Abstract
Depressive symptoms and depression are a common complication of childbirth and a growing body of literature suggests that there are modifiable factors associated with their occurrence. We developed a behavioral educational intervention targeting these factors and successfully reduced postpartum depressive symptoms in a randomized trial among low-income black and Latina women. We now report results of 540 predominantly white, high income mothers in a second randomized trial. Mothers in the intervention arm received a 2-step intervention that prepared and educated mothers about modifiable factors associated with postpartum depressive symptoms (e.g., physical symptoms, low self-efficacy), bolstered social support, and enhanced management skills. The control arm received enhanced usual care. Participants were surveyed prior to randomization, 3-weeks, 3-months, and 6-months postpartum. Depressive symptoms were assessed using the Edinburgh Postnatal Depression Scale (EPDS of 10 or greater). Prevalence of depressive symptoms postpartum were unexpectedly low precluding detection of difference in rates of depressive symptoms among intervention vs. enhanced usual care post hospitalization: 3-weeks (6.0 % vs. 5.6%, p=.83), 3-months (5.1% vs. 6.5%, p=.53) and 6-months (3.6% vs. 4.6%, p=.53).
Keywords: postpartum depression, randomized trial, behavioral intervention, psychosocial
Introduction
Depressive symptoms and depression are one of the most common complications of childbirth and are the leading cause of disease-related disability among women.(Gaynes et al., 2005; Kessler, 2003) Estimates of prevalence rates for these symptoms range from 10 to over 50% depending on the screening instrument used and the population studied.(Beeghly et al., 2003; Vera et al., 1991; Zayas et al., 2002) Symptoms of distress and depression impact hundreds of thousands of women annually in the United States and affect women from all racial/ethnic and socioeconomic backgrounds. Both major depressive disorder and moderate symptoms of depression negatively affect the quality of life and daily functioning of mothers.(Josefsson et al., 2002) Whether these symptoms do or do not reach the level of diagnosed major depressive disorder, they are associated with multiple, negative consequences for mothers and infants.(Dennis et al., 2005; Duer et al., 1988; Herrera et al, 2004; Kroenke et al., 2001, 2003; Matthey et al., 2000; McLearn et al., 2006; Minkovitz et al., 2005; Seguin et al, 1999)
A growing body of literature suggests that potentially modifiable factors associated with depressive symptoms postpartum. Situational factors such as postpartum physical symptoms, infant colic, overload from daily demands, and poor social support are associated with and likely trigger depressive symptoms.(Howell et al., 2010; Howell et al., 2009; Howell et al., 2005; Howell et al., 2006) We hypothesized that one or more of the three sub-sets of depressive symptoms, e.g., somatic, mood, and self critical component, could be triggered and moderated by situational stimuli, and that an intervention designed to normalize the postpartum experience would lower rates of these symptoms. The intervention had three objectives: 1) to clarify the immediate postpartum experience as “normal”, i.e., shared event (e.g., physical symptoms and infant and social demands); 2) provide simple procedures for management and enhancing social support; and 3) define the time frame for recovery. A randomized trial testing this intervention showed a significant reduction in positive depression screens among self-identified black and Latina postpartum mothers for up to six-months of follow up.(Howell et al., 2012)
In this report, we present the results of a second randomized controlled trial testing this intervention among a different socio-demographic cohort of women: white and Asian mothers.
Methods
Study Sample
Participants included 540 self-identified white and Asian postpartum mothers who delivered between July 2009 and April 2010 at a large tertiary inner-city hospital located in East Harlem, New York City. An earlier trial had recruited black and Latina postpartum mothers and therefore only white and Asian (non-black and non-Latina) women were included in this trial. The Program for the Protection of Human Subjects (the Institutional Review Board) at Mount Sinai School of Medicine approved this study. Eligible participants were ≥18 years, had infants with birth weights ≥2500 grams and 5-minute Apgar scores ≥7. Women were identified by an electronic delivery system which includes information on maternal race/ethnicity, maternal age, infant Apgar scores, and infant birth weight.
