Abstract
The emergence of carbapenem resistance in Enterobacteriaceae is an important threat to global health. Reported outcomes of infections with carbapenem-resistant Enterobacteriaceae (CRE) are poor. Very few options remain for the treatment of these virulent organisms. Antibiotics which are currently in use to treat CRE infections include aminoglycosides, polymyxins, tigecycline, fosfomycin, and temocillin. In addition, the role of combination therapy, including carbapenem containing regimens, remains to be defined. There are several important concerns regarding all of these treatment options such as limited efficacy, increasing reports of resistance, and specific toxicities. Data from retrospective studies favor combination therapy over single-agent therapy for the treatment of CRE bloodstream infections. In summary, new antibiotics are greatly needed, as is additional prospective research.
Keywords: Enterobacteriaceae, Carbapenem resistance, Multidrug resistance, Mortality, Bacteremia
1. Introduction
The prevalence of bacterial resistance to antibiotics continues to increase. Regrettably, infections caused by resistant organisms result in a tremendous morbidity and mortality worldwide. In the USA, associated annual additional costs of infections caused by resistant organisms as compared to susceptible organisms are estimated between $21 billion and $34 billion (Spellberg et al., 2011). The Infectious Diseases Society of America (IDSA) recognizes antimicrobial resistance as “one of the greatest threats to human health worldwide” (Spellberg et al., 2011). In addition, antimicrobial resistance was the focus of the 2011 World Health Day of the World Health Organization (WHO). The impact of multidrug resistance (MDR) extends into all aspects of medicine and threatens the significant progress which has been made in transplantation, oncology, and surgery. Understandably, much emphasis has been appropriately placed on methicillin-resistant Staphylococcus aureus (MRSA). In recent years, several new treatment options have become available for MRSA. In addition, true vancomycin resistance remains fortunately rare. However, the threat of MDR in Gram-negative organisms has not led to a similar increase in novel therapeutics. The prevalence of carbapenem resistance in Enterobacteriaceae (CRE) isolated from clinical samples continues to increase globally (Prabaker and Weinstein, 2011; Rhomberg and Jones, 2009; van Duijn et al., 2011).
In the USA, the major challenge at this time is presented by organisms that produce Klebsiella pneumoniae carbapenemase (KPC)–type serine carbapenemases. Especially for CRE, treatment options are generally extremely limited. Medications that retain in vitro activity against CRE are restricted by their side-effect profile, as well as by uncertain in vivo efficacy. While subject to large regional variation, the prevalence of CRE continues to increase globally (Prabaker and Weinstein, 2011; van Duijn et al., 2011).
2. Treatment options for CRE
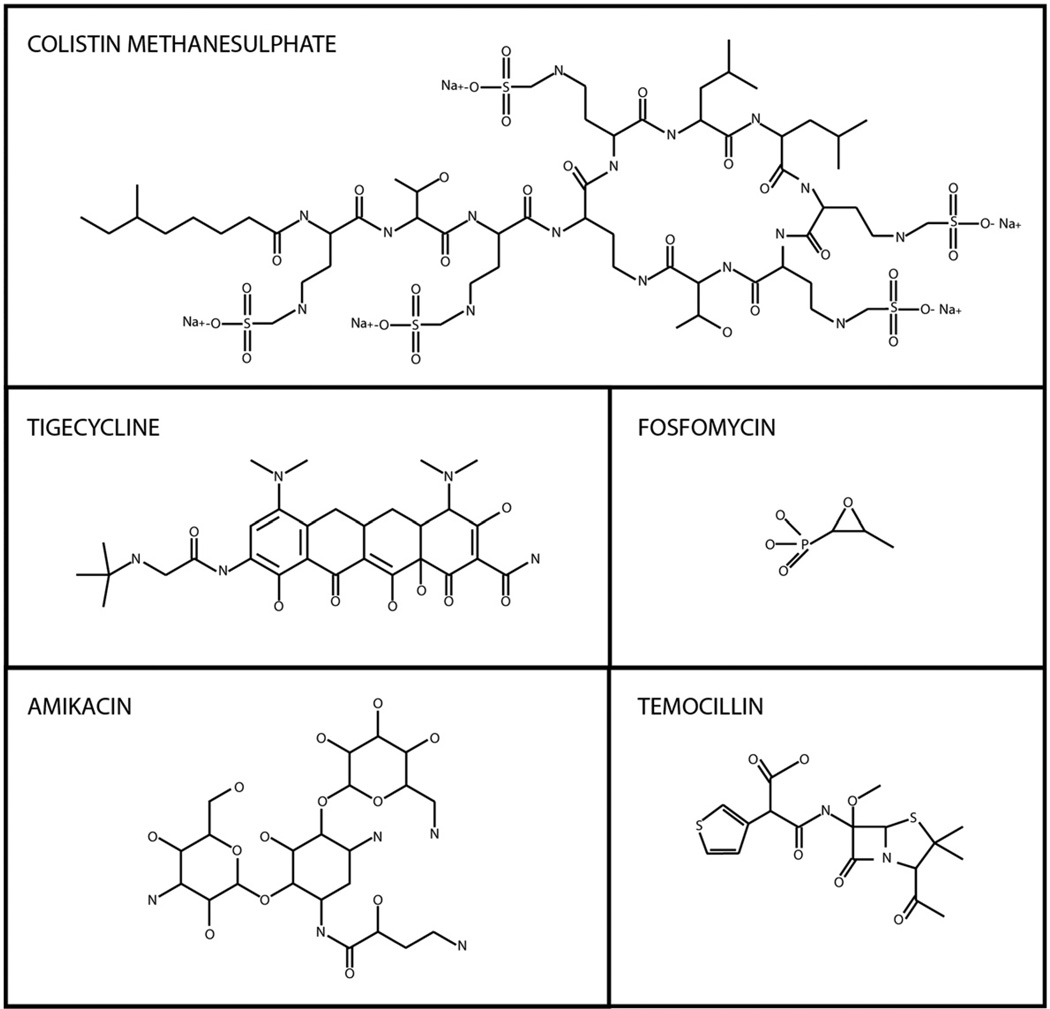
Few treatment options are currently available for CRE. Polymyxins, some aminoglycosides, and tigecycline generally retain in vitro activity against CRE, and these are the most commonly used “drugs of last resort” (Fig. 1). Some experts advocate the use of high-dose prolonged-infusion carbapenem therapy as part of a combination regimen in infections with CRE with carbapenem MICs ≤4 mg/L (Daikos and Markogiannakis, 2011). Also, in vitro and murine model data suggest that double-carbapenem therapy may be effective in some instances (Bulik and Nicolau, 2011). To date, reports evaluating the efficacy and safety of double-carbapenem therapy in the treatment of human infection are scarce. For now, colistin, tigecycline, and aminoglycosides remain the “mainstay of treatment” for invasive CRE infections. Combination therapy may be superior to monotherapy for CRE infections. In a countrywide study by the Veterans Affairs Medical Centers (VAMC) regarding the use of polymyxins and tigecycline, 22% of isolates associated with polymyxin use and 10% of isolates associated with tigecycline use were CRE (Huttner et al., 2012). An increase in days of therapy was observed for both tigecycline and polymyxins from 2006 to 2010. This increase was most pronounced for tigecycline, which showed a 4.2-fold increase. A strong correlation (R = 0.55) was observed between polymyxin use and local resistance when VAMC were analyzed per facility.
