Abstract
Objective
To describe the prevalence of and risk factors for depression in a high-risk population of mothers of ill newborns in Ghana.
Methods
Semi-structured interviews were conducted with women who had a hospitalized newborn at a tertiary teaching hospital in Kumasi, Ghana. Surveys included information on maternal demographics, pregnancy and delivery, interpersonal violence, and social support. Postpartum depression was measured with the Patient Health Questionnaire (PHQ)-9. Bivariable analysis was conducted using analysis of variance, χ2, and Fisher exact tests; multivariable analysis was performed using multinomial logistic regression.
Results
In total, 153 women completed the survey. Fifty (32.7%) had PHQ-9 scores of 5–9, indicating mild depression; 42 (27.4%) had PHQ-9 scores of 10–14, indicating moderate depression; and 15 (9.8%) had scores of 15 or higher, indicative of moderate/severe depression. History of interpersonal violence with current partner predicted depression.
Conclusion
Mothers of sick infants in Ghana are at high risk for symptoms of clinical depression. This is of critical importance because maternal depression affects infant health outcomes and may be particularly important for mothers of sick infants.
Keywords: Ghana, Infant health, Interpersonal violence, Mental health, Postpartum depression
1. Introduction
Pregnancy and the postpartum period are vulnerable times for maternal mental health, with up to 15% of postpartum women in high-income nations experiencing a mood disorder within the previous year and probably a higher rate in low-income nations [1,2]. In general, studies in Africa indicate that rates of depression during pregnancy and the postpartum period are significantly higher and may have longer duration than in high-income countries; the prevalence of postpartum depression in low-income countries ranges from 14% to 50%, depending on the measure and criteria used [3]. A 2010 systematic review of psychological wellbeing in Africa reported a mean prevalence of postpartum depression of 18% among all of the studies reviewed [4]. Mothers of sick, preterm, and low birth weight infants are at even greater risk of perinatal mental illness—including depression, acute stress disorder, and post-traumatic stress disorder—according to studies in high-income countries and a few small studies in Africa [5–7].
Although it is clear that psychiatric disorders cause a significant burden on affected mothers, there is growing evidence that there are also significantly higher risks for the infants of depressed women, ranging from low birth weight, spontaneous abortion, stillbirth, and preterm delivery to reductions in breastfeeding, infant sleep and behavior disorders, and attachment problems [8,9]. In low- and middle-income nations, maternal depression has also been associated with higher prevalence of poor infant nutritional status, diarrhea, and respiratory illness, in addition to putting children at approximately twice the risk of childhood underweight and growth stunting; all of these issues put young children at significant health risk [2,3,10–13].
Ghana is a country in West Africa with a population of approximately 24 million. There are high rates of both maternal mortality (451 per 100 000 live births) and childhood (under-5) mortality (8 per 100 live births) [14]. According to WHO, only 1% of patients with mental disorders receive any form of psychiatric care in Ghana [15]. We were able to identify only 2 published studies of postpartum depression in Ghana. One compared 3 screening instruments for postpartum depression and reported that 11% of 160 respondents had scores representing clinically significant depression [16]. The other looked at postpartum depression among HIV-positive women and found that 10% had symptoms of depression at birth and 9% 6 months later [17].
The aim of the present study was to identify the prevalence of and risk factors for postpartum depression in a group that was anticipated to be at particularly high risk: mothers of sick, hospitalized infants at a major tertiary hospital.
2. Materials and methods
The study was conducted at the Mother–Baby Unit (MBU) of the Komfo Anokye Teaching Hospital (KATH) in Kumasi, Ghana, between June 6 and August 15, 2011. Kumasi is the second-largest city in Ghana and houses one of the major medical schools in the country. It is in the Ashanti region of Ghana (1 of 10 administrative regions) and is representative of the country as a whole in terms of health and socioeconomic indicators [18].
