Abstract
Women have a greater risk of developing posttraumatic stress disorder (PTSD) after exposure to trauma. Although sleep abnormalities have been implicated in the development of PTSD, gender differences in sleep soon after a traumatic event have not been investigated. This secondary analysis examined sleep characteristics using polysomnography in 13 female and 22 male trauma patients within a month of their traumatic injuries and assessed PTSD symptoms at 2-months post-injury. Results revealed more wake after sleep onset in women who developed PTSD compared to men who developed PTSD. Women with subsequent PTSD also had less total sleep time than women without subsequent PTSD. Findings suggest possible contributions of impaired sleep maintenance to the development of PTSD in women.
Epidemiological studies have shown that women have greater lifetime prevalence of PTSD than men (10% vs. 5%), even though men are at greater overall risk for trauma exposure (Breslau et al., 1998; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). A meta-analysis by Tolin and Foa (2006) revealed no gender differences in risks for developing PTSD following traumatic events that are more frequently experienced by women (e.g., child sexual abuse and adult sexual assault) and greater risks for PTSD in women after traumatic events more frequently experienced by men (e.g., accident and nonsexual assault). They suggested that factors other than types of trauma contribute to women’s higher prevalence of PTSD (Tolin & Foa, 2006). Many contributing factors have been explored, yet women’s greater vulnerability to PTSD remains poorly understood.
Insomnia is common among people with PTSD and comprises one of its diagnostic criteria (American Psychiatric Association, 2000). For example, 91% of Vietnam combat veterans, 73% of rape victims, and 40% of individuals from an urban general population with PTSD reported problems falling or staying asleep (Neylan et al., 1998; Ohayon & Shapiro, 2000; Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992). Despite frequent sleep complaints by people with PTSD, polysomnographic (PSG) study findings have not been entirely consistent. Some have found indications of sleep disturbances such as increased wake after sleep onset (WASO) and number of awakenings in PTSD patients (Germain & Nielsen, 2003; Glaubman, Mikulincer, Porat, Wasserman, & Birger, 1990), whereas others did not find impaired sleep initiation or maintenance (Breslau et al., 2004; Lavie, Katz, Pillar, & Zinger, 1998). Our meta-analytic study of PSG studies conducted before 2007 discerned that individuals with PTSD had longer stage 1 sleep, shorter slow-wave-sleep (SWS), and increased rapid-eye-movement (REM) density compared to individuals without PTSD (Kobayashi, Boarts, & Delahanty, 2007).
Prospective studies examining associations between sleep characteristics in an acute phase of trauma and the subsequent development of PTSD symptoms indicated that nightmares about trauma and subjective insomnia symptoms within 2 weeks of a serious injury predicted PTSD symptoms at 6-weeks and 1-year post-injury (Kobayashi, Sledjeski, Spoonster, Fallon, & Delahanty, 2008; Koren, Arnon, Lavie, & Klein, 2002; Mellman, David, Bustamante, Torres, & Fins, 2001). Two of these studies used objective sleep measures (Mellman et al., 2002; Klein, Koren, Arnon, & Lavie, 2003). Mellman et al. (2002) assessed sleep using PSG within one month after injury. Patients who developed PTSD had a greater number of REM periods and shorter duration of continuous REM segments compared to patients without subsequent PTSD. They suggested that disruption of REM sleep contributed to the development of PTSD symptoms. Klein et al. (2003) used actigraphy to assess sleep within one week after a motor vehicle accident and also found no difference in sleep duration or sleep efficiency (SE) between patients who subsequently developed PTSD and those who did not develop PTSD at the 1-year follow up assessment. Due to actigraphy limitations, REM sleep was not examined. Neither study analyzed for gender differences.
