999(91)90097-a. [DOI] [PubMed] [Google Scholar]
- 44.Sluka KA, Rohlwing JJ, Bussey RA, Eikenberry SA, Wilken JM. Chronic muscle pain induced by repeated acid injection is reversed by spinally administered μ- and δ-, but not κ-, opioid receptor agonists. J Pharmacol Exp Ther. 2002;302:1146–50. doi: 10.1124/jpet.102.033167. [DOI] [PubMed] [Google Scholar]
- 45.Besse D, Lombard MC, Zajac JM, Roques BP, Besson JM. Pre- and postsynaptic distribution of mu, delta and kappa opioid receptors in the superficial layers of the cervical dorsal horn of the rat spinal cord. Brain Res. 1990;521:15–22. doi: 10.1016/0006-8993(90)91519-m. [DOI] [PubMed] [Google Scholar]
- 46.Fioravanti B, Vanderah TW. The ORL-1 receptor system: are there opportunities for antagonists in pain therapy? Curr Top Med Chem. 2008;8:1442–51. doi: 10.2174/156802608786264227. [DOI] [PubMed] [Google Scholar]
- 47.Fu X, Wang Y-Q, Wang J, Yu J, Wu G-C. Changes in expression of nociceptin/orphanin FQ and its receptor in spinal dorsal horn during electroacupuncture treatment for peripheral inflammatory pain in rats. Peptides. 2007;28:1220–28. doi: 10.1016/j.peptides.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 48.Fu X, Wang Y-Q, Wu G-C. Involvement of nociceptin/orphanin FQ and its receptor in electroacupuncture-produced anti-hyperalgesia in rats with peripheral inflammation. Brain Res. 2006;1078:212–18. doi: 10.1016/j.brainres.2006.01.026. [DOI] [PubMed] [Google Scholar]
- 49.Pettersson LM, Sundler F, Danielsen N. Expression of orphanin FQ/nociceptin and its receptor in rat peripheral ganglia and spinal cord. Brain Res. 2002;945:266–75. doi: 10.1016/s0006-8993(02)02817-2. [DOI] [PubMed] [Google Scholar]
- 50.Carpenter KJ, Vithlani M, Dickenson AH. Unaltered peripheral excitatory actions of nociceptin contrast with enhanced spinal inhibitory effects after carrageenan inflammation: An electrophysiological study in the rat. Pain. 2000;85:433–41. doi: 10.1016/S0304-3959(99)00301-2. [DOI] [PubMed] [Google Scholar]
- 51.Zhang L-X, Li X-L, Wang L, Han J-S. Rats with decreased brain cholecystokinin levels show increased responsiveness to peripheral electrical stimulation-induced analgesia. Brain Res. 1997;745:158–64. doi: 10.1016/s0006-8993(96)01095-5. [DOI] [PubMed] [Google Scholar]
- 52.Lee G-S, Han J-B, Shin M-K, Hong M-C, Kim S-W, Min B-I, Bae H. Enhancement of electroacupuncture-induced analgesic effect in cholecystokinin-A receptor deficient rats. Brain Res Bull. 2003;62:161–4. doi: 10.1016/j.brainresbull.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 53.Tang N-M, Dong H-W, Wang X-M, Tsui Z-C, Han J-S. Cholecystokinin antisense RNA increases the analgesic effect induced by electroacupuncture or low dose morphine: Conversion of low responder rats into high responders. Pain. 1997;71:71–80. doi: 10.1016/s0304-3959(97)03341-1. [DOI] [PubMed] [Google Scholar]
- 54.Huang C, Hu Z-P, Jiang S-Z, Li H-T, Han J-S, Wan Y. CCKB receptor antagonist L365, 260 potentiates the efficacy to and reverses chronic tolerance to electroacupuncture-induced analgesia in mice. Brain Res Bull. 2007;71:447–51. doi: 10.1016/j.brainresbull.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 55.Chen X-H, Geller EB, Adler MW. CCKB receptors in the periaqueductal grey are involved in electroacupuncture antinociception in the rat cold water tail-flick test. Neuropharmacology. 1998;37:751–7. doi: 10.1016/s0028-3908(98)00028-8. [DOI] [PubMed] [Google Scholar]
- 56.Lee G, Rho S, Shin M, Hong M, Min B-i, Bae H. The association of cholecystokinin-A receptor expression with the responsiveness of electroacupuncture analgesic effects in rat. Neurosci Lett. 2002;325:17–20. doi: 10.1016/s0304-3940(02)00214-8. [DOI] [PubMed] [Google Scholar]
- 57.Shi T, Yang C, Yang D, Gao H, Zhang G, Zhang D, Jiao R, Xu M, Qiao H. L-364,718 potentiates electroacupuncture analgesia through cck-A receptor of pain-related neurons in the nucleus parafascicularis. Neurochem Res. 2011;36:129–38. doi: 10.1007/s11064-010-0281-5. [DOI] [PubMed] [Google Scholar]
- 58.Kim SK, Moon HJ, Park JH, Lee G, Shin M-K, Hong M-C, Bae H, Jin Y-H, Min B-I. The maintenance of individual differences in the sensitivity of acute and neuropathic pain behaviors to electroacupuncture in rats. Brain Res Bull. 2007;74:357–60. doi: 10.1016/j.brainresbull.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 59.Li A, Wang Y, Xin J, Lao L, Ren K, Berman BM, Zhang R-X. Electroacupuncture suppresses hyperalgesia and spinal Fos expression by activating the descending inhibitory system. Brain Res. 2007;1186:171–9. doi: 10.1016/j.brainres.2007.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhao Z-Q. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol. 2008;85:355–75. doi: 10.1016/j.pneurobio.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 61.Mayer DJ. Biological mechanisms of acupuncture. Prog Brain Res. 2000;122:457–77. doi: 10.1016/s0079-6123(08)62157-3. [DOI] [PubMed] [Google Scholar]
- 62.Han JS, Terenius L. Neurochemical basis of acupuncture analgesia. Annu Rev Pharmacol Toxicol. 1982;22:193–220. doi: 10.1146/annurev.pa.22.040182.001205. [DOI] [PubMed] [Google Scholar]
- 63.Cheng RSS, Pomeranz B. Monoaminergic mechanism of electroacupuncture analgesia. Brain Res. 1981;215:77–92. doi: 10.1016/0006-8993(81)90492-3. [DOI] [PubMed] [Google Scholar]
