INTRODUCTION
The current prevalence of hypertension in children is estimated to be about 1-5%, with higher rates among minority adolescents1-3. Primary hypertension (PH) also referred to as essential hypertension, previously considered a disease of adulthood, has now become increasingly common in the pediatric population largely due to the obesity epidemic4,5. Obese children are three times more likely to develop hypertension than their non-obese counterparts6,7. This review therefore focuses on obesity-related teenage hypertension. We also discuss hypertension in non-obese teenagers where significant data exist.
The relationship between obesity and hypertension has been clearly defined in multiple studies across different ethnic and gender groups1,7-12. The etiology of obesity related hypertension has been linked to sympathetic hyperactivity, insulin resistance and vascular structure changes13,14. Sorof et al demonstrated the presence of sympathetic nervous system hyperactivity in obese school- age children, evidenced by increased heart rate and blood pressure variability which contributed to the pathogenesis of isolated systolic hypertension in this cohort 7. Increased sodium content of the cerebrospinal fluid has been shown to increase sympathetic nervous system activity through activation of the renin- angiotensin- aldosterone pathway in the brain13,14. Obese individuals have selective insulin resistance, which leads to increased sympathetic activity and alteration of vascular reactivity and resultant sodium retention as evidenced by decreased urinary sodium excretion15. The lessons learned from the study of the obese hypertensive individuals can be largely applied to the diverse population of hypertensive children.
DEFINITION AND CLASSIFICATION OF PEDIATRIC HYPERTENSION
Pediatric hypertension is usually asymptomatic and can easily be missed by healthcare professionals. The National Heart, Lung and Blood Institute (NHLBI) of the National Institute of Health (NIH) commissioned the Task Force on Blood Pressure Control in Children to develop normative standards for blood pressure. These standards were derived from the survey of more than 83,000 person-visits of infants and children. The percentile curves describe age-specific and gender-specific distributions of systolic and diastolic BP in infants and children adjusted for height 16 and have been updated periodically.
Hypertension in children and adolescents is diagnosed based on age, gender and height- specific references. Hypertension is defined as systolic and/ or diastolic BP greater than the 95th percentile for age, gender and height on three or more separate occasions. BP greater than 90th percentile but less than the 95th percentile for age, sex and height defines “pre-hypertension” and represents a category of patients at high risk for developing hypertension 2,3,17-19. It is crucial for the health care providers to be aware that the BP at the 90th percentile for an older child often exceeds the adult threshold for pre-hypertension of 120/80mmHg. As a result, beginning at 12 years of age, the BP range that defines pre-hypertension includes any BP reading of greater than 120/80mmHg, even if it is less than the 90th percentile 16. We now know that pre-hypertension may not be completely benign and the rate of progression to hypertension was reported to be 7% per year over a 2-year interval 18. Stage I hypertension refers to systolic and or diastolic BP greater than the 95th percentile but less than or equal to the 99th percentile plus 5 mm Hg. There is no data on the progression from stage I to stage II hypertension in children. Stage II hypertension is defined as systolic and/or diastolic BP greater than the 99th percentile plus 5 mm Hg. This represents a more severe form of hypertension, commonly associated with target organ damage. An analysis by the National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents revealed an increased risk for left ventricular hypertrophy (LVH) 20 in participants with stage II hypertension. Surprisingly, in some studies children and adolescents with pre-hypertension have also been found to have a substantially increased left ventricular mass index with a two-fold higher prevalence of LVH than their normotensive counterparts21-23. Classification of hypertension is summarized in Table 1.
Table 1.
Definition and classification of hypertension in children
| Normotensive children | Systolic and/ or diastolic blood pressure < 90th percentile for sex, age and height |
| Pre-hypertension | Systolic and/or diastolic blood pressure greater than the 90th but less than the 95th percentile or blood pressure > 120/80mmHg but less than the 95th percentile. |
| Stage I Hypertension | Systolic and/ or diastolic blood pressure greater than the 95th but less than the 99th percentile plus 5mmHg |
| Stage II Hypertension | Systolic and/or diastolic blood pressure greater than the 99th percentile plus 5mmHg for sex, age and height |
Adapted from Lurbe E, Alvarez J, Redon J. Diagnosis and treatment of hypertension in children. Current hypertension reports 2010;12:480-6; with permission.120
Primary and Secondary Hypertension
Based on the etiology, hypertension can be categorized as primary or essential hypertension (PH) when there is no identifiable cause and secondary hypertension (SH) when there is an underlying cause for hypertension. PH is now the most common cause of hypertension in adolescents and young adults. It is usually characterized by stage I (mild) hypertension and associated with a positive family history of hypertension24. SH should be considered in very young children, those with stage II hypertension and in children with clinical features that suggest systemic diseases associated with hypertension. SH may be due to:
an underlying renal parenchymal disease,
endocrine disease,
vascular or
neurological condition.
Key Message:
Diagnosis of pediatric hypertension is often missed due to the absence of symptoms
Hypertension is diagnosed based on age, gender and height-specific references
- 3 stages of hypertension are:
- ✓pre-hypertension
- ✓stage I hypertension
- ✓stage II hypertension
Based upon etiology, hypertension can be either primary (no identifiable cause) or secondary (underlying cause present)
RISK FACTORS FOR ESSENTIAL HYPERTENSION
A parental family history of hypertension is linked to a twofold-increased risk of developing essential hypertension in children and young adults24-27. This association led to extensive research to elucidate the underlying genetic etiology of PH. Family studies have shown that 20- 40% of cases seen are genetically determined. Different monogenic causes of PH have been established including mutations in the corticosteroidogenic genes, CYP11B1, and HSD11B2 28-30, mutations in the epithelial sodium channel (SCNN1B, SCNN1G), in the WNK serinethreonine kinase, 31,32 and polymorphisms in the renin-angiotensin-aldosterone system (RAAS) 30,33,34. However, pure monogenic causes of PH are still rare.
In a 10- year longitudinal study, African American children were shown to have a significantly greater elevation in systolic BP compared with white children from childhood to adulthood even after adjusting for height, body mass index and socioeconomic status35-38. Recently, mutations in the apolipoprotein-L1 gene in chromosome 22 were discovered and seem to explain the increased prevalence of hypertension-associated nephropathy in the African American population39,40. These mutations are thought to have an autosomal recessive pattern of inheritance and patients who are homozygous for the mutations have a higher likelihood for developing hypertension associated nephropathy, focal segmental glomerulosclerosis and HIV associated nephropathy40-43.
Increasing age and body mass index (BMI) have also been significantly associated with the development of hypertension 44 with a higher prevalence in African Americans and Asians45. There is a growing body of evidence on the inverse relationship between birth weight and hypertension in children and adolescents. A strong association has been observed among patients with a history of low birth weight and intrauterine growth retardation and a more significant relationship is seen when adjustments are made for current body weight. 46-50.
In a recent study by Yang et al, children were found to consume between 1,300mg and 8,100mg of sodium a day (mean of 3,387mg)51. Those with the highest sodium intake were shown to be twice as likely to have elevated blood pressures compared to those with lower sodium intake. This effect was more pronounced in the overweight and obese children. Overweight or obese children in the highest quartile of sodium consumption had more than three times the risk of elevated or high blood pressure as overweight children in the lowest quartile of sodium consumption51.
Key message:
Risk factors for developing primary hypertension:
○ Family history has been linked to increased risk
○ Racial predilection has been seen, African-American population being at higher risk
○ Increasing age and body mass index
○ Low birth weight and intra-uterine growth retardation
○ Increased sodium consumption
DIAGNOSIS OF HYPERTENSION
Clinical evaluation of a hypertensive teen
History
A thorough history is essential in guiding the evaluation and management of a hypertensive adolescent. Detailed information regarding the timing when elevated BP were first noted and the presence of co-morbid conditions is crucial for establishing the diagnosis. For this age group, the clinical history should include questions about the use of anabolic steroids, stimulants and caffeine containing energy drinks which can elevate the BP52. A history of snoring in an obese individual should prompt the evaluation for obstructive sleep apnea. History suggestive of renal disease or an endocrine tumor should be elicited.
Physical Examination
A comprehensive physical examination could suggest the underlying cause of hypertension in children and the presence of target organ damage. Attention to the body mass index is essential to identify overweight and obese patients. Table 2 summarizes the physical findings and laboratory investigations to look for common causes of secondary hypertension in the adolescent.
Table 2.