Fig. 1.
Chemical structures of antimicrobials which may have in vitro activity against carbapenem-resistant Enterobacteriaceae.
2.1. Polymyxins
Polymyxins, polymyxin E (also known as colistimethate) and polymyxin B, are cyclic peptides which differ by 1 amino acid and possess targeted Gram-negative activity. The mechanism of action is through an electrostatic interaction between the cationic polypeptide antimicrobial and the anionic lipopolysaccharides of the bacteria outer membrane leading to a leakage of cellular contents and, ultimately, bacterial cell lysis (Falagas and Kasiakou, 2005).
Colistin is given intravenously as a mix of various colistin methanesulphonate (CMS) or colistimethate compounds. CMS is available as 2 formulations that are labeled differently: Coly-Mycin M® (Monarch Pharmaceuticals, Bristol, TN, USA) in milligrams of colistin base activity and Colomycin® (Forest Laboratories, Bexley, UK) in international units (Table 1). Knowledge of colistimethate and colistin pharmacokinetics is currently evolving due to the advent of reliable assays that can distinguish colistimethate from colistin in biological fluids (Li et al., 2001, 2002).
Table 1.
Comparison of commercially available colistimethate sodium products.
| Colomycin® | Coly-Mycin M® | |
|---|---|---|
| Availability | Europe | USA, Australia |
| Dosing units | International units (IU) | Milligrams of colistin base activity (CBA) |
| Dosing conversion | 5 million IU = 400 mg colistimethate | 150 mg CBA = 400 mg colistimethate |
Colistin demonstrates nonlinear protein binding with both albumin and alpha-1-acid glycoprotein, an acute phase plasma protein (Dudhani et al., 2010). Colistimethate, the inactive prodrug, is hydrolyzed to active colistin and inactive sulfomethylated derivatives. Colistimethate primary undergoes renal clearance and has a short elimination half-life (2–3 h), whereas colistin has a longer half-life (9–13 h) and is minimally excreted in the urine due to extensive renal tubular reabsorption (Garonzik et al., 2011; Li et al., 2004). Reported volumes of distribution of central compartment CMS, peripheral compartment CMS, and formed colistin range from 5.3 to 13.5 L, 5.1 to 29.7L, and 7.2 to 189L, respectively (Couet et al., 2012).
Data describing polymyxin B pharmacokinetics are less available. The volume of distribution was 47 L, and the elimination half-life was 13 h in 1 small study (Jin et al., 2008). For both polymyxins, the pharmacodynamics are best described by area under the curve to minimum inhibitor concentration (AUC/MIC) ratio (Dudhani et al., 2010; Tam et al., 2005). A recent study on the use of CMS in critically ill patients suggests that high-dose extended-interval dosing may be associated with similar toxicity as traditional dosing (Dalfino et al., 2012).
The 2 major safety concerns with polymyxins are nephrotoxicity and neurotoxicity. The exact mechanism of nephrotoxicity is not well understood, and incidence in the contemporary literature varies from 14% to 53% (Falagas et al., 2005; Kwon et al., 2010; Ouderkirk et al., 2003). Total daily dose and longer durations of therapy correlate with increased risk of renal dysfunction; however, it is typically reversible after discontinuation of the drug (Hartzell et al., 2009; Pogue et al., 2011). Recent animal studies suggest possible attenuating effects with the use of melatonin and ascorbic acid (Yousef et al., 2011, 2012). Neurotoxicity can manifest as a spectrum from paresthesias to ataxia to neuromuscular blockade and is reported in approximately 4–6% of patients (Holloway et al., 2006; Linden et al., 2003).
2.2. Tigecycline
Tigecycline is a glycylcycline antimicrobial which was modified to overcome 2 major mechanisms of tetracycline resistance. Tigecycline is bacteriostatic and exerts its mechanism by binding to the 30S ribosomal subunit and inhibiting protein synthesis. In the USA, tigecycline is Food and Drug Administration (FDA) approved for the treatment of skin and skin structure infections, complicated intraabdominal infections, and community-acquired pneumonia.
Tigecycline has a large volume of distribution and extensive tissue penetration in skin, gallbladder, bowel, and intracellular pulmonary tissue (Rodvold et al., 2006). In contrast, the plasma concentrations of tigecycline are relatively low, maximum concentrations of 0.62 µg/mL at steady state dosing with 50 mg every 12 h (Meagher et al., 2005). Elimination primarily occurs through the feces via biliary excretion (59%) with a minority (15–22%) excreted in the urine as unchanged drug. Serum concentrations of tigecycline are generally deemed not adequate to treat blood stream infections, and tigecycline is not approved for this indication (Nix and Matthias, 2010; Tarchini, 2010). Tigecycline has a long elimination half-life, 42 h after multiple doses, and clearance is not affected by renal impairment or mild hepatic impairment.