- 64.Silva JR, Silva ML, Prado WA. Analgesia induced by 2- or 100-Hz electroacupuncture in the rat tail-flick test depends on the activation of different descending pain inhibitory mechanisms. J Pain. 2011;12:51–60. doi: 10.1016/j.jpain.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 65.Yoo YC, Oh JH, Kwon TD, Lee YK, Bai SJ. Analgesic mechanism of electroacupuncture in an arthritic pain model of rats: A neurotransmitter study. Yonsei Med J. 2011;52:1016–21. doi: 10.3349/ymj.2011.52.6.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Baek YH, Choi DY, Yang HI, Park DS. Analgesic effect of electroacupuncture on inflammatory pain in the rat model of collagen-induced arthritis: Mediation by cholinergic and serotonergic receptors. Brain Res. 2005;1057:181–5. doi: 10.1016/j.brainres.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 67.Koo ST, Lim KS, Chung K, Ju H, Chung JM. Electroacupuncture-induced analgesia in a rat model of ankle sprain pain is mediated by spinal α-adrenoceptors. Pain. 2008;135:11–9. doi: 10.1016/j.pain.2007.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang Y, Zhang RX, Zhang M, Shen XY, Li A, Xin J, Ren K, Berman BM, Tan M, Lao L. Electroacupuncture inhibition of hyperalgesia in an inflammatory pain rat model: Involvement of distinct spinal serotonin and norepinephrine receptor subtypes. Br J Anaesth. 2012;109:245–52. doi: 10.1093/bja/aes136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li X, Eisenach JC. α2A-adrenoceptor stimulation reduces capsaicin-induced glutamate release from spinal cord synaptosomes. J Pharmacol Exp Ther. 2001;299:939–44. [PubMed] [Google Scholar]
- 70.Choe ES, Shin EH, Wang JQ. Regulation of phosphorylation of NMDA receptor NR1 subunits in the rat neostriatum by group I metabotropic glutamate receptors in vivo. Neurosci Lett. 2006;394:246–51. doi: 10.1016/j.neulet.2005.10.072. [DOI] [PubMed] [Google Scholar]
- 71.Zhang X, Wu J, Lei Y, Fang L, Willis WD. Protein phosphatase modulates the phosphorylation of spinal cord NMDA receptors in rats following intradermal injection of capsaicin. Mol Brain Res. 2005;138:264–72. doi: 10.1016/j.molbrainres.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 72.Roh DH, Kim HW, Yoon SY, Seo HS, Kwon YB, Han HJ, Beitz AJ, Lee JH. Intrathecal clonidine suppresses phosphorylation of the N-methyl-D-aspartate receptor NR1 subunit in spinal dorsal horn neurons of rats with neuropathic pain. Anesth Analg. 2008;107:693–700. doi: 10.1213/ane.0b013e31817e7319. [DOI] [PubMed] [Google Scholar]
- 73.Stone LS, Vulchanova L, Riedl MS, Wang J, Williams FG, Wilcox GL, Elde R. Effects of peripheral nerve injury on alpha-2A and alpha-2C adrenergic receptor immunoreactivity in the rat spinal cord. Neuroscience. 1999;93:1399–407. doi: 10.1016/s0306-4522(99)00209-2. [DOI] [PubMed] [Google Scholar]
- 74.Zhang Y, Li A, Xin J, Lao L, Ren K, Berman B, Tan M, Zhang R-X. Involvement of spinal serotonin receptors in electroacupuncture anti-hyperalgesia in an inflammatory pain rat model. Neurochem Res. 2011;36:1785–92. doi: 10.1007/s11064-011-0495-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li A, Zhang Y, Lao L, Xin J, Ren K, Berman B, Zhang R. Serotonin receptor 2A/C is involved in electroacupuncture inhibition of pain in an osteoarthritis rat model. Evid Based Complement Alternat Med. 2011;2011:619650. doi: 10.1093/ecam/neq016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Salazar-Colocho P, Del Río J, Frechilla D. Serotonin 5-hT1A receptor activation prevents phosphorylation of NMDA receptor NR1 subunit in cerebral ischemia. J Physiol Biochem. 2007;63:203–11. doi: 10.1007/BF03165783. [DOI] [PubMed] [Google Scholar]
- 77.Maneepak M, Le Grand S, Srikiatkhachorn A. Serotonin depletion increases nociception-evoked trigeminal NMDA receptor phosphorylation. Headache. 2009;49:375–82. doi: 10.1111/j.1526-4610.2009.01341.x. [DOI] [PubMed] [Google Scholar]
- 78.Meng X, Lao L, Shen X-Y, Berman BM, Ren K, Wei P-K, Zhang R-X. Electroacupuncture inhibits spinal interleukin-17A to alleviate inflammatory pain in a rat model. Open Pain J. 2013;6:183–9. [Google Scholar]
- 79.Kellstein DE, Malseed RT, Goldstein FJ. Opioid-monoamine interactions in spinal antinociception: Evidence for serotonin but not norepinephrine reciprocity. Pain. 1988;34:85–92. doi: 10.1016/0304-3959(88)90185-6. [DOI] [PubMed] [Google Scholar]
- 80.Pettersen VL, Zapata-Sudo G, Raimundo JM, Trachez MM, Sudo RT. The synergistic interaction between morphine and maprotiline after intrathecal injection in rats. Anesth Analg. 2009;109:1312–7. doi: 10.1213/ane.0b013e3181b16ff5. [DOI] [PubMed] [Google Scholar]
- 81.Sudo RT, Calasans-Maia JA, Galdino SL, Lima MC, Zapata-Sudo G, Hernandes MZ, Pitta IR. Interaction of morphine with a new alpha2-adrenoceptor agonist in mice. J Pain. 2010;11:71–8. doi: 10.1016/j.jpain.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 82.Qu S-S, Huang Y, Zhang Z-J, Chen J-Q, Lin R-Y, Wang C-Q, Li G-L, Wong HK, Zhao C-H, Pan J-Y, Guo S-C, Zhang Y-C. A 6-week randomized controlled trial with 4-week follow-up of acupuncture combined with paroxetine in patients with major depressive disorder. J Psychiatr Res. 2013;47:726–32. doi: 10.1016/j.jpsychires.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 83.Tao YX. Dorsal horn α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor trafficking in inflammatory pain. Anesthesiology. 2010;112:1259–65. doi: 10.1097/ALN.0b013e3181d3e1ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chiechio S, Nicoletti F. Metabotropic glutamate receptors and the control of chronic pain. Curr Opin Pharmacol. 2012;12:28–34. doi: 10.1016/j.coph.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 85.Choi B-T, Kang J, Jo U-B. Effects of electroacupuncture with different frequencies on spinal ionotropic glutamate receptor expression in complete Freund’s adjuvant-injected rat. Acta Histochemica. 2005;107:67–76. doi: 10.1016/j.acthis.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 86.Wang L, Zhang Y, Dai J, Yang J, Gang S. Electroacupuncture (EA) modulates the expression of NMDA receptors in primary sensory neurons in relation to hyperalgesia in rats. Brain Res. 2006;1120:46–53. doi: 10.1016/j.brainres.2006.08.077. [DOI] [PubMed] [Google Scholar]