Mothers who met initial requirements were deemed eligible if they then self-identified as white, Asian, or other (non-black and non-Latina) minority women when questioned by a clinical research coordinator. The research coordinator approached mothers in hospital between their delivery day and postpartum day #2; approximately 12 to 17 patients were recruited Mondays through Fridays each week. Mothers who consented completed a 20 minute survey and were assigned to intervention or enhanced usual care. Assignment involved giving each patient a number between 1 and 20, based on the order of delivery date, and using a list that had randomly assigned these numbers to intervention and control; the computer randomized list was prepared by the project statistician. The methods were similar to but completely separate from the trial with black and Latina mothers initiated four months earlier.(Howell, et al., 2012)
Intervention
Patients randomized to the intervention arm were given a 2-step behavioral educational intervention. The theoretical underpinning of the intervention was based on the Common-Sense Model (CSM), a model that describes how patients automatically match and consciously interpret changes from their normal physical self to beliefs that they may be acutely or chronically ill, or merely tired or out of sorts. (Leventhal, et al., 2011; McAndrew, et al., 2008) The interpretive process creates expectations about the likely duration of the current state, its consequences for daily activities, and motivates action to return to normal; e.g., take a home remedy, seek care. The dramatic changes (e.g., in shape and weight, etc.) that occur postpartum, can encourage a mother to see herself in her normal pre-pregnant state, a perception that will create unrealistic expectations as to how she should feel and how quickly she should fully recover. These perceptions can encourage premature efforts to return to pre-pregnancy levels of activity and failure to meet expectations can create depressive symptoms. Our behavioral educational intervention was designed to address these potentially modifiable interpretations. It did so by preparing mothers to interpret and normalize triggers of depressive symptoms (e.g., vaginal bleeding, breast pain, etc.), and specified the need to bolster social support and conserve personal resources. Specific, simple actions were suggested to address each of these issues, e.g., symptoms and social needs, realistic time frames were provided for return to normal, and resources were listed in the event problems exceeded specified time lines.
The in-hospital component of the two-step intervention involved a 15-minute, in hospital review of a patient education pamphlet and partner summary sheet by the mother with a masters-trained social worker. The patient education pamphlet described common postpartum physical symptoms, depression, infant colic, and the importance of social support. The partner summary sheet described symptoms of depression, danger signs, and gave partner suggestions of ways to help new moms. The second component of the intervention was a two-week post delivery call in which the social worker assessed patients’ symptoms, skills in symptom management, and other needs. Fidelity of the intervention was maintained by repeated training and review of scripts for both the in-hospital and telephone components of the intervention. Approximately 5% of both in-hospital sessions and two-week telephone needs assessments were observed by a physician or project manager on the team. A co-investigator or project manager shadowed each social worker, completed a intervention monitoring instrument, and shared the results of the assessment with the social worker and investigative team.
Enhanced usual care patients received routine postpartum hospital education, (i.e. discharge materials, television educational programs on infant care, breastfeeding, and peripartum care). To insure equivalent contact, patients assigned to enhanced usual care received a two-week post delivery call to inform them of future surveys and a list of health-related and community resources was mailed to them. The intervention materials were modified to represent white and Asian mothers but were identical in content and based on the same theoretical model.(Howell, et al., 2012) All materials were written at a 6th grade reading level and included pictorials. Interviewers were blinded to study arm assignment. All study participants were interviewed by phone at 3-weeks (mean days = 27.2, SD 5.6; median days = 26, range of 17 to 52), 3-months (mean days = 84.3, SD 7.9; median days = 81, range of 76 to 124) and at 6-months (mean days = 175.5, SD 8.7; median days = 174, range of 162 to 218) to assess depressive symptoms and contributing and buffering factors.
Outcome variable
Postnatal depressive symptoms were assessed using the 10-item Edinburgh Postnatal Depression Scale (EPDS). The EPDS is a commonly used postpartum depression screening instrument and has been validated in many postpartum populations and different languages.(Areis et al., 1996; Boyce et al., 1993; Carpiniello et al., 1997; Cox et al., 1987; Eberhard-Gran et al., 2001; Eberhard-Gran et al., 2001; Ghubash et al., 1997; Harris et al., 1989; Jadresic et al., 1995; Lawrie et al., 1998; Lundh, et al., 1993; Murray et al., 1990; Wickberg et al., 1996; Zelkowitz et al., 1995) The recommended cut-off score of ≥10 has sensitivities of 0.59–0.81 and specificities ranged from 0.77–0.88 for major and minor depression.(Gaynes, et al., 2005) The Patient Health Questionnaire-9 (PHQ-9) was also administered and a comparison was made between the EPDS and PHQ-9 scores over time in a secondary analysis. Women reporting high levels of depressive symptoms (EPDS >13 or PHQ-9 ≥20 or suicidal ideation) at any of the four assessments were referred for psychiatric assessment and possible treatment. They were retained in the study.