Of greatest concern regarding the use of tigecycline as a single agent in the treatment of invasive infections are data which support an increased mortality in those patients treated with tigecycline as compared to other agents. In 2010, tigecycline received an FDA warning regarding increased mortality risk. Four recent meta-analyses have used different analytical tools and have come to different conclusions about this issue (Cai et al., 2011; Prasad et al., 2012; Tasina et al., 2011; Yahav et al., 2011). However, one is struck by the notion that a small but significant increased mortality risk exists with tigecycline, which is most likely secondary to decreased efficacy. For the purpose of this review, it should be noted that the trials studied in these meta-analyses were not designed with regard to the treatment of carbapenem-resistant pathogens.
The most common adverse effects associated with tigecycline therapy are nausea and vomiting. Although generally mild, these gastrointestinal complaints have been reported in up to 30% of patients in some studies and lead to more drug discontinuation in clinical trials versus the comparator antimicrobials.
2.3. Fosfomycin
Fosfomycin, a phosphonic acid derivative, is bactericidal against a broad spectrum of Gram-positive and Gram-negative organisms. The bacterial enzyme pyruvul transferase is inactivated by fosfomycin leading to inhibition of bacterial cell wall synthesis. It is currently available in the USA as an oral powdered sachet of 3 g of fosfomycin (equivalent to 5.61 g of fosfomycin tromethamine). In many European countries, both oral (as either the tromethamine or the calcium salt) and intravenous (as fosfomycin disodium) are available (Wisher, 2012).
Oral bioavailability is improved with the tromethamine salt (37% in fasting conditions) compared to the calcium salt (12%) due to poor solubility and acid degradation (Borsa et al., 1988). Fosfomycin has a low molecular weight and almost negligible protein binding, affording it good distribution into tissues including kidney, bladder wall, prostate, lung, soft tissues, bone, and cerebrospinal fluid (especially with inflamed meninges) (Kuhnen et al., 1987; Matzi et al., 2010; Schintler et al., 2009). Serum concentrations are not equivalent between oral and intravenous formulations, and the use of the oral formulation should generally be restricted to treatment of cystitis (Roussos et al., 2009). Primarily excreted unchanged in the urine (38%), high concentrations of fosfomycin tromethamine persist in the urine for up to 48–72 h. The elimination half-life is 2–3 h for fosfomycin disodium and 6 h for fosfomycin tromethamine in subjects with normal renal function. In patients with renal impairment, the urine recovery is lower and the half-life is significantly prolonged, up to 50 h (Michalopoulos et al., 2011).
Fosfomycin is generally well tolerated. The most common adverse effects of the oral formulations are gastrointestinal which are usually mild and transient. For the intravenous product, the most common adverse effects include phlebitis and allergic reactions. Laboratory alterations, including fluctuations in white blood cell count, eosinophils, bilirubin, and liver function tests, have been reported; however, the changes are generally transient and not clinically significant.
2.4. Aminoglycosides
The aminoglycosides inhibit protein synthesis by binding to the 30S subunit of the ribosome. Plazomicin (ACHN-490), a new sisomicin-derived aminoglycoside currently in development, joins currently available aminoglycosides (amikacin, gentamicin, and tobramycin) and has demonstrated in vitro activity against CRE (Endimiani et al., 2009). Primarily utilized for Gram-negative activity, aminoglycosides exhibit concentration-dependent activity and a prolonged post-antibiotic affect. The pharmacodynamic target for aminoglycosides is peak concentration to MIC ratios of 8–12:1 (Moore et al., 1987). Close monitoring of levels is recommended to ensure sufficient therapeutic levels while minimizing toxicity.
Pharmacokinetic properties are similar among all agents in the class (Edson and Terrell, 1999). They have a volume of distribution that approximates extracellular space. They distribute well into bone, peritoneal fluid, and urine, but have limited penetration into the cerebral spinal fluid and prostrate. The elimination half-life is highly dependent on age and renal function, but for adults with normal renal function it is around 2 h. Excretion is primarily in the urine through glomerular filtration. Aminoglycosides are often used as part of combination regimens.
Nephrotoxicity is one of the major adverse effects of aminoglycosides due to drug accumulation in the proximal renal tubular cells. Typically, nephrotoxicity related to aminoglycoside use is reversible. Ototoxicity is another adverse effect which is often irreversible and can manifest as vestibular or cochlear damage. For longer treatment courses, baseline and periodic follow-up audiology evaluations can be beneficial. Another serious, but less common adverse effect is neuromuscular blockade.
2.5. Temocillin
Temocillin, a semisynthetic derivative of ticarcillin, is primarily available in the United Kingdom and is not available in the USA. As with other beta-lactams, its mechanism is to bind to penicillin-binding proteins and inhibit cell wall synthesis. This drug displays time-dependent activity. Temocillin's spectrum of activity is limited to Enterobacteriaceae, but it is stable against a variety of beta-lactamases (Livermore et al., 2011). In a small in vitro study, the MIC50 and MIC90 were both 32 µg/mL for 33 KPC-producing organisms (mostly K. pneumoniae). Temocillin MIC breakpoints as per the British Society of Antimicrobial Chemotherapy are ≤8 and ≤32 µg/mL, for systemic and urinary infections, respectively. In a larger in vitro study, 4/81 and 26/81 CRE were susceptible at the ≤8 and ≤32 µg/mL breakpoints, respectively. Clinical studies are not available for its use in CRE. Pharmacokinetics are similar to ticarcillin. Temocillin distributes well to most tissues and has relatively high protein binding (70–85%) (Gould et al., 1985). It is primarily eliminated in the urine through glomerular filtration and tubular secretion. Half-life is normally 4–6 h but can be prolonged in renal insufficiency (Boelaert et al., 1983). Temocillin is generally well tolerated. As with other beta-lactams, allergic reactions such as rash can occur.
