Abstract
Strong secular declines in physical activity, increased fat and salt intake, and increased obesity, especially abdominal obesity, mark China's recent nutrition transition. The China Health and Nutrition 2009 Survey collected anthropometry, blood pressure, and fasting blood samples from more than 9,000 individuals ≥ seven years of age. We focus on elevated blood pressure and plasma markers of diabetes, inflammation, and dyslipidemia. We used international definitions of cardiometabolic risk and estimated age- and sex-specific prevalence ratios for each outcome for high waist circumference or overweight. We used logistic regression to assess each risk factor's association with diet, physical activity, overweight, and abdominal obesity. Cardiometabolic risk prevalence was high in all age groups Prevalence ratios for most risk factors were nearly doubled for overweight or high waist circumference groups. Prevalence ratios were higher in younger than older adults. Low physical activity consistently predicted higher cardiometabolic risk across most outcomes and age-sex groups. The co-occurrence of overweight and high waist circumference was highly predictive of dyslipidemia, elevated glycated hemoglobin, and diabetes. High prevalence of cardiometabolic risk factors and their strong association with weight status and abdominal obesity in young adults portend increases in cardiometabolic morbidity and mortality. Early interventions will be required to reverse trends.
Keywords: China, cardiometabolic risk, overweight, abdominal obesity, diet, physical activity
Unprecedented social and economic changes in China have led to patterns of diet and physical activity that are contributing to large increases in the prevalence of overweight and obesity across all ages, regions, and levels of socioeconomic status.1-6 Of particular concern is that waist circumference, an indicator of central fat distribution strongly associated with cardiometabolic (CM) diseases, has increased disproportionately relative to overall body mass.7 This trend is particularly alarming, since Asians are known have higher amounts of central fat at the same body mass index (BMI) compared to Caucasian populations8-15 and tend to develop diabetes and related diseases at a younger age and a lower BMI.16
CM diseases (diabetes, cardiovascular diseases) have increased substantially in China,17, 18 imposing a heavy burden on its health care systems. CM diseases are now the leading cause of morbidity and mortality in China and many other Asian countries.19, 20
Other papers in this issue document important trends in diet, physical activity, and overweight or obesity. These changes have important implications for CM disease risk. Much of the urban Chinese population is now characterized by low levels of physical activity at work, as jobs have become less physically demanding,6, 21 and across China diets are higher in fat and sodium compared to just 20 years ago.22, 23
This paper aims to document the prevalence of CM risk factors among participants in the China Health and Nutrition Survey (CHNS) and to explore factors related to levels of risk with a focus on high blood pressure, indicators of glucose metabolism and insulin resistance, dyslipidemia, and inflammation. In prior publications we reported the prevalence of selected CM risk factors according to levels of urbanization and income24 and explored patterns of CM risk in relation to overweight with a focus on the high burden of CM risk even among those who are not overweight.11 Here we examine differences in CM risk in relation to BMI and waist circumference and relate CM risk to the macronutrient composition of the diet and to levels of physical activity.
Methods
The 2009 CHNS collected fasting blood samples from more than 9,000 individuals, ages 7 yr and above. We use data on non-pregnant youths (< 18 years yr) and adults (18–98 yr) with anthropometry (weight, height, and waist circumference) and blood pressure (n = 9,168), glycated hemoglobin (HbA1c) (n = 9,108), C-reactive protein (CRP) (n = 9,175), and fasting glucose and lipids (n = 8,746). Laboratory analysis methods for the CM biomarkers are described in detail elsewhere (Yan et al 2012).
We used internationally accepted definitions of CM risk. For overweight these include BMI ≥ 25 kg/m2 or the pediatric equivalent defined by the International Obesity Task Force.25 We used the waist to height ratio (WHtR) because of its strong association with diabetes in China26 and common definition for adults and youth, with values > 0.5 indicating central adiposity. We used International Diabetes Federation definitions27 for high blood pressure in adults (systolic ≥ 130 or diastolic ≥ 85 or taking antihypertension medication) and for youths, a blood pressure > 85th percentile of an age-, sex-, and height-specific US reference.28 Lipids-related risk factors include high triacylglycerol (TAG > 150 mg/dL), high low-density lipoprotein cholesterol (LDL > 130 mg/dL), low high-density lipoprotein cholesterol (HDL < 40 mg/dL for men, < 50 mg/dl for youths and women), and atherogenic dyslipidemia (high TAG and low HDL). Markers of glucose control include impaired HbA1c (prediabetic or diabetic HbA1c ≥ 5.6%), diabetes (HbA1c ≥ 6.5%), and insulin resistance (homeostasis model of assessment–insulin resistance, HOMA-IR > 4.65). Inflammation is represented by high CRP (> 3 mg/dL but < 10 mg/dL).
Diet
Dietary intake was estimated from three consecutive 24-hour recalls for each individual supplemented with a daily inventory of all available foods in the household.29, 30 We used the three-day means of energy intake and percentage of energy intake from fat and protein in the analyses.
Physical Activity
Physical activity was assessed using questionnaires that probed the time spent in a typical week at work, in leisure time, in travel, and in doing household chores. We created a summary variable using minutes spent in each activity multiplied by metabolic equivalents (METs) for that activity.31 Total MET minutes at work, leisure, chores, and travel were summed and represented in models divided into physical activity quintiles. Models that included physical activity were restricted to adults owing to the lack of comparable child data.
Socioeconomic and Environmental Variables
We categorized level of education for adults as less than primary school, completed primary school, completed secondary school, and more than secondary school. We represented urbanicity categorized by quintiles of an urbanization index reflecting population size and density and community infrastructure.32 We represented household income, estimated from the sum of individual incomes of all earners in the household, categorized by quintiles. We categorized age to represent youths (7– <18 yrs) and adults (18–<35 yr, 35–<50 yr, 50–<65 yr, and over 65 or greater yrs.
Analysis
We estimated, within age and sex strata, crude prevalence ratios for CM risk factors, comparing rates in overweight versus normal weight and high WHtR versus normal WHtR participants. We used sex-stratified logistic regression to assess the association of diet and physical activity to each CM risk factor, adjusting for age, education, household income, and level of urbanization and for the clustering of individuals within households. We also estimated, using logistic regression, how being overweight alone, having a high WHtR alone, or having both risk factors related to the likelihood of having each CM risk factor, adjusted for the same factors listed above.
