Abstract
Bitemporal hemianopic visual field impairment frequently leads to binocular vision difficulties. Patients with bitemporal hemianopia with pre-existing exophoria complain of horizontal diplopia, sometimes combined with vertical deviation (with pre-existing hyperphoria). The symptoms are a result of the phoria decompensating into a tropia (hemi-slide) due to the lack of retinal correspondence between the remaining nasal fields of both eyes. We measured these effects using a dichoptic perimeter. We showed that aligning the eyes with prisms could prevent diplopia if the bitemporal hemianopia is incomplete. We also describe the successful use of a novel fusion aid – the ‘stereo-typoscope’ – that utilizes midline stereopsis to prevent diplopia resulting from hemi-sliding in patients with complete bitemporal hemianopia.
Keywords: field defects, hemianopsia, tropia, optic chiasm lesions, heteronymous hemianopia
1. Introduction
Bitemporal hemianopia results from compromised nasal fibres of the optic nerves in both eyes due to injuries or lesions at the optic chiasm. The temporal crescents are the only part of the binocular visual field that is lost, and a central 110°–120° of visual field remains; a field that is considered large enough to function normally (Fig. 1a1–1a3) and to qualify for a driving license in numerous states in the USA1, 2 and other countries.3 Therefore, bitemporal hemianopia, though named for the visual field loss, may represent only modest peripheral visual field loss as measured in conventional binocular perimetry (e.g., the Estermann test in the Humphrey Visual Field Analyzer or binocular Goldmann perimetry). However, we have shown4 that when examined in three dimensional space (volume perimetry) one can measure a binocular central field loss beyond the point of fixation, where a central wedge of visual field posterior to the fixation is scotomatous in depth (post-fixational blindness or posterior volume scotoma). This volume scotoma may have some impact on the functionality of patients with bitemporal hemianopia.4–6 The effect, however, is limited to conditions where the fixation plane itself does not block the view behind it (e.g., fixating on a small object or on a transparent surface such as the windshield of the car). While the peripheral and post-fixation field losses are rarely presented symptomatically, patients with bitemporal hemianopia frequently present with binocular vision symptoms. In this paper we discuss these binocular vision difficulties and describe a simple approach and a novel device to treat them.
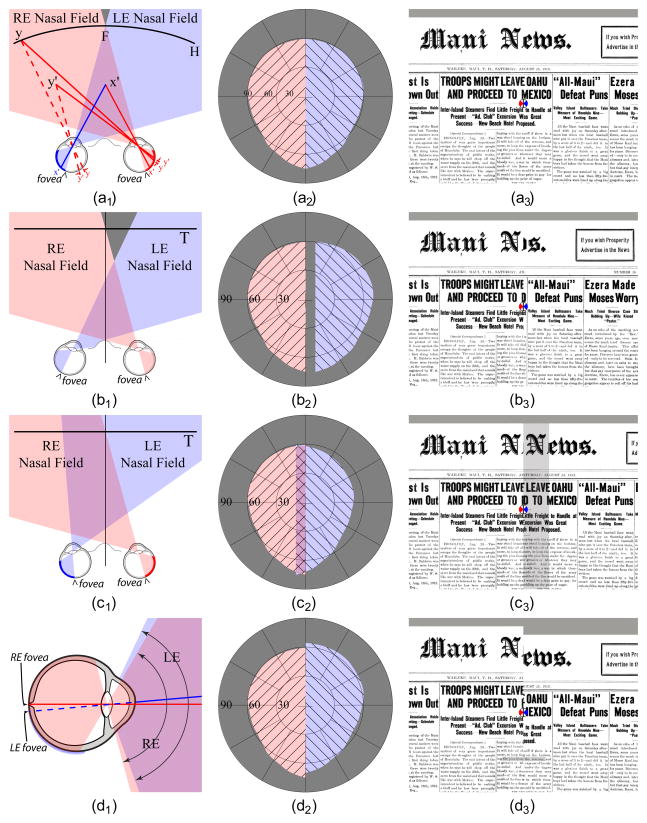
Figure 1.