Although women are more likely to report subjective sleep initiation and maintenance problems than men (Groeger, Zijlstra, & Dijk, 2004; Lindberg et al., 1997), PSG studies of the general population have shown that women have more slow wave sleep (SWS; deep sleep) and more consolidated sleep (less WASO and less stage 1 sleep) than men (Redline et al., 2004; Roehrs, Kapke, Roth, & Breslau, 2006). Research on gender differences in sleep disturbances in individuals with PTSD is scarce. The majority of PSG studies examining PTSD-related sleep disturbances were conducted with men, and there has been no PSG study directly comparing men and women with PTSD. Our meta-analysis showed that findings of less total sleep time (TST), less SWS, and longer sleep onset latency (SOL) were from studies with only male participants (Kobayashi et al., 2007). However, the two studies with only female participants (including one published subsequent to the meta-analysis) revealed longer SOL and more movements measured by actigraphy, and less TST and stage 2 sleep measured by PSG in women with PTSD compared to women without PTSD (Calhoun et al., 2007; Otte et al., 2007). To summarize previous studies, less SWS has been found only in men; impaired sleep initiation and maintenance has been inconsistently found in men (Kobayashi et al., 2007) and more consistently found in women, albeit in a limited number of studies. Gender differences in REM sleep have not been addressed.
To our knowledge, no prospective study has examined gender differences in sleep during an acute phase of trauma, as well as associations between sleep after trauma and the subsequent development of PTSD. Given the gender differences in the risk of developing PTSD and the probable contribution of sleep disturbances to the development of the disorder, there is a need to examine gender differences in sleep characteristics and their associations with the development of PTSD. In this study, we reexamined the archival data obtained in Mellman and colleagues’ prospective study (Mellman et al., 2002; Mellman, Pigeon, Nowell, & Nolan, 2007) for gender differences in objective sleep characteristics soon after a traumatic injury in patients with and without subsequent PTSD. Consistent with the limited data from established PTSD studies, we hypothesized that women who subsequently developed PTSD would have greater impairment in sleep initiation and maintenance, and men with subsequent PTSD would have reduced SWS.
Methods
Participants
Participants were 35 patients (13 females and 22 males) admitted to a Level 1 trauma center at the University of Miami or Dartmouth medical center for injuries from a life-threatening incident (the index incident). They were a subset of participants from a larger descriptive study (160 participants) who completed at least one overnight PSG recording within a month of their injuries. The research procedures were approved by the institutional review boards of the University of Miami and Dartmouth College. Further details are described elsewhere (Mellman et al., 2007). Therefore, we only provide a description of the inclusion and exclusion criteria here.
To be eligible for the parent study, participants must have experienced fear, helplessness, or horror at the time of their injury and been able to recall the incident. Exclusion criteria included intoxication during the incident, clinical or radiological sings of traumatic brain injury, a current major psychiatric disorder (including PTSD and substance use disorders) at the time of injury, and use of psychotropic medication during the month preceding the index incident. Eligibility was assessed through review of trauma registries and hospital charts and screening interviews.
To be selected for the overnight PSG recording, participants must not have had pain significantly interfering with sleep [pain rating level below 25 on a visual analog scale, 0 mm (not at all) to 100 mm (extremely)] within a month of the incident, and not have taken medications affecting the central nervous system, such as sedative hypnotic or anxiolytic medications for 72 hours prior to recording. Low oral doses of narcotic analgesic were allowed, and four participants (2 PTSD positive women; 1 PTSD positive man, 1 PTSD negative man) completed PSG recording while taking low-dose oxycodone. As indicated in the prior report (Mellman et al., 2007), sleep characteristics of participants taking narcotic analgesics did not differ from other participants except for reduced percentage of SWS. Thirty-eight participants completed at least one PSG recording, and three were then excluded due to an apnea/hypopnea index exceeding 10. Sixteen of the 35 remaining participants (4 PTSD positive women, 1 PTSD negative woman, 5 PTSD positive men, and 6 PTSD negative men) were recorded in their hospital bed during their stay, and the other 19 patients (2 PTSD positive women, 6 PTSD negative women, 5 PTSD positive men, and 6 PTSD negative men) were recorded when they returned to a sleep lab in the hospital within a week after hospital discharge. There were no significant differences in settings by gender or PTSD cases (Fisher’s exact test, p = .28). All participants received a full explanation of the study and signed IRB-approved consent forms.