Physical findings and Diagnostic Evaluation of a Hypertensive Adolescent
| Physical Examination | Etiology | Investigation |
|---|---|---|
| General: Overweight, obese, acanthosis nigricans | Primary hypertension/metabolic syndrome | Urinalysis, fasting blood sugar, lipid panel. ABPM to rule out white coat hypertension |
| Edema, pallor, palpable kidneys on abdominal exam (Polycystic kidney disease), rash, arthralgia, growth retardation | Renal parenchymal disease | Urinalysis, serum creatinine, electrolytes, protein/ creatinine, ANA, dsDNAse, complements C3/C4, renal ultrasound |
| Tachycardia, widened pulse pressure, enlarged thyroid, weight loss, tremor | Hyperthyroidism | Thyroid function test: Free T4 and TSH |
| Moon facies, acne, hirsutism, truncal obesity, striae | Cushing's syndrome, steroid therapy, Liddle syndrome | Serum electrolytes, cortisol level, serum aldosterone |
| Weak lower extremity pulses, BP in upper limbs more than 10mmHg greater than lower extremity BP | Coarctation of the aorta | Echocardiography |
| Abdominal bruit | Renal artery stenosis | Renal artery angiography, captopril scintigraphy. |
| Tachycardia, flushing, visual disturbances, episodic hypertension | Pheochromocytoma | 24-hour urine metanephrine. I131 or I123 meta-iodo-benzyl- guanidine |
| Café-au lait spots, axillary or inguinal freckling | Neurofibromatosis | CT scan or MRI |
| Bradycardia, widen pulse pressure | CNS lesion: tumor, bleed | CT scan or MRI |
Blood Pressure Measurement
To obtain an accurate resting BP, patients should be allowed to sit for at least 5 minutes with the back supported and both feet on the ground16. A study of 390 children evaluated at 580 visits by Podoll et al revealed that 74% of BP readings were predominantly higher at the vital sign station using oscillometric devices compared with reading taken by auscultation in the examination room by personnel trained according to the Fourth Task Force recommendations.16,53 Mean differences of 13.2 ± 8.9mmHg for systolic and 9.6 ± 7.6mmHg for diastolic BP were seen. This highlights the importance of proper technique and the need to carefully re-evaluate initial elevated BP readings53.
Blood pressure should be measured with an appropriate-sized cuff in an upper extremity. The preferred method of measurement is by auscultation especially since the normative BP tables for children are based on similar measurements. An appropriate-sized cuff should have an inflatable bladder width that spans at least 40% of the patient’s arm circumference measured at the midpoint between the olecranon (elbow) and the acromion (shoulder). The bladder length should cover 80 to 100% of the arm circumference16. While previous recommendations to determine cuff adequacy included cuff length, current recommendations are based on the cuff width only. Previous recommendations from The Working Group of the Task Force on high blood pressure in children and adolescents was that the width of the BP cuff should cover at least three quarters of the length of the arm measured from the acromion to the olecranon 54. This was however found to result in an exaggeration in pediatric cuff choice. A review by Arafat et al evaluated the appropriateness of this recommendation and reported that if three quarters of the arm length is used to determine cuff size, there would be an overestimation in pediatric cuff selection 55. An update on the Task Force recommendations in 1996 included recommendations for the cuff width of 40% of the mid upper arm circumference with no reference to cuff length or the reason for the change in recommendations 54. The updated recommendation is thought to be due to the fact that the bladder width should be 40% to 50% of the mid upper arm circumference supported by evidence that the correct bladder width to arm circumference ratio is 0.4 55.
BP readings are overestimated when the cuff size is too small increasing the possibility of a wrong diagnosis of hypertension. Elevated BP readings that exceed the 90th percentile obtained by oscillometric devices should be confirmed by auscultation.
In the outpatient setting, documented elevations in blood pressures on 3 separate occasions at least one week apart are essential to confirm the diagnosis. Alternatively, ambulatory blood pressure monitoring (ABPM) could be performed to arrive at the diagnosis of hypertension56-58.
Ambulatory Blood Pressure Monitoring (ABPM)
ABPM forms the basis for the diagnosis when there is discordance in BP readings between daytime ambulatory BP measurements and office BP readings. It is particularly useful in patients with white coat or isolated clinic hypertension and masked hypertension. White coat hypertension is defined as office hypertension and ambulatory normotension while masked hypertension, the opposite, refers to ambulatory hypertension and office normotension.
ABPM utilizes oscillometric measures to obtain BP measurements. BP are measured every 20 to 30 minutes in the patient's home environment over a 24 hour period. Patients are advised to continue their routine activities but avoid rigorous activities during this monitoring period. A record of the actual sleep and wake times is maintained by the patients to enable evaluation of nocturnal dipping patterns and nocturnal hypertension. In our practice, we measure BP every 30 minutes during the day and every hour at night. An adequate ABPM report should have at least 40 to 50 BP readings with at least one reading every hour including at nighttime59. BP load is the percent of BP above the 95th percentile for age, gender and height in the 24-hour period. Based on the ABPM, hypertension is defined as elevated mean systolic BP above the 95th blood pressure percentile and/ or an elevated BP load above 25%. Normative standards have been established and are available for ambulatory BP measurements60.
Twenty-four hour ABPM has become commonplace in pediatric nephrology clinics for diagnosing white coat hypertension and masked hypertension and there is growing evidence supporting its use in the pediatric population. 57,58,60-64. Nephrology groups own and perform ABPM; it is less commonly performed by the cardiologist and rarely by the endocrinologist. Recently Davis et al recommended incorporating ABPM in the primary care setting to increase diagnostic accuracy of hypertension and avoid unnecessary treatment 65. This makes it important for primary care providers to be familiar with the role of ABPM for their patients with discordant BP readings or other diagnostic challenges.
The prevalence of white coat hypertension and masked hypertension in the general population are reported to be 1% and 10% respectively66. Patients with white coat hypertension have a lower risk for cardiovascular mortality than those with masked or sustained hypertension, although they have a greater risk for developing sustained hypertension later67-69. White coat hypertension in children is not associated with the development of LVH or hypertension-related kidney damage unlike PH, which has been linked to microalbuminuria 70-72. It has however been related to a slight increase in left ventricular mass index intermediate in range between normotensive and hypertensive subjects. This finding was highlighted in a study by Lande et al where 81 patients were divided in three groups matched for age and BMI. They were studied and found to have mean left ventricular mass indices of 29.2, 32.3 and 25.1 g/m2 in the normotensive, white coat hypertensive and sustained hypertensive groups respectively73. White coat hypertension has been associated with increased pulse wave velocity which is a marker of increased arterial stiffness and it might signify a greater cardiovascular risk than previously thought 74.
Masked hypertension has also been found to be associated with increased cardiovascular mortality and other target organ damage in adults75. In a study of 592 children aged between 5 and 18 years, Lurbe et al showed that patients with masked hypertension were more likely to be obese and have a family history of hypertension and were at an increased risk of developing sustained hypertension. Masked hypertension was shown to be a precursor of sustained hypertension and LVH in young children and adolescents66. The risk for LVH was found to be similar between participants with stage 1 hypertension and masked hypertension72.
ABPM has been demonstrated to be more closely associated with target organ damage and increased left ventricular mass index, leading to increased cerebrovascular events and a concomitant increase in cardiovascular mortality risk. 73,76,77 White coat hypertension is linked to a low risk for stroke, a finding by Verdicchia et al who reported a hazard ratio for stroke of 1.15 and 2.01 in patients with white coat hypertension and sustained hypertension respectively 78. Researchers from the Dublin outcome study proposed ambulatory arterial stiffness index as a novel marker of cardiovascular mortality. 79-81.
Investigations in a Hypertensive Adolescent
I. Initial Investigations
Initial evaluation should include a urinalysis, serum creatinine and echocardiography to evaluate for LVH. Renal sonography need not be routinely performed in the obese adolescent with a normal physical examination and normal urinalysis results. This was confirmed in a retrospective study by Tuli et al were routine renal imaging in 50 children did not provide any additional diagnostic information to the initial evaluation 82. These recommendations are similar to the evaluation of an adult hypertensive patient.
II. Subsequent Investigations
This includes fasting blood sugar and lipid profile in the obese teenager to rule out co-morbid conditions.
III. Selected Tests in Unusual Cases
Further investigations should be guided by the history, risk factors and symptoms identified as outlined in Table 2.