Survey items also included questions on sociodemographics, clinical characteristics such as antepartum complications, comorbid conditions (e.g. diabetes, hypertension, asthma, thyroid disease, heart disease), past depression history, anxiety, social support, and healthcare factors. Medical charts were reviewed for parity, delivery type, insurance, past medical history, maternal complications, delivery complications, and infant outcomes.
Sample size was powered to detect a clinically meaningful difference in reduction of symptoms of postpartum depression 3 weeks post randomization for women in the intervention arm in comparison with women in enhanced usual care. Assuming that 34% of white and (non-black and non-Latina) women would report depressive symptoms (EPDS≥10) in enhanced usual care (based on our prior research),(Howell, et al., 2006) our recruitment target of 492 patients (246 per arm) met 90% power based on a two-sided 0.05 level chi-squared test to detect a clinically meaningful 13% reduction in depressive symptoms (from 34% to 21%, a relative risk reduction of about 33%). To allow for decreased power due to patient loss at follow-up we planned to enroll 540 participants.
Data Analysis
Data were collected in-person at baseline and by telephone during follow-up interviews by clinical research coordinators blinded to intervention status. Participants in the intervention arm (N=270) and enhanced usual care (N=270) were compared at baseline on demographic and clinical characteristics using t-tests and their non-parametric equivalents, chi-square tests, as appropriate. Group differences were summarized by 95% confidence interval estimates. Overall study attrition rate was low and equivalent across treatment groups. The amount of missing data for our primary outcome measure, EPDS, was low at 3-weeks (7%; 40/540), 3-months (14%; 73/540) and six months (13%; 72/540), and similar between groups at each time point. The primary analysis examined the efficacy of the intervention in reducing the likelihood of positive postpartum depression screens. Logistic regression analyses tested the effect of the intervention on positive depression screens at 3 weeks, 3 months, and 6 months postpartum. To assess change over time across groups for the primary outcome, Generalized Estimating Equations (GEEs), a widely used method for analyzing correlated, longitudinal outcome data with statistical accuracy, were employed.(Zeger et al., 1986) Significance level of 0.05 was used for the primary outcome of postpartum depression and the final model was adjusted for baseline depression screen.
Results
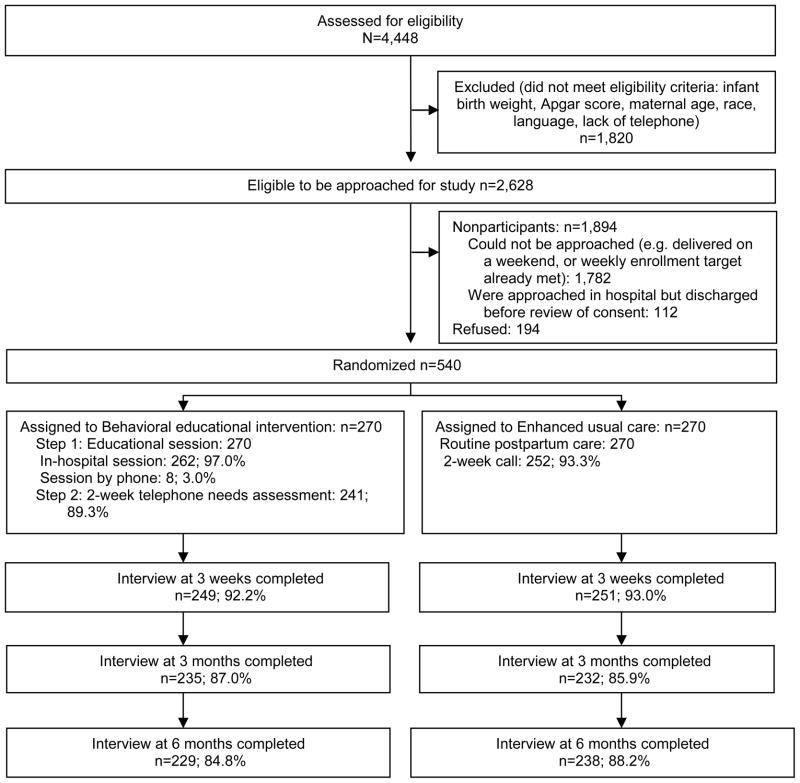
There were 4,448 deliveries over the study period and 2,628 met the initial eligibility criteria (i.e. were ≥18, etc). A random sample of 734 (28%) of the 2628 eligible mothers were approached in hospital and reviewed the study consent form. Of the 734 mothers, 540 (73.6%) completed the consent process and were enrolled in the trial; 194 (26.4%) had declined participation. (Figure 1) Mothers who declined to participate were slightly younger than mothers who consented (mean age of 32 vs. 33; p<.05). Of the 270 mothers randomized to the intervention arm, 262 received the intervention in hospital. Eight mothers were discharged before the social worker could meet with them. Those 8 patients were sent the education materials and the social worker reviewed the educational materials over the phone. Eighty-nine percent (241/270) of the intervention group and 93% (252/270) of the control group were successfully reached for the 2-week calls. Of the 540 enrolled patients, 16 patients withdrew over the 6-month study period. Completion rates for the follow-up interviews were 93% (500/540) at 3-weeks, 86% (467/540) at 3-months, and 86% (467/540) at 6-months. Follow-up was equivalent for intervention and control at 3-weeks (92.2% vs. 93.0%, p=.74), at 3-months (87.0% vs. 85.9%, p=.71) and at 6-months postpartum (84.8% vs. 88.2%, p=.26). There were baseline differences in rates of positive depression screens between women lost to follow-up verses those included in the analyses at 3-weeks: 30% (12/40) lost to follow-up at 3- weeks screened positive versus 11% (57/500) who completed the 3- week survey.