Measures
Polysomnography (PSG)
Overnight PSG recordings were performed as soon as participants met the pain and medication criteria (ranging 7–30 days after their index incidents). Due to logistical barriers such as hospital discharge and limited transportation, the majority of participants completed only one night of PSG recording. Therefore, the first night or the single night was used for data analysis. Recording included one central and one reference electroencephalogram leads, two electrooculograms, a bipolar submental electromyogram, an electrocardiogram lead, finger oximetry, and respiratory strain gage. Trained technicians visually scored each 30-second epoch from a computer screen following standard criteria (Rechstaffen & Kales, 1968). All scorers achieved >90% concordance for epoch staging with reference records. The duration of REM segments was defined as the average length of segments of REM sleep with less than 30 seconds of interruption by wake, movement time, or non-REM sleep.
Clinical interviews
The Clinician Administered PTSD Scale (CAPS: Blake et al., 1995) was administered approximately two months after participants’ index trauma to examine their PTSD diagnostic status and symptom severity. The CAPS is a structured clinical interview that rates frequency and intensity of each of 17 PTSD symptoms on 5-point scales [0 (Never, Not at all) to 4 (Daily or almost daily, Extremely)]. A symptom was considered present if the frequency rating was 1 or greater and if the intensity was 2 or greater. Participants who met the full criteria for PTSD and those who met subthreshold PTSD criteria (meeting criteria for two of the three symptom clusters) were categorized into the PTSD-positive group (n = 16), and the remaining 19 participants were categorized into the PTSD-negative group.
The Structured Interview for DSM-IV (SCID: First, Spitzer, Gibbon, & Williams, 1997) was administered during the initial and follow-up interviews. The SCID is a semi-structured interview designed to assess diagnostic status of psychiatric disorders including mood, anxiety, and substance use disorders. During the initial interview, current psychiatric disorders were screened, and past psychiatric disorders were assessed. New incident psychiatric disorders were evaluated at the 2-month follow-up assessment. Clinical interviews were administered by clinical psychologists or psychiatrists trained by the second author, a licensed psychiatrist (TAM).
Data analysis
SPSS (Version 19, IBM) was used to conduct data analysis. Due to small sample sizes in some groups, non-parametric tests were used. No data transformations were used. An alpha level of .05 was used in all analyses. Participants’ characteristics were examined using the Kruskal-Wallis test. A series of Mann-Whitney U tests were performed to compare sleep parameters by genders within each PTSD status group and also between the PTSD status groups within each gender. Cohen’s ds were computed to evaluate effect sizes.
Results
Participants’ characteristics
Participants’ age and the number of days between injury and PSG were not significantly different between groups (Table 1). As expected, follow-up CAPS scores were greater in the PTSD positive group (Table 1). Types of incident traumatic events included assault (20%), motor vehicle accident (57%), industrial accident (20%), and other (3%). Eighteen participants (3 PTSD positive females, 3 PTSD negative females, 5 PTSD positive males, 7 PTSD negative males, Fisher’s exact test, p = .73) reported having experienced at least one prior traumatic event, but the initial SCID assessment indicated that no participant had PTSD prior to the index incident. Other psychiatric history included past major depression (1 woman and 2 men), past substance use disorder (1 woman and 4 men), and past anxiety disorder (1 woman and 2 men). Three new incident major depressive episodes (1 PTSD positive man and 2 PTSD positive women) were observed at the follow-up assessment.
Table 1.
Participants’ characteristics
| Female | Male | ||||
|---|---|---|---|---|---|
|
| |||||
| PTSD positive n = 6 | PTSD negative n = 7 | PTSD positive n = 10 | PTSD negative n = 12 | Kruskal- Wallis | |
|
| |||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | p | |
| Age | 38.5 (11.1) | 36.0 (11.9) | 33.8 (8.8) | 36.3 (13.4) | .86 |
| Days between injury and PSG | 18.3 (5.5) | 20.6 (6.9) | 18.7 (7.2) | 21.5 (8.5) | .82 |
| Follow-up CAPS total score | 51.2 (12.9) | 23.4 (15.1) | 51.6 (23.5) | 30.4 (22.3) | .01 |
Note. PTSD = posttraumatic stress disorder; PSG = polysomnography; CAPS = Clinician Administered PTSD Scale.