The study center is a busy tertiary hospital; 14 000 deliveries took place there in 2010 and there are approximately 4500 annual admissions to the MBU, which serves sick and premature newborns [19]. Of these newborns, 60% are delivered at KATH and 86% are less than 7 days old at the time of admission. The mortality rate in the MBU is estimated to be 21% per year [19].
Mothers of infants hospitalized in the MBU were recruited as a convenience sample by nursing staff. Study participation was limited to mothers who were at least 18 years of age because births to mothers under 18 are uncommon in Ghana (90% of women aged 15–19 years have never given birth) [18]. An oral or written informed consent form was completed for each oral interview conducted. Trained medical student research assistants conducted the studies, which included a semi-structured, 67-question survey. A translator (nurse, nursing student, or physician) assisted when the participant did not speak English and translated answers in real-time, which were then recorded. The survey was piloted among Ghanaian healthcare providers for cultural appropriateness and among psychiatry experts in Ghana and the USA for content. Quantitative information was collected on maternal demographics, pregnancy history, prenatal care and delivery, depression screening, social support screening, and interpersonal violence. The survey included 5 qualitative questions about mothers’ understandings of the reasons for their infants’ hospitalization, which are not reported here. Each participating mother was offered an instant photograph of her newborn as an incentive. The research was approved by the Institutional Review Board at the University of Michigan and the Committee on Human Research Publication and Ethics of the Kwame Nkrumah University of Science and Technology, which provides approval for studies at KATH.
Most of the demographic questions were taken directly from the Ghana Health Service household questionnaire [18]. In low-resource countries, incomes can vary by year and season and may not be easily quantified by the average person. Therefore, socioeconomic status was assessed by asking women whether, compared with other families, they would describe the amount of money their family had as “below average,” “average,” or “above average.” This approach has been tested in rural Ghana and is correlated with both interviewer-recorded financial status and a list of personal assets or wealth from more extensive interviews [20].
The depression screen used a translated version of the Patient Health Questionnaire (PHQ)-9, which is based on criteria from the Diagnostic Statistical Manual-IV and has better reliability and validity among community-based postpartum women in Ghana than other common postpartum depression screens [16]. A PHQ-9 score of 5–9 is generally accepted to represent risk of mild depression; a score of 10–14 indicates moderate depression; 15–19 indicates moderately severe depression; and scores of 20 or higher are associated with severe depression. For analysis, a 3-category outcome of no depression (score <5), mild depression (5–9), or moderate/severe depression (≥10) was used. Women with positive scores on the PHQ-9 item about suicidal thoughts were referred for further evaluation by medical providers.
In terms of social support, it is extremely common for women in Ghana to have live-in support from family members for several weeks or months after delivery, so another social support question was added to reflect this practice. Women were asked: “Will your mother or mother-in-law or any relative move in to help you when you go home from the hospital with your baby?”
For interpersonal violence, the same screening questions were asked as those used by the Ghana Health Service as part of a national household survey on health; they were based on a shortened version of the Conflict Tactics Scale [18,21].
Prior history of depression is a known risk factor for postpartum depression, so women were asked whether they had ever had a period of 2 weeks or more when they became sad, down, or depressed. The number of days the woman’s infant had been hospitalized was recorded as a proxy for severity, in addition to whether she had any reported history of prior perinatal or child loss, including stillbirth, infant death, or death of an older child (coded as a yes/no question). Current health status was measured by self-assessment as poor, fair, good, very good, or excellent.