Figure 1.
Participants’ flow through study
The overall mean age of enrolled participants was 33 (range 18–48); 89% were white, 9% were Asian, 2.4% had Medicaid insurance, 11% earned ≤ $30,000 annually, and 24% were foreign born. Baseline characteristics of the intervention and control groups are described in Table 1. There were no clinically important differences between the two groups at baseline. The mean EPDS scores at baseline were 4.0 (SD 4.0; range 0–22) in the intervention group and 5.0 (SD 4.0; range 0–19) in the control group.
Table 1.
Demographic and Clinical Characteristics of Trial Participants
| Behavioral Educational Intervention (N=270) | Enhanced Usual Care (N=270) | P value | |
|---|---|---|---|
| Demographic Characteristics | |||
| Age, mean (SD), y | 33 (6) | 32 (5) | 0.12 |
| Race, No. (%) | |||
| Non-Hispanic White or Caucasian | 233 (86) | 246 (91) | 0.17 |
| Asian | 30 (11) | 21 (8) | |
| Other | 7 (3) | 3 (1) | |
| Birthplace, No. (%) | 0.27 | ||
| US Born | 199 (74) | 210 (78) | |
| Foreign Born | 71 (26) | 60 (22) | |
| Language, No. (%) | |||
| English | 270 (100) | 270 (100) | |
| Education, No. (%) | 0.23 | ||
| High School or less | 34 (13) | 44 (16) | |
| Some college or more | 235 (87) | 226 (84) | |
| Insurance, No. (%) | 0.78 | ||
| Medicaid/Medicaid Managed Care | 8 (3) | 6 (2) | |
| Private/Other | 262 (97) | 263 (98) | |
| Marital Status, No. (%) | 0.13 | ||
| Single/Separated/Divorced/Widowed | 8 (3) | 3 (1) | |
| Married/Living as if Married | 262 (97) | 267 (99) | |
| Parity, No. (%) | 0.46 | ||
| Primiparous | 129 (49) | 122 (46) | |
| Multiparous | 135 (51) | 145 (54) | |
| Breastfeeding, No. (%) | 0.01 | ||
| Yes | 257 (95) | 241 (89) | |
| No | 13 (5) | 29 (11) | |
| Clinical Characteristics | |||
| Delivery Type, No. (%) | 0.02 | ||
| C-Section | 90 (34) | 65 (24) | |
| Vaginal Delivery | 178 (66) | 203 (76) | |
| Comorbid Condition, No. (%) | 0.71 | ||
| Yes | 33 (12) | 36 (13) | |
| No | 234 (88) | 232 (87) | |
| Antepartum Complication, No. (%) | 0.36 | ||
| Yes | 58 (21) | 49 (22) | |
| No | 212 (79) | 218 (82) | |
| Past History of Depression, No. (%) | 0.25 | ||
| Yes | 65 (24) | 54 (20) | |
| No | 205 (76) | 216 (80) | |
| Treatment for Depression (medication or therapy/counseling) this Pregnancy, No. (%) | |||
| Yes | 14 (5) | 21 (8) | 0.22 |
| No | 256 (95) | 249 (92) | |
| Positive Baseline Depression Screen (EPDS≥10), No. (%) | 0.37 | ||
| Yes | 31 (11) | 38 (14) | |
| No | 239 (89) | 232 (86) |
In the intention-to-treat analysis (N=540) there was no difference in positive depression screens among mothers in the intervention arm versus those in the control arm: at 3 weeks 6.0% (15/249) vs. 5.6% (14/251), p=.83 respectively; at 3-months 5.1% (12/235) vs. 6.5% (15/232), p=.53 respectively; and at 6-months 3.5% (8/230) vs. 4.6% (11/238), p=.53 respectively. To assess change over time across groups for the primary outcome, we employed generalized estimating equations. An intention-to-treat generalized estimated equation model, for up to six months of follow-up found no differences in rates of depressive symptoms among intervention versus control (OR of 0.97; 95% CI: 0.59–1.61). The time effect and interaction were not significant. Posthoc subgroup analyses examined whether the intervention was more effective among the subgroup of mothers with a high school education or less. There was no difference in positive depression screens among mothers in the intervention arm versus those in the control arm in this subgroup analysis.