Sleep parameters in female and male participants
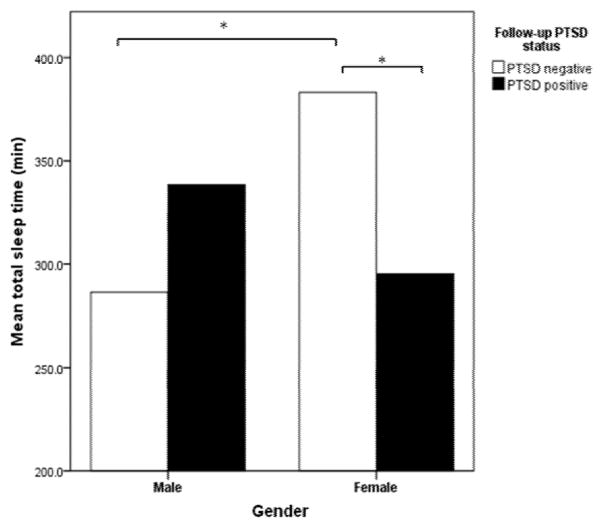
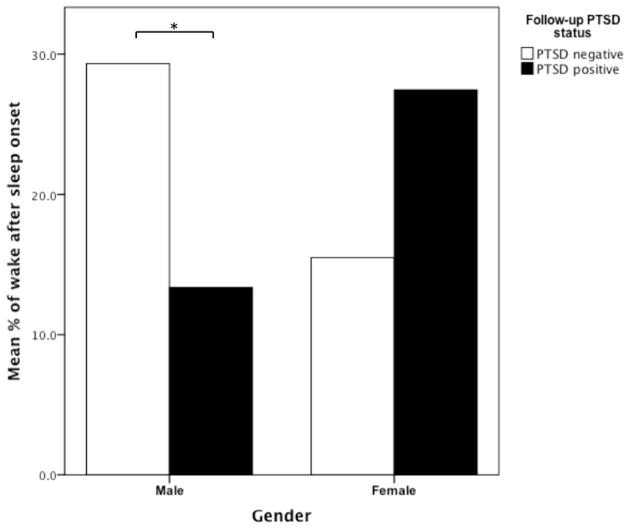
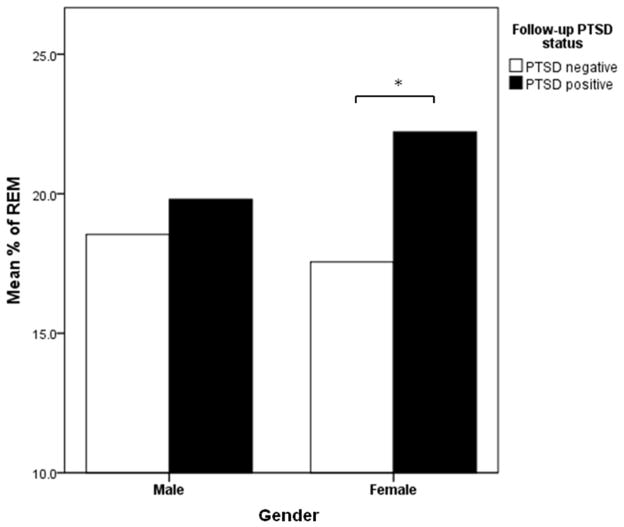
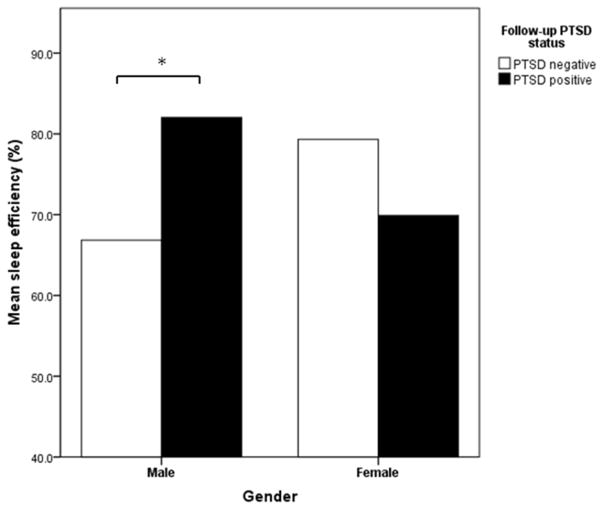
Table 2 shows means and standard deviations of sleep parameters as well as U statistics and effect size estimates (Cohen’s d) for comparisons between PTSD status groups within each gender and between genders within each PTSD status group. Results indicated that time in bed (TIB) and TST were significantly shorter in PTSD-positive females compared to PTSD-negative females, but in males, neither TIB nor TST differ between the PTSD positive and negative groups (Figure 1 for TST). Both WASO (minutes) and percentage of WASO were significantly less in PTSD-positive males compared to PTSD-negative males (Figure 2 for percentage of WASO). A significant difference between PTSD-positive females and males was apparent in WASO (minutes), but in percentage of WASO, the groups were only marginally significantly (p = .07) different despite the large effect size (d = 1.2). Percentage of REM in PTSD-positive females was significantly greater than in PTSD-negative females (Figure 3), but no group differences were found in REM minutes. Greater SE was found in PTSD-positive men compared to PTSD-negative men (Figure 4), which is consistent with less WASO in PTSD-positive men. Given that PTSD-positive and negative men did not differ in SOL, this difference was probably due to the group difference in WASO. All of the significant findings had large effect sizes (d ≥ 1.0).
Table 2.
Sleep Parameters in Female and Male Patients With and Without Subsequent PTSD
| Sleep parameters | Female | Male | PTSD positive | PTSD negative | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| PTSD positive (n = 6) | PTSD negative (n = 7) | PTSD positive (n = 10) | PTSD negative (n =12) | Female vs. Male | Female vs. Male | |||||||
|
| ||||||||||||
| Mean (SD) | Mean (SD) | U | d | Mean (SD) | Mean (SD) | U | d | U | d | U | d | |
| Time in bed | 423.8 (30.5)** | 486.8 (39.1)** | 2 | −1.8 | 408.2 (115.0) | 438.6 (153.1) | 47 | −0.2 | 29 | 0.2 | 50 | 0.4 |
| Total sleep time | 295.3 (78.1)* | 383.1 (45.7)*,+ | 6 | −1.4 | 338.6 (106.6) | 286.4 (113.2)+ | 78 | 0.5 | 21 | −0.4 | 69 | 1.0 |
| % wake after sleep onset | 27.5 (16.5) | 15.5 (10.4) | 33 | 0.9 | 13.3 (7.3)* | 29.3 (15.4)* | 30 | −1.3 | 47 | 1.2 | 20 | −1.0 |