Key Message:
Detailed history and comprehensive physical examination is important to look for underlying cause of hypertension and other co-morbid conditions
Blood pressure estimation by proper technique is crucial
Elevated BP readings >90th percentile obtained by oscillometric devices should be confirmed by auscultation
BP readings are overestimated when the cuff size is small
Elevated blood pressure on 3 separate occasions at least one week apart are essential to confirm the diagnosis
Ambulatory BP monitoring may be performed to diagnose hypertension in cases of discordance between ambulatory BP and office BP readings
MANAGEMENT OF A HYPERTENSIVE TEEN
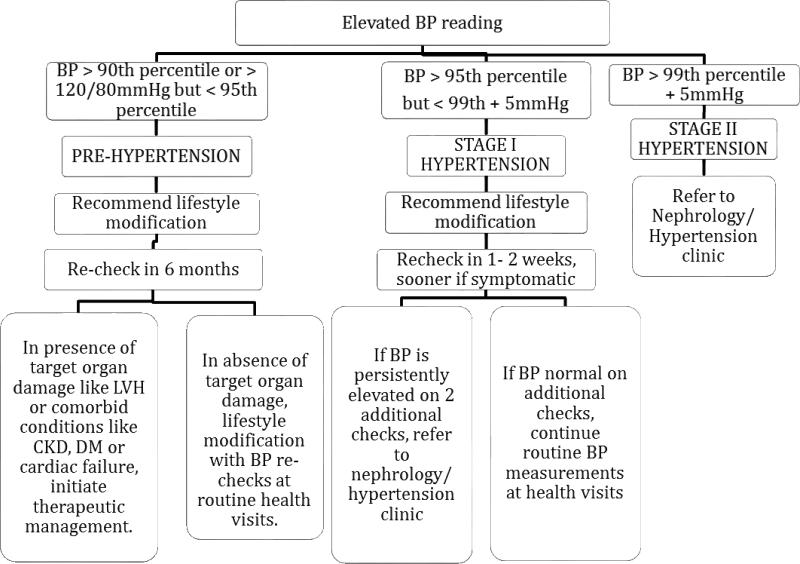
After the diagnosis of hypertension is reached, management should be tailored to the individual patient52. Figure 1 shows an algorithm for the management of teenage hypertension according to the severity.
Figure 1.
Management of hypertension based on severity.
Adapted from Lande et al and The Fourth Task Force for the Diagnosis, Evaluation and Treatment of High Blood Pressure in Children and Adolescents; and Lande MB, Flynn JT. Treatment of hypertension in children and adolescents. Pediatric nephrology (Berlin, Germany) 2009;24:1939-49; with permission.16,52
I. Therapeutic Lifestyle Modification
This is the first line of management of pediatric hypertension and can be the sole modality of therapy in patients diagnosed with pre-hypertension and stage I hypertension. It focuses on dietary management, increased physical activity, stress reduction and avoidance of illicit drug and tobacco use83-85. Dietary management should include an age appropriate, salt-restricted diet with emphasis on weight loss in the overweight or obese children. To have a better chance of success, the entire family should adopt these lifestyle modifications and a primary provider can be instrumental in this endeavor.
II. Pharmacological Therapy
The available evidence on the therapeutic management of pediatric hypertension is based on available evidence and consensus expert opinion when such evidence is lacking. The Fourth Task Force report on High Blood Pressure in Children and Adolescents include the following indications for pharmacological therapy16:
Symptomatic hypertension
Persistent hypertension despite lifestyle modification
Secondary hypertension
Presence of hypertensive target organ damage such as LVH, hypertensive retinopathy, microalbuminuria
Presence of co-morbid conditions that increase cardiovascular risk like diabetes mellitus 16
For patients with uncomplicated PH, the target BP is less than the 95th percentile for age, gender, and height; while it is less than the 90th percentile for patients with co-morbid conditions like diabetes, chronic kidney disease and in those with evidence of target organ damage16.
Choice of antihypertensive medications
There are no specific recommendations on the optimal first line agent for the treatment of pediatric hypertension52,86. The classes of antihypertensive medications that can be used in the pediatric hypertensive patient include:
calcium channel blockers (CCB),
angiotensin converting enzyme inhibitors (ACEI),
angiotensin receptor blocker (ARB),
diuretics, beta-blockers (BB),
alpha-blockers,
central acting agents, vasodilators,
combined alpha and beta-adrenergic antagonists,
renin inhibitors and
Commonly used formulations from the different classes are shown in Table 3.
Table 3.
Classes of Antihypertensive Medications Available in the Market
| 1. Calcium Channel Blockers | Amlodipine, Felodipine, Isradipine, Nifedipine, Diltiazem and Verapamil. |
| 2. Angiotensin Converting Enzyme Inhibitors | Enalapril, Fosinopril, Lisinopril, Quinapril, Captopril, Benzepril and Ramipril |
| 3. Angiotensin Receptor Blocker | Valsartan Losartan Candesartan, Azilsartan, Olmesartan and Irbesartan. |
| 4. Diuretics | Chlorothiazide, Hydrochlorothiazide, Chlorthalidone, Amiloride, 1Spirinolactone, |
| 5. Beta Adrenergic Antagonists | Atenolol, Metoprolol, Propanolol, Labetalol, Timolol, Nadolol and Nevibolol. |
| 6. Peripheral Alpha Antagonists | 2Doxazosin, Prazosin, Terazosin, Phentolamine and Phenoxybenzamine |
| 7. Central Acting Agents | Clonidine, Methyl dopa, Guanfacine and Guanethidine |
| 8. Vasodilators | Hydralazine, Minoxidil and Reserpine |
| 9. Aldosterone Antagonists | Eplerenone, 2Spirinolactone |
| 10. Combination drugs | Amlodipine/ Benazepril, Lisinopril/ Hydrochlorothiazide, Losartan/ Hydrochlorothiazide, Bisoprolol/ Hydrochlorothiazide, Olmesartan/ Hydrochlorothiazide, Olmesartan, Olmesartan/ Hydrochlorothiazide/ Amlodipine |
The general practice is to choose an agent from one of these classes and titrate the dose to achieve therapeutic effect while monitoring for side effects.52,89. Combination therapy is recommended if BP control is not achieved with a single drug16,90. Home BP measurements can be obtained to monitor the patient's response to therapy.
Less than a quarter of all drugs are approved by the FDA for use in children. Despite this, almost all the antihypertensive agents available in the United States have been used in pediatric patients. The Food and Drug Administration Modernization Act (FDAMA) in 1997, resulted in companies being incentivized to conduct clinical trials in pediatrics and has resulted in wider availability of pediatric approved anti-hypertensive agents and dosing recommendations91. The drugs initially approved and the current FDA approved antihypertensive agents in children are outlined in Table 4.
Table 4.
FDA Approved Antihypertensives
| PRE FDAMA | POST FDAMA |
|---|---|
| 1. Propanolol | 1. Children above 1 month - Enalapril |
| 2. Propanolol LA | 2. Children above the age of 1 year - Candesartan |
| 3. Oral Clonidine | 3. Children above 6 years - Lisinopril - Losartan - Valsartan - Amlodipine |
| 4. Transdermal Clonidine | 4. Children above 12 years - Guanfacine |
| 5. Hydralazine | |
| 6. Minoxidil | |
| 7. Hydrochlorothiazide |
Abbreviation: FDAMA, Food and Drug Administration Modernization Act
Adapted from Welch WP, Yang W, Taylor-Zapata P, Flynn JT. Antihypertensive drug use by children: are the drugs labeled and indicated? Journal of clinical hypertension (Greenwich, Conn) 2012;14:388-95; with permission.
Knowledge of the underlying etiology can provide a pathophysiologic approach to guide therapy85. For instance patients with hypertension secondary to steroid use would benefit from diuretic therapy with hydrochlorothiazide given that the underlying mechanism for hypertension in this setting is sodium and water retention.
Treatment with an ACEI or an ARB would be the appropriate therapy for a patient with diabetes to help prevent the progression of diabetic nephropathy.
BB are beneficial in treatment of hypertension associated with hyperthyroidism. BB are indicated after effective alpha blockade in the pre-operative treatment of pheochromocytoma to control the tachycardia associated with high circulating catecholamine levels and alpha blockade. They should be administered only after adequate alpha- blockade, to prevent unopposed alpha-adrenergic activity. BB should be avoided in patients with asthma and diabetes. They are associated with weight gain and should be used with caution in the obese patient.
There is no ideal first line agent for the treatment of PH in the teenager. Among the different antihypertensive classes, ACEI, ARB, CCB, BB or diuretics are frequently used as first line agents. There is no evidence in pediatric hypertension that one agent is superior to another. An ideal first line agent should be effective, have short and long term safety, be readily available, palatable, affordable, have long acting formulations and be easy to administer86. Pediatricians should be familiar with one or two agents from each class and their side effect profile.
It is recommended that a single agent be used at the minimum dose during initiation of pharmacological therapy. Table 5 shows the initial doses of commonly used agents. The dose can be titrated every 2 weeks to achieve control, sooner if the patient is symptomatic. A second agent should be added when the maximum dose is reached or if the patient develops side effects.
Table 5.