Discussion
Our behavioral educational intervention aimed at addressing modifiable factors associated with postpartum depressive symptoms did not and essentially could not reduce depressive symptoms among 540 postpartum mothers as rates of depressive symptoms were low at baseline and subsequent time points among this population of highly educated mostly white women. Our results contrast with the results of our trial recruiting black and Latina mothers (which used the same recruitment strategy and methodologies), in which the odds of a positive depression screen were reduced by 33% for up to six-months of follow-up for mothers randomized to the intervention arm as compared with the control arm. (Howell, et al., 2012)
The results of both of our trials suggest that this intervention may be successful in reducing racial/ethnic disparities in rates of depressive symptoms postpartum. In the trial with black and Latina mothers, the behavioral education intervention successfully lowered the risk of a positive depression screen to roughly the same frequency as the overall rates for white and Asian mothers in the current trial. Rates of depressive symptoms in the intervention group of black and Latina mothers compared with combined rates in the current trial were similar: at 3 weeks 8.8% vs. 5.8% respectively, p=0.43, at 3-months 8.4% vs. 5.8% respectively, p =0.44,. and at 6-months 8.9% vs. 4.0% respectively, p=0.53. By targeting modifiable factors, the intervention helped black and Latina mothers buffer symptoms of depression.
An expanding body of research has documented the association between potentially modifiable factors and postpartum depressive symptoms. For example, postpartum depressive symptoms are associated with physical symptoms (vaginal bleeding; breast pain; etc.), physical functioning, infant colic, and low levels of social support.(Howell et al, 2005; Howell et al., 2009; Howell et al., 2006) Our intervention aimed to prepare and educate mothers about the postpartum experience, to normalize symptoms and other experiences, to provide specific, concrete suggestions for coping with realistic time frames for observing benefits, to bolster personal and social resources, and to better manage postpartum demands. We hypothesize that the intervention likely worked among low-income black and Latina women because the prevalence of their depressive symptoms was higher at baseline and many may have lacked the tools and support necessary to manage postpartum stressors. Providing tools and resources to low-income minority mothers, who are at highest risk of postpartum depressive symptoms, has the potential to lower the burden of depressive symptoms and place them at similar risk as higher-income majority women.
Studies do suggest that interventions selectively targeting women at elevated risk for postpartum depression, may be more effective than universal interventions aimed at preventing postpartum depression. (Dennis, et al., 2013) However there is little consistency in the identification of women “at risk” and a review of 16 antenatal screening tools suggests that there are no measures with acceptable predictive validity to accurately identify asymptomatic women who will later develop postpartum depression.(Austin, et al. 2003). For this trial, we chose to include women regardless of their baseline depressive symptom score, a universal approach that is simple, because we expected much higher rates of depressive symptoms in our participants.