3. Treatment and outcomes
A number of case series and case reports have been published which describe the treatment and outcomes of patients with cultures positive for CRE. However, the expected outcomes and optimal treatment for CRE infections remain undefined at this time for a number of reasons. Firstly, these reports are, for the most part, small single-center, retrospective studies. Secondly, it is difficult to distinguish between infection and colonization, especially retrospectively, when CRE isolates are obtained from nonsterile sites such as wounds or the respiratory tract, or from urine. Thirdly, in the course of a single infectious episode with CRE, multiple antibiotics are often used, sequentially and/or in combination. Fourthly, co-infection or co-colonization with other pathogens is quite common. As risk factors for multidrug-resistant organisms overlap, these pathogens are often multidrug resistant themselves (Safdar and Maki, 2002). Some reports have excluded cases of polymicrobial infection, which improves internal validity, but limits generalizability. Also, CRE infections tend to be associated with delays in the time to effective therapy, which complicates the interpretation of the impact of therapy on outcomes. Finally, CRE are often isolated from patients with multiple comorbidities, which in itself is associated with an increased likelihood of a poor outcome (Neuner et al., 2011). Overall, isolation of CRE from any site—whether this represents clinical infection or not—is associated with poor outcomes. In case series, CRE isolation has been associated with all-cause hospital mortality ranging from 29% to 52% (Hyle et al., 2010; Ku et al., 2012; Marchaim et al., 2011; Souli et al., 2010; Won et al., 2011).
3.1. CRE bloodstream infections
Bloodstream infections (BSIs) with Gram-negative bacilli are generally associated with high mortality (Chow and Yu, 1999). Nonetheless, it is clear that mortality from BSI caused by CRE is increased as compared to BSI caused by more susceptible organisms (Ben-David et al., 2012; Daikos et al., 2009; Mouloudi et al., 2010). In addition, finding CRE in the bloodstream is associated with worse outcomes, as compared to isolation of CRE from other sites. In a case-control study, the impact on mortality of finding CRKP in the bloodstream was evaluated in patients with CRKP infections. Crude mortality was 72% for CRKP BSI, compared to 22% in patients with other sites of CRKP infection (Borer et al., 2009). Functional outcomes are also poor after CRKP BSI. In a series of 60 cases of CRKP BSI, 14-day and in-hospital all-cause mortality were 42% and 58%, respectively (Neuner et al., 2011). Additionally, readmissions were common in those patients who were discharged alive; 72% were readmitted to the hospital within 90 days. Also, most survivors were discharged to long-term care facilities (Neuner et al., 2011). Reported non–antibioticrelated risk factors for mortality in CRKP BSI include increased markers of chronic and acute morbidity such as the Charlson comorbidity score, Pitt bacteremia score, and APACHE II score, as well as age (Ben-David et al., 2012; Daikos et al., 2009; Neuner et al., 2011; Zarkotou et al., 2011).
Regarding optimal therapy for CRE BSI, there is an urgent need for randomized controlled trials to determine which of the currently available agents and, potentially, in which combinations, is associated with the best efficacy and safety profile. In addition, the development of new antibiotics for this important threat is clearly required. Retrospective comparisons favor combination therapy over single-agent therapy, with absolute differences in mortality ranging from 20.2% to 46.7% (Hirsch and Tam, 2010; Qureshi et al., 2012; Tumbarello et al., 2012; Zarkotou et al., 2011). In particular, the triple-drug combination of colistin, tigecycline, and meropenem was associated with lower mortality in one recent study (odds ratio for 30-day mortality 0.27, P = 0.009) (Tumbarello et al., 2012). However, multiple important biases may play an important role in the selection of treatment, and combination therapy may be a surrogate marker for an unmeasured confounding variable.
3.2. CRE urinary tract infections
CRE are most commonly isolated from urine in the majority of studies (Bratu et al., 2005; Marchaim et al., 2011; Perez et al., 2010). Patients who have exposure to extended care facilities and who have chronic indwelling urinary catheters appear to be at the highest risk (Wang et al., 2012). High rates of fecal carriage of CRE have also been reported from long-term care facilities, and these 2 issues likely are both reflective of the increased risk of long-term care residents for symptomatic CRE infections (Lautenbach et al., 2012; Stuart et al., 2011). Not surprisingly, chronic indwelling urinary catheters were found to be associated with an increased risk of fecal carriage of multidrug-resistant organisms (Wang et al., 2012). In addition, the role of long-term care facilities in the dissemination of CRE in health care systems has been highlighted (Perez et al., 2010). The goal of treatment must be clearly defined when evaluating outcomes of and various antibiotic strategies for CRE urinary tract infections. In addition, the impact of the management of urinary catheters—whether it remains in place, is replaced, or is discontinued—probably exceeds the relative impacts of various antibiotics regimens. If alternatives are available, tigecycline should be avoided for treatment of CRE UTI because of its low urinary concentration (Nix and Matthias, 2010). Based on limited available data, aminoglycosides appear to be associated with the highest rates of microbiologic clearance. In a retrospective case series of 21 patients with urinary tract infections with KPC-producing pathogens, all but 1 infection were caused by CRKP. Seven patients were treated with gentamicin, and all 7 had a good clinical and microbiological response (Alexander et al., 2012). Seven patients did not receive antibiotics with in vitro activity in this series; of these, 2 were noted to have a good clinical response and 3 had a good microbiologic response (Alexander et al., 2012). Another retrospective study specifically addressed the issue of clearing CRKP from urine, regardless of whether it represented infection or colonization (Satlin et al., 2011). In this study, aminoglycoside therapy (gentamicin or amikacin) was associated with significantly higher microbiologic clearance rates (88%), when compared to polymyxin B (64%), tigecycline (43%), and untreated (36%). It should be noted that only 10% of CRKP bacteriuria cases which occurred during the study period were included. All others were excluded, most commonly because CRKP was isolated from different sites or patients received an additional agent active against Gram-negative pathogens (Satlin et al., 2011).