Doses of Common Antihypertensive Agents for Out Patient Treatment of Hypertension
| CLASS | DRUG | DOSE |
|---|---|---|
| Angiotensin Converting Enzyme Inhibitors | Captopril | Initial: 0.3–0.5 mg/kg/dose Maximum: 6 mg/kg/day |
| Enalapril | Initial: 0.08 mg/kg/day up to 5 mg/day Maximum: 0.6 mg/kg/day up to 40 mg/day |
|
| Lisinopril | Initial: 0.07 mg/kg/day up to 5 mg/day Maximum: 0.6 mg/kg/day up to 40 mg/day |
|
| Angiotensin Receptor Blockers | Losartan | Initial: 0.7 mg/kg/day up to 50 mg/day Maximum: 1.4 mg/kg/day up to 100 mg/day |
| Alpha and Beta Blockers | Labetalol | Initial: 1–3 mg/kg/day Maximum: 10–12 mg/kg/day up to 1,200 mg/day |
| Beta Blockers | Atenolol | Initial: 0.5–1 mg/kg/day Maximum: 2 mg/kg/day up to 100 mg/day |
| Metoprolol | Initial: 1–2 mg/kg/day Maximum: 6 mg/kg/day up to 200 mg/day |
|
| Propanolol | Initial: 1–2 mg/kg/day Maximum: 4 mg/kg/day up to 640 mg/day |
|
| Calcium Channel Blockers Diuretics | Amlodipine Hydrochlorothiazide | Children 6–17 years: 2.5–5 mg once daily < 6 months old: 2- 4 mg/kg/day 6 months to 2 years: 1- 2 mg/kg/day; maximum 37.5mg 2- 12 years: 1- 2 mg/kg/day; maximum 100mg/day |
*In my practice, I typically start a hypertensive teenager on amlodipine, lisinopril or hydrochlorothiazide, not in any particular order.
Adapted from The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004;114:555-76; with permission.
Following documentation of elevated blood pressures on 3 consecutive occasions, at least 1 week apart, hypertensive patients should receive non-pharmacological therapy including life style modification. Pharmacological therapy should be instituted in symptomatic patients and stage 2 hypertension and, prompt referral should be made to the nephrologist.
Benefits of Anti-hypertensive therapy
There are reports to show the reversal of target organ damage following the institution of antihypertensive therapy in children 92,93,94. Seeman et al reported a regression in LVH in a small pediatric cohort treated with ramipril monotherapy over a 6-month period93.
Other forms of therapy
Bariatric surgery has a role in the treatment of hypertension in the morbidly obese adult and might become an option in the obese pediatric adolescent in the future. A recent study by Visockiene et al demonstrated an improvement in metabolic syndrome including hypertension with up to 30% reduction in weight95.
Renal nerve denervation is a therapeutic option in adults with resistant hypertension, which refers to uncontrolled hypertension despite therapy with 3 or more antihypertensives. Studies in animals and humans have shown that the renal nerves play a role in blood pressure regulation. The efficacy of renal nerve denervation was demonstrated in the Symplicity HTN-2 trial where participants with resistant hypertension were randomized to either a treatment arm managed with renal denervation and baseline antihypertensives or the control arm managed with only baseline antihypertensives. A significant change of −32/-12mmHg in blood pressure in the treatment arm compared to a +1/0mmHg change in the control arm was observed 6 months after intervention. These blood pressure changes persisted at 2 years in a follow up study96-98. While renal nerve denervation has not yet been performed in the pediatric population, it might have a role in the future for the treatment of resistant hypertension in the adolescent hypertensive patient.
Key Message:
Life-style modification can be the sole modality of treatment in many adolescents with hypertension
- Indications for pharmacotherapy include:
- ✓ symptomatic hypertension
- ✓ secondary hypertension
- ✓ persistent hypertension despite life-style modification
- ✓ presence of target organ damage (LVH, retinopathy, microalbuminuria)
- ✓ presence of co-morbid conditions
Target BP is less than 95th percentile for uncomplicated primary hypertension; less than 90th percentile for patients with co-morbid conditions (diabetes, kidney disease, evidence of target organ damage)
No specific recommendations regarding optimal first line agent for treatment of pediatric hypertension
Knowledge of underlying etiology and co-morbid conditions may guide therapy
SPORTS PARTICIPATION FOR THE HYPERTENSIVE ADOLESCENT
There is no evidence to support restricting the hypertensive youth from sports participation. There are no reports of sudden cardiac death associated with sports in hypertensive athletes in the absence of underlying cardiovascular disease like hypertrophic cardiomyopathy52,99.
The AAP recommendations for sports participation in the hypertensive individual includes unrestricted competitive sports participation for individuals with prehypertension or stage 1 hypertension without end organ damage like LVH100. A regular exercise routine and dietary change should be encouraged to promote weight management and BP control as part of lifestyle modification. Individuals with stage 2 hypertension without evidence of end organ damage should be restricted from isometric exercises like weight lifting and push-ups, which can result in an acute rise in BP. This restriction should be in place until BP control is achieved with lifestyle modification and or drug therapy. With attendant cardiovascular disease, eligibility for sports participation should be based on the nature and severity of the coexistent cardiovascular disease 100.
Recommendations from the American College of Sport Medicine include developing a training regimen for the hypertensive athlete, which consists of dynamic and resistance exercises101. Expert opinion recommendations include limiting competitive and highly static sports only in the athlete with uncontrolled stage II hypertension or in the presence of target organ damage16.
Key Message:
Unrestricted competitive sports participation for adolescents with prehypertension, stage 1 hypertension and well-controlled stage 2 hypertension with no target organ damage
Limit competitive and highly static sports for athletes with uncontrolled stage 2 hypertension or with target organ damage
SCREENING CHILDREN FOR HYPERTENSION
AAP recommendations
The American Academy of Pediatrics, the European Society of Hypertension and the European Society of Cardiology recommend regular blood pressure screening in children above the age of 3 years at routine health visits. Despite these recommendations, hypertension in children is still under-diagnosed by clinicians102,103. The presence of elevated BP is more likely to be overlooked in children with normal weight and those without a family history of cardiovascular disease. Children whose blood pressures are less than 120/80mmHg; a measurement which is viewed as normal in adults but which could portend problems in children depending on age, gender, and height; were eight times more likely to have their elevated BP missed. This underscores the need for better BP monitoring in children and adolescents in an attempt to prevent the long-term complications of hypertension104.
On the contrary, a recent review by Thompson et al found that there is limited direct evidence supporting hypertension screening 105 for prevention of cardiovascular diseases. Further study is needed to address the gaps identified on the utility of aggressive hypertension screening in children.
Key message:
Regular BP screening is recommended in children above 3 years of age
Hypertension is under-diagnosed in children
Elevated blood pressure is more likely to be missed in those with normal body weight and negative family history
COMPLICATIONS OF HYPERTENSION IN ADOLESCENTS
Although the long term complications of hypertension such as stroke, cardiac failure, myocardial infarction and kidney disease are rare in the pediatric population, hypertension in children has been shown to be predictive of hypertension in adulthood106-111.
Childhood hypertension has been associated with risk factors of cardiovascular disease including LVH and increased arterial wall thickness22,72,112-119. LVH is the most frequently reported form of end organ damage in hypertensive children and adolescents with a prevalence of 14 to 26% 120. Hypertensive children have an increased left ventricular mass index even after adjustments for age, sex and body mass index which is associated with an increased risk of cardiovascular mortality23. This risk is amplified by arterial stiffening, a cardinal feature in hypertensive individuals.
A correlation between hypertension and lower neurocognitive test scores was seen in the NHANES III survey121. This association was further highlighted in a study conducted by Lande et al of 32 newly diagnosed hypertensive children and adolescents aged between 10 and 18 enrolled from a hypertension clinic. These patients were found to have significantly reduced cognitive function compared with the normotensive controls matched for age, sex, weight, race, IQ and socioeconomic status122. This cognitive impairment might represent an early manifestation of hypertensive damage to the brain that may precede more overt complications like stroke108,123,124. A follow-up study showed that treatment of these hypertensive children resulted in an improvement of their cognitive executive function125. This highlights the role of early diagnosis and optimal treatment.
Renal dysfunction represents a form of hypertension related end organ damage, which manifests as a reduction in glomerular filtration rate and an elevated urine microalbumin excretion. Microalbuminuria correlates well with progression of nephropathy and is a surrogate of increased cardiovascular mortality120. The utility of routine screening for microalbuminuria in the hypertensive child has not been proven.
Uncontrolled hypertension can cause damage to the retinal vasculature126 and the report from the National High Blood Pressure Education Program (NHBPEP) recommends that hypertensive children undergo a retinal exam for evidence of target organ damage54. Retinopathy is very rare in teenagers with isolated hypertension. A study of 83 hypertensive children found just mild abnormalities on retinal examination in only 3 children127.
There is growing evidence that there is increased mortality risk with childhood obesity related to an increased incidence of hypertension, ischemic heart disease, diabetes and stroke 128. This further highlights the importance of advocating lifestyle modification in the treatment of the overweight or obese individual to reduce the risk of premature mortality.
KEY POINTS.
Over the last two decades, essential hypertension has become common in children and adolescents and is related to the obesity epidemic.
Hypertension is under-recognized in children and diagnosis is based on sex-, ageand height- specific normative standards.
Modifiable risk factors for essential hypertension in children like obesity and sodium consumption should be addressed during treatment.
Primary care physicians may play an important role in reduction of cardiovascular mortality by early detection, appropriate management and referral when needed.
Key Message.