Results
Prevalence of Risk Factors
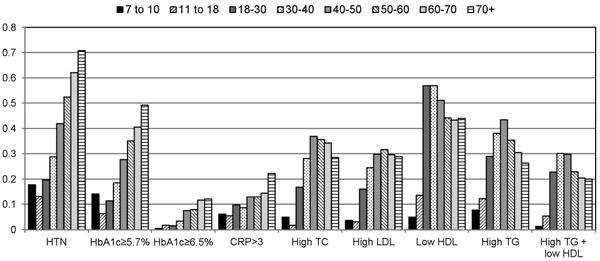
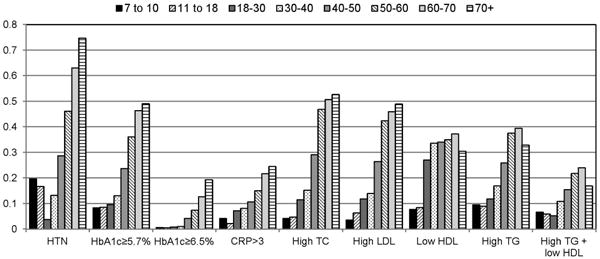
The prevalence of overweight and obesity is higher in middle adulthood than in youth or young adulthood, highest in men after age 30 and women after age 40 (Table 1), but lower in those over 65 yr. The prevalence of high WHtR consistently increased with age in men and women. The prevalence of CM risk factors varied substantially across age and sex groups, with consistent and marked increases with age most apparent for high blood pressure and markers of glucose control (Figure 1).
Table 1. Crude Prevalence Ratios for CM risk factors, comparing high to normal Waist Circumference to height ratio (WHtR>0.5) and Overweight (OW = BMI≥25 kg/m2) to non-overweight groups, China Health and Nutrition Survey, 2009.
| High BP | Impaired HbA1c (pre-diabetic or diabetic,HbA1c≥5.7%) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| High WHtR | Overweight | High WHtR | Overweight | |||||||||||||||
| High BP (prop) | High WHtR (prop) | PR | 95% CI | OW (prop) | PR | 95% CI | Impaired HbA1c (prop) | High WHtR (prop) | PR | 95% CI | OW (prop) | PR | 95% CI | |||||
| Males | ||||||||||||||||||
| <18 | 0.16 | 0.12 | 2.03 | 1.21 | 3.40 | 0.12 | 1.43 | 0.80 | 2.56 | 0.10 | 0.12 | 0.90 | 0.37 | 2.18 | 0.12 | 0.74 | 0.28 | 1.97 |
| 18-<35 | 0.22 | 0.33 | 2.16 | 1.62 | 2.88 | 0.23 | 2.06 | 1.55 | 2.75 | 0.13 | 0.33 | 1.51 | 1.00 | 2.28 | 0.23 | 1.24 | 0.79 | 1.94 |
| 35-<50 | 0.38 | 0.53 | 1.86 | 1.59 | 2.17 | 0.34 | 1.84 | 1.61 | 2.11 | 0.25 | 0.53 | 2.14 | 1.73 | 2.65 | 0.34 | 1.94 | 1.61 | 2.34 |
| 50-<65 | 0.54 | 0.57 | 1.31 | 1.18 | 1.46 | 0.29 | 1.33 | 1.21 | 1.46 | 0.37 | 0.57 | 1.71 | 1.46 | 2.00 | 0.29 | 1.60 | 1.40 | 1.83 |
| 65+ | 0.66 | 0.60 | 1.16 | 1.05 | 1.29 | 0.26 | 1.36 | 1.24 | 1.48 | 0.46 | 0.60 | 1.26 | 1.07 | 1.50 | 0.26 | 1.37 | 1.17 | 1.60 |
| Females | ||||||||||||||||||
| <18 | 0.18 | 0.07 | 1.23 | 0.55 | 2.77 | 1.23 | 1.69 | 0.95 | 3.01 | 0.08 | 0.07 | 1.08 | 0.27 | 4.27 | 0.10 | 1.02 | 0.32 | 3.18 |
| 18-<35 | 0.06 | 0.26 | 4.80 | 2.54 | 9.06 | 4.80 | 5.82 | 3.27 | 10.37 | 0.10 | 0.26 | 2.03 | 1.28 | 3.22 | 0.12 | 1.98 | 1.15 | 3.41 |
| 35-<50 | 0.24 | 0.53 | 2.13 | 1.75 | 2.61 | 2.13 | 2.15 | 1.81 | 2.55 | 0.21 | 0.53 | 2.20 | 1.76 | 2.75 | 0.30 | 2.13 | 1.76 | 2.58 |
| 50-<65 | 0.49 | 0.73 | 1.53 | 1.33 | 1.76 | 1.53 | 1.41 | 1.28 | 1.56 | 0.38 | 0.73 | 1.68 | 1.41 | 2.00 | 0.36 | 1.69 | 1.49 | 1.91 |
| 65+ | 0.69 | 0.77 | 1.28 | 1.13 | 1.45 | 1.28 | 1.16 | 1.07 | 1.26 | 0.49 | 0.77 | 1.30 | 1.07 | 1.58 | 0.31 | 1.61 | 1.41 | 1.83 |
| All | 1.98 | 1.87 | 2.09 | 1.65 | 1.57 | 1.73 | 2.17 | 2.01 | 2.33 | 1.84 | 1.73 | 1.96 | ||||||
| M-H p-value | p<0.001 | p<0.001 | p<0.001 | p=0.012 | ||||||||||||||
| Diabetic (HbA1c≥6.5%) | High HOMA-IR (>4.65) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| High WHtR | Overweight | High WHtR | Overweight | |||||||||||||||
| Diabetic (prop) | High WHtR (prop) | PR | 95% CI | OW (prop) | PR | 95% CI | High HOMA (prop) | High WHtR (prop) | PR | 95% CI | OW (prop) | PR | 95% CI | |||||
| Males | ||||||||||||||||||
| <18 | 0.01 | 0.12 | na | 0.12 | na | na | na | 0.16 | 0.12 | 2.65 | 1.66 | 4.24 | 0.12 | 2.97 | 1.90 | 4.65 | ||
| 18-<35 | 0.02 | 0.33 | 2.39 | 0.81 | 7.01 | 0.23 | 2.15 | 0.71 | 6.46 | 0.16 | 0.33 | 3.12 | 2.14 | 4.55 | 0.23 | 3.12 | 2.19 | 4.43 |
| 35-<50 | 0.06 | 0.53 | 3.03 | 1.81 | 5.07 | 0.34 | 2.72 | 1.77 | 4.18 | 0.17 | 0.53 | 2.66 | 1.98 | 3.56 | 0.34 | 2.61 | 2.04 | 3.34 |
| 50-<65 | 0.09 | 0.57 | 2.79 | 1.83 | 4.24 | 0.29 | 2.54 | 1.82 | 3.53 | 0.14 | 0.57 | 2.25 | 1.64 | 3.08 | 0.29 | 2.66 | 2.04 | 3.46 |
| 65+ | 0.12 | 0.60 | 3.02 | 1.80 | 5.09 | 0.26 | 2.75 | 1.87 | 4.03 | 0.19 | 0.60 | 2.77 | 1.85 | 4.13 | 0.26 | 2.98 | 2.23 | 4.00 |
| Females | ||||||||||||||||||