The urinary agent fosfomycin given orally is, in theory, an attractive option if in vitro susceptibility is retained. However, while multiple studies have reported good in vitro activity of fosfomycin against urinary CRE isolates, clinical data of treating CRE UTI with fosfomycin are lacking (Karageorgopoulos et al., 2012). A report from France showed a 100% response rate in 16 urinary tract infections treated with intravenous fosfomycin for a median of 18 days. However, only 5 were Enterobacteriaceae (Dinh et al., 2012). It is difficult to extrapolate from these data as the specific antibiotic susceptibility patterns were not reported, combination therapy was common, and a prolonged intravenous course was given.
4. Conclusions
CRE are an increasing threat to our population. Invasive CRE infections are associated with worse outcomes as compared to carbapenem-susceptible Enterobacteriaceae infections. This is likely due in part to limited treatment options, which include aminoglycosides, polymyxins, tigecycline, fosfomycin, and temocillin. Available treatment options are limited by pharmacologic properties, side effect profiles, administration issues, and, most of all, efficacy limitations. Nephrotoxicity is the major adverse event associated with the use of aminoglycosides and polymyxins. Reports of increased mortality, increased resistance, and low blood levels limit the use of tigecycline. Fosfomycin is a useful agent for the treatment of urinary tract infections; however, in the USA its use is limited by a lack of availability of the intravenous formulation. With the currently available agents, combination therapy—which may include a carbapenem in spite of in vitro nonsusceptibility—appears to be the reasonable choice for invasive infections, especially bloodstream infections. Not surprisingly, increases in carbapenem MICs have been shown to be associated with increased risk of death. CRE are most commonly isolated from the urinary tract. In these cases, a careful distinction needs to be made between asymptomatic bacteriuria—which does not require treatment—and urinary tract infection. If treatment of urinary isolates is deemed necessary, removal of urinary catheters combined with fosfomycin or aminoglycosides is likely to result in the highest rate of microbiologic clearance. There is an urgent need for control of the spread of CRE by antimicrobial stewardship and infection control measures. In addition, as all our information regarding relative treatment efficacy and toxicity is derived from inherently flawed retrospective studies, randomized controlled trials to compare currently available treatment options are urgently required. Research towards development of novel antibiotics with targeted anti-CRE activity should be a top priority for the pharmaceutical industry, funding agencies, and governments worldwide.
Footnotes
This publication was made possible by a grant from the Clinical and Translational Science Collaborative of Cleveland, UL1TR000439, from the National Center for Advancing Translational Sciences (NCATS) component of the National Institutes of Health and NIH roadmap for Medical Research (D.v.D.). This work was supported in part by Public Health Service grants R01AI072219 and R01AI063517 (R.A.B.) from the National Institutes of Health and funds and/or facilities provided by the Cleveland Department of Veterans Affairs, the Veterans Affairs Merit Review Program, and the Geriatric Research Education and Clinical Center VISN 10 (R.A.B.). In addition, this work was supported by the Research Program Committees of the Cleveland Clinic (D.v.D.), by an unrestricted research grant from the STERIS Corporation (D.v.D.). and by the National Institute of Allergy and Infectious Diseases (NIAID); DMID Protocol Number: 10-0065 (K.S.K.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
This publication was made possible by the Clinical and Translational Science Collaborative of Cleveland, UL1TR000439, from the National Center for Advancing Translational Sciences (NCATS) component of the National Institutes of Health and NIH roadmap for Medical Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Alexander BT, Marschall J, et al. Treatment and clinical outcomes of urinary tract infections caused by KPC-producing Enterobacteriaceae in a retrospective cohort. Clin Ther. 2012;34:1314–1323. doi: 10.1016/j.clinthera.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-David D, Kordevani R, et al. Outcome of carbapenem resistant Klebsiella pneumoniae bloodstream infections. Clin Microbiol Infect. 2012;18:54–60. doi: 10.1111/j.1469-0691.2011.03478.x. [DOI] [PubMed] [Google Scholar]
- Boelaert J, Daneels R, et al. The pharmacokinetics of temocillin in patients with normal and impaired renal function. J Antimicrob Chemother. 1983;11:349–356. doi: 10.1093/jac/11.4.349. [DOI] [PubMed] [Google Scholar]
- Borer A, Saidel-Odes L, et al. Attributable mortality rate for carbapenem-resistant Klebsiella pneumoniae bacteremia. Infect Control Hosp Epidemiol. 2009;30:972–976. doi: 10.1086/605922. [DOI] [PubMed] [Google Scholar]
- Borsa F, Leroy A, et al. Comparative pharmacokinetics of tromethamine fosfomycin and calcium fosfomycin in young and elderly adults. Antimicrob Agents Chemother. 1988;32:938–941. doi: 10.1128/aac.32.6.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bratu S, Landman D, et al. Rapid spread of carbapenem-resistant Klebsiella pneumoniae in New York City: a new threat to our antibiotic armamentarium. Arch Intern Med. 2005;165:1430–1435. doi: 10.1001/archinte.165.12.1430. [DOI] [PubMed] [Google Scholar]