Long-term cardiovascular complications may not be seen in pediatric ages
Hypertension in childhood and adolescence predict hypertension as adults
Childhood hypertension is associated with LVH and increased arterial wall thickness
Lower neurocognitive scores and renal injury has been described with hypertension
SUMMARY.
With the advent of the obesity epidemic, primary hypertension has become an important cause of pediatric hypertension. In concert with obesity, diseases like diabetes mellitus, metabolic syndrome, obstructive sleep apnea, dyslipidemia, orthopedic complications and psychosocial issues have emerged as common pediatric issues. Insulin resistance, sympathetic over activity and vascular structure abnormalities explain the association between obesity and hypertension in the pediatric population. Complications of uncontrolled hypertension including left ventricular hypertrophy and renal dysfunction have become more prevalent in this population as a result. Early diagnosis and management of hypertension is important in preventing long-term complications. The value of weight loss in blood pressure control has been demonstrated in clinical studies and remains the first line of therapy in the pediatric patient who presents with hypertension. Pharmacological therapy is necessary for treatment of symptomatic hypertension and in the presence of target organ damage in order to prevent and in some cases reverse established complications.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURES: The authors have no relevant financial disclosures.
REFERENCES
- 1.Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004;113:475–82. doi: 10.1542/peds.113.3.475. [DOI] [PubMed] [Google Scholar]
- 2.McNiece KL, Poffenbarger TS, Turner JL, Franco KD, Sorof JM, Portman RJ. Prevalence of hypertension and pre-hypertension among adolescents. The Journal of pediatrics. 2007;150:640–4. 4, e1. doi: 10.1016/j.jpeds.2007.01.052. [DOI] [PubMed] [Google Scholar]
- 3.Acosta AA, Samuels JA, Portman RJ, Redwine KM. Prevalence of persistent prehypertension in adolescents. The Journal of pediatrics. 2012;160:757–61. doi: 10.1016/j.jpeds.2011.10.033. [DOI] [PubMed] [Google Scholar]
- 4.Falkner B, Gidding SS, Ramirez-Garnica G, Wiltrout SA, West D, Rappaport EB. The relationship of body mass index and blood pressure in primary care pediatric patients. The Journal of pediatrics. 2006;148:195–200. doi: 10.1016/j.jpeds.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 5.Flynn JT, Falkner BE. Obesity hypertension in adolescents: epidemiology, evaluation, and management. Journal of clinical hypertension (Greenwich, Conn) 2011;13:323–31. doi: 10.1111/j.1751-7176.2011.00452.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sorof J, Daniels S. Obesity hypertension in children: a problem of epidemic proportions. Hypertension. 2002;40:441–7. doi: 10.1161/01.hyp.0000032940.33466.12. [DOI] [PubMed] [Google Scholar]
- 7.Sorof JM, Poffenbarger T, Franco K, Bernard L, Portman RJ. Isolated systolic hypertension, obesity, and hyperkinetic hemodynamic states in children. The Journal of pediatrics. 2002;140:660–6. doi: 10.1067/mpd.2002.125228. [DOI] [PubMed] [Google Scholar]
- 8.Macedo ME, Trigueiros D, de Freitas F. Prevalence of high blood pressure in children and adolescents. Influence of obesity. Revista portuguesa de cardiologia : orgao oficial da Sociedade Portuguesa de Cardiologia = Portuguese journal of cardiology : an official journal of the Portuguese Society of Cardiology. 1997;16:27–30, 7-8. [PubMed] [Google Scholar]
- 9.Morrison JA, Barton BA, Biro FM, Daniels SR, Sprecher DL. Overweight, fat patterning, and cardiovascular disease risk factors in black and white boys. The Journal of pediatrics. 1999;135:451–7. doi: 10.1016/s0022-3476(99)70167-8. [DOI] [PubMed] [Google Scholar]
- 10.Tu W, Eckert GJ, DiMeglio LA, Yu Z, Jung J, Pratt JH. ntensified effect of adiposity on blood pressure in overweight and obese children. Hypertension. 2011;58:818–24. doi: 10.1161/HYPERTENSIONAHA.111.175695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosner B, Cook N, Portman R, Daniels S, Falkner B. Blood pressure differences by ethnic group among United States children and adolescents. Hypertension. 2009;54:502–8. doi: 10.1161/HYPERTENSIONAHA.109.134049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brady TM, Fivush B, Parekh RS, Flynn JT. Racial differences among children with primary hypertension. Pediatrics. 2010;126:931–7. doi: 10.1542/peds.2009-2972. [DOI] [PubMed] [Google Scholar]
- 13.Julius S, Nesbitt S. Sympathetic overactivity in hypertension. A moving target. American journal of hypertension. 1996;9:113S–20S. doi: 10.1016/0895-7061(96)00287-7. [DOI] [PubMed] [Google Scholar]
- 14.Palatini P. Sympathetic overactivity in hypertension: a risk factor for cardiovascular disease. Current hypertension reports. 2001;3(Suppl 1):S3–9. doi: 10.1007/s11906-001-0065-z. [DOI] [PubMed] [Google Scholar]
- 15.Rocchini AP. Insulin resistance, obesity and hypertension. The Journal of nutrition. 1995;125:1718S–24S. doi: 10.1093/jn/125.suppl_6.1718S. [DOI] [PubMed] [Google Scholar]
- 16.The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76. [PubMed] [Google Scholar]
- 17.Redwine KM, Falkner B. Progression of prehypertension to hypertension in adolescents. Current hypertension reports. 2012;14:619–25. doi: 10.1007/s11906-012-0299-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Redwine KM, Acosta AA, Poffenbarger T, Portman RJ, Samuels J. Development of hypertension in adolescents with pre-hypertension. The Journal of pediatrics. 2012;160:98–103. doi: 10.1016/j.jpeds.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 19.Redwine KM, Daniels SR. Prehypertension in adolescents: risk and progression. Journal of clinical hypertension (Greenwich, Conn) 2012;14:360–4. doi: 10.1111/j.1751-7176.2012.00663.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Basiratnia M, Esteghamati M, Ajami GH, et al. Blood pressure profile in renal transplant recipients and its relation to diastolic function: tissue Doppler echocardiographic study. Pediatric nephrology (Berlin, Germany) 2011;26:449–57. doi: 10.1007/s00467-010-1724-6. [DOI] [PubMed] [Google Scholar]
- 21.Richey PA, Disessa TG, Hastings MC, Somes GW, Alpert BS, Jones DP. Ambulatory blood pressure and increased left ventricular mass in children at risk for hypertension. The Journal of pediatrics. 2008;152:343–8. doi: 10.1016/j.jpeds.2007.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Drukteinis JS, Roman MJ, Fabsitz RR, et al. Cardiac and systemic hemodynamic characteristics of hypertension and prehypertension in adolescents and young adults: the Strong Heart Study. Circulation. 2007;115:221–7. doi: 10.1161/CIRCULATIONAHA.106.668921. [DOI] [PubMed] [Google Scholar]
- 23.Stabouli S, Kotsis V, Rizos Z, et al. Left ventricular mass in normotensive, prehypertensive and hypertensive children and adolescents. Pediatric nephrology (Berlin, Germany) 2009;24:1545–51. doi: 10.1007/s00467-009-1165-2. [DOI] [PubMed] [Google Scholar]
- 24.Goldstein IB, Shapiro D, Weiss RE. How family history and risk factors for hypertension relate to ambulatory blood pressure in healthy adults. Journal of hypertension. 2008;26:276–83. doi: 10.1097/HJH.0b013e3282f15c27. [DOI] [PubMed] [Google Scholar]
- 25.Alpay H, Ozdemir N, Wuhl E, Topuzoglu A. Ambulatory blood pressure monitoring in healthy children with parental hypertension. Pediatric nephrology (Berlin, Germany) 2009;24:155–61. doi: 10.1007/s00467-008-0975-y. [DOI] [PubMed] [Google Scholar]
- 26.Giussani M, Antolini L, Brambilla P, et al. Cardiovascular risk assessment in children: role of physical activity, family history and parental smoking on BMI and blood pressure. Journal of hypertension. 2013 doi: 10.1097/HJH.0b013e32835f17c7. [DOI] [PubMed] [Google Scholar]
- 27.Zhou L, Chen Y, Sun N, Liu X. Family history of hypertension and arterial elasticity characteristics in healthy young people. Hypertension research : official journal of the Japanese Society of Hypertension. 2008;31:833–9. doi: 10.1291/hypres.31.833. [DOI] [PubMed] [Google Scholar]