Illustrations of bitemporal hemianopia with various eye deviations. In the rows from top to bottom: Orthotropia, Left Esotropia, Left Exotropia, and Left Hypertropia are shown, respectively. Left column: Illustrations of the eyes’ alignment and monocular field relationships for different conditions (with scale exaggerated to clarify the effects). H: Horopter, F: Fixation target, T: Fixation plane (e.g., the newspaper), RE: Right Eye, LE: Left Eye. Point y and others on the Horopter (in a1) are imaged on corresponding points on the two retinas, but with bitemporal hemianopia they fall on one seeing and one blind point (left eye, for y). Point x′ and similar points on the midline closer than fixation fall on seeing retinas in both eyes but project to opposite cortical hemispheres, preventing normal stereopsis. Point y′ (and similar ones) not on the horopter and away from the midline results in retinal disparity that normally codes depth within the same cortical hemisphere. However, that mechanism is not operable in bitemporal hemianopia, as one of the retinal projections is to a blind hemi-retina. Midline points beyond fixation fall into the post-fixational scotoma (grey wedge in a1 & b1) and are not seen by either eye. Middle column: Consequential binocular visual fields. Lines tilting to the right or left mark the right and left eye’s visual field, respectively. Pink and blue shading identify projection to the left and right hemispheres, respectively. Tropias are exaggerated for clarity. Right column: Simulated percepts. The RE (red) and LE (blue) fixation points, always perceived in the same direction, are marked. Deviations of 3° lateral and 1° vertical are illustrated to scale in this column. (a1–a3): Orthotropic fixation results in mild loss of peripheral vision (temporal crescents) and a normal percept. (b1–b3): Left esotropia shifts the left nasal field to the right, leaving a vertical strip of central scotoma between the two nasal hemifields, resulting in loss of central image parts, such as the letters “ew” in “News”. The percept, however, does not show a blind region, as the retinal directions along the vertical midline on both hemifields both code straight ahead. Under steady fixation the newspaper may look shrunken (b3), but with continued reading or scanning saccades the print column will be fully visible and may be perceived in full width. (c1–c3): Left exotropia shifts the left nasal field to the left, overlapping the right nasal field (crosshatched area in c2), resulting in diplopia. The shaded area in the simulated percept is diplopic and seen by the left eye. (d1–d3): Left hypertropia slides the left nasal hemifield upward causing the right image to be perceived as lower. This may be reported as double vision (split diplopia). The yellow highlighted row of small print appears normal but actually skips to a different line of text. All these effects can make reading very difficult. Frame d1 provides a side view of the two eyes. The view from above would be identical to a1.
Complaints of binocular vision difficulties by patients with bitemporal hemianopia in the absence of extraocular muscle palsies (usually horizontal diplopia or vertical tearing or splitting of the image) have been documented as early as 1929.7 The symptoms arise due to the patient’s inability to fuse images, as there are no overlapping visual field elements (between seeing nasal hemifields and blind temporal hemifields) that fall on corresponding non-blind retinal points.8 This lack of fusion lock across the visual field decompensates any pre-existing phoria into a tropia, with a resulting visual field effect called hemi-sliding.5 The two nasal hemi-fields slide relative to each other horizontally and/or vertically, depending on the phoria.
With a pre-existing exophoria turning into exotropia, patients experience and report diplopia, as a paracentral object is imaged on temporal retinal locations in both eyes (Fig. 1c1–1c3). Uniquely, the diplopia experienced is not accompanied by binocular visual confusion (defined as the percept of two different objects imaged on corresponding retinal points in both eyes, and therefore perceived in the same visual direction), as is the case with exotropia or esotropia without visual field defects (see Fig. S1 in supplemental material). In complete bitemporal hemianopia there are no corresponding points that are functional on both retinas, thus this eliminates the possibility of binocular confusion. The lack of binocular confusion means that the stimulus for binocular rivalry is absent, and the diplopic percept is stable.
Changes in convergence could result in changes in the angle of tropia (i.e., resulting from accommodation changes) and thus changes in the diplopic images’ separation and position relative to each other. If the patient has a pre-existing vertical phoria, the images will be split vertically relative to each other (Fig. 1, d1–d3), possibly reported as diplopia, as parts of the same objects are seen at two different vertical directions. We term this effect split diplopia to distinguish it from frank diplopia (where the images of the same parts of objects are seen in two different directions).
Exotropia may be combined with a vertical deviation, resulting in combined horizontal frank diplopia and vertical split diplopia (not shown in Fig. 1). The vertical deviation per se is generally expected to be stable and minimally affected by horizontal convergence/accommodation changes. Patients with diplopia of either type frequently close or cover one eye to eliminate the bothersome diplopia, in spite of the consequential severe visual field reduction.
The lack of fusion in pre-existing esophoria results in esotropia, causing neither diplopia nor confusion. Instead, the patients experience a central scotoma extending vertically across the whole field (Fig. 1, b1–b3), essentially extending post-fixational blindness to a pre-fixation zone. In esotropia, the intersection of the visual axes is closer than the intended fixation position, and hence the scotoma. Patients with eso deviation might report shrinkage of an object of regard or may notice the loss of some details in the object. This visual perception, though described and illustrated in literature,3, 9 is uncommon. Loss of (pericentral) information is less bothersome (or even unnoticed) compared to the annoyance associated with frank or split diplopia.