| <18 | 0.01 | 0.07 | na | 0.10 | 0.00 | na | na | 0.16 | 0.07 | 2.52 | 1.36 | 4.68 | 0.10 | 2.39 | 1.37 | 4.18 | ||
| 18-<35 | 0.01 | 0.26 | na | 0.12 | 0.00 | na | na | 0.09 | 0.26 | 1.21 | 0.70 | 2.07 | 0.12 | 2.35 | 1.35 | 4.11 | ||
| 35-<50 | 0.03 | 0.53 | 3.10 | 1.60 | 6.01 | 0.30 | 2.96 | 1.71 | 5.11 | 0.13 | 0.53 | 2.50 | 1.82 | 3.42 | 0.30 | 2.29 | 1.75 | 2.99 |
| 50-<65 | 0.09 | 0.73 | 2.82 | 1.69 | 4.69 | 0.36 | 2.04 | 1.48 | 2.81 | 0.16 | 0.73 | 2.43 | 1.70 | 3.46 | 0.36 | 2.27 | 1.80 | 2.87 |
| 65+ | 0.17 | 0.77 | 1.93 | 1.21 | 3.08 | 0.31 | 2.05 | 1.52 | 2.75 | 0.20 | 0.77 | 1.72 | 1.14 | 2.60 | 0.31 | 2.58 | 1.97 | 3.39 |
| All | 3.79 | 3.13 | 4.60 | 2.67 | 2.30 | 3.09 | 2.21 | 1.98 | 2.47 | 2.55 | 2.32 | 2.80 | ||||||
| M-H p-value | p=0.976 | p=0.935 | p=0.216 | p=0.866 | ||||||||||||||
| High LDL (>130 mg/L) | Low HDL (≤40 mg/dL in males and youth, ≤50 mg/dL in females | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| High WHtR | Overweight | High WHtR | Overweight | |||||||||||||||
| High LDL (prop) | High WHtR (prop) | PR | 95% CI | OW (prop) | PR | 95% CI | Low HDL (prop) | High WHtR (prop) | PR | 95% CI | OW (prop) | PR | 95% CI | |||||
| Males | ||||||||||||||||||
| <18 | 0.03 | 0.12 | 1.18 | 0.27 | 5.14 | 0.12 | 0.54 | 0.07 | 4.04 | 0.09 | 0.12 | 2.07 | 1.05 | 4.10 | 0.12 | 1.81 | 0.88 | 3.70 |
| 18-<35 | 0.19 | 0.33 | 1.90 | 1.38 | 2.63 | 0.23 | 1.72 | 1.24 | 2.40 | 0.55 | 0.33 | 1.57 | 1.37 | 1.79 | 0.23 | 1.57 | 1.39 | 1.79 |
| 35-<50 | 0.29 | 0.53 | 1.23 | 1.03 | 1.47 | 0.34 | 1.13 | 0.95 | 1.36 | 0.54 | 0.53 | 1.52 | 1.36 | 1.69 | 0.34 | 1.63 | 1.48 | 1.79 |
| 50-<65 | 0.32 | 0.57 | 1.46 | 1.24 | 1.73 | 0.29 | 1.32 | 1.13 | 1.54 | 0.44 | 0.57 | 1.56 | 1.37 | 1.78 | 0.29 | 1.58 | 1.41 | 1.77 |
| 65+ | 0.28 | 0.60 | 1.62 | 1.25 | 2.10 | 0.26 | 1.58 | 1.26 | 1.99 | 0.44 | 0.60 | 1.72 | 1.42 | 2.09 | 0.26 | 1.70 | 1.46 | 1.98 |
| Females | ||||||||||||||||||
| <18 | 0.05 | 0.07 | 0.00 | . | . | 0.10 | 0.54 | 0.07 | 3.93 | 0.38 | 0.07 | 2.34 | 0.88 | 6.19 | 0.10 | 0.67 | 0.17 | 2.74 |
| 18-<35 | 0.12 | 0.26 | 1.59 | 1.05 | 2.43 | 0.12 | 1.38 | 0.80 | 2.37 | 0.29 | 0.26 | 1.73 | 1.36 | 2.19 | 0.12 | 1.93 | 1.49 | 2.50 |
| 35-<50 | 0.23 | 0.53 | 1.31 | 1.08 | 1.59 | 0.30 | 1.45 | 1.21 | 1.75 | 0.34 | 0.53 | 1.66 | 1.43 | 1.93 | 0.30 | 1.65 | 1.44 | 1.89 |
| 50-<65 | 0.44 | 0.73 | 1.02 | 0.90 | 1.16 | 0.36 | 1.04 | 0.92 | 1.17 | 0.36 | 0.73 | 1.54 | 1.29 | 1.84 | 0.36 | 1.49 | 1.30 | 1.69 |
| 65+ | 0.48 | 0.77 | 1.31 | 1.07 | 1.59 | 0.31 | 1.23 | 1.07 | 1.42 | 0.32 | 0.77 | 1.56 | 1.17 | 2.07 | 0.31 | 1.66 | 1.37 | 2.01 |
| All | 1.76 | 1.64 | 1.88 | 1.42 | 1.33 | 1.52 | 1.56 | 1.48 | 1.64 | 1.65 | 1.58 | 1.74 | ||||||
| M-H p-value | p=0.004 | p=0.007 | p=0.963 | p=0.785 | ||||||||||||||
| High TAG (>150 mg/L) | Atherogenic Dyslipidemia (AD=High TAG and low HDL) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| High WHtR | Overweight | High WHtR | Overweight | |||||||||||||||
| High TAG(prop) | High WHtR (prop) | PR | 95% CI | OW (prop) | PR | 95% CI | AD (prop) | High WHtR (prop) | PR | 95% CI | OW (prop) | PR | 95% CI | |||||
| Males | ||||||||||||||||||
| <18 | 0.10 | 0.12 | 2.68 | 1.47 | 4.86 | 0.12 | 2.49 | 1.34 | 4.61 | 0.03 | 0.12 | 3.57 | 1.27 | 10.03 | 0.12 | 3.74 | 1.32 | 10.49 |
| 18-<35 | 0.32 | 0.33 | 1.92 | 1.54 | 2.40 | 0.23 | 1.85 | 1.49 | 2.31 | 0.25 | 0.33 | 2.29 | 1.75 | 2.99 | 0.23 | 2.38 | 1.84 | 3.08 |
| 35-<50 | 0.42 | 0.53 | 2.06 | 1.77 | 2.38 | 0.34 | 1.91 | 1.69 | 2.16 | 0.30 | 0.53 | 2.38 | 1.96 | 2.89 | 0.34 | 2.48 | 2.10 | 2.92 |
| 50-<65 | 0.35 | 0.57 | 2.01 | 1.69 | 2.38 | 0.29 | 1.79 | 1.56 | 2.06 | 0.23 | 0.57 | 2.26 | 1.79 | 2.86 | 0.29 | 2.18 | 1.80 | 2.64 |
| 65+ | 0.27 | 0.60 | 2.02 | 1.52 | 2.68 | 0.26 | 1.73 | 1.37 | 2.19 | 0.20 | 0.60 | 2.40 | 1.67 | 3.45 | 0.26 | 2.07 | 1.56 | 2.75 |
| Females | ||||||||||||||||||