- 28.Mongia A, Vecker R, George M, et al. Role of 11betaHSD type 2 enzyme activity in essential hypertension and children with chronic kidney disease (CKD). The Journal of clinical endocrinology and metabolism. 2012;97:3622–9. doi: 10.1210/jc.2012-1411. [DOI] [PubMed] [Google Scholar]
- 29.Nguyen KD, Pihur V, Ganesh SK, et al. Effects of rare and common blood pressure gene variants on essential hypertension: results from the Family Blood Pressure Program, CLUE, and Atherosclerosis Risk in Communities studies. Circulation research. 2013;112:318–26. doi: 10.1161/CIRCRESAHA.112.276725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Corvol P, Soubrier F, Jeunemaitre X. Molecular genetics of the renin angiotensin-aldosterone system in human hypertension. Pathologie-biologie. 1997;45:229–39. [PubMed] [Google Scholar]
- 31.Luft FC. Mendelian forms of human hypertension and mechanisms of disease. Clinical medicine & research. 2003;1:291–300. doi: 10.3121/cmr.1.4.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Toka HR, Luft FC. Monogenic forms of human hypertension. Seminars in nephrology. 2002;22:81–8. doi: 10.1053/snep.2002.30206. [DOI] [PubMed] [Google Scholar]
- 33.Poch E, Gonzalez D, Giner V, Bragulat E, Coca A, de La Sierra A. Molecular basis of salt sensitivity in human hypertension. Evaluation of renin-angiotensin aldosterone system gene polymorphisms. Hypertension. 2001;38:1204–9. doi: 10.1161/hy1101.099479. [DOI] [PubMed] [Google Scholar]
- 34.Giner V, Poch E, Bragulat E, et al. Renin-angiotensin system genetic polymorphisms and salt sensitivity in essential hypertension. Hypertension. 2000;35:512–7. doi: 10.1161/01.hyp.35.1.512. [DOI] [PubMed] [Google Scholar]
- 35.Dekkers JC, Snieder H, Van Den Oord EJ, Treiber FA. Moderators of blood pressure development from childhood to adulthood: a 10-year longitudinal study. The Journal of pediatrics. 2002;141:770–9. doi: 10.1067/mpd.2002.128113. [DOI] [PubMed] [Google Scholar]
- 36.Wang X, Poole JC, Treiber FA, Harshfield GA, Hanevold CD, Snieder H. Ethnic and gender differences in ambulatory blood pressure trajectories: results from a 15- year longitudinal study in youth and young adults. Circulation. 2006;114:2780–7. doi: 10.1161/CIRCULATIONAHA.106.643940. [DOI] [PubMed] [Google Scholar]
- 37.Harshfield GA, Treiber FA, Wilson ME, Kapuku GK, Davis HC. A longitudinal study of ethnic differences in ambulatory blood pressure patterns in youth. American journal of hypertension. 2002;15:525–30. doi: 10.1016/s0895-7061(02)02267-7. [DOI] [PubMed] [Google Scholar]
- 38.Manatunga AK, Jones JJ, Pratt JH. Longitudinal assessment of blood pressures in black and white children. Hypertension. 1993;22:84–9. doi: 10.1161/01.hyp.22.1.84. [DOI] [PubMed] [Google Scholar]
- 39.Freedman BI, Murea M. Target organ damage in African American hypertension: role of APOL1. Current hypertension reports. 2012;14:21–8. doi: 10.1007/s11906-011-0237-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Freedman BI, Kopp JB, Langefeld CD, et al. The apolipoprotein L1 (APOL1) gene and nondiabetic nephropathy in African Americans. Journal of the American Society of Nephrology : JASN. 2010;21:1422–6. doi: 10.1681/ASN.2010070730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Freedman BI, Langefeld CD. The new era of APOL1-associated glomerulosclerosis. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2012;27:1288–91. doi: 10.1093/ndt/gfr812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kopp JB, Nelson GW, Sampath K, et al. APOL1 genetic variants in focal segmental glomerulosclerosis and HIV-associated nephropathy. Journal of the American Society of Nephrology : JASN. 2011;22:2129–37. doi: 10.1681/ASN.2011040388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Papeta N, Kiryluk K, Patel A, et al. APOL1 variants increase risk for FSGS and HIVAN but not IgA nephropathy. Journal of the American Society of Nephrology : JASN. 2011;22:1991–6. doi: 10.1681/ASN.2011040434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.He Q, Ding ZY, Fong DY, Karlberg J. Blood pressure is associated with body mass index in both normal and obese children. Hypertension. 2000;36:165–70. doi: 10.1161/01.hyp.36.2.165. [DOI] [PubMed] [Google Scholar]
- 45.Lo JC, Sinaiko A, Chandra M, et al. Prehypertension and hypertension in community-based pediatric practice. Pediatrics. 2013;131:e415–24. doi: 10.1542/peds.2012-1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Edvardsson VO, Steinthorsdottir SD, Eliasdottir SB, Indridason OS, Palsson R. Birth weight and childhood blood pressure. Current hypertension reports. 2012;14:596–602. doi: 10.1007/s11906-012-0311-6. [DOI] [PubMed] [Google Scholar]
- 47.Primatesta P, Falaschetti E, Poulter NR. Birth weight and blood pressure in childhood: results from the Health Survey for England. Hypertension. 2005;45:75–9. doi: 10.1161/01.HYP.0000150037.98835.10. [DOI] [PubMed] [Google Scholar]
- 48.Salgado CM, Jardim PC, Teles FB, Nunes MC. Influence of low birth weight on microalbuminuria and blood pressure of school children. Clinical nephrology. 2009;71:367–74. doi: 10.5414/cnp71367. [DOI] [PubMed] [Google Scholar]
- 49.Martinez-Aguayo A, Aglony M, Bancalari R, et al. Birth weight is inversely associated with blood pressure and serum aldosterone and cortisol levels in children. Clinical endocrinology. 2012;76:713–8. doi: 10.1111/j.1365-2265.2011.04308.x. [DOI] [PubMed] [Google Scholar]
- 50.Barker DJ. Birth weight and hypertension. Hypertension. 2006;48:357–8. doi: 10.1161/01.HYP.0000236552.04251.42. [DOI] [PubMed] [Google Scholar]
- 51.Yang Q, Zhang Z, Kuklina EV, et al. Sodium intake and blood pressure among US children and adolescents. Pediatrics. 2012;130:611–9. doi: 10.1542/peds.2011-3870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lande MB, Flynn JT. Treatment of hypertension in children and adolescents. Pediatric nephrology (Berlin, Germany) 2009;24:1939–49. doi: 10.1007/s00467-007-0573-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Podoll A, Grenier M, Croix B, Feig DI. Inaccuracy in pediatric outpatient blood pressure measurement. Pediatrics. 2007;119:e538–43. doi: 10.1542/peds.2006-1686. [DOI] [PubMed] [Google Scholar]
- 54.Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a working group report from the National High Blood Pressure Education Program. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Pediatrics. 1996;98:649–58. [PubMed] [Google Scholar]
- 55.Arafat M, Mattoo TK. Measurement of blood pressure in children: recommendations and perceptions on cuff selection. Pediatrics. 1999;104:e30. doi: 10.1542/peds.104.3.e30. [DOI] [PubMed] [Google Scholar]
- 56.Bald M. Ambulatory blood pressure monitoring in children and adolescents. Current insights into a new technique. Minerva pediatrica. 2002;54:13–24. [PubMed] [Google Scholar]
- 57.Gavrilovici C, Goldsmith DJ, Reid C, Gubeth-Tatomir P, Covic A. What is the role of ambulatory BP monitoring in pediatric nephrology? Journal of nephrology. 2004;17:642–52. [PubMed] [Google Scholar]
- 58.Graves JW, Althaf MM. Utility of ambulatory blood pressure monitoring in children and adolescents. Pediatric nephrology (Berlin, Germany) 2006;21:1640–52. doi: 10.1007/s00467-006-0175-6. [DOI] [PubMed] [Google Scholar]
- 59.Flynn JT, Urbina EM. Pediatric ambulatory blood pressure monitoring: indications and interpretations. Journal of clinical hypertension (Greenwich, Conn) 2012;14:372–82. doi: 10.1111/j.1751-7176.2012.00655.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Urbina E, Alpert B, Flynn J, et al. Ambulatory blood pressure monitoring in children and adolescents: recommendations for standard assessment: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the council on cardiovascular disease in the young and the council for high blood pressure research. Hypertension. 2008;52:433–51. doi: 10.1161/HYPERTENSIONAHA.108.190329. [DOI] [PubMed] [Google Scholar]
- 61.Lingens N, Dobos E, Witte K, et al. Twenty-four-hour ambulatory blood pressure profiles in pediatric patients after renal transplantation. Pediatric nephrology (Berlin, Germany) 1997;11:23–6. doi: 10.1007/s004670050226. [DOI] [PubMed] [Google Scholar]
- 62.Khan IA, Gajaria M, Stephens D, Balfe JW. Ambulatory blood pressure monitoring in children: a large center's experience. Pediatric nephrology (Berlin, Germany) 2000;14:802–5. doi: 10.1007/s004679900291. [DOI] [PubMed] [Google Scholar]