| Wake after sleep onset | 109.5 (61.7)++ | 71.3 (52.0) | 33 | 0.7 | 49.4 (30.7)*,++ | 109.6 (72.3)* | 30 | −1.0 | 53 | 1.4 | 28 | −0.6 |
| Sleep onset latency | 19.0 (21.0) | 32.4 (20.9) | 12 | −0.6 | 20.3 (22.5) | 31.2 (36.2) | 48 | −0.4 | 26 | −0.1 | 47 | 0 |
| Sleep efficiency (%) | 70.0 (18.4) | 79.3 (12.2) | 10 | −0.6 | 82.0 (7.5)* | 66.8 (18.6)* | 83 | 1.1 | 19 | −1.0 | 54 | 0.8 |
| % REM | 22.2 (6.1)* | 17.6 (2.1)* | 35 | 1.0 | 19.8 (10.7) | 18.5 (8.6) | 66 | 0.1 | 34 | 0.3 | 33 | −0.1 |
| REM | 67.2 (27.2) | 66.0 (10.9) | 27 | 0.1 | 75.4 (49.7) | 51.1 (32.8) | 76 | 0.6 | 25 | −0.2 | 56 | 0.5 |
| % slow-wave sleep | 14.7 (17.2) | 11.6 (9.3) | 19 | 0.2 | 15.0 (12.0) | 15.5 (16.3) | 62 | 0 | 28 | 0 | 40 | −0.3 |
| Slow-wave sleep | 38.6 (36.8) | 44.9 (35.1) | 19 | −0.2 | 46.0 (36.2) | 48.0 (61.8) | 65 | 0 | 30 | −0.2 | 48 | −0.1 |
| REM latency | 94.7 (52.9) | 108.1 (47.6) | 16 | −0.3 | 71.4 (49.6) | 101.8 (100.9) | 54 | −0.4 | 36 | 0.5 | 53 | 0.1 |
| REM density | 5.1 (1.9) | 6.9 (4.1) | 16 | −0.5 | 5.6 (2.4) | 7.1 (5.8) | 54 | −0.3 | 29 | −0.2 | 44 | 0 |
| Number of REM periods | 4.7 (2.4) | 3.7 (1.0) | 19 | 0.6 | 4.4 (1.4) | 3.2 (1.7) | 88 | 0.8 | 18 | 0.2 | 56 | 0.3 |
| Duration of REM segment | 11.7 (4.7) | 17.5 (5.9) | 8 | −1.1 | 8.4 (3.5) | 12.6 (9.4) | 47 | −0.6 | 43 | 0.8 | 59 | 0.6 |
Note. Sleep parameters are expressed in minutes unless otherwise specified.
Significant difference between PTSD positive and negative within a gender, * p ≤ .05, ** p < .01;
Significant difference between genders within a PTSD status group, ++ p = .01, + p < .05.
Figure 1.
Total sleep time for males and females with and without follow-up PTSD.
Note. * p <.05.
Figure 2.
Percentage of wake after sleep onset for males and females with and without follow-up PTSD.
Note. * p <.05
Figure 3.
Percentage of REM for males and females with and without follow-up PTSD.
Note. * p <.05.
Figure 4.
Sleep efficiency for males and females with and without follow-up PTSD.
Note. * p <.05.
Discussion
The present study examined gender differences in sleep characteristics in the aftermath of traumatic injury in patients with and without subsequent PTSD by reanalyzing the archival data from Mellman and colleagues’ prospective study (Mellman et al., 2007). To our knowledge, it is the first report presenting direct comparisons between female and male patients’ sleep characteristics measured by PSG soon after their trauma.