- Bulik CC, Nicolau DP. Double-carbapenem therapy for carbapenemase-producing Klebsiella pneumoniae. Antimicrob Agents Chemother. 2011;55:3002–3004. doi: 10.1128/AAC.01420-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Y, Wang R, et al. Systematic review and meta-analysis of the effectiveness and safety of tigecycline for treatment of infectious disease. Antimicrob Agents Chemother. 2011;55:1162–1172. doi: 10.1128/AAC.01402-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow JW, Yu VL. Combination antibiotic therapy versus monotherapy for Gram-negative bacteraemia: a commentary. Int J Antimicrob Agents. 1999;11:7–12. doi: 10.1016/s0924-8579(98)00060-0. [DOI] [PubMed] [Google Scholar]
- Couet W, Gregoire N, et al. Colistin pharmacokinetics: the fog is lifting. Clin Microbiol Infect. 2012;18:30–39. doi: 10.1111/j.1469-0691.2011.03667.x. [DOI] [PubMed] [Google Scholar]
- Daikos GL, Markogiannakis A. Carbapenemase-producing Klebsiella pneumoniae: (when) might we still consider treating with carbapenems? Clin Microbiol Infect. 2011;17:1135–1141. doi: 10.1111/j.1469-0691.2011.03553.x. [DOI] [PubMed] [Google Scholar]
- Daikos GL, Petrikkos P, et al. Prospective observational study of the impact of VIM-1 metallo-beta-lactamase on the outcome of patients with Klebsiella pneumoniae bloodstream infections. Antimicrob Agents Chemother. 2009;53:1868–1873. doi: 10.1128/AAC.00782-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalfino L, Puntillo F, et al. High-dose, extended-interval colistin administration in critically ill patients: is this the right dosing strategy? A preliminary study. Clin Infect Dis. 2012;54:1720–1726. doi: 10.1093/cid/cis286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinh A, Salomon J, et al. Fosfomycin: efficacy against infections caused by multidrug-resistant bacteria. Scand J Infect Dis. 2012;44:182–189. doi: 10.3109/00365548.2011.616221. [DOI] [PubMed] [Google Scholar]
- Dudhani RV, Turnidge JD, et al. Elucidation of the pharmacokinetic/pharmacodynamic determinant of colistin activity against Pseudomonas aeruginosa in murine thigh and lung infection models. Antimicrob Agents Chemother. 2010;54:1117–1124. doi: 10.1128/AAC.01114-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edson RS, Terrell CL. The aminoglycosides. Mayo Clin Proc. 1999;74:519–528. doi: 10.4065/74.5.519. [DOI] [PubMed] [Google Scholar]
- Endimiani A, Hujer KM, et al. ACHN-490, a neoglycoside with potent in vitro activity against multidrug-resistant Klebsiella pneumoniae isolates. Antimicrob Agents Chemother. 2009;53:4504–4507. doi: 10.1128/AAC.00556-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falagas ME, Bliziotis IA, et al. Outcome of infections due to pandrug-resistant (PDR) Gram-negative bacteria. BMC Infect Dis. 2005;5:24. doi: 10.1186/1471-2334-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falagas ME, Kasiakou SK. Colistin: the revival of polymyxins for the management of multidrug-resistant Gram-negative bacterial infections. Clin Infect Dis. 2005;40:1333–1341. doi: 10.1086/429323. [DOI] [PubMed] [Google Scholar]
- Garonzik SM, Li J, et al. Population pharmacokinetics of colistin methanesulfonate and formed colistin in critically ill patients from a multicenter study provide dosing suggestions for various categories of patients. Antimicrob Agents Chemother. 2011;55:3284–3294. doi: 10.1128/AAC.01733-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould JG, Meikle G, et al. Temocillin concentrations in human tissues. Drugs. 1985;29(Suppl 5):167–170. doi: 10.2165/00003495-198500295-00034. [DOI] [PubMed] [Google Scholar]
- Hartzell JD, Neff R, et al. Nephrotoxicity associated with intravenous colistin (colistimethate sodium) treatment at a tertiary care medical center. Clin Infect Dis. 2009;48:1724–1728. doi: 10.1086/599225. [DOI] [PubMed] [Google Scholar]
- Hirsch EB, Tam VH. Detection and treatment options for Klebsiella pneumoniae carbapenemases (KPCs): an emerging cause of multidrug-resistant infection. J Antimicrob Chemother. 2010;12:12. doi: 10.1093/jac/dkq108. [Epub April 8, 2010]. [DOI] [PubMed] [Google Scholar]
- Holloway KP, Rouphael NG, et al. Polymyxin B and doxycycline use in patients with multidrug-resistant Acinetobacter baumannii infections in the intensive care unit. Ann Pharmacother. 2006;40:1939–1945. doi: 10.1345/aph.1H353. [DOI] [PubMed] [Google Scholar]
- Huttner B, Jones M, et al. Drugs of last resort? The use of polymyxins and tigecycline at US Veterans Affairs Medical Centers: 2005–2010. PLoS One. 2012;7:e36649. doi: 10.1371/journal.pone.0036649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyle EP, Ferraro MJ, et al. Ertapenem-resistant Enterobacteriaceae: risk factors for acquisition and outcomes. Infect Control Hosp Epidemiol. 2010;31:1242–1249. doi: 10.1086/657138. [DOI] [PubMed] [Google Scholar]
- Jin Z, Yang YX, et al. Potato (Solanum tuberosum L. cv. Gogu valley) protein as a novel antimicrobial agent in weanling pigs. J Anim Sci. 2008;86:1562–1572. doi: 10.2527/jas.2007-0414. [DOI] [PubMed] [Google Scholar]
- Karageorgopoulos DE, Wang R, et al. Fosfomycin: evaluation of the published evidence on the emergence of antimicrobial resistance in Gram-negative pathogens. J Antimicrob Chemother. 2012;67:255–268. doi: 10.1093/jac/dkr466. [DOI] [PubMed] [Google Scholar]