- 63.Kanbay M, Turkmen K, Ecder T, Covic A. Ambulatory blood pressure monitoring: from old concepts to novel insights. International urology and nephrology. 2012;44:173–82. doi: 10.1007/s11255-011-0027-6. [DOI] [PubMed] [Google Scholar]
- 64.Flynn JT. Ambulatory blood pressure monitoring should be routinely performed after pediatric renal transplantation. Pediatric transplantation. 2012;16:533–6. doi: 10.1111/j.1399-3046.2011.01626.x. [DOI] [PubMed] [Google Scholar]
- 65.Keefe T, Davis JD. Ambulatory Blood Pressure Monitoring Should be used in the Primary Care Setting to Diagnose Hypertension. American Journal of Hypertension. 2013 doi: 10.1093/ajh/hpt089. [DOI] [PubMed] [Google Scholar]
- 66.Lurbe E, Torro I, Alvarez V, et al. Prevalence, persistence, and clinical significance of masked hypertension in youth. Hypertension. 2005;45:493–8. doi: 10.1161/01.HYP.0000160320.39303.ab. [DOI] [PubMed] [Google Scholar]
- 67.Bidlingmeyer I, Burnier M, Bidlingmeyer M, Waeber B, Brunner HR. Isolated office hypertension: a prehypertensive state? Journal of hypertension. 1996;14:327–32. doi: 10.1097/00004872-199603000-00009. [DOI] [PubMed] [Google Scholar]
- 68.Colombo F, Catarame S, Cossovich P, et al. Isolated office hypertension: are there any markers of future blood pressure status? Blood pressure monitoring. 2000;5:249–54. doi: 10.1097/00126097-200010000-00001. [DOI] [PubMed] [Google Scholar]
- 69.Staessen JA, Asmar R, De Buyzere M, et al. Task Force II: blood pressure measurement and cardiovascular outcome. Blood pressure monitoring. 2001;6:355–70. doi: 10.1097/00126097-200112000-00016. [DOI] [PubMed] [Google Scholar]
- 70.Seeman T, Pohl M, Palyzova D, John U. Microalbuminuria in children with primary and white-coat hypertension. Pediatric nephrology (Berlin, Germany) 2012;27:461–7. doi: 10.1007/s00467-011-2019-2. [DOI] [PubMed] [Google Scholar]
- 71.Stabouli S, Kotsis V, Toumanidis S, Papamichael C, Constantopoulos A, Zakopoulos N. White-coat and masked hypertension in children: association with target-organ damage. Pediatric nephrology (Berlin, Germany) 2005;20:1151–5. doi: 10.1007/s00467-005-1979-5. [DOI] [PubMed] [Google Scholar]
- 72.McNiece KL, Gupta-Malhotra M, Samuels J, et al. Left ventricular hypertrophy in hypertensive adolescents: analysis of risk by 2004 National High Blood Pressure Education Program Working Group staging criteria. Hypertension. 2007;50:392–5. doi: 10.1161/HYPERTENSIONAHA.107.092197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lande MB, Meagher CC, Fisher SG, Belani P, Wang H, Rashid M. Left ventricular mass index in children with white coat hypertension. The Journal of pediatrics. 2008;153:50–4. doi: 10.1016/j.jpeds.2008.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sung SH, Cheng HM, Wang KL, et al. White Coat Hypertension Is More Risky Than Prehypertension: Important Role of Arterial Wave Reflections. Hypertension. 2013 doi: 10.1161/HYPERTENSIONAHA.111.00569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shimbo D, Newman JD, Schwartz JE. Masked hypertension and prehypertension: diagnostic overlap and interrelationships with left ventricular mass: the Masked Hypertension Study. American journal of hypertension. 2012;25:664–71. doi: 10.1038/ajh.2012.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Stabouli S, Kotsis V, Zakopoulos N. Ambulatory blood pressure monitoring and target organ damage in pediatrics. Journal of hypertension. 2007;25:1979–86. doi: 10.1097/HJH.0b013e3282775992. [DOI] [PubMed] [Google Scholar]
- 77.Nadar SK, Tayebjee MH, Messerli F, Lip GY. Target organ damage in hypertension: pathophysiology and implications for drug therapy. Current pharmaceutical design. 2006;12:1581–92. doi: 10.2174/138161206776843368. [DOI] [PubMed] [Google Scholar]
- 78.Verdecchia P, Reboldi GP, Angeli F, et al. Short- and long-term incidence of stroke in white-coat hypertension. Hypertension. 2005;45:203–8. doi: 10.1161/01.HYP.0000151623.49780.89. [DOI] [PubMed] [Google Scholar]
- 79.Dolan E, Thijs L, Li Y, et al. Ambulatory arterial stiffness index as a predictor of cardiovascular mortality in the Dublin Outcome Study. Hypertension. 2006;47:365–70. doi: 10.1161/01.HYP.0000200699.74641.c5. [DOI] [PubMed] [Google Scholar]
- 80.Li Y, Wang JG, Dolan E, et al. Ambulatory arterial stiffness index derived from 24-hour ambulatory blood pressure monitoring. Hypertension. 2006;47:359–64. doi: 10.1161/01.HYP.0000200695.34024.4c. [DOI] [PubMed] [Google Scholar]
- 81.Li Y, Dolan E, Wang JG, et al. Ambulatory arterial stiffness index: determinants and outcome. Blood pressure monitoring. 2006;11:107–10. doi: 10.1097/01.mbp.0000189791.90488.a1. [DOI] [PubMed] [Google Scholar]
- 82.Tuli SY, Dharnidharka VR. Utility of renal imaging in the diagnostic evaluation of obese childhood primary hypertension. Clinical pediatrics. 2005;44:589–92. doi: 10.1177/000992280504400706. [DOI] [PubMed] [Google Scholar]
- 83.Batisky DL. Obesity and the role of lifestyle and dietary intervention in the management of pediatric hypertension. Le Journal medical libanais The Lebanese medical journal. 2010;58:171–4. [PubMed] [Google Scholar]
- 84.Bacon SL, Sherwood A, Hinderliter A, Blumenthal JA. Effects of exercise, diet and weight loss on high blood pressure. Sports medicine (Auckland, NZ) 2004;34:307–16. doi: 10.2165/00007256-200434050-00003. [DOI] [PubMed] [Google Scholar]
- 85.Brierley J, Marks SD. Treating the causes of paediatric hypertension using non-invasive physiological parameters. Medical hypotheses. 2010;75:439–41. doi: 10.1016/j.mehy.2010.04.018. [DOI] [PubMed] [Google Scholar]
- 86.Batisky DL. What is the optimal first-line agent in children requiring antihypertensive medication? Current hypertension reports. 2012;14:603–7. doi: 10.1007/s11906-012-0302-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Blowey DL. Update on the pharmacologic treatment of hypertension in pediatrics. Journal of clinical hypertension (Greenwich, Conn) 2012;14:383–7. doi: 10.1111/j.1751-7176.2012.00659.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Flynn JT. Management of hypertension in the young: role of antihypertensive medications. Journal of cardiovascular pharmacology. 2011;58:111–20. doi: 10.1097/FJC.0b013e31820d1b89. [DOI] [PubMed] [Google Scholar]
- 89.Kavey RE, Daniels SR, Flynn JT. Management of high blood pressure in children and adolescents. Cardiology clinics. 2010;28:597–607. doi: 10.1016/j.ccl.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 90.Flynn JT. Pharmacologic management of childhood hypertension: current status, future challenges. American journal of hypertension. 2002;15:30S–3S. doi: 10.1016/s0895-7061(01)02306-8. [DOI] [PubMed] [Google Scholar]
- 91.Welch WP, Yang W, Taylor-Zapata P, Flynn JT. Antihypertensive drug use by children: are the drugs labeled and indicated? Journal of clinical hypertension (Greenwich, Conn) 2012;14:388–95. doi: 10.1111/j.1751-7176.2012.00656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Litwin M, Niemirska A, Sladowska-Kozlowska J, et al. Regression of target organ damage in children and adolescents with primary hypertension. Pediatric nephrology (Berlin, Germany) 2010;25:2489–99. doi: 10.1007/s00467-010-1626-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Seeman T, Gilik J, Vondrak K, et al. Regression of left-ventricular hypertrophy in children and adolescents with hypertension during ramipril monotherapy. American journal of hypertension. 2007;20:990–6. doi: 10.1016/j.amjhyper.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 94.Sharma M, Kupferman JC, Brosgol Y, et al. The effects of hypertension on the paediatric brain: a justifiable concern. Lancet neurology. 2010;9:933–40. doi: 10.1016/S1474-4422(10)70167-8. [DOI] [PubMed] [Google Scholar]
- 95.Visockiene Z, Brimas G, Abaliksta T, Siauliene L, Liakina V, Strupas K. Metabolic changes one year after laparoscopic adjustable gastric banding operation in morbidly obese subjects. Wideochirurgia i inne techniki malo inwazyjne = Videosurgery and other miniinvasive techniques / kwartalnik pod patronatem Sekcji Wideochirurgii TChP oraz Sekcji Chirurgii Bariatrycznej TChP. 2013;8:13–21. doi: 10.5114/wiitm.2011.30828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Esler MD, Krum H, Schlaich M, Schmieder RE, Bohm M, Sobotka PA. Renal sympathetic denervation for treatment of drug-resistant hypertension: one-year results from the Symplicity HTN-2 randomized, controlled trial. Circulation. 2012;126:2976–82. doi: 10.1161/CIRCULATIONAHA.112.130880. [DOI] [PubMed] [Google Scholar]