Data analysis was performed using Stata/SE version 10.1 (StataCorp, College Station, TX, USA). Data were summarized and the PHQ-9 score was evaluated as a 3-category value (none, mild, or moderate/severe) so that it was more clinically meaningful than a raw score. In bivariable analysis, the PHQ-9 categorical score (none, mild, or moderate/severe) was compared with the demographic values (maternal age, marital status, education level, financial status, rural versus urban residence), health variables (primiparous versus multiparous, type of delivery, singleton versus twin delivery, self-rated poor health, history of depression), and social variables (interpersonal violence, lack of support after delivery). Bivariable analysis was performed using analysis of variance (to compare means), χ2 test, and Fisher exact test (for categories with cell size less than 5) to look at associations with independent predictor variables. The categorical PHQ-9 variable was then tested as the dependent variable in ordinal logistic regression using all of the demographic, health, and perceived social variables as potential confounders. We used the likelihood-ratio test of proportionality of odds across response categories and the Brandt test to determine that the proportional odds assumption was not violated. There was no multicollinearity between variables. The level of statistical significance was set at 0.05.
3. Results
In total, 153 women completed the survey. Average maternal age was 28 years and 109 (71.2%) women were married (Table 1). Virtually all of these postpartum women had government-provided health insurance for the pregnancy.
Table 1.
Social and personal risk factors for postpartum depression a
| Demographics | No depression (n=46) |
Mild depression (n=50) |
Moderate/severe depression (n=57) |
P value |
|---|---|---|---|---|
| Maternal age, y b | 28 ± 5 | 28 ± 6 | 28 ± 6 | 0.170 |
| Married | 34 (73.9) | 32 (64.0) | 43 (75.4) | 0.381 |
| Education | 0.327 | |||
| None/primary | 12 (26.1) | 18 (36.0) | 23 (40.4) | |
| Middle school | 18 (39.1) | 19 (38.0) | 24 (42.1) | |
| Secondary and above | 16 (34.8) | 13 (26.0) | 10 (17.5) | |
| Finances above average | 28 (60.9) | 29 (58.0) | 27 (47.4) | 0.339 |
| Rural residence | 13 (28.3) | 12 (24.0) | 25 (43.9) | 0.069 |
| Pregnancy | ||||
| First pregnancy | 13 (28.3) | 14 (28.0) | 15 (26.3) | 0.971 |
| Home delivery c | 0 (0.0) | 1 (2.0) | 6 (10.5) | 0.024 |
| Vaginal birth | 33 (71.7) | 39 (78.0) | 44 (77.2) | 0.739 |
| Singleton birth c | 38 (82.6) | 48 (96.0) | 56 (98.2) | 0.007 |
| Risk factors | ||||
| Prior depression | 11 (23.9) | 16 (32.0) | 26 (45.6) | 0.063 |
| No relatives helping after birth c | 3 (6.5) | 9 (18.0) | 16 (28.1) | 0.018 |
| Prior stillbirth or infant/child loss | 14 (30.4) | 17 (34.0) | 14 (24.6) | 0.555 |
| Interpersonal violence | 12 (26.1) | 27 (54.0) | 31 (54.4) | 0.006 |
| Poor or fair health status | 5 (10.9) | 11 (22.0) | 20 (35.1) | 0.015 |
Values are given as mean ± SD or number (percentage) unless otherwise indicated.
Analysis of variance for comparison of 3 means.
Fisher exact test for comparison owing to small cell size.
For 42 (27.5%) women, the index pregnancy was their first. Eleven (7.2%) women delivered twins and 142 (92.8%) had a singleton delivery. Overall, 146 (95.4%) participants delivered in a hospital setting, and 116 (75.8%) had a vaginal birth. Mean time since birth was 15 ± 18 days (range, 1–92 days). Fifty-three (34.6%) women reported a history of depression; 28 (18.3%) reported no relatives would be helping them after the birth; 45 (29.4%) had a history of prior loss; 70 (45.8%) reported interpersonal violence with a current partner; and 36 (23.5%) reported their current health status as fair or poor.