| <18 | 0.09 | 0.07 | 0.94 | 0.24 | 3.69 | 0.10 | 1.27 | 0.47 | 3.39 | 0.06 | 0.07 | 2.01 | 0.25 | 15.66 | 0.10 | 1.15 | 0.15 | 8.89 |
| 18-<35 | 0.12 | 0.26 | 2.01 | 1.33 | 3.03 | 0.12 | 2.73 | 1.77 | 4.20 | 0.06 | 0.26 | 2.67 | 1.48 | 4.80 | 0.12 | 3.60 | 1.98 | 6.54 |
| 35-<50 | 0.24 | 0.53 | 2.18 | 1.78 | 2.67 | 0.30 | 2.06 | 1.72 | 2.45 | 0.15 | 0.53 | 2.52 | 1.89 | 3.35 | 0.30 | 2.20 | 1.73 | 2.80 |
| 50-<65 | 0.38 | 0.73 | 1.71 | 1.43 | 2.05 | 0.36 | 1.69 | 1.50 | 1.92 | 0.22 | 0.73 | 2.16 | 1.64 | 2.86 | 0.36 | 1.87 | 1.55 | 2.24 |
| 65+ | 0.36 | 0.77 | 1.80 | 1.36 | 2.39 | 0.31 | 1.81 | 1.52 | 2.16 | 0.20 | 0.77 | 1.89 | 1.24 | 2.87 | 0.31 | 2.39 | 1.83 | 3.12 |
| All | 2.24 | 2.08 | 2.40 | 2.04 | 1.93 | 2.17 | 2.54 | 2.31 | 2.80 | 2.46 | 2.27 | 2.66 | ||||||
| M-H p-value | p=0.716 | p=0.010 | p=0.914 | p=0.276 | ||||||||||||||
| High CRP (>3mg/L, < 10 mgL)) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| High WHtR | Overweight | ||||||||
| High CRP (prop) | High WHtR (prop) | PR | 95% CI | OW (prop) | PR | 95% CI | |||
| Males | |||||||||
| <18 | 0.06 | 0.12 | 4.90 | 2.33 | 10.29 | 0.12 | 2.32 | 0.97 | 5.54 |
| 18-35 | 0.09 | 0.33 | 1.68 | 1.01 | 2.82 | 0.23 | 2.01 | 1.20 | 3.36 |
| 35-50 | 0.12 | 0.53 | 2.04 | 1.46 | 2.84 | 0.34 | 1.85 | 1.37 | 2.50 |
| 50-65 | 0.13 | 0.57 | 1.44 | 1.08 | 1.93 | 0.29 | 1.11 | 0.83 | 1.49 |
| 65+ | 0.19 | 0.60 | 1.15 | 0.83 | 1.59 | 0.26 | 1.50 | 1.10 | 2.06 |
| Females | |||||||||
| <18 | 0.03 | 0.07 | 0.00 | . | . | 0.10 | 2.05 | 0.46 | 9.11 |
| 18-35 | 0.08 | 0.26 | 2.74 | 1.63 | 4.61 | 0.12 | 3.52 | 2.08 | 5.94 |
| 35-50 | 0.10 | 0.53 | 2.48 | 1.73 | 3.57 | 0.30 | 2.29 | 1.68 | 3.12 |
| 50-65 | 0.17 | 0.73 | 1.97 | 1.43 | 2.71 | 0.36 | 2.02 | 1.62 | 2.53 |
| 65+ | 0.24 | 0.77 | 1.52 | 1.07 | 2.16 | 0.31 | 1.84 | 1.44 | 2.35 |
| All | 2.19 | 1.95 | 2.47 | 1.96 | 1.76 | 2.17 | |||
| M-H p-value | p=0.0043 | p=0.0096 | |||||||
Figure 1. Prevalence of selected cardiometabolic factors, by age, China 2009.
Prevalence ratios for CM risk factors in relation to WHtR and overweight (table 1)
Prevalence ratios for high blood pressure and impaired HbA1c (pre-diabetic or diabetic) were heterogeneous across age and sex, and were higher in young to middle aged adults (<50yr) compared to the older age groups. On average, prevalence ratios for high blood pressure were doubled for those with high versus normal WHtR, and 1.65 times greater for overweight compared to normal weight individuals. For pre-diabetes and diabetes, prevalence ratios were more than doubled for those with high WHtR, and 1.8 times higher for overweight compared to normal weight, with significant heterogeneity across age and sex groups. The prevalence ratio for diabetes was 3.8 for high WHtR and 2.7 for overweight. Insulin resistance, indicated by high HOMA-IR, was 2-3 times more prevalent in those with overweight or high WHtR with no significant heterogeneity across age and sex groups.
Markers of dyslipidemia showed a similar pattern. High LDL was nearly 1.8 times more prevalent in those with high WHtR and 1.4 times more prevalent in overweight individuals. These prevalence ratios for high LDL were heterogeneous across age and sex groups with no consistent pattern. In contrast, low HDL was about 1.6 times more prevalent with high WHtR or overweight, and prevalence ratios were similar across age and sex groups. High TAG was about twice as prevalent with high WHtR or overweight in males and females, with higher prevalence ratios in those < 50 yr versus ≥ 50 yr. Atherogenic dyslipidemia was about 2.5 times more prevalent with high WHtR or high overweight and was similar across all age and sex groups. Prevalence ratios for CRP varied substantially among age and sex groups, but the overall prevalence ratio was doubled for high WHtR and overweight.
Correlates of Adverse CM Risk Factors
Associations with dietary fat and physical activity (Table 2)
Table 2.