Experiencing a scotoma means that the patient is not able to see objects that fall in that part of the space, not that the patient notices a hole in the visual field. Even most patients with central scotomas, as due to macular degeneration, do not notice the actual scotoma spontaneously,10 though they are aware of the acuity loss. No such acuity loss accompanies the central scotoma in bitemporal hemianopia with esotropia. If a loss of image detail is noted peripherally, a natural shift to examine it foveally will restore its visibility. On the other hand, if the esotropia is also accompanied by vertical deviation, the vertical hemi-sliding, with its accompanying split diplopia, is very apparent (especially when looking at text) and is likely to be reported spontaneously. Since vertical phoria is less common than horizontal phorias, the likelihood of that syndrome is lower. Patients with bitemporal hemianopia and decompensated esophoria are less likely than those with other phorias to close or patch an eye, as that results in a larger field restriction and does not relieve the central field loss symptoms.
For esophoria (tropia) in bitemporal hemianopia, no treatment is offered in the literature, probably because these patients are less symptomatic in the absence of diplopia. The prevalent treatment options for decompensated exophoria, however, are patching one eye or surgically correcting the exotropia, preferably with adjustable sutures, to either reduce the magnitude of the bothersome diplopia11 or to induce a small level of esotropia.3 Prisms have been suggested to try to neutralize exotropia or to separate the diplopic images widely.9 Both surgery and prisms do not prevent further hemi-sliding due to lack of fusion lock.
Absence of corresponding seeing retinal regions throughout the binocular visual field in complete bitemporal hemianopia makes it difficult to provide a fusional lock. We note, however, that around the vertical midline through fixation, stereopsis is apparently appreciated without stimulation of retinal corresponding points, which have crossed disparity anterior to fixation (e.g., point x’ and its retinal projections in Fig. 1a1) and uncrossed disparity post-fixation (but perceptually blind in bitemporal hemianopia).12, 13 The crossed-disparity images fall on the temporal retinas (shown in Fig. 1a1). These central disparities elicit midline stereopsis, operable even though the binocular images of targets anterior and posterior to fixation are projected to opposite cortical brain hemispheres.12, 13 In normal vision, midline stereopsis, with the two retinal images projecting to separate hemispheres, is restricted to objects within the purple and grey triangles fore and aft of fixation, as shown in Fig. 1a1. Objects within these limited ranges need to be processed across the hemispheres to be perceived in stereo or stimulate convergence. Midline stereopsis can be appreciated within a disparity limit of 2° to 6° from the fixation point.12, 14 Midline stereopsis is believed to be mediated through corpus callosal cross-linking connections between the cortical hemispheres13, 14 or due to imperfect partitioning of nasal and temporal retinal fibres at the optic chiasm.13, 14 Along the midline, fusional vergence eye movements have also been demonstrated.15 Midline stereopsis is used frequently, perhaps even more than stereopsis in other directions, for manual manipulation of objects. Intact midline stereopsis, without stereopsis elsewhere in the visual field, has been reported in a patient with a sectioned optic chiasm, who also showed complete bitemporal hemianopia.12 Furthermore, a patient who underwent callosectomy to prevent epileptic seizures had no midline stereopsis but had intact stereopsis elsewhere in the visual field,16 supporting the role of the corpus callosum in the mediation of midline stereopsis. We hypothesized that fusion lock elicited by midline stereopsis targets in the upper and lower periphery may help prevent hemi-slide.
In stereopsis elicited from directions other than the midline (e.g., point y′ and its retinal projections in Fig. 1a1), the target images are projected to the same hemisphere of the brain (and depth relative to the horopter is signalled by disparity derived in the brain from the difference between the angular distances from y′ to y in each eye, shown in Fig. 1a1; a different measure than is used to define midline stereopsis disparity).
We report here on the measurement of hemi-slide and diplopia using a dichoptic perimeter, we provide a more accurate description of the visual percepts caused by the combination of strabismus and field loss, and we describe a potential new treatment option that elicits midline stereopsis to prevent hemi-sliding in complete bitemporal hemianopia.
2. Methods
Patients
Two patients with bitemporal hemianopia referred to us with complaints of diplopia were enrolled in a preliminary study, with informed consent as approved by the Institutional Review Board of Schepens Eye Research Institute.
Patient 1
43 year old (at first visit) male had surgical removal of pituitary adenoma six years prior. He reported seeing double, more often at near, and was bothered by it, especially while reading.
Patient 2
28 year old (at first visit) male, had bitemporal hemianopia secondary to a head injury from a fall two years prior. He reported seeing double (horizontal and vertical) both at distance and near, but felt it was worse at near, and so patched his right eye when reading and working on the computer. The patient also reported that he could bring the diplopic images closer, but could not maintain that for long.
Measured visual functions for both patients are shown in Table 1.
Table 1.