The rates of depressive symptoms in our cohort were lower than previously published literature including those assessed in our prior longitudinal studies.(Howell, et al., 2005) Over the last decade public awareness for postpartum depression has risen and numerous education campaigns on this topic may have impacted prevalence rates of depressive symptoms at our hospital and in the region. The base rates of depressive symptoms were roughly 20% lower both in the current study and in the successful trial with black and Latina mothers. As behaviors, both symptomatic and non, e.g., adherence, are triggered and moderated by many factors, there are multiple pathways for changing behavior outside the framework of a clinical trial. A number of high profile public awareness campaigns and legislative initiatives aimed at educating women about postpartum depression were put into place in the period between 2002 and 2009.(Postpartum Support International) It is possible that these initiatives and the longitudinal studies conducted in our setting, interacted to generate alternative pathways that normalized and de-stigmatized postpartum depression. Research on public service mental health campaigns have been found to be effective in engendering greater awareness, positive changes in attitudes regarding depression, attitudes toward antidepressants, and to a certain extent treatment seeking behavior.(Paykel et al., 1998)
There were a number of limitations with this trial. First, the rate of positive depressive symptom screens was much lower than previously published rates. It is possible that women with depressive symptoms were less likely to enroll in our randomized controlled trial. However our refusal rate was low. In addition, the low prevalence of depressive symptoms limited the power of this study to detect a difference in rates of depressive symptoms between the intervention and control arms in this trial. This study was powered to intervene on base rates of postpartum depressive symptoms detected in prior longitudinal studies in this same catchment area. The results of this negative trial highlight the importance of monitoring ongoing rates of depressive symptoms, the focus of this behavioral intervention. Second, women with positive depression screens were more likely to be lost to follow-up at 3-weeks. However, the overall rate of positive depression screens was low and only 12 women who screened positive for depression at baseline were lost to follow-up at 3-weeks. Third, we used a depression screening instrument rather than a formal structured interview to diagnose depression. Our intervention was implemented in an obstetrics setting where formal assessments are often too burdensome to perform. Further, positive screens for depression, whether or not they are associated with diagnosis of major depressive disorder are an important measure to assess as they are associated with multiple negative outcomes for mothers and infants. (Zayas et al., 2002; Beeghly et al., 2003; Dennis et al., 2005; McLearn et al., 2006). And finally, this trial was implemented at one institution and the majority of the patients were educated and white which limits the generalizability of our results.
We found that a behavioral education intervention did not reduce postpartum depressive symptoms among a sample of highly educated and predominantly white mothers because their prevalence of depressive symptoms was low. In contrast, the intervention was successful in reducing depressive symptoms among postpartum black and Latina mothers. Postpartum depressive symptoms affect women from all racial/ethnic and socioeconomic backgrounds but are more burdensome for low-income women of color who often have fewer resources available to them and less access to treatment. This simple, low cost intervention appears to be of benefit for low-income women of color and may help address early modifiable factors associated with depressive symptoms. It remains to be demonstrated whether the intervention will prove equally beneficial for a sample of white, non-Latino women reporting higher rates of depressive symptoms.
Acknowledgments
Supported by the National Institute of Mental Health (5R01MH77683) and the National Institute on Minority Health and Health Disparities (5P60MD000270).
Footnotes