- 87.Zhang KM, Wang XM, Mokha SS. Opioids modulate N-methyl-D-aspartic acid (NMDA)-evoked responses of neurons in the superficial and deeper dorsal horn of the medulla (trigeminal nucleus caudalis) Brain Res. 1996;719:229–33. doi: 10.1016/0006-8993(96)00123-0. [DOI] [PubMed] [Google Scholar]
- 88.Jang JY, Kim HN, Koo ST, Shin HK, Choe ES, Choi BT. Synergistic antinociceptive effects of N-methyl-D-aspartate receptor antagonist and electroacupuncture in the complete Freund’s adjuvant-induced pain model. Int J Mol Med. 2011;28:669–75. doi: 10.3892/ijmm.2011.728. [DOI] [PubMed] [Google Scholar]
- 89.Zhang R-X, Wang L, Wang X, Ren K, Berman BM, Lao L. Electroacupuncture combined with MK-801 prolongs anti-hyperalgesia in rats with peripheral inflammation. Pharmacol Biochem Behav. 2005;81:146–51. doi: 10.1016/j.pbb.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 90.Mavrommatis CI, Argyra E, Vadalouka A, Vasilakos DG. Acupuncture as an adjunctive therapy to pharmacological treatment in patients with chronic pain due to osteoarthritis of the knee: A 3-armed, randomized, placebo-controlled trial. Pain. 2012;153:1720–26. doi: 10.1016/j.pain.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 91.Shan S, Qi-Liang M-Y, Hong C, Tingting L, Mei H, Haili P, Yan-Qing W, Zhi-Qi Z, Yu-Qiu Z. Is functional state of spinal microglia involved in the anti-allodynic and anti-hyperalgesic effects of electroacupuncture in rat model of monoarthritis? Neurobiol Dis. 2007;26:558–68. doi: 10.1016/j.nbd.2007.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sun S, Cao H, Han M, Li TT, Zhao ZQ, Zhang YQ. Evidence for suppression of electroacupuncture on spinal glial activation and behavioral hypersensitivity in a rat model of monoarthritis. Brain Res Bull. 2008;75:83–93. doi: 10.1016/j.brainresbull.2007.07.027. [DOI] [PubMed] [Google Scholar]
- 93.Mi WL, Mao-Ying QL, Wang XW, Li X, Yang CJ, Jiang JW, Yu J, Wang J, Liu Q, Wang YQ, Wu GC. Involvement of spinal neurotrophin-3 in electroacupuncture analgesia and inhibition of spinal glial activation in rat model of monoarthritis. J pain. 2011;12:974–84. doi: 10.1016/j.jpain.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 94.Zhang R-X, Li A, Liu B, Wang L, Ren K, Zhang H, Berman BM, Lao L. IL-1ra alleviates inflammatory hyperalgesia through preventing phosphorylation of NMDA receptor NR-1 subunit in rats. Pain. 2008;135:232–9. doi: 10.1016/j.pain.2007.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zhang RX, Liu B, Li A, Wang L, Ren K, Qiao JT, Berman BM, Lao L. Interleukin 1β facilitates bone cancer pain in rats by enhancing NMDA receptor NR-1 subunit phosphorylation. Neuroscience. 2008;154:1533–8. doi: 10.1016/j.neuroscience.2008.04.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Guo W, Wang H, Watanabe M, Shimizu K, Zou S, LaGraize SC, Wei F, Dubner R, Ren K. Glial-cytokine-neuronal interactions underlying the mechanisms of persistent pain. J Neurosci. 2007;27:6006–18. doi: 10.1523/JNEUROSCI.0176-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang L, Berta T, Xu Z-Z, Liu T, Park JY, Ji R-R. TNF-alpha contributes to spinal cord synaptic plasticity and inflammatory pain: Distinct role of TNF receptor subtypes 1 and 2. Pain. 2011;152:419–27. doi: 10.1016/j.pain.2010.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kim HN, Kim YR, Jang JY, Shin HK, Choi BT. Electroacupuncture confers antinociceptive effects via inhibition of glutamate transporter downregulation in complete Freund’s adjuvant-injected rats. Evid Based Complement Alternat Med. 2012;2012:643973. doi: 10.1155/2012/643973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Watkins LR, Maier SF. Glia: A novel drug discovery target for clinical pain. Nat Rev Drug Discov. 2003;2:973–85. doi: 10.1038/nrd1251. [DOI] [PubMed] [Google Scholar]
- 100.Beaudry H, Dubois D, Gendron L. Activation of spinal mu- and delta-opioid receptors potently inhibits substance P release induced by peripheral noxious stimuli. J Neurosci. 2011;31:13068–77. doi: 10.1523/JNEUROSCI.1817-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yonehara N, Sawada T, Matsuura H, Inoki R. Influence of electro-acupuncture on the release of substance P and the potential evoked by tooth pulp stimulation in the trigeminal nucleus caudalis of the rabbit. Neurosci Lett. 1992;142:53–6. doi: 10.1016/0304-3940(92)90618-h. [DOI] [PubMed] [Google Scholar]
- 102.Fu X, Zhu ZH, Wang YQ, Wu GC. Regulation of proinflammatory cytokines gene expression by nociceptin/orphanin FQ in the spinal cord and the cultured astrocytes. Neuroscience. 2007;144:275–85. doi: 10.1016/j.neuroscience.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 103.Kim HN, Kim YR, Jang JY, Shin HK, Choi BT. Electroacupuncture inhibits phosphorylation of spinal phosphatidylinositol 3-kinase/Akt in a carrageenan-induced inflammatory rat model. Brain Res Bull. 2012;87:199–204. doi: 10.1016/j.brainresbull.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 104.Xu Q, Fitzsimmons B, Steinauer J, O’Neill A, Newton AC, Hua XY, Yaksh TL. Spinal phosphinositide 3-kinase-Akt-mammalian target of rapamycin signaling cascades in inflammation-induced hyperalgesia. J Neurosci. 2011;31:2113–2124. doi: 10.1523/JNEUROSCI.2139-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Liu B, Zhang RX, Wang L, Ren K, Qiao JT, Berman BM, Lao L. Effects of pertussis toxin on electroacupuncture-produced anti-hyperalgesia in inflamed rats. Brain Res. 2005;1044:87–92. doi: 10.1016/j.brainres.