Logistic regression models of CM risk factors as outcomes: Odds Rations and 95% Confidence Intervals for associations with diet and physical activity variables, adjusted for age, household income, urbanicity, and education level, and clustering of multiple individuals within households, adults CHNS 2009.
| Overweight | High WHtR | High Blood Pressure | HbA1c≥5.7% | Diabetic | High HOMA-IR | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | Males | Females | Males | Females | Males | Females | |
| % Fat1 | 1.04 | 1.01 | 1.04 | 1.02 | 0.97 | 1.03 | 0.97 | 0.93* | 1.11 | 1.11 | 0.93 | 1.07 |
| [0.96,1.12] | [0.94,1.08] | [0.97,1.11] | [0.95,1.09] | [0.90,1.04] | [0.97,1.11] | [0.90,1.04] | [0.87,1.00] | [0.98,1.26] | [0.99,1.25] | [0.85,1.03] | [0.98,1.17] | |
| % Protein1 | 1.65*** | 1.08 | 1.58*** | 1.13 | 1.03 | 1.07 | 1.26 | 1.42** | 1.30 | 1.19 | 1.31 | 1.64** |
| [1.26,2.17] | [0.85,1.39] | [1.21,2.06] | [0.88,1.46] | [0.80,1.34] | [0.82,1.38] | [0.96,1.65] | [1.10,1.82] | [0.85,1.98] | [0.77,1.84] | [0.95,1.80] | [1.22,2.22] | |
| PA Q2 | 0.93 | 1.04 | 0.82 | 0.97 | 0.96 | 0.91 | 0.86 | 0.88 | 0.79 | 1.14 | 1.02 | 0.76* |
| [0.73,1.18] | [0.85,1.28] | [0.65,1.04] | [0.78,1.20] | [0.76,1.20] | [0.74,1.12] | [0.68,1.09] | [0.72,1.08] | [0.54,1.15] | [0.84,1.54] | [0.77,1.36] | [0.59,0.98] | |
| PA Q3 | 0.96 | 0.75* | 0.90 | 0.73** | 0.9 | 0.71** | 0.96 | 0.68** | 0.73 | 0.61* | 0.79 | 0.68** |
| [0.76,1.21] | [0.59,0.96] | [0.72,1.13] | [0.57,0.92] | [0.72,1.13] | [0.56,0.90] | [0.75,1.22] | [0.54,0.87] | [0.48,1.10] | [0.40,0.95] | [0.58,1.06] | [0.51,0.91] | |
| PA Q4 | 0.86 | 0.78 | 0.73** | 0.76* | 0.78* | 0.79 | 0.71** | 0.63*** | 0.59* | 0.61* | 0.88 | 0.65** |
| [0.68,1.09] | [0.61,1.01] | [0.59,0.91] | [0.59,0.97] | [0.62,0.98] | [0.61,1.02] | [0.56,0.90] | [0.49,0.81] | [0.38,0.91] | [0.38,0.98] | [0.66,1.18] | [0.48,0.89] | |
| PA Q5 | 0.69** | 0.76* | 0.61*** | 0.77* | 0.65*** | 0.84 | 0.78 | 0.79 | 0.64 | 0.77 | 0.84 | 0.56*** |
| [0.52,0.90] | [0.59,0.98] | [0.48,0.78] | [0.60,0.99] | [0.51,0.83] | [0.66,1.08] | [0.60,1.01] | [0.61,1.01] | [0.41,1.01] | [0.50,1.19] | [0.60,1.18] | [0.41,0.77] | |
| High LDL | Low HDL | High TAG | Atherogenic Dyslipidemia | High CRP | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | Males | Females | Males | Females | |||
| %Fat1 | 1.04 | 1.10** | 1.07* | 0.96 | 1.01 | 1.07* | 1.06 | 1.04 | 1.08 | 1.10* | ||
| [0.96,1.12] | [1.03,1.18] | [1.00,1.14] | [0.90,1.02] | [0.94,1.09] | [1.00,1.15] | [0.98,1.14] | [0.96,1.13] | [0.98,1.19] | [1.01,1.19] | |||
| %Protein1 | 1.13 | 1.41** | 1.14 | 0.88 | 1.27 | 1.13 | 1.40* | 1.05 | 1.21 | 1.03 | ||
| [0.86,1.49] | [1.10,1.80] | [0.89,1.47] | [0.69,1.13] | [0.98,1.65] | [0.88,1.46] | [1.05,1.86] | [0.78,1.42] | [0.84,1.74] | [0.76,1.41] | |||
| PA Q2 | 1.04 | 0.97 | 1.00 | 1.06 | 0.94 | 1.05 | 0.89 | 1.10 | 1.02 | 0.99 | ||
| [0.82,1.32] | [0.79,1.19] | [0.80,1.25] | [0.87,1.30] | [0.75,1.19] | [0.86,1.29] | [0.69,1.14] | [0.86,1.41] | [0.75,1.39] | [0.77,1.28] | |||
| PA Q3 | 0.94 | 1.05 | 0.88 | 0.93 | 0.97 | 0.77* | 0.87 | 0.76 | 0.94 | 0.83 | ||
| [0.74,1.19] | [0.84,1.33] | [0.71,1.10] | [0.74,1.16] | [0.77,1.22] | [0.60,0.97] | [0.68,1.12] | [0.57,1.03] | [0.69,1.29] | [0.61,1.12] | |||
| PA Q4 | 0.79 | 0.94 | 0.85 | 0.88 | 0.80 | 0.67** | 0.8 | 0.70* | 0.80 | 0.71* | ||
| [0.62,1.01] | [0.73,1.21] | [0.68,1.06] | [0.69,1.11] | [0.63,1.01] | [0.52,0.86] | [0.62,1.03] | [0.52,0.95] | [0.58,1.10] | [0.51,0.98] | |||
| PA Q5 | 0.87 | 0.87 | 0.56*** | 0.71** | 0.72* | 0.73* | 0.57*** | 0.64** | 0.70* | 0.55*** | ||
| [0.67,1.14] | [0.68,1.12] | [0.44,0.72] | [0.56,0.91] | [0.56,0.94] | [0.57,0.94] | [0.43,0.77] | [0.47,0.86] | [0.49,0.99] | [0.39,0.76] | |||
Percentage of energy from fat or percentage of energy from protein, scaled so that coefficients represent a change of 10 percentage points in the exposure
P<0.05
P<0.01
P<0.001
The main dietary exposures were macronutrient densities. Alternate models examined the percentage of calories from fat alone or with the percentage of calories from protein, adjusting for total energy intake. Consuming a higher percentage of calories from fat was positively associated with an increased likelihood of having high LDL, high TAG, and high CRP in females only and with having low HDL in males. A higher percentage of energy intake from protein, adjusted for the percentage of calories from fat, was associated with increased risk of overweight, high WHtR, and atherogenic dyslipidemia in males and impaired HbA1c, high HOMA-IR, and high LDL in females. For example, an increase of 10 percentage points in energy intake from fat (consistent with the increase between 1991 and 2011 from 22% to 32% of energy intake from fat reported by Barry M. Popkin in this issue) is related to an 8% increase in the likelihood of having high LDL among females. A 1 percentage point increase in the percentage of calories from protein (consistent with the increase between 1991 and 2011 from 12% to 13%) was associated with a 4% increase in risk of high LDL in females or of having atherogenic dyslipidemia in males.
Physical activity was inversely associated with all adverse outcomes and showed a clear dose response with most outcomes, with risk being reduced in the highest compared to the lowest quintile by 30–45%. Higher physical activity was similarly associated with lower CM risk in males and females.