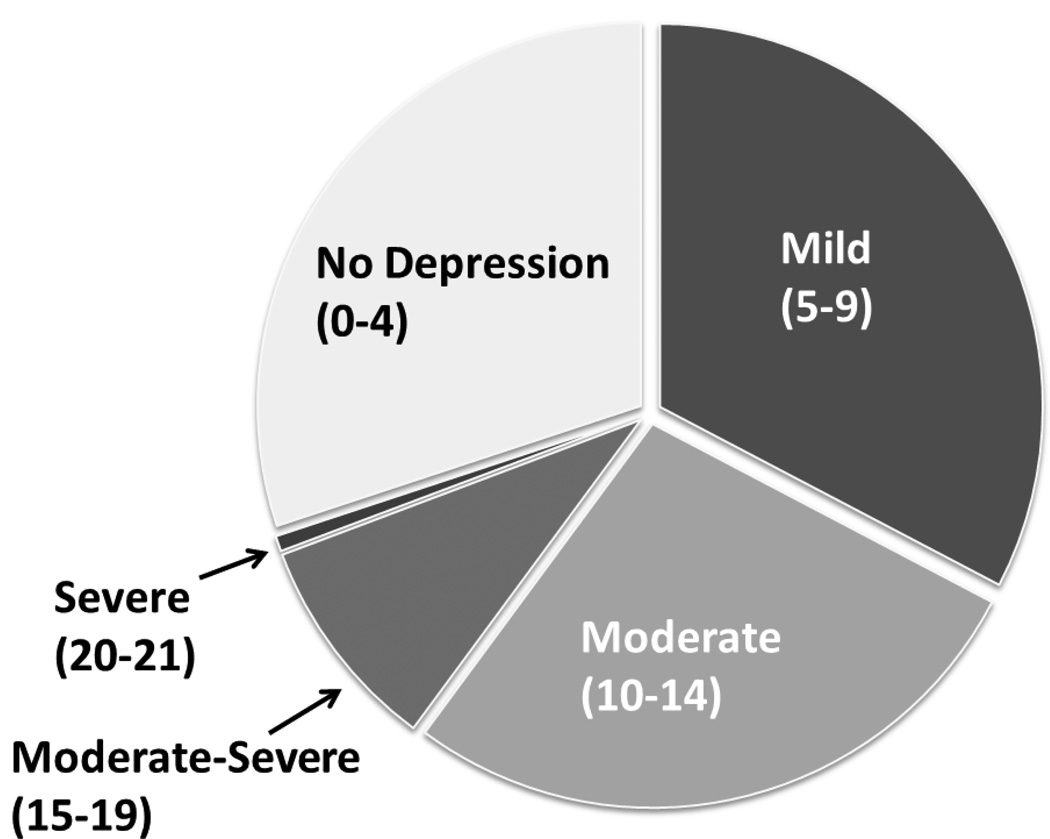
In total, 107 (69.9%) women had PHQ-9 scores indicating some level of depressive symptoms (score of ≥5). Fifty (32.7%) respondents had PHQ-9 scores of 5–9, indicating mild depression; 42 (27.5%) had scores of 10–14, indicating moderate depression (Figure 1). Fourteen (9.2%) mothers had scores of 15–19, indicating moderate depression, and 1 (0.7%) woman had a score above 19, indicative of severe depression.
Figure 1.
Patient Health Questionnaire-9 scores.
In the bivariable analysis, women who reported having a home delivery, having a singleton pregnancy, having no relatives helping them after birth, a history of interpersonal violence with their current partner, or poor/fair personal health status were more likely to have mild or moderate/severe depression scores (Table 1).
Multivariable analysis (ordinal logistic regression) included 12 of the 14 demographic, health, and social predictor variables tested in the bivariable analysis. Two variables (delivery type and twin delivery) were dropped owing to small sample size (values of 0 or 1) in subcategories. Higher levels of depression were significantly associated with history of interpersonal violence with current partner (odds ratio 2.14; 95% confidence interval, 1.11–4.13; P=0.023) and self-rated poor health status (odds ratio 2.89; 95% confidence interval, 1.29–6.45; P=0.01).