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 106.Liang Y, Fang JQ, Du JY, Fang JF. Effect of electroacupuncture on activation of p38MAPK in spinal dorsal horn in rats with complete Freund’s adjuvant-induced inflammatory pain. Evid Based Complement Alternat Med. 2012;2012:568273. doi: 10.1155/2012/568273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Fang JQ, Du JY, Liang Y, Fang JF. Intervention of electroacupuncture on spinal p38 MAPK/ATF-2/VR-1 pathway in treating inflammatory pain induced by CFA in rats. Mol Pain. 2013;9:13. doi: 10.1186/1744-8069-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ji RR, Gereau RWIV, Malcangio M, Strichartz GR. MAP kinase and pain. Brain Res Rev. 2009;60:135–48. doi: 10.1016/j.brainresrev.2008.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Svensson CI, Marsala M, Westerlund A, Calcutt NA, Campana WM, Freshwater JD, Catalano R, Feng Y, Protter AA, Scott B, Yaksh TL. Activation of p38 mitogen-activated protein kinase in spinal microglia is a critical link in inflammation-induced spinal pain processing. J Neurochem. 2003;86:1534–44. doi: 10.1046/j.1471-4159.2003.01969.x. [DOI] [PubMed] [Google Scholar]
- 110.Zhang R-X, Liu B, Qiao J-T, Wang L, Ren K, Berman BM, Lao L. Electroacupuncture suppresses spinal expression of neurokinin-1 receptors induced by persistent inflammation in rats. Neurosci Lett. 2005;384:339–43. doi: 10.1016/j.neulet.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 111.Chen WH, Hsieh CL, Huang CP, Lin TJ, Tzen JT, Ho TY, Lin YW. Acid-sensing ion channel 3 mediates peripheral anti-hyperalgesia effects of acupuncture in mice inflammatory pain. J Biomed Sci. 2011;18:82. doi: 10.1186/1423-0127-18-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wang YQ, Wu GC. In: Neurochemical basis of electroacupuncture analgesia on acute and chronic pain, Acupuncture therapy for neurological diseases. Xia Y, Cao XD, Wu GC, Cheng JS, editors. New York: Springer; 2010. pp. 195–225. [Google Scholar]
- 113.Munro G. Dopamine D1 and D2 receptor agonism enhances antinociception mediated by the serotonin and noradrenaline reuptake inhibitor duloxetine in the rat formalin test. Eur J Pharmacol. 2007;575:66–74. doi: 10.1016/j.ejphar.2007.07.062. [DOI] [PubMed] [Google Scholar]
- 114.Honda K, Ando S, Koga K, Takano Y. The spinal muscarinic receptor subtypes contribute to the morphine-induced antinociceptive effects in thermal stimulation in mice. Neurosci Lett. 2004;371:235–8. doi: 10.1016/j.neulet.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 115.Honda K, Murao N, Ibuki T, Kamiya HO, Takano Y, Honda K, Murao N, Ibuki T, Kamiya H-O, Takano Y. The role of spinal muscarinic acetylcholine receptors in clonidine-induced anti-nociceptive effects in rats. Biol Pharm Bull. 2003;26:1178–80. doi: 10.1248/bpb.26.1178. [DOI] [PubMed] [Google Scholar]
- 116.Takeshige C, Sato T, Mera T, Hisamitsu T, Fang J. Descending pain inhibitory system involved in acupuncture analgesia. Brain Res Bull. 1992;29:617–34. doi: 10.1016/0361-9230(92)90131-g. [DOI] [PubMed] [Google Scholar]
- 117.Zhang Y, Li A, Lao L, Xin J, Ren K, Berman BM, Zhang RX. Rostral ventromedial medulla μ, but not κ, opioid receptors are involved in electroacupuncture anti-hyperalgesia in an inflammatory pain rat model. Brain Res. 2011;1395:38–45. doi: 10.1016/j.brainres.2011.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ji GC, Yu J, Dong ZQ, Wu GC. Changes of expression of il-1 receptor-i mRNA in rat periaqueductal gray after peripheral inflammation and electroacupuncture analgesia. Acupuncture Res. 2003;28:111–4. [Google Scholar]
- 119.Heinisch S, Palma J, Kirby LG. Interactions between chemokine and mu-opioid receptors: Anatomical findings and electrophysiological studies in the rat periaqueductal grey. Brain Behav Immun. 2011;25:360–72. doi: 10.1016/j.bbi.2010.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chu H, Sun J, Xu H, Niu Z, Xu M. Effect of periaqueductal gray melanocortin 4 receptor in pain facilitation and glial activation in rat model of chronic constriction injury. Neurol Res. 2012;34:871–88. doi: 10.1179/1743132812Y.0000000085. [DOI] [PubMed] [Google Scholar]
- 121.Pereira EA, Boccard SG, Moir L, Fitzgerald JJ, Green AL, Aziz TZ. Deep brain stimulation of the anterior cingulate cortex: Targeting the affective component of chronic pain. Neurosurgery. 2013;60(Suppl 1):178. doi: 10.1227/NEU.0000000000000321. [DOI] [PubMed] [Google Scholar]
- 122.Zhang Y, Meng X, Li A, Xin J, Berman BM, Lao L, Tan M, Ren K, Zhang RX. Electroacupuncture alleviates affective pain in an inflammatory pain rat model. Eur J Pain. 2012;16:170–81. doi: 10.1016/j.ejpain.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.LaGraize SC, Borzan J, Peng YB, Fuchs PN. Selective regulation of pain affect following activation of the opioid anterior cingulate cortex system. Exp Neurol. 2006;197:22–30. doi: 10.1016/j.expneurol.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 124.Ruttenl K, De Vry J, Robens A, Tzschentke TM, van der Kam EL. Dissociation of rewarding, anti-aversive and anti-nociceptive effects of different classes of anti-nociceptives in the rat. Eur J Pain. 2011;15:299–305. doi: 10.1016/j.ejpain.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 125.Jensen TS. Opioids in the brain: Supraspinal mechanisms in pain control. Acta Anaesthesiol Scand. 1997;41:123–32. doi: 10.1111/j.1399-6576.1997.tb04626.x. [DOI] [PubMed] [Google Scholar]