We hypothesized that women who subsequently developed PTSD would have greater impairment in sleep initiation and maintenance. We found some indications of impaired sleep maintenance, but not sleep initiation, in women who subsequently developed PTSD. Results indicated significantly reduced TST in women with subsequent PTSD compared to women without subsequent PTSD, which is consistent with the finding in the prior PSG study of women with and without current PTSD (Otte et al., 2007). Although WASO was not significantly different between women with and without subsequent PTSD, female participants with subsequent PTSD had more WASO compared to male participants with subsequent PTSD. Similarly, a greater percentage of WASO in PTSD-positive females than PTSD-positive males was indicated by a large effect size (d = 1.2). Further, a large effect size (d = 0.9) suggests less percentage of WASO in PTSD-positive females compared to PTSD-negative females.
The second hypothesis, that men with subsequent PTSD would have less SWS, was not supported. We did not find less SWS in either male or female participants with subsequent PTSD. It is possible that the reduced sleep depth in men with established PTSD reported in prior studies emerges over time.
Overall, gender differences were not found in sleep architecture except for percentage of REM. Although percentage of REM sleep was greater in women with subsequent PTSD compared to women without PTSD, the amount of REM sleep, in minutes, did not differ. Shorter duration of REM segments in patients with subsequent PTSD was found in the sample combining both genders (Mellman et al., 2007), but in the present separate analyses for men and women, it was not found in either gender probably due to a lack of statistical power. Although it was not statistically significant, it appears that both men and women with subsequent PTSD had shorter duration of REM segments and the increased number of REM segments (at least medium effect sizes), which may suggest contribution of disrupted REM to the development of PTSD in both genders. On the other hand, disrupted maintenance of sleep was indicated only in females with subsequent PTSD. It is, therefore, possible that disrupted maintenance of sleep in the aftermath of trauma contributes to women’s greater risk of developing PTSD.