Visual functions measured for both patients
| Patient 1 | Patient 2 | |||
|---|---|---|---|---|
| Goldmann Perimetry (Target size: V4e) |

|

|

|

|
| Phoria (Cover Test) | Distance: 4Δ BI Near: 18Δ BI |
Distance: 6Δ BI, 3Δ BD (RE) Near: 10Δ BI, 4Δ BD (RE) |
||
| Stereopsis (Randot Stereo Test) | No measurable stereopsis | No measurable stereopsis | ||
| Visual Acuity | RE: 6/9; LE: 6/9 | RE: 6/9; LE: 6/6 | ||
Δ indicates prism dioptres, BI: Base-In, BD: Base-Down, RE: Right Eye, LE: Left Eye
Prism correction
Both patients were fitted with prism glasses using ophthalmic prisms (not press-on). Prism powers that eliminated diplopia for the reading distance (either measured phoria or less than the measured phoria) were prescribed. Phoria was measured using an alternating cover test, neutralizing with prism bars. No particular difficulty due to the field loss was noted in measuring the deviation. Patient 1 was fitted with 6Δ BI for each eye in his reading spectacles. Patient 2 was fitted with 2Δ BD (RE) and 2Δ BU (LE) combined with 5Δ BI in each eye in his distance spectacles, which he also used for reading. Following fitting, the patients were given an hour trial during which they were asked to read or perform near-vision tasks in the lab. Phoria measurements were then repeated and verified for lack of prism adaptation.17 Patients were asked to return in 1, 3, and 12 months, for follow-up and further evaluation and consideration for use of the stereo-typoscope (see section on Stereo-Typoscope).
Dichoptic visual fields (DVF)
DVF perimetry measured the monocular visual fields and their relative positions under binocular viewing conditions. Our DVF perimeter uses ferroelectric liquid crystal shutter goggles and a stereo video projector to accomplish this.18 The central 60° of visual field (but only ~50° with goggles) can be mapped at a viewing distance of 1 meter. The patient is presented with a fixation target seen by both eyes and kinetic perimetry targets were presented monocularly to measure the monocular field positions relative to each other and relative to the fixation target under binocular viewing. In the case of bitemporal hemianopia with tropia, the patient fixates with one eye, even with the binocularly visible fixation target. Patient 1 fixated with his right eye and patient 2 fixated with his left eye.
Diplopia Mapping
Diplopia mapping was performed with the DVF perimeter operated as a standard binocular perimeter without the dichoptic feature (similar to a Tangent Screen). Patients viewed a fixation cross (1.2°) presented binocularly and responded to static perimetry stimuli (1.2° cross, also presented binocularly on the DVF screen) by clicking a buzzer only if the target appeared double. The diplopia test stimuli were presented for 1.9s near locations expected to be visible by at least one eye (as determined from the patient’s dichoptic monocular fields). The stimuli were predominantly presented along the vertical strip of the monocular fields’ overlap. Each stimulus was presented twice in a random order. Diplopia mapping was performed with and without prism correction during the 3-month follow-up visit.
Stereo-Typoscope
We postulated that since midline stereopsis operates without corresponding points (in the usual sense), and since it has been shown to trigger fusional eye movements,15 it could be used to provide peripheral fusional lock for patients with complete bitemporal hemianopia. A midline stereoscopic stimulus, however, is needed. Only anterior (crossed disparity) midline stereopsis can be stimulated in bitemporal hemianopia, as stimuli posterior to fixation (uncrossed disparity) fall in the post-fixational scotoma (Fig. 1a1). To provide anterior midline stereoscopic stimuli we invented a device we call a “stereo-typoscope” (Fig. 2). An ordinary typoscope is a low-vision reading aid, usually made from dark paper or plastic, forming a rectangular frame that, when placed over text, creates a high contrast boundary around a small portion of the reading material. In the stereo-typoscope, instead of using a thin sheet of material, a cardboard of some thickness is used to provide depth/disparity stimulation. The surface has high contrast vertical stripes that provide strong stimuli for disparity and stereopsis in the near periphery. To help the peripheral fusion lock, the phoria of the patient was corrected using prisms, and the eyes’ visual axes were brought to close apposition to be well within the fusible range of midline stereopsis. The stereo-typoscope is placed on the reading material and is moved along while reading, keeping the instantaneously read text within the frame’s window. The lateral sides of the typoscope do not contribute to fusion; they simply connect the upper and lower gratings in position around the text being read, and can be used to manoeuvre the stereo-typoscope. The non-periodic square-wave gratings are easily visible in the peripheral retina. (At 4° retinal eccentricity, visual acuity threshold is about 6/18.19) The non-periodicity of the square wave gratings prevents fusion of non-corresponding bars.
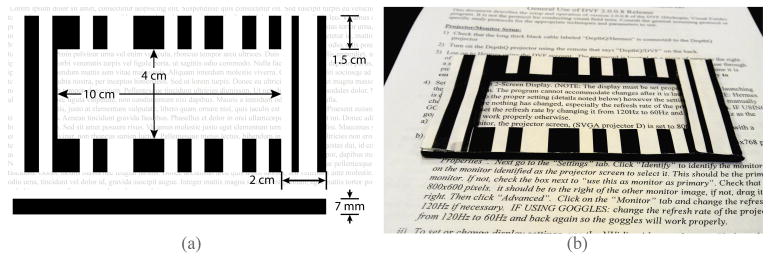
Figure 2.