- 126.Yi M, Zhang H, Lao L, Xing GG, Wan Y. Anterior cingulate cortex is crucial for contra- but not ipsi-lateral electro-acupuncture in the formalin-induced inflammatory pain model of rats. Mol Pain. 2011;7:61. doi: 10.1186/1744-8069-7-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Li T-T, Ren W-H, Xiao X, Nan J, Cheng L-Z, Zhang X-H, Zhao Z-Q, Zhang Y-Q. NMDA NR2A and NR2B receptors in the rostral anterior cingulate cortex contribute to pain-related aversion in male rats. Pain. 2009;146:183–93. doi: 10.1016/j.pain.2009.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Martin G, Nie Z, Siggins GR. mu-Opioid receptors modulate NMDA receptor-mediated responses in nucleus accumbens neurons. J Neurosci. 1997;17:11–22. doi: 10.1523/JNEUROSCI.17-01-00011.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Dai Y, Kondo E, Fukuoka T, Tokunaga A, Miki K, Noguchi K. The effect of electroacupuncture on pain behaviors and noxious stimulus-evoked Fos expression in a rat model of neuropathic pain. J Pain. 2001;2:151–9. doi: 10.1054/jpai.2001.19964. [DOI] [PubMed] [Google Scholar]
- 130.Hwang BG, Min BI, Kim JH, Na HS, Park DS. Effects of electroacupuncture on the mechanical allodynia in the rat model of neuropathic pain. Neurosci Lett. 2002;320:49–52. doi: 10.1016/s0304-3940(02)00027-7. [DOI] [PubMed] [Google Scholar]
- 131.Sun RQ, Wang HC, Wan Y, Jing Z, Luo F, Han JS, Wang Y. Suppression of neuropathic pain by peripheral electrical stimulation in rats: Mu-opioid receptor and NMDA receptor implicated. Exp Neurol. 2004;187:23–9. doi: 10.1016/j.expneurol.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 132.Cidral-Filho FJ, da Silva MD, Moré OO, Córdova MM, Werner MF, Santos ARS. Manual acupuncture inhibits mechanical hypersensitivity induced by spinal nerve ligation in rats. Neuroscience. 2011;193:370–6. doi: 10.1016/j.neuroscience.2011.07.076. [DOI] [PubMed] [Google Scholar]
- 133.Kim JH, Min B-I, Na HS, Park DS. Relieving effects of electroacupuncture on mechanical allodynia in neuropathic pain model of inferior caudal trunk injury in rat: Mediation by spinal opioid receptors. Brain Res. 2004;998:230–6. doi: 10.1016/j.brainres.2003.11.045. [DOI] [PubMed] [Google Scholar]
- 134.Pachman DR, Barton DL, Watson JC, Loprinzi CL. Chemotherapy-induced peripheral Nneuropathy: Prevention and treatment. Clin Pharmacol Ther. 2011;90:377–87. doi: 10.1038/clpt.2011.115. [DOI] [PubMed] [Google Scholar]
- 135.Flatters SJL, Bennett GJ. Studies of peripheral sensory nerves in paclitaxel-induced painful peripheral neuropathy: Evidence for mitochondrial dysfunction. Pain. 2006;122:245–57. doi: 10.1016/j.pain.2006.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Meng X, Zhang Y, Li A, Xin J, Lao L, Ren K, Berman BM, Tan M, Zhang R-X. The effects of opioid receptor antagonists on electroacupuncture-produced anti-allodynia/hyperalgesia in rats with paclitaxel-evoked peripheral neuropathy. Brain Res. 2011;1414:58–65. doi: 10.1016/j.brainres.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Shimoyama M, Toyama S, Tagaito Y, Shimoyama N. Endogenous endomorphin-2 contributes to spinal -opioid antinociception. Pharmacology. 2012;89:145–8. doi: 10.1159/000336770. [DOI] [PubMed] [Google Scholar]
- 138.Sun RQ, Wang HC, Wang Y, Luo F, Han JS. Effect of electroacupuncture with different frequencies on neuropathic pain in a rat model. Chin J Appl Physiol. 2002;18:128–31. [PubMed] [Google Scholar]
- 139.Xing G-G, Liu F-Y, Qu X-X, Han J-S, Wan Y. Long-term synaptic plasticity in the spinal dorsal horn and its modulation by electroacupuncture in rats with neuropathic pain. Exp Neurol. 2007;208:323–32. doi: 10.1016/j.expneurol.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 140.Kim SK, Park JH, Bae SJ, Kim JH, Hwang BG, Min B-I, Park DS, Na HS. Effects of electroacupuncture on cold allodynia in a rat model of neuropathic pain: Mediation by spinal adrenergic and serotonergic receptors. Exp Neurol. 2005;195:430–36. doi: 10.1016/j.expneurol.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 141.Song Z, Meyerson BA, Linderoth B. Spinal 5-HT receptors that contribute to the pain-relieving effects of spinal cord stimulation in a rat model of neuropathy. Pain. 2011;152:1666–73. doi: 10.1016/j.pain.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 142.Xu Q, Yaksh TL. A brief comparison of the pathophysiology of inflammatory versus neuropathic pain. Curr Opin Anaesthesiol. 2011;24:400–7. doi: 10.1097/ACO.0b013e32834871df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yan LP, Wu XT, Yin ZY, Ma C. Effect of electroacupuncture on the levels of amino acid neurotransmitters in the spinal cord in rats with chronic constrictive injury. Acupuncture Res. 2011;36:353–6. 379. [PubMed] [Google Scholar]
- 144.Ma C, Li CX, Yi JL, Yan LP. Effects of electroacupuncture on glutamate and aspartic acid contents in the dorsal root ganglion and spinal cord in rats with neuropathic pain. Acupuncture Res. 2008;33:250–4. [PubMed] [Google Scholar]
- 145.Park J-H, Han J-B, Kim S-K, Park J-H, Go D-H, Sun B, Min B-I. Spinal GABA receptors mediate the suppressive effect of electroacupuncture on cold allodynia in rats. Brain Res. 2010;1322:24–9. doi: 10.1016/j.brainres.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 146.Vidal-Torres A, Carceller A, Zamanillo D, Merlos M, Vela JM, Fernández-Pastor B. Evaluation of formalin-induced pain behavior and glutamate release in the spinal dorsal horn using in vivo microdialysis in conscious rats. J Pharmacol Sci. 2012;120:129–32. doi: 10.1254/jphs.12105sc. [DOI] [PubMed] [Google Scholar]