4. Discussion
In the present study, more than two-thirds of mothers with a hospitalized infant screened positive for any symptoms of depression. Because scores of 10 or higher are typically used as a cutoff strongly indicating depression among respondents, the present study had a 37% rate of positive scores. This number is substantially higher than in the systematic review of depression in Africa by Sawyer et al. [4], who reported the average prevalence of postpartum depression to be 18% (although results varied widely across studies, from 3% to 48%). While there is very high mortality among infants in the KATH MBU, their survival, growth, and wellness after discharge is unknown. Although 18% prevalence is higher than estimates for high-income nations, results across studies in Africa vary widely and the total number of studies was limited [4].
Women in low-income countries have similar risk factors for depression to women in high-income countries, including lack of social support, depression during pregnancy, education level, family stress, partner conflict, and societal stress [22]. The study population had a much higher rate of hospital delivery and cesarean, which probably reflects the fact that the participants were recruited in a hospital setting and that they lived in a region of Ghana with good access to major hospitals and neonatal care. In Ghana, 57% of infants are delivered in a hospital setting, and in the study region the rate is 70% [18]. It is unknown whether women who deliver in more rural, non-hospital settings would be at higher or lower risk. Studies in high-income countries have demonstrated high risk for mental health complications among mothers of sick and premature infants [5,6]. However, most studies in low-income countries have focused on maternal recognition or help-seeking for infant illness symptoms rather than on the impact of the illness on the mother’s mental health.
The present study indicates that lack of perceived social support, poor self-rated health, history of interpersonal violence with current partner, and home delivery are important risk factors for postpartum depression among mothers of sick infants in Ghana. The results for prevalence of interpersonal violence are consistent with those gathered by the Ghana Health Service in their national survey of households [18]. Because interpersonal violence was strongly associated with postpartum depression in the present study, further investigation should be conducted to understand this relationship.
There are significant challenges to providing adequate perinatal mental health care in Ghana, including lack of trained staff, funding barriers, and stigma. In many cases, symptoms of depression in Africa are perceived by providers as social, spiritual, or personal issues rather than a psychiatric condition [12]. As in high-income countries, mental illness is associated with significant stigma in most African nations and may be attributed to weakness, hormones, witchcraft, adultery, abuse, and poverty rather than being recognized as a biopsychosocial illness [23].
Although maternal depression during pregnancy and the postpartum period is well recognized in high-income countries, mental health has been of secondary priority for many low-income nations. As is the case with many resource-poor countries, Ghana has little infrastructure for mental health care, and few people receive psychiatric services [23]. Experts have identified significant challenges to providing appropriate mental health care in Ghana, including lack of trained staff (there are currently just 7 fully trained specialist psychiatrists in Ghana), funding barriers, and stigma. Although psychiatric specialists in Ghana have access to most categories of psychotropic medication, use is extremely limited owing to high cost. However, despite these limitations, work has been done in Ghana to improve mental health services.
Major improvements have also been made in reducing child mortality and maternal health through the UN Millennium Development Goals. However, it has only recently been recognized that maternal mental health impacts on infant growth, illness, and nutritional status—all of which affect child survival [2,3,10].
In terms of limitations, the present study was the largest study in Ghana to date but had a relatively small overall sample size and was targeted to a population of women with sick, hospitalized infants. Formal data on recruitment rate were not collected because we were dependent upon hospital nurses to select eligible patients who were present in the unit and available; however, we were anecdotally aware of only 1 patient who declined to participate, although it is possible others were not reported to us. The surveys were piloted by Ghanaian women but they were not tested on women who met the exact sociodemographic characteristics of the sample, which could limit applicability. Furthermore, a clinical screen—rather than a clinical interview—for depression was used, so symptoms of depression could be determined but a clinical diagnosis could not be given. Finally, although mean time since birth was 15 days, many mothers were within 2 weeks postpartum at the time of interview, indicating that some pregnancy and some postpartum depression could have been measured.