- 97.Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Bohm M. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet. 2010;376:1903–9. doi: 10.1016/S0140-6736(10)62039-9. [DOI] [PubMed] [Google Scholar]
- 98.Kandzari DE, Bhatt DL, Sobotka PA, et al. Catheter-based renal denervation for resistant hypertension: rationale and design of the SYMPLICITY HTN-3 Trial. Clinical cardiology. 2012;35:528–35. doi: 10.1002/clc.22008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Maron BJ, Haas TS, Ahluwalia A, Rutten-Ramos SC. Incidence of cardiovascular sudden deaths in Minnesota high school athletes. Heart rhythm : the official journal of the Heart Rhythm Society. 2013;10:374–7. doi: 10.1016/j.hrthm.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 100.Graham L. AAP updates policy statement on athletic participation by children and adolescents with systemic hypertension. American family physician. 2010;82:1285. [PubMed] [Google Scholar]
- 101.Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA. American College of Sports Medicine position stand. Exercise and hypertension. Medicine and science in sports and exercise. 2004;36:533–53. doi: 10.1249/01.mss.0000115224.88514.3a. [DOI] [PubMed] [Google Scholar]
- 102.Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA : the journal of the American Medical Association. 2007;298:874–9. doi: 10.1001/jama.298.8.874. [DOI] [PubMed] [Google Scholar]
- 103.Lurbe E, Cifkova R, Cruickshank JK, et al. Management of high blood pressure in children and adolescents: recommendations of the European Society of Hypertension. Journal of hypertension. 2009;27:1719–42. doi: 10.1097/HJH.0b013e32832f4f6b. [DOI] [PubMed] [Google Scholar]
- 104.Brady TM, Solomon BS, Neu AM, Siberry GK, Parekh RS. Patient-, provider-, and clinic-level predictors of unrecognized elevated blood pressure in children. Pediatrics. 2010;125:e1286–93. doi: 10.1542/peds.2009-0555. [DOI] [PubMed] [Google Scholar]
- 105.Thompson M, Dana T, Bougatsos C, Blazina I, Norris SL. Screening for Hypertension in Children and Adolescents to Prevent Cardiovascular Disease. Pediatrics. 2013 doi: 10.1542/peds.2012-3523. [DOI] [PubMed] [Google Scholar]
- 106.Lauer RM, Clarke WR, Mahoney LT, Witt J. Childhood predictors for high adult blood pressure. The Muscatine Study. Pediatric clinics of North America. 1993;40:23–40. doi: 10.1016/s0031-3955(16)38478-4. [DOI] [PubMed] [Google Scholar]
- 107.Lauer RM, Clarke WR. Childhood risk factors for high adult blood pressure: the Muscatine Study. Pediatrics. 1989;84:633–41. [PubMed] [Google Scholar]
- 108.Mahoney LT, Clarke WR, Burns TL, Lauer RM. Childhood predictors of high blood pressure. American journal of hypertension. 1991;4:608S–10S. doi: 10.1093/ajh/4.11s.608s. [DOI] [PubMed] [Google Scholar]
- 109.Bao W, Threefoot SA, Srinivasan SR, Berenson GS. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa Heart Study. American journal of hypertension. 1995;8:657–65. doi: 10.1016/0895-7061(95)00116-7. [DOI] [PubMed] [Google Scholar]
- 110.Chen W, Srinivasan SR, Ruan L, Mei H, Berenson GS. Adult hypertension is associated with blood pressure variability in childhood in blacks and whites: the bogalusa heart study. American journal of hypertension. 2011;24:77–82. doi: 10.1038/ajh.2010.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Beckett LA, Rosner B, Roche AF, Guo S. Serial changes in blood pressure from adolescence into adulthood. American journal of epidemiology. 1992;135:1166–77. doi: 10.1093/oxfordjournals.aje.a116217. [DOI] [PubMed] [Google Scholar]
- 112.Tolwinska J, Glowinska B, Urban M, Pieciukiewicz B. [Ultrasonographic evaluation of atherosclerotic changes in carotid and brachial arteries in obese and hypertensive children]. Przeglad lekarski. 2005;62:1346–51. [PubMed] [Google Scholar]
- 113.Sorof JM, Turner J, Martin DS, et al. Cardiovascular risk factors and sequelae in hypertensive children identified by referral versus school-based screening. Hypertension. 2004;43:214–8. doi: 10.1161/01.HYP.0000114696.96318.4e. [DOI] [PubMed] [Google Scholar]
- 114.Sorof JM, Alexandrov AV, Cardwell G, Portman RJ. Carotid artery intimal medial thickness and left ventricular hypertrophy in children with elevated blood pressure. Pediatrics. 2003;111:61–6. doi: 10.1542/peds.111.1.61. [DOI] [PubMed] [Google Scholar]
- 115.Tracy RE, Newman WP, 3rd, Wattigney WA, Srinivasan SR, Strong JP, Berenson GS. Histologic features of atherosclerosis and hypertension from autopsies of young individuals in a defined geographic population: the Bogalusa Heart Study. Atherosclerosis. 1995;116:163–79. doi: 10.1016/0021-9150(95)05525-2. [DOI] [PubMed] [Google Scholar]
- 116.Berenson GS, Srinivasan SR, Bao W, Newman WP, 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. The New England journal of medicine. 1998;338:1650–6. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 117.Sorof JM, Alexandrov AV, Garami Z, et al. Carotid ultrasonography for detection of vascular abnormalities in hypertensive children. Pediatric nephrology (Berlin, Germany) 2003;18:1020–4. doi: 10.1007/s00467-003-1187-0. [DOI] [PubMed] [Google Scholar]
- 118.Sorof JM, Cardwell G, Franco K, Portman RJ. Ambulatory blood pressure and left ventricular mass index in hypertensive children. Hypertension. 2002;39:903–8. doi: 10.1161/01.hyp.0000013266.40320.3b. [DOI] [PubMed] [Google Scholar]
- 119.Chamontin B, Amar J, Barthe P, Salvador M. Blood pressure measurements and left ventricular mass in young adults with arterial hypertension screened at high school check-up. Journal of human hypertension. 1994;8:357–61. [PubMed] [Google Scholar]
- 120.Lurbe E, Alvarez J, Redon J. Diagnosis and treatment of hypertension in children. Current hypertension reports. 2010;12:480–6. doi: 10.1007/s11906-010-0155-x. [DOI] [PubMed] [Google Scholar]
- 121.Lande MB, Kaczorowski JM, Auinger P, Schwartz GJ, Weitzman M. Elevated blood pressure and decreased cognitive function among school-age children and adolescents in the United States. The Journal of pediatrics. 2003;143:720–4. doi: 10.1067/S0022-3476(03)00412-8. [DOI] [PubMed] [Google Scholar]
- 122.Lande MB, Adams H, Falkner B, et al. Parental assessments of internalizing and externalizing behavior and executive function in children with primary hypertension. The Journal of pediatrics. 2009;154:207–12. doi: 10.1016/j.jpeds.2008.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kupferman JC, Lande MB, Adams HR, Pavlakis SG. Primary hypertension and neurocognitive and executive functioning in school-age children. Pediatric nephrology (Berlin, Germany) 2013;28:401–8. doi: 10.1007/s00467-012-2215-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lande MB, Kupferman JC, Adams HR. Neurocognitive alterations in hypertensive children and adolescents. Journal of clinical hypertension (Greenwich, Conn) 2012;14:353–9. doi: 10.1111/j.1751-7176.2012.00661.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lande MB, Adams H, Falkner B, et al. Parental assessment of executive function and internalizing and externalizing behavior in primary hypertension after anti-hypertensive therapy. The Journal of pediatrics. 2010;157:114–9. doi: 10.1016/j.jpeds.2009.12.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chatterjee S, Chattopadhyay S, Hope-Ross M, Lip PL. Hypertension and the eye: changing perspectives. Journal of human hypertension. 2002;16:667–75. doi: 10.1038/sj.jhh.1001472. [DOI] [PubMed] [Google Scholar]
- 127.Foster BJ, Ali H, Mamber S, Polomeno RC, Mackie AS. Prevalence and severity of hypertensive retinopathy in children. Clinical pediatrics. 2009;48:926–30. doi: 10.1177/0009922809339385. [DOI] [PubMed] [Google Scholar]
- 128.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. International journal of obesity (2005) 2011;35:891–8. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]