- 147.Choi IS, Cho JH, An CH, Jung JK, Hur YK, Choi JK, Jang IS. 5-HT(1B) receptors inhibit glutamate release from primary afferent terminals in rat medullary dorsal horn neurons. Br J Pharmacol. 2012;167:356–67. doi: 10.1111/j.1476-5381.2012.01964.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Wang Y-Y, Wei Y-Y, Huang J, Wang W, Tamamaki N, Li Y-Q, Wu S-X. Expression patterns of 5-HT receptor subtypes 1A and 2A on GABAergic neurons within the spinal dorsal horn of GAD67-GFP knock-in mice. J Chem Neuroanat. 2009;38:75–81. doi: 10.1016/j.jchemneu.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 149.Pu L, Xu N, Xia P, Gu Q, Ren S, Fucke T, Pei G, Schwarz W. Inhibition of activity of GABA transporter GAT1 by δ-opioid receptor. Evid Based Complement Alternat Med. 2012;2012:818451. doi: 10.1155/2012/818451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hara K, Saito Y, Kirihara Y, Yamada Y, Sakura S, Kosaka Y. The interaction of antinociceptive effects of morphine and GABA receptor agonists within the rat spinal cord. Anesth Analg. 1999;89:422–7. doi: 10.1097/00000539-199908000-00032. [DOI] [PubMed] [Google Scholar]
- 151.Gim G-T, Lee J-h, Park E, Sung Y-H, Kim C-J, Hwang W-w, Chu J-P, Min B-I. Electroacupuncture attenuates mechanical and warm allodynia through suppression of spinal glial activation in a rat model of neuropathic pain. Brain Res Bull. 2011;86:403–11. doi: 10.1016/j.brainresbull.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 152.Choi DC, Lee JY, Lim EJ, Baik HH, Oh TH, Yune TY. Inhibition of ROS-induced p38MAPK and ERK activation in microglia by acupuncture relieves neuropathic pain after spinal cord injury in rats. Exp Neurol. 2012;236:268–82. doi: 10.1016/j.expneurol.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 153.Cha MH, Nam TS, Kwak Y, Lee H, Lee BH. Changes in cytokine expression after electroacupuncture in neuropathic rats. Evid Based Complement Alternat Med. 2012;2012:792765. doi: 10.1155/2012/792765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Lau WK, Chan WK, Zhang JL, Yung KKL, Zhang HQ. Electroacupuncture inhibits cyclooxygenase-2 up-regulation in rat spinal cord after spinal nerve ligation. Neuroscience. 2008;155:463–68. doi: 10.1016/j.neuroscience.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 155.Wang Z, Ma W, Chabot J-G, Quirion R. Calcitonin gene-related peptide as a regulator of neuronal CaMKII-CREB, microglial p38-NFκB and astroglial ERK-Stat1/3 cascades mediating the development of tolerance to morphine-induced analgesia. Pain. 2010;151:194–205. doi: 10.1016/j.pain.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 156.Park J, Kim S, Kim H, Sun B, Koo S, Choi S, Bae H, Min B-I. Spinal cholinergic mechanism of the relieving effects of electroacupuncture on cold and warm allodynia in a rat model of neuropathic pain. J Physiol Sci. 2009;59:291–8. doi: 10.1007/s12576-009-0035-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Torigoe K, Nakahara K, Rahmadi M, Yoshizawa K, Horiuchi H, Hirayama S, Imai S, Kuzumaki N, Itoh T, Yamashita A, Shakunaga K, Yamasaki M, Nagase H, Matoba M, Suzuki T, Narita M. Usefulness of olanzapine as an adjunct to opioid treatment and for the treatment of neuropathic pain. Anesthesiology. 2012;116:159–69. doi: 10.1097/ALN.0b013e31823c7e56. [DOI] [PubMed] [Google Scholar]
- 158.Dong Z-Q, Xie H, Ma F, Li W-M, Wang Y-Q, Wu G-C. Effects of electroacupuncture on expression of somatostatin and preprosomatostatin mRNA in dorsal root ganglions and spinal dorsal horn in neuropathic pain rats. Neurosci Lett. 2005;385:189–94. doi: 10.1016/j.neulet.2005.05.051. [DOI] [PubMed] [Google Scholar]
- 159.Dong Z-Q, Ma F, Xie H, Wang Y-Q, Wu G-C. Changes of expression of glial cell line-derived neurotrophic factor and its receptor in dorsal root ganglions and spinal dorsal horn during electroacupuncture treatment in neuropathic pain rats. Neurosci Lett. 2005;376:143–8. doi: 10.1016/j.neulet.2004.11.044. [DOI] [PubMed] [Google Scholar]
- 160.Dong Z-Q, Ma F, Xie H, Wang Y-Q, Wu G-C. Down-regulation of GFRα-1 expression by antisense oligodeoxynucleotide attenuates electroacupuncture analgesia on heat hyperalgesia in a rat model of neuropathic pain. Brain Res Bull. 2006;69:30–6. doi: 10.1016/j.brainresbull.2005.08.027. [DOI] [PubMed] [Google Scholar]
- 161.Takasu K, Sakai A, Hanawa H, Shimada T, Suzuki H. Overexpression of GDNF in the uninjured DRG exerts analgesic effects on neuropathic pain following segmental spinal nerve ligation in mice. J Pain. 2011;12:1130–9. doi: 10.1016/j.jpain.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 162.Tsuchioka M, Takebayashi M, Hisaoka K, Maeda N, Nakata Y. Serotonin (5-HT) induces glial cell line-derived neurotrophic factor (GDNF) mRNA expression via the transactivation of fibroblast growth factor receptor 2 (FGFR2) in rat C6 glioma cells. J Neurochem. 2008;106:244–57. doi: 10.1111/j.1471-4159.2008.05357.x. [DOI] [PubMed] [Google Scholar]
- 163.Yoshida N, Kobayashi K, Yu L, Wang S, Na R, Yamamoto S, Noguchi K, Dai Y. Inhibition of TRPA1 channel activity in sensory neurons by the glial cell line-derived neurotrophic factor family member, artemin. Mol Pain. 2011;7:41. doi: 10.1186/1744-8069-7-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Yu J, Zhao C, Luo X. The effects of electroacupuncture on the extracellular signal-regulated kinase 1/2/P2X3 signal pathway in the spinal cord of rats with chronic constriction injury. Anesth Analg. 2013;116:239–46. doi: 10.1213/ANE.0b013e31826f0a4a. [DOI] [PubMed] [Google Scholar]
- 165.Rong PJ, Ma SX. Electroacupuncture Zusanli (ST36) on release of nitric oxide in the gracile nucleus and improvement of sensory neuropathies in Zucker diabetic fatty rats. Evid Based Complement Alternat Med. 2011;2011:134545. doi: 10.1093/ecam/nep103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Cha MH, Bai SJ, Lee KH, Cho ZH, Kim YB, Lee HJ, Lee BH. Acute electroacupuncture inhibits nitric oxide synthase expression in the spinal cord of neuropathic rats. Neurol Res. 2010;32:96–100. doi: 10.1179/016164109X12537002794363. [DOI] [PubMed] [Google Scholar]