The stereo-typoscope is a fusion aid for reading. The frame thickness provides peripheral crossed disparities of the high-contrast vertical square-wave gratings that serve as stimuli for midline stereopsis above and below the reading materials. (a): Dimensional diagram with the measurements of the stereo-typoscope that was given to patient 2 (thickness = 7mm). (b): A picture of a stereo-typoscope similar to the one used by patient 2 (but thickness = 4mm).
The stereo-typoscope provided to patient 2 was 0.7 cm thick (Fig. 2a). At a 40 cm reading distance, the amount of convergence required for interpupillary distance (IPD) 68.5 mm is 9.79° (17.25Δ). With 0.7 cm thickness, the convergence required at 40−0.7 = 39.3cm, is 9.96° (17.56Δ). The difference in convergence provides a crossed disparity stimulus of 0.17° (624″ or 0.30Δ) for peripheral fusion. The typoscope photographed in Fig. 2b is identical, except that it is 4 mm thick.
3. Results
Patient 1
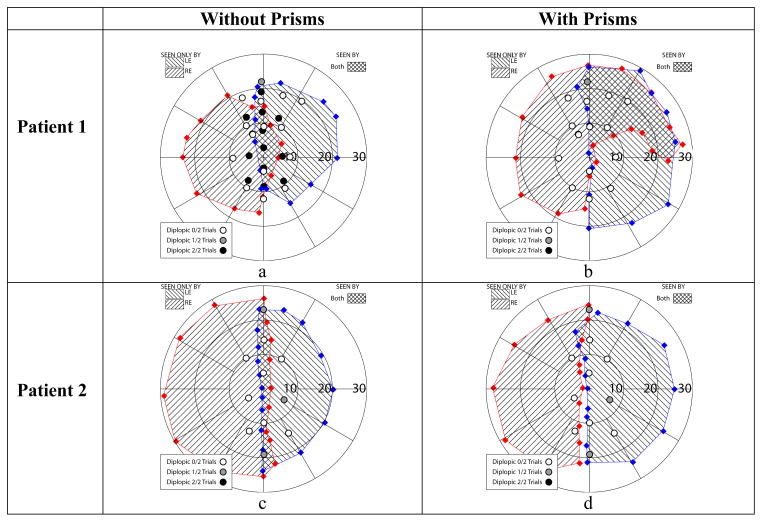
Incomplete bitemporal hemianopia was measured in this patient. Residual superior partial temporal visual field was mapped in the right eye with the Goldmann perimeter (Table 1). In Fig. 3a, without the prisms, overlapping of the nasal fields due to hemi-sliding, consistent with the exodeviation, was recorded with the DVF perimeter, and central diplopia was measured within the overlapping areas. Note, however, that this patient also reported diplopia in some pericentral locations that were not expected to be diplopic. At least some of these locations could be accounted for by fluctuations (increase) in phoria magnitude or variability in fixation. With a change in fixation, the overlapping areas would cover a larger area in the visual field. With the prisms (Fig. 3b), the left eye’s nasal field is shifted to the right and the central overlap is mostly eliminated (within the measurement error of the perimetry). Diplopia was reported once for one point only in a small residual overlapping area superiorly. Interestingly, under the binocular viewing condition without the prisms, the superior temporal residual visual field section that was measured monocularly with the Goldmann was highly reduced, whereas with prisms that residual visual field expansion was also measureable in the DVF. This result was verified with repeated measurement. Diplopia was not expected to be reported (and was not found) in this overlapping area, as the phoria is corrected by the prisms.
Figure 3.
Hemi-sliding recorded with the Dichoptic Visual Fields perimeter without (a and c) and with (b and d) prisms. Patients viewed a fixation target binocularly. Monocular (dichoptic) visual fields under binocular viewing conditions are plotted using red symbols and lines tilting to the right to mark visual fields of the right eye and blue symbols and lines tilting to the left for the left eye. Goggles limit measurement to approximately the central 50°. Black filled circles indicate diplopia reported in 2 of 2 trials, while grey filled circles indicate diplopia reported in 1 of 2 trials. Open circles indicate no diplopia reported in 2 trials. Diplopia mapping was conducted under standard binocular perimetry testing.
With the prism glasses, patient 1 reported no diplopia when reading, and he was able to read comfortably at all follow-up visits. Therefore, a stereo-typoscope was not given to this patient.
Patient 2
After one month of prism spectacle wear, the patient reported that the prism glasses reduced the magnitude of the diplopic image separation, but he still had difficulty reading books and complained of occasional disturbing horizontal and vertical diplopia. In Fig. 3c the measured hemi-sliding of the right eye nasal field to the right without the prisms is illustrated (cross-hatching), with the consequent recording of diplopic responses. With the prism glasses (Fig. 3d), the DVF fields mapped for this patient show the prism effect as a shift of the right eye to the left, resulting in a small central scotoma inferiorly, perhaps due to overcorrection of the exophoria, resulting in an esophoria at the DVF viewing distance of 1 meter. (Prism correction was prescribed for a reading distance of about 40cm.) With the reduction in overlap, we recorded substantial reduction in diplopia.