It is difficult to know the exact reasons for the high rate of depressive symptoms among the mothers in the present study. Certainly, the infants of these women were often extremely ill; given the scarce medical resources and the lack of follow-up care, prognosis is often uncertain, and child illness is an important risk factor by itself. Many women staying on the hospital unit were separated from their families and community support systems. Although several possible risk factors were significant in the bivariable analysis, most were not significant in the multivariable analysis. It is not clear whether risks could be explained by other confounders or whether the sample size was too small to show significance. For some variables, it was not possible to determine whether the depression or the risk factor came first, so cause and effect could not be clearly determined.
Although the present study was small, the findings are notable for high levels of symptoms among the mothers who participated, particularly given the known correlation between maternal depression and poor infant outcome. Although the results cannot be generalized to all mothers, they do provide a mental health snapshot for this population of high-risk mothers. Given that infants of these women are already at medically high risk, it is possible that maternal depression could contribute to worse outcomes. Additional research is planned to explore these correlations and follow outcomes for this cohort. Functional impairment was difficult to assess because all of the women were away from home, caring for their hospitalized infants, but this is something to consider in future research. In addition, at least 1 study in Ghana has noted that women with depression may present with somatic concerns rather than clear mental health worries, so it may be worth exploring physical health and somatic complaints in future studies [24]. The findings of the current study also raise the question of whether interventions to prevent and treat postpartum depression among mothers of sick infants could improve not only maternal mental health but also infant morbidity and mortality. Such a finding could be an exciting advancement in the field of perinatal health.
Synopsis.
Mothers of hospitalized infants in Ghana have high rates of postpartum depression symptoms; this has important implications for subsequent maternal and infant health.
Acknowledgments
The present research was funded by a grant from the University of Michigan GlobalREACH. K.J.G.’s salary was supported by an NIH K-23 training grant through the National Institutes of Mental Health. The funders had no role in research design/conduct, analysis, preparation of results, or manuscript approval.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
The authors have no conflicts of interest.
References
- 1.Vesga-López O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65(7):805–815. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Almond P. Postnatal depression: a global public health perspective. Perspect Public Health. 2009;129(5):221–227. doi: 10.1177/1757913909343882. [DOI] [PubMed] [Google Scholar]
- 3.WHO, UNFPA. Maternal mental health and child health and development in low and middle income countries: report of the meeting held in Geneva, Switzerland, 30 January – 1 February 2008. http://www.who.int/mental_health/prevention/suicide/mmh_jan08_meeting_report.pdf. Published 2008.
- 4.Sawyer A, Ayers S, Smith H. Pre- and postnatal psychological wellbeing in Africa: a systematic review. J Affect Disord. 2010;123(1–3):17–29. doi: 10.1016/j.jad.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 5.Lefkowitz DS, Baxt C, Evans JR. Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the Neonatal Intensive Care Unit (NICU) J Clin Psychol Med Settings. 2010;17(3):230–237. doi: 10.1007/s10880-010-9202-7. [DOI] [PubMed] [Google Scholar]
- 6.Vigod SN, Villegas L, Dennis CL, Ross LE. Prevalence and risk factors for postpartum depression among women with preterm and low-birth-weight infants: a systematic review. BJOG. 2010;117(5):540–550. doi: 10.1111/j.1471-0528.2009.02493.x. [DOI] [PubMed] [Google Scholar]