- 167.Zhang RX, Li A, Liu B, Wang L, Xin J, Ren K, Qiao JT, Berman BM, Lao L. Electroacupuncture attenuates bone cancer-induced hyperalgesia and inhibits spinal preprodynorphin expression in a rat model. Eur J Pain. 2008;12:870–8. doi: 10.1016/j.ejpain.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Zhang RX, Li A, Liu B, Wang L, Ren K, Qiao JT, Berman BM, Lao L. Electroacupuncture attenuates bone cancer pain and inhibits spinal interleukin-1 beta expression in a rat model. Anesth Analg. 2008;105:1482–8. doi: 10.1213/01.ane.0000284705.34629.c5. [DOI] [PubMed] [Google Scholar]
- 169.Lee HJ, Lee JH, Lee EO, Lee HJ, Kim KH, Lee KS, Lee CH, Nam DW, Kim SH, Lee HJ, Ahn KS. Substance P and beta endorphin mediate electroacupuncture induced analgesic activity in mouse cancer pain model. Acupunct Electrother Res. 2009;34:27–40. doi: 10.3727/036012909803861095. [DOI] [PubMed] [Google Scholar]
- 170.Zhang Z, Wang C, Gu G, Li H, Zhao H, Wang K, Han F, Wang G. The effects of electroacupuncture at the ST36 (Zusanli) acupoint on cancer pain and transient receptor potential vanilloid subfamily 1 expression in Walker 256 tumor-bearing rats. Anesth Analg. 2012;114:879–85. doi: 10.1213/ANE.0b013e318246536d. [DOI] [PubMed] [Google Scholar]
- 171.Shinoda M, Ogino A, Ozaki N, Urano H, Hironaka K, Yasui M, Sugiura Y. Involvement of TRPV1 in nociceptive behavior in a rat model of cancer pain. J Pain. 2008;9:687–99. doi: 10.1016/j.jpain.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 172.Chu D, Cheng P, Xiong H, Zhang J, Liu S, Hou X. Electroacupuncture at ST-36 relieves visceral hypersensitivity and decreases 5-HT(3) receptor level in the colon in chronic visceral hypersensitivity rats. Int J Colorectal Dis. 2011;26:569–74. doi: 10.1007/s00384-010-1087-2. [DOI] [PubMed] [Google Scholar]
- 173.Ma XP, Tan LY, Yang Y, Wu HG, Jiang B, Liu HR, Yang L. Effect of electro-acupuncture on substance P, its receptor and corticotropin-releasing hormone in rats with irritable bowel syndrome. World J Gastroenterol. 2009;15:5211–7. doi: 10.3748/wjg.15.5211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wu HG, Jiang B, Zhou EH, Shi Z, Shi DR, Cui YH, Kou S, Liu HR. Regulatory mechanism of electroacupuncture in irritable bowel syndrome: preventing MC activation and decreasing SP VIP secretion. Dig Dis Sci. 2008;53:1644–51. doi: 10.1007/s10620-007-0062-4. [DOI] [PubMed] [Google Scholar]
- 175.Tian L, Huang YX, Tian M, Gao W, Chang Q. Downregulation of electroacupuncture at ST36 on TNF-alpha in rats with ulcerative colitis. World J Gastroenterol. 2003;9:1028–33. doi: 10.3748/wjg.v9.i5.1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Delvaux M, Louvel D, Mamet JP, Campos-Oriola R, Frexinos J. Effect of alosetron on responses to colonic distension in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 1998;12:849–55. doi: 10.1046/j.1365-2036.1998.00375.x. [DOI] [PubMed] [Google Scholar]
- 177.Keszthelyi D, Troost FJ, Simrén M, Ludidi S, Kruimel JW, Conchillo JM, Masclee AA. Revisiting concepts of visceral nociception in irritable bowel syndrome. Eur J Pain. 2012;16:1444–54. doi: 10.1002/j.1532-2149.2012.00147.x. [DOI] [PubMed] [Google Scholar]
- 178.Humes DJ, Simpson J, Smith J, Sutton P, Zaitoun A, Bush D, Bennett A, Scholefield JH, Spiller RC. Visceral hypersensitivity in symptomatic diverticular disease and the role of neuropeptides and low grade inflammation. Neurogastroenterol Motil. 2012;24:318–e163. doi: 10.1111/j.1365-2982.2011.01863.x. [DOI] [PubMed] [Google Scholar]
- 179.Simpson J, Sundler F, Humes DJ, Jenkins D, Scholefield JH, Spiller RC. Post inflammatory damage to the enteric nervous system in diverticular disease and its relationship to symptoms. Neurogastroenterol Motil. 2009;21:847–e58. doi: 10.1111/j.1365-2982.2009.01308.x. [DOI] [PubMed] [Google Scholar]
- 180.Cui KM, Li WM, Gao X, Chung K, Chung JM, Wu GC. Electro-acupuncture relieves chronic visceral hyperalgesia in rats. Neurosci Lett. 2005;376:20–3. doi: 10.1016/j.neulet.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 181.Xu GY, Winston JH, Chen JDZ. Electroacupuncture attenuates visceral hyperalgesia and inhibits the enhanced excitability of colon specific sensory neurons in a rat model of irritable bowel syndrome. Neurogastroenterol Motil. 2009;21:1302–e125. doi: 10.1111/j.1365-2982.2009.01354.x. [DOI] [PubMed] [Google Scholar]
- 182.Xu KD, Liang T, Wang K, Tian DA. Effect of pre-electroacupuncture on p38 and c-Fos expression in the spinal dorsal horn of rats suffering from visceral pain. Chin Med J (Engl) 2010;123:1176–81. [PubMed] [Google Scholar]
- 183.Li C, Yang J, Sun J, Xu C, Zhu Y, Lu Q, Yuan A, Zhu Y, Li L, Zhang W, Liu J, Huang J, Chen D, Wang L, Qin W, Tian J. Brain responses to acupuncture are probably dependent on the brain functional status. Evid Based Complement Alternat Med. 2013;2013:175278. doi: 10.1155/2013/175278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Liu PY, Lu CL, Wang CC, Lee IH, Hsieh JC, Chen CC, Lee HF, Lin HC, Chang FY, Lee SD. Spinal microglia initiate and maintain hyperalgesia in a rat model of chronic pancreatitis. Gastroenterology. 2012;142:165–73. e2. doi: 10.1053/j.gastro.2011.09.041. [DOI] [PubMed] [Google Scholar]
- 185.Gong S, Yin WP, Yin QZ, Gong S, Yin WP, Yin QZ. Involvement of vasopressinergic neurons of paraventricular nucleus in the electroacupuncture-induced inhibition of experimental visceral pain in rats. Acta Physiologica Sinica. 1992;44:434–41. [PubMed] [Google Scholar]
- 186.Lin YP, Peng YB, Yi SX, Tang S. Effect of different frequency electroacupuncture on the expression of substance P and beta-endorphin in the hypothalamus in rats with gastric distension-induced pain. Acupuncture Res. 2009;34:252–7. [PubMed] [Google Scholar]