The stereo-typoscope was given to this patient at the 1 month follow-up to address his persistent complaint of difficulty reading. The patient was instructed in the use of the stereo-typoscope as a fusion aid and to be mindful of the peripheral upper and lower borders. He reported subjective improvement in reading comfort with the stereo-typoscope at the 3 and 12 months follow up. The patient also reported noticing a reduction in the incidence of diplopia involving overlapping lines of text that he had encountered without the stereo-typoscope. He reported being able to read continuously for 45 minutes with this device without patching or needing to close the right eye.
4. Discussion
Traumatic chiasmal syndrome, as in our patient 2, is an uncommon presentation following head injuries.20–23 Compressive lesions of the chiasm commonly show partial bitemporal hemianopia,22 as seen in our patient 1. While some post-operative improvement in visual fields is noted in up to 87% of the patients undergoing pituitary surgery, complete recovery to normal visual fields is only found in about 18%.24, 25 Hemi-sliding and diplopia are more likely to occur in complete or ‘over-complete’ bitemporal hemianopia than in partial bitemporal hemianopia. In a literature review21 it was found that complete and over-complete bitemporal hemianopic visual field defects are more common (67 of 79 cases) than cases with partial bitemporal hemianopia (12 of 79 cases). These statistics suggest that many patients with hemi-slide due to bitemporal hemianopia might benefit from the stereo-typoscope reading device. Hemi-sliding is also noted in patients with heteronymous altitudinal field defects who have no overlapping regions in the residual fields.26 However, the stereo-typoscope will not be beneficial for these patients as vertical midline stereopsis cannot be used to align the eyes.
The magnitude of the deviation in bitemporal hemianopia is expected to be moderate, within the magnitude of phorias, which is typically smaller than those seen in congenital or childhood tropia, and therefore challenging to measure. Illustrations in this paper (Fig. 1 left and centre columns) exaggerated these deviations, but we provided realistically-scaled representations of the hemi-slide (and diplopia) when reading a newspaper (Fig. 1 right column). Considering the magnitude and nature of the hemi-slide is important in evaluating its contribution to the patient’s discomfort. The diplopia (in exo/hyper phoria) is always central, and can be bothersome even if small, though possibly less bothersome than a typical diplopia, as there is no binocular confusion. The central scotoma in esophoria, however, does not affect acuity as it does in other conditions that result in central field loss. Objects that fall into the scotoma become visible with small eye movements, and thus the effect is not easily noticeable, which is why surgery and prism correction aim to err on the eso-deviation side.
The visual effects of bitemporal hemianopia with decompensated phorias are unique and different from those commonly described in strabismus or experienced with the use of full-lens prisms. As a result, prior illustrations were frequently erroneous or inaccurate.3, 27 We provide copies of such illustrations and corrected versions in our supplementary online material. Illustrations of expansion (with exotropia) and shrinking (with esotropia) of observed objects can be misleading, especially when line drawings are used that can create such simplistic impressions.9 As explained earlier, the perception of object size can be restored when the patient scans the scene. However the patient who is steadily fixating, and has attention directed to the effect, may report that objects shrink. We demonstrated this for patient 2. When his exophoria was gradually overcorrected into the eso direction in the phoropter, he reported that the examiner’s face shrank. However, he never noted faces of people or other objects to be expanded with his notable and bothersome diplopia. The usually-small deviation may preclude observation of size changes.
The hemi-slide in both our patients had both horizontal and vertical components that were reduced with prisms (Fig. 3). Patient 1 demonstrated some detection of the kinetic targets in the right superior nasal field when wearing the prisms, also evidenced in the monocular Goldmann perimeter plot (Table 1), but did not show the same residual sensitivity in the temporal superior quadrant under the same DVF conditions without the prisms. We repeated these measurements, as they were surprising. One explanation might be that under the prism-aligned condition neither binocular confusion nor rivalry is stimulated (nor was any diplopia measured in that area). The same is true in the monocular Goldmann test. Without the prisms, hemi-sliding causes misalignment of the right superior temporal field relative to the corresponding retinal areas in the left nasal retina and therefore caused binocular confusion. It is possible that this caused rivalrous suppression of the weaker temporal residual field.
Diplopia mapping with standard binocular perimetry clearly documented the perception of diplopia caused by hemi-sliding along the midline (Fig. 3 a and c) and the reduction of hemi-sliding and diplopia with prism correction (Fig. 3 b and d). A limitation of our diplopia mapping is that the patients knew when they were viewing the targets with their prism correction. This could have biased them to report no (or less) diplopia of the targets seen. A sham prism trial would be needed to eliminate this type of bias. Monocular targets can be used for catch trials in both prism conditions (real and sham). We are pursuing further work to improve these measurements and evaluate the benefit of our proposed treatment with more patients.