Associations with high WHtR and overweight (Table 3)
Table 3. Likelihood of having CM risk factors in relation to weight status (Overweight, OW=BMI≥25 kg/m2) and high waist to height ratio (WHtR>0.50): Odds ratios and 95% confidence intervals from logistic regression models adjusted for age, education, urbanicity, income, clustering of multiple individuals within households, CHNS 2009.
| Impaired HbA1c | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| High BP | (>5.6%) | Diabetic HbA1c (>6.5%) | High HOMA-IR | High CRP (>3, <10) | ||||||||||||
| Males | Females | Males | Females | Males | Females | Males | Females | Males | Females | |||||||
| High WHtR | OR | 1.47*** | 1.79*** | 1.82*** | 1.59*** | 2.17*** | 2.25*** | 1.85*** | 1.72*** | 1.43** | 1.64*** | |||||
| 95% CI | [1.24,1.73] | [1.50,2.13] | [1.52,2.19] | [1.32,1.91] | [1.52,3.10] | [1.55,3.28] | [1.43,2.39] | [1.35,2.21] | [1.12,1.83] | [1.27,2.11] | ||||||
| OW | OR | 1.36 | 1.34 | 2.36*** | 2.21** | 2.32* | 4.59*** | 2.23** | 3.51*** | 1.14 | 2.50** | |||||
| 95% CI | [0.88,2.09] | [0.78,2.31] | [1.52,3.67] | [1.31,3.74] | [1.08,5.00] | [2.07,10.20] | [1.30,3.84] | [1.98,6.21] | [0.60,2.16] | [1.31,4.78] | ||||||
| OW + High WHtR | OR | 3.16*** | 3.16*** | 2.87*** | 3.42*** | 4.28*** | 3.94*** | 4.69*** | 3.76*** | 1.91*** | 3.26*** | |||||
| 95% CI | [2.66,3.74] | [2.64,3.79] | [2.40,3.43] | [2.86,4.09] | [3.09,5.93] | [2.74,5.66] | [3.74,5.88] | [2.98,4.74] | [1.52,2.41] | [2.55,4.16] | ||||||
| N | 3936 | 4406 | 3901 | 4385 | 3903 | 4388 | 3733 | 4231 | 3776 | 4282 | ||||||
| High LDL | Low HDL | High TAG | Atherogenic dyslipidemia | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | Males | Females | |||||||||
| High WHtR | OR | 1.54*** | 1.24* | 1.76*** | 1.58*** | 2.46*** | 1.79*** | 2.29*** | 2.03*** | |||||||
| 95% CI | [1.28,1.85] | [1.04,1.47] | [1.48,2.08] | [1.33,1.88] | [2.05,2.95] | [1.48,2.15] | [1.86,2.82] | [1.59,2.58] | ||||||||
| OW | OR | 1.41 | 1.53 | 2.64*** | 1.97** | 3.49*** | 2.93*** | 3.88*** | 3.37*** | |||||||
| 95% CI | [0.91,2.18] | [0.90,2.59] | [1.73,4.04] | [1.19,3.26] | [2.30,5.28] | [1.74,4.94] | [2.54,5.92] | [1.86,6.09] | ||||||||
| OW + High WHtR | OR | 1.66*** | 1.51*** | 3.52*** | 2.70*** | 3.87*** | 3.61*** | 4.50*** | 3.88*** | |||||||
| 95% CI | [1.38,1.99] | [1.27,1.80] | [2.97,4.18] | [2.27,3.20] | [3.24,4.63] | [3.01,4.34] | [3.69,5.48] | [3.09,4.87] | ||||||||
| N | 3740 | 4237 | 3746 | 4239 | 3750 | 4241 | 3746 | 4239 | ||||||||
In sex-stratified logistic regression models adjusted for age, income, urbanicity, and education, we compared the odds of having a CM risk factor in those who had high WHtR only, overweight only, and overweight plus high WHtR to those with neither condition. Overweight alone was not related to high blood pressure or high LDL. In contrast, high WHtR significantly predicted all CM risk factors. The combination of overweight and high WHtR was a particularly powerful predictor of outcomes related to glucose control. The combination of these two risk factors was associated with a three to five times greater likelihood of elevated HbA1c, diabetes, and insulin resistance. There was not a marked synergism of WHtR and overweight for LDL compared to measures of glucose control. High WHtR and overweight were each independently associated with low HDL, high TAG, and atherogenic dyslipidemia, with synergistic effects of weight status and central obesity demonstrated by much higher odds ratios for males and females with both conditions.
Discussion
The high prevalence of CM risk factors even among youths and young adults portends high morbidity and mortality from diabetes and cardiovascular disease in China. Estimated prevalence rates from the CHNS are comparable to those from several other large population-based studies in China,18, 33 and the results emphasize the need for early life prevention and intervention. Currently 80% of diabetes deaths occur in low- and middle-income countries,34and China has experienced recent, rapid increases in diabetes and other CM diseases.35-38 There are clear disparities in diabetes39-41 and other noncommunicable diseases by sociodemographic and urbanization-related factors18, 42 across China.
Most of the risk is hidden, because owing to inadequate screening more than half of the high blood pressure and diabetes risk indicated by the measurements included in the CHNS was undiagnosed or unrecognized by participants.43 This poses particular challenges and high costs for an overburdened health care system.44
Our work has important implications for intervention. Higher levels of physical activity were quite consistently associated with reduced prevalence of CM risk factors. Another paper in this issue shows clearly that occupation and domestic activities are by far the largest contributors to physical activity among adults, and these types of activity decreased significantly between 1991 and 2011.45 Moreover reduction in physical activity has important implications for weight gain, as shown in prior longitudinal analyses of the CHNS.6 As occupational physical activity declines with increased technological development,46 it becomes even more important to increase leisure time physical activity to promote good health.
Similarly dietary trends have important implications for CM diseases. The percentage of calories from fat in the diet increased from 22% in 1991 to 32% in 2011. We showed that this level of change was associated with an 8% increase in the likelihood of having high LDL in women. Given that younger, more urban females have higher fat intakes, this finding has important implications. In general our observed associations with diet were weaker than those reported in another large national study in 2002 in China that collected dietary data using a food frequency questionnaire.47 For hypertension, sodium intake may be especially important. Recently Du and colleagues48 noted high risks associated with sodium and the sodium-potassium ratio, a critical issue, since by age 50 about half of the adults in the CHNS had raised blood pressures.
The increases in the prevalence of overweight and obesity and in particular the increases in abdominal obesity in China have very strong implications for CM diseases. We showed that the prevalence ratios for many CM risk factors were nearly doubled for overweight individuals and especially for those with abdominal obesity marked by high WHTR. The higher prevalence ratio for younger participants suggests that the CM risks of overweight are even greater for younger individuals, even though the prevalence of risk in this age group is lower than that among older participants. Again this emphasizes the importance of early obesity prevention. A recent paper by our group has shown dramatic increases in waist circumference over the past two decades in China and also a higher waist circumference–BMI ratio over this period at all BMI levels.49 The risks associated with high waist circumference11, 50 and the synergistic effects of overweight and high waist circumference51 are well-known from other large studies in China. We found that the risk of diabetes, insulin resistance, and atherogenic dyslipidemia was about four times greater among overweight adults with a WHtR compared to those with neither risk factor. Overweight alone, even using a BMI cutpoint of 25 kg/m2 was not significantly associated with risk of elevated blood pressure or high LDL. Given the small number of youths with adverse CM outcomes in each exposure category, we were not able to estimate comparable models for youths.