Clinical Trial Registration: Clinicaltrials.gov, www.clinicaltrials.gov, NCT00951717
References
- Areias ME, Kumar R, Barros H, Figueiredo E. Comparative incidence of depression in women and men, during pregnancy and after childbirth. Validation of the Edinburgh Postnatal Depression Scale in Portuguese mothers. Br J Psychiatry. 1996;169(1):30–35. doi: 10.1192/bjp.169.1.30. [DOI] [PubMed] [Google Scholar]
- Austin M, Lumley J. Antenatal screening for postnataldepression: a systematic review. Acta Psychiatrica Scandinavica. 2003;107:10–7. doi: 10.1034/j.1600-0447.2003.02024.x. [DOI] [PubMed] [Google Scholar]
- Beeghly M, Olson KL, Weinberg MK, Pierre SC, Downey N, Tronick EZ. Prevalence, stability, and socio-demographic correlates of depressive symptoms in Black mothers during the first 18 months postpartum. Matern Child Health J. 2003;7(3):157–168. doi: 10.1023/a:1025132320321. [DOI] [PubMed] [Google Scholar]
- Boyce P, Stubbs J, Todd A. The Edinburgh Postnatal Depression Scale: validation for an Australian sample. Aust N Z J Psychiatry. 1993;27(3):472–476. doi: 10.3109/00048679309075805. [DOI] [PubMed] [Google Scholar]
- Carpiniello B, Pariante CM, Serri F, Costa G, Carta MG. Validation of the Edinburgh Postnatal Depression Scale in Italy. J Psychosom Obstet Gynaecol. 1997;18(4):280–285. doi: 10.3109/01674829709080700. [DOI] [PubMed] [Google Scholar]
- Dennis CL, Doswell T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev. 2013 Feb;28;2:CD001134. doi: 10.1002/14651858.CD001134.pub3. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dennis CL, Ross L. Relationships among infant sleep patterns, maternal fatigue, and development of depressive symptomatology. Birth. 2005;32(3):187–193. doi: 10.1111/j.0730-7659.2005.00368.x. [DOI] [PubMed] [Google Scholar]
- Duer S, Schwenk TL, Coyne JC. Medical and psychosocial correlates of self-reported depressive symptoms in family practice. J Fam Pract. 1988;27(6):609–614. [PubMed] [Google Scholar]
- Eberhard-Gran M, Eskild A, Tambs K, Opjordsmoen S, Samuelsen SO. Review of validation studies of the Edinburgh Postnatal Depression Scale. Acta Psychiatr Scand. 2001;104(4):243–249. doi: 10.1034/j.1600-0447.2001.00187.x. [DOI] [PubMed] [Google Scholar]
- Eberhard-Gran M, Eskild A, Tambs K, Schei B, Opjordsmoen S. The Edinburgh Postnatal Depression Scale: validation in a Norwegian community sample. Nord J Psychiatry. 2001;55(2):113–117. doi: 10.1080/08039480151108525. [DOI] [PubMed] [Google Scholar]
- Gaynes BN, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Brody S, Miller WC. Perinatal Depression: Prevalence, Screening Accuracy, and Screening Outcomes. February 2005; Paper presented at the AHRQ Publication No. 05-E006-2; Rockville. 2005. [Google Scholar]
- Ghubash R, Abou-Saleh MT, Daradkeh TK. The validity of the Arabic Edinburgh Postnatal Depression Scale. Soc Psychiatry Psychiatr Epidemiol. 1997;32(8):474–476. doi: 10.1007/BF00789142. [DOI] [PubMed] [Google Scholar]
- Harris B, Huckle P, Thomas R, Johns S, Fung H. The use of rating scales to identify post-natal depression. Br J Psychiatry. 1989;154:813–817. doi: 10.1192/bjp.154.6.813. [DOI] [PubMed] [Google Scholar]
- Herrera E, Reissland N, Shepherd J. Maternal touch and maternal child-directed speech: effects of depressed mood in the postnatal period. J Affect Disord. 2004;81(1):29–39. doi: 10.1016/j.jad.2003.07.001. [DOI] [PubMed] [Google Scholar]
- Howell EA, Balbierz A, Wang J, Parides M, Zlotnick C, Leventhal H. Reducing postpartum depressive symptoms among black and latina mothers: a randomized controlled trial. Obstet Gynecol. 2012;119(5):942–949. doi: 10.1097/AOG.0b013e318250ba48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell EA, Mora PA, Chassin MR, Leventhal H. Lack of preparation, physical health after childbirth, and early postpartum depressive symptoms. J Womens Health (Larchmt) 2010;19(4):703–708. doi: 10.1089/jwh.2008.1338. [DOI] [PubMed] [Google Scholar]
- Howell EA, Mora PA, DiBonaventura MD, Leventhal H. Modifiable factors associated with changes in postpartum depressive symptoms. Arch Womens Ment Health. 2009;12(2):113–120. doi: 10.1007/s00737-009-0056-7. [DOI] [PubMed] [Google Scholar]