Currently no effective treatment exists for managing the symptoms associated with hemi-sliding. We have demonstrated that prism correction of the phoria can be sufficient to alleviate the diplopic symptoms of hemi-slide in partial bitemporal hemianopia, where sufficient area of retinal correspondence is present (patient 1). However prisms alone are not sufficient for alleviating hemi-slide in complete bitemporal hemianopia (patient 2). A simple device (stereo-typoscope) along with prism correction successfully reduced the diplopia experienced during reading in this complete bitemporal hemianope. Peripheral disparity is a strong stimulus for fusion, even overcoming opposing central fusion.28, 29 It is therefore possible that peripheral midline stereo disparity can elicit a strong fusional response, sufficient to establish peripheral fusional lock when using the stereo-typoscope. Alternate approaches to creating peripheral crossed-disparity along the midline above and below fixation could involve peripheral prisms, akin to Peli prisms,30 however, with much lower power embedded in a spectacle prescription for both eyes. This hypothesis needs further testing and direct verification.
Patient 2 is a computer professional who uses his computer for near work. The stereo-typoscope helped him read print. A different approach is needed for on-screen text. The stereo-typoscope aperture was narrow enough to provide adequate peripheral stimuli (Fig. 2). A wide-aperture stereo-typoscope designed for a computer monitor to be mounted along its edges may not be as effective, as the peripheral stimuli may be too far in the periphery when reading in the centre of the monitor. We tried one such stereo-typoscope custom made for the patient’s laptop and found it to be ineffective. With the advent of 3D monitors, it is possible that peripheral stimuli to elicit peripheral fusion can be created as a ‘virtual’ high contrast stereo-typoscope. Developing such a device would be justified once the basic operation and effectiveness of the stereo-typoscope has been established with more patients and under more-controlled test conditions.
Postscript
After the manuscript was accepted for publication, we completed the one month follow-up with a patient with incomplete bitemporal hemianopia who was not reported in the study. This patient was referred to us for complaints of bothersome diplopia when driving. The diplopia was mostly vertical, but also had a horizontal component. The patient had complete superior bitemporal quadrantanopia and only partial inferior bitemporal quadrantanopia. Horizontal and vertical prism correction for the heterophoria were dispensed in both distance and reading spectacles. On follow-up, the patient expressed great comfort with the correction and reported no diplopia with the prism glasses. Without glasses he still experienced occasional diplopia. We confirmed this with modified Goldmann perimetry in which, after mapping the monocular and binocular fields, the overlapping and non-overlapping areas were probed with static brief binocular presentation of targets. The patient reported whether he saw one or two targets during each probe. Diplopia was only noted when tested without the prism glasses and only in the overlapping areas.
Supplementary Material
Acknowledgments
Supported in part by NIH grant R01EY012890 & R01EY023385 (EP) and P30EY003790, and by the Hyderabad Eye Research Foundation (PS). We thank Henry Apfelbaum for help in creating the illustrations.
Footnotes
Disclosure: The authors report no conflicts of interest and have no proprietary interest in any of the materials mentioned in this article.
References
- 1.Peli E, Peli D. Driving With Confidence: A Practical Guide to Driving With Low Vision. Singapore: World Scientific; 2002. [Google Scholar]
- 2.Peli E. Driving with low vision: who, where, when, and why. In: Massof RW, editor. Albert and Jakobiec’s Principles and Practice of Ophthalmology. 3. Philadelphia: Elsevier; 2008. pp. 5369–76. [Google Scholar]
- 3.Krzizok T, Schwerdtfeger G. Bitemporal hemianopia in road traffic. Klin Monbl Augenheilkd. 2006 Sep;223(9):775–9. doi: 10.1055/s-2006-926999. [DOI] [PubMed] [Google Scholar]
- 4.Satgunam P, Apfelbaum HL, Peli E. Volume perimetry: measurement in depth of visual field loss. Optom Vis Sci. 2012;89(9):E1353–63. doi: 10.1097/OPX.0b013e3182678df8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kirkham TH. The ocular symptomatology of pituitary tumours. Proc R Soc Med. 1972 Jun;65(6):517–8. [PMC free article] [PubMed] [Google Scholar]