The present analysis has several limitations that will be addressed by future work with this important sample. We currently have only one round of biomarker data, precluding analysis of risk incidence. However, a future round of data collection is anticipated. In our analysis of diet we focused only on macronutrient densities. A high percentage of energy intake from fat can reflect intake of atherogenic as well as healthy fats. Across all levels of percentages of energy intake from fat, about 60% came from plant sources and 40% from animal sources. Future work will examine fat and carbohydrate compositions of the diet to identify specific atherogenic components.
Despite these limitations our work on the prevalence of CM risk in this population clearly demonstrates the health consequences of China's rapid nutrition transition. At the same time it identifies possible avenues for prevention in the future.
Acknowledgments
This work was supported by the National Institutes of Health (NIH): NHLBI (R01-HL108427). The NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, and approval of the manuscript. This research uses data from the CHNS, funded by NIH: NICHD (R01-HD30880), although no direct support was received from the grant for this analysis. We also are grateful to the Carolina Population Center (R24 HD050924) for general support. We thank Ms. Frances Dancy, BS, University of North Carolina at Chapel Hill Carolina Population Center, for her helpful administrative assistance; and Jim Terry, AB; Guifeng Jin, PhD; and Phil Bardsley, PhD, for programming and technical support.
Abbreviations
- CM
cardiometabolic
- BMI
body mass index
- CHNS
China Health and Nutrition Survey
- HbA1c
glycated hemoglobin
- CRP
C-reactive protein
- WHtR
waist to height ratio
- BP
blood pressure
- TAG
triacylglycerol
- LDL
low-density lipoprotein cholesterol
- HDL
high-density lipoprotein cholesterol
- AD
atherogenic dyslipidemia
- HOMA-IR
homeostasis model of assessment–insulin resistance
- MET
metabolic equivalent
Footnotes
Conflict of Interest: The authors declare no conflict of interest. None of the individuals acknowledged received compensation for any role in the study.
References
- 1.Jones-Smith JC, Gordon-Larsen P, Siddiqi A, Popkin BM. Cross-national comparisons of time trends in overweight inequality by socioeconomic status among women using repeated cross-sectional surveys from 37 developing countries, 1989-2007. Am J Epidemiol. 2011;173:667–75. doi: 10.1093/aje/kwq428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Doak C, Adair L, Bentley M, Fengying Z, Popkin B. The underweight/overweight household: an exploration of household sociodemographic and dietary factors in China. Public Health Nutr. 2002;5:215–21. doi: 10.1079/PHN2001296. [DOI] [PubMed] [Google Scholar]
- 3.Doak CM, Adair LS, Monteiro C, Popkin BM. Overweight and underweight coexist within households in Brazil, China and Russia. J Nutr. 2000;130:2965–71. doi: 10.1093/jn/130.12.2965. [DOI] [PubMed] [Google Scholar]
- 4.Dearth-Wesley T, Wang H, Popkin B. Under- and overnutrition dynamics in Chinese children and adults (1991–2004) Eur J Clin Nutr. 2008;62:1302–07. doi: 10.1038/sj.ejcn.1602853. [DOI] [PubMed] [Google Scholar]
- 5.Wang H, Du S, Zhai F, Popkin BM. Trends in the distribution of body mass index among Chinese adults, aged 20-45 years (1989-2000) Int J Obes. 2006;31:272–78. doi: 10.1038/sj.ijo.0803416. [DOI] [PubMed] [Google Scholar]
- 6.Monda KL, Adair LS, Zhai F, Popkin BM. Longitudinal relationships between occupational and domestic physical activity patterns and body weight in China. Eur J Clin Nutr. 2008;62 doi: 10.1038/sj.ejcn.1602849. [DOI] [PubMed] [Google Scholar]
- 7.Stern D, Smith L, Zhang B, Gordon-Larsen P, Popkin B. Changes in waist circumference relative to body mass index in Chinese adults, 1991 to 2009. doi: 10.1038/ijo.2014.74. In Progress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health OrganisationInternational Association for the Study of Obesity International Obesity Task Force. The Asia-Pacific perspective: redefining obesity and its treatment. Health Communications; Sydney: 2000. pp. 1–56. [Google Scholar]
- 9.Li G, Chen X, Jang Y, et al. Obesity, coronary heart disease risk factors and diabetes in Chinese: an approach to the criteria of obesity in the Chinese population. Obes Rev. 2002;3:167–72. doi: 10.1046/j.1467-789x.2002.00067.x. [DOI] [PubMed] [Google Scholar]
- 10.Tuan NT, Adair LS, Stevens J, Popkin BM. Prediction of hypertension by different anthropometric indices in adults: the change in estimate approach. Public Health Nutr. 2010;13:639–46. doi: 10.1017/S1368980009991479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gordon-Larsen P, Adair LS, Meigs JB, et al. Discordant risk: Overweight and cardiometabolic risk in Chinese adults. Obesity. 2012 doi: 10.1038/oby.2012.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang X, Shu XO, Gao YT, Yang G, Li H, Zheng W. General and abdominal adiposity and risk of stroke in Chinese Women. Stroke. 2009;40:1098–104. doi: 10.1161/STROKEAHA.108.539692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jia Z, Zhou Y, Liu X, et al. Comparison of different anthropometric measures as predictors of diabetes incidence in a Chinese population. Diabetes Res Clin Practice. 2011;92:265–71. doi: 10.1016/j.diabres.2011.01.021. [DOI] [PubMed] [Google Scholar]
- 14.Deurenberg P, Deurenberg-Yap M, Guricci S. Asian are different from Caucasians and from each other in their body mass index/body fat percent relationship. Obes Rev. 2002;3:141–46. doi: 10.1046/j.1467-789x.2002.00065.x. [DOI] [PubMed] [Google Scholar]
- 15.Deurenberg-Yap M, Chew SK, Deurenberg P. Elevated body fat percentage and cardiovascular risks at low body mass index levels among Singaporean Chinese, Malays and Indians. Obes Rev. 2002;2:209–15. doi: 10.1046/j.1467-789x.2002.00069.x. [DOI] [PubMed] [Google Scholar]
- 16.Hu FB. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care. 2011;34:1249–57. doi: 10.2337/dc11-0442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoon KH, Lee JH, Kim JW, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–88. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 18.Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:1090–101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 19.Popkin BM. Will China's nutrition transition overwhelm its health care system and slow economic growth. Health Aff (Millwood) 2008;27:1064–76. doi: 10.1377/hlthaff.27.4.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.He J, Gu D, Wu X, et al. Major causes of death among men and women in China. N Engl J Med. 2005;353:1124–34. doi: 10.1056/NEJMsa050467. [DOI] [PubMed] [Google Scholar]