Certain cautions should accompany interpretation of these findings due to limitations of the study and the secondary analysis approach. First, small sample sizes limited statistical power and types of statistical tests that can be applied. Second, only single night data were available; therefore, results may be influenced by first night effects or chance occurrences. Studies have shown, however, that first night effects are similar in men and women (Goel, Kim, & Lao, 2005) and individuals with and without PTSD (Breslau et al., 2004). Third, the counterintuitive results indicating more WASO and less TST in PTSD-negative men may have contributed to the gender differences in this sample. As there were no significant differences in the recording environment among the groups, we speculate that variable individual effects of injury on sleep could have contributed to the findings. Fourth, all our participants had traumatic injuries and no prior history of PTSD, which may limit generalizability of the present findings to other trauma-exposed populations.
Despite these limitations, our secondary analysis provides unique information regarding gender differences in sleep soon after a traumatic event and development of PTSD. Our findings indicate that poor sleep maintenance in recently injured women is another risk factor to consider in subsequent development of PTSD for women. These results need to be replicated in future studies with larger sample sizes and multiple nights of PSG recordings.
Footnotes
Presented data were collected at the University of Miami and Dartmouth Hitchcock Medical Center, and the study was supported by NIMH grant MH-54006 to Thomas Mellman, M.D.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders - forth edition - text revision. Washington, DC: Author; 2000. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Breslau N, Roth T, Burduvali E, Kapke A, Schults L, Roehrs T. Sleep in lifetime posttraumatic stress disorder a community-based polysomnographic study. Archives of General Psychiatry. 2004;61(5):508–516. doi: 10.1001/archpsyc.61.5.508. [DOI] [PubMed] [Google Scholar]
- Calhoun PS, Wiley M, Dennis MF, Means MK, Edinger JD, Beckham JC. Objective evidence of sleep disturbance in women with posttraumatic stress disorder. Journal of Traumatic Stress. 2007;20(6):1009–1018. doi: 10.1002/jts.20255. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV axis I disorders. Arlington, VA: American Psychiatric; 1997. [Google Scholar]
- Germain A, Nielsen TA. Sleep pathophysiology in posttraumatic stress disorder and idiopathic nightmare sufferers. Biological Psychiatry. 2003;54(10):1092–1098. doi: 10.1016/s0006-3223(03)00071-4. [DOI] [PubMed] [Google Scholar]
- Glaubman H, Mikulincer M, Porat A, Wasserman O, Birger M. Sleep of chronic post-traumatic patients. Journal of Traumatic Stress. 1990;3(2):255–263. [Google Scholar]
- Goel N, Kim H, Lao RP. Gender differences in polysomnographic sleep in young healthy sleepers. Chronobiology International. 2005;22(5):905–915. doi: 10.1080/07420520500263235. [DOI] [PubMed] [Google Scholar]
- Groeger JA, Zijlstra FRH, Dijk DJ. Sleep quantity, sleep difficulties and their perceived consequences in a representative sample of some 2000 British adults. Journal of Sleep Research. 2004;13(4):359–371. doi: 10.1111/j.1365-2869.2004.00418.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Klein E, Koren D, Arnon I, Lavie P. Sleep complaints are not corroborated by objective sleep measures in post-traumatic stress disorder: A 1-year prospective study in survivors of motor vehicle crashes. Journal of Sleep Research. 2003;12:35–41. doi: 10.1046/j.1365-2869.2003.00334.x. [DOI] [PubMed] [Google Scholar]