- 187.Wu HG, Liu HR, Zhang ZA, Zhou EH, Wang XM, Jiang B, Shi Z, Zhou CL, Qi L, Ma XP. Electro-acupuncture relieves visceral sensitivity and decreases hypothalamic corticotropin-releasing hormone levels in a rat model of irritable bowel syndrome. Neurosci Lett. 2009;465:235–7. doi: 10.1016/j.neulet.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 188.Wu JC, Ziea ET, Lao L, Lam EF, Chan CS, Liang AY, Chu SL, Yew DT, Berman BM, Sung JJ. Effect of electroacupuncture on visceral hyperalgesia, serotonin and fos expression in an animal model of irritable bowel syndrome. J Neurogastroenterol Motil. 2010;16:306–14. doi: 10.5056/jnm.2010.16.3.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Zhang JL, Zhang SP, Zhang HQ. Effect of electroacupuncture on thalamic neuronal response to visceral nociception. Eur J Pain. 2009;13:366–72. doi: 10.1016/j.ejpain.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 190.Qi DB, Li WM. Effects of electroacupuncture on expression of c-fos protein and N-methyl-D-aspartate receptor 1 in the rostral ventromedia medulla of rats with chronic visceral hyperalgesia. Zhong Xi Yi Jie He Xue Bao. 2012;10:416–23. doi: 10.3736/jcim20120410. [DOI] [PubMed] [Google Scholar]
- 191.Sanoja R, Tortorici V, Fernandez C, Price TJ, Cervero F. Role of RVM neurons in capsaicin-evoked visceral nociception and referred hyperalgesia. Eur J Pain. 2010;14:120, e1–9. doi: 10.1016/j.ejpain.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Chu WC, Wu JC, Yew DT, Zhang L, Shi L, Yeung DK, Wang D, Tong RK, Chan Y, Lao L, Leung PC, Berman BM, Sung JJ. Does acupuncture therapy alter activation of neural pathway for pain perception in irritable bowel syndrome?: A comparative study of true and sham acupuncture using functional magnetic resonance imaging. J Neurogastroenterol Motil. 2012;18:305–16. doi: 10.5056/jnm.2012.18.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Vickers AJ, Cronin AM, Maschino AC, Lewith G, MacPherson H, Foster NE, Sherman KJ, Witt CM, Linde K. Acupuncture Trialists’ Collaboration: Acupuncture for chronic pain: Individual patient data meta-analysis. Arch Intern Med. 2012;172:1444–53. doi: 10.1001/archinternmed.2012.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Hutchinson AJ, Ball S, Andrews JC, Jones GG. The effectiveness of acupuncture in treating chronic non-specific low back pain: A systematic review of the literature. J Orthop Surg Res. 2012;7:36. doi: 10.1186/1749-799X-7-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Schliessbach J, van der Klift E, Arendt-Nielsen L, Curatolo M, Streitberger K. The effect of brief electrical and manual acupuncture stimulation on mechanical experimental pain. Pain Med. 2011;12:268–75. doi: 10.1111/j.1526-4637.2010.01051.x. [DOI] [PubMed] [Google Scholar]
- 196.Wang K, Bugge J, Bugge S. A randomised, placebo-controlled trial of manual and electrical acupuncture for the treatment of tinnitus. Complement Ther Med. 2010;18:249–55. doi: 10.1016/j.ctim.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 197.Vas J, Méndez C, Perea-Milla E, Vega E, Panadero MD, León JM, Borge MA, Gaspar O, Sánchez-Rodríguez F, Aguilar I, Jurado R. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: Randomised controlled trial. BMJ. 2004;329:1216. doi: 10.1136/bmj.38238.601447.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Sangdee C, Teekachunhatean S, Sananpanich K, Sugandhavesa N, Chiewchantanakit S, Pojchamarnwiputh S, Jayasvasti S. Electroacupuncture versus diclofenac in symptomatic treatment of osteoarthritis of the knee: A randomized controlled trial. BMC Complement Altern Med. 2002;2:3. doi: 10.1186/1472-6882-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Scharf HP, Mansmann U, Streitberger K, Witte S, Krämer J, Maier C, Trampisch HJ, Victor N. Acupuncture and knee osteoarthritis: A three-armed randomized trial. Ann Intern Med. 2006;45:12–20. doi: 10.7326/0003-4819-145-1-200607040-00005. [DOI] [PubMed] [Google Scholar]
- 200.White P, Bishop FL, Prescott P, Scott C, Little P, Lewith G. Practice, practitioner, or placebo? A multifactorial, mixed-methods randomized controlled trial of acupuncture. Pain. 2012;153:455–62. doi: 10.1016/j.pain.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 201.Lin JG, Lo MW, Wen YR, Hsieh CL, Tsai SK, Sun WZ. The effect of high and low frequency electroacupuncture in pain after lower abdominal surgery. Pain. 2002;99:509–14. doi: 10.1016/S0304-3959(02)00261-0. [DOI] [PubMed] [Google Scholar]
- 202.Mi W-L, Mao-Ying Q-L, Liu Q, Wang X-W, Wang Y-Q, Wu G-C. Synergistic anti-hyperalgesia of electroacupuncture and low dose of celecoxib in monoarthritic rats: Involvement of the cyclooxygenase activity in the spinal cord. Brain Res Bull. 2008;77:98–104. doi: 10.1016/j.brainresbull.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 203.Zhang RX, Lao L, Wang X, Ren K, Berman BB. Electroacupuncture combined with indomethacin enhances antihyperalgesia in inflammatory rats. Pharmacol Biochem Behav. 2004;78:793–7. doi: 10.1016/j.pbb.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 204.Song M-J, Wang Y-Q, Wu G-C. Additive anti-hyperalgesia of electroacupuncture and intrathecal antisense oligodeoxynucleotide to interleukin-1 receptor type I on carrageenan-induced inflammatory pain in rats. Brain Res Bull. 2009;78:335–41. doi: 10.1016/j.brainresbull.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 205.Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL., 3rd Sex, gender, and pain: A review of recent clinical and experimental findings. J Pain. 2009;10:447–85. doi: 10.1016/j.jpain.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Mogil JS. Sex differences in pain and pain inhibition: Multiple explanations of a controversial phenomenon. Nat Rev Neurosci. 2012;13:859–66. doi: 10.1038/nrn3360. [DOI] [PubMed] [Google Scholar]