- Ku K, Pogue JM, et al. Retrospective evaluation of colistin versus tigecycline for the treatment of Acinetobacter baumannii and/or carbapenem-resistant Enterobacteriaceae infections. Am J Infect Control. 2012;40(10):983–987. doi: 10.1016/j.ajic.2011.12.014. [DOI] [PubMed] [Google Scholar]
- Kuhnen E, Pfeifer G, et al. Penetration of fosfomycin into cerebrospinal fluid across non-inflamed and inflamed meninges. Infection. 1987;15:422–424. doi: 10.1007/BF01647220. [DOI] [PubMed] [Google Scholar]
- Kwon JA, Lee JE, et al. Predictors of acute kidney injury associated with intravenous colistin treatment. Int J Antimicrob Agents. 2010;35:473–477. doi: 10.1016/j.ijantimicag.2009.12.002. [DOI] [PubMed] [Google Scholar]
- Lautenbach E, Han J, et al. Colonization with extended-spectrum beta-lactamaseproducing Escherichia coli and Klebsiella species in long-term care facility residents. Infect Control Hosp Epidemiol. 2012;33:302–304. doi: 10.1086/664055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Milne RW, et al. A simple method for the assay of colistin in human plasma, using pre-column derivatization with 9-fluorenylmethyl chloroformate in solid-phase extraction cartridges and reversed-phase high-performance liquid chromatography. J Chromatogr B Biomed Sci Appl. 2001;761:167–175. doi: 10.1016/s0378-4347(01)00326-7. [DOI] [PubMed] [Google Scholar]
- Li J, Milne RW, et al. Simple method for assaying colistin methanesulfonate in plasma and urine using high-performance liquid chromatography. Antimicrob Agents Chemother. 2002;46:3304–3307. doi: 10.1128/AAC.46.10.3304-3307.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Milne RW, et al. Pharmacokinetics of colistin methanesulphonate and colistin in rats following an intravenous dose of colistin methanesulphonate. J Antimicrob Chemother. 2004;53:837–840. doi: 10.1093/jac/dkh167. [DOI] [PubMed] [Google Scholar]
- Linden PK, Kusne S, et al. Use of parenteral colistin for the treatment of serious infection due to antimicrobial-resistant Pseudomonas aeruginosa. Clin Infect Dis. 2003;37:e154–e160. doi: 10.1086/379611. [DOI] [PubMed] [Google Scholar]
- Livermore DM, Warner M, et al. What remains against carbapenem-resistant Enterobacteriaceae? Evaluation of chloramphenicol, ciprofloxacin, colistin, fosfomycin, minocycline, nitrofurantoin, temocillin and tigecycline. Int J Antimicrob Agents. 2011;37:415–419. doi: 10.1016/j.ijantimicag.2011.01.012. [DOI] [PubMed] [Google Scholar]
- Marchaim D, Chopra T, et al. Outcomes and genetic relatedness of carbapenem-resistant Enterobacteriaceae at Detroit medical center. Infect Control Hosp Epidemiol. 2011;32:861–871. doi: 10.1086/661597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matzi V, Lindenmann J, et al. Extracellular concentrations of fosfomycin in lung tissue of septic patients. J Antimicrob Chemother. 2010;65:995–998. doi: 10.1093/jac/dkq070. [DOI] [PubMed] [Google Scholar]
- Meagher AK, Ambrose PG, et al. Pharmacokinetic/pharmacodynamic profile for tigecycline—a new glycylcycline antimicrobial agent. Diagn Microbiol Infect Dis. 2005;52:165–171. doi: 10.1016/j.diagmicrobio.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Michalopoulos AS, Livaditis IG, et al. The revival of fosfomycin. Int J Infect Dis. 2011;15:e732–e739. doi: 10.1016/j.ijid.2011.07.007. [DOI] [PubMed] [Google Scholar]
- Moore RD, Lietman PS, et al. Clinical response to aminoglycoside therapy: importance of the ratio of peak concentration to minimal inhibitory concentration. J Infect Dis. 1987;155:93–99. doi: 10.1093/infdis/155.1.93. [DOI] [PubMed] [Google Scholar]
- Mouloudi E, Protonotariou E, et al. Bloodstream infections caused by metallo-beta-lactamase/Klebsiella pneumoniae carbapenemase-producing K. pneumoniae among intensive care unit patients in Greece: risk factors for infection and impact of type of resistance on outcomes. Infect Control Hosp Epidemiol. 2010;31:1250–1256. doi: 10.1086/657135. [DOI] [PubMed] [Google Scholar]
- Neuner EA, Yeh J-Y, et al. Treatment and outcomes in carbapenem-resistant Klebsiella pneumoniae bloodstream infections. Diagn Microbiol Infect Dis. 2011;69:357–362. doi: 10.1016/j.diagmicrobio.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nix DE, Matthias KR. Should tigecycline be considered for urinary tract infections? A pharmacokinetic re-evaluation. J Antimicrob Chemother. 2010;65:1311–1312. doi: 10.1093/jac/dkq116. [DOI] [PubMed] [Google Scholar]
- Ouderkirk JP, Nord JA, et al. Polymyxin B nephrotoxicity and efficacy against nosocomial infections caused by multiresistant Gram-negative bacteria. Antimicrob Agents Chemother. 2003;47:2659–2662. doi: 10.1128/AAC.47.8.2659-2662.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez F, Endimiani A, et al. Carbapenem-resistant Acinetobacter baumannii and Klebsiella pneumoniae across a hospital system: impact of post-acute care facilities on dissemination. J Antimicrob Chemother. 2010;65:1807–1818. doi: 10.1093/jac/dkq191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pogue JM, Lee J, et al. Incidence of and risk factors for colistin-associated nephrotoxicity in a large academic health system. Clin Infect Dis. 2011;53:879–884. doi: 10.1093/cid/cir611. [DOI] [PubMed] [Google Scholar]
- Prabaker K, Weinstein RA. Trends in antimicrobial resistance in intensive care units in the United States. Curr Opin Crit Care. 2011;17:472–479. doi: 10.1097/MCC.0b013e32834a4b03. [DOI] [PubMed] [Google Scholar]