- Howell EA, Mora PA, Horowitz CR, Leventhal H. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstet Gynecol. 2005;105(6):1442–1450. doi: 10.1097/01.AOG.0000164050.34126.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell EA, Mora P, Leventhal H. Correlates of early postpartum depressive symptoms. Matern Child Health J. 2006;10(2):149–157. doi: 10.1007/s10995-006-0116-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jadresic E, Araya R, Jara C. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Chilean postpartum women. J Psychosom Obstet Gynaecol. 1995;16(4):187–191. doi: 10.3109/01674829509024468. [DOI] [PubMed] [Google Scholar]
- Josefsson A, Angelsioo L, Berg G, Ekstrom CM, Gunnervik C, Nordin C, Sydsjo G. Obstetric, somatic, and demographic risk factors for postpartum depressive symptoms. Obstet Gynecol. 2002;99(2):223–228. doi: 10.1016/s0029-7844(01)01722-7. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74(1):5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Lawrie TA, Hofmeyr GJ, de Jager M, Berk M. Validation of the Edinburgh Postnatal Depression Scale on a cohort of South African women. S Afr Med J. 1998;88(10):1340–1344. [PubMed] [Google Scholar]
- Leventhal H, Bodnar-Deren S, Breland JY, Hash-Converse J, Phillips LA, Leventhal EA, Cameron LD. Modeling health and illness behavior: The approach of the commonsense model. In: Baum A, Revenson TA, Singer J, editors. Handbook of Health Psychology. 2. Psychology Press; 2011. pp. 3–35. [Google Scholar]
- Lundh W, Gyllang C. Use of the Edinburgh Postnatal Depression Scale in some Swedish child health care centres. Scand J Caring Sci. 1993;7(3):149–154. doi: 10.1111/j.1471-6712.1993.tb00190.x. [DOI] [PubMed] [Google Scholar]
- Matthey S, Barnett B, Ungerer J, Waters B. Paternal and maternal depressed mood during the transition to parenthood. J Affect Disord. 2000;60(2):75–85. doi: 10.1016/s0165-0327(99)00159-7. [DOI] [PubMed] [Google Scholar]
- McAndrew LM, Musumeci-Szabo TJ, Mora PA, Vileikyte L, Burns E, Halm EA, Leventhal EA, Leventhal H. Using the common sense model to design interventions for the prevention and management of chronic illness threats: from description to process. Br J Health Psychol. 2008;13:195–204. doi: 10.1348/135910708X295604. [DOI] [PubMed] [Google Scholar]
- McLearn KT, Minkovitz CS, Strobino DM, Marks E, Hou W. Maternal depressive symptoms at 2 to 4 months post partum and early parenting practices. Arch Pediatr Adolesc Med. 2006;160(3):279–284. doi: 10.1001/archpedi.160.3.279. [DOI] [PubMed] [Google Scholar]
- Minkovitz CS, Strobino D, Scharfstein D, Hou W, Miller T, Mistry KB, Swartz K. Maternal depressive symptoms and children’s receipt of health care in the first 3 years of life. Pediatrics. 2005;115(2):306–314. doi: 10.1542/peds.2004-0341. [DOI] [PubMed] [Google Scholar]
- Murray L, Carothers AD. The validation of the Edinburgh Post-natal Depression Scale on a community sample. Br J Psychiatry. 1990;157:288–290. doi: 10.1192/bjp.157.2.288. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Hart D, Priest RG. Changes in public attitudes to depression during the Defeat Depression Campaign. Br J Psychiatry. 1998;173:519–522. doi: 10.1192/bjp.173.6.519. [DOI] [PubMed] [Google Scholar]
- Postpartum Support International. US State Legislation. Retrieved May 8, 2012, from http://www.postpartum.net/News-and-Events/Legislation.aspx.
- Seguin L, Potvin L, St-Denis M, Loiselle J. Depressive symptoms in the late postpartum among low socioeconomic status women. Birth. 1999;26(3):157–163. doi: 10.1046/j.1523-536x.1999.00157.x. [DOI] [PubMed] [Google Scholar]
- Vera M, Alegria M, Freeman D, Robles RR, Rios R, Rios CF. Depressive Symptoms among Puerto Ricans: Island Poor Compared with Residents of the New York City Area. Am J Epidemiol. 1991;134(5):502–510. doi: 10.1093/oxfordjournals.aje.a116122. [DOI] [PubMed] [Google Scholar]
- Wickberg B, Hwang CP. The Edinburgh Postnatal Depression Scale: validation on a Swedish community sample. Acta Psychiatr Scand. 1996;94(3):181–184. doi: 10.1111/j.1600-0447.1996.tb09845.x. [DOI] [PubMed] [Google Scholar]
- Zayas LH, Cunningham M, McKee MD, Jankowski KR. Depression and Negative Life Events Among Pregnant African-American and Hispanic Women. Women’s Health Issues. 2002;12(1):16–21. doi: 10.1016/s1049-3867(01)00138-4. [DOI] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- Zelkowitz P, Milet TH. Screening for post-partum depression in a community sample. Can J Psychiatry. 1995;40(2):80–86. doi: 10.1177/070674379504000205. [DOI] [PubMed] [Google Scholar]