- 21.Bell AC, Ge K, Popkin BM. Weight gain and its predictors in Chinese adults. Int J Obes Relat Metab Disord. 2001;25:1079–86. doi: 10.1038/sj.ijo.0801651. [DOI] [PubMed] [Google Scholar]
- 22.Fang C, Beghin J. Urban household oil and fats demand in China: Evidence from urban household survey data. J Comparative Econ. 2002;30:732–53. [Google Scholar]
- 23.Ng SW, Zhai F, Popkin BM. Impacts of China's edible oil pricing policy on nutrition. Soc Sci Med. 2008;66:414–26. doi: 10.1016/j.socscimed.2007.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yan S, Li J, Li S, et al. The expanding burden of cardiometabolic risk in China: the China Health and Nutrition Survey. Obes Rev. 2012;13:810–21. doi: 10.1111/j.1467-789X.2012.01016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mi SQ, Yin P, Hu N, et al. BMI, WC, WHtR, VFI and BFI: Which Indictor is the most efficient screening Index on type 2 diabetes in Chinese community population. Biomed Environ Sci. 2013;26:485–91. doi: 10.3967/0895-3988.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 27.International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome. 2006 http://www.idf.org/webdata/docs/MetS_def_update2006.pdf:
- 28.Silventoinen K, Sarlio-Lahteenkorva S, Koskenvuo M, Lahelma E, Kaprio J. Effect of environmental and genetic factors on education-associated disparities in weight and weight gain: a study of Finnish adult twins. Am J Clin Nutr. 2004;80:815–22. doi: 10.1093/ajcn/80.4.815. [DOI] [PubMed] [Google Scholar]
- 29.Popkin BM, Lu B, Zhai F. Understanding the nutrition transition: measuring rapid dietary changes in transitional countries. Public Health Nutr. 2002;5:947–53. doi: 10.1079/PHN2002370. [DOI] [PubMed] [Google Scholar]
- 30.Zhai F, Guo X, Popkin B, et al. Evaluation of the 24-hour individual recall method in China. Food Nutr Bull. 1996;17:154–61. [Google Scholar]
- 31.Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev. 2012 doi: 10.1111/j.1467-789X.2011.00982.x. no-no. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jones-Smith JC, Popkin BM. Understanding community context and adult health changes in China: development of an urbanicity scale. Soc Sci Med. 2010;71:1436–46. doi: 10.1016/j.socscimed.2010.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li H, Oldenburg B, Chamberlain C, et al. Diabetes prevalence and determinants in adults in China mainland from 2000 to 2010: a systematic review. Diabetes Res Clin Pract. 2012;98:226–35. doi: 10.1016/j.diabres.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization, editor. WHO. The Global Status Report on Noncommunicable Diseases 2010 Editors: World Health Organization. 2011. p. 176. [Google Scholar]
- 35.Lee CM, Huxley RR, Lam TH, et al. Prevalence of diabetes mellitus and population attributable fractions for coronary heart disease and stroke mortality in the WHO South-East Asia and Western Pacific regions. Asia Pac J Clin Nutr. 2007;16:187–92. [PubMed] [Google Scholar]
- 36.Gu D, Gupta A, Muntner P, et al. Prevalence of cardiovascular disease risk factor clustering among the adult population of China: results from the International Collaborative Study of Cardiovascular Disease in Asia (InterAsia) Circulation. 2005;112:658–65. doi: 10.1161/CIRCULATIONAHA.104.515072. [DOI] [PubMed] [Google Scholar]
- 37.Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:1090–101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 38.Gu D, Reynolds K, Wu X, et al. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet. 2005;365:1398–405. doi: 10.1016/S0140-6736(05)66375-1. [DOI] [PubMed] [Google Scholar]
- 39.Zhang X, Kanbur R. Spatial inequality in education and health care in China. China Econ Rev. 2005;16:189–204. [Google Scholar]
- 40.Zheng X, Song X, Chen G, et al. Health inequalities during 20 years of rapid economic development in China (1980-2000): A mortality analysis. Biomed Environ Sci. 2011;24:329–34. doi: 10.3967/0895-3988.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 41.Tang S, Meng Q, Chen L, Bekedam H, Evans T, Whitehead M. Tackling the challenges to health equity in China. Lancet. 2008;372:1493–501. doi: 10.1016/S0140-6736(08)61364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wagner KH, Brath H. A global view on the development of non communicable diseases. Prev Med. 2012;54:38–41. doi: 10.1016/j.ypmed.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 43.Attard S, Herring A, Mayer-Davis E, Popkin B, Meigs J, Gordon-Larsen P. Multilevel examination of diabetes in modernising China: what elements of urbanisation are most associated with diabetes. Diabetologia. 2012;55:3182–92. doi: 10.1007/s00125-012-2697-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yang W, Zhao W, Xiao J, et al. Medical care and payment for diabetes in China: enormous threat and great opportunity. PLoS One. 2012;7:e39513. doi: 10.1371/journal.pone.0039513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ng S, Wang H, Green-Howard A, Su C, Zhang B. The physical activity transition in China: 1989-2011. Obes Rev. 2013 doi: 10.1111/obr.12127. TBD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Monda KL, Gordon-Larsen P, Stevens J, Popkin BM. China's transition: the effect of rapid urbanization on adult occupational physical activity. Soc Sci Med. 2007;64:858–70. doi: 10.1016/j.socscimed.2006.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen CM, Zhao W, Yang Z, Zhai Y, Wu Y, Kong L. The role of dietary factors in chronic disease control in China. Obes Rev. 2008;9(Suppl 1):100–3. doi: 10.1111/j.1467-789X.2007.00448.x. [DOI] [PubMed] [Google Scholar]
- 48.Du S, Nieman A, Batis C, et al. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their impact on hypertension in China. Am J Clin Nutr. 2013 doi: 10.3945/ajcn.113.059121. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stern D, Smith, Lindsey P, Zhang Bing, Gordon-Larsen Popkin, Barry M. Changes in waist circumfrence relative to BMI in China adults from 1993 to 2009. University of North Carolina at Chapel Hill. 2013 [Google Scholar]
- 50.Zhang ZQ, Deng J, He LP, Ling WH, Su YX, Chen YM. Comparison of various anthropometric and body fat indices in identifying cardiometabolic disturbances in chinese men and women. PLoS One. 2013;8:e70893. doi: 10.1371/journal.pone.0070893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hou X, Lu J, Weng J, et al. Impact of waist circumference and body mass index on risk of cardiometabolic disorder and cardiovascular disease in Chinese adults: a national diabetes and metabolic disorders survey. PLoS One. 2013;8:e57319. doi: 10.1371/journal.pone.0057319. [DOI] [PMC free article] [PubMed] [Google Scholar]