- 6.Arditi A. The volume visual field: a basis for functional perimetry. Clin Vis Sci. 1988;3(3):173–83. [Google Scholar]
- 7.Kubie LS, Beckmann JW. Diploplia without extra-ocular palsies, caused by heteronymous defects in the visual fields associated with defective macular vision. Brain. 1929;52:317–33. [PMC free article] [PubMed] [Google Scholar]
- 8.Elkington SG. Preoperative symptomatology in a series of 260 patients. Br J Ophthalmol. 1968;52:322–8. doi: 10.1136/bjo.52.4.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shainberg MJ, Roper-Hall G, Chung SM. Binocular Problems in Bitemporal Hemianopsia. Am Orthoptic J. 1995;45:132–40. [Google Scholar]
- 10.Fletcher DC, Schuchard RA, Renninger LW. Patient awareness of binocular central scotoma in age-related macular degeneration. Optom Vis Sci. 2012;89(9):1395–8. doi: 10.1097/OPX.0b013e318264cc77. [DOI] [PubMed] [Google Scholar]
- 11.Rosenbaum AL, Santiago AP. Clinical Strabismus Management: Principles and Surgical Techniques. Philadelphia: W. B. Saunders Company; 1999. [Google Scholar]
- 12.Blakemore C. Binocular depth perception and the optic chiasm. Vision Res. 1970 Jan;10(1):43–7. doi: 10.1016/0042-6989(70)90060-x. [DOI] [PubMed] [Google Scholar]
- 13.Howard IP. Seeing in Depth: Volume I. Ontario, Canada: I. Porteous; 2002. [Google Scholar]
- 14.Hubel DH. Eye, Brain and Vision. New York: W. H. Freeman & Co; 1988. The Corpus Callosum and Stereopsis; pp. 1–20. [Google Scholar]
- 15.Rashbass C, Westheimer G. Disjunctive eye movements. J Physiol. 1961;159:339–60. doi: 10.1113/jphysiol.1961.sp006812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mitchell DE, Blakemore C. Binocular depth perception and the corpus callosum. Vision Res. 1970 Jan;10(1):49–54. doi: 10.1016/0042-6989(70)90061-1. [DOI] [PubMed] [Google Scholar]
- 17.Carter DB. Effects of prolonged wearing of prism. Am J Optom Arch Am Acad Optom. 1963;40:265–73. doi: 10.1097/00006324-196305000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Woods RL, Apfelbaum HL, Peli E. DLP-based dichoptic vision test system. J Biomed Optics. 2010 Jan-Feb;15(1):1–13. doi: 10.1117/1.3292015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moses RA, William M, Hart J. Adler’sPhysiology of the Eye; Clinical Application. 8. St. Louis, MO: Mosby; 1987. [Google Scholar]
- 20.Datta SGS, Pathak HC. Traumatic chiasmal syndrome. Ind J Neurotr [Case report] 2009;6(2):137–40. [Google Scholar]
- 21.Laursen AB. Traumatic bitemporal hemianopsia. Survey of the literature and report of a case. Acta Ophthalmol (Copenh) 1971;49(1):134–42. doi: 10.1111/j.1755-3768.1971.tb08234.x. [DOI] [PubMed] [Google Scholar]
- 22.Heinz GW, Nunery WR, Grossman CB. Traumatic chiasmal syndrome associated with midline basilar skull fractures. Am J Ophthalmol. 1994 Jan 15;117(1):90–6. doi: 10.1016/s0002-9394(14)73020-x. [DOI] [PubMed] [Google Scholar]
- 23.Kawai K, Narita Y, Nagai A, Nakagomi T, Kobayashi K, Kirino T, et al. Traumatic chiasmal syndrome presenting with bitemporal hemianopsia. J Trauma. 1998 Jan;44(1):224–9. doi: 10.1097/00005373-199801000-00038. [DOI] [PubMed] [Google Scholar]
- 24.Elgamal E, Osman E, El-Watidy S, Jamjoom Z, Hazem A, Al-Khawajah N, et al. Pituitary Adenomas: Patterns Of Visual Presentation And Outcome After Transsphenoidal Surgery - An Institutional Experience. Internet J Ophthal Vis Sci [serial on the Internet] 2006;4(2) [Google Scholar]
- 25.Berkmann S, Fandino J, Müller B, Kothbauer KF, Henzen C, Landolt H. Reply to the letter to the editor “Visual outcomes after pituitary surgery”. Swiss Med Wkly. 2013:143. doi: 10.4414/smw.2013.13803. [DOI] [PubMed] [Google Scholar]
- 26.Borchert MS, Lessell S, Hoyt WF. Hemifield slide diplopia from altitudinal visual field defects. J Neuroophthalmol. 1996 Jun;16(2):107–9. [PubMed] [Google Scholar]
- 27.Wikipedia. Bitemporal Hemianopsia. 2103 Aug 31; Available from: http://en.wikipedia.org/wiki/Bitemporal_hemianopia.
- 28.Burian HM. Fusional movements: the role of peripheral retinal stimuli. Arch Ophthalmol. 1939;21:486–91. [Google Scholar]
- 29.Sullivan MJ, Kertesz AE. Peripheral stimulation and human cyclofusional response. Invest Ophthalmol Vis Sci. 1979;18(12):1287–91. [PubMed] [Google Scholar]
- 30.Peli E. Field expansion for homonymous hemianopia by optically-induced peripheral exotropia. Optom Vis Sci. 2000 Sep;77(9):453–64. doi: 10.1097/00006324-200009000-00006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.