- 7.Ukpong DI, Fatoye FO, Oseni SB, Adewuya AO. Post partum emotional distress in mothers of preterm infants: a controlled study. East Afr Med J. 2003;80(6):289–292. doi: 10.4314/eamj.v80i6.8703. [DOI] [PubMed] [Google Scholar]
- 8.Marcus SM. Depression during pregnancy: rates, risks and consequences--Motherisk Update 2008. Can J Clin Pharmacol. 2009;16(1):e15–e22. [PubMed] [Google Scholar]
- 9.Gold KJ, Marcus SM. Effect of maternal mental illness on pregnancy outcomes. Expert Rev Obstet Gynecol. 2008;3(3):391–401. [Google Scholar]
- 10.Adewuya AO, Ola BO, Aloba OO, Mapayi BM, Okeniyi JA. Impact of postnatal depression on infants' growth in Nigeria. J Affect Disord. 2008;108(1–2):191–193. doi: 10.1016/j.jad.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 11.Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R. Impact of maternal depression on infant nutritional status and illness: a cohort study. Arch Gen Psychiatry. 2004;61(9):946–952. doi: 10.1001/archpsyc.61.9.946. [DOI] [PubMed] [Google Scholar]
- 12.Patel V, Rahman A, Jacob KS, Hughes M. Effect of maternal mental health on infant growth in low income countries: new evidence from South Asia. BMJ. 2004;328(7443):820–823. doi: 10.1136/bmj.328.7443.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Surkan PJ, Kennedy CE, Hurley KM, Black MM. Maternal depression and early childhood growth in developing countries: systematic review and meta-analysis. Bull World Health Organ. 2011;89(8):608–615. doi: 10.2471/BLT.11.088187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Ghana Country Cooperation Strategy at a Glance. http://www.who.int/countryfocus/cooperation_strategy/ccsbrief_gha_en.pdf. Updated May 2012.
- 15.World Health Organization. Helping youth overcome mental health problems. http://www.who.int/mental_health/policy/development/WHO%20MIND_Youth%20mental%20health7.pdf. Published November 7, 2007.
- 16.Weobong B, Akpalu B, Doku V, Owusu-Agyei S, Hurt L, Kirkwood B, et al. The comparative validity of screening scales for postnatal common mental disorder in Kintampo, Ghana. J Affect Disord. 2009;113(1–2):109–117. doi: 10.1016/j.jad.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 17.Okronipa HE, Marquis GS, Lartey A, Brakohiapa L, Perez-Escamilla R, Mazur RE. Postnatal Depression Symptoms are Associated with Increased Diarrhea Among Infants of HIV-Positive Ghanaian Mothers. AIDS Behav. 2012;16(8):2216–2225. doi: 10.1007/s10461-012-0153-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghana Statistical Service, Ghana Health Service, ICF Macro. Ghana Demographic and Health Survey 2008: Key Findings. http://www.measuredhs.com/pubs/pdf/SR172/SR172.pdf. Published 2009.
- 19.KATH. Komfo Anokye Teaching Hospital, Annual Report 2010. Kumasi, Ghana: KATH; 2010. [Google Scholar]
- 20.van Bodegom D, May L, Kuningas M, Kaptijn R, Thomése F, Meij HJ, et al. Socio-economic status by rapid appraisal is highly correlated with mortality risks in rural Africa. Trans R Soc Trop Med Hyg. 2009;103(8):795–800. doi: 10.1016/j.trstmh.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 21.Strauss MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised Conflict Tactics Scales (CTS2): development and preliminary psychometric data. J Fam Issues. 1996;17(3):283–316. [Google Scholar]
- 22.Ramchandani PG, Richter LM, Stein A, Norris SA. Predictors of postnatal depression in an urban South African cohort. J Affect Disord. 2009;113(3):279–284. doi: 10.1016/j.jad.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 23.Ofori-Atta A, Cooper S, Akpalu B, Osei A, Doku V, Lund C, et al. Common understandings of women's mental illness in Ghana: results from a qualitative study. Int Rev Psychiatry. 2010;22(6):589–598. doi: 10.3109/09540261.2010.536150. [DOI] [PubMed] [Google Scholar]
- 24.Turkson SN, Dua AN. A study of the social and clinical characteristics of depressive illness among Ghanaian women--(1988–1992) West Afr J Med. 1996;15(2):85–90. [PubMed] [Google Scholar]