- Prasad P, Sun J, et al. Excess deaths associated with tigecycline after approval based on noninferiority trials. Clin Infect Dis. 2012;54:1699–1709. doi: 10.1093/cid/cis270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qureshi ZA, Paterson DL, et al. Treatment outcome of bacteremia due to KPC-producing Klebsiella pneumoniae: superiority of combination antimicrobial regimens. Antimicrob Agents Chemother. 2012;56:2108–2113. doi: 10.1128/AAC.06268-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhomberg PR, Jones RN. Summary trends for the Meropenem Yearly Susceptibility Test Information Collection Program: a 10-year experience in the United States (1999–2008) Diagn Microbiol Infect Dis. 2009;65:414–426. doi: 10.1016/j.diagmicrobio.2009.08.020. [DOI] [PubMed] [Google Scholar]
- Rodvold KA, Gotfried MH, et al. Serum, tissue and body fluid concentrations of tigecycline after a single 100 mg dose. J Antimicrob Chemother. 2006;58:1221–1229. doi: 10.1093/jac/dkl403. [DOI] [PubMed] [Google Scholar]
- Roussos N, Karageorgopoulos DE, et al. Clinical significance of the pharmacokinetic and pharmacodynamic characteristics of fosfomycin for the treatment of patients with systemic infections. Int J Antimicrob Agents. 2009;34:506–515. doi: 10.1016/j.ijantimicag.2009.08.013. [DOI] [PubMed] [Google Scholar]
- Safdar N, Maki DG. The commonality of risk factors for nosocomial colonization and infection with antimicrobial-resistant Staphylococcus aureus, Enterococcus, Gram-negative bacilli, Clostridium difficile, and Candida. Ann Intern Med. 2002;136:834–844. doi: 10.7326/0003-4819-136-11-200206040-00013. [DOI] [PubMed] [Google Scholar]
- Satlin MJ, Kubin CJ, et al. Comparative effectiveness of aminoglycosides, polymyxin B, and tigecycline for clearance of carbapenem-resistant Klebsiella pneumoniae from urine. Antimicrob Agents Chemother. 2011;55:5893–5899. doi: 10.1128/AAC.00387-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schintler MV, Traunmuller F, et al. High fosfomycin concentrations in bone and peripheral soft tissue in diabetic patients presenting with bacterial foot infection. J Antimicrob Chemother. 2009;64:574–578. doi: 10.1093/jac/dkp230. [DOI] [PubMed] [Google Scholar]
- Souli M, Galani I, et al. An outbreak of infection due to beta-Lactamase Klebsiella pneumoniae carbapenemase 2-producing K. pneumoniae in a Greek university hospital: molecular characterization, epidemiology, and outcomes. Clin Infect Dis. 2010;50:364–373. doi: 10.1086/649865. [DOI] [PubMed] [Google Scholar]
- Spellberg B, Blaser M, et al. Combating antimicrobial resistance: policy recommendations to save lives. Clin Infect Dis. 2011;52(Suppl. 5):S397–S428. doi: 10.1093/cid/cir153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart RL, Kotsanas D, et al. Prevalence of antimicrobial-resistant organisms in residential aged care facilities. Med J Aust. 2011;195:530–533. doi: 10.5694/mja11.10724. [DOI] [PubMed] [Google Scholar]
- Tam VH, Schilling AN, et al. Pharmacodynamics of polymyxin B against Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2005;49:3624–3630. doi: 10.1128/AAC.49.9.3624-3630.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarchini G. Tigecycline and bacteremia—the dangers of post hoc analysis of pooled data. Clin Infect Dis. 2010;51:867–868. doi: 10.1086/656289. [author reply 868]. [DOI] [PubMed] [Google Scholar]
- Tasina E, Haidich AB, et al. Efficacy and safety of tigecycline for the treatment of infectious diseases: a meta-analysis. Lancet Infect Dis. 2011;11:834–844. doi: 10.1016/S1473-3099(11)70177-3. [DOI] [PubMed] [Google Scholar]
- Tumbarello M, Viale P, et al. Predictors of mortality in bloodstream infections caused by KPC-producing Klebsiella pneumoniae: importance of combination therapy. Clin Infect Dis. 2012;55(7):943–950. doi: 10.1093/cid/cis588. [DOI] [PubMed] [Google Scholar]
- van Duijn PJ, Dautzenberg MJ, et al. Recent trends in antibiotic resistance in European ICUs. Curr Opin Crit Care. 2011;17:658–665. doi: 10.1097/MCC.0b013e32834c9d87. [DOI] [PubMed] [Google Scholar]
- Wang L, Lansing B, et al. Infection rate and colonization with antibiotic-resistant organisms in skilled nursing facility residents with indwelling devices. Eur J Clin Microbiol Infect Dis. 2012;31(8):1797–1805. doi: 10.1007/s10096-011-1504-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisher D. Martindale: the complete drug reference: 37th edition. J Med Libr Assoc. 2012;100:U75–U110. [Google Scholar]
- Won SY, Munoz-Price LS, et al. Emergence and rapid regional spread of Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae. Clin Infect Dis. 2011;53:532–540. doi: 10.1093/cid/cir482. [DOI] [PubMed] [Google Scholar]
- Yahav D, Lador A, et al. Efficacy and safety of tigecycline: a systematic review and metaanalysis. J Antimicrob Chemother. 2011;66:1963–1971. doi: 10.1093/jac/dkr242. [DOI] [PubMed] [Google Scholar]
- Yousef JM, Chen G, et al. Melatonin attenuates colistin-induced nephrotoxicity in rats. Antimicrob Agents Chemother. 2011;55:4044–4049. doi: 10.1128/AAC.00328-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yousef JM, Chen G, et al. Ascorbic acid protects against the nephrotoxicity and apoptosis caused by colistin and affects its pharmacokinetics. J Antimicrob Chemother. 2012;67:452–459. doi: 10.1093/jac/dkr483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarkotou O, Pournaras S, et al. Predictors of mortality in patients with bloodstream infections caused by KPC-producing Klebsiella pneumoniae and impact of appropriate antimicrobial treatment. Clin Microbiol Infect. 2011;17:1798–1803. doi: 10.1111/j.1469-0691.2011.03514.x. [DOI] [PubMed] [Google Scholar]