- Kobayashi I, Boarts JM, Delahanty DL. Polysomnographically measured sleep abnormalities in PTSD: A meta-analytic review. Psychophysiology. 2007;44(4):660–669. doi: 10.1111/j.1469-8986.2007.537.x. [DOI] [PubMed] [Google Scholar]
- Kobayashi I, Sledjeski EM, Spoonster E, Fallon WF, Delahanty DL. Effects of early nightmares on the development of sleep disturbances in motor vehicle accident victims. Journal of Traumatic Stress. 2008;21(6):548–555. doi: 10.1002/jts.20368. [DOI] [PubMed] [Google Scholar]
- Koren D, Arnon I, Lavie P, Klein E. Sleep complaints as early predictors of posttraumatic stress disorder: A 1-year prospective study of injured survivors of motor vehicle accidents. American Journal of Psychiatry. 2002;159(5):855–857. doi: 10.1176/appi.ajp.159.5.855. [DOI] [PubMed] [Google Scholar]
- Lavie P, Katz N, Pillar G, Zinger Y. Elevated awaking thresholds during sleep: Characteristics of chronic war-related posttraumatic stress disorder patients. Biological Psychiatry. 1998;44(10):1060–1065. doi: 10.1016/s0006-3223(98)00037-7. [DOI] [PubMed] [Google Scholar]
- Lindberg E, Janson C, Gislason T, Bjornsson E, Hetta J, Boman G. Sleep disturbances in A young adult population: Can gender differences be explained by differences in psychological status? Sleep. 1997;20(6):381–387. doi: 10.1093/sleep/20.6.381. [DOI] [PubMed] [Google Scholar]
- Mellman TA, Bustamante V, Fins AI, Pigeon WR, Nolan B. REM sleep and the early development of posttraumatic stress disorder. American Journal of Psychiatry. 2002;159(10):1696–1701. doi: 10.1176/appi.ajp.159.10.1696. [DOI] [PubMed] [Google Scholar]
- Mellman TA, David D, Bustamante V, Torres J, Fins A. Dreams in the acute aftermath of trauma and their relationship to PTSD. Journal of Traumatic Stress. 2001;14(1):241–247. [Google Scholar]
- Mellman TA, Pigeon WR, Nowell PD, Nolan B. Relationships between REM sleep findings and PTSD symptoms during the early aftermath of trauma. Journal of Traumatic Stress. 2007;20(5):893–901. doi: 10.1002/jts.20246. [DOI] [PubMed] [Google Scholar]
- Neylan TC, Marmar CR, Metzler TJ, Weiss DS, Zatzick DF, Delucchi KL, et al. Sleep disturbances in the vietnam generation: Findings from a nationally representative sample of male Vietnam veterans. American Journal of Psychiatry. 1998;155(7):929–933. doi: 10.1176/ajp.155.7.929. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Shapiro CM. Sleep disturbances and psychiatric disorders associated with posttraumatic stress disorder in the general population. Comprehensive Psychiatry. 2000;41(6):469–478. doi: 10.1053/comp.2000.16568. [DOI] [PubMed] [Google Scholar]
- Otte C, Lenoci M, Metzler T, Yehuda R, Marmar CR, Neylan TC. Effects of metyrapone on hypothalamic-pituitary-adrenal axis and sleep in women with post-traumatic stress disorder. Biological Psychiatry. 2007;61(8):952–956. doi: 10.1016/j.biopsych.2006.08.018. [DOI] [PubMed] [Google Scholar]
- Rechstaffen A, Kales A. A manual for standardized terminology, techniques, and scoring system for sleep stages of human subjects. Los Angeles: University of California-Los Angeles, Brain Information System; 1968. [Google Scholar]
- Redline S, Kirchner HL, Quan SF, Gottlieb DJ, Kapur V, Newman A. The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Archives of Internal Medicine. 2004;164(4):406–418. doi: 10.1001/archinte.164.4.406. [DOI] [PubMed] [Google Scholar]
- Roehrs T, Kapke A, Roth T, Breslau N. Sex differences in the polysomnographic sleep of young adults: A community-based study. Sleep Medicine. 2006;7(1):49–53. doi: 10.1016/j.sleep.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Rothbaum BO, Foa EB, Riggs DS, Murdock T, Walsh W. A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress. 1992;5(3):455–475. [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132(6):959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]